Abstract
Objective
To assess the effects of two different nutritional mode on the occurrence of ventilator-associated pneumonia (VAP) in patients on mechanical ventilation.
Methods
70 patients admitted to the ICU and under mechanical ventilation, were randomly divided into the nasointestinal tube group and nasogastric tube group. Patients from both groups received enteral nutrition, using the same nutritional agent, through intubation. The duration of stay in the ICU, duration of mechanical ventilation, incidence of VAP, nutritional state, and survival of the intestinal tract were compared between the two groups.
Results
The duration of stay in the ICU, duration of mechanical ventilation and incidence of VAP in the nasointestinal tube group was lower than that in the nasogastric tube group (P<0.05). There was an increase in the levels of prealbumin and transferrin in the nasointestinal tube group (P<0.05). However, there were no obvious difference in the nasogastric tube group (P<0.05). The incidence of abdominal distension, diarrhea, regurgitation, aspiration, and hyperglycemia in the nasointestinal tube group was much lower than that in the nasogastric tube group (P < 0.05).
Conclusion
This study showed that enteral nutrition delivery using a nasointestinal way can effectively reduce the incidence of VAP and improve the nutritional status of patients under mechanical ventilation.
Keywords: Ventilator associated pneumonia, Nasogastric nutrition, Nasointestinal nutrition, Mechanical ventilation
1. Introduction
Nosocomial pneumonia is the second most prevalent nosocomial infection in hospital in-patients, with ventilator-associated pneumonia (VAP) being the leading nosocomial infection in patients admitted to the intensive care unit (ICU). Studies have shown that the incidence of VAP in mechanically ventilated patients is between 9% and 69%, which is four times higher than that in patients admitted to the normal ward [1]. VAP can significantly extend the duration of mechanical ventilation, is associated with increased morbidity and mortality, consumes large amounts of health care resources, and increases social and economic burden [2]. Although significant progress has been made over the past two decades in the management of VAP, several issues remain unresolved, and mortality rates continue to be high at 30-40% [3]. Therefore, VAP continues to be a disturbing problem in the care of ICU-patients under mechanical ventilation. Enteral nutrition is an important part of the treatment in patients on ventilation, and can improve the nutritional status and immune function in critically ill patients. It is also an important factor in the prevention of the occurrence of VAP. There exists a close relationship between the mode of delivery of enteral nutrition and the occurrence of VAP. Oropharyngeal secretions or reflux and aspiration of gastric contents are considered important factors in the occurrence of VAP [4]. Though numerous studies have focused on the diagnosis and treatment of VAP, few have focused on identifying routes of nutrient administration that can reduce the incidence of VAP. Therefore, the primary objective of this study was to confirm the possible differences in the incidence of VAP resulting from the use of nasogastric and nasointestinal tubes for nutrition delivery in patients under mechanical ventilation. We further aimed to determine the effectiveness of each of these nutritional delivery methods in reducing the incidence of VAP and mortality.
2. Materials and methods
2.1. Criteria for case selection
VAP refers to pneumonia that occurs more than 48-72 hours after intubation with no evidence of pneumonia at the time of intubation, or the diagnosis of a new pulmonary infection if the initial ICU admission was for pneumonia. Early-onset VAP is defined as the onset of VAP after 48 h but before 5 days after intubation. Late-onset VAP is defined as the onset of VAP 5 days after intubation [5].
2.2. Methods
70 patients (42 men, 28 women, age: 52.9 ± 12.4 years, range: 35-70 years) admitted to the ICU of our hospital between January 2016 and November 2017 and who were under mechanical ventilation for more than 48 h were included in this study. The patients suffered from traumatic brain injury (22 cases), heart disease (18 cases), multiple severe combined injuries (9 cases), respiratory failure (8 cases), cerebral hemorrhage (5 cases), neoplastic disease (4 cases), and other diseases (4 cases). Signed informed consent, on behalf of the patients, was obtained from the family members. Based on the hospital admission identification number and using a pseudo-random number table, the 70 patients were randomly and equally divided into two groups: the nasointestinal and the nasogastric groups. There were no statistically significant differences between the two groups with respect to gender, age, underlying disease, severity, etc. (P> 0.05).
