Abstract
Background.
Between 2001 and 2010 six research groups conducted coordinated prospective studies of carpal tunnel syndrome (CTS) incidence among US workers from various industries to estimate exposure-response relationships.
Objective.
This analysis examined the presence and magnitude of confounding between biomechanical and workplace psychosocial factors and incidence of dominant-hand CTS.
Methods.
1605 participants, without CTS at enrollment, were followed for up to 3.5 years (2471 person-years). Demographic information, medical history and workplace psychosocial stress measures were collected at baseline. Individual workplace biomechanical exposures were collected for each task and combined across the workweek using time-weighted-averaging (TWA). CTS case-criteria were based on symptoms and results of electrophysiological testing. Hazard ratios were estimated with Cox proportional hazard models. Confounding was assessed using causal diagrams and an empirical criterion of 10% or greater change in effect estimate magnitude.
Results.
There were 109 incident CTS cases (IR=4.41/100 person-years; 6.7% cumulative incidence). The relationships between CTS and Forceful Repetition Rate,% time Forceful Hand Exertion, and the TLV-HAL were slightly confounded by Decision Latitude with effect estimates being attenuated toward the null (10%−14% change) after adjustment. The risk of CTS among participants reporting high Job Strain was attenuated toward the null by 14% after adjusting for the HAL Scale or the % time Forceful Hand Exertions.
Conclusion.
Although attenuation of the relationships between CTS and some biomechanical and work psychosocial exposures was observed after adjusting for confounding, the magnitudes were small and confirmed biomechanical and work psychosocial exposures as independent risk factors for incident CTS.
Keywords: prospective, carpal tunnel syndrome, biomechanical exposure, psychosocial exposure, confounding
Introduction
Carpal tunnel syndrome (CTS) is a common work-related peripheral entrapment neuropathy of the median nerve at the wrist that results in high medical treatment costs, lost work time and associated disability1. Early studies of CTS lacked a common case definition, were usually cross sectional in design, and had limited ability to adjust for confounding due to small sample sizes2–6. To address this research gap, six research groups designed coordinated, multi-year, prospective epidemiological studies of US production and service workers from a variety of industries. Detailed subject-level data on biomechanical and work psychosocial exposures were combined with longitudinal assessment of symptoms, physical examination results, electrophysiological measures and personal health and socio-demographic data7. Data from each study were combined into one data set yielding a cohort that was diverse and generalizable to service and manufacturing workers in the US.
A prior publication reported on the relationship between work psychosocial exposure and CTS8. In those analyses, high psychological job demand was associated with CTS risk (HR=1.57; 95% CI: 1.06–2.33), and high decision latitude (control) was protective (HR=0.73; 95% CI: 0.51–1.04). Participants with high job strain (simultaneous high demand and low control) had a nearly 2-fold increase in risk (HR=1.90; 95%CI: 1.11–3.14) compared to those with low job strain (simultaneous high control and low demand), and subjects with high social support had half of the risk of incident CTS compared to those with low social support (HR= 0.54; 95%CI: 0.31–0.95).
We also reported exposure-response relationships between several biomechanical risk factors and CTS incidence, including measures of forceful hand exertion9,10. Participants exposed to higher levels of hand force had a 50–117% increase in the rate of CTS, yet no such increase was observed for those exposed to higher levels of repetition or those spending more time in combinations of any hand exertion (exertions of any force).
One objective of combining data sets across studies was to have sufficient power to estimate exposure-response relationships between CTS and personal, biomechanical and psychosocial factors while minimizing bias from confounding. However, since prior analyses maximized power by retaining larger sample sizes and adjusted models only by personal factors and dissimilar biomechanical exposures (for biomechanical models), none of the prior analyses evaluated both biomechanical exposure and work psychosocial exposures simultaneously (which would have resulted in a smaller sample). To assess the possibility that the relationship between work psychosocial exposure and CTS is confounded by biomechanical exposure, and the possibility that the observed association between biomechanical exposure and CTS is confounded by work psychosocial exposure, further analyses were warranted. The objective of the current analysis was to assess the presence and magnitude of confounding by non-causal pathways using a subset of the cohort who had both biomechanical and work psychosocial information.
Methods
Study Participants and Procedures
Participants.
This cohort included participants enrolled in four different prospective studies with common data on personal, biomechanical, and work psychosocial exposure previously pooled to increase statistical power and generalizability. Participants in each study were at least 18 years of age and employed at a company where workers performed hand-intensive activities. Details on the study design and methods for pooling exposure and health outcome data are available elsewhere7,11. A total of 1995 workers were eligible for participation (Supplemental Figure 1). Subjects were excluded from the analyses if they met the case criteria for CTS or possible polyneuropathy at enrollment (i.e., baseline), resulting in 1605 cohort participants.
Data Collection.
Questionnaires were administered to participants at enrollment to collect information on work history, demographics, medical history, musculoskeletal symptoms and work psychosocial stress. Biomechanical exposures were measured at the individual task level at enrollment and measured again if the job changed, thus creating a time series of biomechanical exposure information. Electrodiagnostic studies (EDS) of median and ulnar nerve function across the wrist were administered to all participants either (a) all participants at baseline and annually or (b) to those reporting upper limb symptoms7. Follow-up assessments of symptoms and EDS were performed at different intervals across the four studies. Investigators responsible for collecting health outcome data were blinded to participant biomechanical and psychosocial exposure status.
