Abstract
Background
Comparison between percutaneous coronary intervention (PCI) using stents and Coronary Artery Bypass Grafting (CABG) remains controversial.
Objective
To conduct a systematic review with meta-analysis of PCI using Stents versus CABG in randomized controlled trials.
Methods
Electronic databases were searched to identify randomized trials comparing PCI using Stents versus CABG for multi-vessel and unprotected left main coronary artery disease (LMCAD). 15 trials were found and their results were pooled. Differences between trials were considered significant if p < 0.05.
Results
In the pooled data (n = 12,781), 30 days mortality and stroke were lower with PCI (1% versus 1.7%, p = 0.01 and 0.6% versus 1.7% p < 0.0001); There was no difference in one and two year mortality (3.3% versus 3.7%, p = 0.25; 6.3% versus 6.0%, p = 0.5). Long term mortality favored CABG (10.6% versus 9.4%, p = 0.04), particularly in trials of DES era (10.1% versus 8.5%, p = 0.01). In diabetics (n = 3,274) long term mortality favored CABG (13.7% versus 10.3%; p < 0.0001). In six trials of LMCAD (n = 4,700) there was no difference in 30 day mortality (0.6%versus 1.1%, p = 0.15), one year mortality (3% versus 3.7%, p = 0.18), and long term mortality (8.1% versus 8.1%) between PCI and CABG; the incidence of stroke was lower with PCI (0.3% versus 1.5%; p < 0.001). Diabetes and a high SYNTAX score were the subgroups that influenced more adversely the results of PCI.
Conclusion
Compared with CABG, PCI using Stents showed lower 30 days mortality, higher late mortality and lower incidence of stroke. Diabetes and a high SYNTAX were the subgroups that influenced more adversely the results of PCI.
Keywords: Myocardial Revascularization/mortality, Percutaneous Coronary Intervention, Drug-Eluting Stents, Stents, Coronary Vessels, Randomized Controlled Trial, Meta-Analysis
Introduction
Percutaneous coronary intervention (PCI) using stents and coronary artery bypass grafting (CABG) are well-accepted alternatives for treatment of coronary artery disease (CAD). A large number of randomized controlled trials (RCT) comparing the two procedures were published.1-23 Most studies were underpowered to evaluate isolated endpoints like death, stroke and acute myocardial infarction (AMI). Several meta-analyses were subsequently carried out, pooling results in order to overcome this limitation.24-31 The largest meta-analysis included a limited number of drug-eluting stent (DES) era trials and/or included also single vessel disease and balloon era trials. On the other side, modern meta-analysis included a lower number of trials (only of DES era) and evaluated specific group of patients.28-32 The objective of this study was to perform a systematic review of RCT comparing stents (bare-metal and drug-eluting) versus CABG in multi-vessel and/or left main coronary disease (LMCAD) pooling data of mortality at different periods of time and using meta-regression analysis to evaluate sub-groups.
Methods
Search strategies
Randomized studies comparing PCI with Stents versus CABG in multivessel lesions and/or obstruction of left main CAD published between January 1990 and December 2017 were searched in the databases MEDLINE and Cochrane library and in bibliographic references published on the subject. The search terms used were: “coronary stents” and “coronary artery bypass surgery” and “randomized controlled trial”.
Inclusion criteria
Clinical trials were included in the review if they were randomized, if had compared PCI with stents versus CABG, if included exclusively multi-vessel and/or LMCAD and if had a follow up of at least 1 year. We did not limit our search to DES trials because bare-metal stents (BMS) are still frequently used in many developing countries, had the peculiarity of evaluating patients with less complex coronary artery disease and there is no definitive evidence that BMS are inferior to DES in the outcome mortality. Figure 7 show a flow diagram of the search strategy in the databases. We identified a total of 15 RCT that satisfied the requirements: AWESOM1, ERACI II,2,3 MASS II,4-6 SOS,7,8 ARTS,9,10 LE MANS,11 SYNTAX,12-14 CÁRDia,15 Boldriot et al.,16 PRECOMBAT,17,18 Va-Cards,19 FREEDOM,20 BEST,21 NOBLE22 and EXCEL.23 Three reviewers (PJNA, ATA and JLAF) assessed the quality of the studies using the Cochrane Collaboration’s tool.
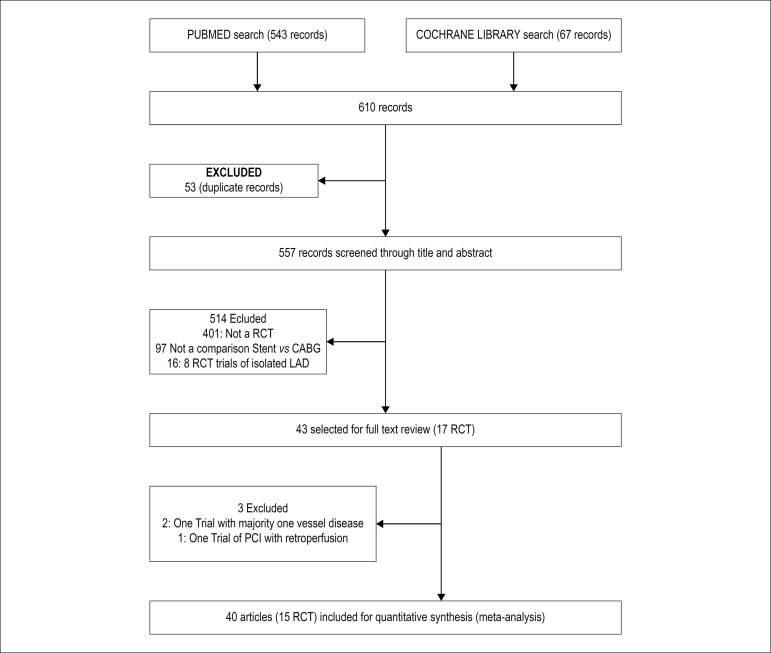
Figure 7.
Study Flow Diagram. RCT: randomized controlled trial; CABG: coronary artery bypass grafting; LAD: left anterior descending; PCI: percutaneous coronary intervention.
Data extraction
Two reviewers (JLAAF and PJNA) obtained the data from the studies, examining abstracts, results, tables, appendices and figures. A third author (BAAF) checked the results.
The main outcomes evaluated were all case-mortality, stroke, AMI and new revascularization. Mortality was divided into early mortality, mortality at one year and late mortality. Early mortality was defined as percentage of deaths that occurred in the first 30 days after the procedure, including deaths after randomization but before the procedure. Late mortality was defined as percentage of deaths reported in the last publication, after at least three years of follow-up. For the incidence of stroke, we considered the events occurring up to 1 year after the procedure. In twelve studies we obtained the results up to 30 days, in 2 studies 9,12 up to 1 year and in one 21 this observation was unavailable. For the incidence of myocardial infarct, we considered the reported up to one year of the procedure. AMI were reported in 13 trials.2-5-15 We did not consider in the pooled data the results of NOBLE because it excluded perioperative myocardial infarct in the majority of the patients.
