Abstract
Purpose
Lung cancer is the leading cause of U.S. cancer deaths and radon is the second leading risk factor for lung cancer. By better understanding geologic variations of radon production in states, comprehensive cancer control efforts could be improved. The study purpose was to assess states with the greatest potential for elevated radon and the likelihood of radon-related actions in National Comprehensive Cancer Control Program (NCCCP) awardee cancer plans.
Methods
Two state-level variables were derived to approximate potential for elevated radon using the Environmental Protection Agency county map and the 2015 U.S. Census. The association between radon potential and inclusion of radon activity within cancer plans was evaluated using logistic regression.
Results
Fifty-one percent of cancer plans recognized an association between radon and cancer risk, and included measurable radon activities. Most states with high radon potential included radon activity in cancer plans. Both measures of radon potential were significantly associated with NCCCP cancer plans including radon activity.
Conclusions
Geospatial analyses help to prioritize radon-related lung cancer activities. In areas with high potential for radon exposure, increasing knowledge about potential for radon exposure may result in increased radon testing, mitigation, or other radon reducing strategies, and ultimately reduction of lung cancer deaths.
Keywords: Radon, Comprehensive cancer control, Lung neoplasms, Neoplasms, Cancer, Population groups, Carcinogens, Environmental health
Introduction
Lung cancer is the leading cause of cancer death in the United States [1] and radon is the second leading risk factor for lung cancer. Further, radon exposure increases lung cancer risk in smokers above smoking alone. Regardless of smoking status, radon exposure is an independent risk factor for lung cancer and responsible for approximately 21,000 cases per year (10–15% of all lung cancer cases) [2–7]. Radon is an invisible, odorless, and tasteless radioactive gas that readily enters homes through cracks in walls, floors, or foundations. It can also be present in water, another potential source of exposure [8]. Local soil composition, foundation type, air sealing, indoor-soil air-pressure differences, and many other characteristics determine radon concentrations within homes [8]. The U.S. Environmental Protection Agency (EPA) estimates that one in 15 residences in the United States (~ 7 million homes) exceed the radon level at which mitigation is recommended to reduce radon exposure [4.0 pCi/L (picocuries per liter of air)] [9]. Picocuries per liter of air, or pCi/L, is used in the United States, as the preferred measurement for the speed of decay in radon. The U.S. Surgeon General and the EPA recommend all homes be tested regardless of geographic location, as homes with elevated radon levels have been identified in all geographic areas [9, 10].
CDC’s National Comprehensive Cancer Control Program (NCCCP) funds comprehensive cancer control planning and implementation in every state, the District of Columbia, six U.S. Associated Pacific Island Jurisdictions (USAPIJs), Puerto Rico, and eight tribes or tribal organizations [11]. NCCCP awardees bring together stakeholders to create plans to prevent or minimize the impact of cancer in communities. As such, cancer plans are designed to be instrumental in developing and prioritizing screening initiatives, education and outreach programs, treatment, and prevention programs to reduce the local cancer burden. From this perspective, NCCCP awardees are uniquely positioned to leverage resources that help promote the use of appropriate activities and strategies to reduce radon exposure. These strategies can include radon testing of residences and buildings, remediating residences where necessary, educating the public and decision-makers about radon testing and radon-resistant construction designs, professional licensing, and radon notification during real estate transactions, among others. Previous studies determined approximately 42% (in the year 2011) and 49% (2015) of NCCCP awardee cancer plans included radon-related activity [12, 13], an indicator of awareness and need for increased testing and radon-resistant construction as lung cancer prevention strategies.
A better understanding of the geologic variations of potentially elevated radon levels (radon potential) and geographic differences in lung cancer burden will inform comprehensive cancer control efforts, allowing for improvements that may more appropriately address the specific burden of radon exposure and lung cancer at the state, territorial, and tribal level. Equipped with such information, NCCCP awardees in corresponding states, territories, and tribes; and coalition partners may be able to better help direct resources and improve compliance with existing local radon-related policies when appropriate. Therefore, the study purpose is to assess the likelihood of radon-related actions in NCCCP awardee cancer plans, and determine where, geographically the greatest need for radon-related activity may exist.
