Capsule Summary:
A 2-hour exposure to 500 μg/m3 wood smoke particles caused neutrophilic airway inflammation in human volunteers, with GSTM1 null genotype being associated with greater inflammatory response to this pollutant.
Keywords: particulate matter, neutrophils, pollutants, wood smoke
To the Editor:
Particulate matter (PM) emissions from burning biomass are a major source of indoor and outdoor air pollution. Wildland fires also accounted for 20% of fine PM emissions in the U.S. in 2012 [1]. Because climate change is associated with increased severity and frequency of wildland fires throughout the world, this problem is only expected to worsen with time [2].
The often abrupt and significantly increased PM generated by biomass combustion is associated with increased risk for asthma, chronic obstructive pulmonary disease (COPD), pneumonia, and cardiovascular disease. Wildfire smoke exposure causes increased emergency room visits, hospitalizations, and premature deaths [3]. Firefighters deployed to wildland fires are frequently exposed to PM levels well in excess of the National Ambient Air Quality Standards for PM2.5 or PM10. Field studies of wildland firefighters reported worsened lung function and increased non-specific bronchial reactivity during a fire season compared to preseason values[4]. Neutrophils and inflammatory cytokines were increased in the airways and peripheral blood of firefighters following work shifts[5].
Intracellular antioxidant enzymes such as glutathione-S-transferase Mu-1 (GSTM1) regulate cellular and mucosal oxidative stress. We have previously shown that individuals with the GSTM1 null genotype (resulting in the absence of GSTM1 protein) have increased susceptibility for the development of neutrophilic bronchitis following exposure to diverse air pollutants including ozone, endotoxin, and particulate matter [6–8]. The objective of this study was to identify if the GSTM1 genotype conferred increased risk of neutrophilic airway inflammation following wood smoke particle (WSP) exposure.
We recruited non-smoking volunteers ages 18-45 years with no history of asthma, negative methacholine test, no acute respiratory illness in the prior 4 weeks, and no current allergic rhinitis symptoms. GSTM1 genotype was determined using methods previously described [6–8]. Written consent was obtained from all participants, and the study was approved by the University of North Carolina Institutional Review Board. The study is listed on ClinicalTrials.gov (NCT02767973).
Baseline induced sputum samples were obtained at the initial study visit. At the next visit, volunteers entered the exposure chamber, which was injected with wood smoke generated by heating red oak wood on an electric heating element. Using previously published methods, participants were exposed to 500 μg/m3 WSP over a 2-hour period with alternating 15-minute periods of rest and exercise on a cycle ergometer at a level sufficient to produce a minute ventilation of 20 L/min/m2 body surface area [9] (additional detail provided in the Online Data Supplement). Induced sputum was obtained at 6 and 24 hours after WSP exposure. The primary endpoint was sputum percent neutrophils (%PMNs) at 24 hours post-WSP compared to baseline samples. Consistent with previous studies at our center, responders were defined as those who experienced a ≥10% increase in sputum %PMN [6,8]. We compared baseline to post-WSP %PMN means using two sample comparison tests, either parametric or non-parametric, depending on whether the normality assumption was met. Data were log transformed as needed to achieve normality. We used Fisher’s Exact Test to determine whether there is an association between GSTM1 genotype and WSP responder status. Linear regression models were generated to further explore the relationship between GSTM1 genotype and WSP-induced change in sputum %PMNs as a continuous variable (additional detail provided in the Online Data Supplement).
Thirty-five non-smoking volunteers were enrolled in the study, with four participants discontinuing prior to WSP exposure. Four participants were unable to provide sputum samples at 24 hours post-WSP exposure. Twenty-seven paired sputum samples (baseline and 24 hours post-WSP) were available for analysis. Demographic information for the study population is found in Table E1. Sixteen participants were GSTM1 sufficient (12 with two copies of the gene, and 4 with only one copy), 10 were GSTM1 null, and one participant’s genotype could not be determined.
