Abstract
The goal of treatment of leptomeningeal metastasis is to improve survival and to maintain quality of life by delaying neurological deterioration. Tumour-specific therapeutic options include intrathecal pharmacotherapy, systemic pharmacotherapy and focal radiotherapy. Recently, improvement of leptomeningeal disease–related progression-free survival by adding intrathecal liposomal cytarabine to systemic treatment versus systemic treatment alone has been observed in a randomised phase III trial for patients with breast cancer with newly diagnosed leptomeningeal metastasis. Safety and efficacy of intrathecal administration of new agents such as trastuzumab are under evaluation. Systemic therapy using targeted agents and immunotherapy has also improved outcome in patients with brain metastasis, and its emerging role in the management of leptomeningeal metastasis needs to better studied in prospective series. Focal radiotherapy is commonly indicated for the treatment of macroscopic disease such as meningeal nodules or clinically symptomatic central nervous system structures, for example, base of skull with cranial nerve involvement or cauda equine syndrome. The role of whole brain radiotherapy is decreasing. An individualised combination of different therapeutic options should be used considering the presentation of leptomeningeal metastasis, as well as the histological and molecular tumour characteristics, the presence of concomitant brain and systemic metastases, and prior cancer-directed treatments.
Keywords: carcinomatous, chemotherapy, cerebrospinal, intrathecal, meningitis, radiotherapy, targeted
Introduction
Leptomeningeal metastasis is defined as the spread of tumour cells within the leptomeninges and the subarachnoid space. Approximately 10% of patients with solid cancer will present with leptomeningeal metastases during the course of disease, commonly in the context of progressive systemic disease. The incidence of central nervous system metastasis, including leptomeningeal metastases, seems to be increasing, possibly due to improved survival of patients with cancer related to the development of new systemic agents that are probably less effective within the central nervous system compartment than outside, and to improved diagnostic assessment. Breast cancer, lung cancer and melanoma are the main primary tumours in patients with leptomeningeal metastasis.
The diagnosis of leptomeningeal metastases can be challenging. It is based on clinical evaluation, cerebrospinal MRI and cerebrospinal fluid (CSF) analysis. According to EANO–ESMO guidelines, the diagnosis of leptomeningeal metastases can be confirmed by detection of tumour cells in the CSF, probable in presence of typical clinical and imaging signs in a patient with a known cancer, or possible (table 1).1 The classification of leptomeningeal metastasis considers also the imaging presentation which guides clinical decision-making independently of the identification of tumour cells in the CSF. Four types have been defined: type A with linear leptomeningeal contrast enhancement only, type B with leptomeningeal nodules only, type C with the combination of both, and type D without positive CSF cytology and with a MRI that is normal except for potentially hydrocephalus.
Table 1.
EANO–ESMO subtypes of leptomeningeal metastases, adapted from the EANO–ESMO leptomeningeal metastases guidelines (Le Rhun et al1)
| Cytology/biopsy | MRI | Confirmed | Probable* | Possible* | Lack of evidence | ||
| Type I: positive CSF cytology or biopsy | IA | + | Linear | + | n.a. | n.a. | n.a. |
| IB | + | Nodular | + | n.a. | n.a. | n.a. | |
| IC | + | Linear+nodular | + | n.a. | n.a. | n.a. | |
| ID | + | Normal | + | n.a. | n.a. | n.a. | |
| Type II: clinical findings and neuroimaging only | IIA | − or equivocal | Linear | n.a.† | With typical clinical signs | Without typical clinical signs | n.a. |
| IIB | − or equivocal | Nodular | n.a. | With typical clinical signs | Without typical clinical signs | n.a. | |
| IIC | − or equivocal | Linear+nodular | n.a. | With typical clinical signs | Without typical clinical signs | n.a. | |
| IID | − or equivocal | Normal | n.a. | n.a. | With typical clinical signs | Without typical clinical signs |
*requires a history of cancer
†not applicable
CSF, cerebrospinal fluid.
Goal of the treatment
Survival for patients with leptomeningeal metastases is poor, limited to a few months in most patients. The median survival has been estimated at 3.5 to 4.4 months for leptomeningeal metastases from breast cancer, 3 to 6 months for leptomeningeal metastases from lung cancer and 1.7 to 2.5 months for leptomeningeal metastases from melanoma. Neurological symptoms and signs are usually fixed and rarely improve with therapeutic interventions. The goal of treatment is therefore to prolong survival and to maintain quality of the life by delaying further neurological deterioration.
