Abstract
Background
Anaplastic thyroid cancer (ATC) is rare, accounting for 1-2% of thyroid malignancies. Median survival is only 3-10 months, and the optimal therapeutic approach has not been established. This study aimed to evaluate outcomes in ATC based on treatment modality.
Methods
Retrospective review was performed for patients treated at a single institution between 1990 and 2015. Demographic and clinical covariates were extracted from the medical record. Overall survival (OS) was modeled using Kaplan Meier curves for different treatment modalities. Univariate and multivariate analyses were conducted to assess the relationships between treatment and disease characteristics and OS.
Results
28 patients with ATC were identified (n = 16 female, n = 12 male; n = 22 Caucasian, n = 6 African-American; median age 70.9). Majority presented as Stage IVB (71.4%). Most patients received multimodality therapy. 19 patients underwent local surgical resection. 21 patients received locoregional external beam radiotherapy (EBRT) with a median cumulative dose of 3,000 cGy and median number of fractions of 16. 14 patients received systemic therapy (n = 11 concurrent with EBRT), most commonly doxorubicin (n = 9). 16 patients were never disease free, 11 patients had disease recurrence, and 1 patient had no evidence of disease progression. Median OS was 4 months with 1-year survival of 17.9%. Regression analysis showed that EBRT (HR: 0.174; 95% CI: 0.050–0.613; p=0.007) and surgical resection (HR: 0.198; 95% CI: 0.065–0.598; p=0.004) were associated with improved OS. Administration of chemotherapy was not associated with OS.
Conclusions
Anaplastic thyroid cancer patients receiving EBRT to the thyroid area/neck and/or surgical resection had better OS than patients without these therapies, though selection bias likely contributed to improved outcomes since patients who can undergo these therapies tend to have better performance status. Prognosis remains poor overall, and new therapeutic approaches are needed to improve outcomes.
1. Introduction
Thyroid cancer is a prevalent disease that affects 5% of females and 1% of males globally [1]. Anaplastic thyroid cancer (ATC) is the rarest histologic subtype, representing 1-2% of thyroid malignancies with approximately 600 new cases in the U.S. annually [2]. It is the most aggressive type of thyroid cancer and causes significant morbidity and mortality. Older age, male gender, bilateral tumors, presence of local invasion, and/or distant metastasis are unfavorable prognostic factors that are present in the majority of ATC cases [3, 4]. Despite multimodality treatment, outcomes are poor with a median survival of 3-10 months and a 20% 1-year survival rate [5]. Most patients experience tumor location-specific and treatment toxicities including airway compromise, dysphagia, esophagitis, and radiation dermatitis [6].
Optimal management of ATC requires multimodality management by surgeons, radiation oncologists, and medical oncologists. First-line curative treatment requires surgical resection. External beam radiation therapy (EBRT) with chemotherapy is generally employed postoperatively or utilized as definitive therapy for unresectable disease [3, 7]. Commonly used radiotherapy regimens include conventional fractionation (1.5-2 Gy/day) and accelerated twice daily radiation with fraction sizes ranging from 1 to 2 Gy [7]. Radiation treatment volumes vary between comprehensive targeting of the surgical bed, bilateral cervical lymphatics, and anterior mediastinum and more limited coverage of macroscopic disease with margin for microscopic extension. Doxorubicin, commonly combined with cisplatin, has been used for systemic therapy with or without EBRT [8, 9] although other drugs such as paclitaxel have also been utilized [10–12]. Palliative treatment of ATC often involves low-dose radiotherapy directed to the neck or metastatic sites with the intent of mitigating local invasion and associated symptoms [3]. Overall, ATC responds poorly to therapy indicating the need for novel treatment modalities [13].
Few studies have evaluated outcomes and toxicities for the treatment of ATC. Additionally, the efficacy of newer radiation therapy techniques, including intensity modulated radiation treatment (IMRT), has not been widely studied for this disease. Given the limited prospective randomized data and small, heterogeneous retrospective studies of EBRT in this disease, the optimal radiotherapy fractionation regimen and technique remain poorly defined. The purpose of this study was to evaluate treatment regimens, outcomes, and toxicities for ATC. We hypothesized that the administration of locoregional EBRT would improve progression-free and overall survival. We also anticipated that radiotherapy would be well-tolerated, with lower toxicity for patients treated with IMRT compared to conventional 2D or 3D conformal radiation treatment.
2. Materials and Methods
2.1. Patient Selection
Records of all adult patients diagnosed with thyroid carcinoma were retrospectively reviewed under an institutional review board-approved protocol at Duke University Medical Center between January 1, 1990, and December 31, 2015. ATC patients who had unavailable electronic and paper health records and patients with nonanaplastic thyroid cancer were excluded (Figure 1).
Figure 1.
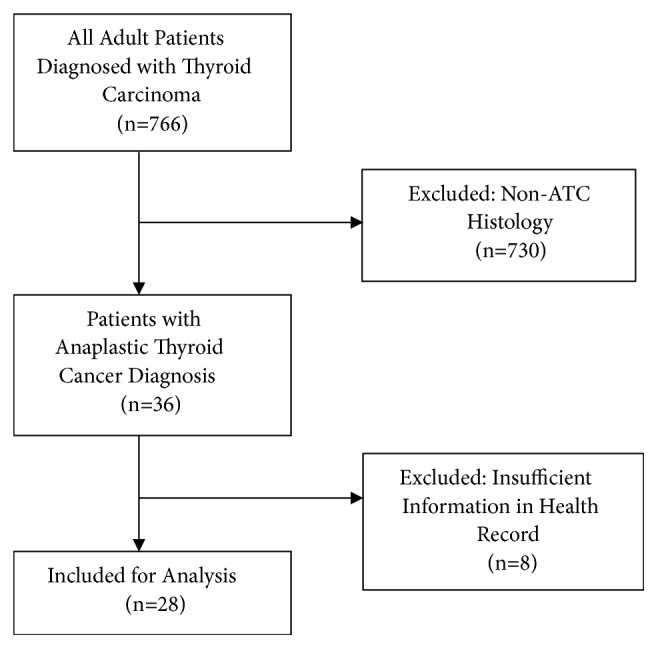
Inclusion criteria.
