Abstract
OBJECTIVES:
To determine whether poor nutritional status can predict postoperative delirium in elderly adults undergoing hip fracture surgery.
DESIGN:
Prospective observational cohort study.
SETTING:
Italian orthogeriatric unit.
PARTICIPANTS:
Individuals aged 70 and older (mean age 84.0 ± 6.6, 74.5% female) consecutively admitted for surgical repair of a proximal femur fracture between September 2012 and April 2016 (N = 415).
MEASUREMENTS:
Participants underwent a comprehensive geriatric assessment including nutritional status, which was evaluated using the Mini Nutritional Assessment Short Form (MNA-SF). The MNA-SF-based three-class stratification was tested using multivariable logistic regression to assess its role in predicting postoperative delirium (outcome).
RESULTS:
Seventy-eight malnourished individuals (MNA-SF score 0–7), 185 at risk of malnutrition (MNA-SF score 8–11), and 152 who were well nourished (MNA-SF score 12–14) were compared. On average, individuals with poor nutritional status were more disabled and more cognitively impaired than those who were well nourished and those at risk of malnutrition. Moreover, those who were malnourished were more likely to have postoperative delirium. Multivariate regression analysis adjusted for age, sex, comorbidity, functional impairment, preoperative cognitive status, and American Society of Anesthesiologists score showed that those who were at risk of malnutrition (odds ratio (OR) = 2.42, 95% confidence interval (CI) = 1.29–4.53) and those who were overtly malnourished (OR = 2.98, 95% CI = 1.43–6.19) were more likely to develop postoperative delirium.
CONCLUSION:
This is the first study in a Western population showing that risk of malnutrition and overt malnutrition, as assessed using the MNA-SF, are independent predictors of postoperative delirium. Accordingly, nutritional status should be assessed in individuals with hip fracture before surgery to determine risk of developing delirium. J Am Geriatr Soc 65:1222–1228, 2017.
Keywords: malnutrition, Mini-Nutritional Assessment Short Form, postoperative delirium, hip fracture; elderly
Hip fracture is an epidemic problem worldwide, and despite the fact that the incidence has fallen in some Western countries,1,2 prevalence is expected to increase in future years because of the aging of the population.3
Delirium and poor nutritional status are two common findings in individuals with hip fracture. Delirium may occur before both and after a surgical procedure4,5 and is often associated with poor clinical, cognitive, and functional outcomes.5 Similarly, poor nutritional status may be present before and after hip fracture6–8 and has been found to be associated with several negative clinical outcomes, such as pressure ulcers,9 functional dependence,10 walking impairment,11 and mortality.11 Although delirium and poor nutritional status may coexist in an individual experiencing hip fracture,9,12 few studies have assessed the effect of their association on clinical outcomes.
This study investigated whether poor nutritional status, as detected using a specific and standardized tool (Mini Nutritional Assessment—Short Form (MNA-SF)), can help identify the development of postoperative delirium in a population of elderly adults with hip fracture. Findings from this study would be clinically relevant because postoperative delirium is partially preventable, and poor nutritional status may be a target condition for intervention or prevention.
METHODS
Study Design and Enrollment Criteria
This prospective observational cohort study was conducted in the Orthogeriatric Unit (OGU) of San Gerardo Hospital, University of Milano-Bicocca (Monza, Italy). All individuals aged 70 and older consecutively admitted to the OGU between September 2012 and April 2016 with a diagnosis of proximal femur fracture (intra- or extracapsular) were considered. Exclusion criteria were a conservative (nonoperative) approach to hip fracture and preoperative delirium.
