Abstract
Resistance to chemical insecticides detected in Aedes aegypti (L.) mosquitoes has been a problem for the National Dengue Control Program (PNCD) over the last years. In order to provide deeper knowledge of resistance to xenobiotics, our study evaluated the susceptibility profile of temephos, diflubenzuron, and cypermethrin insecticides in natural mosquito populations from the Pernambuco State, associating these results with the local historical use of such compounds. Furthermore, mechanisms that may be associated with this particular type of resistance were characterized. Bioassays with multiple temephos and diflubenzuron concentrations were performed to detect and quantify resistance. For cypermethrin, diagnostic dose assays were performed. Biochemical tests were carried out to quantify the activity of detoxification enzymes. In addition, a screening of mutations present in the voltage-gated sodium channel gene (NaV) was performed in samples previously submitted to bioassays with cypermethrin. The populations under study were resistant to temephos and showed a positive correlation between insecticide consumption and the resistance ratio (RR) to the compound. For diflubenzuron, the biological activity ratio (BAR) ranged from 1.3 to 4.7 times, when compared to the susceptible strain. All populations showed resistance to cypermethrin. Altered enzymatic profiles of alpha, p-nitrophenyl acetate (PNPA) esterases and glutathione-S-transferases were recorded in most of these samples. Molecular analysis demonstrated that Arcoverde was the only population that presented the mutated form 1016Ile/Ile. These findings show that the situation is critical vis-à-vis the effectiveness of mosquito control using chemical insecticides, since resistance to temephos and cypermethrin is widespread in Ae. aegypti from Pernambuco.
Keywords: insecticide resistance, chemical control, mosquito control
Aedes aegypti (Linnaeus) (Diptera: Culicidae) is a vector responsible for the transmission of dengue (DENV) (Flaviviridae: Flavivirus), chikungunya (CHIKV) (Togaviridae: Alphavirus), and Zika (ZIKV) (Flaviviridae: Flavivirus) viruses in Brazil. The transmission of CHIKV in the country was initially detected in the city of Oiapoque (Amapá) in September 2014, and later in the Federal District and the states of Bahia, Mato Grosso do Sul, Roraima, and Goiás (Honorio et al. 2015). The first confirmed case of ZIKV transmission in Brazil occurred early in 2015 in Bahia and São Paulo, and then in Rio Grande do Norte, Alagoas, Maranhão, Paraíba, Para, Rio de Janeiro, and Pernambuco (Vasconcelos 2015).
In Brazil, up to October 2018, there were 220,921 probable cases of dengue, with an incidence of 106.4 cases/100,000 inhabitants. The Northeast region had the second highest number of probable cases (62,936 cases, 28.5%). This same region also presented the highest incidence of probable cases of chikungunya fever, with 10,797 cases/100,000 inhabitants (Brasil 2018). When data obtained from 2018 is compared to the previous year, there was a decrease in the number of cases, but the wide distribution of vector species in locations with favorable environmental conditions, the broad circulation of infected individuals and the susceptibility of human populations are also relevant to the increase in the number of cases of these diseases and may contribute to the outbreak of epidemics (Brasil 2014, Brasil 2016). Dengue is preventable with a vaccine, available only in the private sector and capable of protecting about 60% of immunized individuals. There are no vaccines or specific treatments available for Zika and chikungunya. Vector control is, therefore, the main strategy for minimizing the incidence of these three arboviruses.
One of the main vector control strategies of Brazil’s National Dengue Control Program (PNCD) is the use of chemical insecticides. For 14 consecutive years, breeding sites of Ae. aegypti were treated, at least once every 3 mo/yr, with the organophosphate insecticide temephos for the control of larvae. Pyrethroid adulticides were applied in the surroundings of the foci, every 15 d at strategic points, such as cemeteries, recycling stations, and at other sites in the eminence of outbreaks (Braga et al. 2004, Araujo et al. 2013). The same groups of chemical insecticides were used uninterrupted for prolonged periods, leading to the emergence of Ae. aegypti resistance and consequently, failure to control the population. Several studies in Brazil have reported a diagnosis of resistance regarding some of these compounds (Macoris et al. 1999, Lima et al. 2003, Macoris et al. 2003, da-Cunha et al. 2005b).
The widespread resistance to temephos observed in Brazil led to the substitution of this compound by the biological larvicide Bacillus thuringiensis israelensis (Bti) (Barjac) (Bacillales: Bacillaceae) in the 2001/2002 biennium in some Brazilian locations (Fontoura et al. 2012, Araujo et al. 2013). In 2009, both larvicides were replaced by insect growth regulators (IGRs) such as the insect chitin synthesis inhibitors (CSI) diflubenzuron and novaluron (Fontoura et al. 2012, Araujo et al. 2013, Chediak et al. 2016), which were used until 2013 when were replaced by the juvenile hormone analog (JH) pyripxoxyfen (Bellinato et al. 2016). IGRs act by interfering with physiological processes such as insect molting and metamorphosis, characterizing a mechanism of action different from conventional chemical insecticides (Cohen 1987). However, comprehensive studies of the susceptibility profile of Brazilian populations of Ae. aegypti to these compounds were not performed prior to their field application. There is thus no baseline for the natural mortality responses of these populations to pyriproxyfen. Consequently, there is also no information to use to establish criteria for monitoring susceptibility or resistance specific to growth regulators or for the detection of cross-resistance responses with other insecticides.
On the other hand, a study demonstrated that Bti is effective against Brazilian populations of Ae. aegypti, even when some of them are highly resistant (RR > 100 times), indicating a lack of a cross-resistance responses to temephos, which therefore makes Bti a safe biolarvicide for the management of resistant populations (Araujo et al. 2013).
The detection and quantification of resistance to chemical insecticides through in vivo assays continues to be the most widely used way of assisting decision-making regarding the use of a compound in the field. Resistance management must be based on monitoring the susceptibility of field populations in order to prevent the selection of individuals who carry genes that confer resistance on the target populations and may be able to effect timely rotation of the products used in the control programs. These assays qualify and quantify the resistance and, in combination with other biochemical and molecular assays, provide information on the mechanisms potentially involved in this resistance (Brogdon 1989, Scott 1995). Biochemical evaluations are performed to clarify which enzymes are potentially involved in the metabolism of these insecticides and the molecular tools aid diagnosis of resistance by detecting alleles that influence the response of mosquito populations to the compounds used in the controls (Brogdon 1989, Shah 2002).
An applied example of the molecular tool for the diagnosis of resistance is the detection of mutations in the voltage-dependent sodium channel (NaV) gene, the target site of organochlorine insecticides and pyrethroids (Soderlund and Knipple 2003, Soderlund 2010). The structure of the sodium channel protein is organized into four homologous domains (I–IV), each containing six hydrophobic segments (S1–S6) and one P-loop between the S5 and S6 segments (Narahashi 1992, Catterall et al. 2003, Goldin 2003, Martins and Valle 2012). One of the mutations involved in insect resistance to pyrethroids is the Ile1014Phe mutation, located in the IIS6 region of the sodium channel (Bass et al. 2007). This mutation was the first to be associated with the phenotype known as knockdown resistance (Kdr), initially described for Musca domestica (Linnaeus) (Diptera: Muscidae) (Ingles et al. 1996). From this finding, the Ile1014Phe mutation in the NaV gene was also identified in Culex pipiens (Linnaeus) (Diptera: Culicidae) (Martinez-Torres et al. 1999), Anopheles gambiae (Giles) (Diptera: Culicidae) (Martinez-Torres et al. 1998), and Culex quinquefasciatus (Say) (Diptera: Culicidae) (Xu et al. 2005). However, it has not yet been described in Ae. aegypti. For this species there are other substitutions in regions IIS5, Gly923Val, and Leu982Trp (Brengues et al. 2003); IIS6, Ile1011Met, and Val1016Gly (Brengues et al. 2003, Rajatileka et al. 2008); Ile1011Val and Val1016Ile (Saavedra-Rodriguez et al. 2007); and IIIS6, Phe1534Cys (Kawada et al. 2009, Harris et al. 2010, Yanola et al. 2011, Linss et al. 2014). In Brazil, the main mutations already described in Ae. aegypti related resistance are Ile1011Met and Val1016Ile (Martins et al. 2009a,b; Lima et al. 2011; Dolabella et al. 2016; Macoris et al. 2018). However, more recently, other mutations or a combination of them have been described in Brazil (Haddi et al. 2017, Brito et al. 2018).
Although data on resistance can be found in the literature, there are no records in scientific publications about the amount of insecticide applied in each Brazilian locality and what is the correlation between consumption of this insecticide and the resistance level established. Generally, the use of these insecticides varies according to the number of houses and the number and volume of treated containers characterized as Ae. aegypti breeding sites.
The present study aimed to fully evaluate the insecticide susceptibility status of Ae. aegypti from the State of Pernambuco in Brazil and its relationship with the use of these compounds. Possible mechanisms associated with the resistance phenotype were also investigated in order to provide information useful for the management of resistance to these compounds and their effective and rational use in the field. The study is a broader evaluation than that previously undertaken by Araújo et al. (2013).
Methods
Ae. aegypti Field Populations
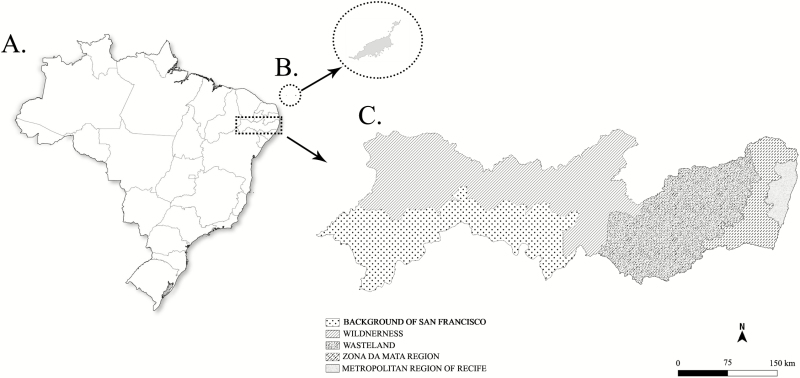
The study was carried out with Ae. aegypti populations from 16 municipalities located in the five meso-regions of the State of Pernambuco (Fig. 1): Recife, Olinda, and Ipojuca (Metropolitan Region); Glória de Goitá (Zona da Mata); Agrestina, Santa Cruz do Capibaribe, Itaiba, and Caruaru (Agreste); Cedro, Salgueiro, Afogados da Ingazeira, São José do Egito, Araripina, Serra Talhada, Arcoverde, and Petrolina (Sertão); as well as Fernando de Noronha Island (State District).
Fig. 1.
Schematic map from Brazil (A), highlighting mosquito collection sites from the Archipelago of Fernando de Noronha (B) and Pernambuco’s Meso regions.
Results regarding the use of temephos and biochemical assays in Ae. aegypti populations from Recife, Gloria do Goitá, Agrestina, Santa Cruz do Capibaribe, Afogados da Ingazeira, São José do Egito, Cedro, Salgueiro, Araripina, and Fernando de Noronha are published in Araujo et al. (2013). These data is also available in the Supp Material (online only).
Collection of Aedes Eggs
Samples of Aedes spp. were collected from 2009 to 2012 using oviposition traps (OVT), according to the methodology recommended by the MoReNAa Network (Brasil 2008). The number of ovitraps installed in each municipality was established according to the number of houses, with: 100 OVT (<50,000 properties); 150 OVT (50,000 ≤ 200,000 properties); 200 OVT (200,000 ≤ 500,000 properties); and 300 OVT (>500,000 properties). These traps were uniformly distributed in the territorial area of the municipalities, and eggs were collected at the same time, according to a schedule established locally. All egg samples were sent to the Culicidae Vector Control Referral Service (SRCCV), at the Aggeu Magalhães Institute/Oswaldo Cruz Foundation (IAM, FIOCRUZ), for the establishment of field populations in the laboratory.