Prognostic factors
Performance status at diagnosis of leptomeningeal metastasis diagnosis is the most important prognostic factor. Other factors include the type of primary tumour, the protein level in the CSF at diagnosis, the administration of systemic or intrathecal pharmacotherapy, and initial response to treatment. The role of whole brain radiotherapy (WBRT) regarding overall survival remains controversial.
Therapeutic options for patients with leptomeningeal metastases
Therapeutic strategies include intrathecal pharmacotherapy, systemic pharmacotherapy and radiotherapy. Intrathecal therapy is widely used for the treatment of leptomeningeal metastases.2 There is a rationale to use intrathecal treatment in patients with floating tumour cells in the CSF and for linear diffuse or ependymal spread enhancement. However, intrathecal therapy has only a limited penetration into solid tumour lesions and may be inefficient and even toxic in case of CSF flow obstructions. In the latter situation, radiotherapy can be used to restore CSF flow—successful restoration should be checked prior the use of an intrathecal treatment.
Only six randomised trials on the treatment of leptomeningeal metastases have been reported.3–8 Four trials have compared different regimens of intra-CSF chemotherapy in patients with leptomeningeal metastases from various primary tumours. Two trials have explored the role of adding intra-CSF chemotherapy to systemic treatment for the management of leptomeningeal metastases from breast cancer. In the first trial, the combination of intraventricular methotrexate and systemic chemotherapy failed to improve the survival in the combined treatment arm (7.57 months in the systemic therapy only arm vs 4.57 months in the combined modality arm).6 Yet, enrolment was stopped after 35 instead of 50 patients because of poor accrual, and a high rate of ventricular infection was noted with 18% of reservoir revisions which may have negatively influenced outcome in the experimental arm. In the Depo-Sein trial (NCT01645839), 73 patients were randomised between systemic treatment alone and liposomal cytarabine plus systemic treatment. The main objective was to demonstrate that adding intrathecal liposomal cytarabine to systemic treatment improved leptomeningeal metastases–related progression-free survival (PFS). Leptomeningeal metastases PFS was 3.8 months in the combined arm versus 2.2 in the systemic treatment alone arm (HR 0.61, 95% CI 0.38 to 0.98, p=0.04) in the intent-to-treat population. Quality of life was preserved in the experimental arm. No significant difference was observed in terms of overall survival in the intent-to-treat population; however, the adjusted HR for overall survival was 0.60 (0.35–1.02) with p=0.06 in the intent-to-treat population.1
The three agents mainly used for intra-CSF treatment of leptomeningeal metastasis are methotrexate, (liposomal) cytarabine and thiotepa. Other compounds are also under evaluation. Trastuzumab has been evaluated in a phase I study in patients with breast cancer with leptomeningeal metastases with Her2-positive tumours, with a good tolerance (NCT01373710).9 Data of a second trial on safety of dose-escalated intrathecal trastuzumab are still pending (NCT01325207).
Intrathecal pharmacotherapy can be administered via repeated lumbar punctures or via ventricular devices. The ventricular route has several advantages, such as avoiding delivery of the drug into the epidural or subdural space, allowing a uniform distribution of the drug and better patient comfort. The safety of ventricular devices has been confirmed in different cohorts with revision rates below 7.4%. A longer PFS was observed for methotrexate, but not for liposomal cytarabine, when using a ventricular device in a secondary analysis of a randomised trial, presumably due to the different half-lives of the agents.10 Altogether, clinical experience and available evidence favour the intraventricular route.
Systemic pharmacotherapy, if active, should cover leptomeningeal lesions with contrast enhancement, reflecting absence of an intact blood–brain or spinal cord barrier, because such pharmacotherapy should reach sites of disease just as good as intravenously administered contrast agent. The disruption of the blood–CSF barrier indicated by elevated CSF protein in many patients with leptomeningeal metastasis suggests that the subarachnoid space may be reached by systemic pharmacotherapy to a certain extent, too. No randomised dedicated trials to explore the role of systemic pharmacotherapy in patients with leptomeningeal metastases have been conducted and only few data regarding systemic pharmacotherapy are available in this population. Systemic agents should be selected according to the primary tumour and its molecular characteristics and prior therapy. Among 32 patients with heavily pre-treated leptomeningeal metastasis with EGFR-mutant non-small cell lung cancer, including 11 patients with the Thr790Met mutation, treated by osimertinib, 10 had an objective imaging response.11 Partial responses and stable disease have been reported after high-dose intravenous thiotepa,12 ANG1005, a paclitaxel/Angiopep-2 drug conjugate,13 and a combination of bevacizumab with etoposide and cisplatin14 in patients with breast cancer with leptomeningeal metastases. A median survival of 16.9 weeks was noted in 25 patients with melanoma with leptomeningeal metastases, with a median of 21.7 weeks for 21 patients treated by immunotherapy or targeted therapy.15 A phase II trial met its primary endpoint with 44% patients alive at 3 months in a cohort of 18 patients with leptomeningeal metastases from various primary tumours, including 15 patients with breast cancer, treated with pembrolizumab (NCT02886585).