Study Population
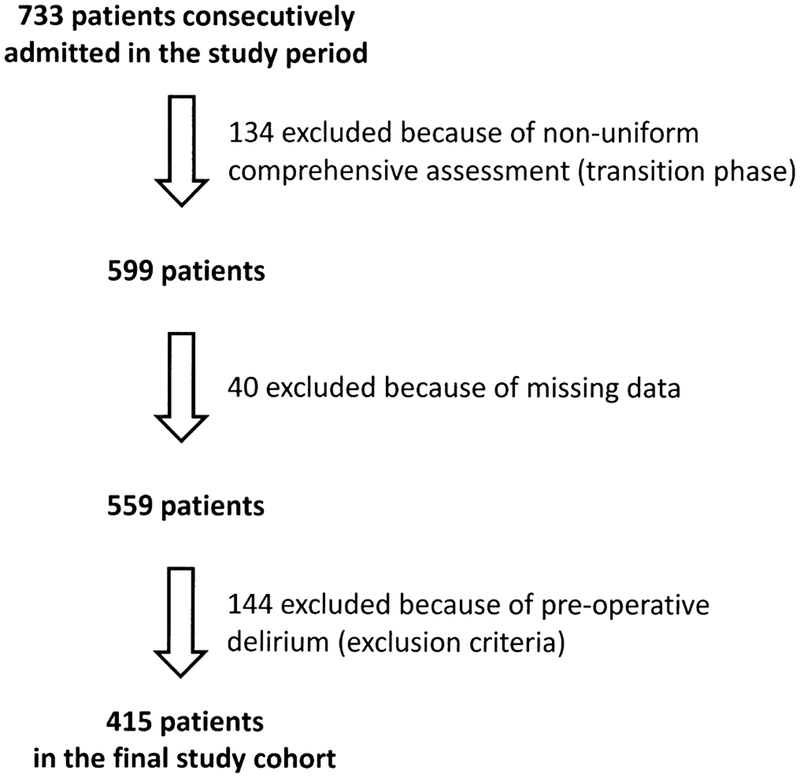
Of 733 individuals hospitalized for hip fracture between September 2012 and April 2016, 134 were excluded because of lack of uniformity in the comprehensive geriatric assessment due to a revision of the OGU protocols and the parallel validation of a different tool for delirium screening, 40 because of missing data, and 144 because of preoperative delirium, leaving a final population of 415 (Figure 1). Baseline characteristics of included and excluded individuals were not substantially different, except that those who were excluded were older (data not shown).
Figure 1.
Flow chart for identification of study cohort among individuals consecutively hospitalized between September 2012 and April 2016.
Comprehensive Geriatric Assessment and data Collection
Participants underwent a comprehensive geriatric assessment within 24 hours of admission, including demographic characteristics, years of education, functional and mental status, comorbidities, severity of illnesses, medications, and nutritional status. Perioperative information was gathered on type of fracture (femoral neck, intertrochanteric, subtrochanteric), type of surgery (hemiarthroplasty, internal fixation), type of anesthesia (general, spinal), American Society of Anesthesiologists (ASA) physical status score,13 and blood transfusions (red blood cell units) received during OGU stay. The ASA physical status score indicates the preoperative fitness of an individual scheduled for surgery [(range 1 (normal healthy individual) to 6 (brain dead)]. The ASA classification system is available at https://www.asahq.org/resources/clinical-information/asa-physical-status-classification-sysyem. Days from admission to surgery, length of hospital stay, and in-hospital mortality were also assessed. Delirium was diagnosed using the Confusion Assessment Method (CAM)14 and confirmed according to Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM-IV-TR) criteria.15 Participants were regularly assessed upon admission to the OGU on weekdays and weekends. Assessors (SZ, AA, VB) were trained physicians and residents, all experts in evaluating and managing individuals with delirium.16–18 The delirium assessment protocol was the same during the preoperative and postoperative phases and started with a CAM-based screening systematically administered twice a day—in the morning and in the afternoon. The nursing staff was also trained to ask for a medical evaluation if a change of mental status was suspected. Delirium was confirmed using the DSM-IV-TR criteria and was registered in days (i.e., even a single episode of delirium was considered to be a day of delirium). Functional status was assessed using the Katz activity of daily living (ADL) scale,19 which evaluates ability to perform six basic functions: feeding, transferring, toileting, dressing, bathing, and continence. One point is assigned if the individual is able to perform the activity independently and 0 if he or she is unable to do so, with total scores ranging from 0 (worst) to 6 (best). The ADL scale was completed based on caregiver or family interview with reference to the participant’s functional status 2 weeks before hip fracture. Mood was assessed using the 15-item Geriatric Depression Scale (GDS).20 Comorbidity was assessed on admission using the Charlson Comorbidity Index (CCI),21 a weighted index that considers 22 conditions and assigns each a score from 1 to 6 depending on its associated relative risk of mortality. Dementia was registered if a preexisting diagnosis of dementia or any previous reference to “cognitive impairment” from a physician (general practitioner or consultant) was certified in the participant’s medical history.
Severity of illnesses was evaluated using the Sequential Organ Failure Assessment (SOFA)22 on admission, a validated tool that predicted 1-month mortality in a large cohort of hospitalized older adults.23 The number and types of medications, together with hemoglobin (g/dL) and serum albumin (g/dL) levels on admission, were also recorded. Cognition was evaluated by preoperatively administering the Mini-Mental State Examination (MMSE)24 once delirium was excluded. The MMSE is a 30-point scale (range 0–30) used to estimate the presence and severity of cognitive impairment by briefly exploring several cognitive domains (orientation, registration and recall, attention and calculation, language, praxis). Scores less than 24 suggest cognitive impairment.
