Introduction
Adaptive behavior is generally defined as the independent performance of skills required for personal and social sufficiency across daily routines and contexts (Sparrow, Cicchetti, & Saulnier, 2016). In both typically developing populations and in individuals with global developmental delays, adaptive skills are largely commensurate with cognitive abilities (Sparrow & Cicchetti, 1989). However, individuals with autism spectrum disorder (ASD) often exhibit significant delays in their adaptive skills, not only in comparison to their chronological age, but also in comparison to their mental age, suggesting that they do not effectively translate their cognitive abilities into real-life adaptive skills (e.g., Stone, Ousley, Hepburn, Hogan, & Brown, 1999; Volkmar et al., 1987; Volkmar, Carter, Sparrow, & Cicchetti, 1993). Historically, an “autism profile” of adaptive behavior has emerged wherein the largest deficits are observed in functional socialization skills, followed by communication and daily living skills (Carter et al., 1998; Loveland & Kelley, 1991; Volkmar et al., 1987). In some studies, the gap between cognition and adaptive skills has been as large as two to three standard deviations in size, and older school-age individuals tend to have a larger gap than younger children (Kanne et al., 2011; Klin et al., 2007; Saulnier & Klin, 2007).
There is evidence to suggest, however, that the large gap between adaptive skills and cognition is only observed in individuals with ASD who do not have cognitive impairment (Fenton et al., 2003; Kanne et al., 2011; Perry, Flanagan, Dunn Geier, & Freeman, 2009). The study of adaptive behavior in this population of individuals with ASD without intellectual disabilities is a pressing priority given that this part of the spectrum now represents the majority of individuals with ASD (e.g., Baio et al., 2018). Also, adults with ASD without intellectual disabilities often fail to achieve adequate levels of independence in life (Farley et al., 2009; Howlin, Goode, Hutton, & Rutter, 2004; Howlin, Moss, Savage, & Rutter, 2013), with impaired socialization and daily living skills often being the areas most associated with poor outcome (e.g., Howlin et al., 2013). Given the importance of these functional skills for successfully navigating the demands of everyday life, there is a need to probe the emergence of adaptive deficits relative to age and cognitive status in order to develop and deliver targeted early interventions.
Studies focusing on infants and toddlers with ASD have found that deficits in adaptive behavior are already present in the toddler period, and that these delays persist into early childhood (Estes et al., 2015; Paul, Loomis, & Chawarska, 2014; Salomone et al., 2018; Stone et al., 1999; Sutera et al., 2007; Ventola, Saulnier, Steinberg, Chawarska, & Klin, 2014). In some studies of toddlers with ASD, social adaptive skills are reported to be more impaired relative to other adaptive skills, particularly in toddlers with average cognition (Perry et al., 2009; Ventola et al., 2014). Ventola et al. (2014) identified very early items from the socialization domain of the Vineland Adaptive Behavior Scales (Sparrow, Cicchetti, & Balla, 2005) that distinguished toddlers with ASD from those with non-ASD developmental delays; these items corresponded to behaviors normatively acquired in the first year of life, such as joint attention skills and responsivity to caregiver’s voice. However, this study did not evaluate longitudinal trajectories of adaptive socialization skills from infancy, leaving open the question of whether these behaviors were outliers or represented early deficits in adaptive socialization more broadly.
Most recently, Salomone et al. (2018) investigated the stability of cognitive and adaptive skills from infancy through middle childhood. This study found that high-risk children, regardless of diagnostic outcome, had lower cognitive and adaptive skills compared to low-risk children across time points. Moreover, high-risk children fell further behind their low-risk peers in adaptive, but not cognitive, skills between 36–84 months. This finding provides evidence for a widening discrepancy between cognitive and adaptive skills after age 3 for both ASD and non-ASD high-risk children.
Current Study
In order to add to this extant evidence, the current study evaluates the emergence of a discrepancy in adaptive skills on an individual level in infants and toddlers and includes high-risk toddlers determined to have subthreshold features of the disorder (i.e., the “broader autism phenotype”). That is, we aim to identify the proportion of infants and toddlers who have below average adaptive skills in light of average cognitive abilities across low-risk toddlers and three groups of high-risk toddlers at 12, 24, and 36 months of age. The point in time at which adaptive skills begin to fall behind average cognitive skills in early development is unknown, yet could be an early risk marker for ASD, especially in the case of children with ASD who do not develop cognitive impairments. Studies to date involving high-risk infant siblings (children who are at greater risk of developing ASD by virtue of being the younger sibling of a child with ASD; Ozonoff et al., 2011) have reported complex cognitive and adaptive behavior profiles characterizing this unique population, with more cognitively able toddlers with ASD typically receiving a later diagnosis due to their relatively strong early developmental skills (Chawarska et al., 2014). In this context, identification of emerging delays in adaptive behavior in light of average cognitive skills in the first three years of life may lead to earlier and more robust diagnosis of this group, which in turn might promote greater access to, and more specific, early intervention. Eligibility criteria for early intervention programs that focus solely on discrete language and/or cognitive skills in lieu of adaptive use of these skills throughout everyday life may result in under-identification of children who can greatly benefit from early intervention, thus pre-empting or at least reducing the impairing lag in adaptive skills that are very likely to reduce their capacity for independence later in life.
To shed light on these important issues, this study compares trajectories of adaptive and cognitive skills from 12 to 36 months of age across four groups of toddlers: high-risk toddlers with ASD, high-risk toddlers with subthreshold autism symptomatology hereon referred to as the broader autism phenotype (BAP; Ozonoff et al., 2014), unaffected high-risk toddlers with no clinical features (UA), and low-risk typically developing toddlers (TD). We aim to 1) identify when in the first three years of development adaptive skills in toddlers with or at risk for ASD begin to fall behind those of their peers and 2) compare the proportion of toddlers with average cognitive abilities who show below average adaptive skills across groups at 12, 24, and 36 months. We hypothesize that, consistent with previous literature (e.g., Charman et al., 2017; Salomone et al., 2018), toddlers with ASD and BAP will have lower adaptive skills than UA and TD toddlers, differences will be most robust in the socialization subdomain, and the divergence will begin as early as 12 months. Moreover, we hypothesize that that an increasing proportion of toddlers with ASD and average cognition will have below average adaptive socialization skills from 12 to 36 months.