No trial has investigated the efficacy and safety of radiotherapy alone (WBRT or craniospinal irradiation) in patients with leptomeningeal metastases. Involved-field radiotherapy using single fractions or fractionated regimens can be used to treat meningeal nodules and symptomatic cerebral or spinal sites. The safety of the combination of intrathecal methotrexate plus dexamethasone and concomitant involved field radiotherapy has been explored in a phase II trial in patients with leptomeningeal metastases from various primaries.16 A median overall survival of 6.5 months and 20.3% of grades 3–4 adverse events were observed. Prolonged responses have been reported in patients presenting with nodular or bulky disease previously treated by WBRT. In the presence of cranial nerve impairment, irradiation of skull base, interpeduncular cistern or the two first cervical vertebrae may be indicated; irradiation of lumbosacral vertebrae may be indicated for cauda equina syndrome.1 No survival benefit of WBRT was observed in most retrospective studies of patients with leptomeningeal metastasis. WBRT may be an option in selected patients with extensive nodular diseased or symptomatic linear meningeal disease or in the presence of concomitant brain metastases. Cerebrospinal radiotherapy is rarely an option for adult patients with leptomeningeal metastases from solid cancers because of the risk of bone marrow toxicity, enteritis and mucositis in a context of concomitant systemic disease and the need of systemic pharmacotherapy.
Combination of treatment
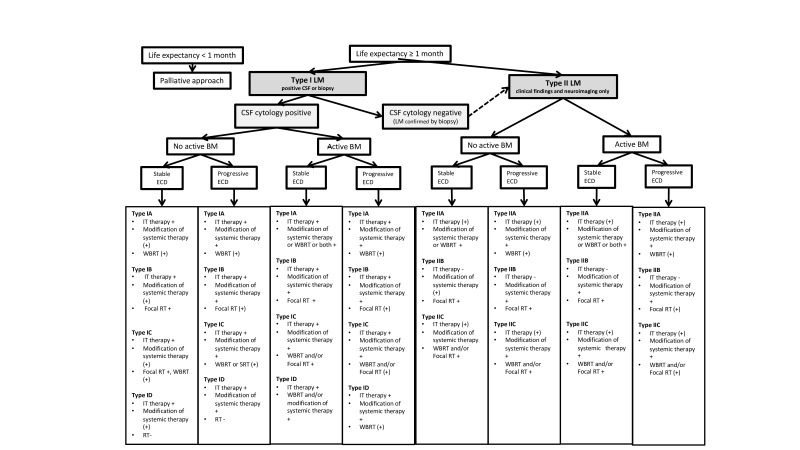
The EANO–ESMO guideline provides expert opinion–based recommendations for the diagnosis and the management of leptomeningeal metastases from solid tumours.1 Treatment depends on pathological and molecular tumour characteristics, prior treatments, general health status, concomitant brain metastases, the evolution of the extra-CNS disease and the presentation of leptomeningeal metastases (figure 1).
Figure 1.
EANO ESMO Therapeutic approach to LM. +, recommended; (+), optional; -, not recommended; BM, brain metastases; CSF, cerebrospinal fluid; ECD, extracranial disease; IT, intrathecal; LM, leptomeningeal metastases; RT, radiotherapy; WBRT, whole brain radiotherapy.
If tumour cells are found in the CSF, intrathecal pharmacotherapy is commonly recommended, irrespective of the MRI presentation. A modification of systemic pharmacotherapy should always be considered if leptomeningeal metastases are diagnosed. Focal radiotherapy should be given for symptomatic nodular disease or in presence of symptomatic lesions of cranial nerves or cauda equina.
If no tumour cells are detected in the CSF, intrathecal therapy can still be considered in the presence of linear meningeal contrast enhancement. It is not recommended in the presence of nodular meningeal disease only.