The enteral nutrition administered to the patients was produced by KangYuan (Beijing) Technology Co., Ltd. The quantity of nutrition administered to the patients was calculated based on the standard formula of 100 kJ.kg-1.d-1. Enteral nutrition was delivered using a pump system. Nasointestinal tube was placed into the descending part of duodenum and the nasogastric tube was placed at the fundus of the stomach. The nutrient was delivered at a rate of 20 ml.kg-1.d-1, six times a day. The maximum drip rate was never more than 125 ml/h.
Ethical approval: The research related to human use has been complied with all the relevant national regulations, institutional policies and in accordance the tenets of the Helsinki Declaration, and has been approved by the authors’ institutional review board or equivalent committee.
2.3. Statistical analysis
All recorded data and results are expressed as mean ± SD, median (interquartile range). P value <0.05 is considered significant. Statistical analyses were conducted using SPSS version 19.0 software. An independent sample t test was used to compare the data between the two groups. The count data between the two groups were compared using the χ2 test. Logistic regression analysis was used to evaluate the correlation between the two sets of data.
3. Results
3.1. Baseline characteristics of patients from the nasogastric tube and nasointestinal tube groups (Table 1)
Table 1.
Baseline characteristics of patients
| Nasogastric group | Nasointestinal group | P value | |
|---|---|---|---|
| Gender (M/F) | 22/13 | 20/15 | 0.625 |
| Age (years) | 54.1±12.1 | 51.7±12.7 | 0.415 |
| Basic disease | |||
| Brain Injury | 9 | 13 | 0.302 |
| Heart disease | 11 | 7 | 0.272 |
| Complex trauma | 6 | 3 | 0.280 |
| Respiratory failure | 5 | 3 | 0.450 |
| Cerebral hemorrhage | 2 | 3 | 0.642 |
| Malignant | 1 | 3 | 0.293 |
| Other diseases | 1 | 3 | 0.293 |
| APACHE* score | 17.8 ± 1.3 | 18.1 ± 1.3 | 0.404 |
*APACHE: Acute physiology and chronic health evaluation
There were no significant differences in the basic characteristics of the two groups of patients included in the study.
3.2. Comparative analysis of mechanical ventilation and VAP incidence
The durations of ICU stay and mechanical ventilation were lower for the nasointestinal tube group than for the nasogastric tube group (P=0.036, Figure 1a). The incidence of VAP was significantly lower for the nasointestinal tube group than for the nasogastric tube group (P=0.018, Figure 1b).
Figure 1.
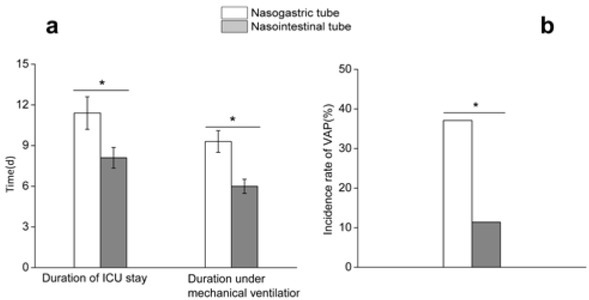
The durations of ICU stay and mechanical ventilation in the nasointestinal tube group were shorter than that in the nasogastric tube group(Fig 1a). The incidence of VAP were significantly lower for the nasointestinal tube group than for the nasogastric tube group (Fig 1b).
3.3. Comparative analysis of nutritional status
An increase in the levels of prealbumin and transferrin was observed in both the groups after the administration of enteral nutrition. At the same time, the levels of prealbumin and transferrin in the nasointestinal tube group were higher after reception of enteral nutrition than before (P = 0.038, Figure 2a). However, there was no significant difference of the level of prealbumin and transferrin in the nasogastric tube group before reception of enteral nutrition and after it respectively (P=0.061, Figure 2 b).
Figure 2.