New revascularization was divided in any form of new revascularization (PCI or CABG) and new revascularization by alternative procedure (PCI for patients of the CABG group or CABG for the patients of the PCI group).
Data synthesis
The characteristics of patients from the eligible studies were obtained through a weighted average of published data. For pooling results of mortality and stroke, the numerator was the number of events and the denominator the total of patients. The total of patients was the number of patients effectively followed, including the deaths. Trials were divided into DES era trials and BMS era trials. Trials that used both types of stents11,15 were classified as DES era trials. We evaluated separately the results of studies in the left main coronary artery and late mortality in the subgroup of patients with diabetes. We also performed analysis of combined major adverse cardiac and cerebrovascular events (MACCE) and assessed the variables age, gender, presence of diabetes, SYNTAX score, and compromised ejection fraction in subgroups based on data published in five trials. Combined MACCE comprised death, AMI, and new revascularization. In order to aggregate the outcomes of mortality and stroke, as well as those of MACCE (in subgroups), we considered whenever possible the absolute number of events and the number of patients followed up. Otherwise, percentages were transformed into absolute numbers.
Statistical analysis
We measured the relative risk and the risk difference after grouping the results of each outcome. In order to assess the statistical significance of the differences between the DES and the surgery groups, we performed a meta-analysis using the Mantel-Haenszel method, with a random-effect model. We calculated the heterogeneity of the studies using Cochran's Q test and the significance of the measure of the meta-analytic effect using the Z test. Finally, we performed a meta-regression analysis using diabetes, age, gender, ejection fraction, and syntax scores as factors. The differences between the results in the PCI and CABG groups were considered significant if p<0.05. The statistical analyses were performed using the program Review Manager (RevMan), version 5.3 (Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014) and SPSS for Windows v 23, IBM Inc. In order to represent the heterogeneity of the studies, we constructed Forest plots. We used the risk difference to plot these graphs since this is a more stable index. The possibility of publication bias was assessed by visual inspection of funnel plots.
Results
Studies Characteristics
The studies (table 1) included a total of 12,781 patients (6,382 in the CABG group and 6,399 in the PCI group). All studies were, considered of quality A or B in terms of adequate randomization, adequate concealment and inexistence of selection bias, but not in terms of adequate making. In all studies, the PCI and CABG groups were similar, with the exception of VaCards where the PCI group had a higher incidence of the previous revascularization (in most of the cases a previous PCI) and showed a higher percentage of patients with ejection fraction < 55%. The mean age of the patients was 64 years; 74% were male; 42% were diabetics; 28% were smokers; 64% were hypertensive. Unstable angina was the clinical presentation in 34%; mean ejection fraction was 58%. With the exception of AWESOME, all studies tended to exclude patients with previous CABG. The mean SYNTAX score was 26. According to number of arteries affected 20% had two vessel disease, 43% had three-vessel disease and 37% had LMCAD (alone or associated with diseases of other arteries). In the CABG group, at least one arterial graft was used in 90% of the patients. In trials of the BMS era surgery was done almost always using on-pump technique; in trials of the era, the DES off-pump technique was used in 28% of the patients. Some characteristics of the studies deserve special mention: ERACI II included more them 90% of patients with unstable angina. AWESOME included only patients with high surgical risk; MASS II included predominantly stable angina and had a clinical arm; LE MANS used drug-eluting and BMS, reserving the DESs for left main coronary arteries with a reference diameter < 3.8 mm; CARDia used initially BMS and only assessed patients with diabetes and multivessel disease; SYNTAX evaluated left main coronary artery obstruction and multivessel disease and used first-generation DESs (TAXUS); FREEDOM and VA CARDS exclusively assessed patients with diabetes and multivessel disease; BEST evaluated patients with multivessel disease and used only everolimus-eluting stents; the study by Boudriot et al. evaluated left main coronary artery obstruction and used only sirolimus-eluting stents; EXCEL evaluated left main coronary artery obstruction and used only everolimus-eluting stents; NOBLE evaluated left main coronary artery obstruction and used mostly a biolimus-eluting stent.
Table 1.
Overview of clinical trials
| Study | Origin | Period of recruitment | Number of Patients | Disease extension | Characteristics | Unstable angina (%) | Average ejection fraction (%) | Off pump surgery (%) | Diabetics (%) |
|---|---|---|---|---|---|---|---|---|---|
| AWESOME | North America (USA) | 1995-2000 | 454 | Two and three vessel disease | BMS. Previous CABG included | 36 | 45 | 0 | 32 |
| ARTS | International | 1997-2000 | 1205 | Two and three vessel disease | BMS. Majority two vessel disease | 30 | 61 | 0 | 21 |
| ERACI II | South America (Argentina) | 1996-1998 | 450 | Two and three vessel disease | BMS. Majority unstable angina | 92 | ND | 0 | 17 |
| SOS | Europe and Canada | 1995-1999 | 988 | Two and three vessel disease | BMS. Majority two vessel disease | 33 | ND | 3 | 15 |
| MASS II | South America (Brazil) | 1995-2000 | 408 | Two and three vessel disease | BMS. Clinical arm | 36 | 65 | 0 | 30 |
| LEMANS | Europe (Poland) | 2001-2004 | 105 | Left main coronary disease | BMS and DESDES if LM < 3.8 | 32 | 53 | 0 | 25 |
| SYNTAX | Europe and USA | 2005-2007 | 1800 | Left main and three vessel disease | DES (Taxus) | 28 | ND | 15 | 35 |
| CARDia | Europe (United Kingdom) | 2002-2007 | 510 | Two and three vessel disease | BMS and DES. Only diabetics. | 22 | 59 | 31 | 100 |
| Boudriot et al | Europe (Germany) | 2003-2009 | 201 | Left main coronary disease | DES (Sirolimus) | ND | ND | 46 | 30 |
| PRECOMBAT | Asia (Korea) | 2003-2009 | 600 | Left main coronary disease | DES (Everolimus) | 45 | 60 | 64 | 42 |
| FREEDOM | International | 2005-2010 | 1900 | Two and three vessel disease | DES. Only diabetes | 30 | 65 | 19 | 100 |
| Va-Cards | North America (USA) | 2006-2010 | 198 | Two and three vessel disease | DES. Only diabetics | ND | ND | ND | 100 |
| BEST | Asia (Korea) | 2008-2013 | 880 | Two and three vessel disease | DES. (Everolimus) | 42 | 59 | 64 | 45 |
| EXCEL | International | 2010-2014 | 1905 | Left main coronary disease | DES. (Everolimus) | 37 | 57 | 29 | 25 |
| NOBLE | Europe | 2008-2015 | 982 | Left main coronary disease | DES (Biolimus) | 18 | 60 | 18 |
AWESOME: Angina with extremely severe outcomes; ERACI II: Argentine randomized study: coronary angioplasty with stenting versus coronary bypass surgery in patients with multivessel disease; MASS II: Medicine, Angioplasty, or Surgery Study; ARTS: Arterial Revascularization Therapies Study; SOS: Stent or Surgery trial. SYNTAX: Synergy between PCI with Taxus and Cardiac Surgery; CARDia: Coronary artery revascularization in diabetic; Le Mans: Left main stenting; FREEDOM: Future Revascularization Evaluation in Patients with Diabetes Mellitus; Va-Cards: Coronary Artery Revascularization in Diabetes in VA Hospitals; BEST: Bypass Surgery and Everolimus-Eluting Stent Implantation in the Treatment of Patients with Multivessel Coronary Artery Disease; PRECOMBAT: Premier of Randomized Comparison of Bypass Surgery versus Angioplasty Using Sirolimus-Eluting Stent in Patients with Left Main Coronary Artery Disease; EXCEL: Coronary Artery Bypass Surgery for Effectiveness of Left Main Revascularization; NOBLE: Nordic-Baltic-British Left Main Revascularization Study. Boldriot et al: J Am Coll Cardiol. 2011; 57: 538-545. DES: drug-eluting stent; BMS: bare-metal stent.