Malnutrition was screened for preoperatively on admission using the MNA-SF,25 a well-known validated tool to detect poor nutritional status that consists of six items: decline in food intake over the past 3 months, weight loss during the last 3 months, mobility, acute disease or psychological stress in the past 3 months, current neuropsychological problems, and body mass index (BMI). BMI was calculated using objectively measured anthropometric data. Calf circumference (according to item F2 of the MNA-SF) was determined using a measuring tape when BMI was not available. Total MNA-SF scores range from 0 to 14, with two cut-offs: a score of 12 or greater denotes normal nutritional status, a score from 8 to 11 denotes risk of malnutrition, and a score of 7 or less denotes overt malnutrition. Composite MNA-SF scores were collected in an electronic database, and the study population was divided into three groups according to the cut-offs, and their baseline and perioperative characteristics and incidence of postoperative delirium were compared. Finally, the baseline variables that might predict postoperative delirium were analyzed.
Statistical Analysis
Differences between the study groups were compared using the Student’s t-test for continuous variables and the chi-square test for categorical variables. Variables that were not normally distributed were compared using the Kruskal–Wallis test for independent samples and described as medians and interquartile ranges (IQRs).
To determine potential predictors of postoperative delirium (outcome), univariate logistic regression analyses were performed to test the associations between the various risk factors and the outcome. Multivariate logistic regression including the variables significantly associated with postoperative delirium at the univariate analyses was then performed. A multicollinearity diagnostic was performed to assess the validity of the regression model by calculating the values of tolerance and the variance inflation factor (1/tolerance). The multivariate logistic regression model was adjusted for age (continuous), sex (dichotomous), and CCI (continuous). An ADL score less than 5 was used to indicate prefracture disability, according to a previous study.26 Cognitive impairment (MMSE score < 24) and use of psychotropic medications, both categorical variables, were dichotomized (yes/no), and nutritional status was treated as a categorical variable (no malnutrition, at risk of malnutrition, overt malnutrition) according to MNA-SF scores.
All analyses were performed using SPSS version 22.0 (IBM Corp., Armonk, NY). Statistical significance was set at P ≤ .05, and all comparisons were two tailed.
RESULTS
The final cohort included 415 individuals (mean age 84.0 ± 6.6, 74.5% female). Table 1 shows the characteristics of the study population divided into three groups according to MNA-SF score: 152 (36.6%) were well nourished, 185 (44.6%) were at risk of malnutrition, and 78 (18.8%) were overtly malnourished. There were no significant differences in sex distribution between the groups. Malnourished participants and those at risk of malnutrition had a similar mean age, but both groups were significantly older than those who were not malnourished. Participants with overt malnutrition were more disabled (lower ADL score) and more cognitively impaired (lower MMSE score, higher prevalence of dementia) than those who were at risk of malnutrition or well nourished. Although the CCI did not differ significantly between the study groups, participants with overt malnutrition had higher ASA scores and a greater incidence of postoperative delirium. Mean time from admission to surgery and mean length of stay were similar for all the groups. Finally, malnourished participants had higher in-hospital mortality than those who were at risk of malnutrition or were well nourished.
Table 1.
Baseline and Perioperative Characteristics of 415 Individuals Undergoing Hip Fracture Surgery, According to Risk of Malnutrition As Assessed Using the Mini-Nutritional Assessment Short Form
| Characteristic | Not Malnourished, n = 152 | At Risk of Malnutrition, n = 185 | Malnourished, n = 78 | P-Value |
|---|---|---|---|---|
| Baseline | ||||
| Age, mean ± SD | 82.9 ± 6.5 | 84.5 ± 6.9 | 84.7 ± 6.3 | .047 |
| Female, n (%) | 112 (73.7) | 138 (74.6) | 59 (75.6) | .95 |
| Education, years, mean ± SD | 5(3) | 5(1) | 5(3) | .23 |
| Katz activity of daily living score, median (IQR) | 6(1) | 4 (4) | 3 (4) | <.001 |
| Mini-Mental State Examination score, median (IQR) | 26 (6) | 21 (12) | 19 (12) | <.001 |
