Abstract
Aim:
To evaluate the shear bond strength and failure mode of total-etch and self-etch bonding agents on human dentin with and without application of 2% chlorhexidine gluconate (CHX).
Materials and Methods:
Eighty extracted premolars were chosen and stored in 10% formalin until use. Samples were mounted in cold cure acrylic resin and the occlusal enamel perpendicular to long axis of each tooth was removed using a low-speed diamond saw under water coolant. The prepared teeth were randomly divided into four groups of 20 samples each according to the adhesive system used. Groups 1 and 2 were the control group in which total-etch and self-etch adhesives were applied as per manufacturer’s instructions, Groups 3 and 4 were the experimental groups in which 2% CHX was applied and blot dried prior to the application of total-etch and self-etch adhesives. A custom-designed rig was fabricated to place composite on samples. The customized rig comprised a cylindrical mold with height of 3 mm and internal diameter of 2.5 mm. Resin was placed in increments of 1 mm and was cured after each increments. After the composite placements, samples were placed in distilled water at 37°C for 24 h. The samples were then thermocycled between 5°C and 55°C in water with a dwell time of 30 s in each temperature to a total of 10,000 cycles. The shear test was performed using universal testing machine and fracture modes were evaluated using stereomicroscope.
Results:
Both the experimental total-etch and self-etch groups showed better shear bond strength than the control groups, which was statistically significant, and also the least mode of failure at the adhesive interface was observed in both the experimental groups.
Conclusion:
2% Chlorhexidine gluconate effectively improved the shear bond strength and helped maintaining the durability of adhesive interface in both total-etch and self-etch adhesives.
KEYWORDS: Chlorhexidine, failure modes, shear bond strength, self-etch, total-etch
INTRODUCTION
Contemporary restorative techniques are based on the adhesive properties of resin-based materials. Following the pioneer approach of Buonocore in 1955, evolution of adhesive techniques has transformed the scope of dental practice over the past two decades.[1]Among the direct tooth-colored restorative materials, resin-based composite provides the best mechanical properties capable of replacing biological tissues in both function and appearance[2] As with other materials, resin-based composite has its own limitations, the most significant problem being durability. Premature loss of bond strength is one of the problems that still affects adhesive restoration and markedly reduces its durability.[3]
In this context, it has been speculated that a decreasing concentration gradient of resin monomer diffusion within the acid-etched dentin and a subsequent resin elution from hydrolytically unstable polymeric hydrogels within the hybrid layers leave the collagen fibrils unprotected and vulnerable to degradation by endogenous matrix metalloproteinases (MMPs).[4]
MMPs are a cell-derived, zinc- and calcium-dependent proteolytic enzyme family, with 26 identified members. They are capable of degrading all extracellular matrix components. Specific enzymes of this family can function beneficially during tissue remodeling and during formation of the extracellular matrix or the mineralization of dentin. Human dentin contains collagenase (MMP-8), gelatinases (MMP-2 and -9), and enamelysin (MMP-20). Dentin collagenolytic and gelatinolytic activities can be suppressed by protease inhibitors, indicating that MMP inhibition could be beneficial in the preservation of hybrid layers[5]
Gendron et al.[6] demonstrated in an in vitro study that application of chlorhexidine is known to have a broad-spectrum MMP-inhibitory effect.
Current adhesive systems commonly used are the total-etch technique or the self-etch technique; hence, our study aimed to evaluate the shear bond strength and mode of failure of total-etch and self-etch bonding agent on human dentin with and without application of 2% chlorhexidine gluconate (CHX).
