Abstract
Food parenting practices and parenting styles are associated with child weight status, dietary intake, and eating behaviors. Although parents maintain a parenting style while also engaging in food parenting practices day-to-day, most studies have examined the separate impact of these two constructs on child outcomes. An examination of both practices and styles will facilitate the identification of how they mutually co-exist and influence child weight and weight-related outcomes. The current study examined the clustering of food parenting practices and parenting styles and evaluated the relationship between these parenting characteristics and child weight status, diet quality and eating behaviors. Children aged 5–7 and their parents (N = 150) from six racial/ethnic groups were recruited through primary care clinics. Latent class analysis classified subgroups based on parenting practices and styles. Regression analyses examined relationships between subgroups and child outcomes. The best-fitting model was two subgroups. Parents in subgroup 1 (n = 37) were more likely to restrict foods, pressure children to eat and less likely to engage in food modeling compared to subgroup 2 (n = 112). Parents in subgroup 1 were more likely to report authoritarian and permissive parenting styles and less likely to report an authoritative parenting style, compared to subgroup 2. Parents in subgroup 1 were more likely to report children who ate to obtain pleasure and who lacked internal cues for hunger than those in subgroup 2. There were no association between subgroups and child weight status, diet quality and other eating behaviors. Future research and interventions should take into consideration how parenting styles and practices mutually influence child weight and weight-related outcomes.
Keywords: latent class analysis, parenting styles, parenting practices, eating, behaviors, child weight
Introduction
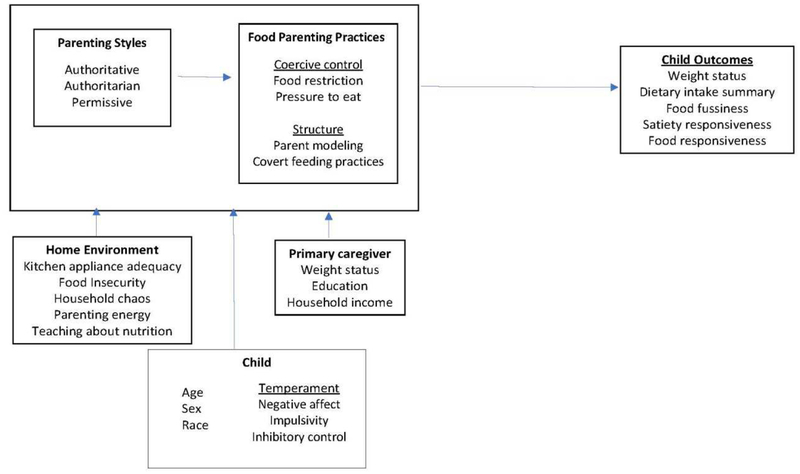
A growing body of evidence suggests that food parenting practices and parenting styles are significant correlates of weight status and eating behaviors in youth (Berge, Wall, Loth, & Neumark-Sztainer, 2010; Vaughn et al., 2016; Yee, Lwin, & Ho, 2017). Parenting styles refer to emotional and relational aspects of parents and are based on the degree of responsiveness and the degree of demandingness of the parent (Maccoby, 1992). The four classic parenting styles are: authoritative (high responsiveness, high demandingness), authoritarian (low responsiveness, high demandingness), permissive (high responsiveness, low demandingness), and neglectful (low responsiveness, low demandingness)(Maccoby, 1992). Review papers have found an association between specific parenting styles and child weight-related outcomes (Berge, 2009; Pinquart, 2014; Vollmer & Mobley, 2013). Specifically, studies suggest an association between authoritative parenting style (high responsiveness, high demandingness) and lower child weight status, healthy dietary intake and physical activity. Parenting practices refer to context-specific behaviors or actions of parents for child-rearing purposes that influence children’s attitudes, behaviors, or beliefs (Vaughn et al., 2016). Thus, food parenting practices refer to feeding-specific behaviors or actions of parents. Recent content and concept maps of fundamental food parenting practices constructs define three higher-order constructs: coercive control, structure, and autonomy support; and each higher-order construct consists of subconstructs (O’Connor et al., 2017; Vaughn et al., 2016). For example, pressure to eat and restriction are subconstructs of coercive control; nutrition support is a subconstruct of autonomy support; and, parental modeling and covert feeding practices are subconstructs of structure. Covert feeding practices refers to controlling food intake in a way that is undetected by the child such as not purchasing unhealthy foods or avoiding specific restaurants (Ogden, Reynolds, & Smith, 2006). Figure 1 illustrates individual, dyadic, and familial factors (e.g., parenting styles and practices) that may influence child health behaviors and weight status.
Figure 1.
Conceptual Framework
Reviews of the existing literature suggest that the food parenting practice constructs and subconstructs described in Vaughn’s construct table significantly influence child eating behaviors and weight status (Vaughn et al., 2016; Yee et al., 2017). Indeed, most of the constructs in Vaughn’s construct map have been found to be either positively or negatively associated with child weight-related outcomes. For example, studies consistently found that parental modeling was positively associated with child healthy dietary intake, and pressure to eat was negatively associated with child weight status and healthy dietary intake but had a positive correlation with unhealthy food consumption. Most studies also found a positive relationship between restriction and child desire for restricted foods, tendency to overeat, intake of snack foods, and adiposity. Unfortunately, studies tend to examine the relationship between parenting practices and one specific child outcome, and do not explore how parenting practices influence a variety of child outcomes. Thus, an examination of more than one child outcome will provide knowledge about how parenting practices uniquely influence various child outcomes. For example, it is possible that covert feeding practices impact child eating behaviors but not weight status. Knowledge about various food parenting practices and child outcomes may lead to novel interventions that are more individualized based on parental characteristics and targeted child outcome.
Research to date has examined specific food parenting practices or parenting styles with child outcomes, but these studies rarely explore how food parenting practices and parenting styles jointly impact child outcomes. For example, researchers have found that food parenting practices are dynamic and that there is an interplay among different practices (Loth, Uy, Neumark-Sztainer, Fisher, & Berge, 2018; Wiggins, Potter, & Wildsmith, 2001). In addition, another study recently showed that parent feeding practices are more state-like than trait-like and fluctuate throughout the day and across the week (Berge, Tate, Trofholz, Loth, et al., 2018). Furthermore, recent review papers argued that parenting styles are more trait-like compared to parenting practices which are less static, and that exploring the interaction of parenting styles and practices may improve intervention efficacy (Kremers et al., 2013; Patrick, Hennessy, McSpadden, & Oh, 2013). Given that all parents engage in multiple food parenting practices within the context of their own parenting style, an examination of both parenting practices and styles will provide knowledge of whether certain food parenting practices align with certain parenting styles. For example, it is possible that more coercive control practices exist alongside specific parenting styles and the co-occurrence of coercive control practices which in turn influences child weight and weight-related behaviors (e.g., dietary intake, physical activity, sedentary behavior). Such knowledge may lead to more real-world recommendations for parents and more efficacious interventions.
In the current study, latent profile analysis was used to examine the clustering of parenting styles and multiple food parenting practices among a cohort of racially, ethnically and socioeconomically diverse families. Latent profile analysis is a statistical approach that evaluates unobserved population heterogeneity and addresses the question: “Can individuals from a heterogenous population be divided into clinically meaningful subgroups?”. One of the primary advantages of this analytic approach is that subgroups are created to maximize homogeneity within groups and are based on observed data used to model theoretical concepts which are not directly measured (Lubke & Muthen, 2005). For example, latent profile analysis may lead to the identification of a common set of food parenting practices and parenting styles associated with healthful child outcomes. Such knowledge may inform interventions that move parents towards the approach with best outcomes and possibly detect parents at greater risk of engaging in food parenting practices that negatively impact child outcomes. In this context, the study addressed the following research questions: (a) Are there unique latent profiles (subgroups) based on food parenting practices (i.e., restriction, pressure to eat, modeling, covert feeding practices) and parenting styles (i.e., permissive, authoritarian, authoritative)? (b) What are the differences and similarities of the latent profiles in food parenting practices and parenting styles? (c) Do latent profiles predict child outcomes (i.e., weight status, healthy dietary intake, eating behaviors)?
