Abstract
An ideal implantation of artificial cervical disc replacement (ACDR) prosthesis should preserve the cervical biomechanics and maintain normal cervical biomechanics. In this study, we designed a novel prosthesis based on the physiological curvature of the cervical endplate, and conducted an in vitro test with cadaveric cervical specimens to study its effect on cervical range of motion (ROM) and facet contact force. Eighteen cadaveric cervical specimens (C2-C7) were evaluated with a 50 N follower load and a moment of ± 2.0 N-m. Testing conditions were as follows: control (group 1), C5-C6 ACDR with a novel prosthesis (group 2), C5-C6 ACDR with the Prestige LP prosthesis (group 3) and C5-C6 cervical discectomy and fusion (ACDF) with cage internal fixation (group 4). The range of motion (ROM) of all segments and facet joint contact force were measured and analyzed. The results showed that there was no significant difference among the group 1, 2 and 3 in terms of ROM (P>0.05). The ROM of C5-C6 in the group 4 showed a significant decrease compared with the group 1, 2, and 3 (P<0.05). The group 2 had a similar facet joint force with the group 1, and there is no statistical difference among the group 1, 2 and 3 (P>0.05). The facet joint force of C5-C6 in the group 4 reduced significantly compared with the other groups (P<0.05). In conclusion, both novel cervical prosthesis and Prestige LP could better preserve the normal cervical ROM and maintain facet joint force than ACDF.
Keywords: Biomechanics, facet contact force, disc prosthesis, range of motion
Introduction
Artificial cervical disc replacement (ACDR) has been extensively used for treating cervical spondylosis in the recent years. Compared with anterior cervical discectomy and fusion (ACDF), it has advantages like maintaining cervical biomechanics like range of motion (ROM), intradiscal pressure and facet joint contact pressure [1-4] while achieving spinal cord decompression. However, there are also some studies suggesting that ACDR could cause complications like subsidence, dislocation, heterotopic ossification, etc. [5-8]. Ideally, the implantation of the ACDR prosthesis should preserve the cervical biomechanics to reduce these complications, and to maintain normal cervical biomechanics are the objective of prosthesis design.
Most of the current available cervical disc prostheses present a flat surface. For example, the Prestige LP prostheses (Medtronic Sofamor Danek Inc, MN, USA) have a ball-in-trough articulation, which allows unconstrained motion similar to the normal physiologic motion at the treated level and adjacent levels, they have achieved good clinical outcomes and have been applied around the world [9,10]. As the morphology of endplates of the cervical spine is convex [11], the prostheses with flat surface could cause mismatch and consequent uneven load distribution on their interface, which could be an important cause of complications [12]. Due to this reason, careful preparation of the endplate of cervical vertebra during operation is required to match the prosthesis with flat surface. In this case, a design of prostheses with convex surface could better match the physiological curvature of the endplate. And hence we designed a novel artificial disc prosthesis based on the physiological convex of cervical endplate, with the advantage of maintaining the integrity of the vertebral endplate and increasing the contact area between the prosthesis and endplate.
To date, many studies have defined the effects of ACDR on the mechanics at the cervical ROM and intradiscal pressure [9,13-15], and few have investigated the effects of ACDR on the facet joints [16-18]. As facet joints are important for the mechanical transmission and three-dimensional motion of the spine, facet contact force is an important index for biomechanical study. In the current study, we tested a novel cervical disc prosthesis in vitro with cadaveric cervical specimens and mainly focused on its effect on the cervical ROM and facet contact force.
Materials and methods
Device design
The novel prosthesis has the ball in socket joint design similar to the Prestige LP prosthesis. The superior and inferior plates are convex shaped with a porous Ti6Al4V structure, which can better match the vertebral endplate anatomy and enlarge the contact area. There are three dentate crests on each plate to improve the initial stability of the prosthesis and avoid implant migration. Porous structure could allow bone ingrowth to the plates (Figure 1).
Figure 1.