MATERIALS AND METHODS
For performing this study, 80 sound human premolars extracted for orthodontic treatment were chosen. Teeth with caries, cracks/physiologic wear, restoration, and developmental anomalies were excluded from the study. After extraction, the teeth were rinsed with saline and cleaned with a scalar tip followed by thorough prophylaxis using rubber cup and pumice slurry. Then they were stored in 10% formalin until use. The teeth were mounted in cold-curing acrylic resin. The occlusal enamel of the samples were removed perpendicular to the long axis of each tooth using a low-speed diamond saw (5000 Buehler; Isomet, Lake Bluff, IL) under water coolant to expose the mid-coronal dentin. The prepared teeth were randomly divided into four groups of 20 samples each. In the total-etch control group, 37% phosphoric acid was applied for 15s, acid gel was removed and rinsed for 15s, excess water was removed by blot drying, two consecutive coats of adhesive were applied, waited for 15 s, and gently dried. The adhesive was left undisturbed for 5 s to allow the solvent to evaporate, and was light-cured for 20 s. In the self-etch control group, the adhesive was applied sufficiently wetting all dentin surfaces uniformly; it was gently agitated for 20 s, solvent was evaporated thoroughly by air blowing until there was no more movement of the adhesive, and then was light-cured for 20 s. In the total-etch experimental group, 37% phosphoric acid was applied for 15 s, acid gel was then removed and rinsed for 15 s, and excess water was removed by blot drying. 2% CHX was applied using a microbrush saturated with the solution for 60 s and excess was removed with a blotting paper, leaving the preparation surface visibly moist. This was followed by application of two consecutive coats of adhesive, waited for 15 s, and gently dried. The adhesive was left undisturbed for 5 s to allow the solvent to evaporate and was light-cured for 20 s. In the self-etch experimental group, CHX was applied using a microbrush saturated with the solution for 60 s and excess was removed with a blotting paper, leaving the preparation surface visibly moist. Adhesive was applied sufficiently wetting all dentin surfaces uniformly, and it was then gently agitated for 20 s. The solvent was evaporated thoroughly by air blowing until there was no more movement of the adhesive and then it was light-cured for 20 s.
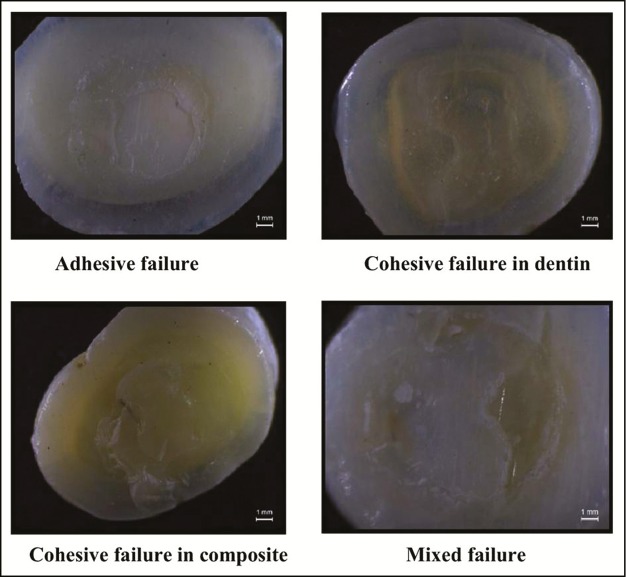
A custom-designed rig [Figure 1] was fabricated to place composite on samples. The rig comprised 3-mm-high cylindrical mold with an internal diameter of 2.5 mm, which was stabilized on a metal holder. The samples were placed on silicone holder above which the cylindrical mold was stabilized firmly on the dentin surface of the samples to prevent vibrations during placement of composite. Equal amounts of composite resin (Filtek Z350 XT 3M ESPE) was measured with a scoop, placed in increments of 1 mm, and cured (Bluephase G2 LED curing light; Ivoclar Vivadent Inc.Schaan; Liechtenstein) after each increments for 40 s. This entire process was conducted in an incubator (ESCO, Hatboro, PA) set at 37°C. The prepared samples were placed in distilled water at 37°C for 24 h. The samples were then thermocycled between 5°C and 55°C in water with a dwell time of 30 s at each temperature to a total of 10,000 cycles (SCTIMST, Trivandrum, India). The shear test was performed using universal testing machine (Instron Z020; Zwick/Roell, Ulm, Germany). To test, a wire loop at a cross head speed of 1 mm/min was used to load the specimens until fracture. The shear bond strength was calculated in megapascals. After testing, the fracture modes were evaluated using stereomicroscope (Stemi 2000 C; Carl Zeiss, Oberkochen, Germany) at ×10. The failure modes were categorized as adhesive failure, cohesive failure in dentin, cohesive failure in composite, and mixed failure as shown in Figure 2.
Figure 1.

Custom-designed rig
Figure 2.
Stereomicroscope images showing different modes of failure
Statistical analysis
For statistical analysis, SPSS, version 20, software (SPSS, Chicago, IL) was used and all the experimental groups were compared statistically using one-way analysis of variance (ANOVA) test. Bonferroni test was conducted to find statistical significance within the groups. Independent t test was conducted to compare the two control and experimental groups. In both the groups, a P value of <0.01 was considered statistically significant.
