Abstract
FEM was technologically innovated which initially aimed at answering structural analysis difficulties involving Mechanics, Civil and Aeronautical Engineering. FEM basically stands for a numerical model of analyzing stresses as well as distortions in the form of any agreed geometry. There for the shape is discretized into the so-called ‘finite elements’ coupled through nodes. Accuracy of the results is determined by type, planning and total number of elements used for a particular study model. 3-D FE model was designed for in-depth qualitative examination of the relations amongst implant, tooth, periodontal ligament, and bone. Scholarly work equating work reliability, validated with a 3-D modeling suggested that meticulous data can be acquired with respect to stress distribution in bone. Comparative results from 3-D FEA studies showed that 3D FEA, when matched with in-vivo strain gauge measurements were corresponding with clinical outcomes. The aim of this review of literature is to provide an overview to show the application of FEM in (Short) implant dentistry.
KEYWORDS: FEM, short implants, stress analysis, platform switched-implants
INTRODUCTION
Since the discovery of dental implants by Brånemark,[1] it has become a ground-breaking reality on the use of dental implants for replacing a missing teeth. Dental implants have become an inseparable part of dental practice and their use in recent years has increased in leaps and bounds. Clinical success of a dental implant mainly depends on its biomechanical behavior, as the pattern of stress distribution in dental implants is completely different from that of a natural tooth.[2] Because the latter has a periodontal ligament that acts as a shock absorber to occlusal forces,[3] success or failure of dental implant mainly depends on a key feature, that is, the manner in which stress is transferred from dental implant to the adjoining alveolar bone.[4,5]
If the occlusal forces around a dental implant are distributed homogenously, then the bone is maintained well. When we look into the literature, several attempts to preserve the marginal bone around dental implants have been made.[6] Contributing factors for marginal bone loss that have been accepted to some degree are biological, clinical, and mechanical factors.[7] It is vital to understand the biomechanical behavior of bony tissues and dental implants to prevent marginal bone loss and implant failure.
To prevent implant failures and complications caused by mechanical and technical factors, these factors have to be evaluated in advance. As a result, use of these essential steps could increase the survival rate of implant-supported restorations. Hence, there has been a dramatic increase in the number of biomechanical studies in the field of implant dentistry in an effort to decrease dental implant failure rates.[8]
Research in different fields of Dentistry needs a methodology that is cost-effective and reproducible. Such an approach may perhaps be situated to guide researchers in biomechanics structure in healthy and pathologic conditions.
In bioengineering field, the application of simulations introduced in recent years certainly is a vital instrument to measure the best clinical option, only if that is precisely sufficient in investigation, particularly physiological conditions. Oral environment in biomechanical research such as restorative dentistry, endodontics, orthodontics, prosthodontics, periodontics, and implantology has been studied in vitro because the oral cavity is an intricate biomechanical system because of its complexity and limited access.[9]
A noninvasive way to predict in vivo contact mechanics is computerized modeling. To investigate stress distribution around the peri-implant bone, various methods have been currently explored. To name a few, we have photoelastic model, strain gauge analysis, and three-dimensional (3D) finite element analysis (FEA).[10] Because of availability of software and the ability to determine 3D stresses and strains, finite element modeling (FEM) is considered the most commonly used method.[11,12]
