Abstract
Objectives
For complicated common bile duct stones (CBDS) that cannot be extracted by endoscopic retrograde cholangiopancreatography (ERCP), management can be safely by open or laparoscopic CBD exploration (CBDE). The study aimed to assess these surgical procedures after endoscopic failure.
Methods
We analyzed 85 patients underwent surgical management of difficult CBDS after ERCP failure, in the period from 2013 to 2018.
Results
Sixty-seven (78.8%) and 18(21.2%) of our patients underwent single and multiple ERCP sessions respectively. An impacted large stone was the most frequent cause of ERCP failure (60%). Laparoscopic CBDE(LCBDE), open CBDE(OCBDE) and the converted cases were 24.7% (n = 21), 70.6% (n = 60), and 4.7% (n = 4) respectively. Stone clearance rate post LCBDE and OCBDE reached 95.2% and 95% respectively, Eleven (12.9%) of our patients had postoperative complications without mortality. By comparing LCBDE and OCBDE; there was a significant association between the former and longer operative time. On comparing, T-tube and 1ry CBD closure in both OCBDE and LCBDE, there was significantly longer operative time, and post-operative hospital stays in the former. Furthermore, in OCBDE group, choledocoscopy had an independent direction to 1ry CBD repair and significant association with higher stone clearance rate, shorter operative time, and post-operative hospital stay.
Conclusion
Large difficult CBDS can be managed either by open surgery or laparoscopically with acceptable comparable outcomes with no need for multiple ERCP sessions due to their related morbidities; furthermore, Open choledocoscopy has a good impact on stone clearance rate with direction towards doing primary repair that is better than T-tube regarding operative time and post-operative hospital stay.
Keywords: Laparoscopic CBDE, Open CBDE, CBD stones
Highlights
-
•
Large difficult CBD stones can be managed either by open surgery or laparoscopically with acceptable comparable outcomes.
-
•
No need for multiple ERCP sessions due to their related morbidities.
-
•
Open choledocoscopy has a good impact on stone clearance rate with direction towards doing primary repair.
-
•
Primary repair is better than T-tube regarding operative time and post-operative hospital stay.
List of abbreviations
- ASA
American society of anesthesia
- BDS
Bile duct stones
- CBD
Common bile duct
- CBDE
Common bile duct exploration
- CBDS
Common bile duct stone
- CHD
Common hepatic duct
- CRP
C-reactive protein
- EPBD
endoscopic papillary ballon dilatation
- ES
Endoscopic sphincterotomy
- ERCP
Endoscopic retrograde cholangio-pancreatography
- HJ
Hepaticojejunostomy
- HPB
Hepatopancreatobiliary
- IOC
Intra-operative cholangiogram
- IRB
Institutional review board
- LC
Laparoscopic cholecystectomy
- LCBDE
Laparoscopic common bile duct exploration
- LCD
Laparoscopic choledochotomy
- LFT
Liver function test
- LTCE
Laparoscopic trans-cystic exploration
- MRCP
Magnetic resonance cholangiopancreatography
- NLI
National Liver Institute
- OC
Open Cholecystectomy
- OCD
Open choledochotomy
- OCBDE
Open common bile duct exploration
- PDS
polydioxanone
- POD
Post-operative day
- TDS
Transduodenal sphinectroplasty
- US
Ultrasonography
1. Introduction
The incidence of common bile duct stones (CBDS) in patients with symptomatic cholelithiasis varies widely in the literature between 5% and 33% according to age [[1], [2], [3], [4], [5]]. CBDS are either primary (originating within the CBD) or secondary (originating in the gallbladder) and pass into the CBD [6,7]. Trans-abdominal ultrasound (US) and magnetic resonance cholangiopancreatography (MRCP) are the most common non-invasive pre-operative imaging modalities for detection of CBDS [8].
However, endoscopic retrograde cholangiopancreatography (ERCP) is the most common invasive tool for their detection. Treatment is advisable to prevent further complications, such as obstructive jaundice, acute cholangitis, and pancreatitis. [[8], [9], [10], [11]] Different modalities for successful treatment of these stones have been reported after advances in minimally invasive techniques as endoscopy, and laparoscopy, however, the optimal treatment is controversial [8,12,13]. They include one- or two-stage procedures; the two-stage procedures involve pre- or post- laparoscopic cholecystectomy- ERCP (LC-ERCP), while the single-stage procedures refer to Open or Laparoscopic CBD exploration (OCBDE or LCBDE) [2,10,[14], [15], [16]]. Pre- or postoperative ERCP is a popular treatment option commonly performed by endoscopists, nevertheless, it is associated with post-procedure complications [8,12,13]. Large, multiple and/or impacted stones in the CBD may be difficult or impossible to retrieve by ERCP [17,18]. Those patients can be managed with LCBDE or OCBDE, where these procedures have a high success rate in salvaging them [9,10,[18], [19], [20]]. To the best of our knowledge, there is little literature on surgical management of difficult CBD stones after ERCP failure, so, our study aimed to analyze this issue.
2. Patients and methods
One hundred patients underwent surgical management of large difficult CBDS after ERCP failure, in the period from the beginning of 2013 to the beginning of 2018 in the department of hepato-pancreato-biliary (HPB) surgery (tertiary care center), National Liver Institute (NLI), University of Menoufia, Menoufia, Egypt, our study included 85 patients after exclusion of cases with data loss, those who did not complete the follow-up and who refused researches. We did this cohort study which is a single-institution retrospective analysis of a prospectively collected database that assessed these surgical procedures of CBDE after endoscopic failure in the period from the beginning of 2013 to mid 2018, where patients were observed from POD1 until the end of June 2018 with a median follow up period of 39 ms, range (6–66 ms) [21]. The study was approved by Our IRB.
The data were collected from our records in our HPB surgery department and the endoscopic unit of hepatology department where written informed consents were obtained from patients regarding procedures, surgeries, and researches [21]. Our work has been reported in line with the STROCSS criteria [22], with researchregistry4588.
The recorded data included patient demographics, pre-ERCP main presentation, No of ERCP sessions, reasons of ERCP failure, post-ERCP complications, stone site ((ampullary, distal CBD, mid CBD, or common hepatic duct(CHD)), size(Small<1.5 cm, large1.5–2 cm, or very large< 2 cm), and NO(single or multiple), CBD diameter per mm, the pre-operative American society of anesthesia(ASA) score, operative details including: Type of operation: LCBDE(laparoscopic choledochotomy(LCD)), or OCBDE(supraduodenal open choledochotomy(OCD), or open transduodenal sphinectroplasty(TDS)), using cholecodoscope during surgery or not, causes of conversion from laparoscopic to open surgery, management of CBD after clearance from stones(primary repair, T-tube insertion, or hepaticojejunostomy(HJ)), operative bleeding, operative time per minutes, postoperative hospital stay per days, patient outcome and lastly follow-up data (Fig. 1, Fig. 2, Fig. 3, Fig. 4, Fig. 5, Fig. 6).
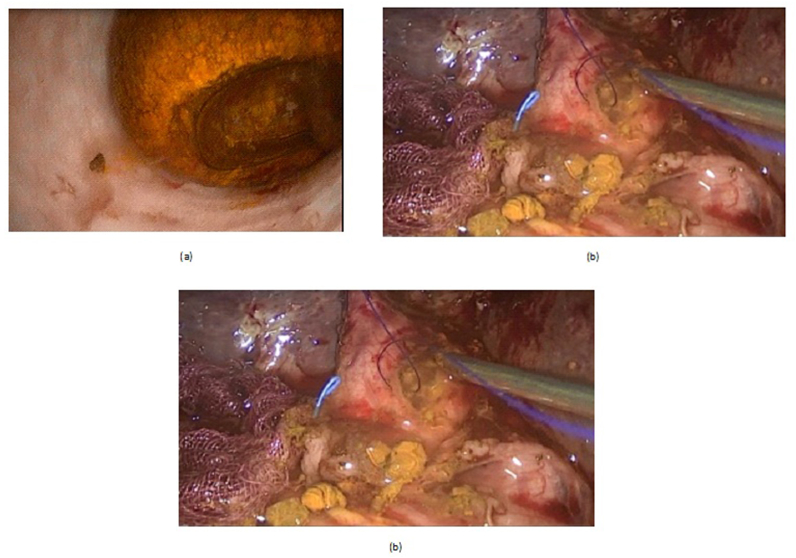
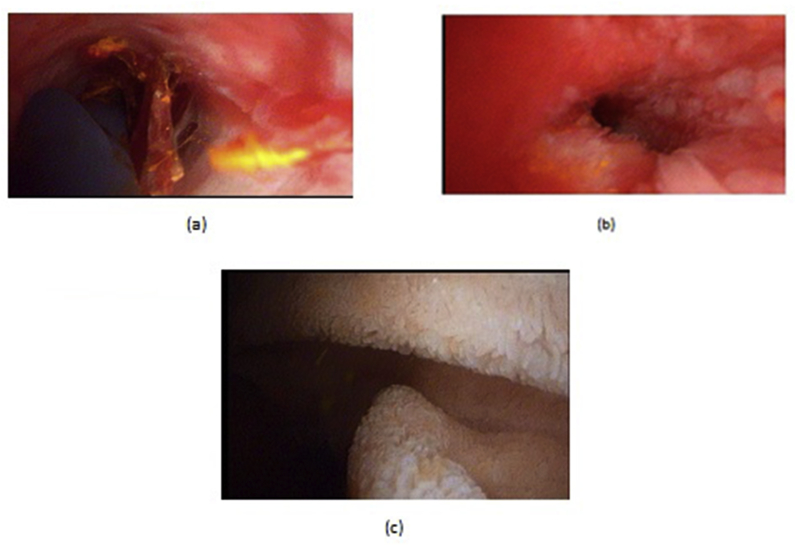
Fig. 1.
A: Laparoscopic cholecodoscopic view of CBD stone, B: laparoscopic cholecodoscopic stone extraction, C: laparoscopic primary closure of CBD.
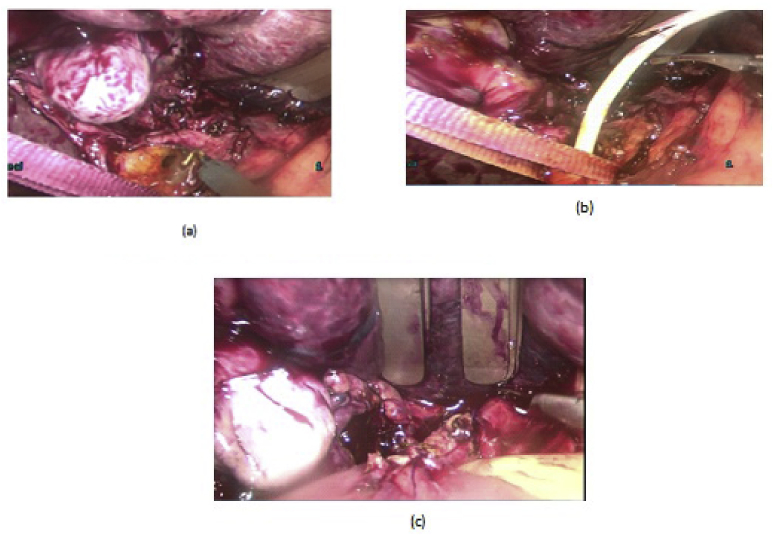
Fig. 2.
(a,b) laparoscopic stone and stent extraction, ©: laparoscopic HJ.
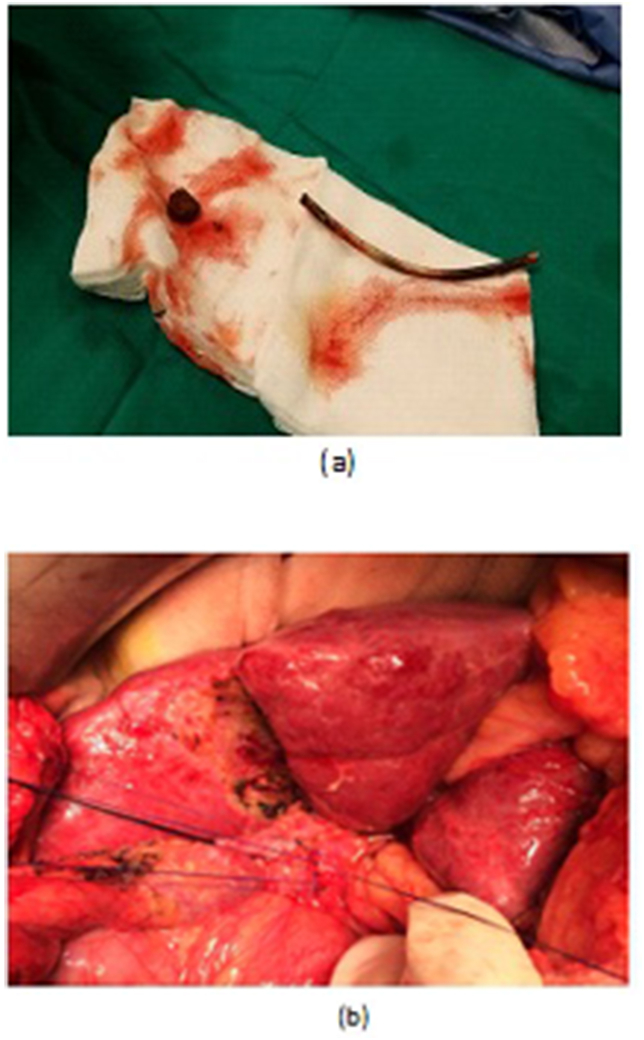
Fig. 3.
a: OCBD extraction of stent and stone. b: Open primary closure of CBD.
Fig. 4.
a, b, OCBD extraction of stent and stones. c,d: Open T-tube insertion, and T-tube cholangiogram.
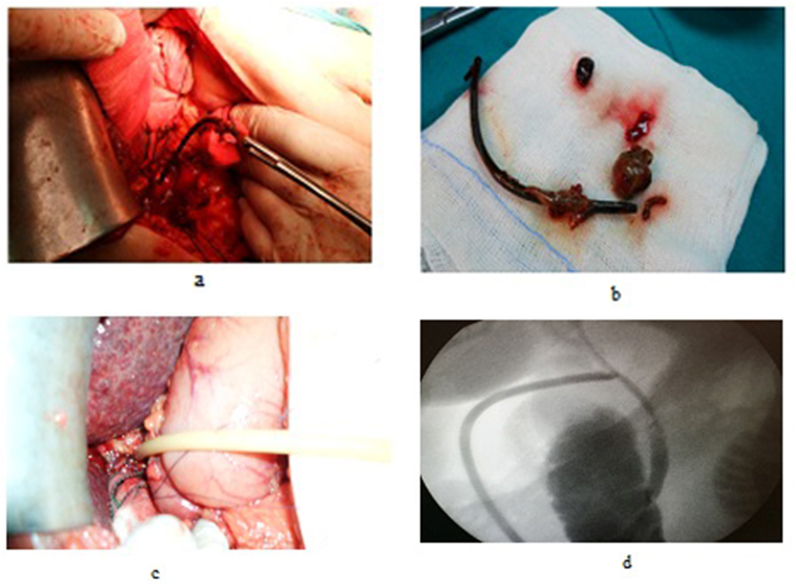
Fig. 5.