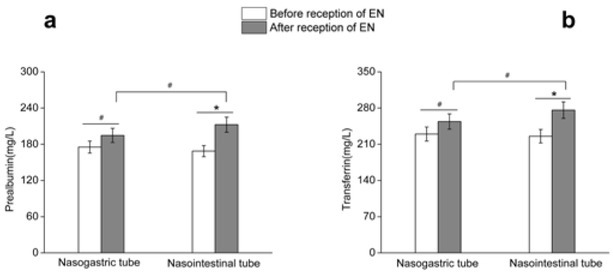
The level of prealbumin and transferrin increased in both groups after the administration of enteral nutrition. There was an increase in the levels of prealbumin and transferrin in the nasointestinal tube group(Fig 2a). However, there were no obvious difference in the nasogastric tube group (Fig 2b).
3.4. Analysis of intestinal tolerance
The incidence of bloating & diarrhea, reflux, aspiration, and hyperglycemia in the nasointestinal tube group was significantly lower than that in the nasogastric tube group (P < 0.05, Figure 3).
Figure 3.
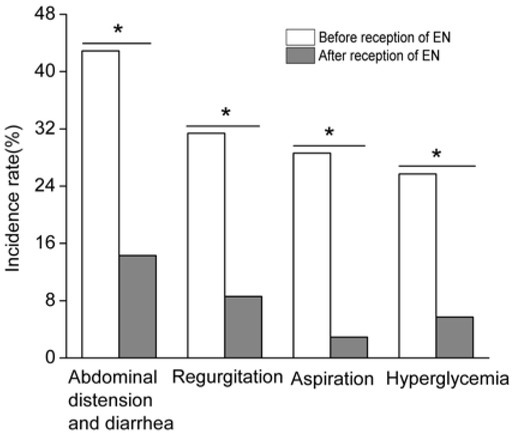
The incidence of bloating & diarrhea, reflux, aspiration, and hyperglycemia in the nasointestinal tube group was significantly lower than that in the nasogastric tube group.
3.5. Incidence of aspiration and VAP
Of the 70 patients from the study, aspiration occurred in 11 patients and VAP in 17 patients. The incidence of VAP in patients with aspiration was significantly higher than that in patients without aspiration. This implies that aspiration can induce VAP. A significant correlation was observed between aspiration and VAP. Logistic regression analysis showed the aspiration rate to be a factor of VAP (B = 1.656, p = 0.017); the relative ratio was 5.236. (Table 2)
Table 2.
Incidence of aspiration and VAP
| Group | VVAP incidence | VAP number | χ2 | P | |
|---|---|---|---|---|---|
| Aspiration | Yes(11) | 54.5% | 6 | 5.691 | 0.017 |
| No(59) | 18.6% | 11 |
4. Discussion
VAP is one of the most common complications observed in patients under mechanical ventilation. It has previously been reported that the use of vasoactive drugs, nasogastric nutrition, and duration of mechanical ventilation are important causes of VAP [6]. Previously, a large number of clinical studies have focused on the diagnosis and treatment of VAP. Few studies have focused on methods to reduce the incidence of VAP by changing the route of administration of nutrients in mechanically ventilated patients.
Malnutrition and low immunity are the most common complications in critically ill patients admitted to the ICU. Mechanical ventilation increases the nutrient consumption, which leads to disease progression and further infection. Therefore, in terms of management of the disease, nutritional support is a key issue. On one hand, it can reduce the decomposition of protein and increase protein synthesis, which increases the potential and occurrence of malnutrition. On the other hand, a good nutritional status helps to increase immunity and reduce the risk of infection. At present, nasointestinal nutrition and nasogastric nutrition are the most common methods of nutritional support. Previous studies have suggested that an enteral nutrition catheter can directly damage the gastro-esophageal sphincter, lead to regurgitation, and increase the incidence of VAP [7]. At the same time, enteral nutrition increases the possibility of aspiration, and previous studies have shown that enteral nutrition is an independent factor for VAP occurrence [8]. However, there are many benefits associated with enteral nutrition, such as nutrition being absorbed directly. The physiological effects of effective enteral nutrition include improved nutritional status in critically ill patients, protection of the gastrointestinal tract, and prevention of bacterial translocation and multiple organ failure.