Initially, FEM was technologically innovated, which aimed at answering structural analysis difficulties involving Mechanics, Civil, and Aeronautical Engineering. FEM basically stands for a numerical model of analyzing stresses as well as distortions in the form of any agreed geometry.[13,14] Therefore, the shape is discretized into the so-called finite elements coupled through nodes. Accuracy of the results is determined by type, planning, and total number of elements used for a particular study model.[15]
3D FEM was designed for in-depth qualitative examination of the relations among implant, tooth, periodontal ligament, and bone. Scholarly work equating work reliability, validated with a 3D modeling, suggested that meticulous data can be acquired with respect to stress distribution in bone. Comparative results from 3D FEA studies showed that 3D FEA results, when matched with in vivo strain gauge measurements, were corresponding to clinical outcomes.[16]
MATERIALS AND METHODS
Protocol
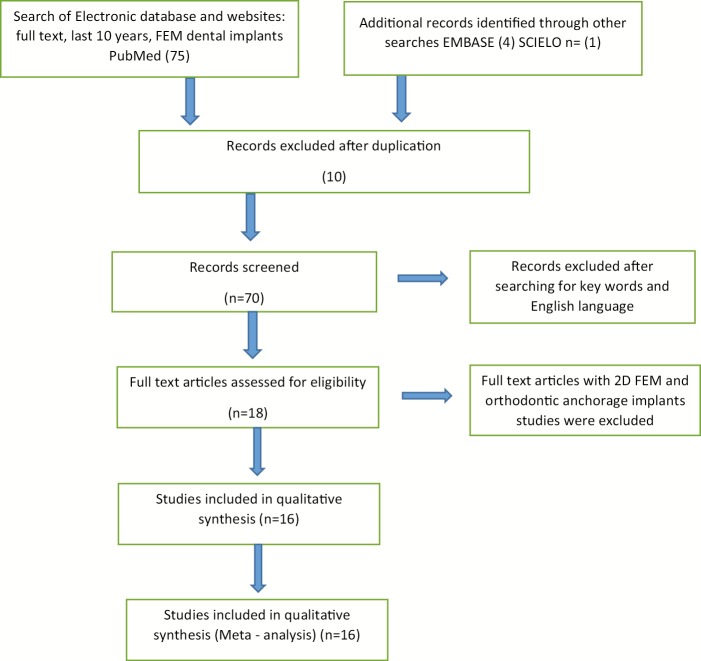
The present systemic review was conducted in accordance with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines [Figure 1].
Figure 1.
Flow diagram (PRISMA format) of the screening and selection process
Eligibility criteria, information sources, and search strategy
A literature survey was conducted from 2008 to May 2018 to identify all aspects of the studies that examined the role of FEM in dental implants. PubMed, EMBASE, and Scielo databases were searched using keywords FEM and Dental Implants with their respective abbreviations according to the search engine used.
Study selection
Full-text article published only in English language were included in the analysis. Search was further filtered to include only research articles. Research article with emphasis on 3D FEM and stress evaluation on cortical bone with periodontal implications were considered for final analysis.
RESULTS
By FEA, researchers predict stress distribution in the contact area between cortical bone and implant as well as around the apex of implants in the trabecular bone, which is explained by the help of tables [Table 1 and 2].
Table 1.
Use of the FEM to evaluate the stress of short implants
| S.No | Author | Year | Study Variables | Conclusion |
|---|---|---|---|---|
| 1 | Yashwant AV et al[17] | 2017 | 5 diverse short implants designs in thread shape were selected with 10 different screws in every group. Polyurethane foam in perpendicular direction was used to load the short implants. Instrom testing machine was used to test pull-out strength. Short implants with reverse buttress thread shape were used as control group. | Trapezoidal fluted short implants displayed the maximum pull out strength when equated to short implants with other thread designs. |
| 2 | Küçükkurt S et al[18] | 2017 | Authors compared the success of sinus lifting and alternative treatment methods in applying dental implants in cases lacking adequate bone due to pneumatization of the maxillary sinus. | LSL method should be the first choice among treatment options. Considering its successful results under conditions of oblique forces, the SIP method may be preferable to the TIP method. In contrast, every effort should be made to avoid the use of DCs. |
| 3 | Yazicioglu D et al[19] | 2016 | Study was conducted to assess stress dissemination in short dental implants as well as bone-to-implant contact ratio in the maxilla posterior region by means of 3D –FEM analysis. | It was observed that von Mises stress were thrice in implants and the cancellous bone with 70% bone-to-implant contact group when compared with that of 100% bone-to-implant contact group. |
| 4 | Sotto-Maior BS et al[20] | 2016 | Research was done to mimic bone remodelling surrounding single implants of different lengths using Finite Element Analysis. This study was carried out to check the theoretical prediction of crestal bone loss by means of clinical results. | Results of the study revealed that mechano- regulatory tissue models may well be engaged in observing the structural alterations in bone when exposed to biomechanical stress. Study also revealed that, implant length did not impact the bone remodeling surrounding single dental implants for the period of one year after loading. |