Methods
Participants
Participants included 69 high-risk siblings of children with ASD and 96 low-risk toddlers from two different sites conducting longitudinal research of ASD in infancy (both sites were NIMH Autism Centers of Excellence, PI: A. Klin). Toddlers were considered to be at high risk for ASD if they had a full biological sibling diagnosed with ASD by a licensed psychologist or medical doctor. Diagnoses of older siblings were confirmed by clinical review of the most recent diagnostic evaluation report and current scores within the ASD range on the Social Responsiveness Scale (SRS; Constantino, 2012) and the Social Communication Questionnaire (SCQ; Rutter, Bailey, & Lord, 2003). When diagnostic confirmation of the older sibling could not be sufficiently ascertained with these criteria (i.e., when SRS/SCQ scores fell below cut-offs and/or when community-based diagnoses were made in the absence of documented testing), a direct assessment was conducted using the Autism Diagnostic Observation Schedule, First or Second Edition (ADOS; Lord et al., 2000, 2012) by a licensed and research reliable psychologist with expertise in diagnosis of ASD. This process was necessary for N=2 high-risk participants and sibling diagnoses were confirmed. Low-risk toddlers were required to have no familial history of ASD in first, second, or third-degree relatives and were ascertained to exhibit typical development via standardized assessments carried out at their 24-month evaluation. Exclusion criteria for both high-risk and low-risk toddlers included gestational age below 34 weeks, major hearing and/or visual impairment, non-febrile seizure disorder, known genetic syndrome, and significant pre-or perinatal complications. Only participants who were seen at the diagnostic outcome visit (36 months for high-risk toddlers and 24 months for low-risk toddlers) were included in this study. Additionally, only high-risk participants who were given a clinical best estimate diagnosis (CBE) of ASD, BAP, or unaffected (i.e., typical development) were included – procedures for determining CBE are described below. In both sites, families were recruited through local pediatric practices, hospitals, OB/GY offices, radio and media ads, and state and local autism organizations. Written informed consent approved by each site’s Institutional Review Board was obtained from all participating families prior to any study procedures.
Procedures
The data reported here are part of a large longitudinal study in which toddlers were evaluated at 12 months, 24 months, and 36 months of age. At the 12- and 24-month visits, toddlers were administered the two standardized assessments that are the focus of the current study: Mullen Scales of Early Learning (Mullen; Mullen, 1995) and Vineland Adaptive Behavior Scales, Second Edition (Vineland; Sparrow, Cicchetti, & Balla, 2005). A full diagnostic evaluation was administered by a licensed psychologist and a licensed speech-language pathologist at 36 months for high-risk toddlers. Because low-risk toddlers were only seen at 12 and 24 months, their full diagnostic evaluation was administered at 24 months. The full diagnostic evaluations included a developmental assessment (Mullen), communication and language assessment (Communication and Symbolic Behavior Scales, Wetherby & Prizant, 2002, at 24 months and Preschool Language Scales, Zimmerman, Steiner, & Pond, 2002, at 36 months), adaptive skill assessment (Vineland), and diagnostic observation (ADOS). Demographic and clinical characteristics of this sample at the diagnostic outcome assessment are presented in Table 1 and include: verbal developmental quotient (VDQ) derived from the expressive and receptive language domains of the Mullen and the ADOS calibrated severity score (CSS). Use of the ADOS CSS allows for standardized comparison of autism symptom severity across individuals of different developmental levels (Gotham, Pickles, & Lord, 2009).
Table 1.
Participant Characteristics by Diagnostic Group
| Characteristic | ASD N=21 | BAP N=19 | UA N=29 | TD N=96 | P-Value |
|---|---|---|---|---|---|
| Sex – Male | 15 (71.4%) | 15 (79%) | 18 (62.1%) | 51 (53.1%) | .115 |
| Race | |||||
| White | 16 (76.2%) | 17 (89.5%) | 25 (86.2%) | 91 (94.8%) | .080 |
| Black | 2 (9.5%) | 0 (0%) | 1 (3.5%) | 1 (1%) | |
| Asian | 1 (4.8%) | 1 (5.3%) | 1 (3.5%) | 3 (3.1%) | |
| Multiracial | 2 (9.5%) | 1 (5.3%) | 2 (6.9%) | 1 (1%) | |
| Ethnicity - Hispanic | 2 (9.5%) | 2 (10.5%) | 2 (6.9%) | 7 (7.3%) | .878 |
| Maternal Education | |||||
| High School or Less | 0 (0%) | 0 (0%) | 1 (3.5%) | 3 (3.1%) | .890 |
| Some College or Vocational | 1 (4.8%) | 1 (5.3%) | 2 (6.9%) | 11 (11.5%) | |
| College Degree | 8 (38.1%) | 7 (36.8%) | 6 (20.7%) | 31 (32.3%) | |
| Post College Degree | 12 (57.1%) | 11 (57.9%) | 20 (69%) | 51 (53.1%) | |
| Age at Each Visit | |||||
| 12-Month Visita | 12.24 ± 0.54 | 11.68 ± 0.48 | 11.69 ± 0.47 | 11.99 ± 0.59 | .001 |
| 24-Month Visitb | 24.15 ± 0.67 | 23.79 ± 1.27 | 23.59 ± 0.63 | 24.22 ± 0.93 | .002 |
| 36-Month Visitc | 36.76 ± 0.77 | 38.16 ± 2.83 | 37.31 ± 2.66 | - | .140 |
| Characterization at 36-Month Outcome (N=69)c | |||||
| Verbal DQd | 94.82 ± 20.65 | 102.28 ± 13.52 | 114.25 ± 12.96 | - | <.001 |
| ADOS Calibrated Severity Scoree | 6.19 ± 2.27 | 2.84 ± 1.61 | 2.07 ± 1.19 | - | <.001 |
Note. Outcome characterization data is presented as raw, unadjusted means. Verbal DQ (mean of 100, standard deviation of 15) was derived from the Mullen Scales of Early Learning, receptive and expressive language domains.
ASD = Autism Spectrum Disorder; BAP = Broader Autism Phenotype; UA = Unaffected; TD = Typically Developing; DQ = Developmental Quotient; ADOS = Autism Diagnostic Observation Schedule (Lord et al., 2000, 2012). CSS = calibrated severity score derived from ADOS.
ASD > BAP, UA, TD; TD > BAP, UA.
ASD > UA; TD > UA.
TD participants were not seen at 36 months.
ASD, BAP < UA.
ASD > BAP, UA
Clinicians who administered the ADOS and Mullen were masked to the risk status of participants. Rather than using strict cut-off scores from the ADOS and/or Mullen for defining our diagnostic outcome groups, diagnosis was determined at the final outcome visit using clinical best estimate (CBE) based on DSM-IV (prior to 2013; American Psychiatric Association, 2000) or DSM-5 (2013 and later; American Psychiatric Association, 2013) criteria. CBE diagnoses were generated via consensus between licensed psychologists and speech-language pathologists using all available information, including assessment scores, behavioral observations, and history of developmental and other concerns provided by parents or caregivers. In line with previous infant longitudinal studies (e.g., Jones & Klin, 2013), a CBE diagnosis of BAP was given to participants who did not meet DSM criteria for ASD, global developmental delay, or language delay, but who still exhibited atypical, subthreshold features associated with ASD that were lower in frequency and/or intensity than the diagnostic threshold for ASD regardless of developmental/language level, based on expert clinical judgement (Ozonoff et al., 2014). As noted, only low-risk toddlers confirmed to be typically developing (TD) at the 24-month visit were included (TD; N=96). High-risk toddlers were included if they were given a CBE of ASD (N=21), broader autism phenotype (BAP; N=19), or no clinical features and thus unaffected (UA; N=29). Five high-risk participants were excluded due to a CBE of global developmental delay without ASD features and six low-risk participants were excluded due to a CBE of language delay (N=5) or anxiety (N=1) at 24 months. Due to the low sample size of toddlers diagnosed with non-ASD developmental delays, these toddlers were not analyzed.