Establishment of Field Populations in the Laboratory
First, the target species were identified and screened, and the populations established in the laboratory using the methodology recommended by the MoReNAa network (Lima et al. 2003). Parental generation was established with at least 700 individuals, males and females, at a ratio of 1:2. When the number of adults was >500 or <700, the F1 generation was established and the tests were carried out with the F2, to guarantee the number of mosquitoes required to perform all the tests. In the tests, larvae and adult females of at least one of the first three generations (F1, F2, and F3) of field-derived populations were used. All populations were kept under standard rearing conditions (photoperiod 12:12, 24 ± 2°C, 60 ± 20%). Adults were fed a 10% sugar solution, and bloodmeal (Gallus sp.) was given twice a week to stimulate egg production. The Rockefeller strain of Ae. aegypti, which was kept in the IAM laboratory for more than 8 yr, was used as a reference for susceptibility and control in the various chemical and biochemical tests.
Larval Bioassays
Third stage larvae (L3) were screened for susceptibility to the organophosphate temephos (Sigma/USA, lots 6333X and SZE9105X, standard containing 97.5 and 95.6% active principle, respectively) and diflubenzuron (Sigma/USA, standard containing 99.5% active principle, lot SZE7200X), a benzoylphenyl urea-based CSI. Homogeneous groups of larvae were exposed to different concentrations of temephos (0.014 mg/liter to 3.6 mg/liter) over a 24-h period for the verification of insecticide mortality rates and definition of lethal concentrations (LC). In each bioassay, three biological replicates were treated with each concentration and three were treated with solvent alone (control), each triplicate containing 20 L3 larvae, in accordance with the WHO protocol (WHO 1981).
For diflubenzuron, larvae were submitted to increasing concentrations of the product, ranging from 0.2 to 6 g/liter, to confirm the adult inhibition rate (emergency inhibition [EI]). The EI was the percentage of larvae and pupae that failed metamorphose before reaching adulthood due to inhibition of chitin synthesis by the product.
For each concentration, eight biological replicates were used with 10 L3 larvae and eight control replicates. Readings were taken on alternate days until full emergence of the adults in the control vessels. The bioassays were repeated three times on alternate days in accordance with the previously described protocols (Martins et al. 2008, Fontoura et al. 2012).
Bioassay of Adults
The susceptibility of adult forms was tested in 16 populations of Ae. aegypti, using cypermethrin, an adulticide belonging to the class of pyrethroids, according to the methodology described by da Cunha et al. (2005). The assay was performed using bottles treated with a single concentration of cypermethrin, 8 g/bottle (Sigma/USA containing 98% active principle, lot 127K1099), considered capable of differentiating susceptible and resistant individuals. Groups of 15 to 25 females from each population were exposed in three bottles impregnated with the insecticide and in a bottle impregnated with acetone (control). The knockdown effect was recorded every 15 min for 120 consecutive minutes, or until all mosquitoes were almost immobile (not able to fly). Mosquitoes were then transferred to containers free of the insecticide where they were kept for 24 h to determine the final mortality rate. The knockdown effect is considered to be a common phenomenon induced by exposure to pyrethroids and characterized by a state of temporary immobility.
Susceptibility assays were repeated at three different times as recommended by a previously described protocol (Brogdon and McAllister 1998). Populations whose mortality rates were <80% were classified as resistant, ≥98% susceptible, ≥80% and <98%, with change in susceptibility (Davidson and Zahar 1973).
History of Insecticide Use in Municipalities
A documentary analysis based on the information system of the yellow fever and dengue program (Sistema de Informação da Febre Amarela e Dengue [SISFAD]) was performed, with the consent of the State Health Department, to evaluate the historical use of temephos in the municipalities. In this analysis, the populations evaluated were divided into three groups, according to the field collection period (2010, 2011, and 2012). The quantity of product used in each of the municipalities, as well as the number of properties and containers treated, was calculated using 2007 as a starting point.
Biochemical Tests
Investigation of the mechanisms underlying metabolic resistance to insecticides was performed through the assessment of glutathione-S-transferase (GSTs), esterase and cytochrome P450 mixed-function oxidase (MFO) enzyme activity. Approximately 100 adult females of the parental generation (F1 to F3) were characterized in each of the investigated localities. Females were anesthetized by cooling and frozen at −70°C in groups of 40 to 50, 24 h after emergence and without blood supply. Homogenates from each female were distributed in 96-well microplates, each containing specific substrates for each enzyme. These plates were then read in a microplate spectrophotometer (ELX808/Biosystem Model), using different filters (340, 405, 570, 620, and 650 nm). Enzyme activity was evaluated using different substrates: α-naphthyl (Sigma/USA #N8505), β-naphthyl (Sigma/USA #N6875) and p-nitrophenyl acetate (Sigma #N8130), specific for α-esterase, β-esterase, and PNPA esterase, respectively; the substrate 3,3′,5,5′-tetramethyl-benzidine dihydrochloride (TMBZ, Sigma/USA #T8768) for MFO activity; 1-chloro-2,4-dinitrobenzene (CDNB, Sigma/USA #C-6396) and reduced glutathione (GSH, Sigma/USA #G6529) for GST. For acetylcholinesterase (ACE), an enzyme involved in the target-site mechanism of resistance to organophosphates compounds, 5,5′-Dithiobis (2-nitrobenzoic acid) (Sigma/USA #D8130) and acetylthiocholine iodide (Sigma/USA #A5751) substrates were used. All these procedures were performed according to the protocol established by the Ministry of Health (Brasil 2006). The Rockefeller strain was used as a parameter and for internal quality control of the biochemical assays.
Molecular Analysis
Females phenotyped as susceptible or resistant in the cypermethrin-impregnated bottle assay were individually used for molecular assays to detect the following Kdr mutations in the NaV gene: Leu982Trp, Ile1011Met, Leu1014Fen, Val1016Ile, and Phe1534Cys. The analysis was performed with approximately 10 individuals from each phenotyped group. After bioassays, mosquitoes were individually placed in 1.5-ml microtubes and stored at −80°C. Subsequently, individual mosquitoes were submitted to genomic DNA extraction, using a previously described protocol (Rudbeck and Dissing 1998). Primers NaV2021-Fw: (5′GACAATGTGGATCGCTTCCCG-3′) and NaV2021-Rev: (5′-GCACGGACGCAATCTGGC-3′) were manually designed based on the sodium channel sequence (AAEL006019 - VectorBase), and their quality was analyzed using the online Oligo - Analyzer software (http://www.idtdna.com/analyzer/applications/oligoanalyzer/). These primers allowed the amplification of codons 982, 1011, 1014, and 1016, generating a 622 bp fragment. PCRs were performed in a final volume of 25 µl containing: 0.4 mM of each primer (forward and reverse), 2.5 mM of MgCl2, Master Mix 1X PCR (Promega/USA), and 20 ng of genomic DNA. PCR conditions were as follows: 5 min at 94°C, followed by 30 cycles of 1 min at 94°C, 1 min at 67°C and 1 min at 72°C, with a final extension at 72°C for 10 min. PCR products were submitted to 1% agarose gel electrophoresis, stained with ethidium bromide and visualized in translucent UV. The amplified fragments were purified using a GFX PCR DNA and Gel Band Purification Kit (Amersham Pharmacia Biotech/England) according to the manufacturer’s protocol. Subsequently, samples were sequenced using both NaV2021 primers in an ABI 3100 capillary sequencer (Applied Biosystems/USA) on the IAM technology platform. Sequences obtained were evaluated for quality, edited, and aligned with the CodonCode Aligner program (v. 3.7.1). The Phe1534Cys mutation was accessed via PCR primers IIP_F (5′-GGTGGAACTTCACCGACTTC-3′) and IIS6_R (5′-GGACGCAATCTGGCTTGTTA-3′), which amplified a 581 bp fragment, in cycling conditions described in Kawada et al. (2009) and Yanola et al. (2011).
Statistical Analysis
LC and EI values were estimated by Log-Probit linear regression, using the SPSS 8.0 for Windows program. The resistance ratio (RR) or biological activity ratio (BAR) of each population for temephos and diflubenzuron, respectively, were calculated in relation to the LC95 and EI95 obtained for Rockefeller. The resistance level of the populations for temephos was classified as high resistance (RR > 10), moderate resistance (5 < RR < 10) and low resistance (3 < RR <5), according to the classification criterion previously described (Mazzarri and Georghiou 1995). For diflubenzuron, there is no established criterion for the classification of resistance in the literature. The Pearson correlation was used to analyze the relationship between the time of use of temephos and the consumption of this insecticide in each municipality, as well as to confirm the existence of a relationship between the RR found for temephos and the BAR for diflubenzuron in the populations investigated. For enzymatic assays, the Rockefeller 99th percentile was calculated for each enzyme. The enzymatic profile of each field population was classified according to the percentage of specimens that presented activity greater than the Rockefeller 99th percentile. When the percentage of individuals was less than 15%, the population was classified as unchanged, when ≥15%<50% altered and when >50% greatly altered (Montella et al. 2007). For the molecular analysis, the association between the frequencies of Kdr mutation and cypermethrin resistance was assessed using Fisher exact test (F).
Results
Larval Bioassays
Populations evaluated by the present study were resistant to temephos and all presented high levels of resistance, especially the Itaíba population, with RR above 100 and the Caruaru, Serra Talhada, and Arcoverde populations with RR over 200 (Table 1). The Ipojuca and Olinda populations presented similar RRs, over 10 and below 25. In the general evaluation of Pernambuco municipalities, four populations presented RRs of over 100 up to as high as 240, including all populations from the Agreste and Sertão (Table 1).
Table 1.
Lethal concentration for 95% of individuals (LC95) and RR for temephos, estimated for Aedes aegypti populations and Rockefeller population (standard susceptibility strain)
| Meso-Region | Year of collection | Population | Number of larvae | LC95 (mg/liter) (95% CI) | Resistance ratio (RR95) |
|---|---|---|---|---|---|
| Rockfeller Standard 1a | 1,260 | 0.014 (0.014–0.016) | 1.0 | ||
| Rockfeller Standard 2b | 1,440 | 0.009 (0.008–0.010) | 1.0 | ||
| Metropolitan | 2012 | Olindab | 1,200 | 0.162 (0.134–0.213) | 18.0 |
| 2012 | Ipojucab | 1,500 | 0.193 (0.154–0.265) | 21.4 | |
| Agreste | 2011 | Itaíbaa | 1,320 | 1.682 (1.215–2.632) | 120.2 |
| 2012 | Caruarub | 1,360 | 2.160 (1.944–2.477) | 240.1 | |
| Sertão | 2012 | S. Talhadaa | 1,320 | 2.803 (2.579–3.098) | 200.2 |
| 2012 | Arcoverdea | 1,320 | 3.116 (2.848–3.477) | 222.6 | |
| Sertão do São Francisco | 2011 | Petrolinaa | 1,760 | 0.545 (0.436–0.723) | 38.9 |
aPopulations of Aedes aegypti submitted to the activity of the 6333X batch, Standard 1.
bPopulations of Aedes aegypti submitted to the activity of the SZE9105X batch, Standard 2, for the lethal concentration (LC95) and for the calculation of the RR. RR95 = LC95 population/LC95 Rockefeller.
The diflubenzuron susceptibility profiles found for eight populations of Ae. aegypti from Pernambuco are described in Table 2. There was also a strong positive correlation between higher RRs for temephos and the higher BARs observed for diflubenzuron, considering the populations evaluated for both products (P = 0.017; ρ = 0.80).
Table 2.
