Abstract
Objective:
The treatment gap between those who need and those who receive care for eating disorders is wide. Scaling a validated, online screener that makes individuals aware of the significance of their symptoms/behaviors is a crucial first step for increasing access to care. The objective of the current study was to determine the reach of disseminating an online eating disorder screener in partnership with the National Eating Disorders Association (NEDA), as well to examine the probable eating disorder diagnostic and risk breakdown of adult respondents. We also assessed receipt of any treatment.
Method:
Participants completed a validated eating disorder screen on the NEDA website over 6 months in 2017.
Results:
Of 71,362 respondents, 91.0% were female; 57.7% 18-24 years; 89.6% non-Hispanic; and 84.7% White. Most (86.3%) screened positive for an eating disorder. In addition, 10.2% screened as high risk for the development of an eating disorder, and only 3.4% as not at risk. Of those screening positive for an eating disorder, 85.9% had never received treatment and only 3.0% were currently in treatment.
Discussion:
The NEDA online screen may represent an important eating disorder detection tool, as it was completed by >71,000 adult respondents over just 6 months, the majority of whom screened positive for a clinical/subclinical eating disorder. The extremely high percentage of individuals screening positive for an eating disorder who reported not being in treatment suggests a wide treatment gap and the need to offer accessible, affordable, evidence-based intervention options, directly linked with screening.
Keywords: eating disorders, referral, screening
Eating disorders are serious mental illnesses (Klump, Bulik, Kaye, Treasure, & Tyson, 2009), and mortality from anorexia nervosa (AN) is the highest of all psychiatric disorders, with the risk of premature death 6-12 times higher in individuals with AN compared to the general population, adjusting for age (Arcelus, Mitchell, Wales, & Nielsen, 2011; Smink, van Hoeken, & Hoek, 2012). Eating disorders are associated with high levels of psychiatric comorbidity, (Hudson, Hiripi, Pope, & Kessler, 2007), and medical complications include cardiovascular, neurological, gastrointestinal, endocrine, and dermatologic problems, among others—eating disorders can affect every organ system (e.g., Forney, Buchman-Schmitt, Keel, & Frank, 2016; Mitchell, 2016; Norris et al., 2016; Sachs, Harnke, Mehler, & Krantz, 2016). These disorders are associated with marked impairment in functioning and are the 12th leading cause of disability in young women in high-income nations (Hoek, 2016).
Unfortunately, statistics indicate that receipt of any treatment for eating disorders is extremely low, and the treatment gap for these devastating problems is wide (Kazdin, Fitzsimmons-Craft, & Wilfley, 2017). In the National Comorbidity Survey-Replication, only 16% of individuals with bulimia nervosa (BN) and 29% of individuals with binge eating disorder (BED) had received treatment in the past 12 months (Hudson et al., 2007). Likewise, less than 20% of college students who screen positive for an eating disorder report receiving treatment (Eisenberg, Nicklett, Roeder, & Kirz, 2011). Thus, few individuals with an eating disorder receive treatment specifically for their disorder, yet these individuals actually exhibit elevated health services use and costs compared to individuals without an eating disorder (Weissman & Rosselli, 2017). Furthermore, the problem of access to care for eating disorders is even worse amongst individuals from minority backgrounds—individuals from racial/ethnic minority backgrounds with eating disorders are significantly less likely than their White counterparts to be diagnosed with an eating disorder, receive care for an eating disorder, or to even be asked by a doctor about eating disorder symptoms (Becker, Franko, Speck, & Herzog, 2003; Cachelin & Striegel-Moore, 2006; Marques et al., 2011).
Actually receiving services for a psychiatric disorder, including an eating disorder, involves multiple steps, including experiencing symptoms, identifying those symptoms as something warranting attention, deciding whether action is required, identifying options for intervention (e.g., “treatment” or something else), seeking and actually obtaining treatment if that option is selected, beginning treatment and remaining in treatment as needed, and with recurrent disorders, completing the process or abbreviated variants of the process again (Kass et al., 2017; Kazdin et al., 2017). Identifying or learning one’s symptoms are something in need of help is thus a crucial first step in accessing care. Having the opportunity to learn that one’s symptoms may be problematic is particularly critical given research suggesting that less than half of individuals with eating disorders recognize they have a problem (Gratwik-Sarll, Mond, & Hay, 2013; Mond, Hay, Rogers, & Owen, 2006). Recognition is even worse when the individual’s eating disorder symptoms do not include self-induced vomiting (Gratwik-Sarll et al., 2013; Mond et al., 2006). Furthermore, research has indicated that self-recognition is associated with help seeking. In one study, close to half of participants who recognized a problem with their eating had ever sought treatment, whereas only one in five participants who did not recognize a problem had sought help (Gratwik-Sarll et al., 2013). These factors highlight the importance of readily available mental health screening that provides individuals with tailored feedback on their symptoms and concrete suggestions for next steps. Notably, such an approach aims to improve eating disorder-related mental health literacy, which is a key component of reducing the public health burden of eating disorders (Mond, 2014, 2016).
To meet this need, we established a partnership with the National Eating Disorders Association (NEDA), the leading non-profit organization related to eating disorders in the U.S., to disseminate an online eating disorders screen. NEDA’s main mission is not to serve eating disorders professionals but rather to support individuals and families affected by eating disorders. NEDA also strives to serve as a catalyst for prevention, cures, and access to quality care (“About Us,” 2018). The purpose of the current study was to report on: 1) reach of the screen to adult respondents over the course of 6 months, including screen reach by week; 2) probable eating disorder diagnoses and risk status, including demographic and anthropometric differences by diagnostic category; and 3) treatment receipt amongst those screening positive for a clinical/subclinical eating disorder, including potential differences in treatment receipt by diagnosis. These data will shed light on the potential for the online screening tool to serve as an eating disorder detection tool and ultimately as a means to address the treatment gap for eating disorders.