Patient demographics, disease stage (American Joint Committee on Cancer 8th edition), leukocytosis (WBC ≥ 10,000/mm3) at time of ATC diagnosis, histology, pathologic characteristics, receipt and details of surgery, radioactive iodine (RAI) treatment, radiotherapy and/or chemotherapy, results and dates of all imaging studies, status at last follow-up, date(s) of recurrence, treatment-related toxicities, locoregional and distant disease control, progression-free survival, and overall survival were compiled. The following surgical parameters were recorded: surgery type (lobectomy, total thyroidectomy, lymph node dissection, and metastasectomy), margin status, pre- and postoperative thyroid-stimulating hormone (TSH) and thyroglobulin antibodies (TgAb), and toxicity. The following RAI treatment parameters were recorded: RAI uptake, number of courses, and dose of RAI. The following radiotherapy parameters were recorded: technique (intensity modulated radiation therapy [IMRT], 2D or 3D conformal radiation therapy, stereotactic radiosurgery [SRS], stereotactic body radiation therapy [SBRT]), treatment intent (curative versus palliative, defined by treating physician in radiation prescription), radiation site, total dose, schedule, in-field and out-of-field recurrence, and toxicity. Total radiation dose was dichotomized into groups (<4,000 cGy versus ≥4,000 cGy) based on other studies showing significantly improvement outcomes with radiation dose ≥4,000 cGy [14–16]. The following chemotherapy parameters were obtained: drug(s) used, number of courses, number of cycles, and toxicity. All data were entered into a secure REDCap database.
2.2. Statistical Analysis
Patient and treatment characteristics were summarized with counts and percentages for categorical variables and with medians and interquartile ranges (IQR) for continuous variables for all patients. Relevant variables specific to receipt of EBRT were also summarized by course, and patient outcomes including recurrence, progression, and cause of death were summarized with counts and percentages.
Overall survival (OS) was modeled using the Kaplan Meier method for different treatment modalities, including dichotomous EBRT vs. no EBRT, surgery vs. no surgery, chemotherapy vs. no chemotherapy, and initial EBRT intent for those who received EBRT. OS was defined as time from ATC diagnosis date to death from any cause, with living patients censored at their date of last assessment. 1-year OS, median OS, and corresponding 95% confidence intervals were presented for all treatment modalities. Recurrence-free survival, defined as time from ATC diagnosis date to first local, regional, or distant recurrence or death from any cause, was also described using Kaplan Meier plots, 1-year survival, and median survival. For recurrence-free survival, patients were censored at their date of last assessment if they did not have any of the specified events.
Cox proportional hazards models were used to assess the univariate and multivariate relationships between OS and selected treatment and patient characteristics. From the univariate model, age, leukocytosis (WBC ≥ 10,000/mm3) at time of ATC diagnosis, and receipt of EBRT, surgery, and chemotherapy were chosen as covariates for the multivariate model predicting OS. Only patients with available data were utilized in each model, and effective sample sizes were included in all tables and figures. No adjustments were made for multiple comparisons. All statistical analyses were conducted using SAS version 9.4 (SAS Institute, Cary, NC).
3. Results
Of the 766 patients diagnosed with thyroid cancer, 28 patients met inclusion criteria (Figure 1). Table 1 describes baseline patient characteristics at the time of anaplastic thyroid cancer diagnosis. Patients were predominantly female (57.1%) and Caucasian (78.6%; African-American, 21.4%). Median age at diagnosis was 70.9 (IQR: 63.8–74.7). 12 patients (42.9%) had leukocytosis (WBC ≥ 10,000/mm3) at the time of their ATC diagnosis. Six patients had an initial or concomitant diagnosis of differentiated thyroid cancer. A majority of patients presented as Stage IVB disease (71.4%), with remaining stage distribution as follows: 7.1% stage IVA, 17.9% stage IVC, and 3.6% unknown.
Table 1.
Patient characteristics.
| All patients (N=28) |
|
|---|---|
| Age at diagnosis (years) | |
| Median (IQR) | 70.9 (63.8 - 74.7) |
|
| |
| Sex | |
| Female | 16 (57.1%) |
| Male | 12 (42.9%) |
|
| |
| Race | |
| Caucasian | 22 (78.6%) |
| African-American | 6 (21.4%) |
|
| |
| Leukocytosis | |
| No | 12 (42.9%) |
| Yes | 12 (42.9%) |
| Unknown | 4 (14.3%) |
|
| |
| Initial or concomitant diagnosis of differentiated thyroid cancer (papillary or follicular) | |
| No | 22 (78.6%) |
| Yes | 6 (21.4%) |
|
| |
| Stage | |
| IVA | 2 (7.1%) |
| IVB | 20 (71.4%) |
| IVC | 5 (17.9%) |
| Unknown | 1 (3.6%) |
|
| |
| T stage | |
| T2 | 1 (3.6%) |
| T3 | 1 (3.6%) |
| T4a | 13 (46.4%) |
| T4b | 12 (42.9%) |
| Unknown | 1 (3.6%) |
|
| |
| N stage | |
| N0 | 9 (32.1%) |
| N1a | 1 (3.6%) |
| N1b | 4 (14.3%) |
| Nx or Unknown | 14 (50.0%) |
|
| |
| M stage | |
| M0 | 7 (25.0%) |
| M1 | 5 (17.9%) |
| Mx or Unknown | 16 (57.1%) |
|
| |
| Lymphovascular invasion | |
| No | 5 (17.9%) |
| Yes | 14 (50.0%) |
| Unknown | 9 (32.1%) |
|
| |
| Extrathyroidal extension | |
| No | 4 (14.3%) |
| Yes | 23 (82.1%) |
| Unknown | 1 (3.6%) |
Counts and column percentages are presented unless otherwise specified.
Table 2 summarizes surgical, RAI, EBRT, and systemic treatment characteristics. Most patients received multimodality therapy. 2 patients (7.1%) received radioactive iodine treatment after their ATC diagnosis due to a synchronous diagnosis of differentiated thyroid cancer. 19 patients (67.9%) underwent thyroid lobectomy or total thyroidectomy. Of these, one patient required an extensive operation (total laryngopharyngectomy). 5 patients did not have postoperative radiation therapy, including 2 patients intended to have radiation therapy but precluded from further treatment due to postoperative complications requiring tracheostomy placement and subsequent decompensation due to aspiration pneumonia and extensive disease. 15 (53.6%) patients had postoperative radiation therapy. Of these patients, 4 had postoperative airway compromise requiring tracheostomy placement, which delayed radiation therapy in 2 patients. The median time between surgery and radiation therapy was 4 weeks.