Personal Factors.
Information on participant age, gender, body mass index (BMI), race/ethnicity, education, smoking status, hand dominance, and co-morbid medical conditions such as rheumatoid arthritis, diabetes mellitus, and thyroid disease were collected. Prior carpal tunnel release surgery and disorders of the distal upper extremity were also assessed. General health was assessed on a 5-point scale. Total years worked at the current employer was collected at study enrollment.
Work Psychosocial Factors.
Information on work psychosocial factors was collected with scales from the Job Content Questionnaire (JCQ). The JCQ Psychological Job Demand and Decision Latitude scales were each dichotomized by splitting the distributions at their respective median values. A four-category Job Strain variable was created by assigning participants to one of the four quadrants resulting from the two split distributions (i.e., high demand, low control; low demand, low control; high demand, high control; and low demand, high control)12. The a priori putative high job strain category was defined as the job strain quadrant characterized by high demand and low control. The Job Strain Ratio was calculated by dividing the Psychological Demand score by the Decision Latitude score.
Biomechanical Exposure.
Seven measures of workplace biomechanical exposures collected at the task level for each participant were used in this analysis; three measures quantified singular exposures (Peak Hand Force, Total Repetition Rate, % time All Exertions), three measures quantified concurrent exposures (HAL Scale, Forceful Repetition Rate, % time Forceful Exertions), and one was a composite measure (ACGIH Threshold Limit Value for Hand Activity Level (TLV-HAL)). Exposure estimates were based on a blinded trained analyst’s observation of each subject performing his/her usual work tasks, measurement of hand forces, weights of tools, force matching required to complete each task, videotape analysis of the task, and interviews of subjects or their supervisors.
Estimates of the highest analyst rated hand force required for each task (Peak Hand Force) was made using the Borg CR-10 rating scale13. The repetitiveness of tasks and allowable recovery were estimated using the analyst rated HAL Scale. Other temporal exertion patterns for repetition and duty cycle were determined by detailed time studies of task-level videos11 and included (a) the number of all hand exertions per minute (Total Repetition Rate), (b) the number of forceful hand exertions per minute (Forceful Repetition Rate), (c) the percent of time for all hand exertions (% time All Exertions) and (d) forceful hand exertions (% time Forceful Exertions). Forceful exertions were defined as those requiring ≥9N pinch force or ≥45N of power grip force or a Borg CR-10 ≥2. Although three approaches to summarize task level exposure at the job level have been previously described11, only TWA summary measures (which included information from all tasks performed) were used for this analysis.
Outcome.
The study outcome was incident CTS of the dominant hand and required (i) symptoms of tingling, numbness, burning, or pain in the thumb, index finger or long finger and (ii) temperature adjusted (32° C) electrodiagnostic study (EDS) results demonstrating median mononeuropathy at the wrist7,14. Median mononeuropathy was defined as (1) peak median sensory latency >3.7ms or onset median sensory latency >3.2ms at 14cm, (2) median distal motor latency >4.5ms, (3) transcarpal sensory difference of > 0.85ms (difference between median and ulnar sensory nerve latency across the wrist), or (4) an absent sensory latency consistent with abnormal EDS and EDS evidence of normal ulnar nerve physiology (i.e., ulnar sensory peak latency <3.68 ms). Participants with symptoms consistent with CTS and concurrent abnormal median and ulnar nerve EDS were classified as possible polyneuropathy and were censored at the time that the case definition criterion was met7. Individuals who were symptomatic without a subsequent EDS were censored at the last date of known CTS case status. Person-time was calculated as the number of days from enrollment to an abnormal EDS with symptoms or censoring due to possible polyneuropathy, dropout or study termination.
Analytical Approach
To help guide this analysis, we constructed causal diagrams (directed acyclic graph (DAG)) to visually encode the hypothesized relationships between covariates, time varying exposures and CTS (Figures 1a&b), and used them to perform a pathway analysis. DAGs are useful tools to identify potential confounders that may bias observed exposure-response associations and to distinguish confounders from intermediate variables on the causal pathway for which adjustment is inappropriate15. A pathway analysis is a logical sequence of exploring causal and non-causal pathways between exposures, covariates and outcomes portrayed in a DAG to better understand the relationships amongst the variables. In a DAG, the points representing variables are called “nodes” and causal pathways from one node to another are depicted with a line or arrow referred to as an “edge” 16. The directionality of the pathway is designated with an arrowhead. A directed or causal path is defined as an unbroken route traced along edges connecting adjacent nodes, entering through the tail and leaving through the arrowhead16. A bidirectional arrow indicating a common cause (U) of two nodes (Biomech1←U→Psychsoc1), can represent multiple variables that were not or could not have been measured, yet were a common ancestor of two nodes, thus creating a non-causal pathway. Essentially, U depicts how one exposure-effect association can be confounded by another despite neither variable being a direct cause of each other. Non-causal pathways from exposure to the outcome include those in the opposite direction of an arrowhead (i.e., a “backdoor path”). To estimate the causal exposure-response relationship using a DAG, all non-causal paths need to be blocked by adjusting for appropriate variables. Adjustment through stratification or conditioning is indicated by a rectangle around the node. Pathways can also be blocked by “colliders” (two arrows pointed to the same variable along the pathway of interest) and caution should be taken not to adjust for a collider which would then “open” the non-causal pathway15. Additionally, adjustment should not be made for any intermediary variables (variables along the causal path and between the primary exposure of interest and the outcome). It is also important to separate exposures and other time-varying covariates into separate nodes by time. For example, when assessing the causal relationship between baseline psychosocial factors and CTS (Figure 1b), it is reasonable to adjust for biomechanical exposure at baseline (Biomech1) to block a non-causal back door pathway, but not to adjust for biomechanical exposure at time two (Biomech2) since it is plausible that work psychosocial stress could cause someone to change his/her job, and thus his/her exposure, making subsequent biomechanical exposure (Biomech2) an intermediary variable (Psychsoc1→ Biomech2→CTS). This approach is based on the assumption that U does not cause CTS other than through measured variables on the DAG.