Adult emergence inhibition for 50% (EI50) and 95% (EI95) of individuals and BAR to diflubenzuron, estimated for Aedes aegypti populations from Pernambuco, Brazil
| Population | Number of larvae | EI50 (mg/liter) (50% CI) | EI95 (mg/liter) (95% CI) | Biological activity ratio (BAR95) |
|---|---|---|---|---|
| Rockefeller | 2,000 | 0.456 (0.351–0.549) | 1.560 (1.400–2.047) | 1.00 |
| Fernando de Noronha | 480 | 1.212 (1.102–1.329) | 2.640 (2.386–2.991) | 1.69 |
| Recife | 1,600 | 1.612 (1.465–1.787) | 3.687 (3.212–4.435) | 2.37 |
| Itaíba | 1,520 | 1.511 (1.346–1.684) | 3.399 (3.001–4.014) | 2.18 |
| Caruaru | 1,200 | 3.761 (3.243–4.410) | 7.293 (6.278–9.098) | 4.67 |
| Cedro | 1,360 | 1.171 (0.981–1.538) | 4.224 (3.376–6.138) | 2.70 |
| Salgueiro | 1,600 | 0.605 (0.306–0.778) | 2.094 (1.791–2.747) | 1.34 |
| Serra Talhada | 1,440 | 2.839 (2.579–3.126) | 7.013 (6.088–8.467) | 4.49 |
| Petrolina | 1,520 | 1.746 (1.495–2.007) | 4.845 (4.255–5.733) | 3.10 |
BAR95 = EI95 population/EI95 Rockefeller.
Adult Bioassay and Cypermethrin Susceptibility Status
Sixteen Ae. aegypti populations from Pernambuco were tested for cypermethrin susceptibility. Results are presented in Table 3 and demonstrate that all field populations are resistant to this insecticide. The knockdown effect at the discriminatory dose was below 85% in the first 15 min of exposure to the pyrethroid and this percentage was the same after 24 h of evaluation (mortality rate). The lowest percentages of mortality (<30%) were observed in the Arcoverde, Petrolina, Itaíba, and Serra Talhada populations, municipalities representing different meso-regions in Pernambuco.
Table 3.
Knockdown effect, mortality rate, and susceptibility status of Aedes aegypti populations from Pernambuco-Brazil to the pyrethroid cypermethrin (8 µg/bottle)
| Knockdown effect (%) | Mortality rate (%) after cypermethrin exposure | |||||||
|---|---|---|---|---|---|---|---|---|
| Exposure time | Recovery time | |||||||
| Meso-Region | Population | Generation | Number of females | 15 min | 30 min | 120 min | 24 h | Susceptibility status |
| Rockefellera | 149 | 94.6 | 100 | 100 | 100 | Susceptible | ||
| Arquipélago | F. de Noronha | F2 | 148 | 83.1 | 97.9 | 100 | 70.2 | Resistant |
| Metropolitana | Recife | F1 | 160 | 14.0 | 52.5 | 93.7 | 32.5 | Resistant |
| Ipojuca | F1 | 134 | 5.20 | 35.8 | 91.0 | 58.2 | Resistant | |
| Olinda | F1 | 145 | 6.90 | 32.4 | 93.8 | 35.2 | Resistant | |
| Mata | G. de Goitá | F1 | 153 | 51.6 | 84.3 | 100 | 66.0 | Resistant |
| Agreste | Santa Cruz | F1 | 139 | 64.7 | 88.5 | 100 | 58.9 | Resistant |
| Agrestina | F2 | 163 | 13.5 | 73.6 | 98.1 | 43.5 | Resistant | |
| Itaíba | F1 | 153 | 1.96 | 18.9 | 85.6 | 27.4 | Resistant | |
| Caruaru | F2 | 167 | 4.80 | 34.7 | 82.6 | 31.7 | Resistant | |
| Sertão | Cedro | F1 | 158 | 72.1 | 90.5 | 100 | 70.8 | Resistant |
| Salgueiro | F1 | 150 | 82.0 | 95.3 | 100 | 68.6 | Resistant | |
| A. da Ingazeira | F1 | 152 | 54.6 | 83.5 | 96.7 | 36.8 | Resistant | |
| S. J. do Egito | F1 | 170 | 42.9 | 86.5 | 99.4 | 64.1 | Resistant | |
| S. Talhada | F2 | 165 | 0.0 | 4.84 | 67.3 | 18.8 | Resistant | |
| Arcoverde | F2 | 148 | 0.0 | 8.80 | 66.9 | 10.8 | Resistant | |
| Sertão do São Francisco | Petrolina | F1 | 158 | 1.9 | 29.1 | 84.8 | 22.1 | Resistant |
aControl strain.
Biochemical Tests
Of the panel of metabolic enzymes tested, β-esterase and MFO were the only ones with unaltered activity in Ae. aegypti populations from Pernambuco. In addition to these, the activity of ACE, an enzyme involved in the target-site mechanism, was also found to be unaltered in such populations. GSTs were the most altered group, with increased activity detected in all the populations evaluated; the PNPA esterase was also classified as altered in all populations, followed by α-esterases with activity modification in four populations (Table 4).
Table 4.
Enzyme activity observed in Aedes aegypti adults of populations from municipalities in Pernambuco-Brazil and the Rockefeller strain
| Ae. aegypti strain | GST (mmol/mg ptn/min) | α-esterase (nmol/mg ptn/min) | β-esterase (nmol/mg ptn/min) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Gena | Number of adultsb | p99c | % >p99d | Classificatione | Number of adults | p99 | % >p99 | Classification | Number of adults | p99 | % >p99 | Classification | |
| Rockefeller | 123 | 1.41 | - | - | 120 | 49.30 | - | - | 113 | 73.58 | - | - | |
| Olinda | F1 | 157 | 3.40 | 89 | HA | 149 | 58.67 | 10 | U | 109 | 87.81 | 3 | U |
| Ipojuca | F1 | 120 | 3.23 | 77 | HA | 197 | 54.98 | 7 | U | 198 | 78.81 | 3 | U |
| Itaíba | F1 | 99 | 2.26 | 32 | A | 118 | 61.38 | 18 | A | 117 | 66.95 | 0 | U |
| Caruaru | F2 | 199 | 4.00 | 98 | HA | 161 | 98.17 | 50 | HA | 185 | 89.03 | 6 | U |
| S. Talhada | F1 | 118 | 2.62 | 81 | HA | 143 | 86.02 | 50 | HA | 156 | 83.23 | 9 | U |
| Arcoverde | F2 | 89 | 2.28 | 48 | A | 155 | 80.03 | 53 | HA | 157 | 84.64 | 4 | U |
| Petrolina | F1 | 152 | 3.35 | 63 | HA | 114 | 54.94 | 11 | U | 108 | 71.95 | 1 | U |
| Ae. aegypti strain | Esterases-PNPA (Δabs/mg ptn/min) | MFO (nmol/mg ptn/min) | ACE (% act)f | ||||||||||
| Gena | Number of adultsb | p99c | % >p99d | Classificatione | Number of adults | p99 | % >p99 | Classification | Number of adults | p99 | % >p99 | Classification | |
| Rockefeller | 116 | 3.69 | - | - | 119 | 66.12 | - | - | 105 | 26 | - | - | |
| Olinda | F1 | 113 | 8.10 | 69 | HA | 159 | 87.94 | 9 | U | 147 | 16.36 | 0 | U |
| Ipojuca | F1 | 134 | 5.32 | 20 | A | 159 | 65.66 | 1 | U | 107 | 16.31 | 0 | U |
| Itaíba | F1 | 114 | 4.91 | 22 | A | 104 | 72.29 | 3 | U | 118 | 18.81 | 1 | U |
| Caruaru | F2 | 111 | 7.81 | 48 | A | 160 | 64.93 | 1 | U | 80 | 23.55 | 0 | U |
| S. Talhada | F1 | 117 | 6.84 | 26 | A | 155 | 35.63 | 0 | U | 153 | 16.69 | 0 | U |
| Arcoverde | F2 | 112 | 4.93 | 18 | A | 159 | 57.17 | 0 | U | 157 | 18.79 | 0 | U |
| Petrolina | F1 | 109 | 5.25 | 32 | A | 155 | 90.92 | 6 | U | 116 | 17.77 | 0 | U |
aGeneration used in the biochemical test.
bNumber of tested individuals.
c99th Percentile for the populations.
dRate of the population with activity higher than the Rockefeller 99th Percentile.
eClassification of enzyme activity compared to control (Rockefeller): unaltered (U); altered (A); and highly altered (HA).
fRate of activity in the presence of propoxur.
History of Temephos Use in Municipalities
A detailed description of the amount of temephos, number of treated establishments and recipients, as well as the RR for each municipality are presented in Table 5. These data were provided by SISFAD and the records available date from the years 2007 to 2011. Consumption was calculated up to the year prior to the field sample collection period. The results regarding the use of temephos and RR showed a strong positive correlation, with a P-value of 0.004 and ρ of 0.6504. The correlation between the number of treated recipients and RR was also significant (P = 0.04; ρ = 0.501).
Table 5.
History of temephos use for Aedes aegypti control by location, period, amount, number of treated locations, and recipients, and the resistance status to the compound
| Population | Period of analysis | Temephos (Kg) | Number of treated establishments | Number of treated recipients | Log Temephos | RR |
|---|---|---|---|---|---|---|
| Fernando de Noronha | 2007–2010 | 0 | 0 | 0 | 0 | 2.4 |
| Recife | 2007–2011 | 1.09 | 0 | 0 | 0.04 | 7.10 |
| Ipojuca | 2007–2011 | 3.087 | 85.222 | 138.801 | 3.49 | 21.4 |
| Olinda | 2007–2011 | 32.992 | 430.006 | 588.581 | 4.52 | 18.0 |
| Glória do Goitá | 2007–2010 | 4.157 | 64.056 | 152.853 | 3.62 | 72.0 |
| Santa Cruz do Capibaribe | 2007–2009 | 179.478 | 317.418 | 536.984 | 5.25 | 142.4 |
| Agrestina | 2007–2010 | 16.718 | 84.106 | 137.540 | 4.22 | 212.6 |
| Itaíba | 2007–2011 | 7.039 | 52.417 | 112.573 | 3.85 | 120.2 |
| Caruaru | 2007–2011 | 404.243 | 1.454.683 | 2.667.190 | 5.61 | 240.1 |
| Cedro | 2007–2009 | 1.713 | 41.791 | 114.300 | 3.23 | 132.7 |
| Salgueiro | 2007–2009 | 8.779 | 226.140 | 484.411 | 3.94 | 60.0 |
| Afogados da Ingazeira | 2007–2010 | 28.380 | 154.196 | 338.565 | 4.45 | 120.6 |
| São José do Egito | 2007–2009 | 26.390 | 134.771 | 365.777 | 4.42 | 124.7 |
| Serra Talhada | 2007–2011 | 96.985 | 457.761 | 1.128.263 | 4.99 | 200.20 |
| Arcoverde | 2007–2011 | 91.632 | 324.487 | 659.327 | 4.96 | 222.6 |
| Araripina | 2007–2009 | 26.719 | 182.570 | 434.923 | 4.43 | 252.7 |
| Petrolina | 2007–2011 | 10.849 | 388.677 | 578.950 | 4.04 | 38.9 |
Molecular Analysis
A 622 bp fragment of the NaV channel gene from over 300 Ae. aegypti mosquitoes was analyzed. No polymorphism was detected at the 982 and 1,014 sites. The Ile1011Met mutation was present in all populations, but no mutant homozygote was observed in either susceptible or resistant individuals. Although the 1011Ile allele frequency was high in both susceptible and resistant individuals, a higher frequency of the allele 1011Met was observed in resistant individuals than in susceptible ones in several populations (Table 6). All populations were found to be in Hardy–Weinberg (HW) disequilibrium for the Ile1011Met locus, although only Salgueiro and Serra Talhada exhibited significant deviation from HW equilibrium, due to an excess of heterozygotes (P = 0.0465 and P = 0.0174, respectively). For the Petrolina and Salgueiro populations, this mutation was associated with resistance (P < 0.05) according to the Fisher test. The Val1016Ile mutation was observed in the Fernando de Noronha, Recife, Olinda, Itaíba, Caruaru, Arcoverde, and Petrolina populations, but only in heterozygote individuals. An excess of heterozygotes was only observed in the Arcoverde population, where the 1016Ile allele was found in the highest frequency of all Pernambuco populations. This was the only population that presented homozygous individuals for the mutation Val1016Ile (Table 7). It is important to point out that we were not able to recover any susceptible individual from Arcoverde in the bioassays. The Fernando de Noronha, Recife, Olinda, Itaíba, Caruaru, and Petrolina populations showed a heterozygote deficit and no association between the presence of this mutation with resistance. Frequencies of the different genotypes in Phe1534Cys mutation are shown in Table 8. Results showed that the mutant allele 1534Cys is widespread in all populations analyzed. Only heterozygous individuals were observed. The 1534Cys allele frequency varied from 0.0 to 0.50 in resistant individuals and from 0.05 to 0.72 in susceptible individuals. It was not possible to associate the presence of this mutation with resistance (P > 0.05) using the Fisher test.