Method
Participants and Procedure
Over the course of 6 months, between 2/26/17 and 8/31/17, 97,799 respondents elected to complete an online eating disorder screening tool that was made freely available on the NEDA website (https://www.nationaleatingdisorders.org/screening-tool). The screening tool was primarily promoted through media articles, telephone calls, chat messages, and emails to the NEDA Helpline, Facebook ads, and awareness campaigns, as well as general website traffic. Notably, the start of this time period included National Eating Disorders Awareness Week (NEDAwareness Week; 2/26/17-3/4/17). The goal of NEDAwareness Week is to increase public awareness of eating disorders through social media campaigns, legislative advocacy, and local events, as well as to connect individuals in need with resources (“About NEDAwareness Week,” 2018).
The NEDA website provides the disclaimer that the screening tool is “appropriate for ages 13 and up,” but respondents of any age are able to complete the screen if they elect to do so. In the current study, we focus on adult respondents, with N = 71,362 respondents ≥ 18 years of age included in the current study. We received institutional review board approval to analyze this de-identified dataset.
Measures
Demographics.
Participants self-identified their gender, age, ethnicity, race, partnership status, household income, zip code, and whether or not they were part of a special population (i.e., veteran or active military duty, caregiver or someone living with emotional/physical illness, student, new or expecting mother, LGBTQ). Participants self-reported their height and current weight, which were used to calculate body mass index (BMI; weight kg/height [m2]). Participants were classified as having: underweight (BMI < 18.5), normal weight (BMI 18.5-24.99), overweight (BMI 25.0-29.99), or obesity (BMI ≥ 30).
Probable eating disorder diagnoses and risk status.
The Stanford-Washington University Eating Disorder Screen (SWED; Graham et al., 2018) is a brief screening tool that assesses eating disorder behaviors, pathology, and impairment and can be used to identify possible DSM-5 eating disorder diagnoses. The SWED includes questions from the Weight Concerns Scale (WCS; Killen et al., 1994) and items adapted from the Eating Disorder Examination-Questionnaire (EDE-Q; Fairburn & Beglin, 1994) and the Eating Disorder Diagnostic Scale (EDDS; Stice, Telch, & Rizvi, 2000). Responses are used to categorize individuals into one of seven possible DSM-5 diagnoses or two risk categories: 1) anorexia nervosa (AN); 2) bulimia nervosa (BN); 3) binge eating disorder (BED); 4) subclinical bulimia nervosa (sub-BN); 5) subclinical binge eating disorder (sub-BED); 6) unspecified feeding or eating disorder (UFED); 7) avoidant/restrictive food intake disorder (ARFID); 8) high risk for an eating disorder; or 9) not at risk for an eating disorder. The SWED screening algorithm was validated in college-age women, with sensitivities ranging from 0.68 (sub-BN) to 0.90 (AN) and specificities ranging from 0.79 (sub-BED) to 0.99 (AN) compared to diagnostic interview (see Graham et al., 2018 for additional information), and has been used in past research among both men and women (Fitzsimmons-Craft et al., 2018). The question, “Are you currently in treatment for an eating disorder?” (with response options of: “no”; “yes”; and “not currently, but in the past” provided) was used to assess eating disorder treatment status. Respondents were provided brief feedback based on their screening results, tailored to their level of eating disorder pathology, and were provided with information on available resources for accessing treatment (e.g., NEDA Helpline) (see online supplemental material).
Analytic Strategy
Data were cleaned based on the following rules: 1) self-reported eating disorder behaviors (i.e., fasting, laxatives/diuretics, excessive exercise, vomiting, binge eating) that were above implausible values (i.e., frequency ≥ 500 over the course of 3 months) were removed and considered missing; 2) biologically implausible weights for adults (i.e., < 50 pounds or > 650 pounds) were removed and considered missing; and 3) biologically implausible heights for adults (i.e., < 48 inches or > 84 inches) were removed and considered missing. In order to generate an eating disorder diagnostic or risk category, respondents were required to have provided data on all SWED items, including height and weight. If these data were missing, an eating disorder diagnostic or risk category was not assigned.