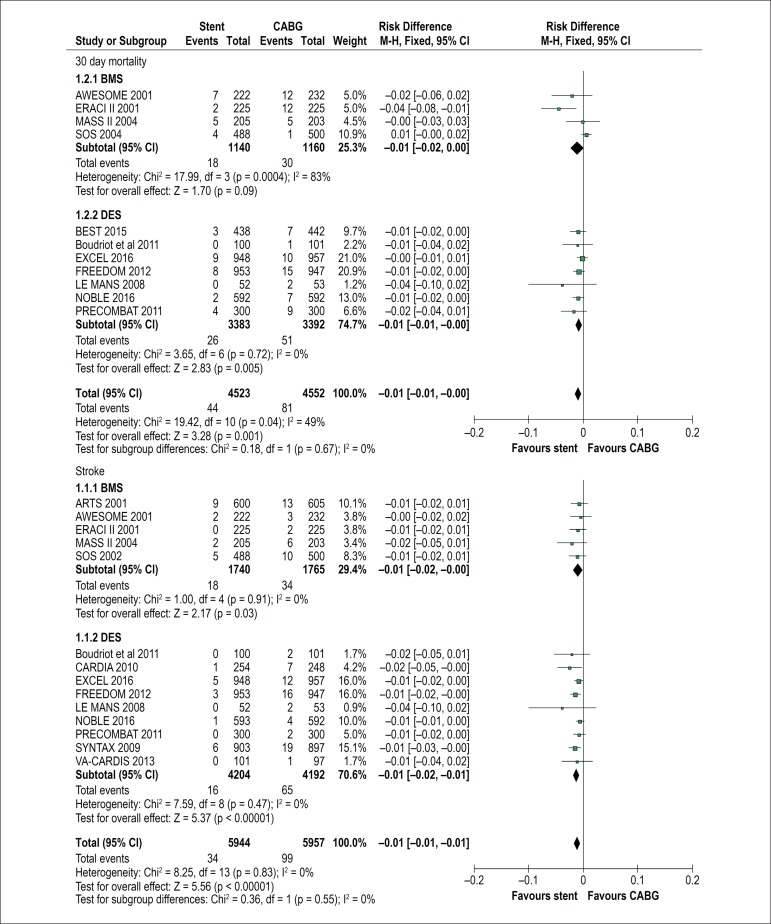
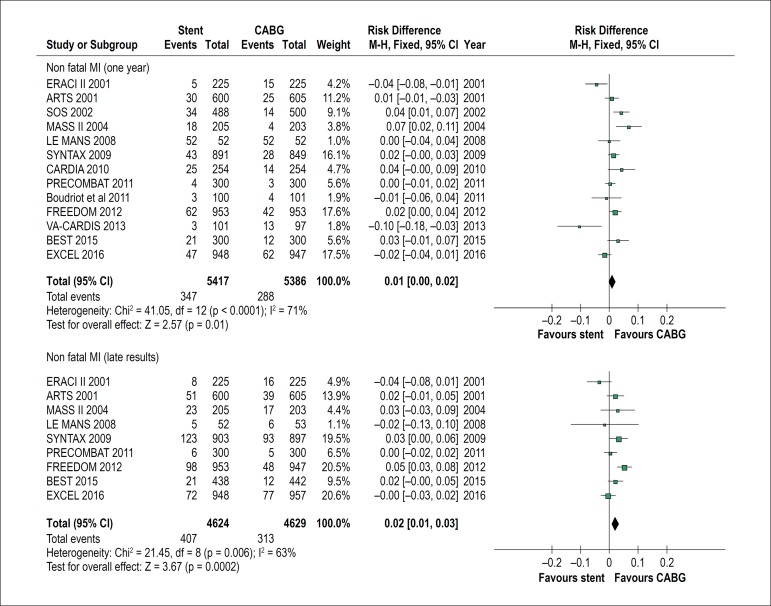
Outcomes
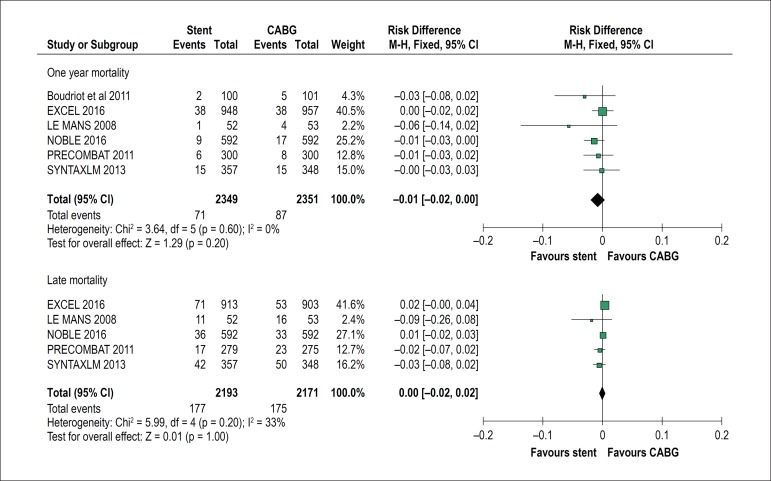
The results are summarized in Figures 1 to 6. Regarding 30-day mortality, the results favoured PCI (1% versus CABG 1.7%, p = 0.01), but the trials showed moderate overall heterogeneity (I2= 49%). The heterogeneity was particularly higher in BMS era trials (I2= 83%) and could be attributed to the significant inferior results of surgery in ERACI II and AWESOME. The incidence of stroke was lower with PCI (0.6% versus CABG 1.7%, p < 0.0001), with trials showing low heterogeneity (I2= 0). There was no difference in mortality up to one year (PCI 3.3% versus CABG 3.7%, p = 0.25) or up to two year (PCI 6.3% versus CABG 6.0%, p = 0.5). Long-term mortality showed a trend to superiority of CABG (10.6% versus 9.4%, p = 0.04), with trials showing moderate heterogeneity (I2= 25%). The differences were significant in trials of DES era (10.1% versus 8.5%, p = 0.01). After excluding FREEDOM (that included only diabetics) the overall difference in long-term mortality between PCI and CABG became not significant (10.2% versus 9.4%, p = 0.17). The incidence of myocardial infarct was lower with CABG (PCI 6.4 % versus CABG 5.3% at one year and PCI 8,8% versus CABG 6.7 % after 3 or more years), but the trials showed high heterogeneity.