| 5 | Kheiralla LS et al[21] | 2014 | In this study physical responses of 3 single crowns reinforced by 3 dissimilar implants under axial, off-axial loading were equated. Strain gauges and finite element analysis was carried out to calculate the strain brought by axial, off-axial functional loads of 300 N. | The researchers concluded that the standard as well as short-wide implants showed preference in reinforcing crowns. It was observed that the standard implant displayed the shortmum strains under axial and off-axial loading using Finite Element Analysis simulation. On the contrary the short-wide implant displayed the shortmal strains under nonaxial loading by means of strain gauge analysis. |
| 6 | Balkaya MC et al[22] | 2014 | The aim remained to evaluate the biomechanical performance of implants by means of a variable number, angulation, and size using three dimensional Finite Element Analysis. | The results of the study revealed reducing cantilever distance using distal implant angulation shortmises stress in and around implant, and cortical bone. |
| 7 | Kang N et al[23] | 2014 | Researchers carried a study to determine the biomechanics of short dental implants. | It was observed that implants with diameter greater than 5.5 mm and superior bone quality may be desirable to get better clinical results. However the researchers also cautioned that forward looking clinical studies were mandatory to confirm this. |
| 8 | Kim S et al[24] | 2104 | A recent in vitro study was carried out to assess biomechanical performance of short dental implants with different heights of residual bone. They also related it by means of standard dental implants ie (<13 mm) residual bone using Finite Element Analysis. | Results revealed that the stimulatory condition without maxillary sinus bone graft revealed additional operational stress dissemination may possibly be attained in 4, 5, 6, or 7 mm of residual bone with short dental implants than in 13 mm of residual bone when compared to regular dental implants. |
| 9 | Baggi L et al[25] | 2013 | The researchers conducted a study with an intention of investigating the effect of implant design, in-bone positioning depth, and post healing crestal structure. This was to evaluate the load transfer means of osseointegrated dental implants based on the platform-switching model. | The study outcome revealed that the recognition of the joint influence of a numerous causes affecting the bone-implant loading transfer mechanisms. The results also provided valuable insights and suggestions for selecting implants. |
| 10 | Toniollo MB et al[26] | 2013 | In this finite element study comparison of stress dissemination on outer surface of dissimilar morse taper implants with variable length of implants as well as proportions of metal- ceramic crowns in order to preserve the occlusal integrity. | It was observed that 5mm implants which were located at the cortical bone level, has higher elastic modulus and may have influenced at the stress distribution. Conversely higher stresses on these implants were able to endure the applied forces considerably well. |
| 11 | Toniollo MB et al[27] | 2012 | The study likened stress dissemination on various bony ridges substituted by diverse lengths of morse taper implants, variable dimensions of metal-ceramic crowns to preserve the occlusal orientation. | They concluded that the cases needing short implant prostheses need cautious assessment and occlusal adjustment. Overloading of short implants, as well as in regular implants, be able to cause stress beyond the physiological threshold of the surrounding bone. |
| 12 | de Carvalho NA et al[28] | 2012 | Research was carried out to calculate stress dissemination in peri-implant bone mimicking the effect on regular as well as platforms switched implants in the maxilla anterior region by means of FEM. | The effect of platform switching was quite obvious on cortical bone when compared with the trabecular bone for the short and long implants. It was observed that the long implants displayed lesser stress values when compared to the short implants, mainly when the platform switched implants were used. |
Table 2.