Supportive care
Supportive care is particularly important in patients with leptomeningeal metastases. The lowest dose of steroids should be used for the shortest time. Seizures should be managed with drugs that do not interact with systemic treatments. Primary seizure prophylaxis is not recommended. Symptomatic hydrocephalus may be relieved by ventriculoperitoneal shunt or a ventricular device. Patient and caregiver need for psycho-oncological support should be explored.
Assessment of leptomeningeal metastasis during follow-up
The follow-up of patients with leptomeningeal metastases should be performed regularly to guide the therapeutic strategy and to adjust supportive care. Clinical and imaging evaluations are usually part of the evaluation of leptomeningeal metastases. The role of repeat CSF cytology remains controversial. The clinical evaluation may be challenging as symptoms and signs may vary depending on the pattern of leptomeningeal metastasis lesions. Symptoms and signs related to brain metastases, extra-CNS progression, neurotoxicity or associated disease can be associated and difficult to distinguish. Thus, clinical deterioration is not necessarily related to leptomeningeal metastasis progression, and biological, neurophysiological and imaging explorations may be needed in case of neurological deterioration. Cerebrospinal MRI should be performed every 2 months for the first 6 months and then every 3 months in case of stable disease, preferably on the same scanner or on scanners with the same field strength.1 Standardised tools should ideally be used for the clinical and imaging evaluation, but no validated tools are currently available. The imaging scorecard proposed by the RANO leptomeningeal metastasis group has been shown not to be useful in clinical practice,17 but is currently undergoing a revision and re-evaluation.
Conclusion
The treatment of leptomeningeal metastases needs to be individualised. The primary tumour and its systemic treatment options as well as clinical, imaging and cytological presentation of leptomeningeal metastases guides the combination of intrathecal therapy, systemic pharmacotherapy and focal radiotherapy. A modification of the systemic treatment should be considered taking into account the histological and molecular subtype of the cancer. Involved-field radiotherapy may have a role for the treatment of meningeal nodules and clinically symptomatic central nervous system involvement. The different options should be discussed according to general and neurological health status, presence of other metastatic sites, including brain metastases, and previous treatment. Dedicated trials are needed to improve levels of evidence for all therapeutic measures for patients with leptomeningeal metastases.
Footnotes
Contributors: ELR designed and conceptualised the manuscript; drafted the manuscript for intellectual content. MP revised the manuscript for intellectual content. MvdB revised the manuscript for intellectual content. NA revised the manuscript for intellectual content. MW designed and conceptualised the manuscript; drafted the manuscript for intellectual content.
Competing interests: ELR has received research grants from Mundipharma and Amgen and honoraria for lectures or advisory board participation from Abbvie, Daiichi Sankyo, Mundipharma and Novartis. MP has received honoraria for lectures, consultation or advisory board participation from the following for-profit companies: Bayer, Bristol-Myers Squibb, Novartis, Gerson Lehrman Group (GLG), CMC Contrast, GlaxoSmithKline, Mundipharma, Roche, Astra Zeneca, AbbVie, Lilly, Medahead, Daiichi Sankyo, Merck Sharp & Dohme. MvdB has received research support from AbbVie and declares honoraria from Celgene, BMS, AbbVie, Agios and Boehringer Ingelheim. NA has received grants from Brainlab AG and personal fees from AstraZeneca. MW has received research grants from Abbvie, Adastra, Dracen, Merck, Sharp & Dohme (MSD), Merck (EMD), Novocure, OGD2, Piqur and Roche, and honoraria for lectures or advisory board participation or consulting from Abbvie, Basilea, Bristol Meyer Squibb, Celgene, Merck Sharp & Dohme (MSD), Merck (EMD), Novocure, Orbus, Roche and Tocagen.
Patient consent for publication: Not required.
Provenance and peer review: Commissioned; internally peer reviewed.