Figure 1.
Stent versus CABG: 30 days mortality (top) and stroke (bottom). The size of each box is proportional to the number of patients of the trial. The bars represent 95% confidence interval. The diamond represents the syntheses of results. DES: trials of the drug-eluting stent era. BMS: trials of the bare-metal stent trials era. CABG: coronary artery bypass grafting. ARTS: Arterial Revascularization Therapies Study; AWESOME: Angina with extremely severe outcomes; ERACI II: Argentine randomized study: coronary angioplasty with stenting versus coronary bypass surgery in patients with multi-vessel disease; MASS II: Medicine, Angioplasty, or Surgery Study; SOS: Stent or Surgery trial; BEST: Bypass Surgery and Everolimus-Eluting Stent Implantation in the Treatment of Patients with Multi-vessel Coronary Artery; Boldriot, trial of Boldriot et al: J Am Coll Cardiol. 2011; 57: 538-545. CARDia: Coronary artery revascularization in diabetic; LE MANS: Left main coronary artery stenting; EXCEL: Coronary Artery Bypass Surgery for Effectiveness of Left Main Revascularization; FREEDOM: Future Revascularization Evaluation in Patients with Diabetes Mellitus NOBLE, Nordic-Baltic-British Left Main Revascularization Study; PRECOMBAT: Premier of Randomized Comparison of Bypass Surgery versus Angioplasty Using Sirolimus-Eluting Stent in Patients with Left Main Coronary Artery Disease; SYNTAX: Synergy between PCI with Taxus and Cardiac Surgery; Va-Cards: Coronary Artery Revascularization in Diabetes in VA Hospitals.
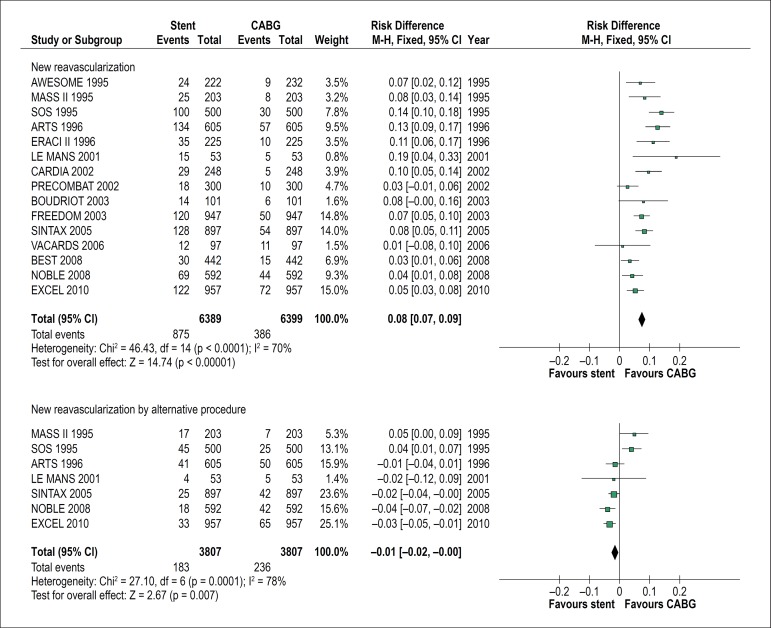
Figure 6.
Stent versus CABG: new revascularization (top) and new revascularization by alternative procedure (bottom). The size of each box is proportional to the number of patients of the trial. The bars represent 95% confidence interval. The diamond represents the syntheses of results. DES: trials of the drug-eluting stent era; BMS: trials of the bare-metal stent trials era; CABG: coronary artery bypass grafting; ARTS: Arterial Revascularization Therapies Study; AWESOME: Angina with extremely severe outcomes; ERACI II: Argentine randomized study: coronary angioplasty with stenting versus coronary bypass surgery in patients with multi-vessel disease; MASS II: Medicine, Angioplasty, or Surgery Study; SOS: Stent or Surgery trial; BEST: Bypass Surgery and Everolimus-Eluting Stent Implantation in the Treatment of Patients with Multi‑vessel Coronary Artery; Boldriot, trial of Boldriot et al: J Am Coll Cardiol. 2011; 57: 538-545. CARDia: Coronary artery revascularization in diabetic; LE MANS: Left main coronary artery stenting; EXCEL: Coronary Artery Bypass Surgery for Effectiveness of Left Main Revascularization; FREEDOM: Future Revascularization Evaluation in Patients with Diabetes Mellitus; NOBLE: Nordic-Baltic-British Left Main Revascularization Study; PRECOMBAT: Premier of Randomized Comparison of Bypass Surgery versus Angioplasty Using Sirolimus-Eluting Stent in Patients with Left Main Coronary Artery Disease; SYNTAX: Synergy between PCI with Taxus and Cardiac Surgery; Va‑Cards: Coronary Artery Revascularization in Diabetes in VA Hospitals.
In 6 studies of LMCAD (n = 4700), there was no difference in 30 days mortality (0.6% versus 1.1%, p = 0.15) between PCI and CABG, but the incidence of stroke was significantly lower after PCI (0.3% versus 1.1%, p = 0.007). There was no difference in one-year mortality (3% versus 3.7%, p = 0.18) or long-term mortality (8.1% versus 8.1%) between PCI and CABG.
Nine trials (n = 4394) reported long-term mortality in diabetics (AWESOME, ARTS, ERACII, MASS II, SOS, SYNTAX, CARDia, FREEDOM and BEST). After pooling of results, CABG was associated with significantly lower long-term mortality (13.7% versus 10.3% CABG, p < 0.0001); After excluding the diabetic patients of these nine trials the overall difference in long-term mortality between PCI and CABG was no longer significant (9.2% versus 9.2%).
The data regarding new revascularization are shown in figure 5. The superiority of surgery over PCI was consistent in all 15 trials. However, if we consider the risk of new revascularization by alternative procedure there was a trend to superiority of PCI in ARTS and in all studies of DES era.
Figure 5.