RESULTS
One-way ANOVA test was conducted [Table 1] to find whether there was any significant difference between the mean shear bond strength of four groups, which was found to be statistically significant (P = 0.000). Bonferroni test was conducted to verify whether the difference is statistically significant between the groups [Table 2]. The result showed that all the pairs differ significantly except Group 1 (total-etch) and Group 4 (self-etch + CHX). Independent t test [Table 3] showed that both the experimental groups showed a higher mean shear bond strength than that for the control group, which was statistically significant. Graph 1 shows the graphical representation of mean shear bond strength of all the four groups.
Table 1.
One-way analysis of variance (ANOVA) for various group comparison
| Groups | n | Mean | Standard deviation | P value |
|---|---|---|---|---|
| Total-etch | 20 | 28.25 | 2.531 | 0.000 |
| Self-etch | 20 | 25.15 | 3.281 | |
| Total-etch + CHX | 20 | 46.20 | 2.546 | |
| Self-etch + CHX | 20 | 29.45 | 1.761 | |
| Total | 80 | 32.26 | 8.631 |
CHX = 2% chlorhexidine
Table 2.
Bonferroni test comparison of mean shear bond strength between four groups
| Group | Mean + SD | P value |
|---|---|---|
| Total-etch (MPa) | 28.25 ± 2.53 | 0.002 |
| Self-etch (MPa) | 25.15 ± 3.28 | |
| Total-etch (MPa) | 28.25 ± 2.53 | <0.001 |
| Total-etch + CHX | 46.20 ± 2.55 | |
| Total-etch (MPa) | 28.25 ± 2.53 | 0.090 |
| Self-etch + CHX | 29.45 ± 1.76 | |
| Self-etch (MPa) | 25.15 ± 3.28 | <0.001 |
| Total-etch + CHX | 46.20 ± 2.55 | |
| Self-etch (MPa) | 25.15 ± 3.28 | <0.001 |
| Self-etch + CHX | 29.45 ± 1.76 | |
| Total-etch + CHX | 46.20 ± 2.55 | <0.001 |
| Self-etch + CHX | 29.45 ± 1.76 |
CHX = 2% chlorhexidine
Table 3.
Independent t test comparison between control and experimental groups
| Group | No of samples | Mean Shear Bond strength (MPa) | Standard deviation |
|---|---|---|---|
| Control | 40 | 26.70 | 3.291 |
| Experimental | 40 | 37.83 | 8.753 |
Graph 1.
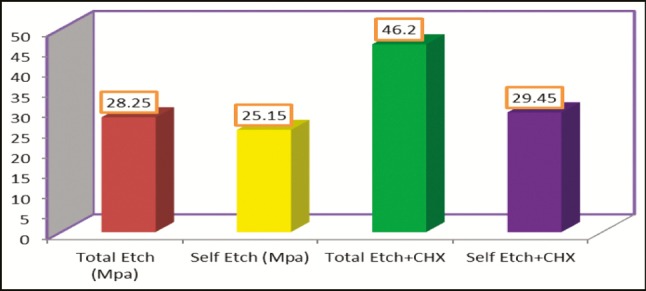
Mean shear bond strength of all four groups
Distribution of the failure mode
The mode of failure percentage was calculated [Table 4] and no failure in the adhesive interface was found in the total-etch with CHX group, but the self-etch with CHX group had 30% failures. Among the control groups, total-etch showed only 30% failure in the adhesive interface, whereas self-etch showed around 55% failure.
Table 4.
Distribution of the failure mode
| Group | Adhesive, n (%) | Cohesive in dentin, n (%) | Cohesive in composite, n (%) | Mixed, n (%) | Total (%) |
|---|---|---|---|---|---|
| Total-etch | 6 (30.0%) | 0 (0.0%) | 10 (50.0%) | 4 (20.0%) | 20 (100.0%) |
| Self-etch | 11 (55.0%) | 0 (0.0%) | 4 (20.0%) | 5 (25.0%) | 20 (100.0%) |
| CHX + total-etch | 0 (0.0%) | 2 (10.0%) | 10 (50.0%) | 8 (40.0%) | 20 (100.0%) |
| CHX + self-etch | 6 (30.0%) | 2 (10.0%) | 5 (25.0%) | 7 (35.0%) | 20 (100.0%) |
DISCUSSION
Mazzoni et al.[7] showed for the first time that the intrinsic MMP activity in the hybrid layer is promoted by etching and adhesive application. These authors observed that unequal enzyme activity in the hybrid layer is intense and continuous at the bottom and irregular at the top. It has been shown that MMP-2 can be released by an etch-and-rinse adhesive and degrade the interfaces of restorations under clinical conditions. Dutra-Correa et al reported that bond degradation by endogenous MMP may not be a problem with mild self-etching adhesives.[8]
Gendron et al.[6] proposed two different mechanisms of action involved in MMP inhibition—a chelating mechanism that sequesters metal ions such as calcium and zinc that inhibit catalytic activation of MMP-2 and MMP-9, and by the interaction of CHX with the essential sulfhydryl groups and/or cysteine present in MMP-active sites in the case of MMP-8.