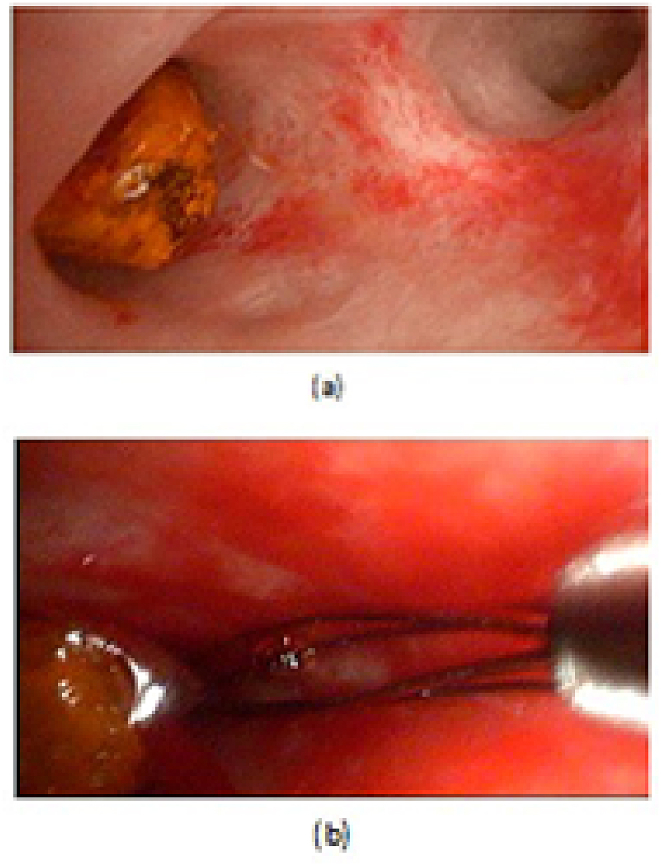
a: A cholecodoscopic view of stone in RT hepatic duct. b: Open cholecodoscopic basket extraction.
Fig. 6.
a: An open cholecodocoscopic view of stone and stent in distal CBD, b,c: cholecodoscopic extraction of stent and stone with duodenal mucosa appearance.
Pre-ERCP presentations (i.e. acute cholecystitis, biliary colic, jaundice, cholangitis, pancreatitis …) were confirmed by careful history taking, clinical examination, laboratory investigations especially liver function tests (LFTs), serum amylase, lipase and C-reactive protein (CRP), and by imaging as abdominal US ± MRCP.
The ERCP procedures were performed by the endoscopic authors of the manuscript with a side-viewing duodenoscope (JF-260 V or TJF-260 V; Olympus Medical Systems, Tokyo, Japan), under general anesthesia. Selective cannulation of the bile duct was achieved using a wire-guided sphincterotome (Clever Cut; Olympus Medical Systems). After successful cannulation, a contrast dye was injected to confirm the presence of CBDS that were extracted with the help of balloon or Dormia basket after performing endoscopic sphincterotomy(ES)(Mechanical lithotripsy was used for large stones (mechanical lithotripter BML 3Q and BML 4Q, Olympus, Tokyo, Japan). A check cholangiogram was performed to confirm the complete clearance of the bile duct. [15,[23], [24], [25]].
The patients were referred to our surgical department after single or multiple sessions of ERCP due to failure to cannulate CBD or to extract stones from CBD after successful cannulation due to their impaction and/or their large sizes despite using mechanical lithotripsy. All cases with successful cannulation but the failure of stone extraction were managed with single or multiple CBD stents (Cotton-Leung or Tannenbaum, Wilson-Cook, Winston-Salem, USA) with the 10-Fr diameter and 7–10 cm length put beside stones for drainage and possible stone fragmentation. The complications related to ERCP were recorded (I.e. bleeding, cholangitis, perforation, pancreatitis …).
2.1. The surgical techniques: (The operations were done by the surgical authors of the manuscript)
LCD: Under general anesthesia; we used the standard four-port technique of LC. Routine trans-cystic intra-operative cholangiography (IOC) was performed in all cases for identification of stones number, site and size. The gallbladder was left in situ for retraction until the operation was completed. When we reached CBD, a longitudinal supraduodenal choledochotomy(1.5–2 cm) was done using scissors or cautery. The CBD stones were entirely retrieved in all patients using cholecodoscopic extraction techniques (4.5-Fr flexible choledochoscope; Karl Storz, Tuttlingen, Germany) by irrigation, balloon or basket with mechanical lithotripsy when needed. The epigastric port was used to accommodate the operating choledochoscope [15,18,[26], [27], [28], [29]]. After all stones were retrieved and clearance of the bile duct was confirmed with choledochoscopy, the choledochotomy was closed with interrupted 4.0 Vicryl sutures in patients with primary closure of CBD and then IOC was done through the cystic duct to confirm absence of stones and leak (Fig. 1). On the other hand, for patients with T-tube drainage, the T-tube was placed in the choledochotomy and secured with sutures, Patients had a cholangiogram on the 6th postoperative day. If the finding was normal, the T-tube was clamped and patients were discharged home with the T-tube in situ then it was removed from 4 to 6 weeks later after normal tube cholangiogram in the outpatient clinic. [23,27,30]. Lastly, laparoscopic HJ was done by 4.0 polydioxanone (PDS) sutures (posterior and anterior interrupted sutures) and a tube drain was placed near the anastomosis and removed days after the operation (Fig. 2) [1,14,31,32].
OCD: It started by open cholecystectomy (OC) and IOC through the cystic duct; then identification of CBD and the junction between the cystic duct and the CBD were done. A complete Kocher's maneuver was performed in order to feel the retro- and intra-pancreatic portion of the CBD for easy extraction of stones and to feel the papilla. Then, two stay sutures were placed transversally at the right and left portions of the duct; then the anterior wall of the supraduodenal part of CBD was opened. The incision was performed with a sharp scalpel, then an exploration of the CBD first proximally and then distally with the Randall forceps occurred for extraction of visible stones. The proximal and distal CBD was then irrigated with saline using a soft catheter. In choledochoscopic cases, the CBD stones were entirely retrieved using choledochoscopic extraction techniques (4.5-Fr flexible choledochoscope; Karl Storz, Tuttlingen, Germany) (Fig. 5, Fig. 6). After all stones were extracted and clearance of the bile duct was confirmed; the management was as mentioned in LCD (Fig. 3, Fig. 4). Lastly, in HJ cases, the biliary-enteric anastomosis was done by 4.0 PDS sutures (posterior continuous and anterior interrupted sutures) [20].
TDS (for impacted stones in the ampulla of Vater): A Kocher maneuver was performed, after which a longitudinal anterior duodenotomy was made at the level of the ampulla, the ampulla and distal CBD were divided for a distance of 1.5–2 cm, directed anteromedially. The sphincter was divided sequentially between small clamps, with sequential suture approximation of the duodenal and bile duct mucosa using fine interrupted absorbable suture 4.0 vicryle. The duodenum was then closed transversely [8,33].
The outcome and follow-up of patients: For detection of postoperative complications (I.e. bile leak, missed, recurrent stones, and/or CBD stricture); patients were followed-up daily during hospital stay until discharge, then every 6 months in the 1st year then yearly until the end of follow-up period by clinical assessment, LFT, US, and others if needed (i.e. MRCP). Comparison between groups and subgroups of patients was done using univariate and multivariate analyses as follow: LCBDE vs. OCBDE, T-tube vs. 1ry repair in LCBDE group, T-tube vs. 1ry repair in OCBDE group, and choledochoscope vs. non-choledochoscope in OCBDE group.
Statistical Techniques: All data were processed with SPSS software (Statistical Product and Service Solutions, version 21, SSPS Inc, Chicago, IL, USA). Categorical variables were expressed in frequency and percentage and analyzed with the chi-square or Fisher exact tests. While continuous data were expressed as the mean and SD and were compared with the T or Mann whitteny tests. Univariate analysis and then multivariate analysis (by Binary logistic regression method) were done to compare different groups and subgroups of patients regarding pre-, intra-, and postoperative data. A P value of <0.05 was considered significant.
3. Results
3.1. Characteristics of patients regarding demographics and ERCP
They were classified as 27(31.8%) males, and 58 (68.2%) females; their mean age was 45.1 ± 11.5 years. Acute cholecystitis, biliary colic, cholangitis, jaundice, and pancreatitis were the main presentation pre-ERCP in 5(5.9%), 35 (41.2%), 5(5.9%), 36(42.4%), and 4(4.7%) of patients respectively. Sixty-seven (78.8%) of patients underwent single ERCP session, while 18 (21.2%) of them underwent multiple sessions. Very large, multiple large, impacted large stones and failed cannulation were the causes of ERCP failure in 13(15.3%), 17 (20%), 51(60%), and 4 (4.7%) of patients respectively. ERCP was complicated with bleeding, cholangitis, impacted dormia, and pancreatitis in 2.4%, 2.4%, 1.2%, and 3.5% of patients respectively. Table 1. On univariate analysis, there was a significant correlation between the number of ERCP sessions and post ERCP complications (27.8% complications with multiple sessions vs.4.5% with single ones; P = 0.009). Table 1.
Table 1.
Characteristics of patients regarding demographics and ERCP.
| Character | (Mean ± SD) or |
|
|---|---|---|
| No | (%) | |
| Gender | ||
| Males | 27 | (68.2%) |
| Females | 58 | (31.8%) |
| Age(years) (Mean ± SD) | 45.1 ± 11.5 | |
| Pre ERCP main presentation | ||
| Acute cholecystitis | 5 | (5.9%) |
| Biliary colic | 35 | (41.2%) |
| Cholangitis | 5 | (5.9%) |
| Jaundice | 36 | (42.4%) |
| Pancreatitis | 4 | (4.7%) |
| No of ERCP sessions | ||
| Single | 67 | (78.8%) |
| Multiple | 18 | (21.2%) |
| Cause of ERCP failure | ||
| Very large stones(<2 cm) | 13 | (15.3%) |
| Multiple large stones | 17 | (20%) |
| Impacted large stones | 51 | (60%) |
| Failed cannulation | 4 | (4.7%) |
| Post ERCP complications | 8 | (9.4%) |
| Bleeding | 2 | (2.4%) |
| Cholangitis | 2 | (2.4%) |
| Impacted dormia | 1 | (1.2%) |
| Pancreatitis | 3 | (3.5%) |
ERCP: Endoscopic retrograde cholangio-pancreatography.
Comparison between LCBDE, and OCBDE, and characteristics of the converted cases: The eighty-five patients were classified as follow: 21 patients completed LCBDE, 60 patients started and completed OCBDE, and 4 patients converted from LCBDE to OCBDE.
In LCBDE group (21 patients): They were classified as 6(28.6%) males, and 15 (71.4%) females; their mean age was 34.05 ± 6.1 years. Three (14.3%), 15(71.4%), and 3(14.3%) of patients had their stones in CHD, mid-CBD, and distal CBD respectively. The mean CBD diameter was 14 ± 4.7 mm, furthermore, the stones were classified into large (1.5–2 cm) and very large (>2 cm) in 18(85.7%) and 3(14.3%) of patients respectively. Nineteen (90.5%), and 2(9.5%) of patients had single, and multiple stones respectively. Stones were 1ry in 1 patient and 2ry in 20 ones. The preoperative ASA score was graded as I, II, and III in 14 (66.7%), 6 (28.6%), and 1(4.8%) of patients respectively. IOC and choledochoscopy were done for all patients. After stone extraction; Primary repair of CBD, T- tube insertion, and HJ were done in 9(42.9%), 11(52.4%), and 1 (4.8%) of them respectively. Operative bleeding affected 1 of patients. The mean operative times and hospital stays were 231.4 ± 49.3 min, and 5.5 ± 3 days respectively. Lastly, the success rate reached 95.2% Table 2. Regarding postoperative complications in this group, they affected 3(14.3%) of patients, where, chest infection, wound infection, missed stones, and bile leak complicated 1(4.8%), 1(4.8%), 1(4.8%), and 2(9.5%) of them respectively; patients with chest and/or wound infection were managed conservatively(grade II according to Clavien grading), patient with missed stone was managed successfully percutaneously with choledochoscopic CBDE through the biliary drainage sinus tract under fluoroscopic control(grade III), however, the 2 cases with biliary leak were managed successfully conservatively as the leak was minor(grade II). Lastly, there was no stricture, recurrent stones or mortality during the long-term follow-up. Table 2.
Table 2.