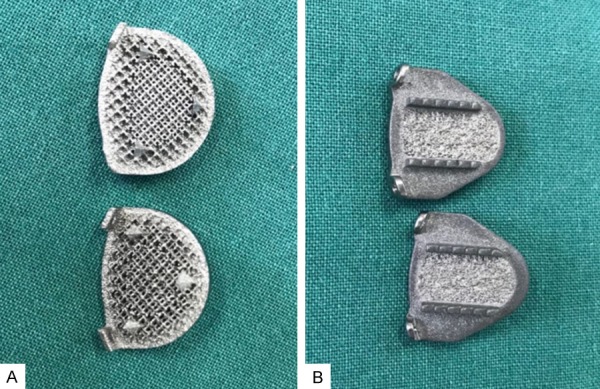
The novel prosthesis (A) and Prestige LP prosthesis (B). The novel prosthesis has convex shaped porous Ti6Al4V structure endplate.
Specimen preparation
Eighteen fresh-frozen human cadaveric cervical spines (C2-T1) were used in the biomechanical test. Radiographs were taken first to exclude flaws like cervical trauma, deformity, obvious degeneration, and osteoporosis, etc. The specimens were kept at -20°C in double-sealed bags, and they were thawed to room temperature 10-16 hours before preparation. Muscular and fascia tissues were removed, and vertebra, intervertebral disc, ligament and facet capsules were entirely preserved. The proximal (C2) and distal (T1) ends of the specimen were embedded in polymethylmethacrylate for stabilization.
Firstly, 6 of the 18 specimens were randomly chosen as group 1 to test the ROM and facet contact force in the intact condition, the the 18 specimens were divided into group 2, 3 and 4 with 6 specimens per group. The specimens in the group 2 were implanted with the novel prosthesis, the specimens in the group 3 were implanted with the Prestige LP prosthesis, and the specimens in the group 4 were treated with cage internal fixation (Figure 2). The prosthesis (novel prosthesis, Prestige LP prosthesis and cage) height chosen was based on the anatomy of each specimen, and 5-mm, 6-mm, and 7-mm-height prostheses were used in different specimens. The complete disc discectomy of C5-C6 was performed as described by Lou et al. [15], and this segment is where prosthesis implantation most frequently performed [18]. Final position of implantation in the C5-C6 disc space was checked using lateral fluoroscopy (Figure 3).
Figure 2.
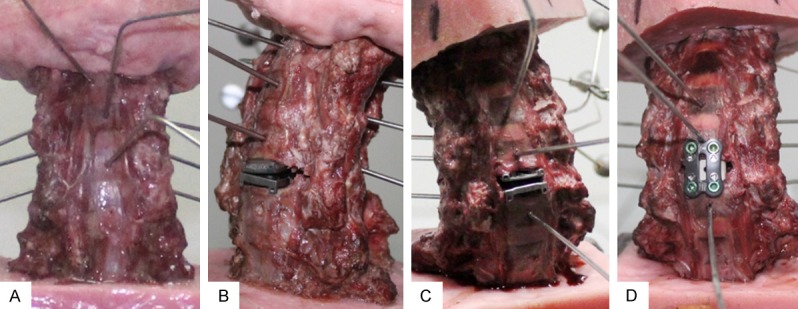
The specimens in the different conditions, wires with tracking marker can be seen within the vertebral bodies. (A) intact, (B) C5-C6 ACDR with novel prosthesis, (C) C5-C6 ACDR with Prestige LP prosthesis, (D) C5-C6 ACDF with cage and fixation.
Figure 3.
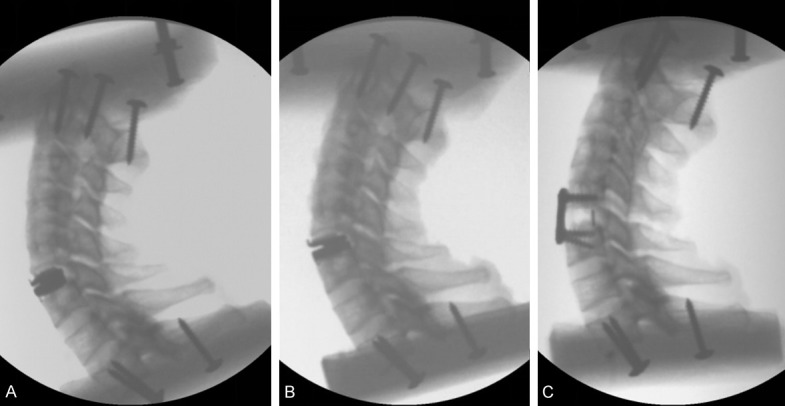
Radiographs of different implanted specimens. (A) C5-C6 ACDR with novel prosthesis, (B) C5-C6 ACDR with Prestige LP prosthesis, (C) C5-C6 ACDF with cage and fixation.