Table 2.
Surgical, radioactive iodine, radiotherapy, and systemic treatment characteristics.
| All patients (N=28) |
|
|---|---|
| Surgery | |
| No | 8 (28.6%) |
| Yes | 20 (71.4%) |
|
| |
| Number of surgeries per patient | |
| 0 | 8 (28.6%) |
| 1 | 14 (50.0%) |
| 2 | 4 (14.3%) |
| 4 | 2 (7.1%) |
|
| |
| Type(s) of surgery | |
| Lobectomy | 7 (25.0%) |
| Thyroidectomy | 12 (42.9%) |
| Lymph node dissection | 9 (32.1%) |
| Metastasectomy | 1 (3.6%) |
|
| |
| Radioactive iodine | |
| No | 24 (85.7%) |
| Yes, after ATC diagnosis | 2 (7.1%) |
| Yes, before ATC diagnosis | 2 (7.1%) |
|
| |
| EBRT to any site | |
| No | 7 (25.0%) |
| Yes | 21 (75.0%) |
|
| |
| EBRT to thyroid bed/neck | |
| No | 9 (32.1%) |
| Yes | 19 (67.9%) |
|
| |
| Total radiation dose (cGy) | |
| < 4,000 | 11 (39.3%) |
| ≥ 4,000 | 6 (21.4%) |
| Unknown | 4 (14.3%) |
|
| |
| Radiation fractionation (fractions/day) | |
| 1 | 8 (28.6%) |
| > 1 | 9 (32.1%) |
| Unknown | 4 (14.3%) |
|
| |
| More than one EBRT treatment course | |
| No | 19 (67.9%) |
| Yes | 9 (32.1%) |
|
| |
| EBRT initial intent | |
| No EBRT | 7 (25.0%) |
| Palliative | 14 (50.0%) |
| Curative | 7 (25.0%) |
|
| |
| EBRT initial technique | |
| No EBRT | 7 (25.0%) |
| 2D | 4 (14.3%) |
| 3D | 3 (10.7%) |
| IMRT/VMAT | 12 (42.9%) |
| Unknown | 2 (7.1%) |
|
| |
| Systemic therapy | |
| No | 14 (50.0%) |
| Yes | 14 (50.0%) |
|
| |
| Type(s) of chemotherapy used with EBRT | |
| Doxorubicin | 4 (14.3%) |
| Doxorubicin, Cisplatin | 2 (7.1%) |
| Doxorubicin, Carboplatin, Paclitaxel | 1 (3.6%) |
| Doxorubicin, Carboplatin, Paclitaxel, Cisplatin, Pemetrexed, Bevacizumab | 1 (3.6%) |
| Doxorubicin, Carboplatin, Paclitaxel, Cyclophosphamide, Vinorelbine, Gemcitabine | 1 (3.6%) |
| Carboplatin, Paclitaxel | 1 (3.6%) |
| Sorafenib | 1 (3.6%) |
|
| |
| All treatments | |
| Surgery + EBRT + Chemotherapy | 10 (35.7%) |
| Surgery + EBRT | 5 (17.9%) |
| EBRT + Chemotherapy | 3 (10.7%) |
| EBRT only | 3 (10.7%) |
| Surgery only | 5 (17.9%) |
| Chemotherapy only | 1 (3.6%) |
| No treatment | 1 (3.6%) |
Counts and column percentages are presented unless otherwise specified.
EBRT = external beam radiation therapy; IMRT = intensity modulated radiation therapy; VMAT = volumetric modulated arc therapy.
21 patients (75.0%) received EBRT to any site, and 19 received locoregional EBRT to the thyroid, thyroid bed, and/or neck. 32.1% of patients had more than one course of EBRT. Of those patients who were treated with EBRT, 66.7% were initially treated with palliative intent and 33.3% were initially treated with curative intent. Initial EBRT course techniques were 2D/3D conformal (n = 7) or IMRT (n = 12), with 2 unknown due to receiving radiotherapy at outside institutions. 14 patients (50.0%) received systemic therapy, 11 of whom had concurrent chemotherapy with EBRT. Of those receiving concurrent chemoradiation, patients most commonly received doxorubicin (n = 9). Two patients (7.1%) received targeted therapy; one received bevacizumab and one received sorafenib.
The median number of EBRT courses was 1 (range, 0–4), and the thyroid/thyroid bed was most commonly targeted (76.5%) (Supplementary Table 1). Other sites targeted by RT included left neck (61.8%), right neck (64.7%), mediastinum (17.6%), and metastases (20.6%). Of the patients who received EBRT to locoregional sites (thyroid, thyroid bed, and/or neck), the median cumulative dose was 3,000 cGy (IQR: 2,100–3,880) and median number of fractions was 16 (IQR: 10–24) (Supplementary Table 2). Locoregional EBRT was completed in 15 patients and discontinued early in 4 patients due to toxicity (n = 2 radiation toxicity, n = 1 chemotherapy toxicity; n = 1 postop complication). Some patients experienced more than one toxicity. Of the 2 patients who discontinued EBRT early due to radiation-specific toxicities, 1 was treated with IMRT and the other was treated with 2D/3D conformal RT. Other radiation toxicities that occurred were fatigue, mucositis, hoarseness, esophagitis, stridor, dermatitis, and neck edema. Of the 12 patients treated with IMRT, 7 (58.3%) had no reported toxicities, 2 (16.7%) had Grade 1 toxicities, and 3 (25.0%) had Grade 3 toxicities. Of the 7 patients treated with 2D/3D conformal RT, 3 (42.9%) had Grade 1 toxicities, 1 (14.3%) had Grade 2 toxicity, and 3 (42.9%) had Grade 3 toxicities. The in-field recurrence rate was 24.1% and EBRT was associated with improved recurrence-free survival (Supplementary Figure 1).
16 patients (57.1%) were never disease free, 11 patients (39.3%) had disease recurrence, and 1 patient (3.6%) had no evidence of disease progression throughout the study period. A majority of patients (n=20; 71.4%) died from thyroid cancer. Other causes of death included treatment toxicity (7.1%), other reasons (3.6%), and unknown (10.7%). Patients receiving surgery, EBRT, and chemotherapy had the best overall survival (Supplementary Figure 2). Pathology slides from 3 of the 5 patients with survival > 1 year were available for review, and a diagnosis of ATC was confirmed in all 3 cases.