Comparison between LCBDE, and OCBDE, and characteristics of the 4 converted cases.
| Character | LCBDE (No = 21) (Mean ± SD) Or No (%) | OCBDE (No = 60) (Mean ± SD) or No (%) | P value Univariate analysis | P value Multivariate analysis | The converted cases (No = 4) (Mean ± SD) Or No (%) |
|---|---|---|---|---|---|
| Gender | >0.05 | ||||
| Males | 6(28.6%) | 20 (33.3%) | 1(25%) | ||
| Females | 15(71.4%) | 40 (66.7%) | 3(75%) | ||
| Age(years) | 34.05 ± 6.1 | 49.6 ± 9.9 | 0.000 | 0.05 | 36.3 ± 13.5 |
| Site of stones | 0.001 | >0.05 | |||
| CHD | 3(14.3%) | 0 | 0 | ||
| Mid-CBD | 15(71.4%) | 29(48.3%) | 2(50%) | ||
| Distal CBD | 3(14.3%) | 26(43.3%) | 2(50%) | ||
| Ampulla | 0 | 5(8.3%) | 0 | ||
| CBD diameter(mm) | 14 ± 4.7 | 15.4 ± 5.02 | >0.05 | 14.3 ± 5.7 | |
| Stone size | 0.1 | >0.05 | |||
| Large(1.5–2 cm) | 18(85.7%) | 43(71.7%) | 3(75%) | ||
| Very large(<2 cm) | 3(14.3%) | 17(28.3%) | 1(25%) | ||
| NO of stones | >0.05 | ||||
| Single | 19(90.5%) | 46(76.7%) | 1(25%) | ||
| Multiple | 2(9.5%) | 14(23.3%) | 3(75%) | ||
| Nature of stones | >0.05 | ||||
| Primary | 1(4.8%) | 1(1.7%) | 1(25%) | ||
| Secondary | 20(95.2%) | 59(98.3%) | 3(75%) | ||
| ASA score | >0.05 | ||||
| I | 14 (66.7%) | 40 (66.7%) | 3(75%) | ||
| II | 6 (28.6%) | 16 (26.7%) | 1(25%) | ||
| III | 1(4.8%) | 4(6.7%) | 0 | ||
| Type of operation | |||||
| LCD | 0 | 0.000 | 4(100%) | ||
| OCD | 0 | 55(91.7%) | 0.000 | 4(100%) | |
| TDS | 0 | 5(8.3%) | 0.1 | 0 | |
| IOC | 21(100%) | 60(100%) | 4(100%) | ||
| choledochoscope | 21(100%) | 38(63.3%) | 0.001 | >0.05 | 4(100%) |
| Primary repair | 9(42.9%) | 30(50%) | >0.05 | 0 | |
| T- tube | 11(52.4%) | 20(33.3%) | 0.1 | >0.05 | 3(75%) |
| HJ | 1(4.8%) | 5(8.3%) | >0.05 | 1(25%) | |
| Operative bleeding | 1(4.8%) | 2(3.3%) | >0.05 | 1(25%) | |
| Operative time(min) | 231.4 ± 49.3 | 160.7 ± 43.4 | 0.000 | 0.02 | 345 ± 13 |
| Post-operative hospital stay(days) | 5.5 ± 3 | 6.1 ± 2.1 | >0.05 | 8 ± 1.4 | |
| Postoperative | |||||
| complications | 3(14.3%) | 7(11.7%) | >0.05 | >0.05 | 1(25%) |
| Chest infection | 1(4.8%) | 5(8.3%) | >0.05 | 1(25%) | |
| Wound infection | 1(4.8%) | 2(3.3%) | >0.05 | 0 | |
| Missed stones | 1(4.8%) | 3(5%) | >0.05 | 0 | |
| Bile leak | 2(9.5%) | 0 | 0.06 | 0 | |
| Stricture | 0 | 0 | |||
| Recurrent stones | 0 | 0 | |||
| Stone clearance rate | 20 (95.2%) | 57(95%) | >0.05 | 4(100%) | |
| Mortality | 0 | 0 | 0 | ||
LCBDE: Laparoscopic common bile duct exploration, OCBDE: Open common bile duct exploration, CHD: Common hepatic duct, CBD: Common bile duct, ERCP: Endoscopic retrograde cholangiopancreatography, ASA: American society of anaesthesia, LCD: Laparoscopic choledochotomy, OCD: Open choledochotomy, TDS: Transduodenal sphinectroplasty, IOC: Intra-operative cholangiogram, HJ: Hepaticojejunostomy.
In OCBDE group (60 patients): They were classified as 20(33.3%) males, and 40 (66.7%) females; their mean age was 49.6 ± 9.9 years. Twenty-nine (48.3%), 26(43.3%), and 5 (8.3%) of patients had their stones in mid-CBD, distal CBD, and ampulla of Vater respectively. The mean CBD diameter was 15.4 ± 5.02 mm, furthermore, the stones were classified into large (1.5–2 cm) and very large (>2 cm) in 43(71.7%) and 17(28.3%) of patients respectively. Forty-six (76.7%), and 14(23.3%) of patients had single, and multiple stones respectively. The mean time of referral to surgery after ERCP failure was 63.3 ± 86.6 days. Stones were 1ry in 1 patient and 2ry in 59 ones. The preoperative ASA score was graded as I, II, and III in 40 (66.7%), 16 (26.7%), and 4(6.7%) of patients respectively. OCD was performed in 55 patients, while TDS was the operation in 5 patients. IOC was done for all patients, while choledochoscope was done in 38(63.3%) of them. After stone extraction; Primary repair of CBD, T- tube insertion, and HJ were done in 30 (50%), 20(33.3%), and 5 (8.3%) of them respectively. Operative bleeding affected 2 of patients. The mean operative times and hospital stays were 160.7 ± 43.4 min, and 6.1 ± 2.1 days respectively. Lastly, success rate reached 95%. Table 2. The incidence of postoperative complications in this group was 7(11.7%) patients, where, chest infection, wound infection, and missed stones affected 5(8.3%), 2(3.3%), and 3(5%) of them respectively; patients with chest and/or wound infection (grade II Clavien) were managed conservatively, the 3 patients with missed stones (grade III) were managed successfully percutaneously with choledochoscopic CBDE through the biliary drainage sinus tract under fluoroscopic control. Lastly, there was no bile leak, stricture, recurrent stones or mortality during the long-term follow-up. Table 2.
When comparing both groups using univariate analysis; patient age was significantly lower, referral time was shorter, choledochoscope use was more frequent, and operative time was significantly longer in the laparoscopic group. On the other hand, on multivariate analysis, there was an independent correlation between longer operative time and LCBDE. Table 2.
Characteristics of the 4 patients converted from LCBDE to OCBDE: They were classified as 1(25%) males, and 3 (75%) females; their mean age was 36.3 ± 13.5 years. Two (50%), and 2(50%) of patients had their stones in mid and distal CBD respectively. The mean CBD diameter was 14.3 ± 5.7 mm (range; 10–22 mm), furthermore, the stones were classified into large (1.5–2 cm) and very large (>2 cm) in 3(75%) and 1(25%) of patients respectively. One(25%), and 3(75%) of patients had single, and multiple stones respectively. The mean time of referral to surgery after ERCP failure was 176.3 ± 18. 4 days (range; 15–300 days). The stones were classified as primary in 1 patient and secondary in 3 patients. The preoperative ASA score was graded as I, and II in 3(75%), 1(25%) of patients respectively. Intra-operative cholangiogram (IOC) and choledochoscopy were done for all patients. They were converted from LCBDE to OCBDE due to adhesions (1 patient), bleeding (1 patient), and technical failure (2 patients). After stone extraction; T- tube insertion, and HJ (1ry stone) were done in 3 (75%), and 1(25%) of them respectively. Operative bleeding affected 1 of them. The mean operative times and post-operative hospital stays were 345 ± 13 min, and 8 ± 1.4 days respectively. Lastly, postoperative chest infection affected 1 (25%) of them that was managed conservatively (Clavien II). Table 2.
Comparison between patients with T- tube insertion and primary closure of CBD:
-
1
In LCBDE group: On univariate analysis, there was a significantly longer operative time, and hospital stays in the subgroup of T-tube insertion. On the other hand, on multivariate analysis, there was no independent correlation between any variable and any of them. Table 3.
-
2
In OCBDE group: On univariate analysis, there was a significant correlation between primary closure of CBD and smaller diameter of CBD, single stone, choledochoscopy, shorter operative times and hospital stays and between multiple CBD stones and T-tube insertion. However, on multivariate analysis, there was no independent correlation between any variable and T- tube insertion or primary CBD closure. Table 4.
Table 3.
T- tube insertion VS primary closure of CBD (LCBDE group).
| Character | T- tube (No = 11) (Mean ± SD) or No (%) | Primary closure (No = 9) (Mean ± SD) or No (%) | P value Univariate analysis | P value Multivariate analysis |
|---|---|---|---|---|
| ASA score | ||||
| I | 7(63.6%) | 6(66.7%) | >0.05 | |
| II | 3(27.3%) | 3(33.3%) | ||
| III | 1(9.1%) | 0 | ||
| CBD diameter(mm) | 13.3 ± 5.6 | 13.4 ± 0.9 | ||
| No of stones | 0.1 | <0.05 | ||
| Single | 9(81.8%) | 9(100%) | ||
| Multiple | 2(18.2%) | 0 | ||
| Operative time(min) | 263.6 ± 37.8 | 191.1 ± 32.2 | 0.000 | <0.05 |
| Hospital stay(days) | 7.6 ± 1 | 3 ± 2.6 | 0.001 | <0.05 |
| Postoperativ | ||||
| complications | 2(18.2%) | 1(11.1%) | >0.05 | |
| Chest infection | 1(9.1%) | 0 | >0.05 | |
| Wound infection | 1(9.1%) | 0 | >0.05 | |
| Missed stones | 1(9.1%) | 0 | >0.05 | |
| Bile leak | 1(9.1%) | 1(11.1) | >0.05 | |
| Stricture | 0 | 0 | ||
| Recurrent stones | 0 | 0 | ||
| Success rate | 10(90.9%) | 9(100%) | >0.05 | |
ASA: American society of anesthesia, CBD: Common bile duct.
Table 4.
T- tube insertion vs. primary CBD closure in OCBDE group.
| Character | T- tube (No = 20) (Mean ± SD)or No (%) | Primary closure (No = 30) (Mean ± SD) or No (%) | P value Univariate analysis | P value Multivariate analysis |
|---|---|---|---|---|
| ASA score | ||||
| I | 15(75%) | 21(70%) | ||
| II | 3(15%) | 7(23.3%) | ||
| III | 2(10%) | 2(6.7%) | ||
| CBD diameter(mm) | 19.7 ± 4.8 | 11.8 ± 2 | 0.000 | >0.05 |
| No of stones | 0.000 | >0.05 | ||
| Single | 8 (40%) | 30(100%) | ||
| Multiple | 12(60%) | 0 | ||
| choledochoscope | 7(35%) | 29(96.7%) | 0.000 | >0.05 |
| Operative time(min) | 177.5 ± 17.1 | 125.3 ± 15.9 | 0.000 | >0.05 |
| Hospital stay(days) | 7.8 ± 0.8 | 4.4 ± 1.4 | 0.000 | >0.05 |
| Postoperative | ||||
| complications | 3(15%) | 3(10%) | >0.05 | |
| Chest infection | 2(10%) | 3(10%) | >0.05 | |
| Wound infection | 1(5%) | 0 | >0.05 | |
| Missed stones | 3(15%) | 0 | 0.05 | >0.05 |
| Bile leak | 0 | 0 | ||
| Stricture | 0 | 0 | ||
| Recurrent stones | 0 | 0 | ||
| Success rate | 17(85%) | 30(100%) | 0.05 | >0.05 |
ASA: American society of anesthesia, CBD: Common bile duct.
Comparison between patients with and without choledochoscope usage in OCBDE group: On univariate analysis, there was a significant correlation between intra-operative choledochoscope and the followings: Primary CBD repair, shorter operative time, shorter hospital stay, lower missed stones, and higher stone clearance rates. However, on multivariate analysis, there was an independent correlation between choledochoscope and performing primary repair of CBD after stone extraction. Table 5.
Table 5.
Choledochoscope usage in OCBDE group.
| Character | Choledochoscope (No = 38) (Mean ± SD) or No (%) | No choledochoscope (No = 22) (Mean ± SD) or No (%) | P value Univariate analysis | P value Multivariate analysis |
|---|---|---|---|---|
| ASA score | ||||
| I | 25(65.8%) | 15(68.2%) | >0.05 | |
| II | 10(26.3%) | 6(27.3%) | ||
| III | 3(7.9%) | 1(4.5%) | ||
| Primary repair | 29(76.3%) | 1(4.5%) | 0.000 | 0.02 |
| T- tube | 7(18.4%) | 13(59.1%) | 0.002 | <0.05 |
| Operative bleeding | 2(5.3%) | 0 | <0.05 | <0.05 |
| Operative time(min) | 140.8 ± 36.1 | 195 ± 32.3 | 0.000 | <0.05 |
| Hospital stay(days) | 5.3 ± 2 | 7.3 ± 1.4 | 0.000 | 0.06 |
| Postoperative | ||||
| complications | 4(10.5%) | 3(13.6%) | <0.05 | |
| Chest infection | 3(7.9%) | 2(9.1%) | <0.05 | |
| Wound infection | 1(2.6%) | 1(4.5%) | <0.05 | |
| Missed stones | 0 | 3(13.6%) | 0.04 | <0.05 |
| Bile leak | 0 | 0 | ||
| Stricture | 0 | 0 | ||
| Recurrent stones | 0 | 0 | ||
| Stone clearance rate | 38(100%) | 19(86.4%) | 0.04 | <0.05 |
ASA: American society of anesthesia.
4. Discussion
Various options for managing CBDS are available such as ERCP, LCBDE, and OCBDE [33,34]. However, ERCP followed by LC for managing concomitant gallbladder and CBDS is currently the preferred method in the majority of hospitals worldwide [2]. Similarly, it is the preferred method in our institute.
ERCP failure to extract stones may be due to failed cannulation (i.e., Juxta-papillary diverticulum, intra-diverticular papilla or small papilla), or failed extraction [[35], [36], [37], [38], [39]]. The failed extraction occur with difficult stones (i.e Mirrizi's syndrome, stricture of the lower CBD, impacted, large (<15 mm), multiple (<3), or intrahepatic duct/cystic duct stones), especially when using standard methods (balloon or basket after ES or endoscopic papillary balloon dilatation (EPBD)) [39,40]. In our study, failed cannulation, very large (<2 cm), multiple large, and/or impacted large stones were the causes of ERCP failure. On the other hand, in Bansal et al., 2014 [23] study, the failure was due to the inability to identify the papilla, unsuccessful cannulation, impacted stones, and duodenal perforation. However, previous operations, anatomic abnormalities and stone impaction were the causes of ERCP failure in Karaliotas et al., 2008 [41] study.
When CBDS clearance become unsuccessful, temporary stenting can serve as a bridge preventing stone impaction and cholangitis by relieving biliary obstruction and ensuring biliary drainage for further planned endoscopic stone removal or operation [3,36]. Furthermore, biliary stenting has some therapeutic benefit in case of difficult stones (I.e. difficult stones become smaller, fragmented and easier to remove at repeat ERCP or even absent after a period of stenting) [25,42,43]. Similarly, in our work, all cases with failure of stone extraction after successful cannulation were managed with single or multiple CBD stents put beside stones for drainage and possible stone fragmentation till further planned endoscopic or surgical extraction.
Post ERCP complications vary widely in the literature between 5 and 38%; due to pancreatitis, duodenal perforation, bleeding, cholangitis, and papillary stenosis [13,18,32,[44], [45], [46], [47], [48], [49], [50], [51]] It was 9.4%, 11%, and 11.1% in ours, Tai et al., 2004 [19], and Koc et al., 2013 [34] studies respectively. Where our ERCP was complicated with pancreatitis, bleeding, cholangitis, and impacted dormia in 3.5%, 2.4%, 2.4%, and 1.2% of patients respectively.