Measures
Adaptive Behavior.
The Vineland Adaptive Behavior Scales, Second Edition (Sparrow, Cicchetti, & Balla, 2005) is a semi-structured caregiver interview that assesses the child’s everyday adaptive functioning. It contains four broad domains: socialization, communication, daily living skills, and motor skills. In the current study, we focused only on adaptive communication, daily living skills, and socialization given that adaptive motor skills have not been studied in older samples given the norm cut-offs and therefore any associations between discrepancies and outcome are less known. Deficits in these skills have historically been the most pronounced in individuals with ASD. Standard scores have a mean of 100 and a standard deviation of 15. Standard scores should remain relatively stable over time if the child’s gains in adaptive skills are commensurate with his or her chronological age. Moreover, one of the main tenants of adaptive behavior is that skills are expected to be adequate; that is, even if an individual has above average or even superior cognition, their adaptive skills should remain solidly within the average range (Sparrow, Cicchetti, & Saulnier, 2016).
Cognitive Development.
The Mullen Scales of Early Learning (Mullen, 1995) is a standardized developmental measure designed for children from birth to 68 months. It provides t-scores and age equivalences for five domains of development: visual reception, gross motor, fine motor, receptive language, and expressive language. Nonverbal developmental quotient (NVDQ) was used in this study as a proxy for cognitive abilities. NVDQ is calculated individually by dividing age equivalences obtained from the visual reception and fine motor domains by the child’s chronological age. This standardization results in scores of 100 for children whose nonverbal skills are commensurate with chronological age, and scores of below 85 for children whose nonverbal skills are below expectations relative to their chronological age.
Statistical Methods
Outcome demographic and clinical characteristics of the study sample were examined by diagnostic group (ASD, BAP, UA, TD) using means and standard deviations for continuous variables, and frequencies and percentages for categorical variables. Statistical differences across outcome groups were determined using one-way analysis of variance (ANOVA) and Chi-square tests of independence for continuous and categorical variables, respectively. When overall statistical significance was ascertained, post hoc pairwise comparisons were executed.
To explore longitudinal trends in cognitive ability (NVDQ) and adaptive skills, within and between diagnostic groups, general linear mixed effects regression was employed. For each regression model, the fixed effects were diagnosis group (4 levels), participant age (continuous), and their interaction. The interaction was included to test for differences in diagnostic group trajectories over participant follow-up. Random effects were the participant-specific intercepts and slopes for participant age. Model covariance structures were modeled separately for each research site (2 levels) using an unstructured variance-covariance matrix, and denominator degrees of freedom were derived using the Between-Within method. Linear slopes and 95% confidence intervals are reported for NVDQ and Vineland standard scores, as appropriate. Model-based, linear trend estimates at 12, 24, and 36 months were further calculated for each measure and compared within and between diagnostic groups. Significance between group slopes and individual trend line estimates (at 12, 24, and 36 months) were calculated using age by diagnosis two-way interaction p-values and post hoc tests.
In order to evaluate clinically relevant discrepancies between cognition and adaptive behavior, each participant was determined to have a discrepancy at each time point if their NVDQ was at least average (≥85) and their Vineland subdomain score was below average (<85). Defining a clinically relevant discrepancy in this way helped to determine gaps between cognition and adaptive behavior that would be clinically meaningful, especially for individuals with high nonverbal cognition. Within these analyses, the percent of participants with average cognition and below average adaptive behavior within each diagnostic group was calculated at each time point and evaluated for significance using Chi-square tests of independence or Fisher’s exact tests, as appropriate (Supplemental Tables 1–2). Results indicated the largest discrepancies existed between combined ASD/BAP versus UA/TD participants. In an effort to increase statistical power and interpretability of findings, especially given the phenotypic similarity of the resultant groups, percentages, odds ratios and 95% confidence intervals were calculated between the ASD/BAP and UA/TD cohorts with regard to clinically relevant discrepancies.
All analyses were performed in SAS v.9.4 (Cary, NC), and statistical significance was evaluated at the 0.05 significance level. Due to the exploratory nature of this analysis, no p-value adjustments were made.
Results
Participant characteristics by diagnostic group are presented in Table 1. Groups did not differ on demographic variables of sex, race, ethnicity, or maternal education. A total of six participants had missed one visit prior to their outcome visit (ASD N=1; BAP N=1; UA N=0; TD N=4). There was a significant difference across diagnostic groups for participant age at the 12- and 24-month visits with the largest average difference being about 2 weeks. Participants were seen within 3–4 weeks of the target age, resulting in very low variability at each time point. At the 36-month outcome visit, VDQ was significantly higher for UA participants than ASD and BAP participants, although group means for all three diagnostic groups were within the average range. As expected, ADOS calibrated severity scores at 36 months were significantly greater for the ASD group compared to the BAP and UA groups.
Trajectories of Cognitive Skills from 12 to 36 Months
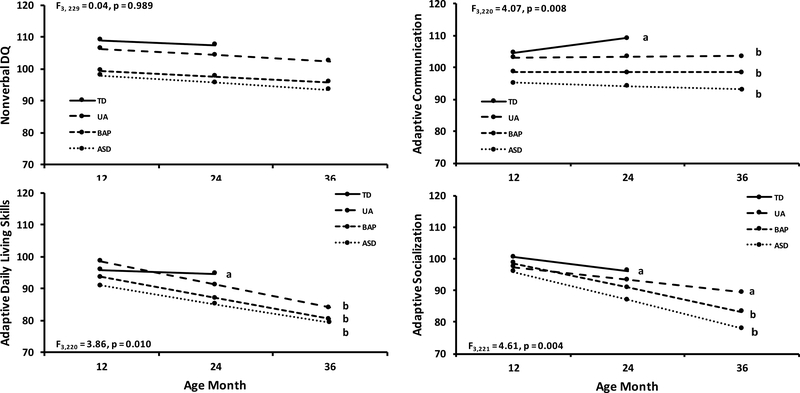
Trajectories of nonverbal cognitive skills (NVDQ) from 12 to 36 months (12 to 24 months for low-risk toddlers) are presented in Figure 1 and corresponding model based estimates are presented in Table 2. NVDQs were in the average to above average range (>85) for all groups across all time points, however the ASD group exhibited a significantly lower NVDQ than the UA and TD groups at each time point (all p < 0.05), see Table 2. Cognitive skills did not differ between ASD and BAP toddlers or between UA and TD toddlers at any time points.
Figure 1.
Model-estimated group trajectories of nonverbal cognitive skills and adaptive skills from 12 to 36 months for all diagnostic groups. Adaptive standard scores derived from the Vineland Adaptive Behavior Scales. Nonverbal DQ standard scores derived from the Mullen Scales of Early Learning, visual reception and fine motor domain. All standard scores have a mean of 100 and standard deviation of 15. Trajectories of adaptive communication and adaptive daily living skills for TDa are significantly different than those of UAb, BAPb, and ASDb. Trajectories of adaptive socialization for TDa and UAa are significantly different from trajectories of ASDb and BAPb. Estimates and p-values are presented in Table 2.