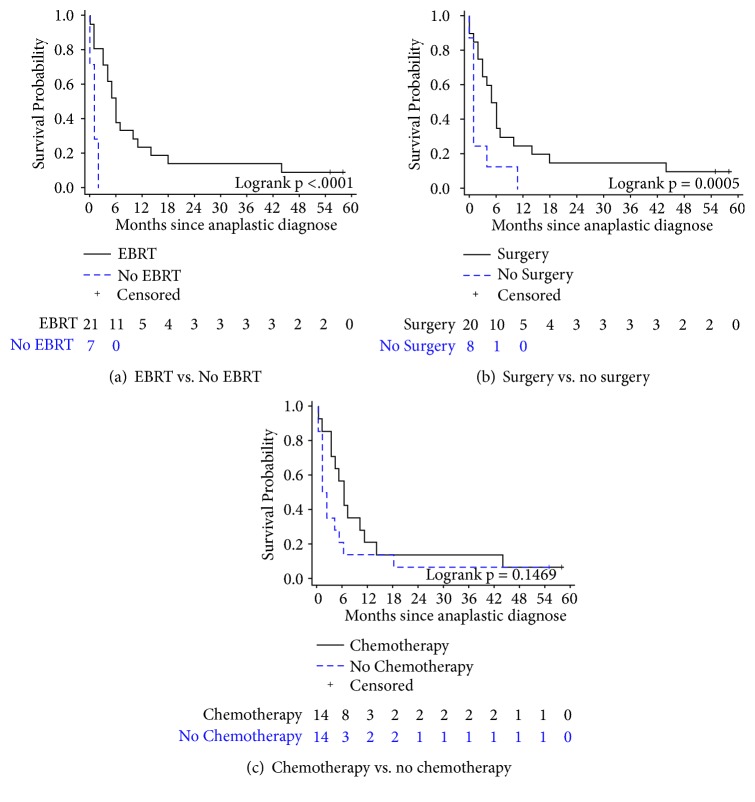
For all patients, median OS was 4 months (95% CI: 1–6 months), with a 1-year survival rate of 17.9%. Median OS after completing the first course of EBRT was 6 months (95% CI: 3–10 months), with a 1-year survival rate of 23.8% (95% CI: 8.7–43.1%) as compared to a median OS of 1 month (95% CI: 0–2 months) and 0.0% 1-year survival rate in patients who did not receive EBRT (Figure 2(a)). Median OS after first surgical resection was 5.5 months (95% CI: 2–10 months), with a 1-year survival rate of 25.0% (95% CI: 9.1–44.9%) as compared to a median OS of 1 month (95% CI: 0–4 months) and 0.0% 1-year survival rate in patients who did not undergo surgery (Figure 2(b)). Patients receiving both surgery and EBRT had significantly better survival than those who received EBRT or surgery alone (p<0.0001 and p=0.0005, respectively). Median OS after receiving chemotherapy was 6 months (95% CI: 3–11 months), with a 1-year survival rate of 21.4% (95% CI: 5.2–44.8%). There was no significant difference in survival between patients who did and did not receive chemotherapy (p=0.15). In patients who received EBRT, IMRT was associated with a greater but not statistically significant 1-year survival rate (33.3%; 95% CI: 10.3–58.8%) as compared to 2D/3D conformal RT (11.1%; 95% CI: 0.6–38.8%). Curative intent RT also was associated with higher 1-year survival rate (42.9%; 95% CI: 9.8–73.4%) as compared to palliative RT (14.3%; 95% CI: 2.3–36.6%; p=0.0001).
Figure 2.
Overall survival for patients who underwent (a) EBRT versus no EBRT, (b) surgery versus no surgery, and (c) chemotherapy versus no chemotherapy.
Univariate (Table 3) and multivariate analyses (Table 4) were conducted to assess contributors to OS. Univariate analysis showed that stage at presentation, total radiation dose (<4,000 cGy vs. ≥4,000 cGy), fractionation scheme (1 vs. 2 fractions/day), receipt of chemotherapy, presence of initial or concomitant differentiated thyroid cancer diagnosis, lymphovascular invasion, extrathyroidal extension, and leukocytosis were not associated with OS (p>0.05). Age, EBRT, and surgery were associated with OS (p<0.05) and were used for multivariate analysis. Receipt of chemotherapy was also incorporated in the multivariate analysis to include all treatment modalities. The multivariate analysis showed that older age at diagnosis (HR: 1.079; 95% CI: 1.022–1.139; p=0.006) was associated with worse OS, while receipt of EBRT (HR: 0.174; 95% CI: 0.050–0.613; p=0.007) and surgery (HR: 0.198; 95% CI: 0.065–0.598; p=0.004) were associated with improved OS. Receipt of chemotherapy was not associated with OS on multivariate analysis (HR: 0.668; 95% CI: 0.274–1.633; p=0.38).
Table 3.
Univariate overall survival analysis (N=28, # events=26, 7% censored).