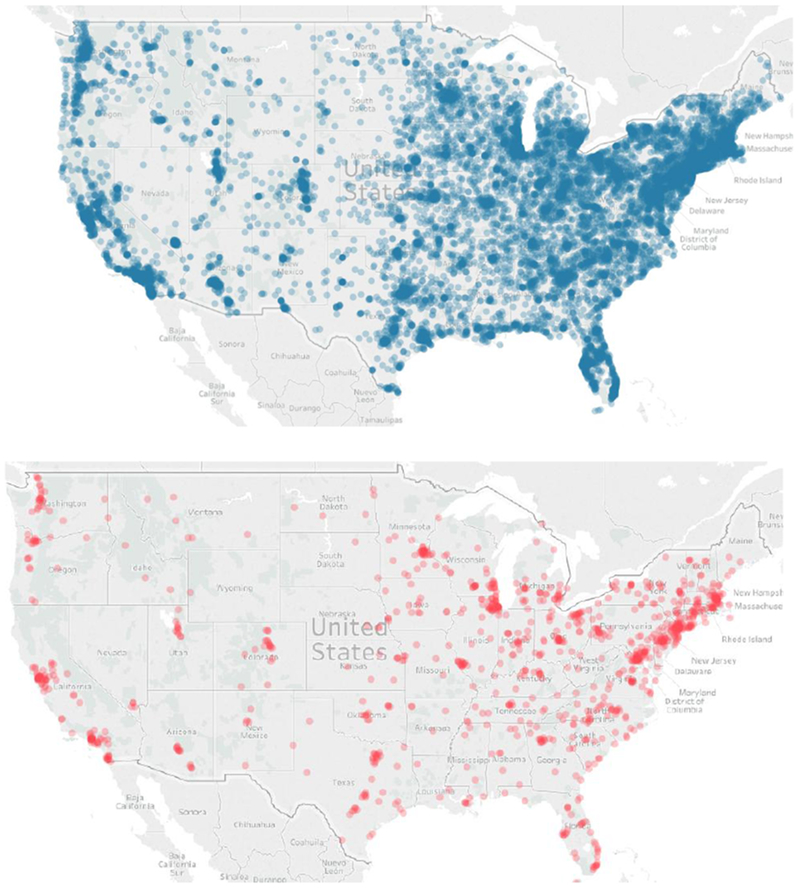
First, reach of the screen (i.e., number of screens completed), including screens completed by week, was examined descriptively. Second, results of the screen regarding eating disorder diagnostic and risk breakdown and data on treatment receipt amongst those screening positive for a clinical/subclinical eating disorder (i.e., AN, BN, BED, sub-BN, sub-BED, UFED, ARFID) were examined descriptively. Using participants’ self-reported zip code data, U.S. maps depicting screen reach and individuals screening positive for a clinical/subclinical eating disorder not in treatment were generated using Tableau version 2018.1. Third, differences in demographic and anthropometric (i.e., BMI) variables by eating disorder diagnostic category (i.e., AN vs. BN/sub-BN vs. BED/sub-BED vs. other eating disorder vs. no eating disorder) were examined using chi-square analyses and analyses of variance (ANOVAs). Fourth, differences in treatment status by the clinical/subclinical eating disorder groups were examined using chi-square analyses, comparing percent currently receiving treatment to percent not currently in treatment and never in treatment. Significance was defined as p < .05. Aside from generating maps using Tableau, all other data analyses were conducted using SPSS version 25.
Results
Screen Reach and Descriptive Statistics
From 2/26/17-8/31/17, the screen was completed 71,362 times by respondents ≥ 18 years of age. Screen reach by week is depicted in Figure 1. As depicted, 16,460 (23.1%) screens were completed during NEDAwareness Week. During weeks outside of NEDAwareness Week, 2,112 respondents completed the screen each week on average. As evidenced in Figure 2A, the screen had a wide geographical reach, with respondents being located in many parts of the U.S. As seen in Table 1, the majority of the sample was female (91.0%), non-Hispanic (89.6%), and White (84.7%). Just over half of the sample was between the ages of 18 and 24 (57.7%). While all four weight classes were represented in the sample, the most common weight status was normal weight (51.5%) and the average BMI (25.38 ± 7.52) was slightly overweight. Of those who completed the screen, 1.2% identified as a veteran or currently active military, 3.7% as a caregiver of someone living with an emotional or physical illness, 47.9% as a student, 2.3% as a new or expecting mother, and 13.3% as LGBTQ.
Figure 1.
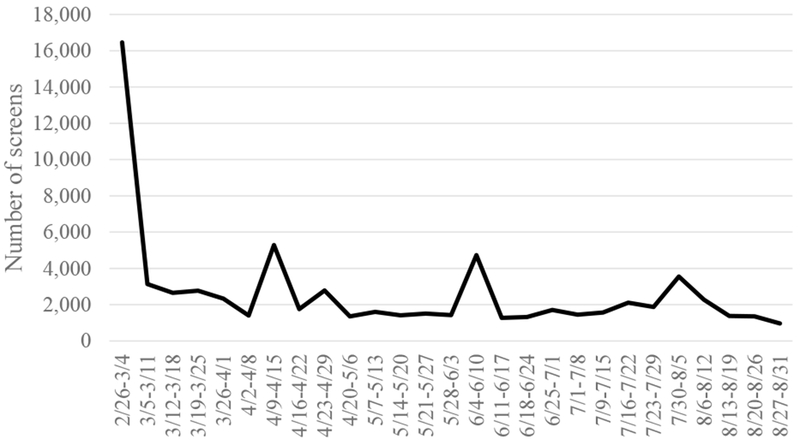
Numbers of screens by week, total N = 71,362; NEDAwareness Week was 2/26-3/4.
Figure 2.
Maps depicting reach of the screen (Map A) and screen respondents screening positive for a clinical/subclinical eating disorder currently in treatment (Map B).
Table 1.