Materials and Methods
Study Design and Population
Data in the current study are from the Family Matters study, a 5-year incremental (Phase I = 2014 – 2016; Phase II: 2017 – 2019), mix-methods, longitudinal study designed to identify factors in the home environment that may be risk and protective factors for childhood obesity. Phase I included an in-depth, mixed-methods, cross-sectional analysis of the home environment for children ages 5 to 7 years from six racial and/ or ethnic groups including African American, Hispanic/Latino, Hmong, Native American, Somali, and white (N = 150; n = 25 per group). The sample was intentionally stratified by race/ethnicity and weight status (overweight/obese = body mass index (BMI) ≥ 85%ile; non-overweight = BMI > 5%ile and < 85%ile) of the study child. Additionally, families were from low-income households (Department of Human and Health Services, 2019), with 70% of families earning less than $35,000 per year.
Eligible children and parents were recruited from primary care clinics within Minneapolis and St. Paul, Minnesota. Potential participants received a phone call (in their own language) within two weeks after recruitment letters had been sent from their clinic to confirm receipt of recruitment letter, answer any questions, review eligibility requirements, and invite study participation. Eligible families participated in two in-home visits over a 10-day period. During the first home visit, written consent/assent were obtained from caregivers and children. In-depth information about the recruitment and eligibility criteria and the procedures and data collection have been published elsewhere (Berge, Trofholz, et al., 2017). Of the original sample, one child/family did not have scores for food parenting practices and was excluded from the current study. The University of Minnesota’s Institutional Review Board Human Subjects Committee approved all protocols used in the Family Matters study.
Measures
Details about study variables (e.g., definition, measure) are described in Table 1.
Table 1.
Description of Study Variables
| Study Variables | Definition | M (SD) | Description |
|---|---|---|---|
| Indicators | |||
| Food restriction1 | Extent to which parents restrict child’s access to foods | 19.11 (6.56) Range: 6–30 |
Constructed from 6 items : 1) “I have to watch out that my child does not eat too many sweets (candy, ice cream, cake, or pastries),” 2) “I have to watch out that my child does not eat too many high-fat foods,” 3) “I have to watch out that my child does not eat too much of his/her favorite foods,” 4) “I intentionally keep some foods out of my child’s reach,” 5) “if I do not guide or regulate my child’s eating, he/she would eat too much of his/her favorite foods,” and 6) “if I do not guide or regulate my child’s eating, he/she would eat too many junk foods.” Higher scores indicating higher restriction. |
| Pressure to eat1 | Parents’ tendency to pressure their children to eat more food | 11.45 (3.91) Range: 4–20 |
Constructed from 4 items: 1) “my child should always eat all of the food on his/her plate,” 2) “I have to be especially careful to make sure my child eats enough,” 3) “if my child says ‘I’m not hungry,’ I try to get him/her to eat anyway,” and 4) if I do not guide or regulate my child’s eating, he/she would eat much less than he/she should.” Higher scores indicating higher pressure to eat. |
| Covert feeding practices2 | Controlling food intake in a way that is undetected by the child | 20.58 (6.05) Range: 7–34 |
Constructed from 7 items: 1) “How often do you avoid going to restaurants or fast food places which sell unhealthy foods with your child?”, 2) “How often do you avoid buying candy and chips to avoid bringing them into the house?”, 3) “How often do you not buy foods that you would like because you do not want your child to have them?”, 4) How often do you try not to eat unhealthy foods when your child is around?”, 5) “How often do you avoid buying cookies, candy, and other treats to avoid bringing them into the house?”, 6) “How often do you avoid having snack foods such as candy and chips in the house?”, and 7) “How often do you avoid having unhealthy foods in the house?”. Higher score indicating higher covert feeding practices. |
| Parent food modeling2 | Parent modeling of healthy food behaviors | 12.33 (2.54) Range: 5–15 |
Constructed from 3 items: 1) “I model healthy eating for my child by eating healthy foods myself,” 2) “I try to eat healthy foods in front of my child, even if they are not my favorite,” and 3) “I show my child how much I enjoy eating healthy foods.” Higher score indicates higher food modeling. |
| Authoritative parenting style3 | Style of parenting that involves warmth & involvement, reasoning/induction, democratic participation, and good- nature/easy-going (high responsiveness, high demandingness) | 15.37(2.78) Range: 8–20 |
Constructed from 4 items: 1) “I know the names of my child’s friends,” 2) “I explain the consequences of my child’s behavior,” 3) “I show patience with my child,” and 4) “I take into account my child’s preferences in making plans for the family.” Higher scores indicating a more authoritative parenting style. |
| Authoritarian parenting style3 | Style of parenting that involves verbal hostility, corporal punishment, nonreasoning/punitive strategies, and directiveness (low responsiveness, high demandingness) | 9.19(2.61) Range: 5–16 |
Constructed from 4 items: 1) “I yell or shout when my child misbehaves,” 2) “I use physical punishment as a way of disciplining my child,” 3) “I punish by taking privileges away from my child with little, if any explanation,” and 4) “I tell my child what to do.” Higher scores indicating a more authoritarian parenting style. |
| Permissive parenting style3 | Style of parenting that involves lack of follow through, ignoring of misbehaviors, and self- confidence (high responsiveness, low demandingness) | 5.76 (2.11) Range: 3–13 |
Constructed from 3 items: 1) “I threaten my child with punishment more often than I actually punish him/her,” 2) “I ignore my child’s misbehavior,” and 3) “I find it difficult to discipline my child.” Higher scores indicating a more permissive parenting style. |
| Child Outcomes | |||
| Food fussiness4 | Being highly selective about the range of foods that are accepted | 16.49 (4.17) Range: 8–30 |
Constructed from 6 items: 1) “my child refuses new foods at first,” 2) “my child enjoys tasting new foods,” 3) “my child enjoys a wide variety of foods,” 4) “my child is difficult to please with meals,” 5) “my child is interested in tasting food he/she hasn’t tasted before,” and 6) my child decides that he/she doesn’t like food even without tasting it.” Three items were reverse coded, and then a score was calculated by summing responses. Higher scores indicate higher food fussiness. |
| Satiety responsiveness4 | Ability to regulate intake of food in relation to satiety | 13.87 (2.91) Range: 6–23 |
Constructed from 5 items:: 1) “my child has a big appetite,” 2) “my child leaves food on his/her plate at the end of a meal,” 3) “my child gets full before his/her meal is finished,” 4) my child cannot eat a meal if he/she has had a snack just before,” and 5) “my child gets full easily.” One item was reverse coded, and then a score was calculated by summing responses. Higher scores indicate higher satiety responsiveness |
| Food responsiveness4 | Susceptibility to the hedonistic qualities of food and lack of internal cues for hunger | 12.49 (3.96) Range: 5–24 |
Constructed from 5 items: 1) “my child is always asking for food,” 2) “given the choice, my child would eat most of the time,” 3) “even if my child is full he/she finds room to eat his/her favorite food,” 4) if given the chance my child would always have food in his/her mouth,” and 5) “if allowed to, my child would eat too much.” A score was calculated by summing responses. Higher score indicates higher food responsiveness. |
| Child’s dietary quality5 | Healthfulness of child dietary intake summary | 57.11 (9.37) Range: 31.18–76.74 |
Constructed from 12 components. Nine components assess adequacy of the diet: (1) total fruit (0–5 points); (2) whole fruit (0–5 points); (3) total vegetables (0–5 points); (4) greens and beans (0–5 points); (5) whole grains (0–10 points); (6) dairy (0–10 points); (7) total protein foods (0–5 points); (8) seafood and plant proteins (0–5 points); and (9) fatty acids (0–10 points). Higher scores reflect higher intake which are desirable. Three components assess food groups and dietary elements that should be consumed in moderation: (10) refined grains (0–10 points); (11) sodium (0–10 points); and (12) empty calories (i.e., energy from solid fats, alcohol, and added sugars; (0–20 points). Higher scores reflect lower intake which are desirable. |