The results of this study confirm previously published findings that resin–dentin interfaces bonded with total-etch adhesives and self-etch adhesives can degrade after short periods.[9,10]
One mechanism of degradation proposed in the literature is the incomplete impregnation of resin into the collagen network and hybrid layer itself.[9] It has recently been speculated that the autodegradation of dentin collagen fibrils is responsible for such findings.[9]
Ercan et al.[11] by evaluating the effect of CHX on human dentinal surface after 24 h in total-etch and self-etch adhesives reported no significant difference on the shear bond strength with the control groups. Hence, initial bond strength was not measured in this study and was measured only after thermocycling at 5°C and 55°C in water with a dwell time of 30 s at each temperature to a total of 10,000 cycles.
The present results revealed that CHX application prior to the two tested adhesives showed significantly higher shear bond strength; therefore, the results support complete acceptance of null hypothesis.
In the total-etch and self-etch experimental group, CHX was applied for 60 s prior to the application of adhesive, as reported in previous studies in which a significant reduction of MMP activity was seen.[12,13]
Total-etch adhesives showed much higher shear bond strength in both the experimental and the control group, which could be due to the involvement of 37% phosphoric acid etching. 37% Phosphoric acid demineralized dentin to a depth of 3–5 µm; the hydroxyapatite-free hybrid layer shows wide open tubules filled with deeper resin tags and densely filled with silica nanofillers, presenting a higher shear bond strength.[8] Hence, CHX application after etching in this group leads to an added advantage of effectively improving the durability this bond strength.
It has been shown that self-etch adhesives can activate MMPs, resulting in degradation of suboptimal infiltrated collagen and loss of bond strength.[14] This could have resulted in least shear bond strength and higher failure rates in the adhesive interface.
Pretreatment of the self-etch group with CHX improved the shear bond strength as CHX has excellent rewetting capacity and a strong affinity to tooth structure, which is thought to improve the bond strength to dentin.[15]
Lafuente[16] reported the beneficial effect of CHX on the stability of hybrid layer formed by an etch-and-rinse and a self-etch adhesive.
37% Phosphoric acid etching has a depth of penetration up to 5 µm in the unaffected dentin.[8] This could lead to higher depth of penetration of CHX during its application and also to deeper resin tags formation; its preservation might have led to least failure in the adhesive interface in the total-etch with CHX group in this study. On the other hand, the depth of penetration of self-etch adhesives is only 2 µm.[8] This would have resulted in weaker resin tags and more failures in the adhesive interface.
According to Pashley et al.[4], degradation of dentin collagen matrix occurs due to slow release of active MMP-2 (or other proteolytic enzymes) from the mineralized dentin matrices during storage, which could be the reason for reduced bond strengths of control groups.
In order to standardize the study, a single operator performed the entire study to minimize the operator-influenced bias. Teeth selected for the study were mostly from the donors who underwent orthodontic extraction. A rig was fabricated for the placement of composite resin, and equal increments of composite resin were placed after measuring with a scoop. Also, the study used only one composite (Filtek Z350 XT 3M ESPE) as the flexural strength and coefficient of thermal expansion may vary for different composites.[17]
The study showed much higher shear bond strength than that of the similar studies, which could be due to the elimination of microvibration during placement and curing of the composite resin with the help of a customized self-stabilized rig used in the study. The use of this rig to place composite on the samples makes this study unique with minimal bias, thereby emphasizing the true effect of bonding of composites to the samples.
The efficacy of CHX to improve the shear bond strength in total-etch and self-etch adhesives, though favorable in our study, still remains the topic of discussion in aged sclerotic dentin and other clinical situations.
