Bevacizumab (BEV) is effective in reducing tumor volume and improving hearing in a subset of neurofibromatosis type 2 (NF2) patients with vestibular schwannoma (VS). Recent prospective clinical trial data demonstrated imaging and hearing response rates of 57% and 36%, respectively, in NF2-related VS patients,1 and therapeutic benefit is not maintained after discontinuation of drug. It is not currently known whether sporadic VS may also respond to bevacizumab.
We report sustained treatment response to low-dose bevacizumab in an adult female patient with progressive sporadic VS. She was diagnosed at age 47 years when a brain MRI obtained after a fall disclosed a right cerebellopontine angle tumor consistent with a VS. Her past medical history is relevant for deafness in the left ear since early childhood, presumably due to mumps and/or administration of ototoxic antibiotics. Imaging surveillance revealed slow continued progression of the VS, and she subsequently developed progressive hydrocephalus requiring placement of a ventriculo-peritoneal shunt. She declined surgery or radiation therapy for treatment of her progressive VS due to concern for the risk of hearing loss in her remaining ear. After informed consent, she began treatment with off-label BEV at a dose of 10 mg/kg every 2 weeks.
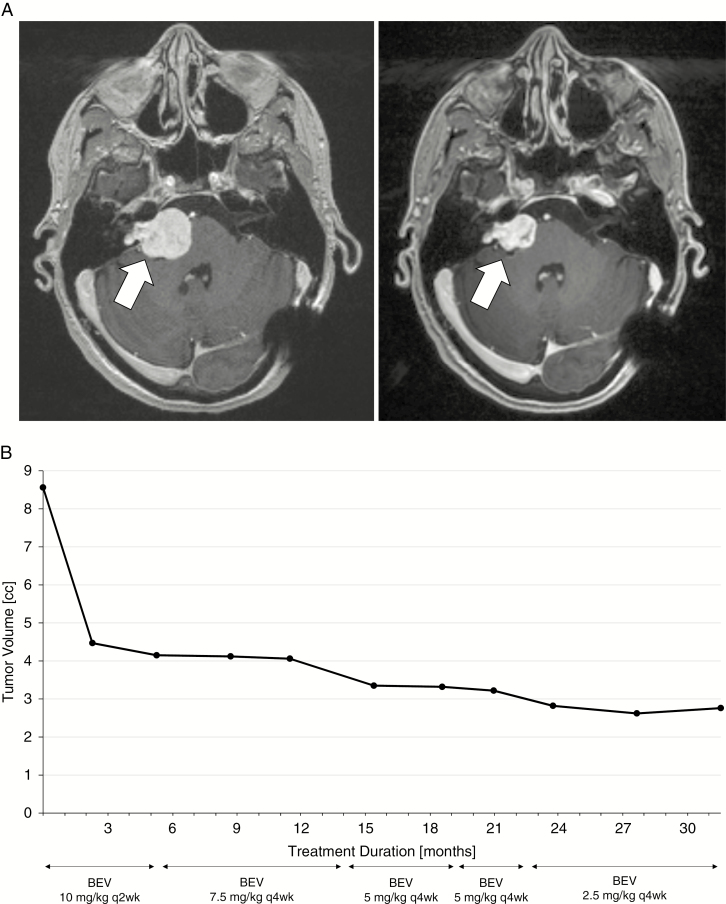
Response assessments included MRIs of the brain with tumor volumetrics as previously described,2 as well as audiograms. At pretreatment baseline, tumor volume was 8.56 cc, with normal hearing in the right ear. She had an excellent imaging response to therapy, which was maintained with stepwise reduction of BEV to a low dose of 2.5 mg/kg every 4 weeks to limit the risk of toxicity3 (Fig. 1). She tolerated therapy well, with no BEV-related toxicity such as hypertension or proteinuria. Most recent tumor volume measured 2.76 cc, which represents a 67.8% shrinkage from pretreatment baseline. She currently continues on therapy for 33+ months, with no evidence of any BEV-related toxicity, and maintaining normal hearing in the right ear.
Fig. 1.
(A) T1-weighted post-contrast MRI showing VS (white arrow) at pretreatment baseline (left panel) and after 32 months on treatment with BEV (right panel). (B) VS tumor volume at baseline and after 32 months on treatment with BEV. Each dotted timepoint represents a tumor volume measurement by MRI volumetrics.
Mean apparent diffusional coefficient (ADC) calculated from diffusion-weighted imaging was 1267 mm2/s at baseline and declined to 1050 mm2/s after 2 months of treatment, corresponding to a 17.1% reduction. Elevated ADC values at baseline and reduction during therapy have previously been shown to be associated with imaging and hearing responses of NF2-related VS to bevacizumab.1,4
Based on our observation, we conclude that sporadic VS may be highly responsive to BEV. Therefore, BEV could represent a novel and effective treatment alternative to be considered for select patients with sporadic VS who may not be good candidates for standard therapy, including surgery or radiation therapy,5 weighing the associated short- and long-term risks as well as costs.6 Further, prospective clinical studies in this patient population appear warranted.
Funding
None.
Conflict of interest statement. No conflicts.
Authorship statement. Data collection, analysis and interpretation: M.A.K., M.H., M.S., S.H. Manuscript writing: M.A.K. Final approval of manuscript: M.A.K., M.H., M.S., S.H.
Acknowledgments
We thank Radiology Informatics and the MSKCC Advanced Imaging Lab (SAIL) for assistance with volumetric analysis.
References
- 1. Blakeley JO, Ye X, Duda DG, et al. Efficacy and biomarker study of bevacizumab for hearing loss resulting from neurofibromatosis type 2-associated vestibular schwannomas. J Clin Oncol. 2016;34(14):1669–1675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Karajannis MA, Legault G, Hagiwara M, et al. Phase II trial of lapatinib in adult and pediatric patients with neurofibromatosis type 2 and progressive vestibular schwannomas. Neuro Oncol. 2012;14(9):1163–1170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Morris KA, Golding JF, Blesing C, et al. ; UK NF2 research group Toxicity profile of bevacizumab in the UK Neurofibromatosis type 2 cohort. J Neurooncol. 2017;131(1):117–124. [DOI] [PubMed] [Google Scholar]
- 4. Li KL, Djoukhadar I, Zhu X, et al. Vascular biomarkers derived from dynamic contrast-enhanced MRI predict response of vestibular schwannoma to antiangiogenic therapy in type 2 neurofibromatosis. Neuro Oncol. 2016;18(2):275–282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Carlson ML, Link MJ, Wanna GB, Driscoll CL. Management of sporadic vestibular schwannoma. Otolaryngol Clin North Am. 2015;48(3):407–422. [DOI] [PubMed] [Google Scholar]
- 6. Schnurman Z, Golfinos JG, Epstein D, Friedmann DR, Roland JT, Kondziolka D. Comparing costs of microsurgical resection and stereotactic radiosurgery for vestibular schwannoma. J Neurosurg. 2018:1–10. doi:10.3171/2018.5.JNS18508. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]