Stent versus CABG: risk difference of long-term major composite adverse outcomes (MACCE) in subgroups. The size of each box is proportional to the number of patients of the subgroups. The bars represent 95% confidence interval. The diamond represents the syntheses of results. CABG: coronary artery bypass grafting. LEE = Lee et al, J Am Coll Cardiol Intv 2016; 9:2481–9 (Meta-analysis of individual patient data of SYNTAX, PRECOMBAT and BEST); EXCEL: Coronary Artery Bypass Surgery for Effectiveness of Left Main Revascularization; FREEDOM, Future Revascularization Evaluation in Patients with Diabetes Mellitus. Low ejection Fraction was defined as < 50% in EXCEL and as < 40% in FREEDOM and LEE.
Subgroups results
Five trials reported long-term results of major Adverse Composite Events (death, myocardial infarct and stroke) in subgroups. In three of them (SYNTAX, PRECOMBAT and BEST) the results were obtained through the collaborative meta-analysis of Lee et al.24 (Figure 4). The pooled data showed that CABG, compared to PCI, was associated with a lower incidence of MACCE (18.4% vs 14.4%, p < 0.0001). The subgroups in which PCI had worse results, when compared with CABG, by meta-regression analysis were presence of diabetes (23% versus 17.5, p < 0.0001) and a high SYNTAX score (22.7 vs. 16.3%, p = 0.001). There was no difference between PCI and CABG in non-diabetics (14.1% versus 12.3%, p = 0.11), low SYNTAX score patients (14.1% vs. 13.3% scores, p = 0.4) and LMCAD patients (14.7% vs 14.1%, p = 0.5). Female sex and old age less significantly influenced the results. Left ventricular dysfunction did not influence the results. Figure 5 shows that the meta-Adjusted value of p for diabetes was 0.03 (adjusted for age or sex) and 0.09 (adjusted for SYNTAX score). The same figure shows that the meta-adjusted value of p for SYNTAX score was 0.03 (adjusted for diabetes).
Figure 4.
Stent versus CABG in left main coronary artery disease: one-year mortality (top) and long-term mortality (bottom). The size of each box is proportional to the number of patients of the trial. The bars represent 95% confidence interval. The diamond represents the syntheses of results. ULMCAD: unprotected left main coronary artery disease. CABG: coronary artery bypass graft. LE MANS: Left Main coronary artery stenting study; SYNTAX LEMANS: subgroup of ULMCAD of SYNTAX (Synergy between PCI with Taxus and Surgery); PRECOMBAT: Premier of Randomized Comparison of Bypass Surgery versus Angioplasty Using Sirolimus-Eluting Stent in Patients with Left Main Coronary Artery Disease; EXCEL: Coronary Artery Bypass Surgery for Effectiveness of Left Main Revascularization; NOBLE: Nordic-Baltic-British Left Main Revascularization Study. Boldriot: Boldriot et al: J Am Coll Cardiol. 2011; 57: 538-545.
Discussion
To our knowledge this meta-analysis is the most comprehensive and up to date overview of randomized trials that compared coronary stents (DES and BMS) versus CABG. It is also the only major meta-analysis of the stent era that evaluated mortality at different times (up to 30 days, up to one year and after three or more years of follow-up). Another peculiarity of the present meta-analysis was the statistical meta-regression analysis of sub-groups.
The superiority of PCI on 30 days mortality is in accord with the New York state Registry33 and with the meta-analysis of Palmerini et al.32 This superiority should be seen with caution considering the heterogeneity of the trials and cannot be extended to patients with high SYNTAX score, considering the mortality curve of the study of Cavalcante et al.30 The significant difference, favoring PCI found in the incidence of stroke is a relevant finding. A recent study showed that, after death (relative weight 0.23), stroke is the most feared event for patients (relative weight 0.18), being considered more important them longevity (relative weight 0.17), myocardial infarct (relative weight 0.14) and risk of repeat revascularization (relative weight 0.11).34The lack of difference in intermediate mortality was an expected finding, having been reported in almost all trials.
The trend superiority of surgery in long-term mortality was shown in other meta-analysis26,29,31 and is probably related to the higher percentage of diabetics in recent trials. Our results of long-term mortality (HR 1.13) were similar to the results of Smit el al.26 (HR 1.11) and Lee et at.29 (HR 1.18). They were much less unfavourable to PCI them the reported by Benedetto et al (HR 1.5).31 The reason for this is that Benedetto et al excluded LMCAD (that presented similar results of mortality with the two methods of revascularization) and BMS trials (that involved patients with less complex CAD), did not include AWESOME and included two years results of VaCards. Another reason for the significant worse comparative results of PCI-stent in the meta-analysis of Benedetto et al. was that diabetics represented 66% of their population. Recently a pooled analysis of an individual database from 11 trials was published by Head et al.35 and their overall results are similar to ours. Small differences can be explained by the fact that they included late results of VACards and did not include AWESOME, CARDia, Boldriot and LEMANS.
LMCAD was, for a long time, an indication type III for PCI, but this concept began to change after four trials showed similar results in mortality.11,12,16,17 However, AHA/ACC guidelines have accepted PCI only as class IIA or IIB indication for LMCAD and yet, only for patients at high surgical risk. In the present study, we found results similar in mortality, while the incidence of stroke was lower, favouring PCI. Our findings are similar to the collaborative study of Head et al and to the meta-analysis of Palmerini et al.32 This study provided also mortality results in subgroups, showing that in patients with low SYNTAX SCORE there was a trend to higher long-term mortality with CABG (HR, 0.68, CI 0.43-1.08; p = 0.09); intermediate SYNTAX score patients had similar results (HR 1.16, CI 0.51-264, p = 0.49). Considering this, we believe that PCI indications for LMCAD in AHA/ACC guidelines may be modified in near future.
Diabetic patients are a present challenge for PCI. A more diffuse atherosclerotic disease is a possible explanation for the worse comparative results of PCI in this population. Our results suggest that there is still a superiority of surgery over PCI in long-term mortality, even in the DES era. There is a hypothesis that the greater mortality of PCI compared to CABG in diabetic patients may be attributed to the presence of more complex lesions in diabetic patients and, not to the metabolic disturbance. The fact that in the subgroup analysis of MACCE results (Figure 5) the meta-Adjusted value was 0.09 (adjusted for SYNTAX score) supports this hypothesis.
This review was not aimed to compare the results of BMS and DES for several reasons: in BMS trials patients had less complex angiographic lesions (average of 2.3 stents per patient in ARTS and SOS trials versus 3.8 stents per patient in SYNTAX, FREEDOM, BEST, PRECOMBAT and CARDia trials) and had a small percentage of diabetic patients. Otherwise, medical adjunctive treatment and results of surgery for patients with failed PCI also evolved. But the good comparative results of PCI in BMS era trials suggest that for patients with less complex lesions, or patients with unstable angina (ERACI II trial) or high surgical risk (AWESOME trial) initial PCI is a good alternative to CABG.
In terms of major adverse composite events, the analysis of subgroups showed that diabetes and a high SYNTAX score were the most important factors to influence adversely the results of PCI. Presence of left ventricular dysfunction did not influence the results, but the number of patients with this finding was small. A high SYNTAX score was an independent risk factor for adverse outcomes, even when adjusted for diabetes, but diabetes was not an independent risk factor for adverse outcomes when adjusted for SYNTAX score.
