Abstract
OBJECTIVES
This study explored variation in the extent of use of electronic health record (EHR)-based health information technology (IT) functionalities across US ambulatory care practices. Use of health IT functionalities in ambulatory care is important for delivering high-quality care, including that provided in coordination with multiple practitioners.
STUDY DESIGN
We used data from the 2014 Healthcare Information and Management Systems Society Analytics survey. The responses of 30,123 ambulatory practices with an operational EHR were analyzed to examine the extent of use of EHR-based health IT functionalities for each practice.
METHODS
We created a novel framework for classifying ambulatory care practices employing 7 domains of health IT functionality. Drawing from the survey responses, we created a composite “use” variable indicating the extent of health IT functionality use across these domains. “Super-user” practices were defined as having near-full employment of the 7 domains of health IT functionalities and “under-users” as those with minimal or no use of health IT functionalities. We used multivariable logistic regression to investigate how the odds of super-use and under-use varied by practice size, type, urban or rural location, and geographic region.
RESULTS
Seventy-three percent of practices were not using EHR technologies to their full capability, and nearly 40% were classified as under-users. Under-user practices were more likely to be of smaller size, situated in the West, and located outside a metropolitan area.
CONCLUSIONS
To achieve the broader benefits of the EHR and health IT, health systems and policy makers need to identify and address barriers to full use of health IT functionalities.
Healthcare organizations across the United States have invested substantially in electronic health record (EHR) systems, incentivized by federal investment and legislation.1 Ambulatory care practices have steadily improved their EHR adoption over the last decade; 2014 estimates indicated that approximately 78% of ambulatory care practices had a certified EHR platform.2,3 There is substantial heterogeneity within this group, however. The EHR acts as a backbone for a range of health information technology (IT) functionalities with multiple potential applications to care delivery; practices vary in their adoption of these functionalities and in the extent of their use of these tools in routine practice.
Empirical data show benefit to processes of care from an array of health IT functionalities, including data repository,4 computerized order entry,5,6 electronic messaging and health information exchange,7 patient-facing tools,8,9 and clinical decision support.5,10 In addition, quality improvements from the EHR and associated functionalities likely transcend the individual provider organization, with some tools (such as health information exchange) designed to work in synergy for coordination of care among multiple practitioners.11 Practices restricting themselves to the more basic features of this technology may limit the potential impact of the EHR on their own performance4,12,13; it is also possible that slow or elementary adopters may have a negative impact on the quality of the health system as a whole.
In this study, we explored variation in the extent of use of EHR- based health IT functionalities in the ambulatory care setting. We used data from the Healthcare Information and Management Systems Society (HIMSS) Analytics ambulatory practice surveys to create a new framework of EHR use across 7 domains of health IT functionality, and we identified practices that were high users of a range of functionalities (“super-users”) and those that used these EHR tools only minimally (“under-users”). Noting that studies on hospital EHR adoption suggest that small and rural hospitals may experience greater barriers in implementing this technology,14 we investigated how the rates of super-use and under-use vary according to practice size, type, urban or rural location, and geographic region.
METHODS
HIMSS conducts annual surveys of US health systems and organizations, with a particular focus on structural characteristics of their EHR and health IT functionalities in use, generating a comprehensive database that has been frequently used in empirical research.15–18 To date, published studies that have employed these data utilized only the data regarding hospitals.19 However, HIMSS also obtains data on ambulatory care practices, defined as facilities providing “preventative, diagnostic, therapeutic, surgical, and/or rehabilitative outpatient care where the duration of treatment is less than 24 hours—and is generally referred to as outpatient care.” We used data from the 2014 ambulatory practice survey, which contains information on more than 75% of US health system–associated ambulatory care practices. HIMSS defines a health system as an organization composed of at least 1 hospital and its associated nonacute facilities, and “associated” as a governance relationship (ie, they are owned, leased, or managed by a health system). Eligible practices for our study were those that indicated they had a “live and operational” EHR and had completed at least 1 health IT functionality survey question. We linked the practice site zip code with a publicly available dataset providing a geographic taxonomy to develop a measure of rurality.20
Existing EHR classifications applicable to the ambulatory care setting have limitations; many are defined by only short lists of Meaningful Use criteria,21 and categorizations of “basic” or “comprehensive” systems are largely hospital-focused. We created a novel framework for classifying ambulatory care practices using 7 domains of health IT functionality, referencing the structure of the HIMSS survey and historical taxonomies (such as that by Des Roches et al22). The 7 domains were data repository, clinical decision support, order entry management, electronic messaging, results management, health information exchange, and patient use. The HIMSS survey asks respondents to indicate if they use any of more than 50 EHR-based health IT functionalities and, in some cases, assesses the intensity of this use (eg, “What proportion of orders are completed using the EHR?”). We matched all of these items to 1 of the 7 domains of functionality (details are given in the eAppendix [available at ajmc.com]).