After ERCP failure, the treatment options are either LCBDE or OCBDE [45,52,53]. Furthermore, they can be performed in the complex [36], and recurrent CBDS [54], because repeated ERCP has increased complication rate [55]. Similarly, in our work, there was a significant correlation between the number of ERCP sessions and post ERCP complications.
With the advancement in laparoscopic techniques, development of new instruments for CBDE and increased experience in laparoscopic biliary surgery, many centers have started performing LCBDE with acceptable results as it is safe and efficient in the treatment of BDS [23,34,45]. Moreover, it requires training, standardization of surgical technique, accurate positioning of the trocars, a certain degree of expertise, and specific operative equipment [27,56]. Furthermore, It became the gold standard for CBDS removal when ERCP fails, [32,57,58] It can be performed by the trans-cystic approach (LTCE) or by LCD [56]. The choice of the approach is made according to the number, size, location of stones, Cystic duct, and CBD diameters, and anatomy of the cystic duct-CBD junction [4,13,14,56,59,60]. LCD is used in case of difficult, impacted, large, and/or multiple stones, and failed LTCE [15,19,35]. Moreover, it reduces the need for second invasive ERCP with reduction of costs and patient discomfort [61]. Furthermore, It provides unrestricted visualization of the biliary system, allows retrieval of difficult stones located in the extra-hepatic or intra-hepatic biliary tree, and carries a higher clearance rate than the trans-cystic approach. [1,29,32]Similarly, we started performing LCBDE recently, where Our LCBDE after ERCP failure was through LCD. In the same line, after ERCP failure, most LCBDE procedures (96%) were performed via choledochotomy in Tang and Li, 2005 [26] study, and 27.7% of LCDs were referred from the gastroenterology unit after one or more failed trials at endoscopic clearance of difficult stones in Paganini et al., 2005 [61] study.
LCD stone clearance rate ranges from 58.3% to 100%, [8,46,62] similarly, it was 80% in our study when including converted cases and 95.2% if excluding them. However, LCD stone clearance rate after ERCP failure was 62.5%, 64.51%, and 100% in Karaliotas et al., 2015 [28], Karaliotas et al., 2008 [41], and Karunadasa et al., 2016 [63] studies respectively, and it was 95.65% when performed after ERCP failure in non-dilated CBD in Jinfeng et al., 2016 [32] study, while it was 83.3% for impacted stones in Khan et al., 2015 [64] study. On the other hand, LCD stone clearance rate ranged between 82% and 100% in Mattila et al., 2017 [65], Quaresima et al., 2017 [4] Tokumura et al., 2002 [66], Grubnik et al., 2012 [67], Jinfeng et al., 2016 [1], Jinfeng et al., 2016 [32], Khaled et al., 2013 [68], Zhou et al., 2017 [15], Zhan et al., 2016 [7], and Vindal et al., 2015 [69] studies.
After LCD, the morbidity rate ranges from 4% to 26.7%, [8,46,62] similarly, after ERCP failure, LCD complication rate was 12.5%, 14.3% and 18.8% in Karaliotas et al., 2008 [41], ours and Karaliotas et al., 2015 [28] studies respectively, however, after ERCP failure, LCD in non-dilated CBD had 8.7% complication rate in Jinfeng et al., 2016 [32] study, on the other hand, the morbidity rate post-LCD ranged between 8.3% and 26.6% in Khaled et al., 2013 [68], Mattila et al., 2017 [65], Quaresima et al., 2017 [4], and Deo et al., 2018 [70] studies. Conversely, there was no major complication after LCD in Zhan et al., 2016 [7] study.
After ERCP failure, post LCD, missed stone rate was 1.09%, 3.2%, and 4.8% in Karaliotas et al., 2008 [41], Karaliotas et al., 2015 [28], and ours studies respectively, however, after ERCP failure, LCD in non-dilated CBD had no retained stone in Jinfeng et al., 2016 [32] study, while the retained stone rate after LCD for impacted stone reached 6.7% in Khan et al., 2015 [64] study, on the other hand, the retained stone rate after LCD was in the range of 1.2% and 8% in Jinfeng et al., 2016 [32], Jinfeng et al., 2016 [1], Mattila et al., 2017 [65], Khaled et al., 2013 [68], Grubnik et al., 2012 [67], Quaresima et al., 2017 [4], Tokumura et al., 2002 [66], and Paganini et al., 2005 [61] studies, conversely, there was no retained stone rate after LCD in Zhan et al., 2016 [7], and Vindal et al., 2015 [69] studies.
The LCD performed after ERCP failure had 6.3%, and 9.5% bile leaks in Karaliotas et al., 2015 [28], and our studies respectively, while LCD done in non-dilated CBD after ERCP failure had 4.35% bile leak in Jinfeng et al., 2016 [32] study, on the other hand, post LCD bile leak was in the range of 1.6% and 11% in Jinfeng et al., 2016 [1], Quaresima et al., 2017 [4], Paganini et al., 2005 [61], Jinfeng et al., 2016 [32], Khaled et al., 2013 [68] Vindal et al., 2015 [69], Tokumura et al., 2002 [66], Zhou et al., 2017 [15], Mattila et al., 2017 [65], and Reinders et al., 2014 [46] studies.
On long-term follow-up after LCD, we did not detect any recurrent stones, similarly, Khaled et al., 2013 [68] had no recurrent stone after their LCD, however, after ERCP failure, LCD in non-dilated CBD had 4.35% recurrent stone rate in Jinfeng et al., 2016 [32] study, on the other hand, the incidence of recurrent stone after LCD ranged between 1.3% and 4.3% in Jinfeng et al., 2016 [1], Jinfeng et al., 2016 [32], Tokumura et al., 2002 [66], Quaresima et al., 2017 [4] and Zhou et al., 2017 [15] studies.
There was no biliary stricture after our LCD, in similar, Jinfeng et al., 2016 [32] did not detect stricture after their LCD that was performed in non-dilated CBD after ERCP failure, also, there was no stricture post LCD in Jinfeng et al., 2016 [1], Quaresima et al., 2017 [4], Cai et al., 2012 [30], Jinfeng et al., 2016 [32], and Paganini et al., 2005 [61] studies. In contrast, Khaled et al., 2013 [68] found 0.8% post LCD stricture.
Despite advances in LCD, previous upper abdominal operations, dense adhesions, impacted, multiple stones, bleeding, and technical difficulties are causes of conversion to open surgery [1,66,70,71]. In similar, There were 4 cases of conversion in our series due to adhesions (1 patient), bleeding (1 patient), and technical failure (2 patients); this conversion reached 16%(4/25), however, the LCD done after ERCP failure conversion rate was 34.3% and 34.4% in Karaliotas et al., 2015 [28], and Karaliotas et al., 2008 [41] studies respectively, while it reached 4.35% in Jinfeng et al., 2016 [32] study that was performed in non-dilated CBD after endoscopic failure, and reached 10% in Khan et al., 2015 [64] study for impacted stones, on the other hand, LCD conversion to open ranged between 0.8% and 26.6% in Tokumura et al., 2002 [66], Grubnik et al., 2012 [67], Jinfeng et al., 2016 [32]. Jinfeng et al., 2016 [1], Quaresima et al., 2017 [4], Korontzi et al., 2012 [18], Mattila et al., 2017 [65], and Deo et al., 2018 [70] studies. Conversely, there was no post-LCD conversion in Zhan et al., 2016 [7], Khaled et al., 2013 [68], and Vindal et al., 2015 [69] studies.
Despite development in endoscopic and laparoscopic techniques, OCBDE is still the choice in some hospitals in developing countries [20,58], in many surgical clinics [66], in eastern Europe [67], in many Asian countries, [27] and in some patients ((I.e. previous surgery with dense adhesions, aberrant biliary ductal anatomy, ……) [8,72]. Furthermore, it is indicated after failure of ERCP [18,26,33,41,73,74]. Similarly, after failure of ERCP, OCBDE was the main procedure in our institution (60/81; 74.1% if excluding converted cases, and 64/85; 75.3% if including them); the reason for this is that OCBDE was our usual operation as we started LCBDE very recently.
The success rate of OCBDE ranges from 89% to 97% [17]. Similarly, it reached 98% in our study. On the other hand, the complication rate after those procedures may reach 11–14% [45]. However, it was 8%, 11.7% and 19% in Neoptolemos et al., 1987, [75] ours, and Kapoor et al., 1996 [76] studies respectively. In another line, the OCBDE performed after ERCP failure had 27% complication rate in Jalal et al., 2018 [72] study.
The retained stone rate after OCBDE ranges from 1% to 8% [73,77]. Similarly, it was 5% in our series, however, Şahiner and Kendirci, 2017 [53] did not detect any retained stones after their OCBDE. On the other hand, after long-term follow-up, we did not detect any bile leak, recurrent stones or biliary strictures after our OCBDE, similarly, Şahiner and Kendirci, 2017 [53] did not find any recurrent stones after their OCBDE. However, Jalal et al., 2018 [72] found 18% bile leak after their OCBDE that was done after ERCP failure, while, Escarce et al., 1995 [78] detected 1.1% strictures after their OCBDE that was performed in the pre-laparoscopic era.
LCBDE when performed by an experienced surgeon results in no additional morbidities as compared to OCBDE, with excellent success rates thus benefits patients with multiple, large and/or impacted stones in a dilated CBD [27]. Similarly, in our work, there was no difference between both techniques regarding morbidities or stone clearance rate with an excellent success rate in both procedures (≤95%). Also, Lin et al., 2017 [79] did not find a difference between both techniques regarding morbidity or stone clearance. In contrast, LCBDE had less morbidity when compared to OCBDE in Qiu et al., 2015, [58] and Grubnik et al., 2012 [76] studies.
We did not find any difference between LCBDE and OCBDE regarding intra-operative bleeding or post-operative hospital stays, conversely, Qiu et al., 2015, [58] and Grubnik et al., 2012 [76] found less bleeding and shorter hospital stay with the LCBDE technique. Similarly, Shelat et al., 2015, [71] and Lin et al., 2017 [79] detected shorter hospitalization with LCBDE. However, on comparing LCBDE with open surgery, we found significant independent longer operative time in the former, similarly, Lin et al., 2017 [79] found significant longer operative time with the LCBDE procedure, on the other hand, there was no difference between both procedures regarding operative time in Shelat et al., 2015, [71] or Grubnik et al., 2012 [76] studies.
After stone removal during LCD, the ductotomy is usually closed either over a T-tube or primarily [80]. Despite, T-tubes are used to prevent bile stasis, decompress the biliary tree by decreasing intra-biliary pressure and edema, achieve a controlled biliary fistula, and provide a percutaneous access for extraction of missed stones; [10,13,81] they have related complications (I.e. Tube displacement, bile leakage, peritonitis, persistent biliary fistula, cholangitis, prolonged hospital stay, fluid and electrolyte disturbances, sepsis, localised pain, discomfort and late biliary stricture, [30,53,68,81] So, primary closure of the CBD after LCD is a safe and efficient alternative with excellent results, avoiding T-tube related complications [56,59]. It can be done when complete stone extraction is ensured during the operation especially with choledochoscopy [66,82]. We used T-tube in 52.4% of our LCD patients; similarly, it was used in the range of 32.3% and 86.7% of patients in Herrero et al., 2013, [56] Tokumura et al., 2002, [66] Grubnik et al., 2012, [67] Quaresima et al.,2017, [4] Paganini et al., 2005, [61] Karaliotas et al., 2008, [41] Mattila et al., 2017, [65] and Deo et al., 2018 [70] studies. On the other hand, primary closure of CBD was performed in 42.9% of our LCD patients, in similar; its use ranged from 5.1% to 100% of patients in Paganini et al., 2005 [61], Tokumura et al., 2002 [66], Quaresima et al., 2017 [4], Grubnik et al., 2012 [67], Herrero et al., 2013 [56], and Koc et al., 2013 [34] studies.
On comparing primary closure with T-tube after LCD, we found a significantly shorter operative time and post-operative hospital stay in the former; similarly, there was shorter operative time and post-operative hospital stay with primary closure technique in different literature studies. Wu et al., 2012 [11], Podda et al., 2016 [13], Zhang et al., 2015 [14], Cai et al., 2012 [30], Herrero et al., 2013 [56], and Khaled et al., 2013 [68] However, T-tube was associated with longer postoperative stay and the time until return to work in Leida et al., 2008 [81] study.
In our study, after LCD, the T-tube was associated with a higher complication rate in comparison to primary closure (18.2% vs 11.1%). Also, Herrero et al., 2013 [56], Khaled et al., 2013 [68], Zhang et al., 2015 [14], Leida et al., 2008 [81], and Wu et al., 2012 [11] noticed similar findings. However, we found less biliary complication rate on comparing primary closure with T-tube after LCD (11.1% vs 18.2% respectively), similarly, Leida et al., 2008 [81] found less biliary complication in the primary closure group, also, Wu et al., 2012 [11] found less biliary complication without a combination of retained stone in the primary closure group, and Podda et al., 2016 [13] found that primary closure was associated with less biliary peritonitis.
After LCD, Tokumura et al., 2002 [66] found a higher incidence of bile leak and lower incidence of retained stone in their primary closure subgroup of patients. In similar, our primary closure technique had a higher biliary leak and lower missed stone in comparison to T-tube (11.1% vs 9.1%, and 0 vs 9.1% respectively). However, Leida et al., 2008 [81] detected a similar incidence of bile leak and missed stone rate between both subgroups of patients (5%, and 2.5% respectively). On the other hand, Cai et al., 2012 [30] noticed comparable bile leak with no missed stone in any of the subgroups. However, on long-term follow-up they did not detect any recurrent stones or CBD stricture, either T-tube or primary closure were done. Similarly, we did not find any recurrence or stricture after any of the techniques.
T-tube placement after OCBDE for stones was the traditional tool for decompression of the CBD and extraction of residual stones through the T-tube tract [11,13,67]. However, T-tube after OCBDE had its related complications (I.e. Wound infection, bile leakage, persistent biliary fistula, cholangitis, prolonged hospital stay, and CBD stenosis) [10,53,[83], [84], [85]]. So, primary closure of CBD after OCD is supported by some authors Seale and Ledet, 1999 [86]. It is safely done with a normal duct when the surgeon is satisfied with CBD clearance [87] and has experienced hands [20]. In similar, we performed primary closure after OCD when we were satisfied with CBD clearance by choledochoscope and by stone number where there was a significant correlation between our 1ry closure and both choledochoscope and single stones.