| Charlson Comorbidity Index, median (IQR) | 1 (3) | 1 (2) | 2 (2) | .08 |
| History of dementia, n (%) | 13 (8.6) | 38 (20.5) | 23 (29.5) | <.001 |
| SOFA on admission, median (IQR) | 0(1) | 0(1) | 0 (2) | .91 |
| SOFA score ≥2, n (%) | 27 (17.8) | 38 (20.5) | 21 (26.9) | .27 |
| Serum albumin, g/dL | 3.4 ± 0.5 | 3.3 ± 0.6 | 3.1 ± 0.5 | <.001 |
| Hemoglobin on admission, g/dL | 12.6 ± 1.6 | 11.7 ± 2.2 | 11.9 ± 1.6 | <.001 |
| Total number of medications, median (IQR) | 5.5 (5) | 6 (5) | 6 (5) | .51 |
| Psychotropic drugs, n (%) | 57 (32.0) | 99 (40.1) | 82 (61.2) | <.001 |
| Time to surgery, days, mean ± SD | 2.6 ± 1.7 | 2.6 ± 1.8 | 2.8 ± 2.3 | .43 |
| Perioperative | ||||
| American Society of Anesthesiologists score, median (IQR) | 3(1) | 3(1) | 3 (0) | <.001 |
| Type of fracture, n (%) | ||||
| Femoral neck | 76 (50.0) | 92 (50.5) | 37 (48.7) | |
| Intertrochanteric | 65 (42.8) | 75 (41.2) | 36 (47.4) | .75 |
| Subtrochanteric | 11 (7.2) | 15 (8.2) | 3 (3.9) | |
| Type of surgery, n (%) | ||||
| Hemiarthroplasty | 58 (38.2) | 68 (36.8) | 26 (33.3) | .77 |
| Open reduction and internal fixation | 94 (61.8) | 117 (63.2) | 52 (66.7) | |
| Type of anesthesia, n (%) | ||||
| General | 40 (27.2) | 45 (25.3) | 17 (21.4) | .73 |
| Spinal | 107 (72.8) | 133 (74.7) | 59 (77.6) | |
| Postoperative delirium, n (%) | 19 (12.5) | 68 (36.8) | 37 (47.4) | <.001 |
| Duration of delirium, days | 3.4 ± 4.1 | 2.7 ± 2.1 | 3.1 ± 3.0 | .57 |
| Blood transfusions, units, median (IQR) | 0.9 ± 1.2 | 1.1 ± 1.5 | 1.2 ± 1.5 | .28 |
| Length of stay, days | 10.6 ± 14.4 | 9.8 ± 8.9 | 10.0 ± 5.6 | .79 |
| In-hospital mortality, n (%) | 0 (0.0) | 3(1.6) | 5 (6.4) | .003 |
SD = standard deviation; IQR = interquartile range; SOFA = sequential organ failure assessment.
The univariate logistic regressions showed a significant association between postoperative delirium and several variables (Table 2), although when the multivariate logistic regression was performed including all variables that were significantly associated during the univariate analyses, a significant association was found between postoperative delirium and age (continuous), male sex, MMSE score less than 24, history of dementia, and abnormal MNA-SF-based nutritional status (Table 3). The CCI was recalculated to avoid redundant information by subtracting 1 point from the total score of all participants with a history of dementia. Risk of malnutrition (odds ratio (OR) = 2.42, P = .006) and overt malnutrition (OR = 2.98, P = .004) were associated with postoperative delirium.
Table 2.
Univariate Logistic Regression Analysis of Potential Risk Factors for Postoperative Delirium
| Variable | Odds Ratio (95% CI) |
|---|---|
| Age | 1.1 (1.0–1.1)a |
| Male sex | 1.4 (0.9–2.2) |
| Education | 1.0 (0.9–1.0) |
| Activity of daily living impairment (<5) | 3.4 (2.2–5.3)a |
| Charlson Comorbidity Index | 1.1 (1.0–1.2) |
| Mini-Mental State Examination score <24 | 7.9 (4.6–13.6)a |
| History of dementia | 5.2 (3.0–8.8)a |
| Psychotropic drug use (yes/no) | 2.0 (1.3–3.1)a |
| Nutritional status (Mini-Nutritional Assessment Short Form score) (reference no malnutrition (≥12)) | |
| Risk of malnutrition (7–11) | 4.1 (2.3–7.2)a |
| Malnourished (<7) | 6.3 (3.3–12.2)a |
| American Society of Anesthesiologists | 1.7 (1.2–2.5)a |
| Score | |
| General anesthesia | 1.0 (0.6–1.7) |
Statistically significant; the one-digit approximation does not show significance in the reported 95% confidence interval (CI).
Table 3.
Multivariate Logistic Regression of Potential Risk Factors for Postoperative Delirium
| Covariates | Odds Ratio (95% CI) |
|---|---|
| Age | 1.0 (1.0–1.1)a |
| Male sex | 1.8 (1.0–3.2)a |
| Activity of daily living impairment (<5) | 0.9 (0.5–1.7) |
| Charlson Comorbidity Index | 1.0 (0.8–1.1) |
| Mini-Mental State Examination score <24 | 4.3 (2.3–8.0)a |
| History of dementia | 2.6 (1.4–5.0)a |
| Psychotropic drug use (yes/no) | 1.4 (0.8–2.4) |
| Nutritional status (Mini-Nutritional Assessment Short Form score) (reference no malnutrition (≥12)) | |
| Risk of malnutrition (7–11) | 2.5 (1.3–4.7)a |
| Malnourished (<7) | 3.0 (1.4–6.2)a |
| American Society of Anesthesiologists score | 1.5 (1.0–2.4) |
This model includes all variables that were significantly associated with postoperative delirium. The Charlson Comorbidity Index has been adjusted by subtracting 1 point from the total score of participants with a history of dementia (considered separately). The model has been checked for collinearity, which was excluded for all the included variables. Estimates are presented one digit beyond the decimal point.