We used a 3-step process to define a practice as a super-user or under-user of health IT functionalities. First, we classified practices into 3 categories based on the number of functionalities employed within each domain. Practices in the lower quartile for their sum total of functionality within a domain were categorized as “low” (score of 0), those in the upper quartile were defined as “high” (score of 2), and practices in the interquartile range were categorized as “moderate” (score of 1). Second, we created a composite “use” variable by summing the domain scores for each practice (composite scores ranged from a minimum of 0 to a maximum of 14). Third, we ranked practices according to this composite variable. We explored the natural distribution of the data in order to identify practices that were low and high outliers on the composite score. We defined practices as super-users if they had a composite score of 12 to 14 and under-users if their composite score was 0 to 2. We performed sensitivity analyses to explore the impact of alternative criteria; our findings were robust to alternate specification of the cut points.
We examined characteristics of practices according to their classification as a super-user or under-user, using Pearson’s χ2 test for the categorical variables and a 2-sided t test for the continuous variable. Variables of interest included the size of the practice (defined as number of affiliated physicians, in 4 categories), location (metropolitan, midsize, small town, or rural), geographical region (Northeast, Midwest, South, or West), and type of practice (primary/family care; single-specialty, multispecialty, and allied health; or urgent care and specialist services). Allied health practices included those practicing podiatry, occupational health, weight management, and holistic medicine, among others. Practices providing “specialist services” were those giving specialty- circumscribed care to a defined population (eg, patients undergoing dialysis or cardiac rehabilitation). Using multivariable logistic regression models, we estimated odds ratios associated with super-user and under-user status, according to practice characteristics. Analyses were performed using Stata version 14.2 (StataCorp LLC; College Station, Texas). We used Quantum Geographic Information Software to create maps showing the distribution of use categories across the United States.
RESULTS
There were 38,638 health system-affiliated practices in the HIMSS data; 32,236 (83.4%) indicated they had a live and operational EHR, and of these, 30,123 (93.5%) provided survey responses. The majority (77.4%) of responding practices in the sample had fewer than 7 associated physicians; however, the distribution of this variable was skewed by some practices with large numbers of physicians (maximum, 2300) such that the median number of physicians per practice was 2 and the mean was 5.6. The dominant practice type was single or multiple specialty and allied health practitioners (62.5%), whereas 30.8% were primary/family medicine. Nearly 75% of practices were located in metropolitan areas; only 4.7% were rurally located.
Table 1 shows the proportions of practices with low, moderate, and high use by domain of health IT functionality. The eAppendix provides the full table of functionalities and frequency of responses and the descriptive characteristics of the total sample and super-user and under-user practices. Among practices indicating any use of computerized physician order entry, only 35.6% used this capacity for more than 75% of orders. Additionally, although the majority of practices were adept at using their EHR for more elementary functions, such as data storage (100% of practices stored transcribed reports electronically and 61.1% used the EHR for nursing documentation), some of the more advanced functionalities (such as the ability to find and modify orders for all patients on a specific medication) were used at much lower rates (29.3%).
TABLE 1.
Number and Percentage of Practices Reporting Use of Health IT Functionalities by EHR Domain [N = 30,123]
| Low Use |
Moderate Use |
High Use |
||||
|---|---|---|---|---|---|---|
| Domain | n | % | n | % | n | % |
| Data repository | 9850 | 32.7 | 9707 | 32.2 | 10,566 | 35.1 |
| Clinical decision support | 12,553 | 41.7 | 9095 | 30.2 | 8475 | 28.1 |
| Order entry management | 12,533 | 41.6 | 5722 | 19.0 | 11,868 | 39.4 |
| Electronic messaging | 14,299 | 47.5 | 8032 | 26.7 | 7792 | 25.9 |
| Results management | 16,897 | 56.1 | 1931 | 6.4 | 11,295 | 37.5 |
| Health information exchange | 12,821 | 42.6 | 8839 | 29.3 | 8463 | 28.1 |
| Patient use of EHR tools | 14,649 | 48.6 | 7043 | 23.4 | 8431 | 28.0 |
EHR indicates electronic health record; IT, information technology.
Table 2 gives the findings of the multivariable analyses, in which 8003 practices were classified as health IT super-users (26.6%). The odds of super-user status were lower for single-specialty, multispecialty, and allied health practices than for primary/family care clinics, and lower still for practices providing specialist services or acute care. The likelihood of super-use increased as the number of affiliated physicians increased, and super-users were more than twice as likely to be located in metropolitan areas than rural. Overall, the odds of being a super-user were highest for practices in the Midwest.
TABLE 2.