Three-dimensional motion testing
Three-dimensional motion testing was conducted with an optical tracking system (Motion Analysis Co., USA). Kirschner wires with a diameter of 2 mm were inserted into the vertebral body, bilateral transverse process and spinous process of each vertebral body of the specimen, with a non-collinear optical marker connecting to the end, and it could be detected by the optical tracking system. Three-dimensional motion testing was performed by applying an axial preload of 50 N to the C2 vertebra to simulate head weight, and a pure moment of ± 2.0 N-m was applied to simulate flexion-extension (FE), lateral bending (LB) and axial rotation (AR), the data of the third cycle were used for analysis [9,19,20]. During the biomechanical tests, all specimens were moistened with normal saline to prevent desiccation.
Facet contact force
Facet contact force was tested with the pressure measuring sensors (Tekscan, Inc., USA). After resecting the left joint capsule of C4-C5, C5-C6 and C6-C7 in all specimens, the sensors were placed into the facet joint (Figure 4). Facet joint maximum contact forces were recorded on the third cycle under 2.0 N-m load for each of the three primary bending directions (AR, LB, extension) [21]. During each test phase, a constant compression preload of 50 N was applied. Flexion was excluded from force analysis since it can unload cervical facet joints within physiological ROM [22]. The pressure data were constantly recorded on the computer.
Figure 4.
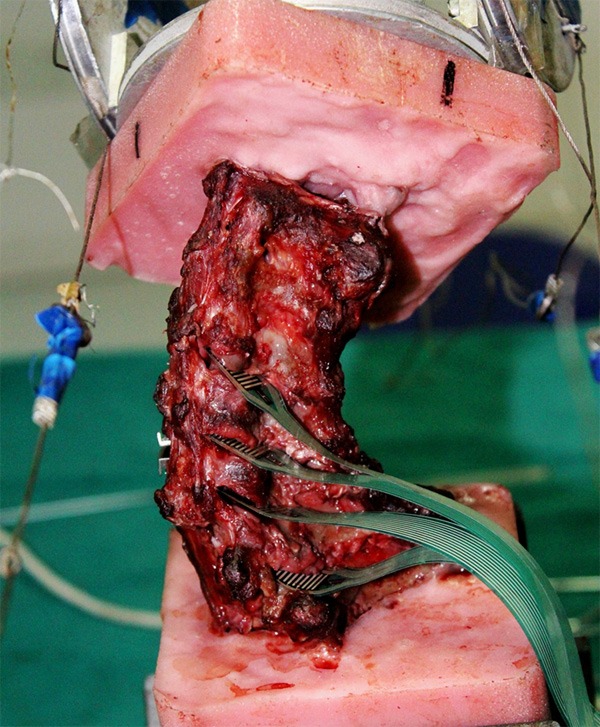
Pressure sensing transducers can be seen within the facet joints at the C3-C7 levels.
Statistical analysis
SPSS 19.0 software (SPSS Inc., Chicago, IL, USA) was used for statistical analysis. Mean values and standard deviations were determined for each parameter. One-way ANOVA was used to determine the statistical differences in groups. A value of P<0.05 was considered statistically significant.
Results
ROM
The ROMs in three motion directions were always recorded at the maximal loading of ± 2 Nm. Total ROM of flexion-extension was 42.83° ± 2.78° in the group 1, 42.96° ± 2.12° in the group 2, 43.34° ± 2.25° in the group 3 and 33.59° ± 2.11° in the group 4; for lateral bending, the ROM was 38.16° ± 2.89° in the group 1, 39.64° ± 2.28° in the group 2, 40.57° ± 2.15° in the group 3 and 33.3° ± 2.08° in the group 4; for axial rotation, the ROM was 36.76° ± 2.14° in the group 1, 38.15° ± 2.22° in the group 2, 39.73° ± 2.43° in the group 3 and 32.69° ± 2.35° in the group 4. There was no statistical difference in terms of the ROM among different directions within the group 1, 2 and 3 (P>0.05), but there was a significant decrease in the group 4 (P<0.05). The ROMs of each segment in the 4 groups were listed in Table 1. The ROMs of each segment among the group 1, 2 and 3 showed no statistical difference (P>0.05). And the ROMs of C5-C6 in the group 4 were significantly lower than those in the group 1, 2 and 3 (P<0.05).
Table 1.