| Child’s weight status | Sex- and age-specific cutoffs were used to classify children as overweight/obese (body mass index [BMI] > 85%ile) or nonoverweight (> 5%ile < 85%ile) (Himes & Dietz, 1994; Kuczmarski et al., 2000). | 75.78 (23.14) Range: 5–99 |
Constructed from child heights and weights which were converted to child body mass index percentile, using Centers for Disease Control and Prevention (CDC) criteria (Kuczmarski et al., 2000). |
| Validation Variables | |||
| Demographic characteristics6 | All demographic variables were based on responses to demographics survey including primary caregiver’s BMI, education, household income, and child’s age, sex and race | Primary caregiver’s BMI was calculated using parent’s reported height and weight, and weight status was classified based on the CDC descriptions (CDC, 2015). | |
| Negative affect (child temperament)7 | Amount of negative affect related to interruption of ongoing tasks or goal blocking | 19.36 (6.82) Range: 1–35 |
Constructed from 5 items: 1) “my child gets quite frustrated when prevented from doing something she/he wants to do”; 2) “my child is quite upset by a little cut or bruise”; 3) “my child tends to become sad if the family’s plans don’t work out”; 4) “when angry about something, my child tends to stay upset for ten minutes or longer”; 5) “my child is NOT afraid of the dark”. One item was reverse coded, and then a score was calculated by summing responses. Higher scores indicate higher negative affect. |
| Impulsivity (child temperament)7 | Speed of response initiation | 16.61 (4.70) Range: 4–27 |
Constructed from 4 items: 1) “my child often rushes into new situations”; 2) “my child seems to be at ease with almost any person”; 3) “my child seems always in a big hurry to get from one place to another”; 4) “my child likes going down high slides or other adventurous activities”. A score was calculated by summing responses. Higher scores indicate higher impulsivity. |
| Inhibitory control (child temperament)7 | Capacity to plan and to suppress inappropriate approach responses under instructions or in novel or uncertain situations | 22.00 (4.39) Range: 4–28 |
Constructed from 4 items: 1) “my child is good at following instructions”; 2) “my child when drawing or coloring in a book, shows strong concentration”; 3) “my child likes the sound of words, such as nursery rhymes”; 4) “my child comments when a parent has changed his/her appearance”. A score was calculated by summing responses. Higher scores indicate higher effortful control. |
| Food insecurity scale8 | Financially-based food insecurity and hunger | 0.85 (1.76) Range: 0–6 |
Constructed from 1) “In the last 12 months, did you (or other adults in your household) ever cut the size of your meals or skip meals because there wasn’t enough money for food?”; 2) “How often did this happen?” (recoded: 1 or 2 = 1, and 3=0); 3) “In the last 12 months, did you ever eat less than you felt you should because there wasn’t enough money to buy food?”; 4) “In the last 12 months, were you ever hungry but didn’t eat because you couldn’t afford enough food?”; 5) “In the last 12 months, the food that we bought just didn’t last, and we didn’t have money to get more”; 6) “In the last 12 months, we couldn’t afford to eat balanced meals”. All 6 are summed to create scale and then the scale is used to create categories (0–1 = high or marginal food security, 2–4: low food security, 5–6: very low food security). |
| Kitchen appliance adequacy9 | Availability of food preparation supplies used for various aspects of food preparation | 17.32 (2.56) Range: 3–19 |
Constructed from yes/no responses to “Do you currently have a (appliance) in working condition in your home? Appliances include: stove, refrigerator, microwave, freezer, large spoon, spatula, can opener, knife, colander, measuring cup, cutting board, measuring spoons, peeler, grater, oven mitt, skillet, saucepan, baking pan, and bowl. All 19 are summed to create scale. Higher scores indicate higher kitchen appliance adequacy. |
| Household chaos10 | Degree of environmental confusion (i.e., disorganization and hurriedness) | 7.60 (2.66) Range: 4–16 |
Constructed from 1) “We almost always seem to be rushed”, 2) “It’s a real zoo in our home”; 3) “No matter what our family plans, it usually doesn’t seem to work out”; 4) “You can’t hear yourself think in our home”. A score was calculated by summing responses. Higher scores indicate higher household chaos. |
| Parenting energy11 | Time scarcity and fatigue as a barrier to planning/preparing meals | 1.36 (0.70) Range: 1–4 |
Constructed from response to the following: “I do not have enough time or energy to feed my child ‘right’” |
| Teaching about nutrition12 | Extent to which parents try to teach children about nutrition | 11.90 (2.20) Range: 7–15 |
Constructed from 1) “I discuss with my child why it’s important to eat healthy foods”; 2) “I discuss with my child the nutritional value of foods”; 3) “I tell my child what to eat and what not to eat without explanation” (reverse coded). All 3 are summed to create scale. A higher score indicates higher parent teaching about nutrition. |
Note:
Child Feeding Questionnaire (Birch et al., 2001);
adapted from previous studies (Berge, Trofholz, et al., 2017; Ogden et al., 2006);
Parenting Practices Questionnaire (Robinson et al., 1995);
Child’s Eating Behavior Questionnaire (Wardle, Guthrie, Sanderson, & Rapoport, 2001);
Healthy Eating Index-2010 scores (Guenther et al., 2014);
Demographics Survey;
Children’s Behavior Questionnaire (Rothbart, Ahadi, Hershey, & Fisher, 2001);
Short Form of the Household Food Security Scale (Blumberg, Bialostosky, Hamilton, & Briefel, 1999);
Food Preparation Checklist (Appelhans, Waring, Schneider, & Pagoto, 2014);
adapted from Confusion, Hubbub, and Order Scale (CHAOS)(Matheny, Wachs, Ludwig, & Phillips, 1995);
adapted from previous studies (Storfer-Isser & Musher-Eizenman, 2013);
adapted from Comprehensive Feeding Practices Questionnaire (Musher-Eizenman & Holub, 2007).
The current study did not assess for neglectful parenting style, a fourth parenting style which has been measured in other literature, because prior research has shown that this parenting style has low prevalence (Berge, Wall, Bauer, & Neumark-Sztainer, 2010; Berge, Wall, Loth, et al., 2010). Secondly, child diet quality, was calculated from three 24-hour dietary recall interviews conducted with the primary caregiver using the Nutrition Data System for Research system, developed by the Nutrition Coordinating Center, University of Minnesota, Minneapolis, MN (Center, 2016; Schakel, Buzzard, & Gebhardt, 1997; Schakel & Himes, 2001; Schakel, Sievert, & Buzzard, 1988). Finally, validation variables were selected based on prior empirical support for associations with parenting practices and styles as well as expert opinion among coauthors of clinical relevance. Validation analyses served two purposes: (1) examination of correlates that may support clinical validity of latent profiles, and (2) description of latent profiles. For example, emotional atmosphere (i.e., chaotic) has been shown to be a predictor of restriction feeding practices during a meal (Berge, Tate, Trofholz, Loth, et al., 2018), and primary caregiver’s level of education was included for descriptive purpose.
Statistical Analyses
Latent profile analysis.
Latent profile analysis, an extension of latent class analysis that allows for the use of continuous “indicator” variables, was used to determine the optimal number and composition in which participants aggregated based on food parenting practices (food restriction, pressure to eat, parent modeling, covert feeding practices) and parenting styles (authoritative, authoritarian, and permissive)(Muthén & Muthén, 1998–2015). An advantage of this analytic approach is that objective criteria (e.g., parsimony indices) are used to evaluate the existence of meaningful subgroups, or latent profiles, including optimal number and composition (Lubke & Muthen, 2005). Since there is not an a priori assumption (e.g., it is not known beforehand which participant belongs to which subgroup), observed data are used to model theoretical concepts which cannot be directly measured (Lubke & Muthen, 2005). These observed data, or indicators, used to characterize latent profiles were selected based on prior theoretical evidence (Vaughn et al., 2016; Yee et al., 2017). Correlations among indicators were small to moderate (rs ranged from .004 for food restriction with parent modeling to .53 for teaching about nutrition with parent modeling), indicating the assumption of conditional independence was likely met.