| N | Deaths | HR (95% CI) | P-Value | |
|---|---|---|---|---|
| Age at ATC diagnosis (years) | 28 | 1.064 (1.014 - 1.116) | 0.011 | |
|
| ||||
| Stage | 0.18 | |||
| IVA | 2 | 1 (50.0%) | Reference | |
| IVB | 20 | 19 (95.0%) | 3.771 (0.499 - 28.468) | |
| IVC | 5 | 5 (100.0%) | 7.246 (0.804 - 65.269) | |
|
| ||||
| Receipt of EBRT | 0.002 | |||
| No EBRT | 7 | 7 (100.0%) | Reference | |
| EBRT | 21 | 19 (90.5%) | 0.133 (0.038 - 0.463) | |
|
| ||||
| Total locoregional radiation dose (cGy) | 0.32 | |||
| < 4,000 | 11 | 9 (81.8%) | Reference | |
| ≥ 4,000 | 6 | 6 (100.0%) | 1.799 (0.568 - 5.700) | |
|
| ||||
| Radiation fractionation (fractions/day) | 0.12 | |||
| 1 | 8 | 7 (87.5%) | Reference | |
| 2 | 9 | 8 (88.9%) | 0.427 (0.147 - 1.235) | |
|
| ||||
| Receipt of surgery | 0.036 | |||
| No surgery | 8 | 8 (100.0%) | Reference | |
| Surgery | 20 | 18 (90.0%) | 0.384 (0.157 - 0.938) | |
|
| ||||
| Receipt of chemotherapy | 0.21 | |||
| No chemotherapy | 14 | 13 (92.9%) | Reference | |
| Chemotherapy | 14 | 13 (92.9%) | 0.605 (0.276 - 1.323) | |
|
| ||||
| Initial or concomitant diagnosis of differentiated thyroid cancer (papillary or follicular) | 0.31 | |||
| No | 22 | 21 (95.5%) | Reference | |
| Yes | 6 | 5 (83.3%) | 0.602 (0.224 - 1.617) | |
|
| ||||
| Lymphovascular invasion | 0.76 | |||
| No | 5 | 5 (100.0%) | Reference | |
| Yes | 14 | 12 (85.7%) | 0.846 (0.287 - 2.491) | |
|
| ||||
| Extrathyroidal extension | 0.21 | |||
| No | 4 | 3 (75.0%) | Reference | |
| Yes | 23 | 22 (95.7%) | 2.182 (0.649 - 7.340) | |
|
| ||||
| Leukocytosis | 0.12 | |||
| No | 12 | 11 (91.7%) | Reference | |
| Yes | 12 | 11 (91.7%) | 1.994 (0.833 - 4.773) | |
Patients with unknown values for a covariate were excluded from the respective univariate analysis.
Counts and row percentages of deaths are presented for all covariates except for age.
Hazard ratios and confidence intervals are from Cox proportional hazards models, with p-values calculated by Wald chi-square tests.
HR = hazard ratio; CI = confidence interval; EBRT = external beam radiation therapy.
Table 4.
Multivariate overall survival analysis (N=28, # events=26, 7% censored).
| HR (95% CI) | P-Value | |
|---|---|---|
| Age at ATC diagnosis (years) | 1.079 (1.022 -1.139) | 0.006 |
|
| ||
| Receipt of EBRT | ||
| No EBRT | Reference | |
| EBRT | 0.174 (0.050 - 0.613) | 0.007 |
|
| ||
| Receipt of surgery | ||
| No surgery | Reference | |
| Surgery | 0.198 (0.065 - 0.598) | 0.004 |
|
| ||
| Receipt of chemotherapy | ||
| No chemotherapy | Reference | |
| Chemotherapy | 0.668 (0.274 - 1.633) | 0.38 |
Hazard ratios and confidence intervals are from a Cox proportional hazards model, with p-values calculated by a Wald chi-square test.
HR = hazard ratio; CI = confidence interval; EBRT = external beam radiation therapy.
4. Discussion
The published literature on treatment of ATC consists mostly of single-institution retrospective studies with some larger studies and one meta-analysis [17–25]. They agree with the poor prognosis of ATC, encourage consideration of stage and prognostic factors for treatment recommendations, and indicate that a combination of surgery, radiotherapy, and chemotherapy is the most effective treatment regimen for anaplastic thyroid cancer. This study confirms that multimodality treatment leads to improved overall survival, with surgery and radiation therapy serving as the most important aspects of the treatment regimen. Chemotherapy did not provide a significant contribution to survival, corroborating prior studies [14, 26]. Interestingly, among variables incorporated in this analysis, receipt of EBRT was a significant predictor of overall survival. Receipt of EBRT also improved recurrence-free survival. Several studies have suggested that higher EBRT dose (≥40 Gy) is associated with prolonged median survival [14–16], however the lack of randomized prospective studies limits conclusions about the optimal fractionation scheme. One study supported hyperfractionation (46 Gy in 29 fractions) after observing improved local control [27], while others have argued against hyperfractionation due to the absence of survival benefit and increased incidence of toxicities, especially myelopathy [28, 29]. This study did not show a survival benefit from higher EBRT dose (≥40 Gy) or hyperfractionation. A recent preclinical study using an orthotopic mouse model of anaplastic thyroid cancer suggests that hypofractionation may be superior for tumor control and overall survival [30]. The optimal radiation dosing and fractionation plan remains unclear, emphasizing the need for prospective multi-institutional trials to investigate EBRT in anaplastic thyroid cancer patients.
The development of IMRT has been advantageous for head and neck cancer treatment, as it facilitates reduction of dose to nearby normal structures, specifically the spinal cord [5]. The patients in the current study experienced minimal radiation-specific toxicities and infrequently discontinued radiation treatment due to toxicity, possibly due to the increased use of IMRT treatments in this population. Although IMRT has been widely accepted as the radiation technique of choice for treatment of head and neck cancers [31], there is a paucity of published evidence supporting the treatment benefit of IMRT specifically in anaplastic thyroid cancer patients [32]. This study demonstrates an association between IMRT and improved 1-year survival relative to 2D/3D RT, which could be due to superior radiation techniques or better supportive care availability.
While curative radiation therapy is designed to treat all gross and microscopic disease to a dose expected to be lethal to the tumor cells, palliative radiation therapy with smaller treatment fields and/or lower dose may be more appropriate for some patients with distressing symptoms and poor functional status caused by their tumor burden. Because of the potential for severe morbidity from both disease invasion and treatment side effects in ATC, curative versus palliative treatment intent should be considered and discussed with the patient. Current guidelines, based off the AJCC TNM 7th edition staging classification, recommend for Stage IVA patients to be treated curatively and Stage IVC patients to be treated palliatively with exceptions based on personalized patient scenarios [7]. However, in the current study, the majority of patients presented as AJCC TNM 8th Stage IVB (1 of whom would be Stage IVA based on the AJCC TNM 7th edition staging classification), for which guidelines recommend curative versus palliative therapy depending on the resectability of the primary tumor. Treatment intent for Stage IVB patients is a complex decision and should be discussed with a multidisciplinary team and the patient, including consideration of the patient's quality of life. This study showed that curative RT intent corresponded with improved survival as compared to palliative intent. This may be related to patient functional status impacting the treating physician's intent and/or improved outcomes with more aggressive therapeutic approach. Despite the caveat that patients with smaller disease burden and better functional status are more likely to undergo curative treatment in the first place, this finding emphasizes the importance of considering treatment intent in selecting a treatment approach, particularly for Stage IVB patients given that one patient in our study was up-staged from IVA to IVB using the AJCC TNM 8th edition staging classification. Thus, we propose that Stage IVB patients with favorable prognostic factors, including younger age (<70 years old), anaplastic transformation from differentiated thyroid carcinoma, lesser disease extension, and smaller primary tumor size (< 5 cm), should be considered for curative intent therapy [18, 33].