Methods
Current cancer plans for all 66 current NCCCP awardees (http://www.cdc.gov/cancer/ncccp/ccc_plans.htm) were reviewed in May 2018. An updated cancer plan was requested from all awardees whose cancer plan ended prior to 2018. Only updated plans available on-line and/or received from awardees were included in the analysis (N = 63). Cancer plans for three NCCCP awardees were not available at the time of the study. Using the Adobe Acrobat Pro version 2015.006 (Adobe Systems Inc, San Jose, CA) search tool, we utilized the key terms “radon,” “radiation,” and “lung” independently to identify plans with possible radon-related activity. All cancer plan activities pertaining to lung cancer and environmental health were reviewed for radon-related content. All activities were then classified as pertaining to one or more of the following: recognition of radon as a carcinogen; improving awareness of radon among their population; home testing for radon; mitigating buildings with elevated radon levels; supporting education or implementation of radon policy activities; and efforts to evaluate radon-specific policy activities.
The EPA county radon zone map [14] was used as a proxy measure for radon potential in all 50 U.S. states and the District of Columbia. This map uses a variety of data to categorize each U.S. county into one of three zones of predicted average indoor radon potential relative to the EPA’s action level of 4 pCi/L: zone 1 counties greater than 4 pCi/L, zone 2 counties 2–4 pCi/L, and zone 3 counties < 2 pCi/L. This map is intended for use by national, state, and local organizations to target their resources and to implement radon-resistant building codes [14].
We derived two state-level variables to approximate radon potential using the EPA county map and the 2015 U.S. Census: (1) percent EPA zone 1 and (2) population-weighted average radon zone. Percent EPA zone 1 was defined as the proportion of counties within each state designated as zone 1 by EPA. This is a basic indicator of total geographic area related to increased potential for radon exposure. For example, New York has 62 counties in the EPA map and 34 (55%) are zone 1. However, zone 1 percentage does not account for the population density within each county (e.g., the city of New York is an EPA zone 3); therefore a population-weighted average radon variable was derived to adjust for state population density within each county by assigning the value equal to its EPA radon zone (i.e., zone 1 = 1, zone 2 = 2, zone 3 = 3) and then weighting it by the estimated population from the U.S. Census Bureau [15] (e.g., the weight of a county with 5000 residents would be five times more than a county with 1000 residents). The weighted average for each state was then calculated across all counties. The population-weighted radon zone variable is on a continuous scale and ranges from 1.0 to 3.0, with one indicating higher potential radon concentration and 3.0 indicating lower potential radon concentration. For example, Georgia has 159 counties: zone 1 (n = 4), zone 2 (n = 55), and zone 3 (n = 100). A simple mean average is equal to 2.6 because most of Georgia’s counties are zone 2 and 3. However, approximately one-third of Georgia’s population resides in four counties, all of which are EPA zone 1. Thus, after adjusting for population density within each EPA zone, the population-weighted average for Georgia moves closer to 2.0 (1.98). All data joining and aggregation to derive these variables were completed using ArcMap 10.5 (ESRI, Redlands, CA, USA).
The association between radon potential and inclusion of radon activity within current NCCCP cancer plans was evaluated for state and the District of Columbia cancer plans only (n = 51) due to lack of EPA-specific data for tribes, territories, and USAPIJs. Using two logistic regression models, one for each of the state-level radon potential variables, we first evaluated the relationship between states’ percent EPA zone 1 and the odds of radon activity included in NCCCP cancer plans. The second model evaluated the relationship between states’ population-weighted average radon zone and the odds of radon activity included in NCCCP cancer plans. These two variables for radon potential were not included in the same model because they were highly correlated. All statistical analyses were conducted using SAS 9.4 (SAS Institute, Cary, NC, USA). Results were considered significant if p < 0.05.
Both logistic regression models controlled for confounding by the incidence of lung cancer and prevalence of non-smokers within each state under the assumption that these two factors might influence cancer plan activity (see equations below).
PercEPA1 = the percent of counties in a given state rated zone 1 by the EPA radon map, PopWtRn = the population-weighted average radon zone in a given state, LC = the age-adjusted state lung cancer incidence (2010–2014), and NeverSmoke = the proportion of the population identified as never smoker in a given state.