Analyses were conducted in Mplus Version 7 (Muthén & Muthén, 1998–2015). In this study, latent profile analysis was utilized to create a more representative measurement of feeding-related parenting by combining food parenting practices and styles into exclusive latent profiles. Individuals were assigned to one of the latent profiles based on their highest posterior probability of profile membership derived from responses to the indicators. We tested the fit of a series of models, ranging from one to six profiles, to the observed data. To approximate the best-fitting model, or correct number of classes, we compared standard fit indices including the Akaike Information Criterion, consistent Akaike Information Criterion, Bayesian Information Criterion, sample-size adjusted Bayesian Information Criterion, Bayes factor, bootstrap likelihood ratio test; Vuong-Lo-Mendell-Rubin adjusted likelihood ratio test, and entropy (Nylund-Gibson & Choi, 2018). We also examined the mean posterior probability of each latent profile (a profile-specific measure of how well the observed variables predict latent profile membership).
Validation analyses compared groups on demographic characteristics, child temperament, household factors and general parenting practices. Analyses were conducted using analyses of variance or Fisher’s Exact test.
Multiple regression models were used to examine the relationship between child dietary intake summary and eating behaviors and latent profiles based on food parenting practices and parenting styles. Logistic regression model was used to examine the relationship between child weight status (non-overweight versus overweight/obese status) and latent profiles based on food parenting practices and parenting styles. All models were controlled for the potential confounders of parent age and weight status, child age, sex and race/ethnicity, and household income and structure. All analyses were conducted in SPSS© software version 22 (IBM, Released 2013).
Results
Latent Profile Analysis
As shown in Table 2, the two-group solution had a higher sample-size adjusted Bayesian Information Criterion compared to other solutions (better fit is associated with lower score) but also had the lowest values for parameters, consistent Akaike Information Criterion and Bayesian Information Criterion as well as the highest value for entropy. Moreover, the two likelihood-based tests (i.e., bootstrap likelihood ratio test; Vuong-Lo-Mendell-Rubin adjusted likelihood ratio test) and the Bayes factor, or the pairwise comparison of fit between two neighboring class models, supported a two-group model.
Table 2.
Model Fit Statistics for Latent Profile Analyses (LCA)
| LCA | Log L | Parameters | AIC | cAIC | BIC | aBIC | BF | BLRT p | VLMR-LRT p | Entropy |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | −2773.71 | 14 | 5575.43 | 5631.48 | 5617.48 | 5573.18 | 0.00 | – | – | – |
| 2 | −2734.78 | 22 | 5513.56 | 5601.64 | 5579.64 | 5510.02 | 8.94 | <.001 | .004 | .833 |
| 3 | −2716.95 | 30 | 5493.89 | 5614.01 | 5584.01 | 5489.07 | >15.00 | <.001 | .51 | .739 |
| 4 | −2706.92 | 38 | 5489.84 | 5641.99 | 5603.99 | 5483.73 | >15.00 | .25 | .68 | .701 |
| 5 | −2694.77 | 46 | 5481.53 | 5665.72 | 5619.72 | 5474.14 | >15.00 | .04 | .03 | .786 |
| 6 | −2684.74 | 54 | 5477.49 | 5693.69 | 5639.69 | 5468.80 | – | .60 | .51 | .831 |
Note: AIC = Akaike Information Criterion; aBIC = adjusted BIC; BIC = Bayesian Information Criterion; BF = Bayes factor; BLRT = bootstrap likelihood ratio test; cAIC = consistent AIC; p = p-value; VLMR-LRT = Vuong-Lo-Mendell-Rubin adjusted likelihood ratio test. Bold values indicate “best” fit for each respective statistic.
Although fit indices did not converge on a single model, which is common, the likelihood and pairwise comparison of fit tests, parsimony, and two of the information criteria supported the two-group model (Nylund-Gibson & Choi, 2018). These results suggest that two subgroups, or latent profiles, within this population fit the data best and provide the clearest delineation of latent profiles based on food parenting practices and parenting styles.
Table 3 provides the average posterior probabilities associated with latent profiles to which individuals were assigned, and values indicate the probability that a parent belongs to the assigned latent profile and no other latent profile (posterior probability).
Table 3.
Means for the Posterior Probabilities Associated with the Two-Profile Model
| Latent Profile | N | 1 | 2 |
|---|---|---|---|
| 1 | 37 | .92 | .08 |
| 2 | 112 | .03 | .97 |
Note. Posterior probabilities are the probability that an individual belongs to the assigned profile and to no other profiles. Values are the average posterior probabilities associated with the profiles to which individuals were assigned.
Based on posterior probability of profile membership for each parent, parents were assigned into one of the two profiles, with 37 parents being assigned to latent profile 1 (LP1) and 112 parents being assigned to latent profile 2 (LP2). For parents assigned to LP1, the mean score for parenting practices were: 21.76 (SD = 5.24) for food restriction, 13.16 (SD = 4.02) for pressure to eat, 11.54 (SD = 2.80) for parent modeling, and 19.92 (SD = 5.64) for covert feeding practices. Regarding parenting styles, the mean scores were 14.14 (SD = 2.75) for authoritative, 11.92 (SD = 1.85) for authoritarian, and 8.35 (SD = 1.48) for permissive. Compared to LP1, parents assigned to LP2 had lower mean scores on food restriction and pressure to eat, 18.24 (SD = 6.74 and 10.88 (SD = 3.71), respectively; and, higher scores on parent modeling and covert feeding practices, 12.59 (SD = 2.41) and 20.80 (SD = 6.19), respectively. For parenting styles, the means scores for LP2 were 15.78 (SD = 2.68) for authoritative, 8.29 (SD = 2.16) for authoritarian, and 4.63 (SD = 1.33) for permissive. Table 4 presents comparisons between the two latent profiles on indicator variables (food parenting practices and parenting styles).
Table 4.
Distribution of Food Parenting Practices and General Parenting Styles between Latent Profiles
| Latent Profile 1 (n = 37) | Latent Profile 2 (n=112) | Test Statistic | |||||
|---|---|---|---|---|---|---|---|
| Variable | M | SD | M | SD | F | p | Effect size |
| Food restriction | 21.76 | 5.24 | 18.24 | 6.74 | 8.39 | .004 | .05 |
| Pressure to eat | 13.16 | 4.02 | 10.88 | 3.71 | 10.04 | .002 | .06 |
| Parent modeling | 11.54 | 2.80 | 12.59 | 2.41 | 4.85 | .03 | .03 |
| Covert feeding practices | 19.92 | 5.64 | 20.80 | 6.19 | .59 | .44 | |
| Parenting styles | |||||||
| Authoritative | 14.14 | 2.75 | 15.78 | 2.68 | 10.30 | .002 | .07 |
| Authoritarian | 11.92 | 1.85 | 8.29 | 2.16 | 84.11 | < .001 | .36 |
| Permissive | 8.35 | 1.48 | 4.63 | 1.33 | 205.88 | < .001 | .58 |
Note: Effect sizes for ANOVAs are partial η2.