Table 2.
Nonverbal DQ and Adaptive Skills Model-Based Estimates and Regression Slopes
| Visit, Estimate (95% CI) | ASD | BAP | UA | TDa | Between-Group Comparison P-Values |
|---|---|---|---|---|---|
| Nonverbal DQ | |||||
| 12 Months | 97.9 (92.7, 103.2) | 99.4 (94.0, 104.7) | 106.4 (102.1, 110.7) | 108.9 (106.3, 111.6) | ASD < UA*; ASD < TD***; BAP < UA*; BAP < TD** |
| 24 Months | 95.7 (91.5, 99.9) | 97.6 (93.1, 102.1) | 104.4 (100.8, 108.0) | 107.5 (104.7, 110.3) | ASD < UA**; ASD < TD***; BAP < UA*; BAP < TD*** |
| 36 Months | 93.5 (87.6, 99.3) | 95.8 (89.8, 101.9) | 102.4 (97.5, 107.3) | - | ASD < UA* |
| Regression Slope | −2.2 (−5.8, 1.4) | −1.8 (−5.2, 1.7) | −2.0 (−4.9, 1.0) | −1.4 (−4.8, 2.0) | NS |
| Communication | |||||
| 12 Months | 95.3 (91.3, 99.2) | 98.6 (94.8, 102.5) | 103.2 (100.0, 106.5) | 104.7 (102.7, 106.8) | ASD < UA**; ASD < TD***; BAP < TD** |
| 24 Months | 94.2 (91.3, 97.1) | 98.6 (95.4, 101.7) | 103.4 (101.0, 105.9) | 109.3 (107.3, 111.3) | All pairwise comparisons, p < 0.05 |
| 36 Months | 93.2 (89.2, 97.1) | 98.5 (94.2, 102.9) | 103.6 (100.4, 106.8) | - | ASD < UA*** |
| Regression Slope | −1.1 (−3.7, 1.6) | −0.04 (−2.6, 2.6) | 0.2 (−1.9, 2.4) | 4.6 (2.2, 7.0)*** | ASD < TD**; BAP < TD*; UA < TD** |
| Daily Living Skills | |||||
| 12 Months | 90.9 (87.0, 94.8) | 93.7 (90.0, 97.4) | 98.5 (95.4, 101.7) | 95.9 (93.7, 98.0) | ASD < UA**; ASD < TD* |
| 24 Months | 85.1 (82.7, 87.6) | 87.1 (84.4, 89.7) | 91.3 (89.3, 93.3) | 94.7 (92.9, 96.6) | ASD < UA***; ASD < TD***; BAP < UA*; BAP < TD***; UA < TD* |
| 36 Months | 79.4 (75.0, 83.7) | 80.5 (76.2, 84.8) | 84.0 (80.4, 87.6) | - | NS |
| Regression Slope | −5.8 (−9.1, −2.4)*** | −6.6 (−9.6, −3.6)*** | −7.3 (−10.0, −4.6)*** | −1.1 (−4.0, 1.7) | ASD < TD*; BAP < TD**; UA < TD** |
| Socialization | |||||
| 12 Months | 95.9 (93.2, 98.7) | 98.6 (95.9, 101.3) | 97.4 (95.1, 99.7) | 100.5 (99.1, 102.0) | ASD < TD**; UA < TD* |
| 24 Months | 86.9 (85.0, 88.9) | 90.9 (88.9, 92.8) | 93.4 (91.8, 95.0) | 96.2 (94.7, 97.6) | All pairwise comparisons, p < 0.05 |
| 36 Months | 77.9 (74.4, 81.5) | 83.2 (79.8, 86.5) | 89.4 (86.5, 92.4) | - | ASD < BAP*; ASD < UA***; BAP < UA** |
| Regression Slope | −9.0 (−11.5, −6.5)*** | −7.7 (−10.1, −5.4)*** | −4.0 (−6.1, −1.9)*** | −4.3 (−6.4, −2.3)*** | ASD < UA**; ASD < TD**; BAP < UA*; BAP < TD* |
p <.05
p <.01
p <.001
TD participants not seen at 36 months.
Regression slopes for all groups did not reach statistical significance, and therefore did not exhibit change over time (i.e., remained stable) from 12 to 24 or 36 months (all p > 0.1). Cognitive trajectories were similar between groups and were not statistically different, see Table 2.
Trajectories of Adaptive Skills from 12 to 36 Months
Trajectories of adaptive skills (communication, daily living skills, and socialization) from 12 to 36 months are presented in Figure 1 and model based estimates are presented in Table 2. Adaptive communication skills remained within the average range and were stable from 12–36 months for all high-risk toddlers. TD toddlers showed a significant increase from 12–24 months and their trajectory was significantly different from those of the UA (p =.008), BAP (p =.011), and ASD (p =.002) toddlers (see Table 2). ASD toddlers scored significantly lower than UA and TD toddlers at all time points and significantly lower than BAP toddlers only at the 24 month time point. ASD and BAP toddlers did not differ at 12 or 36 months. Despite these significant differences, mean scores for all groups at all time points were within the average range.
Daily living skills declined significantly between 12–36 months for all high-risk toddlers, but TD toddlers remained stable between 12 and 24 months. Thus, trajectories for all high-risk toddlers were not significantly different from each other, but were significantly different than the TD group (ASD: p =.036, BAP: p =.009, UA: p =.002). Toddlers with ASD scored an average of 5.76 points lower per year from 12 to 36 months and toddlers with BAP scored an average of 6.6 points lower per year from 12 to 36 months. By 36 months, both ASD and BAP toddlers were scoring in the below average range. UA toddlers also decreased an average of 7.32 points per year from 12 to 36 months and scored significantly lower than TD toddlers at 24 months. ASD toddlers scored significantly lower than UA and TD toddlers at 12 and 24 months. Similar to adaptive communication skills, toddlers with ASD did not differ from toddlers with BAP at any time point.
A significant decline in Vineland socialization standard scores was observed from 12 to 36 months for all groups, but the decline for ASD and BAP toddlers was significantly greater than that of UA (ASD: p =.003, BAP: p =.020) and TD (ASD: p = 0005, BAP: p =.033) toddlers. More specifically, socialization standard scores decreased an average of 9 points each year for ASD toddlers, 7.7 points each year for BAP toddlers, 4 points each year for UA toddlers, and 4.3 points each year for TD toddlers. Trajectories did not differ between ASD and BAP or between UA and TD toddlers. At 12 months, socialization scores for the ASD group were in the average range, but already significantly lower than those of the TD group. At 24 and 36 months, socialization scores for the ASD group were significantly lower than all other groups and fell in the below average range (< 85) by 36 months.