FEM and stress distribution in platform switched-implants
| S.No | Author | Year | Study Variables | Conclusion |
|---|---|---|---|---|
| 1 | Markose J et al[29] | 2017 | Study compared the effect platform switched (PS), sloping shoulder, and regular implants on stress decline in different bone densities using finite element analysis model. | The results of the study revealed that the sloping shoulder implant in subcrestal position were encouraging for bone growth, stress distribution, and maintenance of existing bone. |
| 2 | Aradya A et al[30] | 2016 | Study was intended to assess stress distribution in the across the cortical section of bone with normal abutment and platform switched abutment when subjected to vertical and oblique forces in mandibular posterior region. | The researchers concluded that platform switched abutment caused comparative reduction in von Mises stress in the across the cortical section of bone when matched with normal abutment under vertical and oblique forces in mandibular posterior region. |
| 3 | Xia H et al[31] | 2013 | Study was carried out to evaluate the stress distribution in the bone surrounding a platform-switched implant with marginal bone loss. | The results revealed that PS technique had a biomechanical benefit in case of marginal bone resorption but this gain was faded when bone resorption was intense. |
| 4 | Rismanchian M et al[32] | 2013 | A research was aimed to assess peri-implant bone stress distribution for platform- switched implants when positioned at altered depths. | Researchers established that subcrestal placement of 2-stage platform-switched implants marginally maximises the stress within the cortical bone. |
| 5 | Vargas LC et al[33] | 2013 | Research was done to calculate stress distribution on peri-implant bone by mimicking the biomechanical impact of implants with dissimilar diameters of regular or platform switched abutments using 3-D FEM. | The results of the study revealed that platform switching was more obvious for cortical bone when compared that of trabecular bone. This was mainly seen in large platform diameter reduction. |
DISCUSSION
Application of finite element analysis in dentistry
Meticulous quantifiable information on any place inside a mathematical model can be provided by FEA. As a result, FEA has turned out to be a valued analytical instrument in the estimation of stress and strain in implant systems. One of the salient characteristics of FEM rests in its near physical similarity among the real structure as well as its FEM. However, unnecessary simplification in geometry shall invariably lead to inconsistent results.[34,35,36,37]
Rules generally followed in FEM and implant–bone biomechanics
FEA model can be applied to various physical problems and its power lies in its versatility. The structure that is to be analyzed may have random form, loads, and supporting conditions; in addition, the mesh may be able to amalgamate features of diverse shapes, types, and physical properties.
FEA outcomes give: (1) complete geometry of the implant and surrounding bone to be modeled, (2) boundary conditions, (3) material properties, (4) loading conditions, (5) interface between bone and implant, (6) convergence test, and (7) validation.[2]
Advantages of FEM
It enables the visualization of superimposed structures.
Specification and the material properties of anatomic craniofacial structures can be evaluated.
We can locate the magnitude and direction of an applied force.
It provides stress points that can be measured theoretically.
Physical properties of the analyzed materials are not altered.
It is easy to repeat.
It is a noninvasive technique.
Both static and dynamic analyses can be carried out.
A reduced amount of time spent.
Study can be repeated as many times.
No need to sacrifice animals to evaluate stress and strain.
Disadvantages of FEM
Incorrect information, statistics, and interpretation will yield totally misguiding results.
Need to have computer knowledge.
Need to have thorough information about their mechanical behaviors.
Certain expectations are bound to be accepted. Hence, outcomes will be determined by people associated in the study.
Stress values evaluation and its validity in FEM study
Stress distribution in FEM studies is generally interpreted as von Mises stress, which could be maximum and minimum principal stress or it could be principal strains.[38] von Mises stress is estimated in three planes, that is, x-axis, y-axis, and z-axis using a formula.[39] Validation is done by comparing the current FEM results with that of the previous studies related to a particular topic. It provides knowledge on whether precise models were designed for the study or not. Further, it would corroborate the results of previous studies and it may either support or refute with the literature. The best way to validate FEM results is to conduct in vitro and in vivo experimental studies simultaneously. If the results are good, then it could be recommended for future studies.[40]
CONCLUSION
For better understanding, the biomechanics of dental implants and the use of computer technology alongside with more profound awareness about the concept, methodology, advantages, and limitations of FEA have to be assessed elaborately. As a result, clinicians can use this modern technology to enhance implant survival by well accepting the biomechanics of dental implantology.