Table 6.
Genotypic and allelic frequency of Aedes aegypti kdr mutation 1011 in pyrethroid susceptible and resistant individuals from municipalities in Pernambuco-Brazil
| Genotype | Allele frequency | |||||||
|---|---|---|---|---|---|---|---|---|
| Populations | Phenotype | Ile/Ile | Ile/Met | Met/Met | Total | N | S | R |
| Fernando de Noronha | S | (0.60) | (0.30) | (0.0) | 10 | 20 | 0.85 | 0.15 |
| R | (0.30) | (0.70) | (0.0) | 10 | 0.65 | 0.35 | ||
| Recife | S | (0.66) | (0.34) | (0.0) | 9 | 18 | 0.84 | 0.16 |
| R | (0.44) | (0.56) | (0.0) | 9 | 0.72 | 0.28 | ||
| Ipojuca | S | (0.38) | (0.62) | (0.0) | 9 | 17 | 0.69 | 0.31 |
| R | (0.66) | (0.34) | (0.0) | 8 | 0.84 | 0.16 | ||
| Olinda | S | (1.0) | (0.0) | (0.0) | 9 | 18 | 1.0 | 0.0 |
| R | (0.88) | (0.12) | (0.0) | 9 | 0.95 | 0.05 | ||
| Glória do Goitá | S | (0.80) | (0.20) | (0.0) | 10 | 20 | 0.90 | 0.10 |
| R | (0.50) | (0.50) | (0.0) | 10 | 0.75 | 0.25 | ||
| Santa Cruz do Capibaribe | S | (0.40) | (0.60) | (0.0) | 10 | 17 | 0.70 | 0.30 |
| R | (0.57) | (0.43) | (0.0) | 7 | 0.78 | 0.22 | ||
| Agrestina | S | (0.10) | (0.90) | (0.0) | 10 | 18 | 0.55 | 0.45 |
| R | (0.37) | (0.63) | (0.0) | 8 | 0.68 | 0.32 | ||
| Itaíba | S | (0.60) | (0.40) | (0.0) | 10 | 20 | 0.80 | 0.20 |
| R | (0.20) | (0.80) | (0.0) | 10 | 0.60 | 0.40 | ||
| Caruaru | S | (0.60) | (0.40) | (0.0) | 10 | 20 | 0.80 | 0.20 |
| R | (0.70) | (0.30) | (0.0) | 10 | 0.85 | 0.15 | ||
| Cedro | S | (0.30) | (0.70) | (0.0) | 10 | 20 | 0.65 | 0.35 |
| R | (0.40) | (0.60) | (0.0) | 10 | 0.70 | 0.30 | ||
| Salgueiro | S | (0.40) | (0.60) | (0.0) | 10 | 20 | 0.70 | 0.30 |
| R | (0.0) | (1.0) | (0.0) | 10 | 0.50 | 0.50 | ||
| Afogados da Ingazeira | S | (0.70) | (0.30) | (0.0) | 10 | 16 | 0.85 | 0.15 |
| R | (0.16) | (0.84) | (0.0) | 6 | 0.60 | 0.40 | ||
| São José do Egito | S | (0.30) | (0.70) | (0.0) | 10 | 20 | 0.65 | 0.35 |
| R | (0.20) | (0.80) | (0.0) | 10 | 0.60 | 0.40 | ||
| Serra Talhada | S | (0.20) | (0.80) | (0.0) | 10 | 20 | 0.60 | 0.40 |
| R | (0.10) | (0.90) | (0.0) | 10 | 0.55 | 0.45 | ||
| Arcoverde | S | (1.0) | (0.0) | (0.0) | 4 | 22 | 1.0 | 0.0 |
| R | (0.65) | (0.35) | (0.0) | 20 | 0.82 | 0.18 | ||
| Petrolina | S | (0.70) | (0.30) | (0.0) | 10 | 20 | 0.85 | 0.15 |
| R | (0.10) | (0.90) | (0.0) | 10 | 0.55 | 0.45 | ||
N, number of females; S, susceptible; R, resistant; Ile, isoleucine; Met, methionine.
Table 7.
Genotypic and allelic frequency of Aedes aegypti kdr mutation 1016 in pyrethroid susceptible and resistant individuals from municipalities in Pernambuco-Brazil
| Genotype | Allele frequency | |||||||
|---|---|---|---|---|---|---|---|---|
| Populations | Phenotype | Val/Val | Val/Ile | Ile/Ile | Total | N | S | R |
| Fernando de Noronha | Susceptible | (1.0) | (0.0) | (0.0) | 9 | 19 | 1.0 | 0.0 |
| Resistant | (0.90) | (0.10) | (0.0) | 10 | 0.95 | 0.05 | ||
| Recife | Susceptible | (0.67) | (0.33) | (0.0) | 9 | 20 | 0.84 | 0.16 |
| Resistant | (1.0) | (0.0) | (0.0) | 11 | 1.0 | 0.0 | ||
| Ipojuca | Susceptible | (1.0) | (0.0) | (0.0) | 8 | 18 | 1.0 | 0.0 |
| Resistant | (1.0) | (0.0) | (0.0) | 10 | 1.0 | 0.0 | ||
| Olinda | Susceptible | (0.88) | (0.22) | (0.0) | 9 | 19 | 1.0 | 0.0 |
| Resistant | (0.70) | (0.30) | (0.0) | 10 | 0.95 | 0.05 | ||
| Glória do Goitá | Susceptible | (1.0) | (0.0) | (0.0) | 9 | 19 | 1.0 | 0.0 |
| Resistant | (1.0) | (0.0) | (0.0) | 10 | 1.0 | 0.0 | ||
| Santa Cruz do Capibaribe | Susceptible | (1.0) | (0.0) | (0.0) | 10 | 16 | 1.0 | 0.0 |
| Resistant | (1.0) | (0.0) | (0.0) | 6 | 1.0 | 0.0 | ||
| Agrestina | Susceptible | (1.0) | (0.0) | (0.0) | 10 | 18 | 1.0 | 0.0 |
| Resistant | (1.0) | (0.0) | (0.0) | 8 | 1.0 | 0.0 | ||
| Itaíba | Susceptible | (1.0) | (0.0) | (0.0) | 10 | 20 | 1.0 | 0.0 |
| Resistant | (0.80) | (0.20) | (0.0) | 10 | 0.90 | 0.10 | ||
| Caruaru | Susceptible | (0.80) | (0.20) | (0.0) | 10 | 20 | 0.80 | 0.20 |
| Resistant | (0.70) | (0.30) | (0.0) | 10 | 0.85 | 0.15 | ||
| Cedro | Susceptible | (1.0) | (0.0) | (0.0) | 10 | 20 | 1.0 | 0.0 |
| Resistant | (1.0) | (0.0) | (0.0) | 10 | 1.0 | 0.0 | ||
| Salgueiro | Susceptible | (1.0) | (0.0) | (0.0) | 9 | 17 | 1.0 | 0.0 |
| Resistant | (1.0) | (0.0) | (0.0) | 8 | 1.0 | 0.0 | ||
| Afogados da Ingazeira | Susceptible | (1.0) | (0.0) | (0.0) | 10 | 16 | 1.0 | 0.0 |
| Resistant | (1.0) | (0.0) | (0.0) | 6 | 1.0 | 0.0 | ||
| São José do Egito | Susceptible | (1.0) | (0.0) | (0.0) | 10 | 20 | 1.0 | 0.0 |
| Resistant | (1.0) | (0.0) | (0.0) | 10 | 1.0 | 0.0 | ||
| Serra Talhada | Susceptible | (1.0) | (0.0) | (0.0) | 10 | 20 | 1.0 | 0.0 |
| Resistant | (1.0) | (0.0) | (0.0) | 10 | 1.0 | 0.0 | ||
| Arcoverde | Susceptible | (0.50) | (0.50) | (0.0) | 2 | 22 | 0.75 | 0.25 |
| Resistant | (0.50) | (0.20) | (0.30) | 20 | 0.60 | 0.40 | ||
| Petrolina | Susceptible | (0.70) | (0.30) | (0.0) | 10 | 20 | 0.85 | 0.15 |
| Resistant | (0.60) | (0.40) | (0.0) | 10 | 0.80 | 0.20 | ||
N, number of females; S, susceptible; R, resistant; Ile, isoleucine; Met, methionine.
Table 8.
Genotypic and allelic frequency of Aedes aegypti kdr mutation 1534 in pyrethroid susceptible and resistant individuals from municipalities in Pernambuco-Brazil
| Genotype | Allele frequency | |||||||
|---|---|---|---|---|---|---|---|---|
| Populations | Phenotype | Phe/Phe | Phe/Cys | Cys/Cys | Total | N | S | R |
| Fernando de Noronha | S | 9 (0.90) | 1 (0.10) | 0 (0.0) | 10 | 19 | 0.95 | 0.05 |
| R | 8 (0.88) | 1 (0.12) | 0 (0.0) | 9 | 0.94 | 0.06 | ||
| Recife | S | 1 (0.11) | 8 (0.89) | 0 (0.0) | 9 | 19 | 0.55 | 0.45 |
| R | 1 (0.10) | 9 (0.90) | 0 (0.0) | 10 | 0.55 | 0.45 | ||
| Ipojuca | S | 0 (0.0) | 10 (1.0) | 0 (0.0) | 10 | 20 | 0.50 | 0.50 |
| R | 0 (0.0) | 10 (1.0) | 0 (0.0) | 10 | 0.50 | 0.50 | ||
| Olinda | S | 2 (0.22) | 7 (0.78) | 0 (0.0) | 9 | 19 | 0.61 | 0.39 |
| R | 0 (0.0) | 10 (1.0) | 0 (0.0) | 10 | 0.50 | 0.50 | ||
| Glória do Goitá | S | 0 (0.0) | 10 (1.0) | 0 (0.0) | 10 | 20 | 0.50 | 0.50 |
| R | 0 (0.0) | 10 (1.0) | 0 (0.0) | 10 | 0.50 | 0.50 | ||
| Santa Cruz do Capibaribe | S | 3 (0.30) | 7 (0.70) | 0 (0.0) | 10 | 20 | 0.65 | 0.35 |
| R | 1 (0.10) | 9 (0.90) | 0 (0.0) | 10 | 0.55 | 0.45 | ||
| Agrestina | S | 0 (0.0) | 10 (1.0) | 0 (0.0) | 10 | 20 | 0.50 | 0.50 |
| R | 0 (0.0) | 10 (1.0) | 0 (0.0) | 10 | 0.50 | 0.50 | ||
| Itaíba | S | 7 (0.70) | 3 (0.30) | 0 (0.0) | 10 | 20 | 0.85 | 0.15 |
| R | 6 (0.60) | 4 (0.40) | 0 (0.0) | 10 | 0.80 | 0.20 | ||
| Caruaru | S | 2 (0.20) | 8 (0.80) | 0 (0.0) | 10 | 20 | 0.60 | 0.40 |
| R | 0 (0.0) | 10 (1.0) | 0 (0.0) | 10 | 0.50 | 0.50 | ||
| Cedro | S | 2 (0.20) | 8 (0.80) | 0 (0.0) | 10 | 19 | 0.60 | 0.40 |
| R | 1 (0.11) | 8 (0.89) | 0 (0.0) | 9 | 0.55 | 0.45 | ||
| Salgueiro | S | 2 (0.22) | 7 (0.78) | 0 (0.0) | 9 | 19 | 0.61 | 0.39 |
| R | 2 (0.20) | 8 (0.80) | 0 (0.0) | 10 | 0.60 | 0.40 | ||
| Afogados da Ingazeira | S | 7 (0.70) | 3 (0.30) | 0 (0.0) | 10 | 19 | 0.85 | 0.15 |
| R | 6 (0.67) | 3 (0.33) | 0 (0.0) | 9 | 0.83 | 0.17 | ||
| São José do Egito | S | 3 (0.42) | 4 (0.58) | 0 (0.0) | 7 | 17 | 0.28 | 0.72 |
| R | 10 (1.0) | 0 (0.0) | 0 (0.0) | 10 | 1.0 | 0.0 | ||
| Serra Talhada | S | 5 (0.50) | 5 (0.50) | 0 (0.0) | 10 | 20 | 0.75 | 0.25 |
| R | 4 (0.40) | 6 (0.60) | 0 (0.0) | 10 | 0.70 | 0.30 | ||
| Arcoverde | S | 20 | ||||||
| R | 6 (0.30) | 14 (0.70) | 0 (0.0) | 20 | 0.65 | 0.35 | ||
| Petrolina | S | 4 (0.40) | 6 (0.60) | 0 (0.0) | 10 | 20 | 0.70 | 0.30 |
| R | 4 (0.40) | 6 (0.60) | 0 (0.0) | 10 | 0.70 | 0.30 | ||
N, number of females; S, susceptible; R, resistant; Phe, Phenylalanine; Cys, Cysteine.