On comparing primary closure with T-tube drainage during OCD, we found a significant correlation between the former and shorter operative times and hospital stays with comparable complication rates. Also, Williams et al., 1994 [88] detected similar findings, while, Yamazaki et al., 2006 [89] found a significant reduction in postoperative hospital stay with primary closure when compared with T-tube with comparable complication rate, however, primary closure of CBD after OCD leads to a significantly less hospital stay in comparison to T-tube in Ambreen et al., 2009(85) study.
Choledochoscope that can be introduced through the cystic duct or CBD enables direct visualization of both extra-hepatic and intra-hepatic biliary systems ensuring their complete stones clearance with inspection of the distal bile duct for sphincter of Oddi abnormalities or retained stones [1,7,18]. It can be used with difficult stones [90]. Furthermore, it has various advantages over IOC: Better view, absence of fluoroscopy, lithotripsy performance under direct vision, a lower rate of T-tube usage, shorter operating time, higher rates of CBD clearance, and low rate of missed stones [1,7,18,27,35,85].
We used choledochoscopy in all our LCD cases with 95.2% stone clearance rate and 4.8% missed stone rate. Similarly, Koc et al., 2013 [34], and Chander et al., 2011 [27] used choledochoscope in all their LCBDE cases to ensure stone clearance. In the same line, LCD stone clearance rate using choledochoscopy reached 95%, 96.5% and 100% in Korontzi et al., 2012 [18], Karaliotas et al., 2015 [28] and Tekin, and Ogetman, 2010 [35] studies respectively. While, the retained stone rate after laparoscopic choledochoscopy ranged from 0 to 3.5% in Cai et al., 2012 [30]. Chander et al., 2011 [27] and Karaliotas et al., 2015 [28] studies.
We found a significant correlation between our open choledochoscopy and both higher stone clearance rate and lower missed stone rates, similarly, Ford et al., 2011 [91], Desai and Shokouhi, 2009 [87], and Korontzi et al., 2012 [18] detected better stone clearance rate when open choledochoscopy was used where these rates ranged between 97% and 98% in their studies. On the other hand, Takada et al., 1991 [92], and Schwarz et al., 2007 [93] found lower missed stone rate with open choledochoscopy.
To the best of our knowledge, the literature did not discuss the correlation between open choledochoscopy and performing primary CBD closure after stone removal, however, we found an independent correlation between both issues, with associated shorter operative times and hospital stays, the explanation is that when we used choledochoscope, we were satisfied with CBD stone clearance, so primary closure was done without fear of missed stones, with associated shorter both operative times and post-operative hospital stays. In conclusion: Large difficult CBD stones can be managed either by open surgery or laparoscopically with acceptable comparable outcomes with no need for multiple ERCP sessions due to their related morbidities; furthermore, Open choledochoscopy has a good impact on stone clearance rate with direction towards doing primary repair that is better than T-tube regarding operative time and hospital stay.
Financial support
Forms of support received by each author for this study included good selection of cases, instructive supervision, continuous guidance, valuable suggestions, and good instructions. Furthermore, the authors of the manuscript shared in its data collection, writing, and publication; moreover, the corresponding author did statistical analysis as well.
Ethical approval
The approval by National liver institute (IRB), Menoufia university that was done retrospectively as it was not working at the time of study.
Sources of funding
No source of funding for this research.
Author contribution
Emad Hamdy Gad: Study design, data collection, writing, statistical analysis and publication.
Hazem Zakaria: data collection, writing.
Yasmin Kamel: data collection, writing, statistical analysis.
Ayman Alsebaey: data collection, writing.
Talat Zakaria: data collection, writing.
Mohamed Abbasy: data collection, writing.
Anwar Mohamed: data collection, writing.
Ali Nada: data collection, writing.
Mohamed Housseni: data collection, writing.
Mohammed Al-sayed Abd-elsamee: Reference update.
Conflicts of interest
No conflict of interest to declare.
Trial registry number
Researchregistry4588.
Guarantor
All the authors of this paper accept full responsibility for the work and/or the conduct of the study, had access to the data, and controlled the decision to publish.
Provenance and peer review
Not commissioned, externally peer reviewed.
Acknowledgment
Thanks to the authors of the manuscript to their efforts.
The main limitation of the study is being retrospective with relatively small NO of patients. So, it is advisable to do further studies with larger no and longer follow-up period.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.amsu.2019.05.007.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Jinfeng Z., Yin Y., Chi Z., Junye G. Management of impacted common bile duct stones during a laparoscopic procedure: a Retrospective cohort study of 377 consecutive patients. Int. J. Surg. 2016;32:1–5. doi: 10.1016/j.ijsu.2016.06.006. [DOI] [PubMed] [Google Scholar]; Jinfeng Z, Yin Y, Chi Z, and Junye G. Management of impacted common bile duct stones during a laparoscopic procedure: A Retrospective cohort study of 377 consecutive patients. International Journal of Surgery 2016; 32:1-5. [DOI] [PubMed]
- 2.Tarantino G., Magistri P., Ballarin R., Assirati G., Cataldo A.D., Benedetto F.D. Surgery in biliary lithiasis: from the traditional “open” approach to laparoscopy and the “rendezvous” technique. Hepatobiliary Pancreat. Dis. Int. 2017;16:595–601. doi: 10.1016/S1499-3872(17)60031-6. [DOI] [PubMed] [Google Scholar]; Tarantino G, Magistri P, Ballarin R, Assirati G, Cataldo AD, and Benedetto FD. Surgery in biliary lithiasis: From the traditional “open” approach to laparoscopy and the “rendezvous” technique. Hepatobiliary Pancreat Dis Int 2017; 16:595-601. [DOI] [PubMed]
- 3.Hartery K., Lee C.S., Doherty G.A., Murray F.E., Cullen G., Patchett S.E. Covered self-expanding metal stents for the management of common bile duct stones. Gastrointest. Endosc. 2017;85:181–186. doi: 10.1016/j.gie.2016.05.038. [DOI] [PubMed] [Google Scholar]; Hartery K, Lee CS, Doherty GA, Murray FE, Cullen G, Patchett SE, et al. Covered self-expanding metal stents for the management of common bile duct stones. Gastrointest Endosc 2017; 85:181-186. [DOI] [PubMed]
- 4.Quaresima S., Balla A., Guerrieri M., Campagnacci R., Lezoche E., Paganini A.M. A 23 years experience with laparoscopic common bile duct exploration. HPB 2017, 19, 29–35. (40)Qadri SJF, Khan M, Khan N. Use of pneumatic lithotripsy for managing difficult CBD calculi. Int. J. Surg. 2011;9:59–62. [Google Scholar]; Quaresima S, Balla A, Guerrieri M, Campagnacci R, Lezoche E, and Paganini AM. A 23 years experience with laparoscopic common bile duct exploration. HPB 2017, 19, 29-35. (40)Qadri SJF, Khan M, Khan N. Use of pneumatic lithotripsy for managing difficult CBD calculi. International Journal of Surgery 2011; 9: 59-62.
- 5.Schwab B., Teitelbaum E.N., Barsuk J.H., Soper N.J., Hungness E.S. Single-stage laparoscopic management of choledocholithiasis: an analysis after implementation of a mastery learning resident curriculum. Surgery. 2018;163:503–508. doi: 10.1016/j.surg.2017.10.006. [DOI] [PubMed] [Google Scholar]; Schwab B, Teitelbaum EN, Barsuk JH, Soper NJ, and Hungness ES. Single-stage laparoscopic management of choledocholithiasis: An analysis after implementation of a mastery learning resident curriculum. Surgery 2018; 163: 503-508. [DOI] [PubMed]
- 6.Rosenthal R.J., Rossi R.L., Martin R.F. Options and strategies for the management of choledocholithiasis. World J. Surg. 1998;22:1125–1132. doi: 10.1007/s002689900531. [DOI] [PubMed] [Google Scholar]; Rosenthal RJ, Rossi RL, and Martin RF. Options and strategies for the management of choledocholithiasis. World J. Surg. 1998; 22:1125-1132. [DOI] [PubMed]
- 7.Zhan X., Wang Y., Zhu J., Lin X. Laparoscopic choledocholithotomy with a novel articulating forceps. Surg. Innovat. 2016;23(2):124–129. doi: 10.1177/1553350615591399. [DOI] [PubMed] [Google Scholar]; Zhan X, Wang Y, Zhu J, and Lin X. Laparoscopic choledocholithotomy with a novel articulating forceps. Surgical Innovation 2016; 23(2): 124- 129. [DOI] [PubMed]
- 8.Hungness E.S., Soper N.J. Management of common bile duct stones. J. Gastrointest. Surg. 2006;10(4):612–619. doi: 10.1016/j.gassur.2005.08.015. [DOI] [PubMed] [Google Scholar]; Hungness ES, and Soper NJ. Management of common bile duct stones. Journal of Gastrointestinal Surgery 2006; 10(4): 612-619. [DOI] [PubMed]
- 9.Verbesey J.E., Birkett D.H. Common bile duct exploration for choledocholithiasis. Surg. Clin. 2008;88:1315–1328. doi: 10.1016/j.suc.2008.08.002. [DOI] [PubMed] [Google Scholar]; Verbesey JE, and Birkett DH. Common bile duct exploration for choledocholithiasis. Surg Clin N Am 2008; 88:1315-1328. [DOI] [PubMed]
- 10.Zhu Q.D., Tao C.L., Zhou M.T., Yu Z.P., Shi H.Q., Zhang Q.Y. Primary closure versus T-tube drainage after common bile duct exploration for choledocholithiasis. Langenbeck's Arch. Surg. 2011;396:53–62. doi: 10.1007/s00423-010-0660-z. [DOI] [PubMed] [Google Scholar]; Zhu QD, Tao CL, Zhou MT, Yu ZP, Shi HQ, and Zhang QY. Primary closure versus T-tube drainage after common bile duct exploration for choledocholithiasis. Langenbecks Arch Surg 2011; 396:53-62. [DOI] [PubMed]
- 11.Wu X., Yang Y., Dong P., Gu J., Lu J., Li M. Primary closure versus T-tube drainage in laparoscopic common bile duct exploration: a meta-analysis of randomized clinical trials. Langenbeck's Arch. Surg. 2012;397:909–916. doi: 10.1007/s00423-012-0962-4. [DOI] [PubMed] [Google Scholar]; Wu X, Yang Y, Dong P, Gu J, Lu J, Li M, et al. Primary closure versus T-tube drainage in laparoscopic common bile duct exploration: A meta-analysis of randomized clinical trials. Langenbecks Arch Surg 2012; 397:909-916. [DOI] [PubMed]
- 12.Baucom R.B., Feurer I.D., Shelton1 J.S., Kummerow K., Holzman M.D., Poulose B.K. Surgeons, ERCP, and laparoscopic common bile duct exploration: do we need a standard approach for common bile duct stones? Surg. Endosc. 2016;30(2):414–423. doi: 10.1007/s00464-015-4273-z. [DOI] [PubMed] [Google Scholar]; Baucom RB, Feurer ID, Shelton1 JS, Kummerow K, Holzman MD, and Poulose BK. Surgeons, ERCP, and laparoscopic common bile duct exploration: Do we need a standard approach for common bile duct stones? Surg Endosc 2016;30(2):414-423. [DOI] [PubMed]
- 13.Podda M., Polignano F.M., Luhmann A., Wilson M.S.J., Kulli C., Tait I.S. Systematic review with meta-analysis of studies comparing primary duct closure and T-tube drainage after laparoscopic common bile duct exploration for choledocholithiasis. Surg. Endosc. 2016;30(3):845–861. doi: 10.1007/s00464-015-4303-x. [DOI] [PubMed] [Google Scholar]; Podda M, Polignano FM, Luhmann A, Wilson MSJ, Kulli C, and Tait IS. Systematic review with meta-analysis of studies comparing primary duct closure and T-tube drainage after laparoscopic common bile duct exploration for choledocholithiasis. Surgical Endoscopy 2016; 30(3):845-861. [DOI] [PubMed]
- 14.Zhang W.J., Xu G.F., Huang Q., Luo K.L., Dong Z.T., Li J.M. Treatment of gallbladder stone with common bile duct stones in the laparoscopic era. BMC Surg. 2015;15:7. doi: 10.1186/1471-2482-15-7. [DOI] [PMC free article] [PubMed] [Google Scholar]; Zhang WJ, Xu GF, Huang Q, Luo KL, Dong ZT, Li JM, et al. Treatment of gallbladder stone with common bile duct stones in the laparoscopic era. BMC Surgery 2015; 15:7. [DOI] [PMC free article] [PubMed]
- 15.Zhou Y., Zha W.Z., Wu X.D., Fan R.G., Zhang B., Xu Y.H. Three modalities on management of choledocholithiasis: a prospective cohort study. Int. J. Surg. 2017;44:269–273. doi: 10.1016/j.ijsu.2017.06.032. [DOI] [PubMed] [Google Scholar]; Zhou Y, Zha WZ, Wu XD, Fan RG, Zhang B, Xu YH et al. Three modalities on management of choledocholithiasis: A prospective cohort study. International Journal of Surgery 2017; 44: 269-273. [DOI] [PubMed]
- 16.Rizzutoa A., Fabozzia M., Settembrea A., Reggioa S., Tartagliaa E., Saverioc S.D. Intraoperative cholangiography during cholecystectomy in sequential treatment of cholecystocholedocholithiasis: to be, or not to be, that is the question: a cohort study. Int. J. Surg. 2018;53:53–58. doi: 10.1016/j.ijsu.2018.03.023. [DOI] [PubMed] [Google Scholar]; Rizzutoa A, Fabozzia M, Settembrea A, Reggioa S, Tartagliaa E, Saverioc SD et al. Intraoperative cholangiography during cholecystectomy in sequential treatment of cholecystocholedocholithiasis: To be, or not to be, that is the question: A cohort study. International Journal of Surgery 2018; 53: 53-58. [DOI] [PubMed]
- 17.Duensing R.A., Williams R.A., Collins J.C., Wilson S.E. Common bile duct stone characteristics: correlation with treatment choice during laparoscopic cholecystectomy. J. Gastrointest. Surg. 2000;4:6–12. doi: 10.1016/s1091-255x(00)80027-x. [DOI] [PubMed] [Google Scholar]; Duensing RA, Williams RA, Collins JC, and Wilson SE. Common bile duct stone characteristics: Correlation with treatment choice during laparoscopic cholecystectomy. J Gastrointest Surg. 2000;4:6-12. [DOI] [PubMed]
- 18.Korontzi M.I., Karaliotas Ch, Sgourakis G., Lanitis S., Karaliotas C. Choledochoscopy as a diagnostic and therapeutic tool for common bile duct stones. Hell. J. Surg. 2012;84:347–355. [Google Scholar]; Korontzi MI, Karaliotas Ch, Sgourakis G, Lanitis S, and Karaliotas C. Choledochoscopy as a diagnostic and therapeutic tool for common bile duct stones. Hellenic Journal of Surgery 2012; 84: 347-355.