Figure 1.
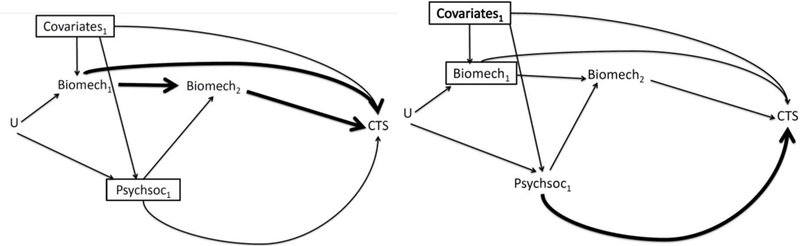
Directed acyclic graphs showing the hypothesized relationship between baseline personal covariates, biomechanical and work psychosocial risk factors at up to two time points. U represents some unmeasured baseline variable related to the specific job someone chooses, (such as educational status) that may be related to both biomechanical and psychosocial exposure. 1a) DAG shows the relationship between biomechanical exposure and CTS (bolded line) 1b) DAG shows the relationship between work psychosocial factors and CTS (bolded line).
Although the causal pathways between work psychosocial exposures, biomechanical exposures and CTS were previously reported, the potential confounding of one class of exposures by the other was not investigated. For example, it is plausible that there is some unmeasured attribute, such as educational status, (Figure 1a, U) associated with both biomechanical and work psychosocial exposures (Biomech1←U→Psychsoc1), thus creating a backdoor pathway between biomechanical exposure at baseline and CTS through work psychosocial factors (Figure 1a, Biomech1←U→Psychsoc1→CTS). Therefore, reassessing the exposure-response relationship of interest (Figure 1a, bold line) while adjusting for work psychosocial exposure at baseline provides important information about the presence and magnitude of potential confounding. Similarly, in the assessment of the relationship between work psychosocial factors and CTS (Figure 1b, bold lines), adjusting for baseline biomechanical exposure (Figure 1b, Biomech1) may reduce confounding bias.
Statistical analysis
Correlations between exposures were estimated using the Spearman rank correlation coefficient. Hazard ratios (HR) between exposures and incident CTS were estimated using Cox proportional hazards regression with robust confidence intervals. Guided by DAGs, the models were adjusted for potential confounding by personal factors related to both exposure and outcome that were not on the causal pathway. Using the forward stepwise procedure, variables were retained in the model if inclusion resulted in a change of the effect estimate of the primary exposure variable by 10% or more17. Ultimately, age, gender, BMI and study site were included in all models. Models where specific biomechanical exposures were the primary exposure of interest were adjusted for dissimilar biomechanical exposures (ie., exposures of a different type)9. For example, the relationship between Peak Hand Force and CTS was adjusted for Total Repetition Rate and wrist posture whereas the model assessing the relationship between Forceful Repetition Rate and CTS was only adjusted for wrist posture. Assessment of confounding of one class of exposures by another (e.g., biomechanical, work psychosocial) used the same process and criteria described above. All analyses were implemented with the Stata statistical package (Stata, College Station, TX).
Results
Of the initial 1995 workers at baseline, 177 were excluded due to prevalent carpal tunnel syndrome (N=163) or possible polyneuropathy (N=14) at enrollment. Of the remaining 1818 eligible workers, 202 were excluded from the analyses due to lack of exposure data or loss to follow-up resulting in a participation rate of 89.9% (n=1605) (Supplemental Figure 1). There were 109 (6.7%) incident CTS cases observed across 2,471 person-years of follow up with an incidence rate of 4.41 per 100 person-years (Table 1). The mean age at baseline was 40.3 years (SD = 10.8) and 90% reported no medical condition. The median years worked at the same company at baseline was 8.4 years (IQR: 2–12) and most participants (79%) worked the day shift. The median follow up time was 2 years (IQR= 1–2.9). Biomechanical and psychosocial exposures varied widely across subjects (Supplemental Table 1).
Table 1.