Discussion
The present study assessed the susceptibility status of Ae. aegypti populations from the state of Pernambuco with regard to various chemical insecticides commonly used in the area. In Brazil, resistance to temephos is widely disseminated and levels reported until 2012 are very heterogeneous. Even those considered high (>10 times) are lower than those observed in the populations evaluated in the present study (Lima et al. 2003, Braga et al. 2004, Lima et al. 2006, Beserra et al. 2007, Montella et al. 2007, Melo-Santos et al. 2010, Lima et al. 2011, Fontoura et al. 2012, Macoris et al. 2014, Bellinato et al. 2016). Resistance to this compound has been reported in the state of Pernambuco even for nontarget species, such as Cx. quinquefasciatus, the Bancroftian filariasis vector that inhabits breeding sites other than Ae. aegypti (Amorim et al. 2013). In a previous study conducted by our group, of the 10 populations evaluated in Pernambuco, only the Fernando de Noronha population was susceptible to the larvicide temephos. It is important to point out that the use of chemical insecticides, in general, to control mosquitoes is not allowed in this archipelago, according to the legislation for Environmental Protection Areas (EPAs). The larval control of Ae. aegypti in this locality has been conducted using the biolarvicide Bti, since 2002. Of the other resistant populations, only mosquitoes derived from the Recife population presented a moderate level of resistance to temephos. This was to be expected since temephos was replaced by Bti in this locality in 2002/2003. The others showed higher levels, most of them with RR > 100 (Araujo et al. 2013).
The history of temephos use among Pernambuco populations of Ae. aegypti confirmed that there are differences in the consumption of the product in different municipalities. The quantity of product used may vary according to the number of houses in each locality, the number of breeding sites that need treatment, as well as the volume of each breeding place. However, we did not have access to all this information, nor to data on the quantity of these products used in the years prior to 2007. The present study was able to confirm an association between the consumption of product in each locality and the level of resistance of the populations (P = 0.004; ρ = 0.6504). The most significant changes in susceptibility were observed in locations with more than 14 yr of consecutive use of the product, taking into account that this product has been routinely used since 1996. Although we detected this correlation using the MoReNAa/PNCD recommendations, the criterion for replacing temephos used until 2005 was restricted to a value of RR > 10 (Brasil 2009).
Melo-Santos et al. (2010) stated that alarming levels of resistance could be a consequence of the structure of the PNCD, which promoted heavy selection pressure for temephos resistance due to the extensive and intensive use of this compound. It is therefore important to remember that resistance to chemical insecticides is a problem that has been affecting the dengue vector control programs in the world and has been well documented for countries in the Caribbean region since the late 1980s (Georghiou et al. 1987, Rawlins and Ragoonansingh 1990, Rawlins 1998). Populations of Ae. aegypti resistant to temephos have also been described in Brazil (Araujo et al. 2013, Gambarra et al. 2013, Bellinato et al. 2016, Chediak et al. 2016), Costa Rica (Bisset et al. 2013), Cuba (Bisset et al. 2004), Bolivia (Biber et al. 2006), Colombia (Ocampo et al. 2011, Santacoloma et al. 2012, Grisales et al. 2013), Argentina (Llinas et al. 2010), El Salvador (Lazcano et al. 2009), India (Tikar et al. 2009, Shetty et al. 2013), Malaysia (Loke et al. 2010), Trinidad (Polson et al. 2011), and Thailand (Komalamisra et al. 2011). The dynamics of resistance may be linked to a number of factors, including the methodology of exposure to the insecticide itself, the preexisting level of sensitivity to the compound, the frequency of the resistance gene(s), the presence of distinct mechanisms of resistance, and the form of resistance inheritance in selected populations (Hemingway et al. 2004).
The populations evaluated in the present study for susceptibility to diflubenzuron showed different temephos RRs and different enzymatic activity profiles. The results obtained may contribute to the establishment of a baseline dose–response, since the samples were collected at the beginning of the use of this compound in the field (year 2012). This and other studies (Bellinato et al. 2016, Garcia et al. 2018) can be used to draw up resistance classification criteria for this compound since temephos is currently the only criterion used (Mazzari and Georghiou 1995). Furthermore, these data serve as a basis for future monitoring in the locations where these insecticides were used routinely.
A study conducted by Fontoura et al. (2012) with populations of Ae. aegypti in Brazil showed that four populations with moderate to high levels of resistance to temephos were considered susceptible to novaluron, with RR90 ranging from 0.83 to 1.71. According to these authors, there was no correlation between resistance to temephos and novaluron. In a more recent study, carried out in Brazil in 12 municipalities, Ae. aegypti, which presented RR95 between 4.0 to 27.1 for temephos, was considered susceptible to diflubenzuron, with an RR95 lower than 2.3 (Bellinato et al. 2016). Similar RRs have been observed in other studies (Marcombe et al. 2011, Lau et al. 2015, Rocha et al. 2015, Garcia et al. 2018). In the present study, RR95 ranged from 1.3 to 4.7. These variations can be considered natural in the population, since the use of diflubenzuron was just beginning and the amount used may not yet have generated heavy selection pressure in the field populations.
We observed that there was a positive correlation between temephos RR and the diflubenzuron BAR (P = 0.017; ρ = 0.80). The use of one chemical compound may induce resistance to another, if the same resistance mechanisms are involved, causing cross-resistance. The populations from Caruaru and Serra Talhada were the ones with the lowest susceptibility profiles to diflubenzuron and these two populations present similar characteristics, such as temephos RRs above 200, and the same enzymatic profile for GSTs (highly altered), alpha esterases (much altered), and PNPA esterases (altered). This suggests that these enzymes may be involved in resistance to these compounds.
Although the Ministry of Health has recommended the use of novaluron and diflubenzuron in the PNCD to replace temephos and these products have also been cleared by the World Health Organization for use in drinking water, it remains to be seen which RRs present some evidence of resistance, since there is no fully comprehensive study in Brazil of the dose-response activity of these CSI for Ae. aegypti populations. The same situation exists regarding pyriproxyfen, which is currently recommended as a primary use product. In addition to not knowing the actual effectiveness of diflubenzuron/novaluron/pyriproxyfen when used in the long term, no susceptibility monitoring of these compounds is routinely performed in Brazil.
The tests showed that all the populations from Pernambuco are resistant to cypermethrin, one of the adulticides used to control Ae. aegypti in Brazil. The last record of the test (24 h), when the insect is no longer in contact with the insecticide, was the reading chosen for the resistance diagnosis, due to the knockdown effect on mosquitoes, which could be confused with mortality. After 30 min of exposure (a lethal time for Rockefeller), only nine of the 16 populations would be classified as resistant, and after 120 min only two would enter this classification. Observing mortality only at these points in time could lead to a misdiagnosis regarding the susceptibility profile of these populations.
The monthly application of pyrethroid insecticides at strategic points such as cemeteries, discarded tires, junkyards, and others, the use in Ultra Low Volume (ULV) as a strategy for interruption of viral transmission, and the free use of sprays by the human population may have contributed to the selection of cypermethrin resistance. This last factor may be related to the resistance to this compound found in the Ae. aegypti population of Fernando de Noronha, since the local people have access to chemical insecticides in the form of sprays for domestic use. Other recent studies suggest that the use of insecticide sprays has maintained selection pressure on the populations of Ae. aegypti in various Brazilian municipalities (Garcia et al. 2018, Macoris et al. 2018). It is also possible that resistant mosquitoes may enter the archipelago passively from other localities since the island receives daily flights from Recife and Natal, seven shipping routes dock there and this may give rise to the spread of the gene among these populations.
Several factors, such as the use of pyrethroids in control programs of other insect vectors and urban pests, as well as cross-resistance with organochlorine DDT, which was used intensively in the 1960s for control of Anopheles gambiae, and eradication of Ae. aegypti, may have contributed to the process of resistance selection in other locations.
In view of the enzymatic changes observed, the high levels of resistance found in these populations are probably related to the mechanism of resistance involving metabolic detoxification. All populations showed altered patterns of glutathione-S-transferases, often related to pyrethroid resistance, which was confirmed in our study for cypermethrin (Enayati et al. 2005). Other studies have also shown that these enzymes are involved in the detoxification of organophosphates (Vontas et al. 2002) and in the metabolism of DDT (Lumjuan et al. 2005). In Brazil, DDT was used in 1940 to control Ae. aegypti during campaigns against yellow fever (Lowy 1998). The use of pyrethroids for control of this species only occurred in 2001 and, in this same year, the MoReNAa Network already detected resistance to this insecticide and changes in the metabolic activity of GSTs (da-Cunha et al. 2005a). These changes can be attributed to the maintenance of resistance alleles, which were selected through the intensive use of DDT, as well as the migration of individuals from other locations to Brazil (Montella et al. 2007).
In the present study, the α-esterases and PNPA esterases exhibited more altered patterns in the majority of the populations evaluated. α-esterases were unaltered only in Olinda, Ipojuca, and Petrolina, and these populations presented the lowest RR for temephos. The change in esterases is related to resistance to organophosphates (Field et al. 1984, Mazzarri and Georghiou 1995, Rodriguez et al. 1999). According to Montella et al. (2007), the dynamics of PNPA-esterase activity observed in several populations monitored by the MoReNAa Network also diverged from the α-EST and β-EST standards, confirming the simultaneous presence of different esterases involved in resistance in Brazilian populations of Ae. aegypti.
In a previous study conducted in Pernambuco evaluating the β-EST enzyme, only the Afogados da Ingazeira mosquito population presented alterations in this enzyme group. The populations from Salgueiro and São José do Egito, although they did not present alterations in the α-EST and β-EST esterases, this population, like most others, was also classified as highly resistant to temephos. Of the 10 populations previously evaluated, four presented alterations in MFO activity and high RR for temephos (Araujo et al. 2013). These mixed-function oxidases are generalist enzymes that detoxify all types of xenobiotics. A variety of studies have been unable to find an association between MFO and organophosphate resistance in Ae. aegypti populations (Rodriguez et al. 1999, Bisset et al. 2001, Montella et al. 2007, Lima et al. 2011). However, Braga et al. (2005) and Andrighetti et al. (2008) detected MFO alterations in Brazilian populations resistant to temephos and cypermethrin (Braga et al. 2005, Andrighetti et al. 2008). According to these authors, changes in these enzymes also suggest caution in the use of alternative insecticides as IGRs because of the possible occurrence of cross-resistance. In our research, no population presented alterations in MFO.