In this article, authors had made an effort to address the basics of FEA in dental implantology. The features that make FEA a powerful tool sufficient to reliably mention on flexible stress states in a complex structure are known.
Similar to any other instrument used to resolve a problem, the explanation made can only be as robust as the suitable application of the instrument itself. Upcoming investigation ought to attempt to correlate results with clinical findings. In doing so, it enhances the validity of the models. In addition, simulate the consequence of saliva, infection and fatigue failure under repetitive, realistic, and cyclic loading conditions have to be evaluated.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Brånemark PI, Adell R, Breine U, Hansson BO, Lindström J, Ohlsson A. Intra-osseous anchorage of dental prostheses. I. Experimental studies. Scand J Plast Reconstr Surg. 1969;3:81–100. doi: 10.3109/02844316909036699. [DOI] [PubMed] [Google Scholar]
- 2.Hsu ML, Chang CL. 1st ed. Rijeka: Sciyo, InTech Europe; 2010. Finite element analysis. Finite element analysis. [Google Scholar]
- 3.Koosha S, Mirhashemi FS. An investigation of three types of tooth implant supported fixed prosthesis designs with 3D finite element analysis. J Dent (Tehran) 2013;10:51–63. [PMC free article] [PubMed] [Google Scholar]
- 4.Glantz PO, Nilner K. Biomechanical aspects of prosthetic implant-borne reconstructions. Periodontol. 2000;1998(17):119–24. doi: 10.1111/j.1600-0757.1998.tb00129.x. [DOI] [PubMed] [Google Scholar]
- 5.Akpinar I, Anil N, Parnas L. A natural tooth’s stress distribution in occlusion with a dental implant. J Oral Rehabil. 2000;27:538–45. doi: 10.1046/j.1365-2842.2000.00511.x. [DOI] [PubMed] [Google Scholar]
- 6.Berglundh T, Persson L, Klinge B. A systematic review of the incidence of biological and technical complications in implant dentistry reported in prospective longitudinal studies of at least 5 years. J Clin Periodontol. 2002;29:197–212. doi: 10.1034/j.1600-051x.29.s3.12.x. discussion 232-3. [DOI] [PubMed] [Google Scholar]
- 7.Rocha S, Wagner W, Wiltfang J, Nicolau P, Moergel M, Messias A, et al. Effect of platform switching on crestal bone levels around implants in the posterior mandible: 3 years results from a multicentre randomized clinical trial. J Clin Periodontol. 2016;43:374–82. doi: 10.1111/jcpe.12522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gaviria L, Salcido JP, Guda T, Ong JL. Current trends in dental implants. J Korean Assoc Oral Maxillofac Surg. 2014;40:50–60. doi: 10.5125/jkaoms.2014.40.2.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Piccioni MRV, Campos EA, Saad JRC, de Andrade MF, Galvão MR, Rached AA. Application of the finite element method in Dentistry. RSBO Revista Sul-Brasileira de Odontologia. 2013;10:369–77. [Google Scholar]
- 10.Srirekha A, Bashetty K. Infinite to finite: An overview of finite element analysis. Indian J Dent Res. 2010;21:425–32. doi: 10.4103/0970-9290.70813. [DOI] [PubMed] [Google Scholar]
- 11.Pesqueira AA, Goiato MC, Filho HG, Monteiro DR, Santos DM, Haddad MF, et al. Use of stress analysis methods to evaluate the biomechanics of oral rehabilitation with implants. J Oral Implantol. 2014;40:217–28. doi: 10.1563/AAID-JOI-D-11-00066. [DOI] [PubMed] [Google Scholar]
- 12.Reddy K, Reddy S, Rao B, Kshitish D, Mannem S. Cervical stress due to normal occlusal loads is a cause for abfraction? —A finite element model study. J Orofac Sci. 2012;4:120–3. [Google Scholar]
- 13.Bathe KJ. Finite element procedures. Chapter 4. Upper Saddle River (NJ): Prentice-Hall; 1996. pp. 148–377. [Google Scholar]