CONCLUSION
2% chlorhexidine gluconate effectively improved the shear bond strength and helped in maintaining the durability of adhesive interface in both total-etch and self-etch adhesives.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Breschi L, Mazzoni A, Ruggeri A, Cadenaro M, Di Lenarda R, De Stefano Dorigo E. Dental adhesion review: Aging and stability of the bonded interface. Dent Mater. 2008;24:90–101. doi: 10.1016/j.dental.2007.02.009. [DOI] [PubMed] [Google Scholar]
- 2.Lynch CD, Blum IR, Frazier KB, Haisch LD, Wilson NH. Repair or replacement of defective direct resin-based composite restorations: Contemporary teaching in U.S. and Canadian dental schools. J Am Dent Assoc. 2012;143:157–63. doi: 10.14219/jada.archive.2012.0126. [DOI] [PubMed] [Google Scholar]
- 3.Carrilho MR, Carvalho RM, Tay FR, Yiu C, Pashley DH. Durability of resin-dentin bonds related to water and oil storage. Am J Dent. 2005;18:315–9. [PubMed] [Google Scholar]
- 4.Pashley DH, Tay FR, Yiu C, Hashimoto M, Breschi L, Carvalho RM, et al. Collagen degradation by host-derived enzymes during aging. J Dent Res. 2004;83:216–21. doi: 10.1177/154405910408300306. [DOI] [PubMed] [Google Scholar]
- 5.Moon PC, Weaver J, Brooks CN. Review of matrix metalloproteinases’ effect on the hybrid dentin bond layer stability and chlorhexidine clinical use to prevent bond failure. Open Dent J. 2010;4:147–52. doi: 10.2174/1874210601004010147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gendron R, Grenier D, Sorsa T, Mayrand D. Inhibition of the activities of matrix metalloproteinases 2, 8, and 9 by chlorhexidine. Clin Diagn Lab Immunol. 1999;6:437–9. doi: 10.1128/cdli.6.3.437-439.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mazzoni A, Nascimento FD, Carrilho M, Tersariol I, Papa V, Tjäderhane L, et al. MMP activity in the hybrid layer detected with in situ zymography. J Dent Res. 2012;91:467–72. doi: 10.1177/0022034512439210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dutra-Correa M, Saraceni CH, Ciaramicoli MT, Kiyan VH, Queiroz CS. Effect of chlorhexidine on the 18-month clinical performance of two adhesives. J Adhes Dent. 2013;15:287–92. doi: 10.3290/j.jad.a29533. [DOI] [PubMed] [Google Scholar]
- 9.Loguercio AD, Stanislawczuk R, Polli LG, Costa JA, Michel MD, Reis A. Influence of chlorhexidine digluconate concentration and application time on resin-dentin bond strength durability. Eur J Oral Sci. 2009;117:587–96. doi: 10.1111/j.1600-0722.2009.00663.x. [DOI] [PubMed] [Google Scholar]
- 10.Reis A, Grandi V, Carlotto L, Bortoli G, Patzlaff R, Rodrigues Accorinte Mde L, et al. Effect of smear layer thickness and acidity of self-etching solutions on early and long-term bond strength to dentin. J Dent. 2005;33:549–59. doi: 10.1016/j.jdent.2004.12.003. [DOI] [PubMed] [Google Scholar]
- 11.Ercan E, Erdemir A, Zorba YO, Eldeniz AU, Dalli M, Ince B, et al. Effect of different cavity disinfectants on shear bond strength of composite resin to dentin. J Adhes Dent. 2009;11:343–6. [PubMed] [Google Scholar]
- 12.Hebling J, Pashley DH, Tjäderhane L, Tay FR. Chlorhexidine arrests subclinical degradation of dentin hybrid layers in vivo. J Dent Res. 2005;84:741–6. doi: 10.1177/154405910508400811. [DOI] [PubMed] [Google Scholar]
- 13.Carrilho MR, Carvalho RM, de Goes MF, di Hipólito V, Geraldeli S, Tay FR, et al. Chlorhexidine preserves dentin bond in vitro. J Dent Res. 2007;86:90–4. doi: 10.1177/154405910708600115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shafiei F, Alikhani A, Alavi AA. Effect of chlorhexidine on bonding durability of two self-etching adhesives with and without antibacterial agent to dentin. Dent Res J (Isfahan) 2013;10:795–801. [PMC free article] [PubMed] [Google Scholar]
- 15.Sharma V, Rampal P, Kumar S. Shear bond strength of composite resin to dentin after application of cavity disinfectants—SEM study. Contemp Clin Dent. 2011;2:155–9. doi: 10.4103/0976-237X.86438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lafuente D. SEM analysis of hybrid layer and bonding interface after chlorhexidine use. Oper Dent. 2012;37:172–80. doi: 10.2341/10-251-L. [DOI] [PubMed] [Google Scholar]
- 17.Salz U, Bock T. Testing adhesion of direct restoratives to dental hard tissue—A review. J Adhes Dent. 2010;12:343–71. doi: 10.3290/j.jad.a19741. [DOI] [PubMed] [Google Scholar]