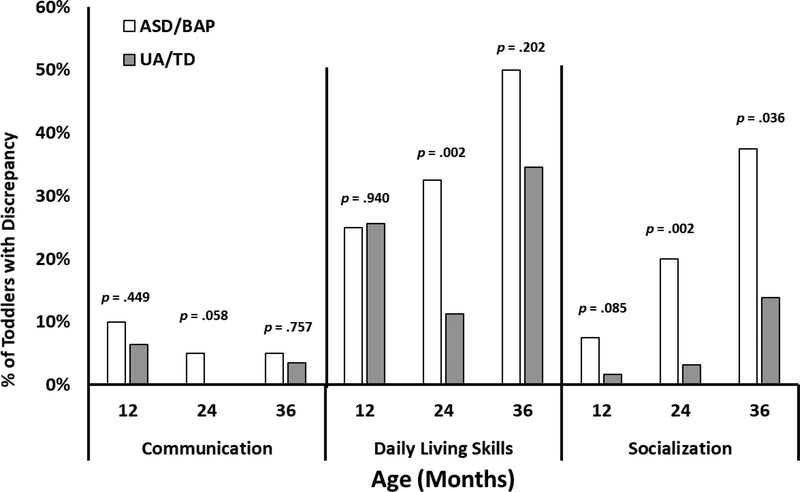
Discrepancy Between Adaptive and Cognitive Skills from 12 to 36 Months
The percent of participants in each group (ASD/BAP and UA/TD) who showed both average cognitive abilities and below average adaptive skills are shown in Figure 2. The magnitude of these discrepancies is shown in Supplemental Figure 1. Examination of adaptive communication skills revealed that very few (≤ 10%) of toddlers with average cognition showed below average adaptive communication skills at each time point and this pattern did not differ between the ASD/BAP and UA/TD groups. The odds of a toddler with ASD/BAP having below average adaptive communication skills compared to their average cognitive abilities, relative to a UA/TD toddler, was not significant at any time point.
Figure 2.
Percent of participants within diagnostic groups showing a discrepancy in each adaptive domain (Communication, Daily Living Skills, Socialization). Discrepancy is defined as average cognition (NVDQ ≥ 85) and below average adaptive skills (<85). p-values calculated from Chi-square tests of independence or Fisher’s exact tests at each time point.
In regard to daily living skills, 25% of ASD/BAP toddlers and 25.6% of TD/UA toddlers with average cognition showed below average daily living skills at 12 months of age. The magnitude of the discrepancy between cognition and daily living scores for ASD/BAP toddlers was 19.0 points (SD = 8.1). This increased to 32.5% (an average difference of 15.3 points, SD = 6.0) at 24 months and 50% (an average difference of 22.8 points, SD = 11.7) at 36 months. These proportions were significantly greater than those of UA/TD toddlers for which 11.2% showed a discrepancy (average difference of 21.0 points, SD= 10.3) at 24 months and 34.5% showed a discrepancy (average difference of 25.1 points, SD = 17.9) at 36 months. The odds of a toddler with ASD features (i.e., ASD or BAP) having below average adaptive daily living skills compared to their average cognitive abilities, relative to a UA/TD toddler, was significant at 24 months (OR = 3.82, 95% CI: (1.61, 9.06); p =.002) and at 36 months (OR = 1.90, 95% CI: (0.71, 5.09); p =.202). That is, by 36 months the odds of a toddler with ASD/BAP and average cognition having below average adaptive daily living skills was 1.9 times (90%) higher than the odds of a UA toddler.
Finally, 8% of the ASD/BAP group with average cognition was exhibiting below average adaptive socialization scores with an average discrepancy of 17.4 points (SD = 5.0) at 12 months. This increased to 20% at 24 months (mean discrepancy of 17.5 points, SD = 12.1) and 38% at 36 months (mean discrepancy of 18.9 points, SD = 9.7). The magnitude of the discrepancy across all visits was, on average, greater than 1 standard deviation (see Supplemental Figure 1 for the distribution). In contrast, only 2% of the UA/TD group with average cognition had below average socialization skills at 12 months, which increased to 3% at 24 months and 14% at 36 month visits. The odds of an ASD/BAP toddler with average cognition having below average adaptive socialization, relative to a UA/TD toddler, was marginally significant at 12 months (OR = 4.99, 95% CI: (0.80, 30.98); p =.085) and significant at 24 months (OR = 7.56, 95% CI: (2.14, 26.71); p =.002) and 36 months (OR = 3.75, 95% CI: (1.09, 12.89); p =.036). That is, by 36 months the odds of an ASD/BAP toddler with average cognition having below average socialization skills was 3.75 times higher than that of a UA toddler.
Discussion
This study investigated trajectories of emerging adaptive and cognitive skills in infants and toddlers later diagnosed with ASD in order to examine whether the pattern often found in older individuals with ASD, where adaptive functioning falls significantly behind cognitive ability, is present early in development, possibly before the diagnosis can be made. Our findings confirm that toddlers later diagnosed with ASD, as well as those with subclinical autism symptomology (BAP), relative to unaffected siblings and typically developing peers, exhibit considerably different trajectories of adaptive skills compared to cognitive skills from 12 to 36 months of age, particularly for adaptive socialization and daily living skills. While toddlers with ASD and BAP made normative gains in cognitive abilities over time, they failed to make comparable gains in everyday socialization and daily living skills. Unaffected high-risk toddlers exhibited a similar pattern of daily living skill acquisition as the ASD and BAP toddlers. This pattern resulted in stable trajectories of nonverbal cognitive standard scores and declining trajectories of adaptive socialization and daily living skills standard scores for ASD and BAP toddlers. Not only are daily living and socialization scores decreasing over time, but the odds of having both average cognitive skills and below average adaptive socialization and daily living skills increased from 12 to 36 months for toddlers with ASD symptomology. This discrepancy was already apparent as early as 12 months for some infants who were later diagnosed with ASD. Interestingly, adaptive communication skills remained stable for all high-risk groups and thus showed very little divergence from nonverbal cognitive skills.
Notably, most toddlers who were diagnosed with ASD and all toddlers in the BAP group had nonverbal cognitive abilities within the average to above average range. This is consistent with previous research on high-risk infant siblings where, relative to clinically-referred samples, they tend to not exhibit significant nonverbal cognitive delays (e.g., Gamliel, Yirmiya, Jaffe, Manor, & Sigman, 2009; Landa & Garrett-Mayer, 2006). There is emerging evidence to suggest that ascertainment biases could account for ASD toddlers having stronger abilities overall compared to, for example, clinically-referred or community based samples by nature of being so closely monitored and evaluated over time (e.g., Sacrey, Zwaigenbaum, Szatmari et al., 2017). It is likely that the high cognitive level of our sample accounts for the stable adaptive communication skills in the current study given that adaptive communication and cognitive abilities are highly correlated (e.g., Kanne et al., 2011) and good receptive and expressive communication skills can facilitate performance on cognitive tasks. Even though adaptive communication skills for high-risk unaffected infants were statistically lower than low-risk TD infants, their scores remained within the average range and stable over time, very similar to their nonverbal cognitive scores. Yet, despite strong cognitive skills for toddlers with ASD and BAP, significant discrepancies – above and beyond what would be expected for their average cognition – were still observed.