To describe the incidence of lung cancer in the United States, we analyzed cancer incidence data from the CDC’s U.S Cancer Statistics (USCS) [16] using average annual age-adjusted incidence rates for new cases of trachea, lung, and bronchus (C33.9–34.9) cancer diagnosed during 2010–2014. Data from all registries except Nevada met U.S. Cancer Statistics publication criteria [17], covering 99% of the U.S. population (Nevada was therefore excluded from logistic regression modeling because their registry data did not meet USCS publication criteria and n = 50 for all logistic regression analyses). Per registry standards, only cases of invasive cancer (i.e., cancer that has spread beyond the layer of tissue in which it developed and is growing into surrounding health tissues) were included. Smoking data were obtained from CDC’s 2016 Behavioral Risk Factor Surveillance System (BRFSS) [18] to determine the proportion of adults in each state who self-identified as having never smoked. The BRFSS is an ongoing surveillance system designed to measure behavioral risk factors for the non-institutionalized adult population (aged 18 years of age and older). BRFSS is a representative, state-based telephone survey that recruits residents via landline or mobile phone [18].
Results
Eighty-four percent (53 of 63) of cancer plans included at least one key word potentially associated with radon (Table 1). Fifty-one percent (32 of 63) of cancer plans recognized an association between radon and cancer risk, and included at least one measurable activity related to radon. Specific types of radon-related activities in the cancer plans reviewed included: improve awareness of radon as a risk factor for lung cancer (44%), increase residential radon testing (41%), supporting radon mitigation (29%), supporting education or increased implementation of existing radon policy (27%), and evaluation of existing radon policies (6%).
Table 1.
Radon content and activities in National Comprehensive Cancer Control Program plans, 2017
| Total plans reviewed | Radon-related termsa | Recognition | Measurable activities | Awareness | Home testing (identify) | Mitigation | Supporting radon policy activities | Policy evaluation |
|---|---|---|---|---|---|---|---|---|
| N | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) |
| 63 | 53 (84.1) | 32 (50.8) | 32 (50.8) | 28 (44.4) | 26 (41.3) | 18 (28.6) | 17 (27.0) | 4 (6.3) |
All plans reviewed were searched for the key terms “radon” and “radiation”
Of the 50 states included in the logistic regression analysis (i.e., the District of Columbia and all states except Nevada), the mean for percent EPA zone 1 counties was 33% (n = 50), with states ranging from 100% EPA zone 1 (n = 2) to 0% EPA zone 1 (n = 13), and a median percent EPA zone 1 of 25% (Fig. 1). All 50 states included had an average population-weighted average radon zone closer to 2.0 (n = 50), with states ranging from 1.0 (n = 2) to 3.0 (n = 3) and a median 1.8. Overall (including all states), the average EPA zone not weighted by population was similar (closer to 2.0), but some individual states’ weighted and unweighted average radon zone varied greatly.
Fig. 1.
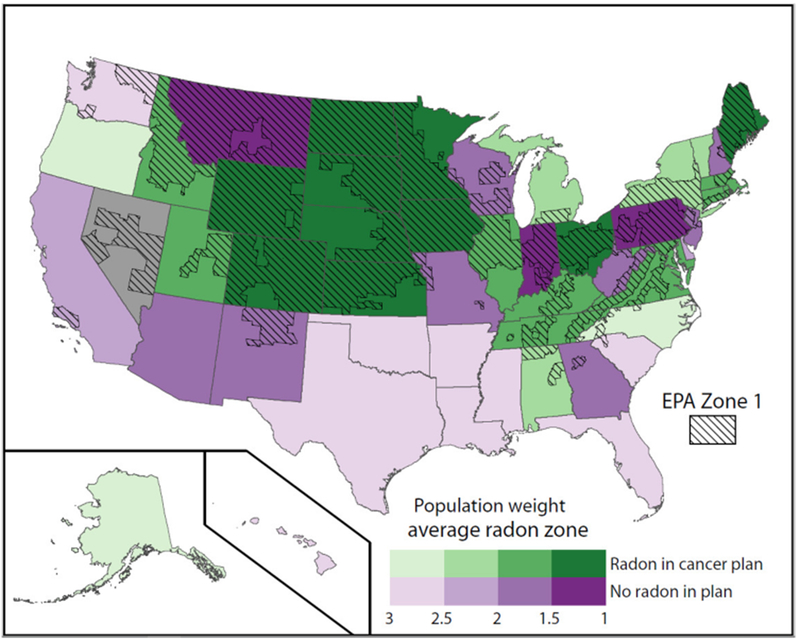
EPA Zone 1 counties, population-weighted average radon zone, and presence of radon activity in NCCCP grantee cancer plans. EPA zone 1 counties are represented on the map with hashmarks. Increasing radon concentration is indicated by increasingly darker color shading (green or purple). Green shading indicates that at least one radon activity is included in the state cancer plan. Purple shading indicates that no radon-related activity are included in the state cancer plan. Gray shading indicates that Nevada was excluded from logistic regression modeling because their registry data did not meet USCS publication criteria All states (and the District of Columbia) are included in this analysis (n = 51). (Color figure online)
Population-weighted average radon zone and radon activity in NCCCP cancer plans for each state are also shown in Fig. 1. The majority of states with a high percent of EPA zone 1 counties (75–100%) and population-weighted average radon zone with higher potential radon concentration (1.0–1.5) included at least one radon activity in their cancer plan (33 of 36, 92%). A few states (i.e., Iowa, Montana, Pennsylvania) with a high percent of EPA zone 1 counties and population-weighted average radon zone with higher potential radon concentration did not include radon activity in their most recent cancer plan (3 of 36, 8%).
