Abstract
Amiodarone has a well-established and extensive side effect profile: pulmonary fibrosis, thyroid toxicity, corneal deposits, and skin discoloration. However, in some rare instances epididymitis/orchitis is a side effect of amiodarone. Symptoms range from testicular pain to swelling and erythema.1,2 The mechanism of how this toxicity occurs is unknown. In this case report, we will discuss the case of an elderly patient who developed epididymitis and orchitis after several years of tolerating amiodarone without any adverse events. Our patient underwent a full workup with testicular ultrasound, evaluation by the urology and cardiology services. His amiodarone was discontinued with complete resolution of symptoms.
Data sources
A community hospital in Stratford, NJ.
Study selection
88 year old male patient with multiple comorbidities.
Data extraction
Obtaining medical records on Soarian Cerner system.
Data synthesis
Article analysis obtained from PubMed.
Introduction
There are several causes for orchitis and epididymitis: sexually transmitted infections (STIs), trauma, chemical with backflow of urine, Tuberculosis, and vasculitic diseases such as Behcet's disease. Orchitis and epididymitis due to amiodarone can also present with a spectrum of clinical presentations. Chronic epididymyalgia in the absence of fever and leukocytosis is the chief symptom of this clinical entity.1 Non-infectious epididymitis must be diagnosed with a careful medical history to prevent unnecessary antibiotic usage.1 The purpose of this case report is to show early and clear identification of the toxicity and follow its management.
Case report
An 88-year-old white male presented to the emergency department at our institution with new-onset testicular pain and swelling. He had a past medical history of hypothyroidism, hypertension, sick sinus syndrome with pacemaker, paroxysmal atrial fibrillation, prostate cancer, and neurogenic bladder. He was on amiodarone 100 mg once a day since 2012. Prior to this admission, the patient had been hospitalized recently for right thigh, hip, and back pain. He was discharged to subacute rehabilitation where he started having generalized weakness followed by 3 weeks of progressive testicular pain and swelling. However, he did not having any difficulty urinating, frequency, urgency, fevers, chills, dysuria, hematuria, urinary incontinence or retention. After being discharged home, he experienced a loss of appetite with a 10 pound weight loss over 2 months, dizziness and lightheadedness. When he saw his primary care physician, it was recommended that he undergo a testicular ultrasound with evaluation at our hospital. His vital signs were the following: blood pressure 165/77, pulse of 80, respiratory rate of 18, temperature 97.3, and SpO2 100% on room air.