It is important to note that the declining adaptive socialization and daily living standard scores do not reflect developmental regression or a loss of skills. These toddlers are in fact making gains in adaptive behavior, but are failing to make the large gains that would be expected given their chronological age. The fact that these cognitively-able toddlers with ASD are not making gains in adaptive behavior in ways commensurate with their stable gains in cognition, confirms that the poor adaptive skills often observed during standardized assessments and naturalistic observation in the first years of life, are also observed and reported by parents. These results add to existing literature, suggesting that parental report of early toddler skills are consistent with clinician observations and predictive of ASD (Macari et al., 2018; Rowberry et al., 2015). Additionally, all high-risk toddlers in the current study showed declining standard scores in adaptive daily living skills and by 36 months even the unaffected high-risk siblings were nearing the below average range. This unexpected finding is in contrast to previous work (Salomone et al., 2018) in which between-group differences in daily living skills were not apparent until age 7 years and suggests that even siblings without ASD features experience challenges in acquiring adaptive daily living skills at a normative rate. While the present study used the survey interview version of the Vineland-II, Salomone et al. (2018) used the parent/caregiver rating form and this difference may explain some of the inconsistent findings between the two studies. Still, further examination of trajectories of daily living skills for toddlers with ASD and ASD features is needed. Our findings of stable adaptive communication skills for all high-risk infants in the first three years of life and impaired socialization skills for those with ASD were consistent with those of Salomone et al. (2018). High-risk unaffected toddlers experienced a decline in socialization scores from 12–36 months, but their scores remained within the average range and the decline was significantly less than that of the toddlers with ASD. This study uniquely contributes to the literature with evidence that a substantial proportion of toddlers with clinical and subclinical levels of ASD features show a discrepancy between cognition and adaptive skills by 36 months of age.
Beginning in the first years of life, infants later diagnosed with ASD experience difficulty translating their repertoire of cognitive skills into functional, independently displayed, adaptive behavior that is critical for navigating the demands of everyday life. Our results suggest that this phenomenon emerges very early in development – in fact, prior to diagnosis – and raises the question of whether this early-emerging gap could be predictive of future challenges, and, if so, whether early intervention could reduce the cumulative impact of this derailment.
Many early intervention programs focus primarily on skill acquisition and school readiness, but may fail to emphasize everyday social and practical adaptive abilities, such as play and interaction with other children, early conversational skills, emotion regulation, and self-care. The very early-emerging delays in the acquisition of adaptive daily living and socialization skills are likely to have cumulative consequences that significantly affect later quality of life and interfere with the potential for independent living. This is of great importance given that adult outcome studies have highlighted adaptive behavior (in particular, functional socialization and daily living skills) as a stronger predictor of good outcome compared to cognition or language alone (e.g., Farley et al., 2009; Howlin, Goode, Hutton, & Rutter, 2004; Howlin, Moss, Savage, & Rutter, 2013). Moreover, greater gaps between cognition and adaptive behavior in adults with ASD have been shown to be associated with comorbid psychopathology (Kraper, Kenworthy, Popal, Martin, & Wallace, 2017).
There were two particularly interesting and surprising findings of this study. First is the declining adaptive socialization scores for the TD group, a finding that has not been reported previously in the literature. This decline was less in magnitude than that of the ASD/BAP groups and scores remained within the average range at all time points, calling to question whether this decline is clinically significant. All participants in this study were administered the Vineland-II, despite the recent release of the Vineland-3 (Sparrow, Cicchetti, & Saulnier, 2016), which is an updated measure with updated norms. The Vineland-II was normed using a cross-sectional study so it is possible that some of the individual variation over time that we observed in the current longitudinal design may not be reflected in the original norms. The use of potentially outdated Vineland-II norms for participants in this study may be a contributing factor to the declining socialization scores for TD participants and a possible limitation to the current study. This issue will benefit from future studies that use the Vineland-3 interview and updated norms. Still, despite the drop in scores at 24 months, TD participant scores remained solidly average.
Second, we were surprised to see the discrepant trajectory of adaptive socialization and daily living skills, relative to cognition, in toddlers displaying subthreshold symptoms ASD – the siblings characterized by a “broader autism phenotype”. This pattern was less pronounced, but not statistically different, than that observed in toddlers diagnosed with ASD. Children given a CBE of BAP do not meet clinical thresholds for ASD, and are, therefore, unlikely to meet eligibility criteria for early intervention services. Given the widening gap between adaptive and cognitive skills evidenced in this group from the age of 12 months, there is a need for research studies to follow these children into later ages, when social adaptive demands increase, in order to adequately examine the extent to which their levels of “non-clinical” symptomatology impact, or not, their eventual outcomes (Messinger et al., 2013). It is possible they will experience significant social challenges after the age of three, making the argument that these children should be eligible for early intervention services in the first years of life.
This study is among few that examine longitudinal profiles of adaptive development prior to diagnosis, but is has several limitations. First, findings for high-risk sibling samples are not immediately generalizable to clinically-referred and community-based samples of children with ASD (Sacrey et al., 2017). For example, these biological siblings who go on to develop ASD may exhibit a qualitatively distinct form of the disorder (Frazier et al., 2015); more research is needed to better understand these differences. Second, our low-risk sample of toddlers ascertained as typically developing were only followed up to 24 months, and not to 36 months as the other groups. Third, it is important to consider the confound that the CBE diagnosis is determined using all available clinical information, including the Mullen and Vineland. However all clinicians determining the CBE were masked to the aims and hypotheses of the current study and if any measure contributes to the CBE more heavily than others it is the ADOS, social communication and play profiles, and broad parent report of behaviors outside of the clinic. Fourth, our longitudinal sample of both high-risk and low-risk toddlers originated from highly educated families. This could account for the inflated cognitive scores which, in turn, could also impact the associations found across measures. Therefore, there is a need for studies of samples that are more varied in terms of parental education and socioeconomic levels. Although we did not track whether toddlers in this study received early intervention services, this is unlikely given the high verbal and nonverbal abilities of this ASD sample. Finally, this study would benefit from replication with larger sample sizes, especially when comparing the ASD and BAP groups. It is likely that significant heterogeneity exists, even within each diagnostic group, and larger samples will allow for exploration of individual trajectories and identification of phenotypic subgroups.
Accordingly, future directions in this area of research should include the examination of a community-based sample over time. By examining adaptive and cognitive behavior across sampling approaches and resulting cohorts, the concerns identified in this study may be validated and potential mediating factors, such as parental or other environmental variables may be identified. As noted, following infant siblings of children with ASD into older ages, when functional social demands increase (e.g., upon entering kindergarten or later), will be of great importance, not only in regard to children who meet criteria for ASD but also for children exhibiting subthreshold levels of ASD symptomatology. Finally, item-based analyses (e.g., Klin, Volkmar, & Sparrow, 1992; Ventola, Saulnier, Steinberg, Chawarska, & Klin, 2014) could better elucidate which behaviors are developmentally acquired but not independently translated into real-life application at these tender ages. Adaptive behavior is, by nature, modifiable. Therefore, regardless of diagnosis, identification of specific adaptive deficits could inform treatment and intervention programs regarding which behaviors should be targeted and prioritized in order to effect maximal, enduring impact on functional development.