While surgery and EBRT provide improved local control of anaplastic thyroid cancer, the aggressive nature of the disease commonly results in metastatic spread and death. Unfortunately, ATC is poorly responsive to chemotherapy [14, 26, 34]. Targeted therapy and immunotherapy may bring new opportunities for systemic treatment options. Many mutations, including BRAF, NRAS, TP53, HRAS, KRAS, PIK3CA, and RB1, have been identified as potential targets [35]. Several prospective trials have begun studying agents aimed at these mutations. Tyrosine kinase inhibitors, including axitinib, sorafenib, imatinib, and lenvatinib have been shown to cause partial response or stable disease in some ATC patients [36–39]. A phase II trial investigating dabrafenib, a BRAF inhibitor, in combination with trametinib, a MEK inhibitor, showed that this regimen caused a 69% response rate with minimal toxicities [40]. Additionally, case reports have shown initial tumor response from vemurafenib [41], erlotinib [42], and neoadjuvant valproic acid [5, 43]. Novel systemic therapies should also be considered for reducing morbidity in patients being treated palliatively or in patients with acute disease progression. In our study, the two patients who received targeted therapy (bevacizumab or sorafenib) did so under palliative conditions. Even though both of these patients had disease progression while on targeted therapy, they both experienced minimal drug toxicity and had a greater than average overall survival (>4 months) following their ATC diagnosis. Additionally, two reports have shown that the use of a selective BRAF inhibitor was effective in preventing tracheostomy placement after providing rapid relief in patients with impending airway compromise [44]. Overall, further development of systemic therapies should be investigated to improve survival and reduce morbidity in this disease.
This study has several limitations. First, it is a retrospective review, which is prone to bias, misclassification, and measurement error. Second, only 36 patients with ATC were identified at our institution over a 25-year time period, and 8 of these patients had insufficient information in their medical record. Thus, this study is limited by a small number of subjects and poor statistical power. Furthermore, patient performance status was often not readily identifiable in the medical record. Although the multivariate analysis adjusted for factors related to disease prognosis, there were likely unmeasured factors, such as patient performance status, that were related to both treatment decisions and outcomes. Finally, a majority of patients were never disease free through the study time period, producing underestimations for recurrence rate and difficulty interpreting local control. These limitations further emphasize the need for multicenter prospective studies to investigate ATC treatment options in order to identify the most favorable multimodality approach.
5. Conclusions
Despite the limitations in this study and others, several themes have emerged. Surgical resection with EBRT is the most effective modality for local control and has been associated with improved survival. Administering a higher EBRT dose by IMRT is preferred [18], but the optimal RT fractionation scheme remains unclear. Chemotherapy is primarily used for radiosensitization, and the development of more effective systemic therapies is necessary. Inclusion of anaplastic thyroid cancer patients in clinical trials involving targeted and immunotherapies will be helpful for further understanding systemic treatment options. Until better systemic therapies are developed and refined for anaplastic thyroid cancer, likelihood of cure for patients with this aggressive disease remains low, particularly when presenting with later stages of disease.
Data Availability
The clinical data used to support the findings of this study are included within the article and within the supplementary information files.
Conflicts of Interest
No conflicts of interest exist. No competing financial interests exist.
Supplementary Materials
Supplementary Table 1 describes treatment characteristics for patients who underwent EBRT to any body site. Supplementary Table 2 describes treatment characteristics for patients who underwent EBRT to the thyroid/thyroid bed/neck. Supplementary Figure 1 shows the recurrence-free survival for patients who underwent EBRT versus no EBRT. Supplementary Figure 2 shows the overall survival for all patients according to treatment regimen.
References
- 1.Haugen B. R., Alexander E. K., Bible K. C., et al. 2015 American Thyroid Association Management Guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: The American Thyroid Association Guidelines Task Force on thyroid nodules and differentiated thyroid cancer. Thyroid. 2016;26(1):1–133. doi: 10.1089/thy.2015.0020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Howlader N. N. A., Krapcho M., Miller D., et al. SEER Cancer Statistics Review. 1975-2013. http://seer.cancer.gov/csr/1975_2013/ [Google Scholar]
- 3.Sun X. S., Sun S. R., Guevara N., et al. Chemoradiation in anaplastic thyroid carcinomas. Critical Review in Oncology/Hematology. 2013;86(3):290–301. doi: 10.1016/j.critrevonc.2012.10.006. [DOI] [PubMed] [Google Scholar]