Odds of Super- or Under-Use by Practice Characteristicsa
| Super-User |
Under-User |
|||
|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | |
| Practice Size (number of associated physicians) | ||||
| <7 | Reference | |||
| 7–19 | 1.61 | (1.49–1.75) | 0.77 | (0.71–0.83) |
| 20–99 | 2.06 | (1.82–2.32) | 0.66 | (0.58–0.75) |
| ≥100 | 3.24 | (2.95–3.55) | 0.78 | (0.71–0.85) |
| Practice Type | ||||
| Primary/family | Reference | |||
| Single or multiple specialty, allied health | 0.89 | (0.83–0.94) | 1.08 | (1.03–1.14) |
| Specialist services and urgent care | 0.64 | (0.57–0.72) | 1.40 | (1.27–1.55) |
| Location | ||||
| Rural | Reference | |||
| Small town | 1.02 | (0.84–1.22) | 0.99 | (0.86–1.13) |
| Midsize | 0.99 | (0.83–1.18) | 0.95 | (0.84–1.08) |
| Metropolitan | 2.45 | (2.10–2.85) | 0.61 | (0.54–0.68) |
| Region | ||||
| Northeast | Reference | |||
| Midwest | 2.05 | (1.90–2.22) | 0.59 | (0.56–0.64) |
| South | 1.32 | (1.22–1.42) | 0.98 | (0.92–1.04) |
| West | 0.93 | (0.85–1.03) | 1.16 | (1.07–1.26) |
OR indicates odds ratio.
Analysis excludes 115 practices without accurate zip code information.
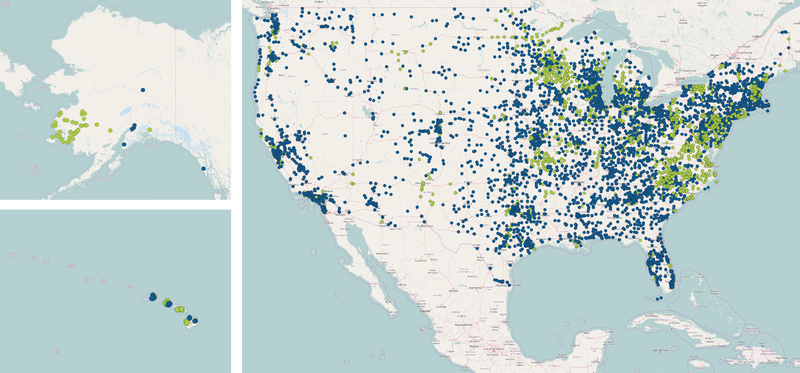
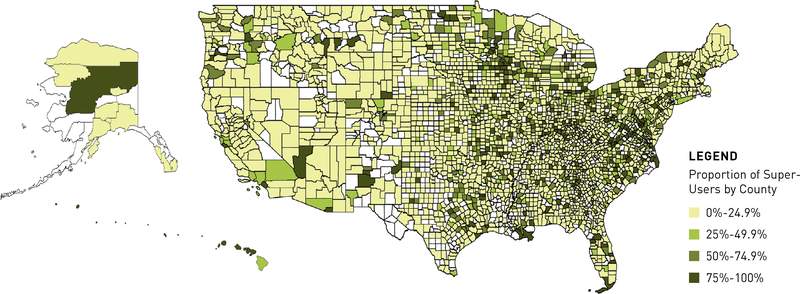
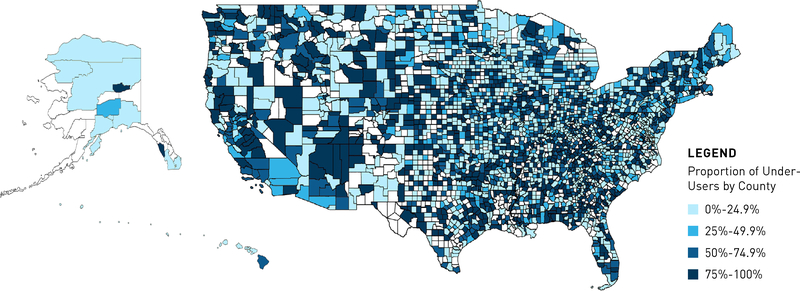
In contrast, 11,706 practices (38.9%) were classified as health IT under-users. Under-user practices were more likely to be situated in the West, have fewer affiliated physicians, and be located outside of metropolitan centers. Compared with primary/family care practices, single-specialty, multispecialty, and allied health practices were more likely to be under-users, as were those that provided specialist or acute care services. Figures 1, 2, and 3 give the geographical location of super- and under-users and the proportion of these practices by county.
FIGURE 1.
Location of Super-User (Green) and Under-User (Blue) Practices
FIGURE 2.
Proportion of Super-User Practices, by County
FIGURE 3.