- 19.Tai C.K., Tang C.N., Ha J.P., Chau C.H., Siu W.T., Li M.K. Laparoscopic exploration of common bile duct in difficult choledocholithiasis. Surg. Endosc. 2004;18:910–914. doi: 10.1007/s00464-003-8216-8. [DOI] [PubMed] [Google Scholar]; Tai CK, Tang CN, Ha JP, Chau CH, Siu WT, and Li MK. Laparoscopic exploration of common bile duct in difficult choledocholithiasis. Surg Endosc 2004; 18:910-914. [DOI] [PubMed]
- 20.Naraynsingh V., Hariharan S., Ramdass M.J., Dan D., Shukla P., Maharaj R. Open common bile duct exploration without T-tube insertion– two decade experience from a limited resource setting in the Caribbean. Indian J. Surg. 2010;72:185–188. doi: 10.1007/s12262-010-0060-1. [DOI] [PMC free article] [PubMed] [Google Scholar]; Naraynsingh V, Hariharan S, Ramdass MJ, Dan D, Shukla P, and Maharaj R. Open common bile duct exploration without T-tube insertion- two decade experience from a limited resource setting in the Caribbean. Indian J Surg 2010; 72:185-188. [DOI] [PMC free article] [PubMed]
- 21.Gad E.H., Abdelsamee M.A., Kamel Y. Hepatic arterial and portal venous complications after adult and pediatric living donor liver transplantation, risk factors, management and outcome (A retrospective cohort study) Ann. Med. Surg. 2016;8:28–39. doi: 10.1016/j.amsu.2016.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]; Gad EH, Abdelsamee MA, and Kamel Y. Hepatic arterial and portal venous complications after adult and pediatric living donor liver transplantation, risk factors, management and outcome (A retrospective cohort study). Annals of Medicine and Surgery 2016; 8: 28-39. [DOI] [PMC free article] [PubMed]
- 22.Agha R.A., Borrelli M.R., Vella-Baldacchino M., Thavayogan R., Orgill D.P., for the STROCSS Group The STROCSS statement: strengthening the reporting of cohort studies in surgery. Int. J. Surg. 2017;46:198–202. doi: 10.1016/j.ijsu.2017.08.586. [DOI] [PMC free article] [PubMed] [Google Scholar]; Agha RA, Borrelli MR, Vella-Baldacchino M, Thavayogan R and Orgill DP, for the STROCSS Group. The STROCSS Statement: Strengthening the Reporting of Cohort Studies in Surgery. International Journal of Surgery 2017; 46:198-202. [DOI] [PMC free article] [PubMed]
- 23.Bansal V.K., Misra M.C., Rajan K., Kilambi R., Kumar S., Krishna A. Single-stage laparoscopic common bile duct exploration and cholecystectomy versus two-stage endoscopic stone extraction followed by laparoscopic cholecystectomy for patients with concomitant gallbladder stones and common bile duct stones: a randomized controlled trial. Surg. Endosc. 2014;28:875–885. doi: 10.1007/s00464-013-3237-4. [DOI] [PubMed] [Google Scholar]; Bansal VK, Misra MC, Rajan K, Kilambi R, Kumar S, Krishna A et al. Single-stage laparoscopic common bile duct exploration and cholecystectomy versus two-stage endoscopic stone extraction followed by laparoscopic cholecystectomy for patients with concomitant gallbladder stones and common bile duct stones: A randomized controlled trial. Surg Endosc 2014; 28:875-885. [DOI] [PubMed]
- 24.Okuno M., Iwashita T., Yoshida K., Maruta A., Uemura S., Nakashima M. Significance of endoscopic sphincterotomy preceding endoscopic papillary large balloon dilation in the management of bile duct stones. Dig. Dis. Sci. 2016;61:597–602. doi: 10.1007/s10620-015-3891-6. [DOI] [PubMed] [Google Scholar]; Okuno M, Iwashita T, Yoshida K, Maruta A, Uemura S, Nakashima M et al. Significance of endoscopic sphincterotomy preceding endoscopic papillary large balloon dilation in the management of bile duct stones. Dig Dis Sci 2016; 61:597-602. [DOI] [PubMed]
- 25.Li T., Wen J., Bie K., Lu Y., Gong B. Long-term outcomes of endoscopic papillary balloon dilation for removal of bile duct stones in Billroth II gastrectomy patients. Hepatobiliary Pancreat. Dis. Int. 2018;17:257–262. doi: 10.1016/j.hbpd.2018.03.015. [DOI] [PubMed] [Google Scholar]; Li T, Wen J, Bie K, Lu Y, and Gong B. Long-term outcomes of endoscopic papillary balloon dilation for removal of bile duct stones in Billroth II gastrectomy patients. Hepatobiliary Pancreatic Diseases International 2018; 17: 257-262. [DOI] [PubMed]
- 26.Tang C.N., Li M.K.W. Technical aspects in the laparoscopic management of complicated common bile duct stones. J. Hepatobiliary Pancreat. Surg. 2005;12:444–450. doi: 10.1007/s00534-005-1029-5. [DOI] [PubMed] [Google Scholar]; Tang CN and Li MKW. Technical aspects in the laparoscopic management of complicated common bile duct stones. J Hepatobiliary Pancreat Surg 2005; 12:444-450. [DOI] [PubMed]
- 27.Chander J., Vindal A., Lal P., Gupta N., Ramteke V.K. Laparoscopic management of CBD stones: an Indian experience. Surg. Endosc. 2011;25:172–181. doi: 10.1007/s00464-010-1152-5. [DOI] [PubMed] [Google Scholar]; Chander J, Vindal A, Lal P, Gupta N, and Ramteke VK. Laparoscopic management of CBD stones: An Indian experience. Surg Endosc 2011; 25:172-181. [DOI] [PubMed]
- 28.Karaliotas C., Sgourakis G., Lanitis S., Kouloura A., Karkoulias K., Karaliotas Ch. Laparoscopic transcystic or transcholedochal choledochoscopy during common bile duct exploration for stones?Differences and similarities. Hell. J. Surg. 2015;87(5):394–406. [Google Scholar]; Karaliotas C, Sgourakis G, Lanitis S, Kouloura A, Karkoulias K, Karaliotas Ch et al. Laparoscopic transcystic or transcholedochal choledochoscopy during common bile duct exploration for stones?Differences and similarities. Hellenic Journal of Surgery 2015; 87(5): 394-406.
- 29.Xu Y., Dong C., Ma K., Long F., Jiang K., Shao P. Spontaneously removed biliary stent drainage versus T-tube drainage after laparoscopic common bile duct exploration. Medicine. 2016;95(39):1–4. doi: 10.1097/MD.0000000000005011. [DOI] [PMC free article] [PubMed] [Google Scholar]; Xu Y, Dong C, Ma K, Long F, Jiang K, Shao P, et al. Spontaneously removed biliary stent drainage versus T-tube drainage after laparoscopic common bile duct exploration. Medicine 2016; 95(39):1-4. [DOI] [PMC free article] [PubMed]
- 30.Cai H., Sun D., Sun Y., Bai J., Zhao H., Miao Y. Primary closure following laparoscopic common bile duct exploration combined with intraoperative cholangiography and choledochoscopy. World J. Surg. 2012;36:164–170. doi: 10.1007/s00268-011-1346-6. [DOI] [PubMed] [Google Scholar]; Cai H, Sun D, Sun Y, Bai J, Zhao H, and Miao Y. Primary closure following laparoscopic common bile duct exploration combined with intraoperative cholangiography and choledochoscopy. World J Surg 2012; 36:164-170. [DOI] [PubMed]
- 31.Lyon M., Menon S., Jain A., Kumar H. Use of biliary stent in laparoscopic common bile duct exploration. Surg. Endosc. 2015;29:1094–1098. doi: 10.1007/s00464-014-3797-y. [DOI] [PubMed] [Google Scholar]; Lyon M, Menon S, Jain A, and Kumar H. Use of biliary stent in laparoscopic common bile duct exploration. Surg Endosc 2015; 29:1094-1098. [DOI] [PubMed]
- 32.Jinfeng Z., Yin Y., Chi Z., Junye G. Laparoscopic management after failed endoscopic stone removal in nondilated common bile duct. Int. J. Surg. 2016;29:49–52. doi: 10.1016/j.ijsu.2016.03.037. [DOI] [PubMed] [Google Scholar]; Jinfeng Z, Yin Y, Chi Z, and Junye G. Laparoscopic management after failed endoscopic stone removal in nondilated common bile duct. International Journal of Surgery 2016; 29: 49-52. [DOI] [PubMed]
- 33.Costi R., Mazzeo A., Tartamella F., Manceau C., Vacher B., Valverde A. Cholecystocholedocholithiasis: a case–control study comparing the short- and long-term outcomes for a ‘‘laparoscopy-first’’ attitude with the outcome for sequential treatment (systematic endoscopic sphincterotomy followed by laparoscopic cholecystectomy) Surg. Endosc. 2010;24:51–62. doi: 10.1007/s00464-009-0511-6. [DOI] [PubMed] [Google Scholar]; Costi R, Mazzeo A, Tartamella F, Manceau C, Vacher B, and Valverde A. Cholecystocholedocholithiasis: A case-control study comparing the short- and long-term outcomes for a ‘‘laparoscopy-first’’ attitude with the outcome for sequential treatment (systematic endoscopic sphincterotomy followed by laparoscopic cholecystectomy). Surg Endosc 2010; 24:51-62. [DOI] [PubMed]
- 34.Koc B., Karahan S., Adas G., Tutal F., Guven H., Ozsoy A. Comparison of laparoscopic common bile duct exploration and endoscopic retrograde cholangiopancreatography plus laparoscopic cholecystectomy for choledocholithiasis: a prospective randomized study. Am. J. Surg. 2013;206:457–463. doi: 10.1016/j.amjsurg.2013.02.004. [DOI] [PubMed] [Google Scholar]; Koc B, Karahan S, Adas G, Tutal F, Guven H, and Ozsoy A. Comparison of laparoscopic common bile duct exploration and endoscopic retrograde cholangiopancreatography plus laparoscopic cholecystectomy for choledocholithiasis: A prospective randomized study. The American Journal of Surgery 2013; 206: 457-463. [DOI] [PubMed]
- 35.Tekin A., Ogetman Z. Laparoscopic exploration of the common bile duct with a rigid scope in patients with problematic choledocholithiasis. World J. Surg. 2010;34:1894–1899. doi: 10.1007/s00268-010-0534-0. [DOI] [PubMed] [Google Scholar]; Tekin A, and Ogetman Z. Laparoscopic exploration of the common bile duct with a rigid scope in patients with problematic choledocholithiasis. World J Surg 2010; 34:1894-1899. [DOI] [PubMed]
- 36.Martin J.A. Endoscopic retrograde cholangiopancreatography in the management of bile duct stones. Tech. Gastrointest. Endosc. 2012;14:156–163. [Google Scholar]; Martin JA. Endoscopic retrograde cholangiopancreatography in the management of bile duct stones. Techniques in Gastrointestinal Endoscopy 2012; 14: 156-163.