- 14.Gultekin BA, Gultekin P, Yalcin S. Finite element analysis— New trends and developments. 1st ed. Rijeka: Sciyo, InTech Europe; 2012. [Google Scholar]
- 15.Chen L. In: Finite element analysis-New trends and developments. Ebrahimi F, editor. London: IntechOpen Limited; 2012. SE1 9SG, UK, ISBN 978-953-51-0769-9. [Google Scholar]
- 16.Danza M, Zollino I, Paracchini L, Riccardo G, Fanali S, Carinci F. 3D finite element analysis to detect stress distribution: Spiral family implants. Maxillofac Oral Surg. 2009;8:334–9. doi: 10.1007/s12663-009-0081-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yashwant AV, Dilip S, Krishnaraj R, Ravi K. Does change in thread shape influence the pull out strength of mini implants? An in vitro study. J Clin Diagn Res. 2017;11:ZC17–20. doi: 10.7860/JCDR/2017/25774.9808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Küçükkurt S, Alpaslan G, Kurt A. Biomechanical comparison of sinus floor elevation and alternative treatment methods for dental implant placement. Comput Methods Biomech Biomed Engin. 2017;20:284–93. doi: 10.1080/10255842.2016.1218482. [DOI] [PubMed] [Google Scholar]
- 19.Yazicioglu D, Bayram B, Oguz Y, Cinar D, Uckan S. Stress distribution on short implants at maxillary posterior alveolar bone model with different bone-to-implant contact ratio: Finite element analysis. J Oral Implantol. 2016;42:26–33. doi: 10.1563/aaid-doi-D-14-00003. [DOI] [PubMed] [Google Scholar]
- 20.Sotto-Maior BS, Mercuri EG, Senna PM, Assis NM, Francischone CE, Del Bel Cury AA. Evaluation of bone remodeling around single dental implants of different lengths: A mechanobiological numerical simulation and validation using clinical data. Comput Methods Biomech Biomed Engin. 2016;19:699–706. doi: 10.1080/10255842.2015.1052418. [DOI] [PubMed] [Google Scholar]
- 21.Kheiralla LS, Younis JF. Peri-implant biomechanical responses to standard, short-wide, and mini implants supporting single crowns under axial and off-axial loading (an in vitro study) J Oral Implantol. 2014;40:42–52. doi: 10.1563/AAID-JOI-D-11-00102. [DOI] [PubMed] [Google Scholar]
- 22.Balkaya MC. Investigation of influence of different implant size and placement on stress distribution with 3-dimensional finite element analysis. Implant Dent. 2014;23:716–22. doi: 10.1097/ID.0000000000000158. [DOI] [PubMed] [Google Scholar]
- 23.Kang N, Wu YY, Gong P, Yue L, Ou GM. A study of force distribution of loading stresses on implant-bone interface on short implant length using 3-dimensional finite element analysis. Oral Surg Oral Med Oral Pathol Oral Radiol. 2014;118:519–23. doi: 10.1016/j.oooo.2014.05.021. [DOI] [PubMed] [Google Scholar]
- 24.Kim S, Kim S, Choi H, Woo D, Park YB, Shim JS, et al. A three-dimensional finite element analysis of short dental implants in the posterior maxilla. Int J Oral Maxillofac Implants. 2014;29:e155–64. doi: 10.11607/jomi.3210. [DOI] [PubMed] [Google Scholar]
- 25.Baggi L, Di Girolamo M, Vairo G, Sannino G. Comparative evaluation of osseointegrated dental implants based on platform-switching concept: Influence of diameter, length, thread shape, and in-bone positioning depth on stress-based performance. Comput Math Methods Med. 2013;2013:250929. doi: 10.1155/2013/250929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Toniollo MB, Macedo AP, Rodrigues RC, Ribeiro RF, Mattos Mda G. Three-dimensional finite element analysis of the stress distribution on morse taper implants surface. J Prosthodont Res. 2013;57:206–12. doi: 10.1016/j.jpor.2013.02.003. [DOI] [PubMed] [Google Scholar]