Proportion of Under-User Practices, by County
DISCUSSION
We examined variation in the extent of use of EHR-based health IT functionalities in a national sample of US ambulatory care practices. Among 30,123 practices that were affiliated with a health system and had an operational EHR, only 27% were super-users, meaning they were maximally using EHR functionalities designed to improve patient care and facilitate high-quality performance across the broader health system. Of concern was that nearly 40% of ambulatory practices were categorized as under-users, indicating minimal use of the EHR and associated health IT functionalities. Under-use was more likely in smaller practices, those located outside of metropolitan centers, non-primary care practices, and those situated in the West.
There are likely multiple factors involved in EHR and health IT under-use by ambulatory care practices. Cost has been cited as the primary barrier to adopting an EHR system23; similarly, upgrading a basic EHR to one more comprehensive may not be financially possible for practices with limited resources. Cost may also be a factor for these practices because of the health IT support resources required to train users and maintain the systems. Smaller and rural practices were more likely to be under-users, a pattern also seen in the adoption of EHR and health IT in hospitals.24 These types of practices may face financial, human resource, or structural barriers that impede their ability to use their EHR to full capacity. We found that super-use was least prevalent in practices providing specialist-level care and services; it is possible that these practices are less well served by existing health IT functionalities and require specific tools developed for more specialized clinical scenarios.
Policy makers should consider how to address the barriers of the small, nonmetropolitan, and specialist practices to using their health IT functionalities more fully, as the relative under-use of these tools has far-reaching implications. First, suboptimal use of critical health IT functionalities may have direct relevance for the quality of care provided by an individual practice as part of routine patient care. Second, under-use of these technologies (such as health information exchange) may have consequences for the quality of care provided across the ambulatory care sector. Current policies, such as shared risk programs, encourage community-based strategies to avoid costly hospitalizations; similarly, value-based purchasing holds providers accountable for care delivered by multiple practitioners. It is also notable that the diversity of ambulatory care providers has expanded in recent years25; our sample included more than 50 types of ambulatory specialty services. This trend and the aforementioned policies suggest that communication and care coordination among ambulatory care providers is more crucial than ever.
Third, the interoperability of the broader digital health system is essential for the network benefits of health IT and EHR systems, yet differences in EHR capacity between the US hospital sector and ambulatory care are substantial. For example, transitions in care are a crucial task for both primary and tertiary health providers. The Office of the National Coordinator for Health Information Technology reported that approximately 49% of hospitals could generate a care summary document in 2014 (a low estimate that shows room for improvement)26; however, only 39% of ambulatory practices in our sample were able to create and transmit an equivalent report. Especially telling is the 2013 estimate that 77% of hospitals had the capacity to send laboratory results to ambulatory providers27 compared with the 49% of ambulatory practices that were able to communicate with hospitals for clinical information. Hospitals with advanced EHR systems are fundamentally limited if there are functional restrictions on their ability to interact with caregivers and organizations in the community setting
Limitations
This study has some limitations. First, we used 2014 reported data, and practices may have since expanded their health IT functionality. However, changes since this time are likely to be incremental only; given that we have focused on the “outliers” of EHR use, it is unlikely that there would be substantial alterations in the proportions of either super- or under-users. Second, this is the first publication using HIMSS ambulatory care data, and their validity has not been examined by the research community. However, many published studies have used the HIMSS hospital dataset,15–17 which utilizes the same sampling and survey methodology as the ambulatory practice survey that provided the data in our study. One such study describes this source as the “industry standard for information on EMR [electronic medical record] adoption.”18 Accordingly, a strength of our study is its presentation of the first-ever analysis of the corresponding data from HIMSS about ambulatory care health IT use. The HIMSS survey represents one of the most comprehensive assessments of use of health IT that currently exists; our study extended the current taxonomy of EHR systems well beyond that of “basic” and “comprehensive.” Finally, the survey includes only ambulatory practices that are affiliated with a health system. Given a presumed desire for system interoperability, we might expect greater use of some health IT functionalities (such as health information exchange) by the ambulatory practices in our sample compared with independent practices. The use of this subset, in conjunction with our focus on those practices with a preexisting operational EHR, suggests that our results may overestimate the true proportion of super-users in the broader ambulatory care setting and that the national rate is even lower; the reverse is also likely true for the estimates of under-users.
CONCLUSIONS
Although it is critical for ambulatory care practices to have the building block of the EHR, a substantial proportion of these practices use this technology only minimally, indicating there is capacity for significant improvement. It is important that policy makers and healthcare providers understand the limits of health IT functionality in ambulatory care practices, as strategies aimed at improving the coordination of care or those relying on the EHR as a vehicle for intervention may be hindered by the technological capacity of ambulatory care partners. We also suggest that policy makers identify the barriers limiting the use of these tools in ambulatory care (in particular those related to small, rural, and specialty practices) and consider how best to facilitate the full use of a range of EHR-based health IT functionalities. Investment in EHR-based health IT capacity of individual ambulatory practices will likely have benefits to providers across the ambulatory setting and to the performance of the broader health system.