Analysis of samples showed a significant increase in sputum neutrophil content between the baseline measurement and 24 hours post-WSP, with a mean increase of 10% ± 5.5 (SEM) in sputum %PMNs (p=0.0001) (Figure 1A). Eighteen (67%) participants met our prespecified criteria for WSP responders. Among responders, there was a mean increase of 26% ±2.9 in sputum %PMNs at 24 hours post-WSP (p<0.0001)(Figure 1B). Among non-responders, we found a significant decrease in %PMNs 24 hours post-WSP exposure (Figure 1C-D).
Figure 1. Wood smoke particle exposure induces neutrophilic airway inflammation in healthy volunteers.
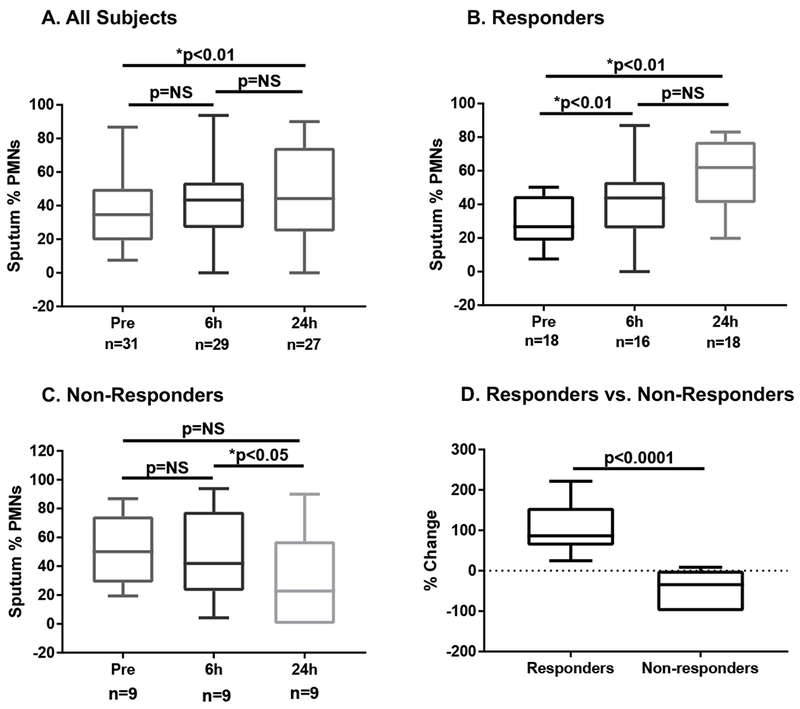
Healthy volunteers underwent exposure to WSP and provided induced sputum samples before exposure and 6 and 24 hours after exposure. A) All participants; B) Responders, defined by a ≥ 10 percent increase in sputum %PMNs; C) Non-Responders; D) Responders experienced a significantly greater change in sputum %PMNs from baseline at 24 hours post-WSP exposure compared to non-responders and all participants. Wilcoxon-signed rank tests were used to compare post-WSP sputum to baseline sputum (data represented as mean ± SEM; p values derived from log transformed data).
We next investigated the impact of GSTM1 status on the airway response to WSP exposure. Both GSTM1 null and sufficient volunteers had a significant increase in %PMNS at 24 hours compared to baseline measurements (Figure 2A-B). However, GSTM1 nulls experienced a greater percent change from baseline in sputum %PMNs following WSP exposure than GSTM1 sufficient participants (89.3% ± 31.9 vs 33.7% ±18.9, p=0.046) (Figure 2C). The impact of GSTM1 null status was more pronounced in the responder group (160% ±22.8 vs 75.7% ± 11, p=0.004) (Figure 2D). We did not find a significant relationship between GSTM1 null genotype and being classified as a WSP responder by our prespecified criteria (RR 0.85, 95% CI 0.34, 2.18; p>0.99). Of GSTM1 sufficient participants, there was no difference in PMN response to WSP based on gene copy number. Linear regression analyses demonstrated that GSTM1 null individuals experienced, on average, a 28% greater WSP-induced change in sputum %PMNs compared to GSTM1 sufficient individuals (p<0.01) (Table E2).
Figure 2. GSTM1 null participants experienced greater WSP-induced airway neutrophil influx.

GSTM1 null (A) and sufficient (B) participants experienced a significant increase in sputum neutrophil content at 24 hours post-WSP exposure. GSTM1 null participants showed a more robust neutrophilic response than sufficient individuals (C), and this relationship was greatest in responders (D). Wilcoxon-signed rank tests were used to compare 24h post-WSP sputum to baseline sputum (data represented as mean ± SEM; p values derived from log transformed data).