- 4.Sharifi A., Shojaeifard A., Soroush A., Jafari M., Abdehgah A. G., Mahmoudzade H. Predictors of regional lymph node recurrence after initial thyroidectomy in patients with thyroid cancer. Journal of Thyroid Research. 2016;2016 doi: 10.1155/2016/4127278.4127278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Smallridge R. C., Copland J. A. Anaplastic thyroid carcinoma: pathogenesis and emerging therapies. Clinical Oncology. 2010;22(6):486–497. doi: 10.1016/j.clon.2010.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stavas M. J., Shinohara E. T., Attia A., Ning M. S., Friedman J. M., Cmelak A. J. Short course high dose radiotherapy in the treatment of anaplastic thyroid carcinoma. Journal of Thyroid Research. 2014;2014 doi: 10.1155/2014/764281.764281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Smallridge R. C., Ain K. B., Asa S. L., et al. American Thyroid Association guidelines for management of patients with anaplastic thyroid cancer. Thyroid. 2012;22(11):1104–1139. doi: 10.1089/thy.2012.0302. [DOI] [PubMed] [Google Scholar]
- 8.de Crevoisier R., Baudin E., Bachelot A., et al. Combined treatment of anaplastic thyroid carcinoma with surgery, chemotherapy, and hyperfractionated accelerated external radiotherapy. International Journal of Radiation Oncology • Biology • Physics. 2004;60(4):1137–1143. doi: 10.1016/j.ijrobp.2004.05.032. [DOI] [PubMed] [Google Scholar]
- 9.Shimaoka K., Schoenfeld D. A., DeWys W. D., Creech R. H., DeConti R. A randomized trial of doxorubicin versus doxorubicin plus cisplatin in patients with advanced thyroid carcinoma. Cancer. 1985;56(9):2155–2160. doi: 10.1002/1097-0142(19851101)56:9<2155::AID-CNCR2820560903>3.0.CO;2-E. [DOI] [PubMed] [Google Scholar]
- 10.Higashiyama T., Ito Y., Hirokawa M., et al. Induction chemotherapy with weekly paclitaxel administration for anaplastic thyroid carcinoma. Thyroid. 2010;20(1):7–14. doi: 10.1089/thy.2009.0115. [DOI] [PubMed] [Google Scholar]
- 11.Ain K. B., Egorin M. J., DeSimone P. A. Treatment of anaplastic thyroid carcinoma with paclitaxel: phase 2 trial using ninety-six-hour infusion. collaborative anaplastic thyroid cancer health intervention trials (CATCHIT) group. Thyroid. 2000;10(7):587–594. doi: 10.1089/thy.2000.10.587. [DOI] [PubMed] [Google Scholar]
- 12.Onoda N., Sugino K., Higashiyama T., et al. The safety and efficacy of weekly paclitaxel administration for anaplastic thyroid cancer patients: a nationwide prospective study. Thyroid. 2016;26(9):1293–1299. doi: 10.1089/thy.2016.0072. [DOI] [PubMed] [Google Scholar]
- 13.Aldehaim M., Mahmood R., Hussain F., et al. Anaplastic thyroid cancer: a retrospective analysis of 120 cases. The Gulf Journal of Oncology. 2014:32–37. [PubMed] [Google Scholar]
- 14.Pierie J.-P. E. N., Muzikansky A., Gaz R. D., Faquin W. C., Ott M. J. The effect of surgery and radiotherapy on outcome of anaplastic thyroid carcinoma. Annals of Surgical Oncology. 2002;9(1):57–64. doi: 10.1245/aso.2002.9.1.57. [DOI] [PubMed] [Google Scholar]
- 15.Wang Y., Tsang R., Asa S., Dickson B., Arenovich T., Brierley J. Clinical outcome of anaplastic thyroid carcinoma treated with radiotherapy of once- and twice-daily fractionation regimens. Cancer. 2006;107(8):1786–1792. doi: 10.1002/cncr.22203. [DOI] [PubMed] [Google Scholar]
- 16.Sherman E. J., Lim S. H., Ho A. L., et al. Concurrent doxorubicin and radiotherapy for anaplastic thyroid cancer: a critical re-evaluation including uniform pathologic review. Radiotherapy & Oncology. 2011;101(3):425–430. doi: 10.1016/j.radonc.2011.09.004. [DOI] [PubMed] [Google Scholar]
- 17.Mohebati A., Dilorenzo M., Palmer F., et al. Anaplastic thyroid carcinoma: A 25-year single-institution experience. Annals of Surgical Oncology. 2014;21(5):1665–1670. doi: 10.1245/s10434-014-3545-5. [DOI] [PubMed] [Google Scholar]
- 18.Sugitani I., Miyauchi A., Sugino K., Okamoto T., Yoshida A., Suzuki S. Prognostic factors and treatment outcomes for anaplastic thyroid carcinoma: ATC research consortium of Japan cohort study of 677 patients. World Journal of Surgery. 2012;36(6):1247–1254. doi: 10.1007/s00268-012-1437-z. [DOI] [PubMed] [Google Scholar]
- 19.Haigh P. I., Ituarte P. H. G., Wu H. S., et al. Completely resected anaplastic thyroid carcinoma combined with adjuvant chemotherapy and irradiation is associated with prolonged survival. Cancer. 2001;91(12):2335–2342. doi: 10.1002/1097-0142(20010615)91:12<2335::AID-CNCR1266>3.3.CO;2-T. [DOI] [PubMed] [Google Scholar]
- 20.Ito K.-I., Hanamura T., Murayama K., et al. Multimodality therapeutic outcomes in anaplastic thyroid carcinoma: Improved survival in subgroups of patients with localized primary tumors. Head & Neck. 2012;34(2):230–237. doi: 10.1002/hed.21721. [DOI] [PubMed] [Google Scholar]
- 21.Park J. W., Choi S. H., Yoon H. I., et al. Treatment outcomes of radiotherapy for anaplastic thyroid cancer. Radiation Oncology Journal. 2018;36(2):103–113. doi: 10.3857/roj.2018.00045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Foote R. L., Molina J. R., Kasperbauer J. L., et al. Enhanced survival in locoregionally confined anaplastic thyroid carcinoma: a single-institution experience using aggressive multimodal therapy. Thyroid. 2011;21(1):25–30. doi: 10.1089/thy.2010.0220. [DOI] [PubMed] [Google Scholar]
- 23.Kwon J., Kim B. H., Jung H.-W., Besic N., Sugitani I., Wu H.-G. The prognostic impacts of postoperative radiotherapy in the patients with resected anaplastic thyroid carcinoma: A systematic review and meta-analysis. European Journal of Cancer. 2016;59:34–45. doi: 10.1016/j.ejca.2016.02.015. [DOI] [PubMed] [Google Scholar]
- 24.Goffredo P., Thomas S. M., Adam M. A., Sosa J. A., Roman S. A. Impact of timeliness of resection and thyroidectomy margin status on survival for patients with anaplastic thyroid cancer: an analysis of 335 cases. Annals of Surgical Oncology. 2015;22(13):4166–4174. doi: 10.1245/s10434-015-4742-6. [DOI] [PubMed] [Google Scholar]
- 25.Baek S.-K., Lee M.-C., Hah J. H., et al. Role of surgery in the management of anaplastic thyroid carcinoma: Korean nationwide multicenter study of 329 patients with anaplastic thyroid carcinoma, 2000 to 2012. Head & Neck. 2017;39(1):133–139. doi: 10.1002/hed.24559. [DOI] [PubMed] [Google Scholar]