- 37.Cecinato P., Fuccio L., Azzaroli F., Lisotti A., Correale L., Hassan C. Extracorporeal shock wave lithotripsy for difficult common bile duct stones: a comparison between 2 different lithotripters in a large cohort of patients. Gastrointest. Endosc. 2015;81:402–409. doi: 10.1016/j.gie.2014.04.059. [DOI] [PubMed] [Google Scholar]; Cecinato P, Fuccio L, Azzaroli F, Lisotti A, Correale L, Hassan C et al. Extracorporeal shock wave lithotripsy for difficult common bile duct stones: A comparison between 2 different lithotripters in a large cohort of patients. Gastrointest Endosc 2015; 81:402-409. [DOI] [PubMed]
- 38.Lohb W.L., Tunga J.Y.M., Tana T.H.Y., Tana L.T., Tana S., Ngoia S.S. Novel use of a balloon dilatation catheter to enable mechanical lithotripsy of difficult common bile duct stones after initial failed attempt: a case report. Int. J. Surg. Case Rep. 2018;43:9–12. doi: 10.1016/j.ijscr.2018.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]; Lohb WL, Tunga JYM, Tana THY, Tana LT, Tana S, and Ngoia SS. Novel use of a balloon dilatation catheter to enable mechanical lithotripsy of difficult common bile duct stones after initial failed attempt: A case report. International Journal of Surgery Case Reports 2018; 43 9-12. [DOI] [PMC free article] [PubMed]
- 39.Gutierrez O.I.B., Bekkali N.L.H., Raijman I., Sturgess R., Sejpal D.V., Aridi H.D. Efficacy and safety of digital single-operator cholangioscopy for difficult biliary stones. Pancreas,biliary tract, and liver. Clin. Gastroenterol. Hepatol. 2018;16:918–926. doi: 10.1016/j.cgh.2017.10.017. [DOI] [PubMed] [Google Scholar]; Gutierrez OIB, Bekkali NLH, Raijman I, Sturgess R, Sejpal DV, Aridi HD et al. Efficacy and safety of digital single-operator cholangioscopy for difficult biliary stones. Pancreas,biliary tract, and liver. Clinical Gastroenterology and Hepatology 2018; 16:918-926. [DOI] [PubMed]
- 40.Qadri S.J.F., Khan M., Khan N. Use of pneumatic lithotripsy for managing difficult CBD calculi. Int. J. Surg. 2011;9:59–62. doi: 10.1016/j.ijsu.2010.08.009. [DOI] [PubMed] [Google Scholar]; Qadri SJF, Khan M, Khan N. Use of pneumatic lithotripsy for managing difficult CBD calculi. International Journal of Surgery 2011; 9: 59-62. [DOI] [PubMed]
- 41.Karaliotas C., Sgourakis G., Goumas C., Papaioannou N., Lilis C., Leandros E. Laparoscopic common bile duct exploration after failed endoscopic stone extraction. Surg. Endosc. 2008;22:1826–1831. doi: 10.1007/s00464-007-9708-8. [DOI] [PubMed] [Google Scholar]; Karaliotas C, Sgourakis G, Goumas C, Papaioannou N, Lilis C, and Leandros E. Laparoscopic common bile duct exploration after failed endoscopic stone extraction. Surg Endosc 2008; 22:1826- 1831. [DOI] [PubMed]
- 42.Cerefice M., Sauer B., Javaid M., Smith L.A., Gosain S., Argo C.K. Complex biliary stones: treatment with removable self-expandable metal stents: a new approach. Gastrointest. Endosc. 2011;74:520–526. doi: 10.1016/j.gie.2011.05.026. [DOI] [PubMed] [Google Scholar]; Cerefice M, Sauer B, Javaid M, Smith LA, Gosain S, Argo CK et al. Complex biliary stones: Treatment with removable self-expandable metal stents: A new approach. Gastrointest Endosc 2011;74:520-526. [DOI] [PubMed]
- 43.Yang J., Peng J.Y., Chen W. Endoscopic biliary stenting for irretrievable common bile duct stones: indications, advantages, disadvantages, and follow-up results. The Surgeon, J. Roy. Coll. Surg. Edinburgh Ireland. 2012 Aug;10(4):211–217. doi: 10.1016/j.surge.2012.04.003. Surgeon. Epub 2012 May 29. [DOI] [PubMed] [Google Scholar]; Yang J, Peng JY, and Chen W. Endoscopic biliary stenting for irretrievable common bile duct stones: Indications, advantages, disadvantages, and follow-up results. The Surgeon, Journal of the Royal Colleges of Surgeons of Edinburgh and Ireland. The surgeon 2 0 1 2;1 0: 2 1 1-2 1 7. [DOI] [PubMed]
- 44.Paganini A.M., Guerrieri M., Sarnari J., Sanctis A.D., Ambrosio G.D., Lezoche G. Thirteen years experience with laparoscopic transcystic common bile duct exploration for stones: effectiveness and long-term results. Surg. Endosc. 2007;21:34–40. doi: 10.1007/s00464-005-0286-3. [DOI] [PubMed] [Google Scholar]; Paganini AM, Guerrieri M, Sarnari J, Sanctis AD, Ambrosio GD, Lezoche G et al. Thirteen years experience with laparoscopic transcystic common bile duct exploration for stones: Effectiveness and long-term results. Surg Endosc 2007; 21: 34-40. [DOI] [PubMed]
- 45.Sharma A., Dahiya P., Khullar R., Soni V., Baijal M., Chowbey P.K. Management of common bile duct stones in the laparoscopic era. Indian J. Surg. 2012;74(3):264–269. doi: 10.1007/s12262-012-0593-6. [DOI] [PMC free article] [PubMed] [Google Scholar]; Sharma A, Dahiya P, Khullar R, Soni V, Baijal M, and Chowbey PK. Management of common bile duct stones in the laparoscopic era. Indian J Surg 2012; 74(3):264-269. [DOI] [PMC free article] [PubMed]
- 46.Reinders J.S.K., Gouma D.J., Ubbink D.T., Ramshorst B.V., Boerma D. Transcystic or transductal stone extraction during single-stage treatment of choledochocystolithiasis: a systematic review. World J. Surg. 2014;38:2403–2411. doi: 10.1007/s00268-014-2537-8. [DOI] [PubMed] [Google Scholar]; Reinders JSK, Gouma DJ, Ubbink DT, Ramshorst BV, and Boerma D. Transcystic or transductal stone extraction during single-stage treatment of choledochocystolithiasis: A systematic review. World J Surg 2014; 38:2403-2411. [DOI] [PubMed]
- 47.Kuo C.M., Chiu Y.C., Liang C.M., Lu L.S., Tai W.C., Kuo Y.H. Limited precut sphincterotomy combined with endoscopic papillary balloon dilation for common bile duct stone removal in patients with difficult biliary cannulation. BMC Gastroenterol. 2016;16:70. doi: 10.1186/s12876-016-0486-4. [DOI] [PMC free article] [PubMed] [Google Scholar]; Kuo CM, Chiu YC, Liang CM, Lu LS, Tai WC, Kuo YH et al. Limited precut sphincterotomy combined with endoscopic papillary balloon dilation for common bile duct stone removal in patients with difficult biliary cannulation. BMC Gastroenterology 2016; 16:70. [DOI] [PMC free article] [PubMed]
- 48.Chandrasekhara V., Khashab M.A., Muthusamy V.R., Acosta R.D., Agrawal D., Bruining D.H. Adverse events associated with ERCP. Gastrointest. Endosc. 2017;85(1):32–47. doi: 10.1016/j.gie.2016.06.051. [DOI] [PubMed] [Google Scholar]; Chandrasekhara V, Khashab MA, Muthusamy VR, Acosta RD, Agrawal D, Bruining DH et al. Adverse events associated with ERCP. Gastrointestinal endoscopy 2017; 85(1): 32-47. [DOI] [PubMed]
- 49.Netinatsunton N., Sottisuporn J., Attasaranya S., Witeerungrot T., Siripun A., Pattarapuntakul T. Prospective randomized trial of EUS-assisted ERCP without fluoroscopy versus ERCP in common bile duct stones. Gastrointest. Endosc. 2017;86:1059–1065. doi: 10.1016/j.gie.2017.03.1539. [DOI] [PubMed] [Google Scholar]; Netinatsunton N, Sottisuporn J, Attasaranya S, Witeerungrot T, Siripun A, Pattarapuntakul T et al. Prospective randomized trial of EUS-assisted ERCP without fluoroscopy versus ERCP in common bile duct stones. Gastrointest Endosc 2017; 86:1059-1065. [DOI] [PubMed]
- 50.Park C.H., Jung J.H., Nam E., Kim E.H., Kim M.G., Kim J.H. Comparative efficacy of various endoscopic techniques for the treatment of common bile duct stones: a network meta-analysis. Gastrointest. Endosc. 2018;87:43–57. doi: 10.1016/j.gie.2017.07.038. [DOI] [PubMed] [Google Scholar]; Park CH, Jung JH, Nam E, Kim EH, Kim MG, Kim JH, et al. Comparative efficacy of various endoscopic techniques for the treatment of common bile duct stones: A network meta-analysis. Gastrointest Endosc 2018;87:43-57. [DOI] [PubMed]
- 51.Buxbaum J., Sahakian A., Ko C., Jayaram P., Lane C., Yu C.Y. Randomized trial of cholangioscopy-guided laser lithotripsy versus conventional therapy for large bile duct stones. Gastrointest. Endosc. 2018;87:1050–1060. doi: 10.1016/j.gie.2017.08.021. [DOI] [PubMed] [Google Scholar]; Buxbaum J, Sahakian A, Ko C, Jayaram P, Lane C, Yu CY et al. Randomized trial of cholangioscopy-guided laser lithotripsy versus conventional therapy for large bile duct stones. Gastrointest Endosc 2018; 87:1050-1060. [DOI] [PubMed]
- 52.Williams E.J., Green J., Beckingham I., Parks R., Martin D., Lombard M. Guidelines on the management of common bile duct stones (CBDS) Gut. 2008;57(7):1004–1021. doi: 10.1136/gut.2007.121657. [DOI] [PubMed] [Google Scholar]; Williams EJ, Green J, Beckingham I, Parks R, Martin D, and Lombard M. Guidelines on the management of common bile duct stones (CBDS). Gut 2008; 57(7):1004-1021. [DOI] [PubMed]
- 53.Şahiner İ.T., Kendirci M. Retrospective clinical study of the effects of T-tube placement for bile duct stricture. Med. Sci. Monit. 2017;23:4328–4333. doi: 10.12659/MSM.906630. [DOI] [PMC free article] [PubMed] [Google Scholar]; Şahiner İT, and Kendirci M. Retrospective clinical study of the effects of T-tube placement for bile duct stricture. Med Sci Monit 2017; 23: 4328-4333. [DOI] [PMC free article] [PubMed]
- 54.Uchiyama K., Onishi H., Tani M., Kinoshita H., Kawai M., Ueno M. Long-term prognosis after treatment of patients with choledocholithiasis. Ann. Surg. 2003;238:97–102. doi: 10.1097/01.sla.0000077923.38307.84. [DOI] [PMC free article] [PubMed] [Google Scholar]; Uchiyama K, Onishi H, Tani M, Kinoshita H, Kawai M, Ueno M et al. Long-term prognosis after treatment of patients with choledocholithiasis. Ann Surg 2003; 238: 97-102. [DOI] [PMC free article] [PubMed]
- 55.Hey S.Y., Driscoll P.J., Yalamarthi S., Robson A.J. Analysis of endoscopic and surgical management of common bile duct stones in the laparoscopic era. Int. J. Surg. 2014;12:S13–S117. [Google Scholar]; Hey SY, Driscoll PJ, Yalamarthi S, and Robson AJ. Analysis of endoscopic and surgical management of common bile duct stones in the laparoscopic era. International Journal of Surgery 2014; 12: S13-S117.
- 56.Herrero A., Philippe C., Guillon F., Millat B., Borie F. Does the surgeon's experience influence the outcome of laparoscopic treatment of common bile duct stones? Surg. Endosc. 2013;27:176–180. doi: 10.1007/s00464-012-2416-z. [DOI] [PubMed] [Google Scholar]; Herrero A, Philippe C, Guillon F, Millat B, and Borie F. Does the surgeon’s experience influence the outcome of laparoscopic treatment of common bile duct stones? Surg Endosc 2013; 27:176-180. [DOI] [PubMed]
- 57.Zhou Y., Wu X.D., Fan R.G., Zhou G.J., Mu X.M., Zha W.Z. Laparoscopic common bile duct exploration and primary closure of choledochotomy after failed endoscopic sphincterotomy. Int. J. Surg. 2014;12:645–648. doi: 10.1016/j.ijsu.2014.05.059. [DOI] [PubMed] [Google Scholar]; Zhou Y, Wu XD, Fan RG, Zhou GJ, Mu XM, Zha WZ, et al., Laparoscopic common bile duct exploration and primary closure of choledochotomy after failed endoscopic sphincterotomy, Int. J. Surg. 2014; 12: 645-648. [DOI] [PubMed]
- 58.Qiu J., Yuan H., Chen S., Wu H. Laparoscopic common bile duct exploration in cirrhotic patients with choledocholithiasis. J. Clin. Gastroenterol. 2015;49:132–136. doi: 10.1097/MCG.0000000000000068. [DOI] [PubMed] [Google Scholar]; Qiu J, Yuan H, Chen S, and Wu H. Laparoscopic common bile duct exploration in cirrhotic patients with choledocholithiasis. J Clin Gastroenterol 2015;49:132-136. [DOI] [PubMed]
- 59.Zhu H.Y., Xu M., Shen H.J., Yang C., Li F., Li K.W. A meta-analysis of single-stage versus two-stage management for concomitant gallstones and common bile duct stones. Clin. Res. Hepatol. Gastroenterol. 2015;39:584–593. doi: 10.1016/j.clinre.2015.02.002. [DOI] [PubMed] [Google Scholar]; Zhu HY, Xu M, Shen HJ, Yang C, Li F, Li KW et al. A meta-analysis of single-stage versus two-stage management for concomitant gallstones and common bile duct stones. Clinics and Research in Hepatology and Gastroenterology 2015; 39: 584-593. [DOI] [PubMed]
- 60.Gupta N. Role of laparoscopic common bile duct exploration in the management of choledocholithiasis. World J. Gastrointest. Surg. 2016;8(5):376–381. doi: 10.4240/wjgs.v8.i5.376. [DOI] [PMC free article] [PubMed] [Google Scholar]; Gupta N. Role of laparoscopic common bile duct exploration in the management of choledocholithiasis. World J Gastrointest Surg 2016; 8(5): 376-381. [DOI] [PMC free article] [PubMed]
- 61.Paganini A.M., Guerrieri M., Sarnari J., Sanctis A.D., Ambrosio G.D., Lezoche G. Long-term results after laparoscopic transverse choledochotomy for common bile duct stones. Surg. Endosc. 2005;19:705–709. doi: 10.1007/s00464-004-8944-4. [DOI] [PubMed] [Google Scholar]; Paganini AM, Guerrieri M, Sarnari J, Sanctis AD, Ambrosio GD, Lezoche G et al. Long-term results after laparoscopic transverse choledochotomy for common bile duct stones. Surg Endosc 2005; 19: 705-709. [DOI] [PubMed]
- 62.Vecchio R., MacFayden B.V. Laparoscopic common bile duct exploration. Langenbeck's Arch. Surg. 2002;387:45–54. doi: 10.1007/s00423-002-0289-7. [DOI] [PubMed] [Google Scholar]; Vecchio R, and MacFayden BV: Laparoscopic common bile duct exploration. Langenbeck’s Arch Surg 2002; 387:45-54. [DOI] [PubMed]
- 63.Karunadasa M.S.E., Rathnasena B.G.N., Nanayakkara K.D.L. Management of choice for common bile duct stones: laparoscopic common bile duct exploration (LCBDE), first SRI Lankan experience. HPB. 2016;18(S1):e385–e601. [Google Scholar]; Karunadasa MSE, Rathnasena BGN and Nanayakkara KDL. Management of choice for common bile duct stones: Laparoscopic common bile duct exploration (LCBDE), first SRI Lankan experience. HPB 2016; 18 (S1): e385-e601.
- 64.Khan J., Nassar M.K., Lau J., Qandeel H., Nassar A. Management of impacted bile duct stones encountered during laparoscopic bile duct exploration(LCBDE) Int. J. Surg. 2015;23:S15–S134. [Google Scholar]; Khan J, Nassar MK, Lau J, Qandeel H, and Nassar A. Management of impacted bile duct stones encountered during laparoscopic bile duct exploration(LCBDE). International Journal of Surgery 2015; 23: S15-S134.