- 27.Toniollo MB, Macedo AP, Rodrigues RC, Ribeiro RF, de Mattos Mda G. Three-dimensional finite element analysis of stress distribution on different bony ridges with different lengths of morse taper implants and prosthesis dimensions. J Craniofac Surg. 2012;23:1888–92. doi: 10.1097/SCS.0b013e31826cf199. [DOI] [PubMed] [Google Scholar]
- 28.de Carvalho NA, de Almeida EO, Rocha EP, Freitas AC, Jr, Anchieta RB, Kina S. Short implant to support maxillary restorations: Bone stress analysis using regular and switching platform. J Craniofac Surg. 2012;23:678–81. doi: 10.1097/SCS.0b013e31824dbab7. [DOI] [PubMed] [Google Scholar]
- 29.Markose J, Suresh S, Eshwar S, Rekha K, Jain V, Manvi S. Comparison of platform switched and sloping shoulder implants on stress reduction in various bone densities: Finite element analysis. J Contemp Dent Pract. 2017;18:510–5. doi: 10.5005/jp-journals-10024-2075. [DOI] [PubMed] [Google Scholar]
- 30.Aradya A, Kumar UK, Chowdhary R. Influence of different abutment diameter of implants on the peri-implant stress in the crestal bone: A three-dimensional finite element analysis–—In vitro study. Indian J Dent Res. 2016;27:78–85. doi: 10.4103/0970-9290.179836. [DOI] [PubMed] [Google Scholar]
- 31.Xia H, Wang M, Ma L, Zhou Y, Li Z, Wang Y. The effect of platform switching on stress in peri-implant bone in a condition of marginal bone resorption: A three-dimensional finite element analysis. Int J Oral Maxillofac Implants. 2013;28:e122–7. doi: 10.11607/jomi.2965. [DOI] [PubMed] [Google Scholar]
- 32.Rismanchian M, Askari N, Shafiei S. The effect of placement depth of platform-switched implants on periimplant cortical bone stress: A 3-dimensional finite element analysis. Implant Dent. 2013;22:165–9. doi: 10.1097/ID.0b013e31827f34d0. [DOI] [PubMed] [Google Scholar]
- 33.Vargas LC, de Almeida EO, Rocha EP, Kina S, Anchieta RB, Júnior AC, et al. Regular and switching platform: Bone stress analysis with varying implant diameter. J Oral Implantol. 2013;39:326–31. doi: 10.1563/AAID-JOI-D-10-00157. [DOI] [PubMed] [Google Scholar]
- 34.Shilpa T. Finite element analysis: A boon to dentistry. J Oral Biol Craniofac Res. 2014;4:200–3. doi: 10.1016/j.jobcr.2014.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.El-Anwar MI, El-Zawahry MM. A three dimensional finite element study on dental implant design. J Genet Eng Biotechnol. 2011;9:77–82. [Google Scholar]
- 36.DeTolla DH, Andreana S, Patra A, Buhite R, Comella B. Role of the finite element model in dental implants. J Oral Implantol. 2000;26:77–81. doi: 10.1563/1548-1336(2000)026<0077:TROTFE>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 37.Van Staden RC, Guan H, Loo YC. Application of the finite element method in dental implant research. Comput Methods Biomech Biomed Engin. 2006;9:257–70. doi: 10.1080/10255840600837074. [DOI] [PubMed] [Google Scholar]
- 38.Bahuguna R, Anand B, Kumar D, Aeran H, Anand V, Gulati M. Evaluation of stress patterns in bone around dental implant for different abutment angulations under axial and oblique loading: A finite element analysis. Natl J Maxillofac Surg. 2013;4:46–51. doi: 10.4103/0975-5950.117882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Akin JE. Finite element analysis concepts: Via SolidWorks. Singapore: World Scientific; 2010. [Google Scholar]
- 40.Omori M, Sato Y, Kitagawa N, Shimura Y, Ito M. A biomechanical investigation of mandibular molar implants: Reproducibility and validity of a finite element analysis model. Int J Implant Dent. 2015;1:10. doi: 10.1186/s40729-015-0011-5. [DOI] [PMC free article] [PubMed] [Google Scholar]