The segment ROM in flexion, extension, lateral bending and axial rotation
| Group | Segment | Flexion | Extension | Left lateral bending | Right lateral bending | Left axial rotation | Right axial rotation |
|---|---|---|---|---|---|---|---|
| Group 1 | C4-C5 | 6.59 | 4.7 | 4.7 | 5.43 | 6.1 | 6.32 |
| C5-C6 | 5.44 | 4.66 | 4.68 | 4.13 | 5.64 | 7.16 | |
| C6-C7 | 6.01 | 5.53 | 5.43 | 4.46 | 5.32 | 6.22 | |
| Group 2 | C4-C5 | 6.65 | 4.51 | 5.16 | 5.53 | 6.58 | 8.01 |
| C5-C6 | 5.8 | 5.22 | 5.25 | 5.09 | 5.83 | 7.01 | |
| C6-C7 | 5.91 | 5.07 | 5.16 | 4.33 | 5.38 | 6.06 | |
| Group 3 | C4-C5 | 6.66 | 4.52 | 5.18 | 5.53 | 6.59 | 8.01 |
| C5-C6 | 6.02 | 5.44 | 5.46 | 5.32 | 6.04 | 7.26 | |
| C6-C7 | 6.12 | 5.28 | 5.36 | 4.47 | 5.59 | 6.27 | |
| Group 4 | C4-C5 | 6.31 | 4.9 | 5.54 | 5.76 | 7.7 | 8.52 |
| C5-C6 | 1.52* | 1.21* | 1.72* | 0.99* | 1.29* | 1.76* | |
| C6-C7 | 6.06 | 4.49 | 5.51 | 4.67 | 6.25 | 7.17 |
Compare with other groups;
P<0.05.
Facet joint contact force
During flexion, right bending and left rotation, the facet joints dissociate and the pressure is taken as 0N, while the maximal facet joint force during extension, left bending and right rotation in the four groups were recorded (Figure 5). The group 2 showed a similar facet joint force with the group 1, and there was no statistical difference among the group 1, 2 and 3. In the group 4, the maximal facet joint force at C5-C6 segment in extension, left bending and right rotation was 6.9 N, 13.4 N and 5.9 N, respectively, significantly lower than the other groups (P<0.05). And the group 2 had a similar facet joint force with the group 1.
Figure 5.
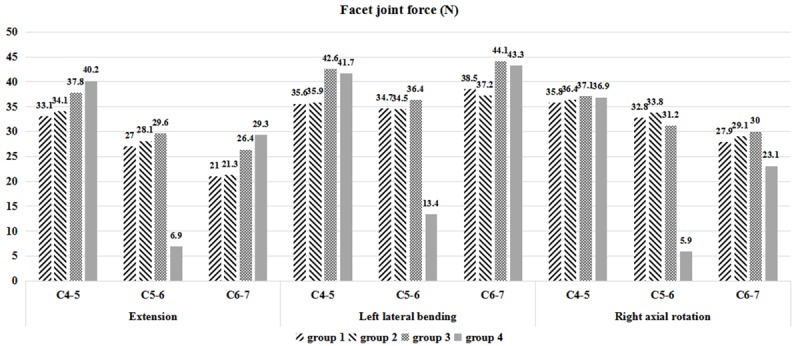
The facet joint contact force at C4-C5, C5-C6, C6-C7 segments in different groups.
Discussion
ACDR has become a successful surgery method for cervical spondylosis, as it can better preserve the cervical biomechanics. So far, there are a number of artificial cervical disc prostheses for clinical use. Due to the different designs and structures of the prostheses, complications like adjacent segment degeneration and prosthesis subsidence have been reported [5-8,23], suggesting that ACDR also had the problem of biomechanical mismatch. In this situation, we designed a novel artificial cervical disc prosthesis. After being implanted into the human spinal specimens, we tested the ROM and facet joint contact force on adjacent segments to assess the biomechanical function of this novel prosthesis.
To preserve the normal ROM of the surgical segment is the key to maintaining cervical biomechanics for ACDR. There are still controversies using displacement controlled versus load-controlled protocol during the cervical ROM test in vitro [24]. The load-control testing mode may appear more physiologically representative as the weight of the head and muscle forces in the neck presumably do not change before and after surgery [9,15]. Hence, in the current study, we used load-controlled protocol for biomechanical tests. We adopted a 50 N follower load to increase clinical practicability, and applied a moment loading of 2 N-m to simulate the physiological ROM [21,25].