Demographic characteristics. (%)
| Demographics (cohort with exposure data) n(%) | Total N=1605 | N | Cases(n) |
|---|---|---|---|
| Gender | 1605 | 109 | |
| Male | 888 (55%) | 51 | |
| Female | 717 (45%) | 58 | |
| Age (years) | 1605 | 109 | |
| < 30 years of age | 324 (20%) | 19 | |
| ≥ 30 & <40 years of age | 424 (26%) | 23 | |
| ≥ 40 & <50 years of age | 531 (33%) | 40 | |
| ≥ 50 years of age | 326 (20%) | 27 | |
| Ethnicity | 1581 | 106 | |
| Caucasian | 881 (55%) | 69 | |
| Hispanic | 415 (26%) | 12 | |
| African American | 118 (7%) | 11 | |
| Asian | 124 (8%) | 9 | |
| Other | 43 (3%) | 5 | |
| Education | 1596 | 108 | |
| Some High School or less | 390 (24%) | 18 | |
| High School Graduate or above | 1206 (76%) | 90 | |
| Handedness | 1605 | 109 | |
| Left Handed | 126 (8%) | 12 | |
| Right Handed | 1479 (92%) | 97 | |
| Body Mass Index | 1599 | 109 | |
| Body Mass Index (<25) | 542 (34%) | 23 | |
| Body Mass Index (≥25 & <30: Overweight) | 556 (35%) | 30 | |
| Body Mass Index (≥30: Obese) | 501 (31%) | 56 | |
| General Health | 1279 | 94 | |
| Very Good or Excellent | 501 (39%) | 29 | |
| Good | 584 (46%) | 49 | |
| Fair or Poor | 194 (15%) | 16 | |
| Medical Condition | 1605 | 109 | |
| No Medical Condition | 1438 (90%) | 93 | |
| Current Medical Condition | 167 (10%) | 16 | |
| Diabetes | 61 (4%) | 5 | |
| Rheumatoid Arthritis | 23 (1%) | 0 | |
| Thyroid Disease (hyper/hypo) | 78 (5%) | 11 | |
| Pregnancy | 12 (1%) | 0 | |
| Smoking Status | 1598 | 107 | |
| Never Smoked | 927 (58%) | 58 | |
| Currently Smokes | 415 (26%) | 31 | |
| Previously Smoked | 256 (16%) | 18 |
Among the biomechanical exposures, moderate to strong correlations were observed for measures that included some measure of force (Table 2). None of the work psychosocial measures had correlations with any of the biomechanical measures of greater than r = 0.26.
Table 2.
Correlations between personal, biomechanical and work psychosocial exposure variables.
| Psychol. Demand |
Decision Latitude |
Total Support |
Job Strain Ratio |
Peak Hand Force |
HAL Scale |
Repetition Rate |
Forceful Repetition Rate |
% Time Total Exert. |
% Time Forceful Exertion |
ACGIH TLV for HAL |
|
|---|---|---|---|---|---|---|---|---|---|---|---|
| Psychological Demand | 1.00 | ||||||||||
| Decision Latitude | −0.08 | 1.00 | |||||||||
| Total Support | −0.20 | 0.34 | 1.00 | ||||||||
| Job Strain Ratio | 0.84 | −0.57 | −0.32 | 1.00 | |||||||
| Peak Hand Force | 0.09 | 0.04 | 0.10 | 0.06 | 1.00 | ||||||
| HAL Scale | 0.22 | 0.18 | 0.18 | 0.08 | 0.47 | 1.00 | |||||
| Total Repetition Rate | −0.04 | −0.11 | −0.25 | 0.04 | −0.27 | −0.28 | 1.00 | ||||
| Forceful Repetition Rate | 0.18 | 0.06 | −0.05 | 0.13 | 0.56 | 0.39 | 0.21 | 1.00 | |||
| % Time Total Exertion | −0.26 | −0.02 | −0.13 | −0.18 | −0.53 | −0.56 | 0.57 | −0.38 | 1.00 | ||
| % Time Forceful Exertion | 0.15 | 0.08 | −0.01 | 0.09 | 0.53 | 0.33 | 0.17 | 0.91 | −0.29 | 1.00 | |
| ACGIH TLV for HAL | 0.18 | 0.11 | 0.17 | 0.09 | 0.86 | 0.78 | −0.37 | 0.60 | −0.68 | 0.55 | 1.00 |
When models estimating associations between biomechanical exposures and CTS were adjusted for Psychological Demand (Table 3), effect estimates were minimally affected (1% to 4% change). However, when adjusted for Decision Latitude, effect estimates for Forceful Repetition Rate,% time Forceful Exertion, and the TLV-HAL were decreased from 10% to 14% in comparison to associations without adjustment for Decision Latitude. There was a similar pattern for models adjusted for the Job Strain Ratio, however, only the effect estimates for Forceful Repetition Rate and CTS changed by more than 10%.
Table 3.