The evaluation of mutations related to target-site changes in the sodium channel demonstrated that the Ile1011Met mutation is widespread in all populations studied. However, only populations from Petrolina and Salgueiro showed an association between this mutation and resistance to cypermethrin (P < 0.05). It is still not clear whether the replacement of an isoleucine by a methionine or valine at site 1011 (domain IIS6) is related to resistance to pyrethroids (Brengues et al. 2003, Martins et al. 2009b), which demonstrates that other resistance mechanisms, such as the metabolic mechanism, also investigated in the present study, may be involved. Although the Val1016Ile mutation was not present in all populations, it was present in homozygotes in the Arcoverde population, where more females survived the adulticide test. It is important to point out that a larger sample is required to evaluate the circulation of the 1016Ile allele in this particular population. This mutation has been associated with resistance to pyrethroids in previous studies. Du et al. (2013) demonstrated that its presence allows the binding of both permethrin and deltamethrin in the sodium channel. These mutations were described by Saavedra-Rodriguez et al. (2007) in populations of Ae. aegypti from Latin America and, in Brazil, this mutation has been described by Martins et al. (2009a), Lima et al. (2011), Dolabella et al. (2016), and Macoris et al. (2018). Some of these evaluations also demonstrated an association between these mutations and resistance. In the present study, the Val1016Ile and Ile1011Met mutations were observed in individuals with both susceptible and resistant phenotypes, which made it difficult to associate it with the resistance found in Pernambuco populations. It is possible that co-dominance, which occurs when both alleles are expressed, may be involved in the phenotypes found. Ramphul et al. (2009) demonstrated that populations of An. gambiae that had the Leu1014Ser mutation were resistant to DDT. According to these authors, the presence of this mutation is related to a co-dominant effect in heterozygous individuals, which results in an intermediate phenotype. Besides this, analysis of a larger number of samples and of the haplotype background may reveal more associations between these mutations and the phenotype.
According to previous studies, Ae. aegypti does not present amino acid substitutions at the classic kdr 1014 site, unlike many other insects and mosquitoes of the genera Anopheles (Weetman et al. 2010) and Culex (Chen et al. 2010). This is probably because the Ae. aegypti sodium channel site 1014 is encoded by a CTA instead of the ATT codon described in most other insects. For this reason, two simultaneous nucleotide substitutions would be required to switch from Leucine (CTA) to Phenylalanine (TTT) or Serine (TCA) (Saavedra-Rodriguez et al. 2007, Martins et al. 2009a). The mutation at site 982, described for a population of Ae. aegypti from Vietnam and associated with resistance to permethrin and lambda cyhalothrin at this location (Brengues et al. 2003), was also not found in the populations investigated in the present study. In a study by Ramphul et al. (2009), populations of Anopheles gambiae presented the Leu1014Ser mutation in association with DDT resistance, and according to these authors, the presence of this mutation is related to a co-dominant effect in heterozygous individuals, which results in an intermediate phenotype. In the present study, mutations were found in both phenotyped and susceptible as well as resistant individuals (Val1016Ile and Ile1011Met) was, which made it difficult to associate these mutations with the resistance found in the populations evaluated (Ramphul et al. 2009). The presence of the Phe1534Cys mutation was evaluated in the present study, and no association was found with cypermethrin resistance (P > 0.05). The presence of this mutation has already been described in Brazil (Linss et al. 2014, Haddi et al. 2017, Garcia et al. 2018) and other research highlights its importance in resistance to pyrethroids and DDT (Harris et al. 2010, Yanola et al. 2011, Du et al. 2013). A heterozygote deficit was observed in some of the populations investigated here (Caruaru, Itaiba, Olinda, and Recife). Because these areas were hotspots for pyrethroid compounds, used for public health and/or agricultural purposes, our hypothesis is that the massive use of such insecticides may lead to a selective benefit for homozygotic individuals, since kdr is a recessive trait.
More recently in Brazil, a new mutation, V410L, has been described that, alone or in combination with the F1534C mutation, drastically reduces the sensitivity of sodium channels to type I and type II pyrethroids in Ae. aegypti (Haddi et al. 2017). The presence of these mutations may compromise the use of pyrethroids in vector control, and continuous investigation is recommended regarding their presence, as well as the calculation of their frequencies for the monitoring of resistance (Soderlund and Knipple 2003, Saavedra-Rodriguez et al. 2007, Martins et al. 2009a).
Conclusions
Due to the diversity of responses found for the populations evaluated in this study, it is evident that each of them presents peculiar characteristics related to a series of factors, both biological and operational, that lead to selection pressure caused by the use of insecticide, which does not occur in the same way in all localities. This variety of responses is not always easy to interpret and shows how different these populations are and how different the strategies used to control them should be. A standard form of control for all these populations is therefore unfeasible. Investment in the use of insecticides by the PNCD, increasing both the cost and the impact of these actions within the program is not evaluated. The wide genetic diversity that exists in the natural populations of Ae. aegypti in Brazil (Bracco et al. 2007, Scarpassa et al. 2008), the wide range of genes associated with the metabolism of toxic compounds present in the genome of this species (Strode et al. 2008, Strode et al. 2012), and the operational failures of the PNCD have enabled the mosquito to respond rapidly to the products used, giving rise to the need to replace these products.
To continue the use of these compounds, we must constantly monitor the susceptibility of Ae. aegypti to the insecticides used in the PNCD, as well as the resistance-related mutations and the genes expressed after exposure to the insecticidal compounds. In this way, the effectiveness of these products can be evaluated and health managers make more appropriate decision regarding their management.
Thus, in order to elaborate an innovative and effective program, we believe that it is necessary to adopt measures that significantly reduce the use of chemical insecticides to control of Ae. aegypti. More attention must be paid to changing the environmental conditions that determine the persistence of Ae. aegypti breeding in urban areas, especially when related to deficiencies in basic sanitation and water supply. Moreover, effective community/social participation and the use of integrated technologies to eliminate eggs, larvae, and adult mosquitoes are necessary to guarantee the sustainability of control programs.
Supplementary Material
Acknowledgments
We thank the National Dengue Control Program of the Brazilian Secretary of Health Surveillance/Ministry of Health (PNCD/SVS/MS) and Fundação Oswaldo Cruz/Vice-Presidência de Pesquisa e Laboratórios de Referência/Serviço de Referência em Controle de Culicídeos Vetores/Instituto Aggeu Magalhães (FIOCRUZ/ VPPLR/SRCCV/IAM-PERNAMBUCO); the IAM insectarium team for technical support; and all field teams from the municipalities for Ae. aegypti egg sampling. This study received support from the Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq PRONEX Rede Dengue 550116/2010-9, CNPq 590154/2011-7, CNPq 472491/2012-1) and the Fundação de Amparo à Ciência e Tecnologia do Estado de Pernambuco (FACEPE-PPSUS grant APQ 1361-4.00/08).
References Cited
- Amorim L. B., Helvecio E., de Oliveira C. M., and Ayres C. F.. 2013. Susceptibility status of Culex quinquefasciatus (Diptera: Culicidae) populations to the chemical insecticide temephos in Pernambuco, Brazil. Pest Manag. Sci. 69: 1307–1314. [DOI] [PubMed] [Google Scholar]
- Andrighetti M. T. M., Cerone F., Rigueti M., Galvani K. C., and Macoris M. L. G.. 2008. Effect of pyriproxyfen in Aedes aegypti populations with different levels of susceptibility to the organophosphate temephos. Dengue Bulletin. 32: 186–198. [Google Scholar]
- Araújo A. P., Araujo Diniz D. F., Helvecio E., de Barros R. A., de Oliveira C. M., Ayres C. F., de Melo-Santos M. A., Regis L. N., and Silva-Filha M. H.. 2013. The susceptibility of Aedes aegypti populations displaying temephos resistance to Bacillus thuringiensis israelensis: a basis for management. Parasit. Vectors. 6: 297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bass C., Nikou D., Donnelly M. J., Williamson M. S., Ranson H., Ball A., Vontas J., and Field L. M.. 2007. Detection of knockdown resistance (kdr) mutations in Anopheles gambiae: a comparison of two new high-throughput assays with existing methods. Malar. J. 6: 111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bellinato D. F., Viana-Medeiros P. F., Araújo S. C., Martins A. J., Lima J. B., and Valle D.. 2016. Resistance status to the insecticides temephos, deltamethrin, and diflubenzuron in Brazilian Aedes aegypti populations. Biomed Res. Int. 2016: 8603263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beserra E. B., Fernandes C. R., de Queiroga M. d. e. F., and de Castro F. P. Jr. 2007. [Resistance of Aedes aegypti (L.) (Diptera: Culicidae) populations to organophosphates temephos in the Paraíba State, Brazil]. Neotrop. Entomol. 36: 303–307. [DOI] [PubMed] [Google Scholar]
- Biber P. A., Dueñas J. R., Almeida F. L., Gardenal C. N., and Almirón W. R.. 2006. Laboratory evaluation of susceptibility of natural subpopulations of Aedes aegypti larvae to temephos. J. Am. Mosq. Control Assoc. 22: 408–411. [DOI] [PubMed] [Google Scholar]
- Bisset J. A., Rodríguez M. M., Molina D., Díaz C., and Soca L. A.. 2001. [High esterases as mechanism of resistance to organophosphate insecticides in Aedes aegypti strains]. Rev. Cubana Med. Trop. 53: 37–43. [PubMed] [Google Scholar]
- Bisset J. A., Magdalena Rodríguez M., Fernández D., and Pérez O.. 2004. [Status of resistance to insecticides and resistance mechanisms in larvae from Playa municipality collected during the intensive campaign against Aedes aegypti in Havana City, 2001-2002]. Rev. Cubana Med. Trop. 56: 61–66. [PubMed] [Google Scholar]
- Bisset J. A., Marín R., Rodríguez M. M., Severson D. W., Ricardo Y., French L., Díaz M., and Pérez O.. 2013. Insecticide resistance in two Aedes aegypti (Diptera: Culicidae) strains from Costa Rica. J. Med. Entomol. 50: 352–361. [DOI] [PubMed] [Google Scholar]
- Bracco J. E., Capurro M. L., Lourenço-de-Oliveira R., and Sallum M. A.. 2007. Genetic variability of Aedes aegypti in the Americas using a mitochondrial gene: evidence of multiple introductions. Mem. Inst. Oswaldo Cruz. 102: 573–580. [DOI] [PubMed] [Google Scholar]
- Braga I. A., Lima J. B., Soares S. d. a. S., and Valle D.. 2004. Aedes aegypti resistance to temephos during 2001 in several municipalities in the states of Rio de Janeiro, Sergipe, and Alagoas, Brazil. Mem. Inst. Oswaldo Cruz. 99: 199–203. [DOI] [PubMed] [Google Scholar]
- Braga I. A., Mello C. B., Montella I. R., Lima J. B., Martins A. d. e. J., Medeiros P. F., and Valle D.. 2005. Effectiveness of methoprene, an insect growth regulator, against temephos-resistant Aedes aegypti populations from different Brazilian localities, under laboratory conditions. J. Med. Entomol. 42: 830–837. [DOI] [PubMed] [Google Scholar]
- Brasil 2006. Quantification methodology for enzyme activity related to insecticide resistance in Aedes aegypti/Ministry of Health of Brazil, Fundação Oswaldo Cruz. Ministério da Saúde, Brasília: http://bvsms.saude.gov.br/bvs/publicacoes/manual_novo_protocolo_dengue.pdf [Google Scholar]
- Brasil 2008. Secretaria de Vigilância em Saúde. Rede Nacional de Monitoramento da Resistência de Aedes aegypti a Inseticidas (Rede MoReNAa): metodologia de amostragem. Ministério da Saúde, Brasília. [Google Scholar]
- Brasil 2009. Ministério da Saúde, Secretaria de Vigilância em Saúde. Rede Nacional de Monitoramento da Resistência de Aedes aegypti a Inseticidas (Rede MoReNAa). Reunião de avaliação do monitoramento da resistência das populações de Aedes aegypti do Brasil. Ministério da Saúde, Brasília. [Google Scholar]
- Brasil 2014. http://www1.saude.ba.gov.br/entomologiabahia/photoartwork2/downloads/Plano-contingencia-chikungunya-anexos-final.pdf Plano de Contingência para a Introdução do Vírus Chikungunya.