However, inappropriate enteral nutrition can lead to VAP, whose mechanisms include reflux of stomach contents, bacterial colonization in the stomach, and shift of the duodenum towards the airways [1,9]. It has been demonstrated that the use of gastric mucosal protective agents that can adjust the stomach pH and prevent reflux of stomach contents is ineffective in the treatment of VAP, while the use of oral antimicrobials can prevent the occurrence of VAP [10]. In addition, positive pressure ventilation changes the chest pressure, and indirectly increases the intra-abdominal pressure, which further increases the chances of gastroesophageal reflux and the risk of VAP [11]. In our study, we observed that there exists an obvious correlation between aspiration and VAP. The incidence of VAP in patients with aspiration is about 5.2-fold higher than that in patients without aspiration. Therefore, an appropriate mode of enteral nutrition can improve the prognosis of critically ill patients. However, the reported study showed that enteral nutrition volume is not correlated with lower respiratory tract infection in patients on mechanical ventilation, which indicated the way of enteral nutrition is more closely related to ventilator-associated pneumonia [12].
A previous study showed that the rate of VAP in patients who were nasoduodenal fed was 10%, whereas the rate of VAP in patients who had nasogastric feeding was 20%, which indicated nasoduodenal feeding helped to reduce the incidence of VAP [13]. Our study shows that, compared to nasogastric enteral nutrition, nasointestinal enteral nutrition can significantly reduce the incidence of intestinal reflux, aspiration, bloating, diarrhea, high blood sugar and other complications, and enhance intestinal tolerability. Nasointestinal enteral nutrition can also significantly improve the levels of plasma prealbumin and transferrin. Prealbumin and transferrin are important indicators used to evaluate the nutritional status of the patient and the effects of nutritional support. Existing literature shows that nasointestinal nutrition can not only
increase the levels of nutrition indicators, such as prealbumin and transferrin, but also reduce the production of inflammatory markers, such as interleukin-6 (IL-6) and tumor necrosis factor (TNF)-α [14].
Our results suggest that nasointestinal nutrition can significantly shorten the ICU stay and duration of mechanical ventilation, as well as reduce the incidence of VAP. The nasogastric nutrient solution can increase the stomach pH, which is conducive to bacterial reproduction, and consequently induce VAP [15]. In addition, nasogastric tubes are more likely to cause reflux and vomiting, which leads to colonization of bacteria in the mouth and reflux of gastric contents into the lungs, and results in VAP. Nasoduodenal feedings achieved nutritional goals earlier than those who received nasogastric feeding, and nasoduodenal feeding group has a lower rate of vomiting and VAP in the medical ICU setting [16].
In summary, nasointestinal nutrition can improve the nutritional status of patients and improve the prognosis of the patients under mechanical ventilation. Furthermore, it can reduce reflux, aspiration, and other adverse reactions, thereby decreasing the incidence of VAP. Therefore, the nasointestinal way is more effective and safer than the nasogastric tube in patients requiring enteral nutrition.
Footnotes
Conflict of interest
Conflict of interest statement: The authors confirm that this article content has no conflict of interests
References
- [1].Fagon JY, Chastre J, Hance AJ. Nosocomial pneumonia in ventilated patients:a cohort study evaluating attributable mortality and hospital stay[J] Am J Med. 1993;94(3):281–288. doi: 10.1016/0002-9343(93)90060-3. [DOI] [PubMed] [Google Scholar]