Biomechanical exposure and risk of CTS, (i) unadjusted for work psychosocial exposure, and adjusted for: (ii) Job Strain Ratio (iii) Psychological Demand, and (iv) Decision Latitude. All models (i-iv) are adjusted for age, gender, BMI, study site and dissimilar biomechanical exposures9.
| Cutoffs | Cohort | Cases | (i) Unadjusted for Psychosocial Factors HR (95% CI) |
(ii) adj. for Job Strain Ratio HR (95% CI) |
(iii) adj. for Psychological Demand HR (95% CI) |
(iv) adj. for Decision Latitude HR (95% CI) |
|||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Peak Force (CR-10) | 1109 | 79 | |||||||||
| Lower Half | ≤ 3 | 42 | 1.00 | - | 1.00 | - | 1.00 | - | 1.00 | - | |
| Upper Half | >3 | 37 | 1.38 | (0.85–2.26) | 1.30 | (0.79–2.13) | 1.37 | (0.84–2.24) | 1.28 | (0.78–2.08) | |
| Total Repetition Rate | 1109 | 79 | |||||||||
| Lower Half | ≤ 16.4 | 47 | 1.00 | - | 1.00 | - | 1.00 | - | 1.00 | - | |
| Upper Half | > 16.4 | 32 | 1.03 | (0.61–1.74) | 0.96 | (0.57–1.62) | 1.01 | (0.60–1.70) | 0.97 | (0.57–1.65) | |
| % Time All Exertions | 1109 | 79 | |||||||||
| Lower Half | ≤ 68% | 38 | 1.00 | - | 1.00 | - | 1.00 | - | 1.00 | - | |
| Upper Half | > 68% | 41 | 1.18 | (0.75–1.88) | 1.19 | (0.75–1.89) | 1.19 | (0.75–1.90) | 1.16 | (0.73–1.84) | |
| HAL Scale | 1370 | 90 | |||||||||
| Lower Half | ≤ 4.4 | 41 | 1.00 | - | 1.00 | - | 1.00 | - | 1.00 | - | |
| Upper Half | > 4.4 | 49 | 1.90 | (1.17–3.10) | 1.82 | (1.12–2.97) | 1.89 | (1.16–3.07) | 1.79 | (1.09–2.93) | |
| Forceful Repetition Rate | 1423 | 92 | |||||||||
| Lower Half | ≤ 4.9 | 51 | 1.00 | - | 1.00 | - | 1.00 | - | 1.00 | - | |
| Upper Half | > 4.9 | 41 | 1.41 | (0.87–2.30) | 1.26 | (0.75–2.12) | 1.35 | (0.82–2.24) | 1.23 | (0.74–2.05) | |
| % Time Forceful Exertions | 1423 | 92 | |||||||||
| Lower Half | ≤ 19% | 43 | 1.00 | - | 1.00 | - | 1.00 | - | 1.00 | - | |
| Upper Half | > 19% | 49 | 2.17 | (1.36–3.46) | 2.03 | (1.26–3.26) | 2.11 | (1.32–3.39) | 1.95 | (0.62–1.96) | |
| ACGIH TLV for HAL | 1390 | 95 | |||||||||
| Lower Half | ≤ 0.56 | 41 | 1.00 | - | 1.00 | - | 1.00 | - | 1.00 | - | |
| Upper Half | > 0.56 | 54 | 1.85 | (1.20–2.86) | 1.71 | (1.10–2.66) | 1.84 | (1.19–2.84) | 1.68 | (1.07–2.62) | |
Due to differences in the number of participants who were missing data, models varied in sample size. For clarity, only models of similar sample size are presented in Table 4. Each adjusted model was compared to unadjusted models of the exact same cohort. All adjusted models in the same table had unadjusted models with virtually identical hazard ratios; thus only one unadjusted model is shown. The effect estimates quantifying the relationship between Psychological Demand,Decision Latitude and CTS were slightly attenuated toward the null when adjusted for the % time Forceful Hand Exertion (11%) and the HAL Scale (10%) (Table 4). The effect estimates quantifying the relationship between high Job Strain and CTS had similar magnitudes of attenuation when adjusted for Peak Hand Force,HAL Scale and % time Forceful Hand Exertion.
Table 4.
a) Work Psychosocial exposure and risk of CTS, (i) unadjusted for biomechanical exposure, and adjusted for: (ii) Peak hand Force (iii) HAL Scale, (iv) Forceful Repetition Rate, (v) % Time Forceful Exertions, (vi) Total Repetition Rate (vii) % Time All Exertions and (viii) ACGIH TLV for HAL. All models (i-viii) are adjusted for age, gender, BMI, study site.