We have shown that 2-hour exposure to 500 μg/m3 WSP induces significant airway neutrophilia in healthy volunteers and to a larger degree in GSTM1 null volunteers, supporting the hypothesis that this genotype is a risk factor for airway inflammation in response to WSP exposure. This same challenge protocol will be used to explore the effect of GSTM1 and additional susceptibility factors such as BMI, sex, smoking or pre-existing disease (such as asthma) on airway and systemic responses to wood smoke inhalation. We are also using WSP, O3 and endotoxin challenge protocols to assess candidate anti-inflammatory treatments and personal monitoring sensor arrays designed to prevent or mitigate WSP-induced airway inflammation.
In summary, PM-related adverse health effects attributable to burning biomass represent a crucial public health concern. Individuals with GSTM1 null genotype displayed an exaggerated inflammatory response to inhaled wood smoke, demonstrating that non-disease specific genes like GSTM1 should be considered important risk factors for wood smoke-induced disease.
Supplementary Material
Acknowledgments
Sources of Support:
Research reported in this publication was entirely supported by the National Institute of Environmental Health Sciences of the National Institutes of Health under award number R01ES025124 and Assistance Agreement No. 83578501-0 awarded by the U.S. Environmental Protection Agency to the University of North Carolina. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the Environmental Protection Agency. EPA does not endorse any products or commercial services mentioned in this publication. EMA is supported by 5T32ES007018-42. MLH and AJB are supported by R01HL135235.
Abbreviations:
- PM
particulate matter
- GSTM1
Glutathione-S-transferase mu-1
- WSP
wood smoke particle
- PMN
neutrophil
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declarations of Interest: None
References:
- 1.US EPA Air Emissions Inventories. National Emissions Inventory (NEI) Data 2011. [Available from: https://www.epa.gov/air-emissions-inventories/2011-national-emissions-inventory-nei-data.
- 2.Hurteau MD, Westerling AL, Wiedinmyer C, Bryant BP. Projected effects of climate and development on California wildfire emissions through 2100. Environ Sci Technol 2014;48(4):2298–304. [DOI] [PubMed] [Google Scholar]
- 3.Reid CE, Brauer M, Johnston FH, Jerrett M, Balmes JR, Elliott CT. Critical Review of Health Impacts of Wildfire Smoke Exposure. Environ Health Perspect 2016;124(9): 1334–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Liu D, Tager IB, Balmes JR, Harrison RJ. The effect of smoke inhalation on lung function and airway responsiveness in wildland fire fighters. Am Rev Respir Dis 1992; 146(6): 1469–73. [DOI] [PubMed] [Google Scholar]
- 5.Swiston JR, Davidson W, Attridge S, Li GT, Brauer M, van Eeden SF. Wood smoke exposure induces a pulmonary and systemic inflammatory response in firefighters. Eur Respir J 2008;32(1):129–38. [DOI] [PubMed] [Google Scholar]
- 6.Alexis NE, Zhou H, Lay JC, Harris B, Hernandez ML, Lu TS, et al. The glutathione-S-transferase Mu 1 null genotype modulates ozone-induced airway inflammation in human subjects. J Allergy Clin Immunol. 2009;124(6):1222–8 e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chen B-Y, Chen C-H, Chuang Y-C, Kim H, Honda Y, Chiang H-C, et al. Schoolchildren’s antioxidation genotypes are susceptible factors for reduced lung function and airway inflammation caused by air pollution. Environ Res 2016;149:145–50. [DOI] [PubMed] [Google Scholar]
- 8.Dillon MA, Harris B, Hernandez ML, Zou B, Reed W, Bromberg PA, et al. Enhancement of systemic and sputum granulocyte response to inhaled endotoxin in people with the GSTM1 null genotype. Occup Environ Med 2011;68(10):783–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ghio AJ, Soukup JM, Case M, Dailey LA, Richards J, Berntsen J, et al. Exposure to wood smoke particles produces inflammation in healthy volunteers. Occup Environ Med 2012;69(3):170–5. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