In the present review despite the clear superiority of CABG in the outcome of new revascularization, it is possible to notice the progressive improvement of PCI results. This was particularly striking when we consider the outcome “new revascularization by alternative procedures”, in which there was a tendency to superiority of PCI in the DES era.
The evidence presented here should be used to inform patients, helping them in choosing the more adequate form of revascularization in multi-vessel and LMCAD. Some patients may prefer having PCI to avoid the higher morbidity and short-term mortality of surgery. Other patients may put greater emphasis on the superiority of surgery regarding long-term mortality. However, PCI using second generation DES may still be considered as an alternative to CABG, having similar mortality results, for patients with LMCAD of low or intermediate complexity (SYNTAX score < 33). This may also be the case for multi-vessel disease patients with lesions of low complexity (SYNTAX score < 23). For all other patients, particularly if diabetics, surgery remains the best form of revascularization. There is the possibility that second-generation DES and a more functional strategy, using free fractional reserve and avoiding unnecessary revascularizations will improve the comparative results of PCI in the future. The one year results of the SYNTAX II36 study suggests that this will be true, but long-term follow-up is waited and a randomized trial with contemporary CABG is warranted.
The present study presents important limitations. It is a meta-analysis of published data and not a collaborative meta-analysis with access to individual data of patients. The inclusion of BMS era trials can also be criticized. It should also be noted that 30 days mortality and late mortality showed moderate heterogeneity, reducing the robustness of our results. Otherwise, our findings apply only to patients for whom revascularization may be performed using either method, without high surgical risk, no history of prior surgical revascularization, normal or near-normal ejection fraction and with the procedures carried out in institutions of excellence.
Conclusion
PCI using stents when compared to CABG was associated with a trend to lower mortality at 30 days, similar one-year mortality, lower incidence of stroke up to one-year, and a trend to higher long-term mortality. There was no long-term mortality difference in non-diabetics and in LMCAD patients. In terms of composite adverse outcomes, the SYNTAX score and diabetes were the most important factors to consider when choosing between the two methods of revascularization.
Figure 2.
STENT versus CABG: One-year mortality (top) and late mortality (bottom). The size of each box is proportional to the number of patients of the trial. The bars represent 95% confidence interval. The diamond represents the syntheses of results. DES: trials of the drug-eluting stent era; BMS: trials of the bare-metal stent trials era; CABG: coronary artery bypass grafting; ARTS: Arterial Revascularization Therapies Study; AWESOME: Angina with extremely severe outcomes; ERACI II: Argentine randomized study: coronary angioplasty with stenting versus coronary bypass surgery in patients with multi-vessel disease; MASS II: Medicine, Angioplasty, or Surgery Study; SOS: Stent or Surgery trial; BEST: Bypass Surgery and Everolimus-Eluting Stent Implantation in the Treatment of Patients with Multi-vessel Coronary Artery; Boldriot, trial of Boldriot et al: J Am Coll Cardiol. 2011; 57: 538-545. CARDia: Coronary artery revascularization in diabetic; LE MANS: Left main coronary artery stenting; EXCEL: Coronary Artery Bypass Surgery for Effectiveness of Left Main Revascularization; FREEDOM: Future Revascularization Evaluation in Patients with Diabetes Mellitus; NOBLE: Nordic-Baltic-British Left Main Revascularization Study; PRECOMBAT: Premier of Randomized Comparison of Bypass Surgery versus Angioplasty Using Sirolimus-Eluting Stent in Patients with Left Main Coronary Artery Disease; SYNTAX: Synergy between PCI with Taxus and Cardiac Surgery; Va-Cards: Coronary Artery Revascularization in Diabetes in VA Hospitals.
Figure 3.
Stent versus CABG: Acute myocardial infarct at one year (top) and after three or more years (bottom). The size of each box is proportional to the number of patients of the trial. The bars represent 95% confidence interval. The diamond represents the syntheses of results. DES: trials of the drug-eluting stent era; BMS: trials of the bare-metal stent trials era; CABG: coronary artery bypass grafting; ARTS: Arterial Revascularization Therapies Study; AWESOME: Angina with extremely severe outcomes; ERACI II: Argentine randomized study: coronary angioplasty with stenting versus coronary bypass surgery in patients with multi-vessel disease; MASS II: Medicine, Angioplasty, or Surgery Study; SOS: Stent or Surgery trial; BEST: Bypass Surgery and Everolimus-Eluting Stent Implantation in the Treatment of Patients with Multi-vessel Coronary Artery; Boldriot, trial of Boldriot et al: J Am Coll Cardiol. 2011; 57: 538-545. CARDia: Coronary artery revascularization in diabetic; LE MANS: Left main coronary artery stenting; EXCEL: Coronary Artery Bypass Surgery for Effectiveness of Left Main Revascularization; FREEDOM: Future Revascularization Evaluation in Patients with Diabetes Mellitus; NOBLE: Nordic-Baltic-British Left Main Revascularization Study; PRECOMBAT: Premier of Randomized Comparison of Bypass Surgery versus Angioplasty Using Sirolimus-Eluting Stent in Patients with Left Main Coronary Artery Disease; SYNTAX: Synergy between PCI with Taxus and Cardiac Surgery; Va-Cards: Coronary Artery Revascularization in Diabetes in VA Hospitals.
Footnotes
Sources of Funding
There were no external funding sources for this study.
Study Association
This study is not associated with any thesis or dissertation work.
Ethics approval and consent to participate
This article does not contain any studies with human participants or animals performed by any of the authors.
Author contributions
Conception and design of the research and critical revision of the manuscript for intellectual content: Andrade PJN; acquisition of data: Andrade PJN, Falcão JLAA, Falcão BAA; analysis and interpretation of the data and writing of the manuscript: Andrade PJN, Falcão JLAA, Falcão BAA, Rocha HAL; statistical analysis: Rocha HAL.
Potential Conflict of Interest
No potential conflict of interest relevant to this article was reported.