Table 2 shows the results of logistic regression analyses. There is a significant association between both variables approximating radon potential (i.e., the percent of zone 1 counties and the population-weighted average radon) in a state and the odds of that state’s cancer plan including radon activity (after controlling for lung cancer incidence and the proportion of the population who were never smokers). Each percentage increase in EPA zone 1 counties resulted in a 4% (OR 1.04, 95% CI 1.02 to 1.07) increase in the odds of radon activity inclusion in cancer plans. Similarly, for each increase in population-weighted average radon zone (i.e., increase from 1.0 (higher radon potential) to 2.0 (lower radon potential) indicating more of the population is located in zones with lower predicted radon potential) there is an 84% (OR 0.16, 95% CI 0.05 to 0.54) decrease in the odds of radon’s inclusion in cancer plans. In both equations, the two control variables were not significant.
Table 2.
Adjusted logistic regression for the association between radon potential and inclusion of radon activity in NCCCP awardee state cancer plans
| Odds ratio (95% confidence interval) | |
|---|---|
| Percent EPA zone 1 | 1.04 (1.02, 1.07) |
| Population-weighted EPA zone 1 | 0.16 (0.05, 0.51) |
Regression analyses included all states and the District of Columbia with high-quality cancer incidence data (N = 50, Nevada was excluded). Rates were adjusted for lung cancer incidence and adult smoking prevalence. Cancer incidence data were from the most recent year of United States Cancer Statistics and covered 99% of the U.S. population. Smoking data were from the 2016 Behavioral Risk Factor Surveillance System. EPA radon zones and population-weighted radon zones were calculated as described in the “Methods”. Population weights were from the U.S. Census Bureau
Discussion
We identified NCCCP awardees with radon activity in their respective cancer plans, geographic areas where there is a higher radon potential, and whether radon potential was associated with cancer plan radon activity. States with high radon potential could consider including and prioritizing radon-related activities and actions, if not already in progress. Although the majority of states located in geographic regions identified with a high percent of EPA zone 1 counties and with population-weighted average radon zone with higher potential radon concentration already included radon-related activities, additional states, such as Iowa, Montana, and Pennsylvania, may need to assess current cancer plan radon-related activities. These states could improve lung cancer prevention efforts (particularly for non-smokers) by working with local partners (e.g., real estate agents, builders, radon professionals, state radon program) that have existing knowledge of radon reduction efforts. Regardless of state policies, research has shown that people who report hearing of radon-related health issues are 2–4 times more likely to test their home for radon, and including information on radon associations with cancer risk in cancer plans could increase awareness of this issue [19].
As part of the Federal and National Radon Action Planning to better identify and address radon exposure in the United States [20], CDC encourages state cancer control plans to prioritize radon by including strategies for reducing radon. This study yielded several positive findings. Higher radon potential was associated with increased odds of radon activity in NCCCP cancer plans. Sustained increases in radon-related information and activities in cancer plans were also shown (from 2010 [42%] to 2015 [49%] to 2018 [51%]), which highlights cancer coalitions’ increasing awareness of the cancer risk posed by radon and how prevention efforts can reduce risk for lung cancer. Recent cancer plans have increased activities related to supporting education or increased implementation of an existing radon policy (27%) and evaluation of existing radon policies (6%). States with existing radon laws and required certifications for radon mitigation professionals could incorporate support of these policies into their cancer plans to promote radon reduction planned activities or those already in progress.