Denotes statistical significance, even though the one-digit approximation does not allow visualization in the reported 95% confidence interval (CI).
DISCUSSION
This study, performed in a population of elderly adults undergoing surgical repair of hip fracture, found that being at risk of malnutrition or being overtly malnourished, according to the MNA-SF, is independently associated with postoperative delirium. In particular, a dose-effect relationship was found between poor nutritional status and postoperative delirium; individuals identified as being overtly malnourished were 3.0 times as likely as those with normal nutritional status to develop postoperative delirium, and those at risk of becoming malnourished were 2.5 times as likely. To the best of the authors’ knowledge, this is the first study to assess the role of being at risk of malnutrition (adopting the three-class stratification of the MNA-SF tool) in predicting postoperative delirium. A Taiwanese study explored the relationship between MNA-SF-assessed nutritional status and postoperative delirium in an Asian population, but that study differed substantially regarding the cohort (younger participants, mostly undergoing elective orthopedic surgery) and the approach (dichotomization of MNA-SF score instead of using three distinct categories).27
Postoperative delirium is a common complication of hip fracture, with an incidence ranging from 25% to 65%.5,28 It is associated with a number of poor clinical outcomes, including greater emotional burden for those with hip fracture29 and caregivers,30 worsening of cognitive31 and functional performance,26,32 greater rate of discharge to places other than home,32 and short- and long-term mortality.17,33 In addition, the longer the duration of delirium, the higher the risk of death after 6 months post-hip fracture surgery.16 Delirium may be prevented in 30% to 40% of cases.34 One such study, performed in individuals undergoing surgery for hip fracture, demonstrated that a comprehensive geriatric approach in the preoperative phase reduced the incidence of delirium by more than one-third and of severe delirium by more than half.28 Another study of 120 elderly adults with hip fracture found that a nurse-led interdisciplinary intervention program reduced duration and severity of delirium, although it did not affect its incidence.35
Therefore, because postoperative delirium may be prevented or at least mitigated in elderly adults with hip fracture, identification of its potential predictors could be an important target for clinicians and healthcare operators. Furthermore, by showing that a MNA-SF score of less than 11 independently predicts greater risk of development of postoperative delirium, clinicians may be able to identify individuals who are at risk of negative events and improve their prognostication attitude.36
These findings expand knowledge about delirium in individuals with hip fracture. The National Institute of Clinical Excellence recommends assessment of nutritional status for delirium prevention, but only a few studies are cited to support this assertion. In a study of 83 elderly adults undergoing elective surgery, nutritional assessment was one of the multicomponent interventions used to reduce postoperative delirium, but only 20% of participants had orthopedic problems, whereas the remaining had gastrointestinal, urological, or miscellaneous problems.37 Another study38 was a historically controlled trial during which baseline data were collected for 28 days from one group of participants and from another group during the subsequent 3 months. The investigators did not use standardized tools to detect poor nutritional status but instead evaluated nutritional status by determining whether dentures were fitted properly and whether participants were adequately positioned in front of their meals. Nutritional supplements and temporary nasogastric tubes were used if needed.38 One previous study adopted a similar nutritional assessment (inspection of correct denture usage and proper positioning at meals).28 Nutritional interventions were warranted by providing assistance at meals if needed, and feeding individuals who were unable to take food orally through temporary nasogastric tubes.28 One previous study used the full MNA tool (rather than the short form) to assess nutritional status; it was a randomized controlled trial of 174 individuals with delirium in six general medicine units from acute hospitals that found that only 9.2% of intervention participants and 13.8% of control participants were well nourished, but it did not assess whether poor nutritional status was an independent predictor of delirium.39 A recent study used the MNA-SF to determine nutritional status in a population of individuals undergoing elective (knee, hip, spinal) and urgent (hip fracture) orthopedic surgery27 and to assess its potential in predicting postoperative delirium. The authors found that MNA-SF score independently predicted postoperative delirium (OR = 2.85, 95% CI = 1.19–6.87), after adjusting for age, sex, MMSE score, and CCI, although only 17.5% of these individuals were at risk of undernutrition or were overtly undernourished (MNA-SF score ≤ 11), a finding that does not match with the typical features of older adults with hip fracture; 88.8% of study participants underwent elective rather than acute surgery.27