On physical exam, he had testicular swelling with erythema bilaterally. The testes were tender to palpation, and descended bilaterally without palpable lesions or masses. The left testicle was grossly enlarged and firmer than the right testicle. Digital rectal examination showed a firm, smooth grade 2 in size prostate without any palpable nodules.
His urinalysis showed nitrates with few bacteria and 2–3 WBC, negative for any signs of infection. Urine culture was positive for Escherichia coli with <10,000 colonies.
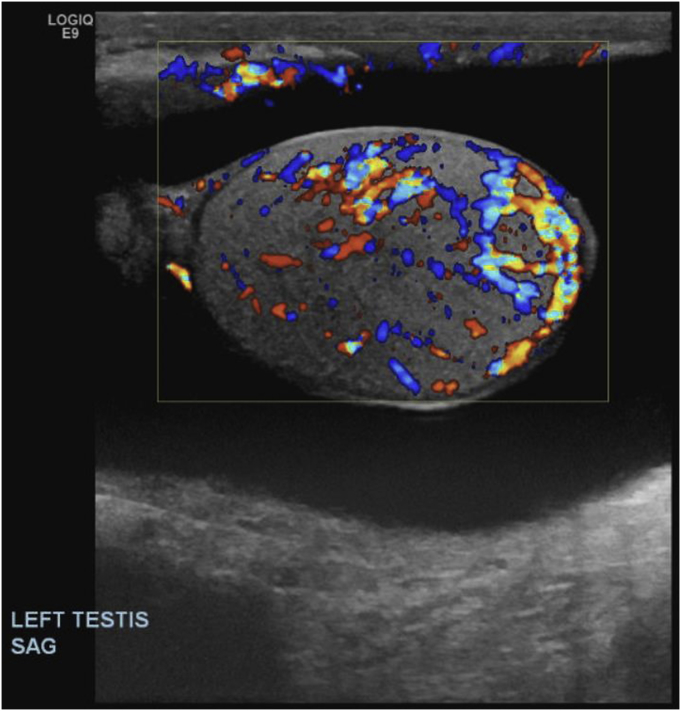
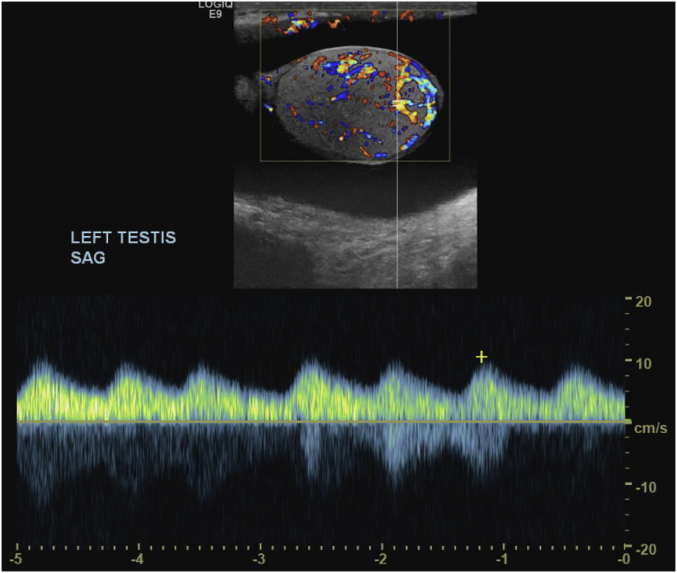
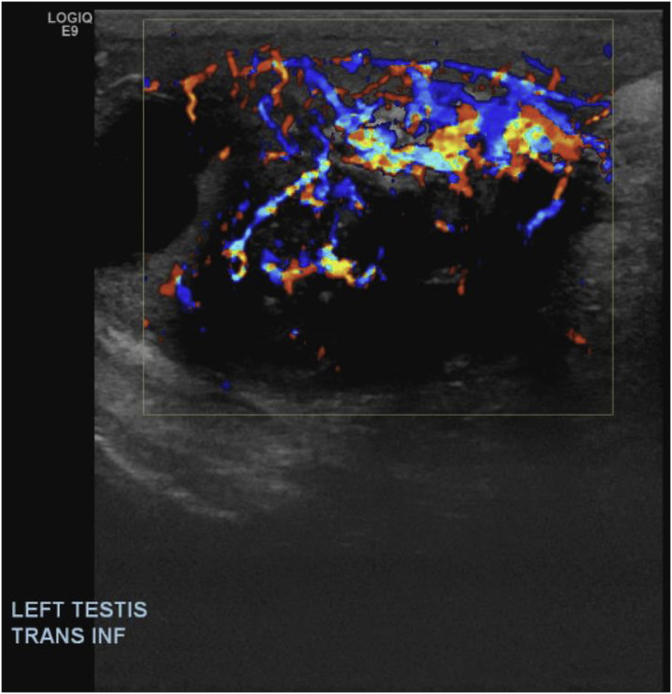
Doppler testicular ultrasound illustrated bilateral hydroceles, left greater than right with hyperemia of left testis and Epididymo-Orchitis (seen in Fig. 1, Fig. 2, Fig. 3). Renal ultrasound did not show acute findings.
Fig. 1.
Doppler Testicular Ultrasound of Left Testes demonstrating hyperemia and Epididymo-Orchitis.
Fig. 2.
Doppler Testicular Ultrasound of Left Testes demonstrating hyperemia and Epididymo-Orchitis.
Fig. 3.
Doppler Testicular Ultrasound of Left Testes demonstrating hyperemia and Epididymo-Orchitis.
He was initially treated with levaquin 750 mg IV. After being examined by the urology service, he was switched from levaquin to ceftriaxone for treatment and amiodarone was stopped. The cardiology service agreed with cessation of amiodarone and recommended addition of diltiazem for rate control. On the medical floor, he was found to have a post void residual over 700 cc and was experiencing discomfort. At that time he was noted to have an elevated creatinine. Attempts to place both a Foley catheter and coude catheter were unsuccessful, thus the urology service performed a bedside cystoscopy on which a dense stricture in his bulbar/membranous urethra was visualized. The urethra was subsequently dilated and an 18-French Council tip foley catheter was placed. Following this procedure, his bladder started draining clear amber urine. After two days of hospitalization and treatment, his testicular swelling started to decrease and his testicular pain began to improve. The remainder of the hospital course was unremarkable. He stopped taking his amiodarone outpatient as well.