Approximately one-third of NCCCP cancer plans had no mention of radon, and almost half did not include measurable activity related to radon. Most of these states were in areas with low potential for radon exposure. NCCCP awardees receive funding [21], which they use to support coalitions to identify the highest burden cancers in their jurisdictions and strategically prioritize interventions to reduce those cancers. Our study provides valuable information that can help awardees with this prioritization. The geospatial analyses presented here can serve as a useful model that can be adapted to other cancer types and areas along the continuum for NCCCP awardees. They may also be helpful for other public health programs in prioritizing their activities and resources.
EPA states that all homes should be tested for radon regardless of geographic location, as homes with elevated radon levels have been identified in all geographic areas [9]. There are additional federal and state programs to help fund radon reduction in homes that are affordable to families with limited incomes. EPA funds state and tribal radon control programs to subsidize or encourage radon testing in residences and schools, encourage radon-resistant building practices, and develop professional licensure programs (http://www.epa.gov/radon/sirgprogram.html). State radon offices [14] are the most knowledgeable source of state-specific information related to radon potential, policies, testing/mitigation programs and subsidies, radon professionals, and ongoing radon-related environmental activities. NCCCP awardees in areas with high potential for radon exposure would benefit from adding respective state and local radon officials to their cancer coalition. This could lead to leveraging existing resources and infrastructure that help to improve cancer control in their communities. NCCCP awardees in areas with low potential for radon exposure could consider contacting local radon professionals to proactively establish an ongoing relationship in the case that cancer-related radon priorities change in their state.
This study is subject to at least five limitations. First, NCCCP cancer plans are static and represent the priorities when written, and may not reflect the most up-to-date or complete view of awardee and/or state activities related to radon, and three NCCCP cancer plans published after Spring 2018, were not included. Second, some states may be addressing radon in ways not reflected in the NCCCP cancer plan. For example, several states require certification for radon mitigation professionals and/or notification policies for single-family home transactions [22]. Yet still, other states’ radon efforts may be concentrated in the Department of Environmental Protection as opposed to the Health Department, which may influence the degree of existing collaboration. Third, the association between radon potential and NCCCP cancer plan radon activity may be influenced by other explanatory variables (e.g., political, socioeconomic, behavioral, environmental) which we did not examine in this study. Fourth, currently, the only national resource for radon data is the EPA Radon Zone map created/published in [9]. More recently state radon programs have begun collecting, analyzing, and publishing radon testing result information by county. However, these data are state specific and the data collection methods vary by state. The National Environmental Public Health Tracking Network has convened a national radon-working group that is in the process of developing a national radon database. Finally, in regard to estimating potential for radon exposure, the number of counties in each state is variable (e.g., western states often have fewer/larger counties) and the percent of EPA zone measure could possibly be skewed. We attempted to validate this estimate through the use of a second estimate that adjusted for population density within counties.
In summary, more than 150,000 men and women in the United States die from lung cancer each year [1]. Our geospatial analyses help NCCCP awardees to prioritize their radon-related lung cancer activities. In areas with high potential for radon exposure, NCCCP awardees could consider having multiple specific objectives and strategies to reduce exposure and prevent lung cancer, as resources allow. At a minimum, simply increasing knowledge about radon as a major risk factor for lung cancer, especially among non-smokers, may be beneficial. NCCCP awardees can synergistically work with other public health professionals in their state to ensure that all homes are tested for radon.
Acknowledgments
All authors were involved in conceptualizing, executing, developing, and reviewing this manuscript. The contents of this article have not been previously presented elsewhere.
Funding This study was funded by the Centers for Disease Control and Prevention.
Footnotes
Publisher's Disclaimer: Disclaimer The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Conflict of interest The authors declare that they have no conflict of interest.
Informed consent It was obtained from all individual participants included in the study.
Research involving human and animal rights This article does not contain any studies with human participants or animals by any of the authors.