Screen Results and Demographics (N=71,362)
| No. (%) | |
|---|---|
| Gender (n=71,256) | |
| Female | 64,848 (91.0%) |
| Male | 4,292 (6.0%) |
| Other | 2,116 (3.0%) |
| Age (n=71,256) | |
| 18-24 | 41,108 (57.7%) |
| 25-34 | 16,340 (22.9%) |
| 35-44 | 6,825 (9.6%) |
| 45-54 | 4,115 (5.8%) |
| 55-64 | 2,166 (3.0%) |
| 65+ | 702 (1.0%) |
| Weight status (n=64,516) | |
| Underweight | 6,378 (9.9%) |
| Normal weight | 33,197 (51.5%) |
| Overweight | 11,897 (18.4%) |
| Obesity | 13,044 (20.2%) |
| Ethnicity (n=51,400) | |
| Non-Hispanic/Non-Latino | 46,055 (89.6%) |
| Hispanic/Latino | 5,345 (10.4%) |
| Race (n=67,608) | |
| White | 57,297 (84.7%) |
| Black | 1,772 (2.6%) |
| Asian | 3,465 (5.4%) |
| More than one | 2,985 (4.4%) |
| Other | 2,089 (3.1%) |
| Partnership status (n=70,921) | |
| Single | 34,939 (49.3%) |
| Partnered, living separately | 11,103 (15.7%) |
| Living with partner | 7,251 (10.2%) |
| Married or domestic partnership | 15,363 (21.7%) |
| Divorced/Separated | 1,971 (2.8%) |
| Widowed | 294 (0.4%) |
| Household income (n=68,813) | |
| < $40,000 | 20,012 (29.1%) |
| $40,000-79,999 | 13,373 (19.5%) |
| $80,000-149,999 | 10,769 (15.6%) |
| > $150,000 | 5,578 (8.1%) |
| Prefer not to answer | 19,801 (27.7%) |
Note. For each variable, we list the n for which data on that particular variable were available.
Eating disorder diagnostic and risk categories were able to be assigned for 64,595 participants. Eating disorder pathology was prevalent among the sample: 86.3% screened as having a possible clinical or subclinical eating disorder. Specifically, 5.7% of the sample (n = 3,688) screened as AN, 11.0% (n = 7,123) as BN, 4.2% (n = 2,725) as BED, 23.7% (n = 15,290) as sub-BN, 3.9% (n = 2,529) as sub-BED, 33.3% (n = 21,519) as UFED, and 4.5% (n = 2,923) as ARFID. In addition, 10.2% (n = 6,602) screened as high risk for the development of an eating disorder, and only 3.4% (n = 2,196) as not at risk for an eating disorder.
Differences in Demographic and Anthropometric Variables by Eating Disorder Diagnostic Category
As depicted in Table 2, gender, age, ethnicity, race, partnership status, household income, and BMI all differed by eating disorder diagnostic category (ps < .001). Respondents classified as screening positive for AN, BN/sub-BN, and BED/sub-BED had higher rates of self-identifying as female compared with respondents classified as other eating disorder (i.e., AFRID and UFED) and no eating disorder (i.e., high risk and low risk). Respondents classified as screening positive for AN were most likely to report being between 18-24 years of age (69.3%), and those classified as BED/sub-BED were least likely to report being between 18-24 years of age (44.0%). Those classified as having possible AN were most likely to report being single (57.7%), while those without an eating disorder were the least likely to report being single (40.1%). Those classified as having possible AN and BN/sub-BN were most likely to report having a household income < $40,000/year (43.6%, 43.2%), while those without an eating disorder were the least likely to report having a household income <$40,000/year (31.9%). While the vast majority of the sample self-identified as being non-Hispanic and White, individuals classified as having possible BED/sub-BED had the highest rates of individuals who self-identified as non-Hispanic (92.0%) and White (88.5%). Self-reported BMI was the lowest for those classified as screening positive for AN (16.91) and highest for those classified as BED/Sub-BED (31.67).
Table 2.
Demographic differences by eating disorder diagnostic category (n = 64,595)
| AN (n=3,688) | BN/sub-BN (n=22,413) | BED/sub-BED (n=5,254) | Other ED (n=24,442) | No ED (n=8,798) | Overall Significance | |
|---|---|---|---|---|---|---|
| Gender (% Female) | 92.8a | 92.1a | 92.8a | 89.5b | 90.5b | X2(4,64,589) = 138.22; p<.001 Cramer’s V = .05 |
| Age (% 18-24) | 69.3a | 65.2b | 44.0c | 58.5d | 46.9e | X2(4,64,589) = 1538.56; p<.001 Cramer’s V = .15 |
| Ethnicity (% non-Hispanic) | 91.9a | 88.9b | 92.0a | 89.4b | 89.2b | X2(4,46,196) = 50.96; p<.001 Cramer’s V = .03 |
| Race (% White) | 84.1ab | 83.7a | 88.5c | 84.7ab | 85.2b | X2(4,61,434) = 76.27; p<.001 Cramer’s V = .04 |
| Partnership status (% single) | 57.7a | 54.9b | 41.5c | 49.1d | 40.1e | X2(4,64,331) = 803.68; p<.001 Cramer’s V = .11 |
| Household Income (% < 40,000) | 43.6a | 43.2a | 36.3b | 40.5c | 31.9d | X2(4,45249) = 274.33; p<.001 Cramer’s V = .08 |
| BMI | 16.91a | 25.96b | 31.67c | 24.93d | 24.88d | F(4,64,586) = 2489.58; p<.001 Partial eta squared = .15 |
Note. AN = anorexia nervosa, BN = bulimia nervosa, sub-BN = subclinical bulimia nervosa, BED = binge eating disorder, sub-BED = subclinical binge eating disorder, UFED = unspecified feeding or eating disorder, ARFID = avoidant/restrictive food intake disorder, Other ED = UFED + ARFID, No ED = high risk for an eating disorder + no risk for an eating disorder.
Groups sharing the same superscript are not significantly different from each other (p<0.05).
Eating Disorder Treatment Receipt and Differences in Treatment Receipt across Diagnostic Categories
As depicted in Table 3, rates of treatment amongst those with a clinical/subclinical eating disorder were low in the sample, with only 3.0% of the sample reporting that they were currently in treatment and only 11.1% reporting having received eating disorder treatment in the past. In total, 85.9% reported not receiving any eating disorder treatment at any point. Figures 2B and 2C geographically depict individuals with a clinical/subclinical eating disorder currently in treatment and not currently in treatment, respectively.