Discussion
Amiodarone is an iodinated benzofuran derivative with class I, II, III and IV antiarrhythmic properties that was initially used as an antianginal agent. Unfortunately, amiodarone has many adverse effects. Common side effects include pulmonary, gastrointestinal, thyroid, skin and central nervous system manifestations. Genitourinary manifestations such as epididymitis and erectile dysfunction have an incidence of <1%.2 Risk factors for genitourinary complications include duration of administration (7–15 months), dose (usually >700 mg/day) and blood concentration.3 Our patient was taking 100 mg of amiodarone daily since 2012.
Causes of epididymitis include post obstructive pathology, post-traumatic, Behcet's disease, Mycobacterium tuberculosis, sexually transmitted infections, gram-negative bacterium, and drug induced.1 Amiodarone usually causes bilateral testicular involvement and chronic epididymyalgia, in the absence of lever and leukocytosis, which was seen in our patient.
After withdrawal of the drug, our patient clinically improved which is consistent with the observation that reducing or withdrawing the drug could alleviate epididymitis.1,4 The pathogenesis of amiodarone induced epididymitis is unknown. Concentrations of amiodarone and its metabolite desethylamiodarone in the testicular tissue can be > 25,000 times higher than in the plasma.3 Our patient was experiencing testicular swelling for weeks. Infectious etiology of the epididymo-orchitis was ruled out because our patient did not have a urinary tract infection: as it is a clinical diagnosis and he was not experiencing symptoms such as fevers, chills frequency, urgency or dysuria. His urine sample was not completely “sterile,” but there was no evidence of infection. His urine culture was “positive” for E. coli, with <10,000 CFU, but >100,000 colonies are required for a clinically relative diagnosis and to be certain this is not contamination, which led us to believe that it is more likely that his symptoms were secondary to amiodarone. Furthermore, the patient had a urethral stricture seen on cystoscopy and a foley catheter was placed for acute urinary retention >500 cc. While the stricture could have contributed to the diagnosis, patients with strictures usually present with lower urinary tract symptoms (LUTS), 54% of patients have progressive LUTS as their presenting complaint and 93% of patients have LUTS as part of their symptom complex,5 which our patient denied having. This patient also underwent radiation to his prostate in 2013, but the epididymo-orchitis was not likely from radiation because side effects from radiation are rare after two months post treatment.
Conclusion
This is not the first occurrence of amiodarone induced epididymitis and orchitis, however, the prognosis, presentation, and findings seen on testicular ultrasound can vary. Although supportive care is the mainstream treatment, patients can face permanent testicular damage. This case depicts why it is important to recognize a rare side effect of amiodarone early, and to discontinue the drug as soon as possible.
Conflicts of interest
None.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.eucr.2019.100929.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Cicek T., Cicek Demir C., Coban G., Coner A. Amiodarone induced epididymitis: a case report. Iran Red Crescent Med J. 2014;16(1) doi: 10.5812/ircmj.13929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Goldschlager N., Epstein A.E., Naccarelli G.V. A practical guide for clinicians who treat patients with amiodarone: 2007. Practice Guidelines Sub-committee. North American Society of Pacing and Electrophysiology (HRS) Heart Rhythm. 2007;4(9):1250. doi: 10.1016/j.hrthm.2007.07.020. Epub 2007 Jul 20. [DOI] [PubMed] [Google Scholar]
- 3.Shen Yi. Karger Publishers; 18 June 2014. Amiodarone-Induced Epididymitis: A Pathologically Confirmed Case Report and Review of the Literature.www.karger.com/Article/Abstract/361038 [DOI] [PubMed] [Google Scholar]
- 4.Nikolaou M., Ikonomidis I., Lekakis I., Tsiodras S., Kremastinos D. Amiodarone-induced epididymitis: A case report and review of the literature. International Journal of Cardiology. 2007;121(1) doi: 10.1016/j.ijcard.2007.05.079. [DOI] [PubMed] [Google Scholar]
- 5.Rourke Clinical spectrum of presenting signs and symptoms of anterior urethral stricture: detailed analysis of single-institutional cohort. Urology. 2012;79:1163–1167. doi: 10.1016/j.urology.2012.01.044. https://www-sciencedirect-com.ezproxy.rowan.edu/science/article/pii/S009042951201018 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.