References
- 1.U.S. Cancer Statistics Working Group (2017) United States cancer statistics: 1999–2014 incidence and mortality web-based report. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention and National Cancer Institute, Atlanta [Google Scholar]
- 2.Leffalle L, Kripke M (2010) 2008–2009 president’s cancer panel: reducing environmental cancer risk. In: What we can do now. U.S. Department of Health and Human Services, National Institutes of Health, National Cancer Institute, Washington, DC [Google Scholar]
- 3.National Research Council (1999) Health effects of exposure to radon: BEIR VI. National Research Council Commission on Life Sciences, Washington, DC [Google Scholar]
- 4.Samet JM, Avila-Tang E, Boffetta P, Hannan LM, Olivo-Marston S, Thun MJ et al. (2009) Lung cancer in never smokers: clinical epidemiology and environmental risk factors. Clin Cancer Res 15(18):5626–5645. 10.1158/1078-0432.ccr-09-0376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Darby S, Hill D, Auvinen A, Barrios-Dios JM, Baysson H, Bochicchio F et al. (2005) Radon in homes and risk of lung cancer: collaborative analysis of individual data from 13 European casecontrol studies. BMJ 330(7485):223–226. 10.1136/bmj.38308.477650.63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Krewski D, Lubin JH, Zielinski JM, Alavanja M, Catalan VS, Field RW et al. (2005) Residential radon and risk of lung cancer—a combined analysis of 7 north American case-control studies. Epidemiology 16(2):137–145. 10.1097/01.ede.0000152522.80261.e3 [DOI] [PubMed] [Google Scholar]
- 7.Lubin JH, Wang ZY, Boice JD Jr, Xu ZY, Blot WJ, De Wang L et al. (2004) Risk of lung cancer and residential radon in China: pooled results of two studies. Int J Cancer 109(1):132–137. 10.1002/ijc.11683 [DOI] [PubMed] [Google Scholar]
- 8.U.S. Environmental Protection Agency. EPA assessment of risks from radon in homes (2003) http://www.epa.gov/radon/pdfs/402-r-03-003.pdf Accessed 21 June 2018
- 9.U.S. Environmental Protection Agency (2016) Consumer’s guide to radon reduction. U.S. Environmental Protection Agency, Washington, D.C. [Google Scholar]
- 10.U.S. Department of Health and Human Services (2009) The surgeon general’s call to action to promote health homes. In: U.S. Department of Health and Human Services OotSG, editor. Rockville [Google Scholar]
- 11.Division of Cancer Prevention and Control Centers for Disease Control and Prevention. National Comprehensive Cancer Control Program (NCCCP) (2017) https://www.cdc.gov/cancer/ncccp/ Accessed 3rd April 2017
- 12.Acree P, Puckett M, Neri A (2017) Evaluating progress in radon control activities for lung cancer prevention in national comprehensive cancer control program plans, 2011–2015. Journal of community health 42(5):962–967. 10.1007/s10900-017-0342-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Neri A, Stewart SL, Angell W (2013) Radon control activities for lung cancer prevention in national comprehensive cancer control program plans, 2005–2011. Prev Chronic Dis 10:E132 10.5888/pcd10.120337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.U.S. Environmental Protection Agency. EPA Map of Radon Zones (1993) https://www.epa.gov/radon/epa-map-radon-zones Accessed 20 March 2018
- 15.U.S. Census Bureau. American Community Survey, 2015 American Community Survey 1-Year Estimates generated using American FactFinder (2015) http://factf.inder2.census.gov Accessed 28 March 2017
- 16.U.S. Cancer Statistics Working Group (2017) United States cancer statistics: 1999–2014 incidence and mortality web-based report. Atlanta, GA: http://www.cdc.gov/uscs [Google Scholar]
- 17.U.S. Cancer Statistics Working Group (2017) U.S. Cancer Statistics Publication Criteria. Atlanta [Google Scholar]
- 18.Centers for Disease Control and Prevention (2015) BRFSS Survey Data and Documentation. 2017 https://www.cdc.gov/brfss/annual_data/annual_2015.html Accessed 19 April 2018
- 19.Neri A, McNaughton C, Momin B, Puckett M, Gallaway MS (2018) Measuring public knowledge, attitudes, and behaviors related to radon to inform cancer control activities and practices. Indoor Air 28(4):604–610. 10.1111/ina.12468 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.U.S. Environmental Protection Agency. The National Radon Action Plan - A Strategy for Saving Lives. Washington DC: (2015) http://www.epa.gov/radon/national-radon-action-plan-strategysaving-lives Accessed 21 May 2018 [Google Scholar]
- 21.Centers for Disease Control and Prevention. Cancer Prevention and Control Programs for State, Territorial, and Tribal Organizations (CDC-RFA-DP17–1701, CFDA 93.898) (2017) https://www.grants.gov/web/grants/search-grants.html Accessed 15 June 2017
- 22.Environmental Law Institute. Database of Indoor Air Quality Laws - Database Excerpt: Radon Laws. Environmental Law Institute, Washington, DC: (2017) https://www.eli.org/buildings/database-state-indoor-air-quality-laws Accessed 21 June 2018 [Google Scholar]