References
- 1.Morrison DA, Sethi G, Sacks J, Henderson W, Grover F, Sedlis S, et al. Percutaneous coronary intervention versus coronary artery bypass graft surgery for patients with medically refractory myocardial ischemia and risk factors for adverse outcomes with bypass: a multicenter, randomized trial. Investigators of the Department of Veterans Affairs Cooperative Study #385, the Angina With Extremely Serious Operative Mortality Evaluation (AWESOME) J Am Coll Cardiol. 2001;38(1):143–149. doi: 10.1016/s0735-1097(01)01366-3. [DOI] [PubMed] [Google Scholar]
- 2.Rodriguez A, Bernardi V, Navia J, Baldi J, Grinfield L, Martinez J, et al. Argentine Randomized Study: Coronary Angioplasty with Stenting versus Coronary Bypass Surgery in patients with Multiple-Vessel Disease (ERACI II): 30-day and one-year follow-up results. ERACI II Investigators. J Am Coll Cardiol. 2001;37(1):51–58. doi: 10.1016/s0735-1097(00)01052-4. [DOI] [PubMed] [Google Scholar]
- 3.Rodriguez AE, Baldi J, Ferna'ndez Pereira C, Navia J, Rodriguez Alemparte M, Delacasa A, et al. Five-year follow-up of the Argentine randomized trial of coronary angioplasty with stenting versus coronary bypass surgery in patients with multiple vessel disease (ERACI II) J Am Coll Cardiol. 2005;46(4):582–588. doi: 10.1016/j.jacc.2004.12.081. [DOI] [PubMed] [Google Scholar]
- 4.Hueb W, Soares PR, Gersh BJ, Cesar LA, Luz PL, Puig LB, et al. The medicine, angioplasty, or surgery study (MASS-II): a randomized, controlled clinical trial of three therapeutic strategies for multivessel coronary artery disease: one-year results. J Am Coll Cardiol. 2004;43(10):1743–1751. doi: 10.1016/j.jacc.2003.08.065. [DOI] [PubMed] [Google Scholar]
- 5.Hueb W, Lopes NH, Gersh BJ, Soares P, Machado LA, Jatene FB, et al. Five-year follow-up of the Medicine, Angioplasty, or Surgery Study (MASS II): a randomized controlled clinical trial of 3 therapeutic strategies for multivessel coronary artery disease. Circulation. 2007;115(9):1082–1089. doi: 10.1161/CIRCULATIONAHA.106.625475. [DOI] [PubMed] [Google Scholar]
- 6.Hueb W, Lopes N, Gersh BJ, Soares PR, Ribeiro EE, Pereira AC, et al. Ten-year follow-up survival of the Medicine, Angioplasty, or Surgery Study (MASS II): a randomized controlled clinical trial of 3 therapeutic strategies for multivessel coronary artery disease. Circulation. 2010;122(10):949–957. doi: 10.1161/CIRCULATIONAHA.109.911669. [DOI] [PubMed] [Google Scholar]
- 7.SOS investigators Coronary artery bypass surgery versus percutaneous coronary intervention with stent implantation in patients with multivessel coronary artery disease (the Stent or Surgery trial): a randomised controlled trial. Lancet. 2002;360(9338):965–970. doi: 10.1016/S0140-6736(02)11078-6. [DOI] [PubMed] [Google Scholar]
- 8.Booth J, Clayton T, Pepper J, Nugara F, Flather M, Sigwart U, et al. Randomized, controlled trial of coronary artery bypass surgery versus percutaneous coronary intervention in patients with multivessel coronary artery disease: six-year follow-up from the Stent or Surgery Trial (SoS) Circulation. 2008;118(4):381–388. doi: 10.1161/CIRCULATIONAHA.107.739144. [DOI] [PubMed] [Google Scholar]
- 9.Serruys PW, Unger F, Sousa JE, Jatene A, Bounier HJ, Schomberger JP, et al. Comparison of coronary-artery bypass surgery and stenting for the treatment of multivessel disease. N Engl J Med. 2001;344(15):1117–1124. doi: 10.1056/NEJM200104123441502. [DOI] [PubMed] [Google Scholar]
- 10.Serruys PW, Ong AT, van Herwerden LA, Sousa JE, Jatene A, Bonnier JJ, et al. Five-year outcomes after coronary stenting versus bypass surgery for the treatment of multivessel disease: the final analysis of the Arterial Revascularization Therapies Study (ARTS) randomized trial. J Am Coll Cardiol. 2005;46(4):575–581. doi: 10.1016/j.jacc.2004.12.082. [DOI] [PubMed] [Google Scholar]
- 11.Buszman PE, Kiesz SR, Bochenck A, Peszek-Przrya E, Szkiobka I, Debwski M, et al. Acute and late outcomes of unprotected left main stenting in comparison with surgical revascularization. J Am Coll Cardiol. 2008;51(5):538–545. doi: 10.1016/j.jacc.2007.09.054. [DOI] [PubMed] [Google Scholar]
- 12.Serruys PW, Morice MC, Kappetei AP, Colombo A, Holmes DR, Mack MJ, et al. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N Eng J Med. 2009;360(10):961–972. doi: 10.1056/NEJMoa0804626. [DOI] [PubMed] [Google Scholar]
- 13.Mohr FW, Morice MC, Kappetein AP, Feldman TE, Ståhle E, Colombo A, et al. Coronary artery bypass graft surgery versus percutaneous coronary intervention in patients with three-vessel disease and left main coronary disease: 5-year follow-up of the randomised, clinical SYNTAX trial. Lancet. 2013;381(9867):629–638. doi: 10.1016/S0140-6736(13)60141-5. [DOI] [PubMed] [Google Scholar]
- 14.Morice MC, Serruys PW, Kappetein AP, Feldman TE, Ståhle E, Colombo A, et al. Five-year outcomes in patients with left main disease treated with either percutaneous coronary intervention or coronary artery bypass grafting in the synergy between percutaneous coronary intervention with taxus and cardiac surgery trial. Circulation. 2014;129(23):2388–2394. doi: 10.1161/CIRCULATIONAHA.113.006689. [DOI] [PubMed] [Google Scholar]
- 15.Kapur A, Hall RJ, Macik IS, Qureshi AC, Butts J, de Belder M, et al. Randomized comparison of percutaneous coronary intervention with coronary artery bypass grafting in diabetic patients: 1-year results of the CARDia (Coronary Artery Revascularization In Diabetics) trial. J Am Coll Cardiol. 2010;55(5):432–440. doi: 10.1016/j.jacc.2009.10.014. [DOI] [PubMed] [Google Scholar]
- 16.Boudriot E, Thiele H, Walther T, Liebetrau C, Boeckstegers P, Pohl T, et al. Randomized comparison of percutaneous coronary intervention with Sirolimus eluting stents versus coronary artery bypass grafting in unprotected in unprotected left main stenosis. J Am Coll Cardiol. 2011;57(5):538–545. doi: 10.1016/j.jacc.2010.09.038. [DOI] [PubMed] [Google Scholar]