The current study found a high prevalence of malnutrition among 415 selected individuals because those at risk of malnutrition (n = 185) and those with overt malnutrition (n = 78) together accounted for approximately 63% of the study cohort. This finding is in line with the literature because the prevalence of poor nutritional status may range from 50% to 80%.9,35,39–41
The idea that poor nutritional status was associated in a dose-effect manner with postoperative delirium is noteworthy and suggests that there may be a continuum between levels of poor nutritional status and risk of developing this acute complication. Accordingly, awareness of the potential benefits of good nutritional status in elderly adults may include reducing the likelihood of developing postoperative delirium or mitigating its severity and duration in case of hospital admission. The finding that cognitive impairment is a predictor of postoperative delirium is in line with previous literature showing that it is a predisposing factor for the development of this acute complication in individuals undergoing surgical intervention.5,42
An implication of the current study is that the MNA-SF should be routinely administered to individuals with hip fracture before surgery to determine whether they are at risk of developing postoperative delirium.43 An advantage of using the MNA-SF is that it is quick and easy to administer. Strengths of this approach are the accurate method of diagnosing delirium, including the CAM algorithm and the DSM-IV-TR criteria; the prospective design aimed specifically at evaluating MNA-SF-based nutritional status to predict postoperative delirium; and the low degree of heterogeneity of the study population, which included elderly adults with hip fracture who were undergoing surgical repair.
Some methodological concerns about this investigation must be discussed in light of the findings. One limitation of the study is that it was performed at a single, urban, academic hospital, and thus the results might not be generalized to other settings. Another potential limitation is that preexisting dementia was reported if any citation in the individual’s medical history was found; dementia is frequently underreported in medical notes, and thus it may have been underestimated in the results. The MMSE was administered on admission to every participant as a part of a comprehensive assessment once the presence of delirium was excluded. Despite being performed in individuals who did not have delirium on admission, the beginning of a hospitalization for hip fracture does not represent the ideal time to evaluate cognitive impairment because of the presence of potential confounders such as pain. A further limitation pertains to the MNA-SF itself, which is partially based on information that the individuals or their proxies report, so recall bias cannot be completely excluded. Finally, delirium assessors were not blinded to preoperative MNA status and baseline characteristics.
In conclusion, assessing MNA-SF before surgery may help physicians predict risk of developing postoperative delirium in elderly adults undergoing hip fracture surgery. Because delirium is an emergency medical complication and therefore a potentially life-threatening condition affecting older hospitalized adults, the results of this study will have important implications. First, this work supports the routine use of tools to assess nutritional status to determine their risk of developing delirium. This should prompt the use of nonpharmacological methods of preventing postoperative delirium in high-risk individuals. Second, this evidence could be transferred to the setting of elective surgery to pave the way for interventional trials; nutritional interventions or supplementation strategies could be suitable methods of preventing postoperative delirium or reducing its severity and duration.
ACKNOWLEDGMENTS
Dr. Pasinetti has a Career Scientist Award in the Research and Development Unit and is the Director of the Basic and Biomedical Research and Training Program; Geriatric Research, Education, and Clinical Center; James J. Peters Veterans Affairs Medical Center. The contents of this manuscript do not represent the views of the U.S. Department of Veterans Affairs or the U.S. government. Preliminary data from this study were presented as an abstract at the 68th Gerontological Society of America annual scientific meeting, Orlando, Florida, November 18–22, 2015. We extend our sincere appreciation to Dr. Federico Rea, MSc, for his contribution in the statistical review of the final version of this manuscript.
Footnotes
Conflict of Interest: The authors declare that the present manuscript was unfunded and that they have no conflicts of interest to disclose in relation to its preparation. Data collection and all the analyses comply with the current Italian laws and the ethical committee of the University of Milano-Bicocca. All individuals included in the database (or their legal proxies) gave permission to receive hospital treatments, for recording of personal healthcare information, and for the use of these data for research purposes. All written consent forms are stored in the archive of San Gerardo Hospital ASST Monza. Data have been de-identified and protected, in line with the privacy policy of ASST Monza and University of Milano-Bicocca. This prospective study was conducted according to the Helsinki II Declaration.
Sponsor’s Role: None.