| Cut- offs |
(N) | (n) | (i) Unadjusted HR (95% CI) |
(ii) adj. for Peak Hand Force HR (95% CI) |
(iii) adj. for HAL Scale HR (95% CI) |
(iv) adj. for Forceful Repetition Rate HR (95% CI) |
(v) adj. for % Time Forceful Hand Exertions HR (95% CI) |
||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Psychological Demand | 1476 | 99 | |||||||||||
| Lower Half | < 31 | 40 | 1.00 | - | 1.00 | - | 1.00 | - | 1.00 | - | 1.00 | - | |
| Upper Half | ≥ 31 | 59 | 1.35 | (0.91–2.01) | 1.32 | (0.89–1.97) | 1.33 | (0.89–1.97) | 1.31 | (0.87–1.97) | 1.21 | (0.80–1.83) | |
| Decision Latitude | 1469 | 98 | |||||||||||
| Lower Half | < 60 | 42 | 1.00 | - | 1.00 | - | 1.00 | - | 1.00 | - | 1.00 | - | |
| Upper Half | ≥ 60 | 56 | 0.83 | (0.55–1.26) | 0.88 | (0.58–1.34) | 0.95 | (0.62–1.45) | 0.85 | (0.55–1.31) | 0.88 | (0.58–1.35) | |
| Job Strain | 1466 | 98 | |||||||||||
| Low Strain | 27 | 1.00 | - | 1.00 | - | 1.00 | - | 1.00 | - | 1.00 | - | ||
| Passive Strain | 29 | 1.27 | (0.74–2.16) | 1.27 | (0.75–2.16) | 1.24 | (0.73–2.09) | 1.30 | (0.75–2.23) | 1.19 | (0.68–2.09) | ||
| Active Strain | 13 | 1.11 | (0.57–2.16) | 1.07 | (0.55–2.09) | 0.93 | (0.47–1.83) | 1.16 | (0.59–2.29) | 1.11 | (0.56–2.20) | ||
| High Strain | 29 | 1.51 | (0.90–2.54) | 1.41 | (0.84–2.38) | 1.32 | (0.78–2.25) | 1.46 | (0.84–2.52) | 1.34 | (0.77–2.31) | ||
| Job Strain Ratio | 1466 | 98 | |||||||||||
| Lower Half | < 0.53 | 42 | 1.00 | - | 1.00 | - | 1.00 | - | 1.00 | - | 1.00 | - | |
| Upper Half | ≥ 0.53 | 56 | 1.82 | (1.23–2.71) | 1.73 | (1.15–2.61) | 1.63 | (1.08–2.45) | 1.80 | (1.18–2.76) | 1.65 | (1.07–2.54) | |
|
Cut- offs |
(N) | (n) |
(i) Unadjusted HR (95% CI) |
(vi) adj. for Total Repetition Rate HR (95% CI) |
(vii) adj. for % Time All Hand Exertions HR (95% CI) |
(viii) adj. for ACGIH TLV for HAL HR (95% CI) |
|||||||
| Psychological Demand | 1176 | 84 | |||||||||||
| Lower Half | < 31 | 38 | 1.00 | - | 1.00 | - | 1.00 | - | 1.00 | - | |||
| Upper Half | ≥ 31 | 46 | 1.15 | (0.75–1.76) | 1.14 | (0.74–1.75) | 1.14 | (0.74–1.76) | 1.31 | (0.88–1.96) | |||
| Decision Latitude | 1482 | 83 | - | ||||||||||
| Lower Half | < 60 | 35 | 1.00 | - | 1.00 | - | 1.00 | - | 1.00 | - | |||
| Upper Half | ≥ 60 | 48 | 0.83 | (0.53–1.29) | 0.84 | (0.53–1.32) | 0.84 | (0.53–1.33) | 0.95 | (0.62–1.46) | |||
| Job Strain | 1479 | 83 | |||||||||||
| Low Strain | 25 | 1.00 | - | 1.00 | - | 1.00 | - | 1.00 | - | ||||
| Passive Strain | 23 | 1.10 | (0.62–1.96) | 1.10 | (0.62–1.95) | 1.10 | (0.62–1.96) | 1.27 | (0.75–2.17) | ||||
| Active Strain | 13 | 1.20 | (0.61–2.36) | 1.18 | (0.60–2.31) | 1.18 | (0.60–2.34) | 1.00 | (0.50–1.98) | ||||
| High Strain | 22 | 1.33 | (0.75–2.35) | 1.30 | (0.73–2.32) | 1.30 | (0.73–2.32) | 1.31 | (0.77–2.22) | ||||
| Job Strain Ratio | 1165 | 83 | |||||||||||
| Lower Half | < 0.53 | 40 | 1.00 | - | 1.00 | - | 1.00 | - | 1.00 | - | |||
| Upper Half | ≥ 0.53 | 43 | 1.62 | (1.05–2.50) | 1.60 | (1.03–2.48) | 1.59 | (1.02–2.49) | 1.63 | (1.09–2.45) | |||
Discussion
The purpose of this analysis was to replicate two prior prospective studies of a working population that assessed the relationship between personal, psychosocial and biomechanical factors and risk of CTS while using DAGs to guide an assessment for confounding. The most important finding in this analysis was that although some bias did exist from confounding (i.e., non-causal pathways), the magnitude was small and the 10% change in effect estimate criterion was rarely met. Further, the small changes in effect estimates could be due to random fluctuations versus attenuation. Therefore, previously observed exposure-response relationships between biomechanical factors and CTS were not likely due to confounding by psychosocial factors and previously observed exposure response relationships between psychosocial factors and CTS were not likely due to confounding by biomechanical factors. Further, these findings suggest that it is perhaps unnecessary to be critical or dismissive of other studies that investigate the relationship between and an upper extremity musculoskeletal disorder (or at least CTS) and biomechanical exposure without adjusting for work psychosocial exposure, or vice versa, among cohorts similar to those of the current study. Rather, findings from the current large and generalizable study suggest that both biomechanical exposure and work psychosocial exposure appear to be independent risk factors of incident CTS.
Psychological Demand has been suggested as a surrogate measure for physical exertion18. Others have found that measures of work psychosocial stress and physical exertion are independently associated with health outcome measures19. None of the work psychosocial measures such as Psychological Demand or Decision Latitude or Total Support were strongly correlated with any measures of biomechanical exposures. Our data indicate that, in fact, they are independent of one another.