TAKEAWAY POINTS.
As of 2014, 73% of ambulatory practices were not using electronic health record (EHR]-based functionalities to their full capability, and nearly 40% were classified as health information technology (IT) “under-users.”
Under-use of health IT in ambulatory care has implications for the ability of the health system as a whole to provide coordinated and efficient care.
Facilitating the full use of a range of health IT tools in the ambulatory setting may help the broader health system gain the full benefit of investments in EHR-based technologies.
Efforts to increase the use of health IT functionalities should focus on practices that are small, are located in nonmetropolitan areas, and provide specialty care.
Acknowledgments
The authors wish to thank Julie Lai and Julie Newell of RAND Health for their assistance in preparing the data and performing the GIS mapping.
Source of Funding: Support for this research was made possible by a Harkness Fellowship in Healthcare Policy and Practice (Dr Rumball-Smith), awarded by The Commonwealth Fund. This work was also supported, in whole or in part, through a cooperative agreement (1U19HS024067-01) between the RAND Corporation and the Agency for Healthcare Research and Quality. The content and opinions expressed in this publication are solely the responsibility of the authors and do not reflect the official position of the Agency, HHS, or the Commonwealth Fund or its directors, officers, or staff.
Appendix
eAppendix Table 1.
Distribution of Responses by EHR Domain and HIT Functionality
| Frequency (%) | Median (mean) | Range | Interquartile range | |
|---|---|---|---|---|
| Domain: Use of data repository capacity | 4 (6.1) | 1 – 12 | 1 – 11 | |
| Clinical research data analysis | 9542 (31.7) | |||
| Current encounter procedures | 13302 (44.2) | |||
| Current encounter vital signs including height, weight, blood pressure, temperature, etc | 12467 (41.4) | |||
| Nursing documentation | 18391 (61.1) | |||
| Physician documentation | 18206 (60.4) | |||
| Problem lists | 13251 (44.0) | |||
| Structured document templates (e.g. diabetic workup, annual physical, etc.) creating discrete data | 15269 (50.7) | |||
| Transcribed reports are stored electronically | 30123 (100.0) | |||
| Ability to create growth charts from the capture of structured data (vital signs, immunizations, BMI, etc.) | 12637 (42.0) | |||
| Ability to incorporate current encounter procedures into standardized format (e.g. CCD, CCR) | 12546 (41.6) | |||
| Medication lists on-line for all patients | 14011 (46.5) | |||
| Medication reconciliation | 13225 (43.9) | |||
| Domain: Clinical decision support | 2 (3.1) | 0 – 10 | 0 – 6 | |
| Basic medication screening (drug/drug, drug/allergy) | 16182 (53.7) | |||
| Clinical guidelines or protocols | 13551 (45.0) | |||
| Data from the community based EHR is incorporated into the EMR’s rules engine and triggers alerts | 5653 (18.8) | |||
| Genomics profiling is incorporated into the EMR and could result in a suggested order or order change | 1829 (6.1) | |||
| Preventive medicine (e.g. immunizations, follow-up testing) | 14805 (49.1) | |||
| Receipt of diagnostics results trigger relevant clinical alerts and clinical guidance/recommended care | 9018 (29.9) | |||
| Remote device monitoring process alerts clinician when clinically significant changes in data are detected | 4319 (14.3) | |||
| Capable of comparing patient follow-up recommendations to care rendered by all providers with access to the community-based EMR and variance and compliance alerts are generated | 5664 (18.8) | |||
| EMR suggests recommended follow-up based on date, patient problem list and procedures rendered by current provider and others. | 9894 (32.8) | |||
| Follow-up notices sent to the patients are initiated by flags set by provider | 11245 (37.3) | |||
| Domain: Order entry management | 2 (1.8) | 0 – 4 | 0 – 3 | |
| Ability to find and modify orders for all patients on a specific medication | 8824 (29.3) | |||
| e-Prescribing for new medications | 17281 (57.4) | |||
| e-Prescribing for refill medication requests | 16906 (56.1) | |||
| 75% or more orders completed in this way | 10720 (35.6) | |||
| Domain: Electronic messaging | 1 (2.0) | 0 – 5 | 0 – 5 | |
| Consult communications | 12494 (41.5) | |||
| Disease management communications | 8634 (28.7) | |||
| Internal clinic communications | 15545 (51.6) | |||
| Patient communications | 11120 (36.9) | |||
| Referral communications | 12620 (41.9) | |||
| Domain: Results management | 0 (1.03) | 0 – 3 | 0 – 2 | |