Parents assigned to LP1 had higher scores on food restriction, F(1, 147) = 8.39, p = .004, partial η2 = .05 and pressure to eat, F(1, 147) = 10.04, p = .002, partial η2 = .056, and lower scores on parent modeling, F(1, 147) = 4.85, p = .03, partial η2 = .03, compared to those assigned to LP2. In other words, parents in LP1 were more likely to restrict certain foods offered to child and pressure child to eat, and less likely to engage in food modeling, compared to parents in LP2. However, effect sizes were small (< .1). Regarding parenting styles, parents in LP1 had higher scores on authoritarian, F(1, 147) = 84.11, p < .001, partial η2 = .36, and permissive, F(1, 147) = 205.88, p < .001, partial η2 = .58, and lower scores on authoritative, F(1, 147) = 10.30, p = .002, partial η2 = .07, compared to parents in LP2. These findings suggest that parents in LP1 were more likely to report permissive and authoritarian parenting and less likely to report authoritative parenting, compared to those in LP2. Going forward, LP1 will be referred to as, “Authoritarian and Permissive Parenting Style and Controlling Feeding Practices” and LP2 will be referred to as “Authoritative Parenting Style and Less Controlling Feeding Practices.” Controlling Feeding Practices refers to restricting foods offered to the child and pressuring the child to eat. Effect sizes were moderate for permissive and authoritarian parenting, and small for authoritative parenting.
Validation Analyses
Tables 5 and 6 present distributions of demographic characteristics, child temperament, household factors and general parenting practices between latent profiles.
Table 5.
Distribution of Demographics Characteristics between Latent Profiles
| Latent Profile 1 (n = 37) | Latent Profile 2 (n=112) | Test Statistic | |||||
|---|---|---|---|---|---|---|---|
| Variable | M | SD | M | SD | F | p | ES |
| Child’s age in years | 6.30 | .74 | 6.43 | .82 | .78 | .38 | |
| Primary caregiver’s body mass index | 32.92 | 7.34 | 30.09 | 7.09 | 4.34 | .04 | .03 |
| N | % | n | % | Fisher’s Exact p | |||
| Child | |||||||
| Sex (female) | 17 | 46 | 53 | 47 | .99 | ||
| Race | |||||||
| White | 2 | 8 | 22 | 20 | .10 | ||
| Black | 11 | 30 | 13 | 12 | |||
| Hispanic | 8 | 22 | 17 | 15 | |||
| Hmong | 4 | 11 | 21 | 19 | |||
| Native American | 5 | 14 | 20 | 18 | |||
| Somali | 6 | 16 | 19 | 17 | |||
| Primary Caregiver | |||||||
| Education | |||||||
| Middle school or junior high | 7 | 19 | 8 | 7 | .13 | ||
| Some high school | 3 | 8 | 14 | 13 | |||
| High school or GED | 16 | 43 | 44 | 39 | |||
| Vocational, technical, trade, or other certification program | 7 | 19 | 10 | 9 | |||
| Associate degree | 2 | 5 | 9 | 8 | |||
| Bachelor’s degree | 1 | 3 | 10 | 9 | |||
| Graduate or professional degree | 1 | 3 | 13 | 12 | |||
| Other | 0 | 0 | 4 | 4 | |||
| Income | |||||||
| Less than $20,000 | 15 | 41 | 35 | 31 | .88 | ||
| $20,000–$34,000 | 14 | 38 | 41 | 37 | |||
| $35,000–$49.999 | 3 | 8 | 13 | 12 | |||
| $50,000–$74,999 | 3 | 8 | 9 | 8 | |||
| $75,000–$99,999 | 1 | 3 | 6 | 5 | |||
| $100,000 or more | 1 | 3 | 8 | 7 | |||
| Weight status | |||||||
| Non-overweight | 3 | 8 | 32 | 29 | .03 | ||
| Overweight | 10 | 27 | 28 | 25 | |||
| Obese | 24 | 65 | 52 | 46 | |||
Note: ES = effect size. Effect sizes for ANOVAs are partial η2.
Table 6.
Distribution of Child Temperament, Household Factors, and General Parenting between Latent Profiles
| Latent Profile 1 (n = 37) | Latent Profile 2 (n = 112) | Test Statistic | |||||
|---|---|---|---|---|---|---|---|
| Variable | M | SD | M | SD | F | p | ES |
| Child Temperament | |||||||
| Negative affect | 22.73 | 6.14 | 18.24 | 6.69 | 13.02 | < .001 | .08 |
| Impulsivity | 17.89 | 4.45 | 16.19 | 4.72 | 3.73 | .06 | |
| Inhibitory control | 21.32 | 4.21 | 22.22 | 4.44 | 1.17 | .28 | |
| Parenting energy | 1.57 | .90 | 1.29 | .61 | 4.64 | .03 | .03 |
| Kitchen appliance adequacy | 16.73 | 2.74 | 17.51 | 2.49 | 2.60 | .11 | |
| Teaching about nutrition | 10.89 | 2.45 | 12.23 | 2.01 | 11.07 | .001 | .07 |
| Household chaos | 8.89 | 2.61 | 7.18 | 2.55 | 12.40 | .001 | .08 |
| Food insecurity scale | 1.46 | 2.21 | .65 | 1.54 | 6.08 | .02 | .04 |
Note: ES = effect size. Effect sizes for ANOVAs are partial η2.
Parent weight status differed between latent profiles (Fisher’s Exact p = .03), in that the Authoritarian and Permissive Parenting Style and Controlling Feeding Practices group had more parents who were obese compared to the Authoritative Parenting Style and Less Controlling Feeding Practices group. Although effect sizes were small (< .1), there were significant differences in children’s temperament (anger/frustration), F(1, 147) = 13.02, p < .001, partial η2 = .08, parenting energy, F(1, 147) = 4.64, p = .03, partial η2 = .03, teaching about nutrition, F(1, 147) = 1.07, p = .001, partial η2 = .07, household chaos, F(1, 147) = 12.40, p = .001, partial η2 = .08, and food insecurity, F(1, 147) = 6.08, p = .02, partial η2 = .04. Specifically, parents in the Authoritarian and Permissive Parenting Style and Controlling Feeding Practices group reported children with higher negative affect, had less time or energy to feed their child “right”, were less likely to teach their child about nutrition, had higher household chaos, and had higher food insecurity, compared to parents in the Authoritative Parenting Style and Less Controlling Feeding Practices group. There were not significantly differences between latent profiles on child age, sex, race and temperament (impulsivity and inhibitory control), primary caregiver education level and income, and kitchen appliance adequacy.
Latent Profiles and Children’s Weight Status, Healthy Dietary Intake, and Eating Behaviors
Membership to a particular latent profile contributed significantly to the model predicting food responsiveness, explaining 3.9% of the variance after adjusting for parent age and weight status, child age, sex and race/ethnicity, and household income and structure, adjusted R2 = .125, Δ adjusted R2 = .036, F(17, 131) = 2.25, p = .006. Specifically, on average, parents in the Authoritarian and Permissive Parenting Style and Controlling Feeding Practices group were more likely to have children who ate to obtain pleasure and who lacked internal cues for hunger than parents in the Authoritative Parenting Style and Less Controlling Feeding Practices group (see Table 7).
Table 7.