- Brasil 2016. http://portalsaude.saude.gov.br/images/pdf/2016/abril/26/2016-014---Dengue-SE13-prelo.pdf Monitoramento dos casos de dengue, febre de chikungunya e febre pelo vírus Zika até a Semana Epidemiológica 13, 2016.
- Brasil 2018. http://portalms.saude.gov.br/images/pdf/2018/outubro/31/BE-2018-050-Monitoramento-dos-casos-de-dengue--febre-de-chikungunya-e-doen--a-aguda-pelo-v--rus-Zika-at---a-Semana-Epidemiol--gica-41-de-2018-ajustado.pdf Monitoramento dos casos de dengue,febre de chikungunya e doença aguda pelo vírus Zika até a Semana Epidemiológica 43 de 2018.
- Brengues C., Hawkes N. J., Chandre F., McCarroll L., Duchon S., Guillet P., Manguin S., Morgan J. C., and Hemingway J.. 2003. Pyrethroid and DDT cross-resistance in Aedes aegypti is correlated with novel mutations in the voltage-gated sodium channel gene. Med. Vet. Entomol. 17: 87–94. [DOI] [PubMed] [Google Scholar]
- Brito L. P., Carrara L., de Freitas R. M., Lima J. B. P., and Martins A. J.. 2018. Levels of resistance to pyrethroid among distinct kdr alleles in Aedes aegypti laboratory lines and frequency of kdr Alleles in 27 natural populations from Rio de Janeiro, Brazil. Biomed Res. Int. 2018: 2410819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brogdon W. G. 1989. Biochemical resistance detection: an alternative to bioassay. Parasitol. Today 5: 56–60. [DOI] [PubMed] [Google Scholar]
- Brogdon W. G., and McAllister J. C.. 1998. Simplification of adult mosquito bioassays through use of time-mortality determinations in glass bottles. J. Am. Mosq. Control Assoc. 14: 159–164. [PubMed] [Google Scholar]
- Catterall W. A., Chandy K.G., Clapham D. E., Gutman G. A., Hofmann F., Harmar A. J., Abernethy D. R., and Spedding M.. 2003. International Union of Pharmacology: approaches to the nomenclature of voltage-gated ion channels. Pharmacol. Rev.. 55: 573–574. [DOI] [PubMed] [Google Scholar]
- Chediak M., G Pimenta F. Jr, Coelho G. E., Braga I. A., Lima J. B., Cavalcante K. R., Sousa L. C., Melo-Santos M. A., Macoris M. d. e. L., Araújo A. P., et al. 2016. Spatial and temporal country-wide survey of temephos resistance in Brazilian populations of Aedes aegypti. Mem. Inst. Oswaldo Cruz. 111: 311–321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen L., Zhong D., Zhang D., Shi L., Zhou G., Gong M., Zhou H., Sun Y., Ma L., He J., et al. 2010. Molecular ecology of pyrethroid knockdown resistance in Culex pipiens pallens mosquitoes. PLoS One 5: e11681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen E. 1987. Chitin biochemistry - synthesis and inhibition. Annu. Rev. Entomol. 32:71–93. [Google Scholar]
- da-Cunha M. P., Lima J. B., Brogdon W. G., Moya G. E., and Valle D.. 2005. Monitoring of resistance to the pyrethroid cypermethrin in Brazilian Aedes aegypti (Diptera: Culicidae) populations collected between 2001 and 2003. Mem. Inst. Oswaldo Cruz. 100: 441–444. [DOI] [PubMed] [Google Scholar]
- Davidson G., and Zahar A. R.. 1973. The practical implications of resistance of malaria vectors to insecticides. Bull. World Health Organ. 49: 475–483. [PMC free article] [PubMed] [Google Scholar]
- Dolabella S. S., Santos R. L., Silva M. C., Steffler L. M., Ribolla P. E., Cavalcanti S. C., Jain S., and Martins A. J.. 2016. Detection and distribution of V1016Ikdr mutation in the voltage-gated sodium channel gene in Aedes aegypti (Diptera: Culicidae) populations from sergipe state, Northeast Brazil. J. Med. Entomol. 53: 967–971. [DOI] [PubMed] [Google Scholar]
- Du Y., Nomura Y., Satar G., Hu Z., Nauen R., He S. Y., Zhorov B. S., and Dong K.. 2013. Molecular evidence for dual pyrethroid-receptor sites on a mosquito sodium channel. Proc. Natl. Acad. Sci. U. S. A. 110: 11785–11790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enayati A. A., Ranson H., and Hemingway J.. 2005. Insect glutathione transferases and insecticide resistance. Insect Mol. Biol. 14: 3–8. [DOI] [PubMed] [Google Scholar]
- Field W. N., Hitchen J. M., and Rees A. T.. 1984. Esterase activity in strains of Aedes aegypti (Diptera: Culicidae) tolerant and susceptible to the organophosphate insecticide malathion. J. Med. Entomol. 21: 412–418. [DOI] [PubMed] [Google Scholar]
- Fontoura N. G., Bellinato D. F., Valle D., and Lima J. B.. 2012. The efficacy of a chitin synthesis inhibitor against field populations of organophosphate-resistant Aedes aegypti in Brazil. Mem. Inst. Oswaldo Cruz. 107: 387–395. [DOI] [PubMed] [Google Scholar]
- Gambarra W. P., Martins W. F., de Lucena Filho M. L., de Albuquerque I. M., Apolinário O. K., and Beserra E. B.. 2013. Spatial distribution and esterase activity in populations of Aedes (Stegomyia) aegypti (Linnaeus) (Diptera: Culicidae) resistant to temephos. Rev. Soc. Bras. Med. Trop. 46: 178–184. [DOI] [PubMed] [Google Scholar]
- Garcia G. A., David M. R., Martins A. J., Maciel-de-Freitas R., Linss J. G. B., Araújo S. C., Lima J. B. P., and Valle D.. 2018. The impact of insecticide applications on the dynamics of resistance: the case of four Aedes aegypti populations from different Brazilian regions. Plos Negl. Trop. Dis. 12: e0006227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Georghiou G. P., Wirth M., Tran H., Saume F., and Knudsen A. B.. 1987. Potential for organophosphate resistance in Aedes aegypti (Diptera: Culicidae) in the Caribbean area and neighboring countries. J. Med. Entomol. 24: 290–294. [DOI] [PubMed] [Google Scholar]
- Goldin A. L. 2003. Mechanisms of sodium channel inactivation. Curr. Opin. Neurobiol. 13: 284–290. [DOI] [PubMed] [Google Scholar]
- Grisales N., Poupardin R., Gomez S., Fonseca-Gonzalez I., Ranson H., and Lenhart A.. 2013. Temephos resistance in Aedes aegypti in Colombia compromises dengue vector control. Plos Negl. Trop. Dis. 7: e2438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haddi K., Tomé H. V. V., Du Y., Valbon W. R., Nomura Y., Martins G. F., Dong K., and Oliveira E. E.. 2017. Detection of a new pyrethroid resistance mutation (V410L) in the sodium channel of Aedes aegypti: a potential challenge for mosquito control. Sci. Rep. 7: 46549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris A. F., Rajatileka S., and Ranson H.. 2010. Pyrethroid resistance in Aedes aegypti from Grand Cayman. Am. J. Trop. Med. Hyg. 83: 277–284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hemingway J., Hawkes N. J., McCarroll L., and Ranson H.. 2004. The molecular basis of insecticide resistance in mosquitoes. Insect Biochem. Mol. Biol. 34: 653–665. [DOI] [PubMed] [Google Scholar]
- Honório N. A., Câmara D. C., Calvet G. A., and Brasil P.. 2015. Chikungunya: an arbovirus infection in the process of establishment and expansion in Brazil. Cad. Saude Publica. 31: 906–908. [DOI] [PubMed] [Google Scholar]
- Ingles P. J., Adams P. M., Knipple D. C., and Soderlund D. M.. 1996. Characterization of voltage-sensitive sodium channel gene coding sequences from insecticide-susceptible and knockdown-resistant house fly strains. Insect Biochem. Mol. Biol. 26: 319–326. [DOI] [PubMed] [Google Scholar]
- Kawada H., Higa Y., Komagata O., Kasai S., Tomita T., Thi Yen N., Loan L. L., Sánchez R. A., and Takagi M.. 2009. Widespread distribution of a newly found point mutation in voltage-gated sodium channel in pyrethroid-resistant Aedes aegypti populations in Vietnam. Plos Negl. Trop. Dis. 3: e527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Komalamisra N., Srisawat R., Phanbhuwong T., and Oatwaree S.. 2011. Insecticide susceptibility of the dengue vector, Aedes aegypti (L.) in Metropolitan Bangkok. Southeast Asian J. Trop. Med. Public Health 42: 814–823. [PubMed] [Google Scholar]
- Lau K. W., Chen C. D., Lee H. L., Norma-Rashid Y., and Sofian-Azirun M.. 2015. Evaluation of insect growth regulators against field-collected Aedes aegypti and Aedes albopictus (Diptera: Culicidae) from Malaysia. J. Med. Entomol. 52: 199–206. [DOI] [PubMed] [Google Scholar]
- Lazcano J. A., Rodríguez M. M., San Martín J. L., Romero J. E., and Montoya R.. 2009. [Assessing the insecticide resistance of an Aedes aegypti strain in El Salvador]. Rev. Panam. Salud Publica 26: 229–234. [PubMed] [Google Scholar]
- Lima J. B., Da-Cunha M. P., Da Silva R. C., Galardo A. K., Soares Sda S., Braga I. A., Ramos R. P., and Valle D.. 2003. Resistance of Aedes aegypti to organophosphates in several municipalities in the State of Rio de Janeiro and Espirito Santo, Brazil. Am. J. Trop. Med. Hyg. 68: 329–333. [PubMed] [Google Scholar]
- Lima E. P., de Oliveira Filho A. M., de Oliveira Lima J. W., Ramos Júnior A. N., de Góes Cavalcanti L. P., and Pontes R. J.. 2006. Aedes aegypti resistance to temefos in counties of Ceará State]. Rev. Soc. Bras. Med. Trop. 39: 259–263. [DOI] [PubMed] [Google Scholar]
- Lima E. P., Paiva M. H., de Araújo A. P., da Silva E. V., da Silva U. M., de Oliveira L. N., Santana A. E., Barbosa C. N., de Paiva Neto C. C., Goulart M. O., et al. 2011. Insecticide resistance in Aedes aegypti populations from Ceará, Brazil. Parasit. Vectors. 4: 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linss J. G., Brito L. P., Garcia G. A., Araki A. S., Bruno R. V., Lima J. B., Valle D., and Martins A. J.. 2014. Distribution and dissemination of the Val1016Ile and Phe1534Cys Kdr mutations in Aedes aegypti Brazilian natural populations. Parasit Vectors. 7: 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Llinas G. A., Seccacini E., Gardenal C. N., and Licastro S.. 2010. Current resistance status to temephos in Aedes aegypti from different regions of Argentina. Mem. Inst. Oswaldo Cruz. 105: 113–116. [DOI] [PubMed] [Google Scholar]
- Loke S. R., Andy-Tan W. A., Benjamin S., Lee H. L., and Sofian-Azirun M.. 2010. Susceptibility of field-collected Aedes aegypti (L.) (Diptera: Culicidae) to Bacillus thuringiensis israelensis and temephos. Trop. Biomed. 27: 493–503. [PubMed] [Google Scholar]
- Löwy I. 1998. [Representing and intervening in public health: viruses, mosquitoes and Rockefeller Foundation experts in Brazil]. Hist. Cienc. Saude. Manguinhos. 5: 647–677. [PubMed] [Google Scholar]
- Lumjuan N., McCarroll L., Prapanthadara L. A., Hemingway J., and Ranson H.. 2005. Elevated activity of an Epsilon class glutathione transferase confers DDT resistance in the dengue vector, Aedes aegypti. Insect Biochem. Mol. Biol. 35: 861–871. [DOI] [PubMed] [Google Scholar]