REFERENCES
- 1.Melton LJ, Kearns AE, Atkinson EJ et al. Secular trends in hip fracture incidence and recurrence. Osteoporos Int 2009;20:687–694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Giversen IM. Time trends of age-adjusted incidence rates of first hip fractures: A register-based study among older people in Viborg County, Denmark, 1987–1997. Osteoporos Int 2006;17:552–564. [DOI] [PubMed] [Google Scholar]
- 3.Mazzola P, De Filippi F, Castoldi G et al. A comparison between two co-managed geriatric programmes for hip fractured elderly patients. Aging Clin Exp Res 2011;23:431–436. [DOI] [PubMed] [Google Scholar]
- 4.Siddiqi N, House AO, Holmes JD. Occurrence and outcome of delirium in medical in-patients: A systematic literature review. Age Ageing 2006;35:350–364. [DOI] [PubMed] [Google Scholar]
- 5.Inouye SK, Westendorp RG, Saczynski JS. Delirium in elderly people. Lancet 2014;383:911–922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Goisser S, Schrader E, Singler K et al. Malnutrition according to Mini Nutritional Assessment is associated with severe functional impairment in geriatric patients before and up to 6 months after hip fracture. J Am Med Dir Assoc 2015;16:661–667. [DOI] [PubMed] [Google Scholar]
- 7.Drevet S, Bioteau C, Maziere S et al. Prevalence of protein-energy malnutrition in hospital patients over 75 years of age admitted for hip fracture. Orthop Traumatol Surg Res 2014;100:669–674. [DOI] [PubMed] [Google Scholar]
- 8.Takeuchi K, Aida J, Ito K et al. Nutritional status and dysphagia risk among community-dwelling frail older adults. J Nutr Health Aging 2014;18:352–357. [DOI] [PubMed] [Google Scholar]
- 9.Olofsson B, Stenvall M, Lundstrom M et al. Malnutrition in hip fracture patients: An intervention study. J Clin Nurs 2007;16:2027–2038. [DOI] [PubMed] [Google Scholar]
- 10.Li HJ, Cheng HS, Liang J et al. Functional recovery of older people with hip fracture: Does malnutrition make a difference? J Adv Nurs 2013;69:1691–1703. [DOI] [PubMed] [Google Scholar]
- 11.Gumieiro DN, Rafacho BP, Goncalves AF et al. Mini Nutritional Assessment predicts gait status and mortality 6 months after hip fracture. Br J Nutr 2013;109:1657–1661. [DOI] [PubMed] [Google Scholar]
- 12.Ahmed S, Leurent B, Sampson EL. Risk factors for incident delirium among older people in acute hospital medical units: A systematic review and meta-analysis. Age Ageing 2014;43:326–333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.American Society of Anesthesiologists. New classification of physical status. Anesthesiology 1963;24:111. [Google Scholar]
- 14.Inouye SK, van Dyck CH, Alessi CA et al. Clarifying confusion: The confusion assessment method. A new method for detection of delirium. Ann Intern Med 1990;113:941–948. [DOI] [PubMed] [Google Scholar]
- 15.American Psychiatric Association. DSM-IV-TR: Diagnostic and Statistical Manual of Mental Disorders, 4th Ed., Text Revision. Washington, D.C.: American Psychiatric Association, 2000. [Google Scholar]
- 16.Bellelli G, Mazzola P, Morandi A et al. Duration of postoperative delirium is an independent predictor of 6-month mortality in older adults after hip fracture. J Am Geriatr Soc 2014;62:1335–1340. [DOI] [PubMed] [Google Scholar]
- 17.Mazzola P, Bellelli G, Broggini V et al. Postoperative delirium and pre-fracture disability predict 6-month mortality among the oldest old hip fracture patients. Aging Clin Exp Res 2015;27:53–60. [DOI] [PubMed] [Google Scholar]
- 18.Bellelli G, Mazzone A, Morandi A et al. The effect of an impaired arousal on short- and long-term mortality of elderly patients admitted to an acute geriatric unit. J Am Med Dir Assoc 2016;17:214–219. [DOI] [PubMed] [Google Scholar]
- 19.Katz S, Ford AB, Moskowitz RW et al. Studies of illness in the aged. The Index of ADL: A standardized measure of biological and psychosocial function. JAMA 1963;185:914–919. [DOI] [PubMed] [Google Scholar]
- 20.Sheikh JI, Yesavage JA, eds. Geriatric Depression Scale (GDS): Recent evidence and development of a shorter version In: Brink TL, ed. Clinical Gerontology: A Guide to Assessment and Intervention. New York: Haworth Press; 1986, pp 165–173. [Google Scholar]
- 21.Charlson ME, Pompei P, Ales KL et al. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J Chronic Dis 1987;40:373–383. [DOI] [PubMed] [Google Scholar]
- 22.Ferreira FL, Bota DP, Bross A et al. Serial evaluation of the SOFA score to predict outcome in critically ill patients. JAMA 2001;286:1754–1758. [DOI] [PubMed] [Google Scholar]