Multiple Regression Predicting Child Food Responsiveness
| Predictor Variables | Step 1 | Step 2 | Step 3 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| R2 | β | 95.0% CIs | R2 | β | 95.0% CIs | R2 | β | 95.0% CIs | ||||
| .067* | .089* | .125** | ||||||||||
| PC’s age | −.101 | −.154 | .042 | −.124 | −.169 | .031 | −.107 | −.158 | .039 | |||
| TC’s age | .075 | −.417 | 1.165 | .062 | −.522 | 1.143 | .081 | −.415 | 1.222 | |||
| TC’s Sex (Male) | −.020 | −1.422 | 1.104 | −.074 | −1.884 | .717 | −.082 | −1.923 | .627 | |||
| Black | .314 | 1.007 | 5.740 | .283 | .398 | 5.680 | .229 | −.172 | 5.081 | |||
| Hispanic | .150 | −.590 | 3.761 | .187 | −.546 | 4.485 | .157 | −.818 | 4.135 | |||
| Hmong | .126 | −.972 | 3.640 | .151 | −.921 | 4.117 | .158 | −.799 | 4.138 | |||
| Native American | .158 | −.523 | 3.858 | .130 | −1.191 | 3.936 | .119 | −1.262 | 3.765 | |||
| Somali | .010 | −2.086 | 2.295 | −.003 | −2.597 | 2.535 | −.022 | −2.755 | 2.283 | |||
| Two Parents | ||||||||||||
| with Others | .002 | −2.047 | 2.084 | −.004 | −2.076 | 1.972 | ||||||
| One Parents | ||||||||||||
| Only | .023 | −1.843 | 2.404 | .005 | −2.025 | 2.150 | ||||||
| One Parent with | ||||||||||||
| Others | .114 | −.664 | 2.764 | .138 | −.412 | 2.964 | ||||||
| Income 2 | −.165 | −2.894 | .192 | −.157 | −2.800 | .226 | ||||||
| Income 3 | .016 | −2.137 | 2.541 | .019 | −2.047 | 2.537 | ||||||
| Income 4 | .045 | −1.949 | 3.245 | .046 | −1.879 | 3.209 | ||||||
| Income 5 | .116 | −1.238 | 5.562 | .124 | −1.014 | 5.652 | ||||||
| Income 6 | −.120 | −5.207 | 1.235 | −.108 | −4.946 | 1.373 | ||||||
| Latent Profile | −.209 | −3.378 | −.431 | |||||||||
Note. PC = primary caregiver. TC = target child. β = standardized β. R2 = adjusted R2
p < .05,
p < .01 for change in adjusted R2.
None of the other variables in the model were significantly associated with food responsiveness. Membership to a particular latent profile did not contribute to the models predicting child weight status, dietary intake summary, and other eating behaviors (i.e., food fussiness, satiety responsiveness) (see Table 8).
Table 8.
Multiple Regression Predicting Child Food Responsiveness
| Child Weight Status | Dietary Intake | Food Fussiness | Satiety Responsiveness | |||||
|---|---|---|---|---|---|---|---|---|
| Cox & Snell R2 | B | Adjusted R2 | Standardized β | Adjusted R2 | Standardized β | Adjusted R2 | Standardized β | |
| Step 1 | .151** | .193** | .065* | .002 | ||||
| PC’s age | .303 | .025 | .001 | .004 | ||||
| PC’s weight status | 2.105 | |||||||
| TC’s age | .020 | −.122 | −.084 | −.029 | ||||
| TC’s sex | −.141 | .028 | .151 | −.007 | ||||
| TC’s race/ethnicity | ||||||||
| Black | −.614 | −.339 | .050 | −.199 | ||||
| Hispanic | −.022 | .124 | .207 | −.186 | ||||
| Hmong | .191 | −.124 | .071 | .027 | ||||
| Native | −.482 | −.080 | .303 | −.089 | ||||
| American | ||||||||
| Somali | −.373 | .192 | .017 | −.036 | ||||
| Step 2 | .281** | .170 | .042 | .021 | ||||
| Household composition | ||||||||
| 2 parents with other adults | 1.650 | −.012 | .012 | −.024 | ||||
| 1 parent only | −1.069 | −.053 | .088 | .259 | ||||
| 1 parents with other adults | −.841 | .031 | .081 | .026 | ||||
| Household income | ||||||||
| Income 2 | −1.146 | −.125 | −.012 | .086 | ||||
| Income 3 | −1.708 | −.070 | .033 | .078 | ||||
| Income 4 | −.680 | −.069 | −.053 | .018 | ||||
| Income 5 | .808 | .053 | .045 | −.028 | ||||
| Income 6 | 2.517 | −.027 | −.139 | .109 | ||||
| Step 3 | .284 | .172 | .045 | .033 | ||||
| Latent profile | −.365 | .093 | −.104 | −.138 | ||||
Note. PC = primary caregiver. TC = target child. Coefficients are from the last step of each analysis.
p < .05,
p < .01 for change in R2.
Discussion
The current study addressed significant research gaps by using latent profile analysis to identify homogenous subgroups of parents based on both food parenting practices and parenting styles. In addition, this study examined the relationship between subgroups of parents and child weight, eating behaviors, and diet quality. Results suggest two subgroups of parents, and significant differences between the two groups in food parenting practices and parenting styles. Certain parenting styles appear to be related to more controlling parental behaviors, while others appear related to more teaching and modeling food-related behaviors. Specifically, parents in the Authoritarian and Permissive Parenting Style and Controlling Feeding Practices group were more likely to restrict certain foods offered to child and pressure child to eat, and less likely to engage in food modeling, compared to parents in the Authoritative Parenting Style and Less Controlling Feeding Practices. Related to child outcomes, parents in the Authoritarian and Permissive Parenting Style and Controlling Feeding Practices group were more likely to have children who ate to obtain pleasure and who lacked internal cues for hunger compared to parents in the Authoritative Parenting Style and Less Controlling Feeding Practices group. These findings extend prior research using parenting practices or styles and indicate that profiles related to both style and practices influence important child food-related outcomes and suggests that future research and interventions should consider the interaction of parenting styles and food parenting practices.
In the current study, there were significant differences in parenting styles between the two parent groups. Parents in the Authoritarian and Permissive Parenting Style and Controlling Feeding Practices group were more likely to engage in coercive control parenting practices such as restricting certain foods and pressuring child to eat compared to the Authoritative Parenting Style and Less Controlling Feeding Practices group. This finding supports the notion that parents with an authoritarian style of parenting tend to exhibit high demandingness/control and low responsiveness/nurturance. Although slightly counterintuitive, parents in the Authoritarian and Permissive Parenting Style and Controlling Feeding Practices group also were more likely to endorse a permissive parenting style compared to the Authoritative Parenting Style and Less Controlling Feeding Practices group. An explanation for this finding is that parents who use a permissive parenting style may be more influenced by contextual factors such as stress and chaos resulting in more controlling food parenting practices.(Berge, Tate, Trofholz, Fertig, et al., 2018; Berge, Tate, Trofholz, Loth, et al., 2018; Loth et al., 2018). Indeed, our previous research indicates that environmental factors influence parents use of more coercive feeding practices (Berge, Tate, et al., 2017; Loth et al., 2018) and we found parents in the Authoritarian and Permissive Parenting Style and Controlling Feeding Practices group reported higher household chaos, higher food insecurity, less time or energy to feed their child “right,” and a child with higher negative affect.
Consistent with previous research, findings in this study indicate that parents engage in multiple food parenting practices (Berge, Tate, Trofholz, Loth, et al., 2018; Loth, MacLehose, Fulkerson, Crow, & Neumark-Sztainer, 2013a, 2013b; Loth et al., 2018; Vaughn et al., 2016). In a qualitative study that explored momentary impacts on food parenting practices (Loth et al., 2018), parents described how their feeding practices were easily influenced by momentary factors (e.g., schedule changes, parental stress, child behavior) and how such factors shifted parents away from structure and autonomy supportive feeding practices towards coercive and indulgent feeding practices. Thus, it is possible that parents in the Authoritarian and Permissive Parenting Style and Controlling Feeding Practices group engage in multiple feeding practices such as restricting “unhealthy” foods and pressuring child to eat “healthy” foods in response to their chaotic environment and stress. It also is possible that using numerous parenting practices contribute to the chaotic environment that influences eating regulation in children (Berge, Wall, Loth, et al., 2010).