| All lab reports are electronically imported and stored in discrete structured form OR Textual/data results may be returned via HL 7 transactions and stored directly into patient records | 12716 (42.2) | |||
| Textual/data results returned electronically in formats such as PDF, CCR, and CCD, and then attached to patient record | 11183 (37.1) | |||
| Output from diagnostic and intelligent medical devices are incorporated directly into patient’s EMR when appropriate. | 7627 (25.3) | |||
| Domain: Health information exchange | 4 (5.3) | 1 – 13 | 1 – 10 | |
| Capable of exchanging data across multiple vendor platforms for the purpose of health information exchange | 10254 (34.0) | |||
| Web browser on physician/nurse desktops for access to online reference material, eligibility information, lab results, etc. | 30123 (100.0) | |||
| With external registries for reporting of patient data (e.g. immunization, disease or device) | 10087 (33.5) | |||
| With governmental agencies (e.g. local, county, state) | 11475 (38.1) | |||
| With hospitals for clinical information OR web-only access | 14663 (48.7) | |||
| With hospitals for demographic and insurance information | 13516 (44.9) | |||
| With internal disease registries lor case management | 5631 (18.7) | |||
| With other clinics for clinical information | 13585 (45.1) | |||
| With pharmacies or pharmacy clearinghouses (e.g. SureScripts) | 13636 (45.3) | |||
| With reference laboratories | 12149 (40.3) | |||
| With the Centers for Disease Control | 5286 (17.5) | |||
| Ability to transmit standardized format (e.g. CCD, CCR) or other standardized individual components of patient’s electronic record | 11680 (38.8) | |||
| Ability to update the patient’s EHR where there is a community-based HIE | 7983 (26.5) | |||
| Domain: Patient use | 1 (1.6) | 0 – 4 | 0 – 4 | |
| A patient portal allowing the patient to see personal health information, pay bills, request a schedule, request an appointment, etc. | 11663 (38.7) | |||
| Email communications with physicians or nurses | 12506 (41.5) | |||
| Patient Health Record | 10816 (35.9) | |||
| Patient specific medical education content | 12183 (40.4) | |||
All functionalities are questions taken verbatim from the Healthcare Information and Management Systems Society survey on ambulatory care practices. BMI = Body Mass Index, CCD = Continuity of Care Document; CCR = Continuity of Care Record; PDF = Portable Document Format; HL 7= Health Level 7 format; EHR = Electronic health Record; EMR = Electronic Medical Record; HIE = Health information Exchange.
Tables A2 and A3 show the descriptive characteristics of the practices, according to their super-user and under-user status of EHR-based HIT functionalities, and that of the total sample. Note that the super- and under- categories are not complementary; the majority of practices fall into the middle ‘unclassified’ category of being neither a super nor under-user. Also note that the significance of the p-values likely reflects the large sample size; differences between the groups may not be practically meaningful.
eAppendix Table 2.
Descriptive Characteristics of Ambulatory Care Practices Defined as Super-users of EHR-Based HIT Functionalities
| Super-user (%) | p | Total (%) | ||
|---|---|---|---|---|
| 8003 (26.6) | 30123 | |||
| Median, mean | 3,9.2 | < 0.0001 | 2,5.6 | |
| Size (number of associated physicians) | < 7 | 5303 (66.3) | < 0.0001 | 23324 (77.4) |
| 7–19 | 1146 (14.3) | 3415 (11.3) | ||
| 20–99 | 487 (6.1) | 1222 (4.1) | ||
| >100 | 1067 (13.3) | 2162 (7.2) | ||
| Practice Type | Primary | 2458 (30.7) | <0.0001 | 9289 (30.8) |
| Single or multiple specialty, allied health | 5116 (63.9) | 18823 (62.5) | ||
| Specialist services and urgent care | 429 (5.4) | 2011 (6.7) | ||
| Location | Rural | 222 (2.8) | <0.0001 | 1402 (4.7) |
| Small town | 355 (4.5) | 2234 (7.4) | ||
| Mid-size | 590 (7.4) | 3933 (13.1) | ||
| Metropolitan | 6833 (85.4) | 22518 (74.8) | ||
| Region | Northeast | 1310 (16.4) | <0.0001 | 6141 (20.4) |
| Midwest | 3264 (40.8) | 9756 (32.4) | ||
| South | 2496 (31.2) | 9767 (32.4) | ||
| West | 933 (11.7) | 4459 (14.8) |
P values calculated with Pearson’s χ2 for categorical variables, they estimate the statistical significance of differences in proportions between categories of practice variables in super-use practices compared to the total sample. Two-sided t test performed to test significance of difference in mean number of associated physicians. The analysis for the location excludes 36 practices which did not have an accurate zip code-rurality crosswalk.
eAppendix Table 3.