The Prestige LP prosthesis could well preserve the ROM of the surgical segment and adjacent segments [10]. Similarly, our in vitro study found no statistical difference in flexion-extension, lateral bending and axial rotation among C4-C5, C5-C6 and C6-C7 segments between the two ACDR prostheses, which could be explained by the similar joint structure of the two prostheses. Compared with the group 1, the two ACDR groups (group 2 and 3) slightly increased in C5-C6 segment, while the ROMs of the adjacent segments of C4-C5 and C6-C7 did not change significantly, which indirectly indicated that the incidence of adjacent segment disease might be reduced after ACDR. In group 4, the ROM in each direction showed significant decrease while that in the adjacent segments showed slight increase with no statistical difference. After ACDF, there would be a compensatory increase in the ROM of the adjacent segments, which could be one of the causes of accelerating degeneration of the adjacent segments. While Rao et al. found no significant increase in the ROM of the adjacent segments after ACDF, and they suggested that degeneration of the adjacent segment would be a natural course of cervical spondylosis [26].
Cervical facet joint constitutes the spinal canal and the posterior wall of intervertebral foramina. The spinal cord and nerves could be compressed due to facet joint degeneration and cause neurologic symptoms. In addition to participating in cervical motor function, facet joints also bear nearly 30% of the load of cervical vertebra [27]. The facet joint maintains cervical stability by resisting compression and axial shear. Abnormal changes in facet joint pressure can lead to facet joint degeneration, pain and neurological symptoms. Destruction of the facet joint could also increase the stress in annulus fibrosus and cervical ROM [28]. In the current study, we directly measured the facet joint force by placing the Tekscan pressure sensor into the facet joint and the computer could record the stress distribution, which is more direct and accurate than other methods to measure the facet joint force. We only placed the pressure sensor unilaterally, which could avoid the problem of disturbed stability due to bilateral facet capsule incision. We found that after C5-C6 ACDR, the ROM of the surgical segment was preserved, and the facet joint force change in every direction showed no statistical difference among the novel prosthesis group, the Prestige LP group and the control group. But a marked decrease in the facet joint force change in flexion, left bending and right rotation could be observed in the cage internal fixation group compared with the other three groups (P<0.05). Some studies suggest that abnormal decrease in the facet joint force could also accelerate the facet joint degeneration, as it could cause enlargement of the facet capsule and hence the facet joint and the surrounding tissue could be more vulnerable [28]. Compared with ACDF, our novel prosthesis and the Prestige LP could better maintain the fact joint force and delay the facet joint degeneration, and the novel prosthesis showed more similar stress with the intact group. Consistently, in vitro studies on the biomechanics of ACDR also suggested that ACDR could maintain the normal force of the facet joint [17,29].
There are some limitations in the current study. As the measurement of the facet joint force requires incision of the facet joint capsule, it could destroy the integrity of the cervical spine and cause changes in the cervical ROM and facet joint force. And the intradiscal pressure needs to be tested in the future. As the human spinal specimens are difficult to obtain, we only applied a limited number of samples, and studies with larger sample sizes and clinical studies would be necessary.
In conclusion, this in vitro study suggested that both novel cervical prosthesis and Prestige LP could preserve the normal cervical ROM and facet joint force than ACDF.
Acknowledgements
This work was supported partially by the National Key Research and Development Program of China (No. 2017YFC1104903), Liaoning Science and Technology Project (No. 2015225014) and Liaoning Natural Science Foundation (No. 20180550926).
Disclosure of conflict of interest
None.