- [2].De Haan JJ, Thuijls G, Lubbers T. Protection against early intestinal compromise by lipid-rich enteral nutrition through cholecystokinin receptors[J] Critical Care Medicine. 2010;38(7):1592–1597. doi: 10.1097/CCM.0b013e3181e2cd4d. [DOI] [PubMed] [Google Scholar]
- [3].Torres A, Ewig S, Lode H. European HAP working group. Defining, treating and preventing hospital acquired pneumonia: European perspective[J] Intensive Care Med. 2009;35:9–29. doi: 10.1007/s00134-008-1336-9. [DOI] [PubMed] [Google Scholar]
- [4].Singer P, Anbar R, Cohen J. The tight calorie control study ( TICACOS) : a prospective, randomized, controlled pilot study of nutritional support in critically ill patients[J] Intensive Care Med. 2011;37(4):601–609. doi: 10.1007/s00134-011-2146-z. [DOI] [PubMed] [Google Scholar]
- [5].MS Niederman,DE Craven. Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare- associated pneumonia[J] Am J Respir Crit Care Med. 2005;171(4):388– 416. doi: 10.1164/rccm.200405-644ST. [DOI] [PubMed] [Google Scholar]
- [6].Kusahara DM, Enz Cda C, Avelar AF. Risk Factors for Ventilator-Associated Pneumonia in Infants and Children: a Cross- sectional Cohort Study[J] Am J Crit Care. 2014;23(11):469–476. doi: 10.4037/ajcc2014127. [DOI] [PubMed] [Google Scholar]
- [7].Joshi N, Localio AR, Hamory BH. A predictive risk index for nosocomial pneumonia in the intensive care unit[J] Am J Med. 1992;93:135–142. doi: 10.1016/0002-9343(92)90042-a. [DOI] [PubMed] [Google Scholar]
- [8].Doig GS, Heighes PT, Simpson F. Early enteral nutrition reduces mortality in trauma patients requiring intensive care: a meta-analysis of randomised controlled trials[J] Injury. 2011;42(1):50–56. doi: 10.1016/j.injury.2010.06.008. [DOI] [PubMed] [Google Scholar]
- [9].Reignier J, Mercier E, Le Gouge A. Effect of Not Monitoring Residual Gastric Volume on Risk of Ventilator-Associated Pneumonia in Adults Receiving Mechanical Ventilation and Early Enteral Feeding A Randomized Controlled Trial[J] JAMA. 2013;309(3):249–256. doi: 10.1001/jama.2012.196377. [DOI] [PubMed] [Google Scholar]
- [10].Montejo JC, Minambres E, Bordeje L. Gastric residual volume during enteral nutrition in ICU patients: the REGANE study[J] Intensive Care Med. 2010;36(8):1386–1393. doi: 10.1007/s00134-010-1856-y. [DOI] [PubMed] [Google Scholar]
- [11].Heyland DK, Drover JW, MacDonald S. Effect of postpyloric feeding on gastroesophageal regurgitation and pulmonary microaspiration: results of a randomized controlled trial[J] Crit Care Med. 2001;29:1495–1501. doi: 10.1097/00003246-200108000-00001. [DOI] [PubMed] [Google Scholar]
- [12].Colomar A, Guardiola B, Llompart-Pou JA. Enteral nutrition volume is not correlated with lower respiratory tract infection in patients on mechanical ventilation[J] Medicina Intensiva. 2017;41(6):330–338. doi: 10.1016/j.medin.2016.09.009. [DOI] [PubMed] [Google Scholar]
- [13].Sönmez Düzkaya D, Yildiz S. Effect of two different feeding methods on preventing ventilator associated pneumonia in the paediatric intensive care unit (PICU): A randomised controlled study[J] Aust Crit Care. 2016;29(3):139–145. doi: 10.1016/j.aucc.2015.11.001. [DOI] [PubMed] [Google Scholar]
- [14].Bing Wan, Hai-yan Fu, Jiang-tao Yin. Early jejunal feeding by bedside placement of a nasointestinal tube significantly improves nutritional status and reduces complications in critically ill patients versus enteral nutrition by a nasogastric tube[J] Asia Pac Journal Clin Nutr. 2015;24(1):51–57. doi: 10.6133/apjcn.2015.24.1.03. [DOI] [PubMed] [Google Scholar]
- [15].Torres A, El-Ebiary M, Soler N. Stomach as a source of colonization of the respiratory tract during mechanical ventilation: association with ventilator-associated pneumonia[J] Eur Respir J. 1996;9(8):1729–1735. doi: 10.1183/09031936.96.09081729. [DOI] [PubMed] [Google Scholar]
- [16].Hsu CW, Sun SF, Lin SL. Duodenal versus gastric feeding in medical intensive care unit patients: A prospective, randomized, clinical study[J] Critical Care Medicine. 2009;37(6):1866–1872. doi: 10.1097/CCM.0b013e31819ffcda. [DOI] [PubMed] [Google Scholar]