Supplementary Material
Acknowledgements:
We thank the participants and families involved in this study whose dedication made this work possible. We also thank research staff and psychologists at the Marcus Autism Center for their contributions to this study and Courtney McCracken and Lawrence Scahill for their helpful comments and suggestions regarding the statistical methods.
Contributor Information
Jessica Bradshaw, Department of Psychology, University of South Carolina.
Scott Gillespie, Department of Pediatrics, Emory University School of Medicine.
Cheryl Klaiman, Marcus Autism Center, Children’s Healthcare of Atlanta, Department of Pediatrics, Emory University School of Medicine.
Ami Klin, Marcus Autism Center, Children’s Healthcare of Atlanta, Department of Pediatrics, Emory University School of Medicine.
Celine Saulnier, Marcus Autism Center, Children’s Healthcare of Atlanta, Department of Pediatrics, Emory University School of Medicine.
References
- American Psychiatric Association. (2000). Diagnostic and Statistical Manual of Mental Disorders: DSM-IV-TR (4th ed.). Arlington, VA: American Psychiatric Association. [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders: DSM-5 (5th ed.). Arlington, VA: American Psychiatric Association. [Google Scholar]
- Baio J, Wiggins L, Christensen DL, Maenner MJ, Daniels J, Warren Z,…Dowling NF (2018). Prevalence of Autism Spectrum Disorder Among Children Aged 8 Years - Autism and Developmental Disabilities Monitoring Network, 11 Sites, United States, 2014. Morbidity and Mortality Weekly Report. Surveillance Summaries (Washington, D.C. : 2002), 67(6), 1–23. 10.15585/mmwr.ss6706a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carter A, Volkmar FR, Sparrow SS, Wang JJ, Lord C, Dawson G,…Schopler E (1998). The Vineland Adaptive Behavior Scales: Supplementary norms for individuals with autism. Journal of Autism and Developmental Disorders, 28(4), 287–302. [DOI] [PubMed] [Google Scholar]
- Charman T, Young GS, Brian J, Carter A, Carver LJ, Chawarska K,…Zwaigenbaum L (2017). Non-ASD outcomes at 36 months in siblings at familial risk for autism spectrum disorder (ASD): A baby siblings research consortium (BSRC) study. Autism Research : Official Journal of the International Society for Autism Research, 10(1), 169–178. 10.1002/aur.1669 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chawarska K, Klin A, Paul R, & Volkmar F (2007). Autism spectrum disorder in the second year: Stability and change in syndrome expression. Journal of Child Psychology and Psychiatry, 48(2), 128–138. 10.1111/j.1469-7610.2006.01685.x [DOI] [PubMed] [Google Scholar]
- Chawarska K, Shic F, Macari S, Campbell DJ, Brian J, Landa R,…Bryson S (2014). 18-month predictors of later outcomes in younger siblings of children with autism spectrum disorder: A baby siblings research consortium study. Journal of the American Academy of Child and Adolescent Psychiatry, 53(12), 1317–1327.e1. 10.1016/j.jaac.2014.09.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Constantino JN (2012). Social Responsiveness Scale, Second Edition (SRS-2). Los Angeles: Western Psychological Services. [Google Scholar]
- Estes A, Munson J, Rogers SJ, Greenson J, Winter J, & Dawson G (2015). Long-term outcomes of early intervention in 6-year-old children with autism spectrum disorder. Journal of the American Academy of Child and Adolescent Psychiatry, 54(7), 580–587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farley MA, McMahon WM, Fombonne E, Jenson WR, Miller J, Gardner M,…Coon H (2009). Twenty-year outcome for individuals with autism and average or near-average cognitive abilities. Autism Research, 2(2), 109–118. 10.1002/aur.69 [DOI] [PubMed] [Google Scholar]
- Fenton G, D’Ardia C, Valente D, Del Vecchio I, Fabrizi A, & Bernabei P (2003). Vineland adaptive behavior profiles in children with autism and moderate to severe developmental delay. Autism : The International Journal of Research and Practice, 7(3), 269–87. 10.1177/1362361303007003004 [DOI] [PubMed] [Google Scholar]
- Frazier TW, Youngstrom EA, Hardan AY, Georgiades S, Constantino JN, & Eng C (2015). Quantitative autism symptom patterns recapitulate differential mechanisms of genetic transmission in single and multiple incidence families. Molecular Autism, 6(1), 58 10.1186/s13229-015-0050-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gamliel I, Yirmiya N, Jaffe DH, Manor O, & Sigman M (2009). Developmental Trajectories in Siblings of Children with Autism: Cognition and Language from 4 Months to 7 Years. Journal of Autism and Developmental Disorders, 39(8), 1131–1144. 10.1007/s10803-009-0727-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gotham K, Pickles A, & Lord C (2009). Standardizing ADOS Scores for a Measure of Severity in Autism Spectrum Disorders. Journal of Autism and Developmental Disorders, 39(5), 693–705. 10.1007/s10803-008-0674-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howlin P, Goode S, Hutton J, & Rutter M (2004). Adult outcome for children with autism. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 45(2), 212–29. [DOI] [PubMed] [Google Scholar]
- Howlin P, Moss P, Savage S, & Rutter M (2013). Social outcomes in mid- to later adulthood among individuals diagnosed with autism and average nonverbal IQ as children. Journal of the American Academy of Child and Adolescent Psychiatry, 52(6), 572–81.e1. 10.1016/j.jaac.2013.02.017 [DOI] [PubMed] [Google Scholar]
- Jones W, & Klin A (2013). Attention to eyes is present but in decline in 2–6-month-old infants later diagnosed with autism. Nature, 504(7480), 427–31. 10.1038/nature12715 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kanne SM, Gerber AJ, Quirmbach LM, Sparrow SS, Cicchetti DV, & Saulnier CA (2011). The Role of Adaptive Behavior in Autism Spectrum Disorders: Implications for Functional Outcome. Journal of Autism and Developmental Disorders, 41(8), 1007–1018. 10.1007/s10803-010-1126-4 [DOI] [PubMed] [Google Scholar]
- Klin A, Saulnier CA, Sparrow SS, Cicchetti DV, Volkmar FR, & Lord C (2007). Social and Communication Abilities and Disabilities in Higher Functioning Individuals with Autism Spectrum Disorders: The Vineland and the ADOS. Journal of Autism and Developmental Disorders, 37(4), 748–759. 10.1007/s10803-006-0229-4 [DOI] [PubMed] [Google Scholar]
- Klin A, Volkmar FR, & Sparrow SS (1992). Autistic Social Dysfunction: Some Limitations of the Theory of Mind Hypothesis. Journal of Child Psychology and Psychiatry, 33(5), 861–876. 10.1111/j.1469-7610.1992.tb01961.x [DOI] [PubMed] [Google Scholar]