References
- 1.Cason GW, Herkowitz HN. Cervical intervertebral disc replacement. J Bone Joint Surg Am. 2013;95:279–285. doi: 10.2106/JBJS.J.01042. [DOI] [PubMed] [Google Scholar]
- 2.Pandey PK, Pawar I, Gupta J, Verma RR. Comparison of outcomes of single-level anterior cervical discectomy with fusion and single-level artificial cervical disc replacement for single-level cervical degenerative disc disease. Spine (Phila Pa 1976) 2017;42:E41–E49. doi: 10.1097/BRS.0000000000001696. [DOI] [PubMed] [Google Scholar]
- 3.Gornet MF, Lanman TH, Burkus JK, Hodges SD, McConnell JR, Dryer RF, Copay AG, Nian H, Harrell FE Jr. Cervical disc arthroplasty with the Prestige LP disc versus anterior cervical discectomy and fusion, at 2 levels: results of a prospective, multicenter randomized controlled clinical trial at 24 months. J Neurosurg Spine. 2017;26:653–667. doi: 10.3171/2016.10.SPINE16264. [DOI] [PubMed] [Google Scholar]
- 4.Burkus JK, Traynelis VC, Haid RW Jr, Mummaneni PV. Clinical and radiographic analysis of an artificial cervical disc: 7-year follow-up from the prestige prospective randomized controlled clinical trial: clinical article. J Neurosurg Spine. 2014;21:516–528. doi: 10.3171/2014.6.SPINE13996. [DOI] [PubMed] [Google Scholar]
- 5.Hacker FM, Babcock RM, Hacker RJ. Very late complications of cervical arthroplasty results of 2 controlled randomized prospective studies from a single investigator site. Spine. 2013;38:2223–2226. doi: 10.1097/BRS.0000000000000060. [DOI] [PubMed] [Google Scholar]
- 6.Pickett GE, Sekhon LH, Sears WR, Duggal N. Complications with cervical arthroplasty. J Neurosurg Spine. 2006;4:98–105. doi: 10.3171/spi.2006.4.2.98. [DOI] [PubMed] [Google Scholar]
- 7.van der Houwen EB, Baron P, Veldhuizen AG, Burgerhof JG, van Ooijen PM, Verkerke GJ. Geometry of the intervertebral volume and vertebral endplates of the human spine. Ann Biomed Eng. 2010;38:33–40. doi: 10.1007/s10439-009-9827-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Penzkofer R, Hofberger S, Spiegl U, Schilling C, Schultz R, Augat P, Gonschorek O. Biomechanical comparison of the end plate design of three vertebral body replacement systems. Arch Orthop Trauma Surg. 2011;131:1253–9. doi: 10.1007/s00402-011-1284-7. [DOI] [PubMed] [Google Scholar]
- 9.Yu CC, Hao DJ, Huang DG, Qian LX, Feng H, Li HK, Zhao SC. Biomechanical analysis of a novel prosthesis based on the physiological curvature of endplate for cervical disc replacement. PLoS One. 2016;11:e0158234. doi: 10.1371/journal.pone.0158234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Peng CW, Yue WM, Basit A, Guo CM, Tow BP, Chen JL, Nidu M, Yeo W, Tan SB. Intermediate results of the prestige LP cervical disc replacement: clinical and radiological analysis with minimum two-year follow-up. Spine (Phila Pa 1976) 2011;36:E105–111. doi: 10.1097/BRS.0b013e3181d76f99. [DOI] [PubMed] [Google Scholar]
- 11.Lou J, Liu H, Rong X, Li H, Wang B, Gong Q. Geometry of inferior endplates of the cervical spine. Clin Neurol Neurosurg. 2016;142:132–136. doi: 10.1016/j.clineuro.2016.01.027. [DOI] [PubMed] [Google Scholar]
- 12.Muller-Gerbl M, Weisser S, Linsenmeier U. The distribution of mineral density in the cervical vertebral endplates. Eur Spine J. 2008;17:432–438. doi: 10.1007/s00586-008-0601-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cunningham BW, Hu N, Zorn CM, McAfee PC. Biomechanical comparison of single- and two-level cervical arthroplasty versus arthrodesis: effect on adjacent-level spinal kinematics. Spine J. 2010;10:341–349. doi: 10.1016/j.spinee.2010.01.006. [DOI] [PubMed] [Google Scholar]
- 14.Demetropoulos CK, Sengupta DK, Knaub MA, Wiater BP, Abjornson C, Truumees E, Herkowitz HN. Biomechanical evaluation of the kinematics of the cadaver lumbar spine following disc replacement with the ProDisc-L prosthesis. Spine (Phila Pa 1976) 2010;35:26–31. doi: 10.1097/BRS.0b013e3181c4eb9a. [DOI] [PubMed] [Google Scholar]