- Macoris M. L. G., Andrighetti M. T., Takaku L., Glasser C. M., Garbeloto V.C., and Cirino V.C.. 1999. Changes in susceptibility of Aedes aegypti to organophosphates in municipalities in the state of Sao Paulo, Brazil. Revista de Saúde Pública. 33: 521–522. [DOI] [PubMed] [Google Scholar]
- Macoris M. L. G., Andrighetti M. T. M., Takaku L., Glasser C. M., Garbeloto V. C., and Bracco J. E.. 2003. Resistance of Aedes aegypti from the State of Sao Paulo, Brazil, to organophosphates insecticides. Memórias do Instituto Oswaldo Cruz. 98: 703–708. [DOI] [PubMed] [Google Scholar]
- Macoris M. L., Andrighetti M. T., Wanderley D. M., and Ribolla P. E.. 2014. Impact of insecticide resistance on the field control of Aedes aegypti in the State of Sao Paulo. Rev. Soc. Bras. Med. Trop. 47: 573–578. [DOI] [PubMed] [Google Scholar]
- Macoris M. L., Martins A. J., Andrighetti M. T. M., Lima J. B. P., and Valle D.. 2018. Pyrethroid resistance persists after ten years without usage against Aedes aegypti in governmental campaigns: lessons from Sao Paulo State, Brazil. PLoS Negl Trop Dis. 12: e0006390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marcombe S., Darriet F., Agnew P., Etienne M., Yp-Tcha M. M., Yebakima A., and Corbel V.. 2011. Field efficacy of new larvicide products for control of multi-resistant Aedes aegypti populations in Martinique (French West Indies). Am. J. Trop. Med. Hyg. 84: 118–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez-Torres D., Chandre F., Williamson M. S., Darriet F., Berge J.B., Devonshire A. L., Guillet P., Pasteur N., and Pauron D.. 1998. Molecular characterization of pyrethroid knockdown resistance (kdr) in the major malaria vector Anopheles gambiae s.s. Insect. Mol. Biol. 7: 179–184. [DOI] [PubMed] [Google Scholar]
- Martinez-Torres D., Chevillon C., Brun-Barale A., Berge J. B., Pasteur N. and Pauron D. 1999. Voltage-dependent Na+ channels in pyrethroid-resistant Culex pipiens L mosquitoes. Pestic. Sci. 55: 1012–1020. [Google Scholar]
- Martins A. J., and Valle D.. 2012. The pyrethroid knockdown resistance, pp. 17–38. InSoloneskiss M. L. S. (ed.), Insecticides. Intech, La Plata, Argentina. [Google Scholar]
- Martins A. J., Belinato T. A., Lima J. B., and Valle D.. 2008. Chitin synthesis inhibitor effect on Aedes aegypti populations susceptible and resistant to organophosphate temephos. Pest Manag. Sci. 64: 676–680. [DOI] [PubMed] [Google Scholar]
- Martins A. J., Lima J. B., Peixoto A. A., and Valle D.. 2009a. Frequency of Val1016Ile mutation in the voltage-gated sodium channel gene of Aedes aegypti Brazilian populations. Trop. Med. Int. Health 14: 1351–1355. [DOI] [PubMed] [Google Scholar]
- Martins A. J., Lins R. M., Linss J. G., Peixoto A. A., and Valle D.. 2009b. Voltage-gated sodium channel polymorphism and metabolic resistance in pyrethroid-resistant Aedes aegypti from Brazil. Am. J. Trop. Med. Hyg. 81: 108–115. [PubMed] [Google Scholar]
- Mazzarri M. B., and Georghiou G. P.. 1995. Characterization of resistance to organophosphate, carbamate, and pyrethroid insecticides in field populations of Aedes aegypti from Venezuela. J. Am. Mosq. Control Assoc. 11: 315–322. [PubMed] [Google Scholar]
- Melo-Santos M. A., Varjal-Melo J. J., Araújo A. P., Gomes T. C., Paiva M. H., Regis L. N., Furtado A. F., Magalhaes T., Macoris M. L., Andrighetti M. T., et al. 2010. Resistance to the organophosphate temephos: mechanisms, evolution and reversion in an Aedes aegypti laboratory strain from Brazil. Acta Trop. 113: 180–189. [DOI] [PubMed] [Google Scholar]
- Montella I. R., Martins A. J., Viana-Medeiros P. F., Lima J. B., Braga I. A., and Valle D.. 2007. Insecticide resistance mechanisms of Brazilian Aedes aegypti populations from 2001 to 2004. Am. J. Trop. Med. Hyg. 77: 467–477. [PubMed] [Google Scholar]
- Narahashi T. 1992. Nerve membrane Na+ channels as targets of insecticides. Trends Pharmacol. Sci. 13: 236–241. [DOI] [PubMed] [Google Scholar]
- Ocampo C. B., Salazar-Terreros M. J., Mina N. J., McAllister J., and Brogdon W.. 2011. Insecticide resistance status of Aedes aegypti in 10 localities in Colombia. Acta Trop. 118: 37–44. [DOI] [PubMed] [Google Scholar]
- Polson K. A., Brogdon W. G., Rawlins S. C., and Chadee D. D.. 2011. Characterization of insecticide resistance in Trinidadian strains of Aedes aegypti mosquitoes. Acta Trop. 117: 31–38. [DOI] [PubMed] [Google Scholar]
- Rajatileka S., Black W. C. IV, Saavedra-Rodriguez K., Trongtokit Y., Apiwathnasorn C., McCall P. J., and Ranson H.. 2008. Development and application of a simple colorimetric assay reveals widespread distribution of sodium channel mutations in Thai populations of Aedes aegypti. Acta Trop. 108: 54–57. [DOI] [PubMed] [Google Scholar]
- Ramphul U., Boase T., Bass C., Okedi L. M., Donnelly M. J., and Müller P.. 2009. Insecticide resistance and its association with target-site mutations in natural populations of Anopheles gambiae from eastern Uganda. Trans. R. Soc. Trop. Med. Hyg. 103: 1121–1126. [DOI] [PubMed] [Google Scholar]
- Rawlins S. C. 1998. Spatial distribution of insecticide resistance in Caribbean populations of Aedes aegypti and its significance. Rev. Panam. Salud Publica. 4: 243–251. [DOI] [PubMed] [Google Scholar]
- Rawlins S. C., and Ragoonansingh R.. 1990. Comparative organophosphorus insecticide susceptibility in Caribbean populations of Aedes aegypti and Toxorhynchites moctezuma. J. Am. Mosq. Control Assoc. 6: 315–317. [PubMed] [Google Scholar]
- Rocha H. D. R., Paiva M. H. S., Silva N. M., de Araújo A. P., Camacho D. D. R. D. R. A., Moura A. J. F. D., Gómez L. F., Ayres C. F. J., and Santos M. A. V. M.. 2015. Susceptibility profile of Aedes aegypti from Santiago Island, Cabo Verde, to insecticides. Acta Trop. 152: 66–73. [DOI] [PubMed] [Google Scholar]
- Rodríguez M. M., Bisset J. A., Milá L. H., Calvo E., Díaz C., and Alain Soca L.. 1999. [Levels of insecticide resistance and its mechanisms in a strain of Aedes aegypti of Santiago de Cuba]. Rev. Cubana Med. Trop. 51: 83–88. [PubMed] [Google Scholar]
- Rudbeck L., and Dissing J.. 1998. Rapid, simple alkaline extraction of human genomic DNA from whole blood, buccal epithelial cells, semen and forensic stains for PCR. Biotechniques. 25: 588–590, 592. [DOI] [PubMed] [Google Scholar]
- Saavedra-Rodriguez K., Urdaneta-Marquez L., Rajatileka S., Moulton M., Flores A. E., Fernandez-Salas I., Bisset J., Rodriguez M., McCall P. J., Donnelly M. J., et al. 2007. A mutation in the voltage-gated sodium channel gene associated with pyrethroid resistance in Latin American Aedes aegypti. Insect Mol. Biol. 16: 785–798. [DOI] [PubMed] [Google Scholar]
- Santacoloma L., Chaves B., and Brochero H. L.. 2012. [Susceptibility of natural populations of dengue vector to insecticides in Colombia]. Biomedica. 32: 333–343. [DOI] [PubMed] [Google Scholar]
- Scarpassa V. M., Cardoza T. B., and Cardoso Junior R. P.. 2008. Population genetics and phylogeography of Aedes aegypti (Diptera: Culicidae) from Brazil. Am. J. Trop. Med. Hyg. 78: 895–903. [PubMed] [Google Scholar]
- Scott J. A. 1995. The molecular-genetics of resistance - resistance as a response to stress. Fla. Entomol. 78: 399–414. [Google Scholar]
- Shah R., Armstrong K., Worner S. P., and Chapman R. B.. 2002. Investigation of a PCR-based methods for insecticide resistance monitoring. Pak. J. Biol. Sci. 5: 1070–1073. [Google Scholar]
- Shetty V., Sanil D., and Shetty N. J.. 2013. Insecticide susceptibility status in three medically important species of mosquitoes, Anopheles stephensi, Aedes aegypti and Culex quinquefasciatus, from Bruhat Bengaluru Mahanagara Palike, Karnataka, India. Pest Manag. Sci. 69: 257–267. [DOI] [PubMed] [Google Scholar]
- Soderlund D. M. 2010. State-dependent modification of voltage-gated sodium channels by pyrethroids. Pestic. Biochem. Physiol. 97: 78–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soderlund D. M., and Knipple D. C.. 2003. The molecular biology of knockdown resistance to pyrethroid insecticides. Insect Biochem. Mol. Biol. 33: 563–577. [DOI] [PubMed] [Google Scholar]
- Strode C., Wondji C. S., David J. P., Hawkes N. J., Lumjuan N., Nelson D. R., Drane D. R., Karunaratne S. H., Hemingway J., Black W. C. IV, et al. 2008. Genomic analysis of detoxification genes in the mosquito Aedes aegypti. Insect Biochem. Mol. Biol. 38: 113–123. [DOI] [PubMed] [Google Scholar]
- Strode C., de Melo-Santos M., Magalhães T., Araújo A., and Ayres C.. 2012. Expression profile of genes during resistance reversal in a temephos selected strain of the dengue vector, Aedes aegypti. PLoS One 7: e39439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tikar S. N., Kumar A., Prasad G. B., and Prakash S.. 2009. Temephos-induced resistance in Aedes aegypti and its cross-resistance studies to certain insecticides from India. Parasitol. Res. 105: 57–63. [DOI] [PubMed] [Google Scholar]
- Vasconcelos P. F. C. 2015. Doença pelo vírus Zika: um novo problema emergente nas Américas? Rev Pan-Amazônica Saúde. 2, 9–10. [Google Scholar]
- Vontas J. G., Small G. J., Nikou D. C., Ranson H., and Hemingway J.. 2002. Purification, molecular cloning and heterologous expression of a glutathione S-transferase involved in insecticide resistance from the rice brown planthopper, Nilaparvata lugens. Biochem. J. 362: 329–337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weetman D., Wilding C. S., Steen K., Morgan J. C., Simard F., and Donnelly M. J.. 2010. Association mapping of insecticide resistance in wild Anopheles gambiae populations: major variants identified in a low-linkage disequilbrium genome. PLoS One 5: e13140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO 1981. WORLD HEALTH ORGANIZATION. Instructions for Determining the Susceptibility or Resistance of Mosquito Larvae to Insecticides. World Health Organization, Geneva, Switzerland: p. 6. [Google Scholar]
- Xu Q., Liu H., Zhang L., and Liu N.. 2005. Resistance in the mosquito, Culex quinquefasciatus, and possible mechanisms for resistance. Pest Manag. Sci. 61: 1096–1102. [DOI] [PubMed] [Google Scholar]
- Yanola J., Somboon P., Walton C., Nachaiwieng W., Somwang P., and Prapanthadara L. A.. 2011. High-throughput assays for detection of the F1534C mutation in the voltage-gated sodium channel gene in permethrin-resistant Aedes aegypti and the distribution of this mutation throughout Thailand. Trop. Med. Int. Health 16: 501–509. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.