Table 3.
Eating disorder treatment status by possible DSM-5 clinical/subclinical diagnosis (n=55,797)
| Across diagnostic categories | AN (n=3,688) | BN (n=7,123) | BED (n=2,725) | Sub-BN (n=15,290) | Sub-BED (n=2,529) | UFED (n=21,519) | ARFID (n=2,923) | Significance | |
|---|---|---|---|---|---|---|---|---|---|
| % No | 85.9 | 73.2 | 81.3 | 90.8 | 87.1 | 90.2 | 86.7 | 93.0 | - |
| % Not currently but in the past | 11.1 | 19.5 | 14.3 | 6.7 | 10.6 | 8.1 | 10.6 | 6.0 | - |
| % Yes | 3.0 | 7.3a | 4.4b | 2.5c | 2.3c | 1.7d | 2.8c | 1.1d | X2(6,55,791) = 364.16; p<.001 Cramer’s V = .08 |
Note. AN = anorexia nervosa, BN = bulimia nervosa, BED = binge eating disorder, sub-BN = subclinical bulimia nervosa, sub-BED = subclinical binge eating disorder, UFED = unspecified feeding or eating disorder, ARFID = avoidant/restrictive food intake disorder; significance test comparing %yes vs. % no and not currently but in the past. Groups sharing the same superscript are not significantly different from each other (p<0.05).
Rates of current eating disorder treatment differed by eating disorder diagnosis (p < .001). Those screening positive for AN were most likely to be currently in treatment for an eating disorder (7.3%), followed by those screening positive for BN (4.4%). Rates of current treatment were lowest in those screening positive for AFRID (1.1%) and sub-BED (1.7%).
Discussion
The current study reported on our collaboration with NEDA, the leading non-profit organization related to eating disorders in the U.S., to disseminate an online eating disorders screen. To our knowledge, this is among the first instances of a large-scale, national dissemination of a screening tool for eating disorders outside of surveillance research in the U.S. or elsewhere, which was confirmed by contacting leading eating disorders researchers in other countries who would have been aware of such efforts if they existed (P. Diedrichs, personal communication, December 6, 2018; L. Hart, personal communication, December 7, 2018; C. Jacobi, personal communication, December 6, 2018; D. Nicholls, personal communication, December 16, 2018; S. Paxton, personal communication, December 7, 2018; Z. Yager, personal communication, December 5, 2018). The most similar effort is a project underway in Israel, funded and supported by Super-Pharm, the largest and leading drugstore chain in Israel, to provide online screening for eating disorders and access to an evidence-based online intervention, with the screen being completed by over 34,000 individuals over the course of just five weeks (S. Sadeh-Sharvit, January 14, 2019). Advertising efforts for this initiative were supported by Saatchi & Saatchi, a global communications and advertising agency network, and Keshet Media Group, Israel’s leading TV channel and digital content platform. The campaign included national television spots and key social media opinion leaders.
We note that there is one other related effort underway in Australia—The Reach out and Recovery (ROAR) website provides access to online screening for those who think they have eating disorder symptoms and then generates a report that can be taken to the individual’s general practitioner (McLean, Caldwell, & Robertson, 2019). Over the course of 16 months, the site was accessed by nearly 2,400 individuals (McLean et al., 2019). In the current study, we reported on reach of the NEDA online screen to adults over the course of 6 months, probable eating disorder diagnoses and risk status, and self-reported treatment receipt. Results highlight a number of key findings.
First, we screened over 71,000 adults for an eating disorder in just six months, and screen respondents were located in many parts of the U.S. We note that 23.1% of those screens were completed during NEDAwareness Week, highlighting the benefit of harnessing national public awareness campaigns to disseminate a screening tool and increase detection of eating disorders. During weeks outside of NEDAwareness Week, 2,112 respondents completed the screen each week on average. As can be seen in Figure 1, aside from NEDAwareness week, there were other weeks when screen completion was elevated. It is possible that screen completion may have been elevated during these weeks due to media coverage by celebrities about eating disorders (i.e., 4/9/17-4/15-17 = Nancy Kerrigan talks about eating disorders (Gomez, 2017); 6/4/17-6/10/17 = Trojan Bellisario interview about eating disorders (Adams, 2017); 7/30/17-8/5/17 = Popsugar streams Trojan Bellisario interview (Johnson, 2017)). Indeed, research has indicated that mental health-related media can elevate awareness of mental health concerns (Ayers, Althouse, Leas, Dredze, & Allem, 2017). It is also notable that the majority of the sample was female, young, non-Hispanic, and White. Given research indicating that eating disorders do not discriminate and that they affect individuals of all genders, ages, races, and ethnicities (Schaumberg et al., 2017), it is likely that the demographic characteristics of the current sample are a reflection of the sampling strategy utilized rather than a true reflection of the demographic characteristics of individuals with eating disorders in the U.S. Instead, it may be that stereotypes about eating disorders impact disorder recognition and who chooses to take the screen (e.g., Grillot & Keel, 2018; Räisänen & Hunt, 2014). In the future, screening initiatives, such as those reported in the current study, might be paired with campaigns dedicated toward improving awareness of the occurrence and adverse impact of eating disorder behaviors among individuals from marginalized demographic sectors (e.g., Mitchison, Hay, Slewa-Younan, & Mond, 2014) to encourage greater participation in screening by such individuals. This is particularly crucial given the lack of provider recognition of eating disorders in such subgroups (e.g., Currin, Schmidt, & Waller, 2007; Marques et al., 2011).