- 23.Mazzola P, Bellelli G, Perego S et al. The sequential organ failure assessment score predicts 30-day mortality in a geriatric acute care setting. J Gerontol A Biol Sci Med Sci 2013;68A:1291–1295. [DOI] [PubMed] [Google Scholar]
- 24.Folstein MF, Folstein SE, McHugh PR. ‘Mini-mental state’. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 1975;12:189–198. [DOI] [PubMed] [Google Scholar]
- 25.Kaiser MJ, Bauer JM, Ramsch C et al. Validation of the Mini Nutritional Assessment short-form (MNA-SF): A practical tool for identification of nutritional status. J Nutr Health Aging 2009;13:782–788. [DOI] [PubMed] [Google Scholar]
- 26.Marcantonio ER, Flacker JM, Michaels M et al. Delirium is independently associated with poor functional recovery after hip fracture. J Am Geriatr Soc 2000;48:618–624. [DOI] [PubMed] [Google Scholar]
- 27.Chu CS, Liang CK, Chou MY et al. Short-Form Mini Nutritional Assessment as a useful method of predicting the development of postoperative delirium in elderly patients undergoing orthopedic surgery. Gen Hosp Psychiatry 2016;38:15–20. [DOI] [PubMed] [Google Scholar]
- 28.Marcantonio ER, Flacker JM, Wright RJ et al. Reducing delirium after hip fracture: A randomized trial. J Am Geriatr Soc 2001;49:516–522. [DOI] [PubMed] [Google Scholar]
- 29.Morandi A, Lucchi E, Turco R et al. Delirium superimposed on dementia: A quantitative and qualitative evaluation of patient experience. J Psychosom Res 2015;79:281–287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Morandi A, Lucchi E, Turco R et al. Delirium superimposed on dementia: A quantitative and qualitative evaluation of informal caregivers and health care staff experience. J Psychosom Res 2015;79:272–280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Davis DH, Muniz Terrera G, Keage H et al. Delirium is a strong risk factor for dementia in the oldest-old: A population-based cohort study. Brain 2012;135(Pt 9):2809–2816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Krogseth M, Wyller TB, Engedal K et al. Delirium is a risk factor for institutionalization and functional decline in older hip fracture patients. J Psychosom Res 2014;76:68–74. [DOI] [PubMed] [Google Scholar]
- 33.Witlox J, Eurelings LS, de Jonghe JF et al. Delirium in elderly patients and the risk of postdischarge mortality, institutionalization, and dementia: A meta-analysis. JAMA 2010;304:443–451. [DOI] [PubMed] [Google Scholar]
- 34.Inouye SK, Bogardus ST Jr, Charpentier PA et al. A multicomponent intervention to prevent delirium in hospitalized older patients. N Engl J Med 1999;340:669–676. [DOI] [PubMed] [Google Scholar]
- 35.Milisen K, Foreman MD, Abraham IL et al. A nurse-led interdisciplinary intervention program for delirium in elderly hip-fracture patients. J Am Geriatr Soc 2001;49:523–532. [DOI] [PubMed] [Google Scholar]
- 36.Carpintero P, Caeiro JR, Carpintero R et al. Complications of hip fractures: A review. World J Orthop 2014;5:402–411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Harari D, Hopper A, Dhesi J et al. Proactive care of older people undergoing surgery (‘POPS’): Designing, embedding, evaluating and funding a comprehensive geriatric assessment service for older elective surgical patients. Age Ageing 2007;36:190–196. [DOI] [PubMed] [Google Scholar]
- 38.Wong Tin Niam DM, Bruce JJ, Bruce DG. Quality project to prevent delirium after hip fracture. Australas J Ageing 2005;24:174–177. [Google Scholar]
- 39.Pitkala KH, Laurila JV, Strandberg TE et al. Multicomponent geriatric intervention for elderly inpatients with delirium: A randomized, controlled trial. J Gerontol A Biol Sci Med Sci 2006;61:176–181. [DOI] [PubMed] [Google Scholar]
- 40.Pimlott BJ, Jones CA, Beaupre LA et al. Prognostic impact of pre-operative albumin on short-term mortality and complications in patients with hip fracture. Arch Gerontol Geriatr 2011;53:90–94. [DOI] [PubMed] [Google Scholar]
- 41.Cameron ID, Kurrle SE, Uy C et al. Effectiveness of oral nutritional supplementation for older women after a fracture: Rationale, design and study of the feasibility of a randomized controlled study. BMC Geriatr 2011;11:32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Oh ES, Li M, Fafowora TM et al. Preoperative risk factors for postoperative delirium following hip fracture repair: A systematic review. Int J Geriatr Psychiatry 2015;30:900–910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.National Institute for health and Clinical Excellence NICE quality standard 63 guidance.nice.org.uk/qs63, July 2014. [Google Scholar]