- Kraper CK, Kenworthy L, Popal H, Martin A, & Wallace GL (2017). The Gap Between Adaptive Behavior and Intelligence in Autism Persists into Young Adulthood and is Linked to Psychiatric Co-morbidities. Journal of Autism and Developmental Disorders. 10.1007/s10803-017-3213-2 [DOI] [PubMed] [Google Scholar]
- Landa R, & Garrett-Mayer E (2006). Development in infants with autism spectrum disorders: a prospective study. Journal of Child Psychology and Psychiatry, 47(6), 629–638. 10.1111/j.1469-7610.2006.01531.x [DOI] [PubMed] [Google Scholar]
- Lord C, Risi S, Lambrecht L, Cook EH, Leventhal B, DiLavore P,…Rutter M (2000). The Autism Diagnostic Observation Schedule—Generic: A Standard Measure of Social and Communication Deficits Associated with the Spectrum of Autism. Journal of Autism and Developmental Disorders, 30(3), 205–223. [PubMed] [Google Scholar]
- Lord C, Rutter M, DiLavore P, Risi S, Gotham K, & Bishop S (2012). Autism diagnostic observation schedule: ADOS-2. Torrance, CA: Western Psychological Services. [Google Scholar]
- Loveland KA, & Kelley ML (1991). Development of adaptive behavior in preschoolers with autism or Down syndrome. American Journal of Mental Retardation : AJMR, 96(1), 13–20. [PubMed] [Google Scholar]
- Macari SL, Wu GC, Powell KK, Fontenelle S, Macris DM, & Chawarska K (2018). Do Parents and Clinicians Agree on Ratings of Autism-Related Behaviors at 12 Months of Age? A Study of Infants at High and Low Risk for ASD. Journal of Autism and Developmental Disorders, 48(4), 1069–1080. 10.1007/s10803-017-3410-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Messinger D, Young GS, Ozonoff S, Dobkins K, Carter A, Zwaigenbaum L,…Sigman M (2013). Beyond Autism: A Baby Siblings Research Consortium Study of High-Risk Children at Three Years of Age. Journal of the American Academy of Child & Adolescent Psychiatry, 52(3), 300–308.e1. 10.1016/j.jaac.2012.12.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mullen E (1995). Mullen Scales of Early Learning. Circle Pines, MN: American Guidance Service. [Google Scholar]
- Ozonoff S, Young GS, Belding A, Hill M, Hill A, Hutman T,…Iosif A-M (2014). The Broader Autism Phenotype in Infancy: When Does It Emerge? Journal of the American Academy of Child & Adolescent Psychiatry, 53(4), 398–407.e2. 10.1016/j.jaac.2013.12.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ozonoff S, Young GS, Carter A, Messinger D, Yirmiya N, Zwaigenbaum L,…Stone WL (2011). Recurrence Risk for Autism Spectrum Disorders: A Baby Siblings Research Consortium Study. Pediatrics, 128(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paul R, Loomis R, & Chawarska K (2014). Adaptive Behavior in Toddlers Under two with Autism Spectrum Disorders. Journal of Autism and Developmental Disorders, 44(2), 264–270. [DOI] [PubMed] [Google Scholar]
- Perry A, Flanagan HE, Dunn Geier J, & Freeman NL (2009). Brief Report: The Vineland Adaptive Behavior Scales in Young Children with Autism Spectrum Disorders at Different Cognitive Levels. Journal of Autism and Developmental Disorders, 39(7), 1066–1078. 10.1007/s10803-009-0704-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rowberry J, Macari S, Chen G, Campbell D, Leventhal JM, Weitzman C, & Chawarska K (2015). Screening for Autism Spectrum Disorders in 12-Month-Old High-Risk Siblings by Parental Report. Journal of Autism and Developmental Disorders, 45(1), 221–229. 10.1007/s10803-014-2211-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rutter M, Bailey A, & Lord C Social Communication Questionnaire (SCQ) (2003). Torrance, CA, CA: Western Psychological Services. [Google Scholar]
- Sacrey L-AR, Zwaigenbaum L, Szatmari P, Bryson S, Georgiades S, Brian J,…Elsabbagh M (2017). Brief Report: Characteristics of preschool children with ASD vary by ascertainment. Journal of Autism and Developmental Disorders, 47(5), 1542–1550. 10.1007/s10803-017-3062-z [DOI] [PubMed] [Google Scholar]
- Salomone E, Shephard E, Milosavljevic B, Johnson MH, Charman T, & Team TB (2018). Adaptive Behaviour and Cognitive Skills: Stability and Change from 7 Months to 7 Years in Siblings at High Familial Risk of Autism Spectrum Disorder. Journal of Autism and Developmental Disorders, 48(9), 2901–2911. 10.1007/s10803-018-3554-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saulnier CA, & Klin A (2007). Brief report: social and communication abilities and disabilities in higher functioning individuals with autism and Asperger syndrome. Journal of Autism and Developmental Disorders, 37(4), 788–93. 10.1007/s10803-006-0288-6 [DOI] [PubMed] [Google Scholar]
- Sparrow SS, & Cicchetti DV (1989). Vineland Adaptive Behavior Scales In Newmark C (Ed.), Major Psychological Assessment Instruments (2nd ed., pp. 199–231). Boston: Allyn & Bacon. [Google Scholar]
- Sparrow SS, Cicchetti DV, & Balla DA (2005). Vineland Adaptive Behavior Scales, Second Edition (Vineland II) (2nd ed.). San Antonio, TX: Pearson. [Google Scholar]
- Sparrow SS, Cicchetti DV, & Saulnier CA (2016). Vineland Adaptive Behavior Scales, Third Edition (Vineland-3) (3rd ed.). San Antonio, TX: Pearson. [Google Scholar]
- Stone WL, Ousley OY, Hepburn SL, Hogan KL, & Brown CS (1999). Patterns of adaptive behavior in very young children with autism. American Journal of Mental Retardation : AJMR, 104(2), 187–99. [DOI] [PubMed] [Google Scholar]
- Sutera S, Pandey J, Esser E, Rosenthal M, Wilson L, Barton M, & Fein D (2007). Predictors of optimal outcome in toddlers diagnosed with autism spectrum disorders. Journal of Autism and Developmental Disorders, 37, 98–107. [DOI] [PubMed] [Google Scholar]
- Ventola P, Saulnier CA, Steinberg E, Chawarska K, & Klin A (2014). Early-emerging social adaptive skills in toddlers with autism spectrum disorders: an item analysis. Journal of Autism and Developmental Disorders, 44(2), 283–293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volkmar FR, Carter A, Sparrow SS, & Cicchetti DV (1993). Quantifying social development in autism. Journal of the American Academy of Child and Adolescent Psychiatry, 32(3), 627–32. 10.1097/00004583-199305000-00020 [DOI] [PubMed] [Google Scholar]
- Volkmar FR, Sparrow SS, Goudreau D, Cicchetti DV, Paul R, & Cohen DJ (1987). Social deficits in autism: an operational approach using the Vineland Adaptive Behavior Scales. Journal of the American Academy of Child and Adolescent Psychiatry, 26(2), 156–61. 10.1097/00004583-198703000-00005 [DOI] [PubMed] [Google Scholar]
- Wetherby AM, & Prizant BM (2002). Communication and symbolic behavior scales: developmental profile. Paul H Brookes Publishing. [Google Scholar]
- Zimmerman IL, Steiner VG, & Pond RE (2002). Preschool Language Scale (4th; ed.). San Antonio, TX: Pearson. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.