Second, we demonstrated that eating disorder pathology was high amongst screen respondents, with 86.3% screening positive for a possible clinical or subclinical eating disorder, and only 3.4% screening as not at risk for an eating disorder. Epidemiological data from the U.S. have demonstrated lifetime prevalence of 0.6% for AN, 1.0% for BN, 2.8% for BED, and 1.2% for subthreshold BED (Hudson et al., 2007). Screen respondents in the current study self-selected to complete the online screening tool, which likely explains the much greater level of eating disorder pathology in this sample. In our work implementing an online platform for eating disorders screening and intervention across public universities in the state of Missouri in the U.S. (Fitzsimmons-Craft et al., 2018) and as part of a randomized controlled trial in 28 geographically diverse U.S. universities (Fitzsimmons-Craft et al., 2019), we similarly demonstrated a high level of eating disorder risk in those who chose to participate in the online screen. This is a key finding as it suggests the current screen attracts respondents with elevated eating disorder pathology and thus, when disseminated widely, has the capability of increasing detection and access to care for individuals at risk for or with eating disorders. Indeed, in just 6 months, we identified 55,367 respondents who screened positive for an clinical or subclinical eating disorder and who were not in treatment, highlighting the promise of this approach for increasing problem recognition and access to care.
Third, findings highlight demographic and anthropometric differences across eating disorder diagnostic and risk groups. Consistent with past research, self-reported BMI was highest among those screening positive for BED and sub-BED, and was lowest for those screening positive for AN (Duncan, Ziobrowski, & Nicol, 2017). On average, those classified as having BED/sub-BED reported BMIs indicative of having obesity (i.e., BMI > 30). Those classified as screening positive for the more traditional eating disorder diagnostic categories (i.e., AN, BN, BED, sub-BN, sub-BED) were also more likely to report being female than those screening positive for other eating disorders (i.e., UFED or AFRID) or screened as not having an ED. Notably, those who screened positive for AN were younger and those who screened positive for BED/sub-BED were older than any of the other diagnostic/risk categories, which is not surprising given differences in the average age of onset across the ED spectrum (Hudson et al., 2007). Differences in household income and partnership status also reflect this trend.
Finally, we found that rates of treatment receipt were extremely low. Amongst respondents screening positive for a clinical/subclinical eating disorder, 85.9% had not received any treatment, and only 3.0% were currently in treatment. These results are in line with other published work suggesting a wide treatment gap for individuals with eating disorders (Eisenberg et al., 2011; Hudson et al., 2007; Kazdin et al., 2017). The undertreatment of BED in particular is also notable, suggesting that, in line with other work, individuals with BED may be even less likely to be identified by providers or to themselves recognize their symptoms as something in need of treatment compared to individuals with other eating disorders (Reas, 2017).
Strengths of this study include our partnership with the leading non-profit organization for eating disorders in the U.S. to disseminate a validated online screen for eating disorders, resulting in screen completion by over 71,000 adult respondents over the course of just 6 months. However, findings should be interpreted in the context of limitations. Most notably, the online screening tool was not implemented as a population-based screen. Thus, results should not be understood to be representative of the eating disorder pathology of the U.S. population as a whole. While the current study presents data from the largest known eating disorders screening initiative outside of surveillance research, only a small subset of the U.S. population was screened. We note that other work highlights the considerable challenges of reaching people, even with digital approaches (e.g., DeBar et al., 2009; Lindenberg, Moessner, Harney, McLaughlin, & Bauer, 2011). Indeed, in our team’s work disseminating online screening and offering online interventions for eating disorders in U.S. universities (Fitzsimmons-Craft et al., 2018, 2019), we have found than an average of 1.9-2.5% of undergraduate students take the online screen, even when using considerable recruitment efforts. Notably, our intention with the current effort was not necessarily to reach the entire U.S. population and the recruitment efforts utilized prioritized reaching those with elevated eating disorder symptomatology. Screen results are suggestive of the eating disorder risk level of adults who voluntarily elected to complete an online eating disorder screen. Additionally, screening results are based solely on an online self-report questionnaire rather than diagnostic interviews and there was no assessment of the clinical significance of the putative “disorders,” although research has indicated that the SWED has acceptable sensitivity and specificity for identifying most eating disorder diagnoses for college women (Graham et al., 2018). Future work will need to specifically validate this tool in college men. Furthermore, the failure to assess whether individuals who screened positive for an eating disorder believed they might currently have an eating disorder and to more thoroughly assess help-seeking behavior (e.g., type of treatment accessed) might also be considered limitations. Future screening initiatives should consider adding questions about these issues.
In conclusion, nationally-disseminated online screening may represent an important eating disorder detection strategy, as the majority of respondents who self-selected to complete the tool screened positive for a clinical/subclinical eating disorder. The extremely high percentage of individuals screening positive for an eating disorder who reported not being in treatment suggests a wide treatment gap and the need to directly link screening with accessible, affordable, evidence-based intervention options.
Supplementary Material
Acknowledgments
This research was supported by R01 MH100455, T32 HL007456, T32 HL130357, K01 DK116925, and F32 HD089586 from the National Institutes of Health.
References
- About NEDAwareness Week. (2018). Retrieved from https://www.nationaleatingdisorders.org/sites/default/files/Partner%20Packet%202018_FINAL.pdf.