When our first publication using the combined dataset was published, we reported an increase in risk of CTS (HR=1.86; 95%CI: 1.11–3.14) among those with high Job Strain and a protective effect (HR=0.54; 95%CI: 0.31–0.95) of Total Support8. At that time, biomechanical exposures were not included in the analysis. Consequently, it was of interest to assess whether the findings were biased due to confounding from biomechanical exposures. Figure 1b shows that adjusting for biomechanical exposure at baseline blocks a non-causal pathway to CTS through some unmeasured attribute (U) that determines choice of work, and thus is associated with both biomechanical and work psychosocial exposure. From this analysis, it appears that adjusting for certain biomechanical exposures (HAL Scale or % time Forceful Hand Exertions) could attenuate Job Strain effect estimates toward the null up to about 14%. Applying this magnitude of attenuation, the adjusted effect estimate would change from 1.86 to approximately 1.65, still indicating an increase in risk of CTS among those with high Job Strain. Total Support would have been negligibly affected since the changes in effect estimates in this subcohort were minimal, and biased only slightly away from the null. Thus, it appears that high Job Strain is an important risk factor for CTS and support from co-workers and supervisors is protective.
To maximize power and generalizability, two prior publications assessing the exposure-response relationship between biomechanical exposures and CTS9,10, models did not control for potential confounding by work psychosocial measures. However, using the directed acyclic graph in Figure 1a, confounding by work psychosocial exposure could occur through a back door, non-causal pathway through some unmeasured variable (U). The magnitude of bias from not blocking this pathway was unknown. By using a smaller subset of individuals with complete data in this analysis, we found that the magnitude of the bias would have been minimal since most of the effect estimates in these fully adjusted models changed less than 10%. In fact, all biomechanical exposure effect estimates adjusted for Psychological Demand changed less than 5%. Decision latitude had the biggest impact with 9 to 14% reductions of effect estimates resulting in slight attenuations toward the null. Decision latitude had the biggest impact on biomechanical measures that included some metric of force (Peak Hand Force, Forceful Repetition Rate, Forceful Hand Exertions, and TLV for HAL). It is a plausible that there is some unknown factor associated with participant willingness to accept jobs requiring forceful hand exertion only if there is adequate decision latitude in performing such physically rigorous work. For example, U could include where participants grew up (and what jobs were available) or having parents who worked similar jobs. Thus, blocking the backdoor path through U (Figure 1a) using Decision Latitude as the work psychosocial measure of choice, may lead to slightly less biased effect estimates, however the difference is negligible. In our prior analyses of biomechanical exposures and risk of CTS, there were strong associations between several measures of force and incident CTS, and those associations would have remained, albeit somewhat attenuated, had we adjusted for Decision Latitude in the larger cohort analysis. Of equal importance is that Total Repetition Rate and % time all exertions, which were not associated with increased rate of CTS, were not confounded through U on a non-causal path. Therefore, it stands that Total Repetition Rate and % time all exertions are not important independent risk factors for CTS in this cohort.
To corroborate our results by addressing the non-collapsibility of hazard ratios, we developed logistic models for the exposure of interest and used them to develop inverse probability weights (IPWs) to standardize the population with respect to the potential confounder20. Results were very similar to the ones presented; for example, with respect to the model estimating the rate of CTS associated Psychological Demand adjusting for the TLV-HAL using IPWs, HRs were nearly identical to the models conditional on TLV-HAL, and, similarly, slightly attenuated compared to the unadjusted model. Similarly, when estimating the rate of CTS associated with the % time Forceful Exertion adjusting for the Decision Latitude using IPWs, HRs were similar to models conditional on Decision Latitude and even closer to the unadjusted model. Thus, the use of conditional models presented no concerns of bias from the non-collapsibility properties of hazard ratios in this analysis.
Although some data was missing at random, the reduction in sample size of some models was due to slight differences in study design across the four studies pooled. Some exposures, like total repetition rate, were not collected for anyone within a particular study. Therefore, some analyses have different cohorts based on study design versus missing data that may have been differential to outcome or exposure status.
Conclusion
Measures of psychosocial exposure were not strongly correlated with biomechanical exposures. Decision latitude was a weak confounder of the relationship between certain biomechanical exposures (including forceful hand exertions) and the rate of CTS. The association between Total Support and incident CTS was not confounded by biomechanical exposures in this analysis. The HAL Scale and % time forceful hand exertion were weak confounders of the relationship between Job Strain and CTS. Despite not being able to adjust for confounding by biomechanical or psychosocial exposures in prior analyses using the larger pooled cohort, elevated effect estimates would have persisted after applying the same magnitude of confounding discovered in these analyses. Therefore, our prior findings that Job Strain, various measures of hand force (Peak Hand Force,Forceful Repetition Rate, and % time Forceful Hand Exertion) and the TLV-HAL increase the rate of CTS suggest they should be considered in future workplace intervention studies. Finally, it is worth noting that these results are from a pooled data set where each study group had actual investigator exposure and health outcome data collected from over 55 service and production companies across the United States. Thus, findings from this pooled UEMSD Consortium are highly generalizable and should be taken into consideration when designing work place injury prevention programs.
Supplementary Material
WHAT THIS PAPER ADDS:
The relationship between important biomechanical exposures of forceful hand exertion and incident CTS were confounded slightly by decision latitude.
The relationship between Job Strain and CTS was confounded slightly by the biomechanical factors HAL Scale and % time spent in Forceful Hand Exertion.