Descriptive Characteristics of Ambulatory Care Practices Defined as Under-users of EHR-Based HIT Functionalities
| Under-user (%) | p | Total (%) | ||
|---|---|---|---|---|
| 11706 (38.9) | 30123 | |||
| Median, mean | 2, 4.3 | < 0.0001 | 2, 5.6 | |
| Size (Number of associated physicians) | < 7 | 9465 (80.9) | < 0.0001 | 23324 (77.4) |
| 7–19 | 1142 (9.6) | 3415 (11.3) | ||
| 20–99 | 365 (3.1) | 1222 (4.1) | ||
| >100 | 734 (6.3) | 2162 (7.2) | ||
| Practice Type | Primary | 3534 (30.2) | < 0.0001 | 9289 (30.8) |
| Single or multiple specialty, allied health | 7267 (62.1) | 18823 (62.5) | ||
| Specialist services and urgent care | 905 (7.7) | 2011 (6.7) | ||
| Location | Rural | 640 (5.5) | <0.0001 | 1402 (4.7) |
| Small town | 1041 (8.9) | 2234 (7.4) | ||
| Mid-size | 1844 (15.8) | 3933 (13.1) | ||
| Metropolitan | 8179 (69.9) | 22518 (74.8) | ||
| Region | Northeast | 2556 (21.8) | <0.0001 | 6141 (20.4) |
| Midwest | 3042 (26.0) | 9756 (32.4) | ||
| South | 4089 (34.9) | 9767 (32.4) | ||
| West | 2019 (17.3) | 4459 (14.8) |
P values calculated with Pearson’s χ2 for categorical variables, they estimate the statistical significance of differences in proportions between categories of practice variables in under-use practices compared to the total sample. Two-sided t test was performed to test significance of difference in mean number of associated physicians. The analysis for the location excludes 36 practices which did not have an accurate zip code-rurality crosswalk.
Footnotes
Author Disclosures: The authors report no relationship or financial interest with any entity that would pose a conflict of interest with the subject matter of this article.
Contributor Information
Juliet Rumball-Smith, RAND Health, Santa Monica, CA; Northland District Health Board, Whangarei, New Zealand.
Paul Shekelle, RAND Health, Santa Monica, CA; General Internal Medicine, Greater Los Angeles VA Healthcare System, Los Angeles, CA..
Cheryl L. Damberg, RAND Health, Santa Monica, CA.
REFERENCES
- 1.American Recovery and Reinvestment Act of 2009, S 1, 111th Cong (2009).
- 2.Jamoom EW, Yang N, Hing E. Adoption of certified electronic health record systems and electronic information sharing in physician offices: United States, 2013 and 2014 NCHS data brief, no. 236. National Center for Health Statistics; website. cdc.gov/nchs/products/databriefs/db236.htm. Published January 2016 Accessed May 1, 2017. [PubMed] [Google Scholar]
- 3.Office-based physician electronic health record adoption. Office of the National Coordinator for Health Information Technology website. dashboard.healthit.gov/quickstats/pages/physician-ehr-adoption-trends.php. Published 2015 Accessed May 1, 2017.
- 4.Ancker JS, Kern LM, Edwards A, et al. ; HITEC Investigators. Associations between healthcare quality and use of electronic health record functions in ambulatory care. JAm Med Inform Assoc. 2015;22(4):864–871. doi: 10.1093/jamia/ocv030. [DOI] [PubMed] [Google Scholar]
- 5.Prgomet M, Li L, Niazkhani Z, Georgiou A, Westbrook JI. Impact of commercial computerized provider order entry (CPOE) and clinical decision support systems (CDSSs) on medication errors, length of stay, and mortality in intensive care units: a systematic review and meta-analysis. J Am Med Inform Assoc. 2017;24(2):413–422. doi: 10.1093/jamia/ocw145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jones SS, Rudin RS, Perry T, Shekelle PG. Health information technology: an updated systematic review with a focus on meaningful use. Ann Intern Med. 2014;160(1):48–54. doi: 10.7326/M13-1531. [DOI] [PubMed] [Google Scholar]
- 7.Fontaine P, Ross SE, Zink T, Schilling LM. Systematic review of health information exchange in primary care practices. J Am Board Fam Med. 2010;23(5):655–670. doi: 10.3122/jabfm.2010.05.090192. [DOI] [PubMed] [Google Scholar]
- 8.Schnipper JL, Gandhi TK, Wald JS, et al. Effects of an online personal health record on medication accuracy and safety: a cluster-randomized trial. J Am Med Inform Assoc. 2012;19(5):728–734. doi: 10.1136/amiajnl-2011-000723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Druss BG, Ji X, Glick G, von Esenwein SA. Randomized trial of an electronic personal health record for patients with serious mental illnesses. Am J Psychiatry. 2014;171(3):360–368. doi: 10.1176/appi.ajp.2013.13070913. [DOI] [PubMed] [Google Scholar]