- About Us. (2018). Retrieved from https://www.nationaleatingdisorders.org/about-us/our-work
- Adams C (2017, May 31). Troian Bellisario on how eating disorder inspired new film feed: ‘It was like poking a sleeping dragon’. People . Retrieved from https://people.com/tv/troian-bellisario-eating-disorder-new-film-feed/. [Google Scholar]
- Arcelus J, Mitchell AJ, Wales J, & Nielsen S (2011). Mortality rates in patients with anorexia nervosa and other eating disorders: a meta-analysis of 36 studies. Archives of General Psychiatry, 68, 724–731. doi: 10.1001/archgenpsychiatry.2011.74 [DOI] [PubMed] [Google Scholar]
- Ayers JW, Althouse BM, Leas EC, Dredze M, & Allem JP (2017). Internet searches for suicide following the release of 13 Reasons Why. JAMA Internal Medicine, 177, 1527–1529. doi: 10.1001/jamainternmed.2017.3333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker AE, Franko DL, Speck A, & Herzog DB (2003). Ethnicity and differential access to care for eating disorder symptoms. International Journal of Eating Disorders, 33, 205–212. doi: 10.1002/eat.10129 [DOI] [PubMed] [Google Scholar]
- Cachelin FM, & Striegel-Moore RH (2006). Help seeking and barriers to treatment in a community sample of Mexican American and European American women with eating disorders. International Journal of Eating Disorders, 39, 154–161. doi: 10.1002/eat.20213 [DOI] [PubMed] [Google Scholar]
- Currin L, Schmidt U, & Waller G (2007). Variables that influence diagnosis and treatment of the eating disorders within primary care settings: a vignette study. International Journal of Eating Disorders, 40, 257–262. doi: 10.1002/eat.20355 [DOI] [PubMed] [Google Scholar]
- DeBar LL, Yarborough BJ, Striegel-Moore RH, Rosselli F, Perrin N, Wilson GT, … & Lynch F (2009). Recruitment for a guided self-help binge eating trial: potential lessons for implementing programs in everyday practice settings. Contemporary Clinical Trials, 30, 326–333. doi: 10.1016/j.cct.2009.02.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duncan AE, Ziobrowski HN, & Nicol G (2017). The prevalence of past 12-month and lifetime DSM-IV eating disorders by BMI category in US men and women. European Eating Disorders Review , 25, 165–171. doi: 10.1002/erv.2503 [DOI] [PubMed] [Google Scholar]
- Eisenberg D, Nicklett EJ, Roeder K, & Kirz NE (2011). Eating disorder symptoms among college students: Prevalence, persistence, correlates, and treatment-seeking. Journal of American College Health, 59, 700–707. doi: 10.1080/07448481.2010.546461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairburn CG, & Beglin SJ (1994). Assessment of eating disorders: Interview or self-report questionnaire?. International Journal of Eating Disorders, 16, 363–370. [PubMed] [Google Scholar]
- Fitzsimmons-Craft EE, Balantekin KN, Eichen DM, Graham AK, Monterubio GE, Sadeh-Sharvit S, … Wilfley DE (2019). Screening and offering online programs for eating disorders: Reach, pathology, differences across risk groups, and program uptake at 28 U.S. universities. Manuscript submitted for publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fitzsimmons-Craft EE, Firebaugh M, Graham AK, Eichen DM, Monterubio GE, Balantekin KN,…Wilfley DE (2018). State-wide university implementation of an onine platform for eating disorders screening and intervention. Advance online publication. doi: 10.1037/ser0000264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forney KJ, Buchman-Schmitt JM, Keel PK, & Frank GK (2016). The medical complications associated with purging. International Journal of Eating Disorders, 49, 249–259. doi: 10.1002/eat.22504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gomez P (2017, April 12). Nancy Kerrigan developed eating disorder to cope with stress of 1994 attack: ‘I was wasting away’. People . Retrieved from https://people.com/celebrity/nancy-kerrigan-anorexia-stress-1994-attack-exclusive/. [Google Scholar]
- Graham AK, Trockel M, Weisman H, Fitzsimmons-Craft EE, Balantekin KN, Wilfley DE & Taylor CB (2018). A screening tool for detecting eating disorder risk and diagnostic symptoms among college-age women. Journal of American College Health. Manuscript in press. doi: 10.1080/07448481.2018.1483936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gratwick-Sarll K, Mond J, & Hay P (2013). Self-recognition of eating-disordered behavior in college women: Further evidence of poor eating disorders “mental health literacy”?. Eating Disorders, 21, 310–327. doi: 10.1080/10640266.2013.797321 [DOI] [PubMed] [Google Scholar]
- Grillot CL, & Keel PK (2018). Barriers to seeking treatment for eating disorders: The role of self-recognition in understanding gender disparities in who seeks help. International Journal of Eating Disorders. Advance online publication. doi: 10.1002/eat.22965 [DOI] [PubMed] [Google Scholar]
- Hoek HW (2016). Review of the worldwide epidemiology of eating disorders. Current Opinion in Psychiatry, 29, 336–339. doi: 10.1097/YCO.0000000000000282 [DOI] [PubMed] [Google Scholar]
- Hudson JI, Hiripi E, Pope HG, & Kessler RC (2007). The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biological Psychiatry, 61, 348–358. doi: 10.1016/j.biopsych.2006.03.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson K (2017, August 4). Troian Bellisario on how her eating disorder is like sobriety: “This is a journey”. Popsugar. Retrieved from https://www.popsugar.com/beauty/Troian-Bellisario-Feed-Video-Interview-43827761. [Google Scholar]