Results from this study showed that latent profile predicted food responsiveness such that on average parents in the Authoritarian and Permissive Parenting Style and Controlling Feeding Practices group had higher food responsiveness scores or were more likely to report their child ate to obtain pleasure and lacked internal cues for hunger. Prior research indicates that restricting food and pressuring to eat are linked to both desirable and undesirable food consumption (Yee et al., 2017). In fact, coercive parenting practices (e.g., food restriction, pressure to eat) have been shown to have unintended negative consequences on child eating behaviors such as increased unhealthy food consumption, tendency towards overeating and increased desire for restricted foods (Vaughn et al., 2016; Yee et al., 2017). Although coercive parenting practice may lead to the child eating more healthy foods in the moment, the child tends to choose less healthy options once independent. Thus, structure and autonomy support provide the child with scaffolding which allows freedom to learn within a supportive environment and make more healthful choices in the future. In this study, not only were their children more likely to eat to obtain pleasure and lacked internal cues for hunger, but parents in the Authoritarian and Permissive Parenting Style and Controlling Feeding Practices group also were more likely to restrict foods and pressure their child to eat. Since parents in the Authoritarian and Permissive Parenting Style and Controlling Feeding Practices group also reported a more chaotic environment, it is possible that the relationship between chaotic environments and food parenting practices is bi-directional; and both affect the regulation of eating. For example, a chaotic environment (i.e., disorganization and hurriedness) during dinner may contribute to coercive parenting practices and the increased use of coercive parenting practices may contribute to a more chaotic environment. Future research should aim to better understand how and why environmental factors influence engagement in different food parenting practices, and how this complex relationship impacts child outcomes. Future studies also should examine whether parenting styles function as moderators or mediators of the association between parenting practices and child outcomes.
This study had several strengths, including the use of more advanced statistical analysis, adjustments for confounding factors, the measurement of both parenting style and parenting practices, in addition to child eating behaviors, and a sample that included racially/ethnically and socioeconomically diverse families. There are several limitations that should be taken into consideration when interpreting the findings. First, self-report measures and interview were used, and responses may be based on expectations and societal norms. Future studies would benefit from multiple informants and more objective measures such as observations (Berge et al., 2014). Second, the developmental stage of children included in this study is a limitation because results are not generalizable to other stages of development. In a meta-analysis, Yee et al. (2017) examined age as a moderator for the relationship between parenting practices and child food consumption and found that the effects of pressuring to eat on healthy food consumption was significant only among younger, and not older, children. Thus, it is possible that findings from this study may not be generalizable or replicable in populations of older children. Third, this is a cross-sectional study and thus we have identified associations and not causality. Finally, our relatively small sample size and analytic strategy both limit the generalizable of the results to other populations. For example, based on the uneven group sizes in the two-group solution, it is possible that we identified one unique group and the other group was the remaining heterogeneous sample. Although the two-group solution appears to have theoretical clarity, the model was not predictive of numerous outcomes. Thus, future studies would benefit from larger sample sizes to determine whether a more nuanced grouping of parents better differentiate child eating and weight outcomes. Additionally, latent profile analysis is dependent on the indicators included in the models, and thus there may be other food parenting practices and styles (e.g., neglectful parenting style) that were not included and may be more helpful in explaining how practices and styles together impact child weight and weight-related outcomes. Although our results may reflect our unique sample, there may be high internal validity to identify processes that exist for this sample.
Conclusions
This study identified unique latent profiles (subgroups) based on food parenting practices and parenting styles and explored differences and similarities of the latent profiles (i.e., demographics, general parenting, child temperament, and household factors). Moreover, this study demonstrated how latent profiles predict child food responsiveness, or susceptibility to the hedonistic qualities of food and lack of internal cues for hunger. Indeed, findings from this study indicate that parents of children aged 5–7 years utilize a broad range of food parenting practices, and a subgroup of parents may use more coercive control and structure strategies. Results suggest that it may be important for clinicians to provide guidance and education to parents about the dynamic interplay among parenting styles and food parenting practices such as ecological momentary interventions. Future interventions may help parents to identify ways of establishing and maintaining structure and autonomy supportive parenting practices despite the environment and life stressors.
Since parenting practices are more fluid and parents engage in multiple goal-oriented approaches throughout a meal or day or week, identification of ways to help parents adopt food parenting practices that do not necessarily fit with their parenting style may be beneficial. For example, a more authoritarian parent may require assistance in learning autonomy supportive parenting practices, and a more permissive parent may require assistance in establishing structure parenting practices. This study provided another approach to examining the complexity of food parenting practices and gives clinicians and researchers an opportunity to better understand how combinations of parenting practices and styles impact child eating outcomes. Future research should continue to examine the broad range and interplay of parenting styles and food parenting practices to better understand the role of parents in child’s weight and eating behaviors.
Acknowledgments:
Thank you to the research group at the University of Minnesota for their feedback in the initial phases of development for this research study.
Funding Source: All phases of this study were supported by grants from the National Institutes of Health (R01HL126171 and T32MH082761).
Financial Disclosure: The authors have indicated they have no financial relationships relevant to this article to disclose.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest: The authors have indicated they have no potential conflicts of interest to disclose.
References
- Appelhans BM, Waring ME, Schneider KL, & Pagoto SL (2014). Food preparation supplies predict children’s family meal and home-prepared dinner consumption in low-income households. Appetite, 76, 1–8. doi: 10.1016/j.appet.2014.01.008. [DOI] [PubMed] [Google Scholar]
- Berge JM (2009). A review of familial correlates of child and adolescent obesity: What has the 21st century taught us so far? Int J Adolesc Med Health, 21(4), 457–483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berge JM, Rowley S, Trofholz A, Hanson C, Rueter M, MacLehose RF, & Neumark-Sztainer D (2014). Childhood obesity and interpersonal dynamics during family meals. Pediatrics, 134(5), 923–932. doi: 10.1542/peds.2014-1936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berge JM, Tate A, Trofholz A, Fertig A, Crow S, Neumark-Sztainer D, & Miner M (2018). Examining within- and across-day relationships between transient and chronic stress and parent food-related parenting practices in a racially/ethnically diverse and immigrant population: Stress types and food-related parenting practices. Int J Behav Nutr Phys Act, 15(1), 7. doi: 10.1186/s12966-017-0629-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berge JM, Tate A, Trofholz A, Fertig AR, Miner M, Crow S, & Neumark-Sztainer D (2017). Momentary parental stress and food-related parenting practices. Pediatrics, 140(6). doi: 10.1542/peds.2017-2295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berge JM, Tate A, Trofholz A, Loth K, Miner M, Crow S, & Neumark-Sztainer D (2018). Examining variability in parent feeding practices within a low-income, racially/ethnically diverse, and immigrant population using ecological momentary assessment. Appetite, 127, 110–118. doi: 10.1016/j.appet.2018.04.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berge JM, Trofholz A, Tate AD, Beebe M, Fertig A, Miner MH, … Neumark-Sztainer D (2017). Examining unanswered questions about the home environment and childhood obesity disparities using an incremental, mixed-methods, longitudinal study design: The Family Matters study. Contemp Clin Trials, 62, 61–76. doi: 10.1016/j.cct.2017.08.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berge JM, Wall M, Bauer KW, & Neumark-Sztainer D (2010). Parenting characteristics in the home environment and adolescent overweight: a latent class analysis. Obesity, 18(4), 818–825. doi: 10.1038/oby.2009.324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berge JM, Wall M, Loth K, & Neumark-Sztainer D (2010). Parenting style as a predictor of adolescent weight and weight-related behaviors. J Adolesc Health, 46(4), 331–338. doi: 10.1016/j.jadohealth.2009.08.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birch LL, Fisher JO, Grimm-Thomas K, Markey CN, Sawyer R, & Johnson SL (2001). Confirmatory factor analysis of the Child Feeding Questionnaire: A measure of parental attitudes, beliefs and practices about child feeding and obesity proneness. Appetite, 36(3), 201–210. doi: 10.1006/appe.2001.0398 [DOI] [PubMed] [Google Scholar]
- Blumberg SJ, Bialostosky K, Hamilton WL, & Briefel RR (1999). The effectiveness of a short form of the Household Food Security Scale. Am J Public Health, 89(8), 1231–1234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (2015). Assessing your weight. Retrieved from https://www.cdc.gov/healthyweight/ (Accessed on February 15, 2019).