References
- 1.Le Rhun E, Weller M, Brandsma D, et al. . EANO-ESMO clinical practice guidelines for diagnosis, treatment and follow-up of patients with leptomeningeal metastasis from solid tumours. Ann Oncol 2017;28(suppl_4):iv84–99. 10.1093/annonc/mdx221 [DOI] [PubMed] [Google Scholar]
- 2.Le Rhun E, Rudà R, Devos P, et al. . Diagnosis and treatment patterns for patients with leptomeningeal metastasis from solid tumors across Europe. J Neurooncol 2017;133:419–27. 10.1007/s11060-017-2452-6 [DOI] [PubMed] [Google Scholar]
- 3.Grossman SA, Finkelstein DM, Ruckdeschel JC, et al. . Randomized prospective comparison of intraventricular methotrexate and thiotepa in patients with previously untreated neoplastic meningitis. Eastern Cooperative Oncology Group. J Clin Oncol 1993;11:561–9. 10.1200/JCO.1993.11.3.561 [DOI] [PubMed] [Google Scholar]
- 4.Hitchins RN, Bell DR, Woods RL, et al. . A prospective randomized trial of single-agent versus combination chemotherapy in meningeal carcinomatosis. J Clin Oncol 1987;5:1655–62. 10.1200/JCO.1987.5.10.1655 [DOI] [PubMed] [Google Scholar]
- 5.Glantz MJ, Jaeckle KA, Chamberlain MC, et al. . A randomized controlled trial comparing intrathecal sustained-release cytarabine (DepoCyt) to intrathecal methotrexate in patients with neoplastic meningitis from solid tumors. Clin Cancer Res 1999;5:3394–402. [PubMed] [Google Scholar]
- 6.Boogerd W, van den Bent MJ, Koehler PJ, et al. . The relevance of intraventricular chemotherapy for leptomeningeal metastasis in breast cancer: a randomised study. Eur J Cancer 2004;40:2726–33. 1990 10.1016/j.ejca.2004.08.012 [DOI] [PubMed] [Google Scholar]
- 7.Shapiro WR, Schmid M, Glantz M, et al. . A randomized phase III/IV study to determine benefit and safety of cytarabine liposome injection for treatment of neoplastic meningitis. J Clin Oncol;24(No 18_suppl). [Google Scholar]
- 8.Le Rhun E, Mailliez A, Wallet J, et al. . 371OIntra-CSF liposomal cytarabine plus systemic therapy as initial treatment of breast cancer leptomeningeal metastasis: a randomised, open-label trial. Annals of Oncology 2018;29(suppl_8):viii122–32. 10.1093/annonc/mdy273.359 [DOI] [Google Scholar]
- 9.Bonneau C, Paintaud G, Trédan O, et al. . Phase I feasibility study for intrathecal administration of trastuzumab in patients with HER2 positive breast carcinomatous meningitis. Eur J Cancer 2018;95:75–84. 10.1016/j.ejca.2018.02.032 [DOI] [PubMed] [Google Scholar]
- 10.Glantz MJ, Van Horn A, Fisher R, et al. . Route of intracerebrospinal fluid chemotherapy administration and efficacy of therapy in neoplastic meningitis. Cancer 2010;116:1947–52. 10.1002/cncr.24921 [DOI] [PubMed] [Google Scholar]
- 11.Yang JC-H, Kim D-W, Kim S-W, et al. . Osimertinib activity in patients (PTS) with leptomeningeal (LM) disease from non-small cell lung cancer (NSCLC): updated results from Bloom, a phase I study. JCO 2016;34(15_suppl):9002 10.1200/JCO.2016.34.15_suppl.9002 [DOI] [Google Scholar]
- 12.Chahal J, Stopeck A, Clarke K, et al. . Intravenous thiotepa for treatment of breast cancer-related leptomeningeal carcinomatosis: case series. Neurol Sci 2015;36:1691–3. 10.1007/s10072-015-2259-1 [DOI] [PubMed] [Google Scholar]
- 13.Tang S, Kumthekar P, Brenner AJ, et al. . 1005, a novel brain-penetrant taxane derivative, for the treatment of recurrent brain metastases and leptomeningeal carcinomatosis from breast cancer. Annals of Oncology 2016;27:103–13. [Google Scholar]
- 14.P-F W, Lin C-H, Kuo C-H, et al. . A pilot study of bevacizumab combined with etoposide and cisplatin in breast cancer patients with leptomeningeal carcinomatosis. BMC Cancer 2015;15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Geukes Foppen MH, Brandsma D, Blank CU, et al. . Targeted treatment and immunotherapy in leptomeningeal metastases from melanoma. Ann Oncol 2016;27:1138–42. 10.1093/annonc/mdw134 [DOI] [PubMed] [Google Scholar]
- 16.Pan Z, Yang G, He H, et al. . Concurrent radiotherapy and intrathecal methotrexate for treating leptomeningeal metastasis from solid tumors with adverse prognostic factors: a prospective and single-arm study. Int J Cancer 2016;139:1864–72. 10.1002/ijc.30214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Le Rhun E, Devos P, Boulanger T, et al. . The RANO leptomeningeal metastasis group proposal to assess response to treatment: lack of feasibility and clinical utility and a revised proposal. Neuro-Oncol 2019;56 10.1093/neuonc/noz024 [DOI] [PMC free article] [PubMed] [Google Scholar]