- 65.Mattila A., Mrena J., Kellokumpu I. Cost-analysis and effectiveness of one-stage laparoscopic versus two-stage endo-laparoscopic management of cholecystocholedocholithiasis: a retrospective cohort study. BMC Surg. 2017;17(79):1–8. doi: 10.1186/s12893-017-0274-2. [DOI] [PMC free article] [PubMed] [Google Scholar]; Mattila A, Mrena J, and Kellokumpu I. Cost-analysis and effectiveness of one-stage laparoscopic versus two-stage endo-laparoscopic management of cholecystocholedocholithiasis: A retrospective cohort study. BMC Surgery 2017;17(79):1-8. [DOI] [PMC free article] [PubMed]
- 66.Tokumura H., Umezawa A., Cao H., Sakamoto N., Imaoka Y., Ouchi A. Laparoscopic management of common bile duct stones: transcystic approach and choledochotomy. J. Hepatobiliary Pancreat. Surg. 2002;9:206–212. doi: 10.1007/s005340200020. [DOI] [PubMed] [Google Scholar]; Tokumura H, Umezawa A, Cao H, Sakamoto N, Imaoka Y, Ouchi A et al. Laparoscopic management of common bile duct stones: Transcystic approach and choledochotomy. J Hepatobiliary Pancreat Surg 2002; 9:206-212. [DOI] [PubMed]
- 67.Grubnik V.V., Tkachenko A.I., Ilyashenko V.V., Vorotyntseva K.O. Laparoscopic common bile duct exploration versus open surgery: comparative prospective randomized trial. Surg. Endosc. 2012;26:2165–2171. doi: 10.1007/s00464-012-2194-7. [DOI] [PubMed] [Google Scholar]; Grubnik VV, Tkachenko AI, Ilyashenko VV, and Vorotyntseva KO. Laparoscopic common bile duct exploration versus open surgery: Comparative prospective randomized trial. Surg Endosc 2012; 26:2165-2171. [DOI] [PubMed]
- 68.Khaled Y.S., Malde D.J., Souza C.D., Kalia A., Ammori B.J. Laparoscopic bile duct exploration via choledochotomy followed by primary duct closure is feasible and safe for the treatment of choledocholithiasis. Surg. Endosc. 2013;27:4164–4170. doi: 10.1007/s00464-013-3015-3. [DOI] [PubMed] [Google Scholar]; Khaled YS, Malde DJ, Souza CD, Kalia A, and Ammori BJ. Laparoscopic bile duct exploration via choledochotomy followed by primary duct closure is feasible and safe for the treatment of choledocholithiasis. Surg Endosc 2013; 27:4164-4170. [DOI] [PubMed]
- 69.Vindal A., Chander J., Lal P., Mahendra B. Comparison between intraoperative cholangiography and choledochoscopy for ductal clearance in laparoscopic CBD exploration: a prospective randomized study. Surg. Endosc. 2015;29:1030–1038. doi: 10.1007/s00464-014-3766-5. [DOI] [PubMed] [Google Scholar]; Vindal A, Chander J, Lal P, and Mahendra B. Comparison between intraoperative cholangiography and choledochoscopy for ductal clearance in laparoscopic CBD exploration: A prospective randomized study. Surg Endosc 2015; 29:1030-1038. [DOI] [PubMed]
- 70.Deo K.B., Adhikary S., Khaniya S., Shakya V.C., Agrawal C.S. Laparoscopic choledochotomy in a solitary common duct stone: a prospective study. Minim. Invasive Surg. 2018;2018:1–5. doi: 10.1155/2018/8080625. [DOI] [PMC free article] [PubMed] [Google Scholar]; Deo KB, Adhikary S, Khaniya S, Shakya VC, and Agrawal CS. Laparoscopic choledochotomy in a solitary common duct stone: A prospective study. Minimally Invasive Surgery 2018; 2018:1-5. [DOI] [PMC free article] [PubMed]
- 71.Shelat V.G., Chan C.Y., Liau K.H., Ho C.K. Laparoscopic exploration can salvage failed endoscopic bile duct stone extraction. Singap. Med. J. 2012;53(5):313–317. [PubMed] [Google Scholar]; Shelat VG, Chan CY, Liau KH, and Ho CK, “Laparoscopic exploration can salvage failed endoscopic bile duct stone extraction,” Singapore Medical Journal 2012;53(5):313-317. [PubMed]
- 72.Jalal Q., Forouzanfar A., Bhatt A., Al-Mukhtar A., Thorpe J.G., Majeed A.W. Case series of ante-grade biliary stenting: an option during bile duct exploration. Int. J. Surg. Open. 2018;10:10–14. [Google Scholar]; Jalal Q, Forouzanfar A, Bhatt A, Al-Mukhtar A, Thorpe JG, and Majeed AW. Case series of ante-grade biliary stenting: An option during bile duct exploration. International Journal of Surgery Open 2018; 10:10-14.
- 73.Boerma D., Schwartz M.P. Management of common bile-duct stones and associated gallbladder stones: surgical aspects. Best Pract. Res. Clin. Gastroenterol. 2006;20(6):1103–1116. doi: 10.1016/j.bpg.2006.04.002. [DOI] [PubMed] [Google Scholar]; Boerma D, and Schwartz MP. Management of common bile-duct stones and associated gallbladder stones: Surgical aspects. Best Practice & Research Clinical Gastroenterology2006; 20(6): 1103-1116. [DOI] [PubMed]
- 74.Deal A.K., Murthy S., Wason S., Vingan H., Fabrizio M. Percutaneous transhepatic holmium laser lithotripsy of a large common bile duct stone. Radiol. Case Rep. 2016;11:361–364. doi: 10.1016/j.radcr.2016.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]; Deal AK, Murthy S, Wason S, Vingan H, and Fabrizio M. Percutaneous transhepatic holmium laser lithotripsy of a large common bile duct stone. Radiology Case Reports 2016;11: 361-364. [DOI] [PMC free article] [PubMed]
- 75.Neoptolemos J.P., CarrLocke D.L., Fossat D.D. Prospective randomized study of preoperative endoscopic surgery versus surgery alone for common bile duct stones. BMJ. 1987;294:470. doi: 10.1136/bmj.294.6570.470. [DOI] [PMC free article] [PubMed] [Google Scholar]; Neoptolemos JP, CarrLocke DL, and Fossat DD: Prospective randomized study of preoperative endoscopic surgery versus surgery alone for common bile duct stones. B.M.J. 1987; 294:470. [DOI] [PMC free article] [PubMed]
- 76.Kapoor R., Kanshik S.P., Saroswat V.A. Prospective randomized trial comparing endoscopic sphincterotomy followed by surgery with surgery alone in good risk patients with choledocholithiasis. HPB Surg. 1996;9:145. doi: 10.1155/1996/64373. [DOI] [PMC free article] [PubMed] [Google Scholar]; Kapoor R, Kanshik SP, and Saroswat VA: Prospective randomized trial comparing endoscopic sphincterotomy followed by surgery with surgery alone in good risk patients with choledocholithiasis. H.P.B. Surg.1996; 9:145. [DOI] [PMC free article] [PubMed]
- 77.Moreaux J. Traditional surgical management of common bile duct stones: a prospective study during a 20 year experience. Am. J. Surg. 1995;169:220–226. doi: 10.1016/S0002-9610(99)80141-X. [DOI] [PubMed] [Google Scholar]; Moreaux J. Traditional surgical management of common bile duct stones: A prospective study during a 20 year experience. Am J Surg 1995; 169: 220-226. [DOI] [PubMed]
- 78.Escarce J.J., Shea J.A., Chen W., Qian Z., Schwartz J.S. Outcomes of open cholecystectomy in the elderly: a longitudinal analysis of 21,000 cases in the pre-laparoscopic era. Surgery. 1995;117:156–164. doi: 10.1016/s0039-6060(05)80079-0. [DOI] [PubMed] [Google Scholar]; Escarce JJ, Shea JA, Chen W, Qian Z, and Schwartz JS. Outcomes of open cholecystectomy in the elderly: A longitudinal analysis of 21,000 cases in the pre-laparoscopic era. Surgery 1995; 117: 156-164. [DOI] [PubMed]
- 79.Lin Y.F., Tian Y.F., Uen Y.H. Common bile duct exploration for elderly patients with choledocholithiasis: is laparoscopic method better? Formos J. Surg. 2017;50:158–162. [Google Scholar]; Lin YF, Tian YF, and Uen YH. Common bile duct exploration for elderly patients with choledocholithiasis: Is laparoscopic method better? Formos J Surg 2017; 50:158-162.
- 80.Petelin J.B. Surgical management of common bile duct stones. Gastrointest. Endosc. 2002;56:s183–s189. doi: 10.1067/mge.2002.1290131. [DOI] [PubMed] [Google Scholar]; Petelin JB. Surgical management of common bile duct stones. Gastrointestinal Endoscopy 2002;56:s183-s189. [DOI] [PubMed]
- 81.Leida Z., Ping B., Shuguang W., Yu H. A randomized comparison of primary closure and T-tube drainage of the common bile duct after laparoscopic choledochotomy. Surg. Endosc. 2008;22:1595–1600. doi: 10.1007/s00464-007-9731-9. [DOI] [PubMed] [Google Scholar]; Leida Z, Ping B, Shuguang W, and Yu H. A randomized comparison of primary closure and T-tube drainage of the common bile duct after laparoscopic choledochotomy. Surg Endosc 2008; 22:1595-1600. [DOI] [PubMed]
- 82.Liu D., Cao F., Liu J., Xu D., Wang Y., Li F. Risk factors for bile leakage after primary closure following laparoscopic common bile duct exploration: a retrospective cohort study. BMC Surg. 2017;17(1):1–8. doi: 10.1186/s12893-016-0201-y. [DOI] [PMC free article] [PubMed] [Google Scholar]; Liu D, Cao F, Liu J, Xu D, Wang Y and Li F. Risk factors for bile leakage after primary closure following laparoscopic common bile duct exploration: A retrospective cohort study. BMC Surgery 2017; 17(1):1-8. [DOI] [PMC free article] [PubMed]
- 83.Wills V.L., Gibson K., Karihaloo C., Jorgensen J.O. Complications of biliary T-tubes after choledochotomy. ANZ J. Surg. 2002;72:177–180. doi: 10.1046/j.1445-2197.2002.02308.x. [DOI] [PubMed] [Google Scholar]; Wills VL, Gibson K, Karihaloo C, and Jorgensen JO. Complications of biliary T-tubes after choledochotomy. ANZ J Surg 2002;72:177-180. [DOI] [PubMed]
- 84.Hotta T., Taniguchi K., Kobayashi Y., Johata K., Sahara M., Naka T. Biliary drainage tube evaluation after common bile duct exploration for choledocholithiasis. Hepato-Gastroenterology. 2003;50:315–321. [PubMed] [Google Scholar]; Hotta T, Taniguchi K, Kobayashi Y, Johata K, Sahara M, Naka T,et al. Biliary drainage tube evaluation after common bile duct exploration for choledocholithiasis. Hepatogastroenterology 2003;50:315-321. [PubMed]
- 85.Ambreen M., Shaikh A.R., Jamal A., Qureshi J.N., Dalwani A.G., Memon M.M. Primary closure versus T-tube drainage after open choledochotomy. Asian J. Surg. 2009;32(1):21–25. doi: 10.1016/S1015-9584(09)60004-X. [DOI] [PubMed] [Google Scholar]; Ambreen M, Shaikh AR, Jamal A, Qureshi JN, Dalwani AG and Memon MM. Primary closure versus T-tube drainage after open choledochotomy. Asian J Surg 2009;32(1):21-25. [DOI] [PubMed]
- 86.Seale A.K., Ledet W.P. Primary common bile duct closure. Arch. Surg. 1999;134:22–24. doi: 10.1001/archsurg.134.1.22. [DOI] [PubMed] [Google Scholar]; Seale AK, and Ledet WP. Primary common bile duct closure. Arch Surg 1999;134:22-24. [DOI] [PubMed]
- 87.Desai R., Shokouhi B.N. Common bile duct stones – their presentation, diagnosis and management. Indian J. Surg. 2009;71:229–237. doi: 10.1007/s12262-009-0050-3. [DOI] [PMC free article] [PubMed] [Google Scholar]; Desai R and Shokouhi BN. Common bile duct stones - Their presentation, diagnosis and management. Indian J Surg 2009; 71:229-237. [DOI] [PMC free article] [PubMed]
- 88.Williams J.A., Treacy P.J., Sidey P., Worthley C.S., Townsend N.C., Russell E.A. Primary duct closure versus T-tube drainage following exploration of the common bile duct. Aust. N. Z. J. Surg. 1994;64:823–826. doi: 10.1111/j.1445-2197.1994.tb04556.x. [DOI] [PubMed] [Google Scholar]; Williams JA, Treacy PJ, Sidey P, Worthley CS, Townsend NC, and Russell EA. Primary duct closure versus T-tube drainage following exploration of the common bile duct. Aust NZ J Surg 1994; 64:823-826. [DOI] [PubMed]
- 89.Yamazaki M., Yasuda H., Tsukamoto S., Koide Y., Yarita T., Tezuka T. Primary closure of the common bile duct in open laparotomy for common bile duct stones. J. Hepatobiliary Pancreat. Surg. 2006;13:398–402. doi: 10.1007/s00534-005-1097-6. [DOI] [PubMed] [Google Scholar]; Yamazaki M, Yasuda H, Tsukamoto S, Koide Y, Yarita T, Tezuka T et al. Primary closure of the common bile duct in open laparotomy for common bile duct stones. J Hepatobiliary Pancreat Surg 2006; 13:398-402. [DOI] [PubMed]
- 90.Cuendis-Velαzquez A., Rojano-Rodriguez M.E., Morales- Chαvez C.E., González Angulo-Rocha A., Fernández-Castro E., Aguirre-Olmedo I. Intraoperative choledochoscopy usefulness in the treatment of difficult biliary stones. Revista de Gastroenterologνa de Mexico. 2014;79:22–27. doi: 10.1016/j.rgmx.2013.10.001. [DOI] [PubMed] [Google Scholar]; Cuendis-Velαzquez A, Rojano-Rodriguez ME, Morales- Chαvez CE, Gonzalez Angulo-Rocha A, Fernandez-Castro E, Aguirre-Olmedo I, et al. Intraoperative choledochoscopy usefulness in the treatment of difficult biliary stones. Revista de Gastroenterologνa de Mexico 2014; 79:22-27. [DOI] [PubMed]
- 91.Ford J.A., Soop M., Du J., Loveday B.P., Rodgers M. Systematic review of intraoperative cholangiography in cholecystectomy. Br. J. Surg. 2011;99:160–167. doi: 10.1002/bjs.7809. [DOI] [PubMed] [Google Scholar]; Ford JA, Soop M, Du J, Loveday BP, and Rodgers M: Systematic review of intraoperative cholangiography in cholecystectomy. Br J Surg 2011;99:160-167. [DOI] [PubMed]
- 92.Takada T., Yasuda H., Uchiyama K., Hasegawa H., Shikata J. Choledochoscopy during biliary surgery for reducing the risk of overlooked stones. Surg. Endosc. 1991;5:192–195. doi: 10.1007/BF02653262. [DOI] [PubMed] [Google Scholar]; Takada T, Yasuda H, Uchiyama K, Hasegawa H, and Shikata J. Choledochoscopy during biliary surgery for reducing the risk of overlooked stones. Surg Endosc 1991;5:192-195. [DOI] [PubMed]
- 93.Schwarz J., Simsa J., Pazdírek F. Our experience with preoperative choledochoscopy. Rozhl Chir. 2007;86:180–183. [PubMed] [Google Scholar]; Schwarz J, Simsa J, and Pazdirek F. Our experience with preoperative choledochoscopy. Rozhl Chir 2007;86:180-183. [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.