- 17.Park SJ, Kim YH, Park DW, Yun SC, Ahn JM, Song HG, et al. Randomized trial of stents versus bypass surgery for left main coronary artey disease. N Engl J Med. 2011;364(18):1718–1727. doi: 10.1056/NEJMoa1100452. [DOI] [PubMed] [Google Scholar]
- 18.Ahn JM, Roh JH, Kim YH, Park DW, Yun SC, Lee PH, et al. Randomized Trial of Stents Versus Bypass Surgery for Left Main Coronary Artery Disease: 5-Year Outcomes of the PRECOMBAT Study. J Am Coll Cardiol. 2015;65(20):2198–2206. doi: 10.1016/j.jacc.2015.03.033. [DOI] [PubMed] [Google Scholar]
- 19.Kamalesh M, Shap TG, Tang C, Shunk K, Ward HB, Walsh J, et al. Percutaneous coronary intervention versus Coronary artery bypass surgery in United States veterans with diabetes. J Am Coll Cardiol. 2013;61(8):807–816. doi: 10.1016/j.jacc.2012.11.044. [DOI] [PubMed] [Google Scholar]
- 20.Farkouh ME, Dornanski M, Sleeper LA, Siami FS, Dangas G, Mack M, et al. Strategies for multivessel revascularization in patients with diabetes. N Engl J Med. 2012;367(25):2375–2384. doi: 10.1056/NEJMoa1211585. [DOI] [PubMed] [Google Scholar]
- 21.Park SJ, Ahn KM, Kim YH, Park DW, Yun SC, Lee JY, et al. Trial of everolimus-eluting stents or bypass surgery for coronary disease. N Engl J Med. 2015;372(13):1204–1212. doi: 10.1056/NEJMoa1415447. [DOI] [PubMed] [Google Scholar]
- 22.Makikallia T, Holm NR, Lindsay M, Spence MS, Erglis A, Menown IB, et al. Percutaneous coronary angioplasty versus coronary artery bypass grafting in treatment of unprotected left main stenosis (NOBLE): a prospective, randomized, open-label, non-inferiority trial. Lancet. 2016;388(10061):2743–2752. doi: 10.1016/S0140-6736(16)32052-9. [DOI] [PubMed] [Google Scholar]
- 23.Stone GW, Sabik JF, Serruys PW, Simonton CA, Généreux P, Puskas J, et al. Everolimus-stenting or bypass surgery for left main coronary artery disease. N Engl J Med. 2016;375(23):2223–2235. doi: 10.1056/NEJMoa1610227. [DOI] [PubMed] [Google Scholar]
- 24.Bravata DM, Gienger AL, McDonad KM, Sundaram V, Perez MV, Varghese R, et al. Sistematic review: the comparative effectiveness of percutaneous coronary intervention and coronary artery bypass graft surgery. Ann Intern Med. 2007;147(10):703–716. doi: 10.7326/0003-4819-147-10-200711200-00185. [DOI] [PubMed] [Google Scholar]
- 25.Hlatky MA, Boothroyd DB, Bravata DM, Boersma E, Booth J, Brooks MM, et al. Coronary artery bypass surgery compared with percutaneous coronary interventions for multivessel disease: a collaborative analysis of individual patient data from ten randomised trials. Lancet. 2009;373(9670):1190–1197. doi: 10.1016/S0140-6736(09)60552-3. [DOI] [PubMed] [Google Scholar]
- 26.Smit Y, Valyen J, Kopennaal H, Eefting E, Kappetein AP, Mariani MA. Percutaneous coronary invervention versus coronary artery bypass grafting: a meta-analysis. J Thorac Cardiovasc Surg. 2015;149(3):831–838. doi: 10.1016/j.jtcvs.2014.10.112. [DOI] [PubMed] [Google Scholar]
- 27.Andrade PJ, Medeiros MM, Andrade AT, Lima AA. Coronary angioplasty versus CABG: review of randomized trials. Arq Bras Cardiol. 2011;97(3):e60–e69. doi: 10.1590/s0066-782x2011001200021. [DOI] [PubMed] [Google Scholar]
- 28.Andrade PJN, Rocha HAL, Falcão JLAA, Andrade AT, Falcão BAA. Drug-eluting stents Versus Coronary Artery Bypass Grafting in Multivessel Disease and Left Main Obstruction: Meta-analysis of Randomized Clinical Trials. Int J Cardiovasc Sci. 2018;31(2):152–162. [Google Scholar]
- 29.Lee CW, Ahn JM, Cavalcante R, Sotomi Y, Onuma Y, Suwannasom P, et al. Coronary artery bypass surgery versus drug-eluting stent implantation for left main or multi vessel coronary artery disease: a meta-analysis of individual patient data. JACC Cardiovasc Interv. 2016;9(24):2481–2489. doi: 10.1016/j.jcin.2016.10.008. [DOI] [PubMed] [Google Scholar]
- 30.Cavalcante R, Sotomi Y, Lee CW, Ahn JM, Farook V, Tateish H, et al. Outcomes after Percutaneous Coronary intervention and Bypass surgery in patients with unprotected left main disease. J Am Coll Cardiol. 2016;68(10):999–1009. doi: 10.1016/j.jacc.2016.06.024. [DOI] [PubMed] [Google Scholar]
- 31.Benedetto U, Gaudino M, Ng C, Biondi-Zoccai G, Dàscenzo F, Frati G, et al. Coronary surgery is superior to drug eluting stents in multivessel disease: Systematic review and meta-analysis of contemporary randomized controlled trials. Int J Cardiol. 2016 May 01;210:19–24. doi: 10.1016/j.ijcard.2016.02.090. [DOI] [PubMed] [Google Scholar]
- 32.Palmerini T, Serruys P, Kappetein AP, Genereux P, Riva DD, Reggianni LB, et al. Clinical outcomes with percutaneous coronary revascularization versus coronary artery bypass grafting surgery in patients with unprotected left main coronary artery disease: a meta-analysis of six randomized trials and 4,686 patients. Am Heart J. 2017 Aug;190:54–63. doi: 10.1016/j.ahj.2017.05.005. [DOI] [PubMed] [Google Scholar]
- 33.Bangalore S, Guo Y, Samadashvili Z, Blecker S, Jinfeng X, Hannan EL. Everolimus-Eluting Stents or Bypass Surgery for Multivessel Coronary Disease. N Eng J Med. 2015;372(13):1213–1222. doi: 10.1056/NEJMoa1412168. [DOI] [PubMed] [Google Scholar]
- 34.Tong BC, Huber JC, Ascheim DD, Puskas JD, Ferguson TB Jr, Blackstone EH, et al. Weighting composite events endpoints in clinical trials: essential evidence for the heart team. Ann Thorac Surg. 2012;94(6):1908–1913. doi: 10.1016/j.athoracsur.2012.05.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Head SJ, Milojevic M, Daemen J, Ahn JM, Boersma E, Christiansen EH, et al. Mortality after coronary artery bypass grafting versus percutaneous coronary intervention with stenting for coronary artery disease: a polled analysis of individual patient data. Lancet. 2018;391(10124):939–948. doi: 10.1016/S0140-6736(18)30423-9. [DOI] [PubMed] [Google Scholar]
- 36.Escaned J, Collet C, Ryan N, De Maria GL, Walsh S, Sabate M, et al. Clinical outcomes of state-of-the-art percutaneous coronary revascularization in patients with de novo three vessel disease: 1-year results of the SYNTAX II study. Eur Heart J. 2017;38(42):3124–3134. doi: 10.1093/eurheartj/ehx512. [DOI] [PMC free article] [PubMed] [Google Scholar]