Psychological demand and decision latitude were not strongly correlated with measures of biomechanical exposure.
Due to missing data, prior analyses did not adjust for confounding by biomechanical and psychosocial exposures in the full cohort. However, based on the small degree of attenuation observed after adjustment, the previously reported exposure-response estimates would have persisted even after controlling for psychosocial or biomechanical exposures.
Job strain and forceful hand exertion (Analyst-rated Peak Hand Force,Forceful Repetition Rate, and % time Forceful Hand Exertion) are independent risk factors for CTS.
Acknowledgements:
This study was supported by research funding from the Center for Disease Control / National Institute for Occupational Safety and Health (R01OH009712). The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the National Institute for Occupational Safety and Health. We would like to acknowledge the efforts of the research assistants from each of the research study groups that made the collection of the data possible and the study participants and employers for their time and willingness to participate in this study.
Footnotes
Financial Disclosure: No co-author reported having a direct financial interest in the results of the research supporting this article.
References
- 1).Foley M, Silverstein B, Polissar N . The economic burden of carpal tunnel syndrome: long-term earnings of CTS claimants in Washington State. Am J Ind Med. 2007;50:155–72. [DOI] [PubMed] [Google Scholar]
- 2).Mondelli M, Giannini F, Giacchi M. Carpal Tunnel syndrome incidence in a general population. Neurology. 2002;58(2):289–94. [DOI] [PubMed] [Google Scholar]
- 3).Violante FS, Armstrong TJ, Fiorentini C, et al. Carpal tunnel syndrome and manual work: a longitudinal study. Journal of Occupational and Environmental Medicine. 2007;49(11):1189–1196. [DOI] [PubMed] [Google Scholar]
- 4).Silverstein BA, Fine LJ, & Armstrong TJ Occupational factors and carpal tunnel syndrome. American Journal of Industrial Medicine. 1987;11(3):343–358. [DOI] [PubMed] [Google Scholar]
- 5).Fung BK, Chan KY, Lam LY, et al. Study of wrist posture, loading and repetitive motion as risk factors for developing carpal tunnel syndrome. Hand Surg. 2007;12(1):13–18. [DOI] [PubMed] [Google Scholar]
- 6).Maghsoudipour M, Moghimi S, Dehghaan F, et al. Association of occupational and non-occupational risk factors with the prevalence of work related carpal tunnel syndrome. Journal of Occupational Rehabilitation. 2008;18(2):152–156. [DOI] [PubMed] [Google Scholar]
- 7).Dale AM, Harris-Adamson C Rempel D, et al. Prevalence and incidence of CTS in US working populations: Pooled analysis of six prospective studies. Scand J Work Environ Health. 2013;39(5):495–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8).Harris-Adamson C, Eisen EA, Dale AM, et al. Personal and Workplace Psychosocial Risk Factors for Carpal Tunnel Syndrome: A Pooled Study Cohort. Occup Environ Med. 2013;70(8):529–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9).Harris-Adamson C, Eisen EA, Kapellusch J, et al. Biomechanical risk factors for carpal tunnel syndrome: a pooled study of 2474 workers. Occup Environ Med. 2015;72(1):33–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10).Kapellusch J, Gerr FE, Malloy EJ, et al. Exposure-Response Relationships for the ACGIH TLV for Hand Activity Level: Results from a Pooled Data Study of Carpal Tunnel Syndrome. Scand J Work Environ Health. 2014;40(6):610–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11).Kapellusch J, Garg A, Bao S, et al. Pooling Job Physical Exposure Data from Multiple Sites in a study of Carpal Tunnel Syndrome. Ergonomics. 2013;56(6):1021–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12).Karasek R, Brisson C, Kawakami N, et al. The Job Content Questionnaire ( JCQ): an instrument for internationally comparative assessments of psychosocial job characteristics. J Occup Health Psychol 1998;3:322–55. [DOI] [PubMed] [Google Scholar]
- 13).Borg G Psychophysical bases of perceived exertion. Medicine & Science in Sports & Exercise. 1982;14(5):377–381. [PubMed] [Google Scholar]
- 14).Rempel D, Evanoff B, Amadio P, et al. Consensus criteria for the classification of carpal tunnel syndrome in epidemiologic studies. Am J Public Health. 1998;88:1447–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15).Shrier I and Platt RW. Reducing bias through directed acyclic graphs. BMC Medical Research Methodology. 2008;8(70):1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16).Greenland S, Pearl J, Robins JM. Causal Diagrams for Epidemiologic Research. Epidemiology. 1999;10:37–48. [PubMed] [Google Scholar]
- 17).Greenland S Modeling and variable selection in epidemiologic analysis. Am J Public Health . 1989;79:340–349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18).Kawakami N & Fujigaki Y. Reliability and validity of the Japanese version of job Content Questionnaire: replication and extension in computer company employees. Ind Health. 1996; 34(4):295–306. [DOI] [PubMed] [Google Scholar]
- 19).Krause N, Ragland DR, Greiner BA, et al. Psychosocial job factors associated with back and neck pain in public transit operators. Scand J Work Environ Health. 1997;23(3):179–86. [DOI] [PubMed] [Google Scholar]
- 20).Austin PC. The performance of different propensity score methods for estimating marginal hazard ratios. Stat Med. 2013; 32(16):2837–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