- 26.Yau T., Lo C. Y., Epstein R. J., Lam A. K. Y., Wan K. Y., Lang B. H. Treatment outcomes in anaplastic thyroid carcinoma: Survival improvement in young patients with localized disease treated by combination of surgery and radiotherapy. Annals of Surgical Oncology. 2008;15(9):2500–2505. doi: 10.1245/s10434-008-0005-0. [DOI] [PubMed] [Google Scholar]
- 27.Tennvall J., Lundell G., Wahlberg P., et al. Anaplastic thyroid carcinoma: three protocols combining doxorubicin, hyperfractionated radiotherapy and surgery. British Journal of Cancer. 2002;86(12):1848–1853. doi: 10.1038/sj.bjc.6600361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dandekar P., Harmer C., Barbachano Y., et al. Hyperfractionated Accelerated Radiotherapy (HART) for anaplastic thyroid carcinoma: toxicity and survival analysis. International Journal of Radiation Oncology • Biology • Physics. 2009;74(2):518–521. doi: 10.1016/j.ijrobp.2008.08.016. [DOI] [PubMed] [Google Scholar]
- 29.Wong C. S., Van Dyk J., Simpson W. J. Myelopathy following hyperfractionated accelerated radiotherapy for anaplastic thyroid carcinoma. Radiotherapy & Oncology. 1991;20(1):3–9. doi: 10.1016/0167-8140(91)90105-P. [DOI] [PubMed] [Google Scholar]
- 30.Oweida A., Phan A., Vancourt B., et al. Hypofractionated radiotherapy is superior to conventional fractionation in an orthotopic model of anaplastic thyroid cancer. Thyroid. 2018;28(6):739–747. doi: 10.1089/thy.2017.0706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.O'Sullivan B., Rumble R. B., Warde P. Intensity-modulated Radiotherapy in the treatment of head and neck cancer. Clinical Oncology. 2012;24(7):474–487. doi: 10.1016/j.clon.2012.05.006. [DOI] [PubMed] [Google Scholar]
- 32.O'Neill J. P., Shaha A. R. Anaplastic thyroid cancer. Oral Oncology. 2013;49(7):702–706. doi: 10.1016/j.oraloncology.2013.03.440. [DOI] [PubMed] [Google Scholar]
- 33.Akaishi J., Sugino K., Kitagawa W., et al. Prognostic factors and treatment outcomes of 100 cases of anaplastic thyroid carcinoma. Thyroid. 2011;21(11):1183–1189. doi: 10.1089/thy.2010.0332. [DOI] [PubMed] [Google Scholar]
- 34.Schlumberger M., Parmentier C., Droz J., Sarrazin D., Delisle M., Couette J. Combination therapy for anaplastic giant cell thyroid carcinoma. Cancer. 1991;67(3):564–566. doi: 10.1002/1097-0142(19910201)67:3<564::AID-CNCR2820670306>3.0.CO;2-E. doi: 10.1002/1097-0142(19910201)67:3<564::AID-CNCR2820670306>3.0.CO;2-E. [DOI] [PubMed] [Google Scholar]
- 35.Chen H., Luthra R., Routbort M. J., et al. Molecular profile of advanced thyroid carcinomas by next-generation sequencing: Characterizing tumors beyond diagnosis for targeted therapy. Molecular Cancer Therapeutics. 2018;17(7):1575–1584. doi: 10.1158/1535-7163.MCT-17-0871. [DOI] [PubMed] [Google Scholar]
- 36.Ha H. T., Lee J. S., Urba S., et al. A phase II study of imatinib in patients with advanced anaplastic thyroid cancer. Thyroid. 2010;20(9):975–980. doi: 10.1089/thy.2010.0057. [DOI] [PubMed] [Google Scholar]
- 37.Gupta-Abramson V., Troxel A. B., Nellore A., et al. Phase II trial of sorafenib in advanced thyroid cancer. Journal of Clinical Oncology : Official Journal of the American Society of Clinical Oncology. 2008;26(29):4714–4719. doi: 10.1200/JCO.2008.16.3279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cohen E. E. W., Rosen L. S., Vokes E. E., et al. Axitinib is an active treatment for all histologic subtypes of advanced thyroid cancer: results from a phase II study. Journal of Clinical Oncology : Official Journal of the American Society of Clinical Oncology. 2008;26(29):4708–4713. doi: 10.1200/jco.2007.15.9566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tahara M., Kiyota N., Yamazaki T., et al. Lenvatinib for anaplastic thyroid cancer. Frontiers in Oncology. 2017;7, article no. 25 doi: 10.3389/fonc.2017.00025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Subbiah V., Cabanillas M. E., Kreitman R. J., et al. Dabrafenib and trametinib treatment in patients with locally advanced or metastatic BRAF V600–mutant anaplastic thyroid cancer. Journal of Clinical Oncology. 2018;36(1):7–13. doi: 10.1200/JCO.2017.73.6785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Marten K. A., Gudena V. K. Use of vemurafenib in anaplastic thyroid carcinoma: a case report. Cancer Biology & Therapy. 2015;16(10):1430–1433. doi: 10.1080/15384047.2015.1071734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hogan T., Yu J. J., Williams H. J., Altaha R., Liang X., He Q. Oncocytic, focally anaplastic, thyroid cancer responding to erlotinib. Journal of Oncology Pharmacy Practice : Official Publication of the International Society of Oncology Pharmacy Practitioners. 2009;15(2):111–117. doi: 10.1177/1078155208101212. [DOI] [PubMed] [Google Scholar]
- 43.Noguchi H., Yamashita H., Murakami T., et al. Successful treatment of anaplastic thyroid carcinoma with a combination of oral valproic acid, chemotherapy, radiation and surgery. Endocrine Journal. 2009;56(2):245–249. doi: 10.1507/endocrj.K08E-016. [DOI] [PubMed] [Google Scholar]
- 44.Cabanillas M. E., Ferrarotto R., Garden A. S., et al. Neoadjuvant BRAF-and Immune-directed therapy for anaplastic thyroid carcinoma. Thyroid. 2018;28(7):945–951. doi: 10.1089/thy.2018.0060. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table 1 describes treatment characteristics for patients who underwent EBRT to any body site. Supplementary Table 2 describes treatment characteristics for patients who underwent EBRT to the thyroid/thyroid bed/neck. Supplementary Figure 1 shows the recurrence-free survival for patients who underwent EBRT versus no EBRT. Supplementary Figure 2 shows the overall survival for all patients according to treatment regimen.
Data Availability Statement
The clinical data used to support the findings of this study are included within the article and within the supplementary information files.