- 15.Lou J, Li Y, Wang B, Meng Y, Gong Q, Liu H. Biomechanical evaluation of cervical disc replacement with a novel prosthesis based on the physiological curvature of endplate. J Orthop Surg Res. 2018;13:41. doi: 10.1186/s13018-018-0748-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zander T, Rohlmann A, Bergmann G. Influence of different artificial disc kinematics on spine biomechanics. Clin Biomech. 2009;24:135–142. doi: 10.1016/j.clinbiomech.2008.11.008. [DOI] [PubMed] [Google Scholar]
- 17.Jaumard NV, Bauman JA, Guarino BB, Gokhale AJ, Lipschutz DE, Weisshaar CL, Welch WC, Winkelstein BA. ProDisc cervical arthroplasty does not alter facet joint contact pressure during lateral bending or axial torsion. Spine. 2013;38:E84–E93. doi: 10.1097/BRS.0b013e31827b8a2d. [DOI] [PubMed] [Google Scholar]
- 18.Yuan W, Zhang H, Zhou X, Wu W, Zhu Y. The influence of artificial cervical disc prosthesis height on the cervical biomechanics: a finite element study. World Neurosurg. 2018;113:e490–e498. doi: 10.1016/j.wneu.2018.02.062. [DOI] [PubMed] [Google Scholar]
- 19.Wilke HJ, Wenger K, Claes L. Testing criteria for spinal implants: recommendations for the standardization of in vitro stability testing of spinal implants. Eur Spine J. 1998;7:148–154. doi: 10.1007/s005860050045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yu CC, Hao DJ, Ma YL, Huang DG, Li HK, Feng H, Hou Q. The role of posterior longitudinal ligament in cervical disc replacement: an ovine cadaveric biomechanical analysis. Med Sci Monit. 2016;22:1843–1849. doi: 10.12659/MSM.899138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Patel VV, Wuthrich ZR, McGilvray KC, Lafleur MC, Lindley EM, Sun D, Puttlitz CM. Cervical facet force analysis after disc replacement versus fusion. Clin Biomech (Bristol, Avon) 2017;44:52–58. doi: 10.1016/j.clinbiomech.2017.03.007. [DOI] [PubMed] [Google Scholar]
- 22.Chang UK, Kim DH, Lee MC, Willenberg R, Kim SH, Lim J. Changes in adjacent-level disc pressure and facet joint force after cervical arthroplasty compared with cervical discectomy and fusion. J Neurosurg Spine. 2007;7:33–39. doi: 10.3171/SPI-07/07/033. [DOI] [PubMed] [Google Scholar]
- 23.Verma K, Gandhi SD, Maltenfort M, Albert TJ, Hilibrand AS, Vaccaro AR, Radcliff KE. Rate of adjacent segment disease in cervical disc arthroplasty versus single-level fusion: meta-analysis of prospective studies. Spine (Phila Pa 1976) 2013;38:2253–2257. doi: 10.1097/BRS.0000000000000052. [DOI] [PubMed] [Google Scholar]
- 24.Barrey C, Campana S, Persohn S, Perrin G, Skalli W. Cervical disc prosthesis versus arthrodesis using one-level, hybrid and two-level constructs: an in vitro investigation. Eur Spine J. 2012;21:432–442. doi: 10.1007/s00586-011-1974-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Miura T, Panjabi MM, Cripton PA. A method to simulate in vivo cervical spine kinematics using in vitro compressive preload. Spine. 2002;27:43–48. doi: 10.1097/00007632-200201010-00011. [DOI] [PubMed] [Google Scholar]
- 26.Rao RD, Wang M, McGrady LM, Perlewitz TJ, David KS. Does anterior plating of the cervical spine predispose to adjacent segment changes? Spine. 2005;30:2788–2792. doi: 10.1097/01.brs.0000190453.46472.08. [DOI] [PubMed] [Google Scholar]
- 27.Pal GP, Sherk HH. The vertical stability of the cervical spine. Spine (Phila Pa 1976) 1988;13:447–449. doi: 10.1097/00007632-198805000-00001. [DOI] [PubMed] [Google Scholar]
- 28.Zdeblick TA, Abitbol JJ, Kunz DN, McCabe RP, Garfin S. Cervical stability after sequential capsule resection. Spine (Phila Pa 1976) 1993;18:2005–2008. doi: 10.1097/00007632-199310001-00013. [DOI] [PubMed] [Google Scholar]
- 29.Stieber JR, Quirno M, Kang M, Valdevit A, Errico TJ. The facet joint loading profile of a cervical intervertebral disc replacement incorporating a novel saddle-shaped articulation. J Spinal Disord Tech. 2011;24:432–6. doi: 10.1097/BSD.0b013e3182027297. [DOI] [PubMed] [Google Scholar]