- Kass AE, Balantekin KN, Fitzsimmons-Craft EE, Jacobi C, Wilfley DE, & Taylor CB (2017). The economic case for digital interventions for eating disorders among United States college students. International Journal of Eating Disorders , 50, 250–258. doi: 10.1002/eat.22680 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kazdin AE, Fitzsimmons-Craft EE, & Wilfley DE (2017). Addressing critical gaps in the treatment of eating disorders. International Journal of Eating Disorders, 50, 170–189. doi: 10.1002/eat.22670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Killen JD, Taylor CB, Hayward C, Wilson DM, Haydel KF, Hammer LD, … & Kraemer H (1994). Pursuit of thinness and onset of eating disorder symptoms in a community sample of adolescent girls: A three-year prospective analysis. International Journal of Eating Disorders, 16, 227–238. doi: [DOI] [PubMed] [Google Scholar]
- Klump KL, Bulik CM, Kaye WH, Treasure J, & Tyson E (2009). Academy for eating disorders position paper: eating disorders are serious mental illnesses. International Journal of Eating Disorders , 42, 97–103. doi: 10.1002/eat.20589 [DOI] [PubMed] [Google Scholar]
- Lindenberg K, Moessner M, Harney J, McLaughlin O, & Bauer S (2011). E-health for individualized prevention of eating disorders. Clinical Practice & Epidemiology in Mental Health , 7, 74–83. doi: 10.2174/1745017901107010074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marques L, Alegria M, Becker AE, Chen CN, Fang A, Chosak A, & Diniz JB (2011). Comparative prevalence, correlates of impairment, and service utilization for eating disorders across US ethnic groups: Implications for reducing ethnic disparities in health care access for eating disorders. International Journal of Eating Disorders, 44, 412–420. doi: 10.1002/eat.20787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell JE (2016). Medical comorbidity and medical complications associated with binge-eating disorder. International Journal of Eating Disorders, 49, 319–323. doi: 10.1002/eat.22452 [DOI] [PubMed] [Google Scholar]
- Mitchison D, Hay P, Slewa-Younan S, & Mond J (2014). The changing demographic profile of eating disorder behaviors in the community. BMC Public Health, 14, 943. doi: 10.1186/1471-2458-14-943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mond JM (2014). Eating disorders “mental health literacy”: An introduction. Journal of Mental Health , 23, 51–54. doi: 10.3109/09638237.2014.889286 [DOI] [PubMed] [Google Scholar]
- Mond JM (2016). Optimizing prevention programs and maximizing public health impact are not the same thing. Eating Disorders, 24, 20–28. doi: 10.1080/10640266.2015.1113824 [DOI] [PubMed] [Google Scholar]
- Mond J, Hay P, Rodgers B, & Owen C (2006). Self-recognition of disordered eating among women with bulimic-type eating disorders: A community-based study. International Journal of Eating Disorders, 39, 747–753. doi: 10.1002/eat.20306 [DOI] [PubMed] [Google Scholar]
- Norris ML, Harrison ME, Isserlin L, Robinson A, Feder S, & Sampson M (2016). Gastrointestinal complications associated with anorexia nervosa: A systematic review. International Journal of Eating Disorders, 49, 216–237. doi: 10.1002/eat.22462 [DOI] [PubMed] [Google Scholar]
- Räisänen U, & Hunt K (2014). The role of gendered constructions of eating disorders in delayed help-seeking in men: a qualitative interview study. BMJ Open, 4(4), e004342. doi: 10.1136/bmjopen-2013-004342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reas DL (2017). Public and healthcare professionals’ knowledge and attitudes toward binge eating disorder: A narrative review. Nutrients, 9, 1267. doi: 10.3390/nu9111267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sachs KV, Harnke B, Mehler PS, & Krantz MJ (2016). Cardiovascular complications of anorexia nervosa: A systematic review. International Journal of Eating Disorders, 49, 238–248. doi: 10.1002/eat.22481 [DOI] [PubMed] [Google Scholar]
- Schaumberg K, Welch E, Breithaupt L, Hübel C, Baker JH, Munn-Chernoff MA, … & Hardaway AJ (2017). The Science Behind the Academy for Eating Disorders’ Nine Truths About Eating Disorders. European Eating Disorders Review, 25, 432–450. doi: 10.1002/erv.2553 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLean SA, Caldwell B, & Roberton M (2019). Reach Out and Recover: Barriers to help-seeking in individuals seeking support for eating disorders. Manuscript in preparation. [DOI] [PubMed] [Google Scholar]
- Smink FR, Van Hoeken D, & Hoek HW (2012). Epidemiology of eating disorders: incidence, prevalence and mortality rates. Current Psychiatry Reports, 14, 406–414. doi: 10.1007/s11920-012-0282-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Telch CF, & Rizvi SL (2000). Development and validation of the Eating Disorder Diagnostic Scale: a brief self-report measure of anorexia, bulimia, and binge-eating disorder. Psychological Assessment, 12, 123–131. doi: 10.1037/1040-3590.12.2.123 [DOI] [PubMed] [Google Scholar]
- Taylor CB, Ruzek JI, Fitzsimmons-Craft EE, Graham AK, & Balantekin KN (2018). A systematic digital approach to implementation and dissemination of eating disorders interventions to large populations identified through online screening: implications for post-traumatic stress. mHealth, 4: 25. doi: 10.21037/mhealth.2018.05.06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weissman RS, & Rosselli F (2017). Reducing the burden of suffering from eating disorders: Unmet treatment needs, cost of illness, and the quest for cost-effectiveness. Behaviour Research and Therapy, 88, 49–64. doi: 10.1016/j.brat.2016.09.006 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.