- 10.Mishuris RG, Linder JA, Bates DW, Bitton A. Using electronic health record clinical decision support is associated with improved quality of care. Am J Manag Care. 2014;20(10):e445–e452. [PubMed] [Google Scholar]
- 11.Walker J, Pan E, Johnston D, Adler-Milstein J, Bates DW, Middleton B. The value of health care information exchange and interoperability. Health Aff (Millwood). 2005;(suppl Web exclusives):W5–W10, W15–W18. [DOI] [PubMed] [Google Scholar]
- 12.Linder JA, Ma J, Bates DW, Middleton B, Stafford RS. Electronic health record use and the quality of ambulatory care in the United States. Arch Intern Med. 2007;167(13):1400–1405. doi: 10.1001/archinte.167.13.1400. [DOI] [PubMed] [Google Scholar]
- 13.Krist AH, Beasley JW, Crosson JC, et al. Electronic health record functionality needed to better support primary care. J Am Med Inform Assoc. 2014;21(5):764–771. doi: 10.1136/amiajnl-2013-002229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Adler-Milstein J, DesRoches CM, Kralovec P, et al. Electronic health record adoption in US hospitals: progress continues, but challenges persist. Health Aff(Millwood). 2015;34(12):2174–2180. doi: 10.1377/hlthaff.2015.0992. [DOI] [PubMed] [Google Scholar]
- 15.Hillestad R, Bigelow J, Bower A, et al. Can electronic medical record systems transform health care? potential health benefits, savings, and costs. Health Aff (Millwood). 2005;24(5):1103–1117. doi: 10.1377/hlthaff.24.5.1103. [DOI] [PubMed] [Google Scholar]
- 16.McCullough JS, Parente S, Town R. Health information technology and patient outcomes: the role of organizational and informational complementarities. NBER working paper No. 18684. National Bureau of Economic Research website; nber.org/papers/w18684. Published January 2013 Accessed May 1, 2017. [Google Scholar]
- 17.Miller AR, Tucker C. Privacy protection and technology diffusion: the case of electronic medical records. ManagSci. 2009;55(7):1077–1093. doi: 10.1287/mnsc.1090.1014. [DOI] [Google Scholar]
- 18.Dranove D, Garthwaite C, Li B, Ody C. Investment subsidies and the adoption of electronic medical records in hospitals. J Health Econ. 2015;44:309–319. doi: 10.1016/j.jhealeco.2015.10.001. [DOI] [PubMed] [Google Scholar]
- 19.Furukawa MF, Raghu TS, Spaulding TJ, Vinze A. Adoption of health information technology for medication safety in U.S. hospitals, 2006. Health Aff (Millwood). 2008;27(3):865–875. doi: 10.1377/hlthaff.27.3.865. [DOI] [PubMed] [Google Scholar]
- 20.RUCA version 2.0. Rural Health Research Center website. ruralhealth.und.edu/ruca. Updated August 4, 2014 Accessed March 7, 2017.
- 21.Hsiao CJ, Hing E. Use and characteristics of electronic health record systems among office-based physician practices: United States, 2001–2013 NCHS data brief no. 143. National Center for Health Statistics website; cdc.gov/nchs/products/databriefs/db143.htm. Published January 2014 Accessed April 2017. [Google Scholar]
- 22.DesRoches CM, Campbell EG, Rao SR, et al. Electronic health records in ambulatory care—a national survey of physicians. N Engl J Med. 2008;359(1):50–60. doi: 10.1056/NEJMsa0802005. [DOI] [PubMed] [Google Scholar]
- 23.Boonstra A, Broekhuis M. Barriers to the acceptance of electronic medical records by physicians from systematic review to taxonomy and interventions. BMC Health Serv Res. 2010;10:231. doi: 10.1186/1472-6963-10-231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Adler-Milstein J, Salzberg C, Franz C, Orav EJ, Bates DW. The impact of electronic health records on ambulatory costs among Medicaid beneficiaries. Medicare Medicaid Res Rev. 2013;3(2):a03. doi: 10.5600/mmrr.003.02.a03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Johansen ME, Kircher SM, Huerta TR. Reexamining the ecology of medical care. N Engl J Med. 2016;374(5):495–496. doi: 10.1056/NEJMc1506109. [DOI] [PubMed] [Google Scholar]
- 26.Electronic health information exchange performance reported to the Medicare EHR incentive program, 2014. Office of the National Coordinator for Health Information Technology website; dashboard.healthit.gov/quickstats/pages/eligible-provider-electronic-hie-performance.php. Published September 2015 Accessed April 2017. [Google Scholar]
- 27.U.S. hospital adoption of computerized capabilities to meet Meaningful Use Stage 2 objectives. Office of the National Coordinator for Health Information Technology website; dashboard.healthit.gov/quickstats/pages/FIG-Hospital-Adoption-Meaningful-Use-Stage-Two-2013.php. Published April 2014 Accessed March 5, 2017. [Google Scholar]