- Center, N. C. (2016). The Nutrition Coodinating Center (NCC). Retrieved from http://www.ncc.umn.edu/ (Accessed on November 3, 2018).
- Department of Human and Health Services (2019). Annual update of the HHS poverty guidelines. Retrieved from http://www.federalregister.gov/d/2018-00814 (Accessed on March 1, 2019).
- Guenther PM, Kirkpatrick SI, Reedy J, Krebs-Smith SM, Buckman DW, Dodd KW, … Carroll RJ (2014). The Healthy Eating Index-2010 is a valid and reliable measure of diet quality according to the 2010 Dietary Guidelines for Americans. J Nutrition, 144(3), 399–407. doi: 10.3945/jn.113.183079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Himes JH, & Dietz WH (1994). Guidelines for overweight in adolescent preventive services: recommendations from an expert committee. The Expert Committee on Clinical Guidelines for Overweight in Adolescent Preventive Services. Am J Clin Nutr, 59(2), 307–316. doi: 10.1093/ajcn/59.2.307 [DOI] [PubMed] [Google Scholar]
- IBM, C. (Released 2013). IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp. [Google Scholar]
- Kremers S, Sleddens E, Gerards S, Gubbels J, Rodenburg G, Gevers D, & van Assema P (2013). General and food-specific parenting: Measures and interplay. Childhood Obesity, 9(1), S22–S31. doi: 10.1089/chi.2013.0026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuczmarski RJ, Ogden CL, Grummer-Strawn LM, Flegal KM, Guo SS, Wei R, … Johnson CL (2000). CDC growth charts: United States. Adv Data, 314, 1–27. [PubMed] [Google Scholar]
- Loth KA, MacLehose RF, Fulkerson JA, Crow S, & Neumark-Sztainer D (2013a). Eat this, not that! Parental demographic correlates of food-related parenting practices. Appetite, 60(1), 140–147. doi: 10.1016/j.appet.2012.09.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loth KA, MacLehose RF, Fulkerson JA, Crow S, & Neumark-Sztainer D (2013b). Food-related parenting practices and adolescent weight status: A Population-based study. Pediatrics, 131(5), e1443–e1450. doi: 10.1542/peds.2012-3073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loth KA, Uy M, Neumark-Sztainer D, Fisher JO, & Berge JM (2018). A qualitative exploration into momentary impacts on food parenting practices among parents of pre-school aged children. Appetite, 130, 35–44. doi: 10.1016/j.appet.2018.07.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lubke GH, & Muthen B (2005). Investigating population heterogeneity with factor mixture models. Psychol Methods, 10(1), 21–39. doi: 10.1037/1082-989x.10.1.21 [DOI] [PubMed] [Google Scholar]
- Maccoby EE (1992). The role of parents in the socialization of children: An historical overview. Developmental Psychology, 28(6), 1006–1017. doi: 10.1037/0012-1649.28.6.1006 [DOI] [Google Scholar]
- Matheny AP, Wachs TD, Ludwig JL, & Phillips K (1995). Bringing order out of chaos: Psychometric characteristics of the confusion, hubbub, and order scale. J Applied Developmental Psychol, 16(3), 429–444. doi: 10.1016/0193-3973(95)90028-4 [DOI] [Google Scholar]
- Musher-Eizenman D, & Holub S (2007). Comprehensive Feeding Practices Questionnaire: Validation of a new measure of parental feeding practices. J Pediatr Psychol, 32(8), 960–972. doi: 10.1093/jpepsy/jsm037 [DOI] [PubMed] [Google Scholar]
- Muthén L, & Muthén B (1998–2015). Mplus User’s Guide. (7th ed.). Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- Nylund-Gibson K, & Choi AY (2018). Ten frequently asked questions about latent class analysis. Translational Issues Psychol Sci, 4(4), 440–461. doi: 10.1037/tps0000176 [DOI] [Google Scholar]
- O’Connor TM, Masse LC, Tu AW, Watts AW, Hughes SO, Beauchamp MR, … Vaughn A (2017). Food parenting practices for 5 to 12 year old children: A concept map analysis of parenting and nutrition experts input. Int J Behav Nutr Phys Act, 14(1), 122. doi: 10.1186/s12966-017-0572-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogden J, Reynolds R, & Smith A (2006). Expanding the concept of parental control: A role for overt and covert control in children’s snacking behaviour? Appetite, 47(1), 100–106. doi: 10.1016/j.appet.2006.03.330 [DOI] [PubMed] [Google Scholar]
- Patrick H, Hennessy E, McSpadden K, & Oh A (2013). Parenting styles and practices in children’s obesogenic behaviors: scientific gaps and future research directions. Child Obes, 9 Suppl, S73–86. doi: 10.1089/chi.2013.0039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinquart M (2014). Associations of general parenting and parent–child relationship with pediatric obesity: A meta-analysis. J Pediatric Psychology, 39(4), 381–393. doi: 10.1093/jpepsy/jst144 [DOI] [PubMed] [Google Scholar]
- Robinson CC, Mandleco B, Olsen SF, & Hart CH (1995). Authoritative, authoritarian, and permissive parenting practices: Development of a new measure. Psychological Reports, 77(3), 819–830. doi: 10.2466/pr0.1995.77.3.819 [DOI] [Google Scholar]
- Rothbart MK, Ahadi SA, Hershey KL, & Fisher P (2001). Investigations of temperament at three to seven years: The Children’s Behavior Questionnaire. Child Development, 72(5), 1394–1408. doi: 10.1111/1467-8624.00355 [DOI] [PubMed] [Google Scholar]
- Schakel SF, Buzzard IM, & Gebhardt SE (1997). Procedures for estimating nutrient values for food composition databases. J Food Composition Analysis, 10(2), 102–114. [Google Scholar]
- Schakel SF, & Himes JH (2001). Maintaining a nutrient database in a changing marketplace: Keeping pace with changing food products- a research perspective. J Food Composition Analysis, 14(3), 315–322. [Google Scholar]
- Schakel SF, Sievert YA, & Buzzard IM (1988). Sources of data for developing and maintaining a nutrient database. J Am Diet Assoc, 88(10), 1268–1271. [PubMed] [Google Scholar]
- Storfer-Isser A, & Musher-Eizenman D (2013). Measuring parent time scarcity and fatigue as barriers to meal planning and preparation: Quantitative scale development. J Nutrition Edu Beh, 45(2), 176–182. doi: 10.1016/j.jneb.2012.08.007 [DOI] [PubMed] [Google Scholar]
- Vaughn AE, Ward DS, Fisher JO, Faith MS, Hughes SO, Kremers SP, … Power TG (2016). Fundamental constructs in food parenting practices: A content map to guide future research. Nutr Rev, 74(2), 98–117. doi: 10.1093/nutrit/nuv061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vollmer RL, & Mobley AR (2013). Parenting styles, feeding styles, and their influence on child obesogenic behaviors and body weight. A review. Appetite, 71, 232–241. doi: 10.1016/j.appet.2013.08.015 [DOI] [PubMed] [Google Scholar]
- Wardle J, Guthrie CA, Sanderson S, & Rapoport L (2001). Development of the Children’s Eating Behaviour Questionnaire. J Child Psychol Psychiatry, 42(7), 963–970. [DOI] [PubMed] [Google Scholar]
- Wiggins S, Potter J, & Wildsmith A (2001). Eating your words: Discursive psychology and the reconstruction of eating practices. J Health Psychol, 6(1), 5–15. doi: 10.1177/135910530100600101 [DOI] [PubMed] [Google Scholar]
- Yee AZ, Lwin MO, & Ho SS (2017). The influence of parental practices on child promotive and preventive food consumption behaviors: a systematic review and meta-analysis. Int J Behav Nutr Phys Act, 14(1), 47. doi: 10.1186/s12966-017-0501-3 [DOI] [PMC free article] [PubMed] [Google Scholar]