Abstract
Background:
Prior research has revealed that cervical collars elevate intracranial pressure (ICP) in patients with traumatic brain injury. Two recent small studies evaluated the change in optic sheath nerve diameter (ONSD) measured by ultrasound as a proxy for ICP following cervical collar placement in healthy volunteers.
Objective:
We sought to validate the finding that ONSD measured by ultrasound increases after cervical collar placement within an independent data set.
Methods:
This was a prospective, crossover study involving volunteers. Participants were randomized to either have the ONSD measured first without a cervical collar or initially with a cervical collar. Two sonographers performed independent ONSD diameter measurements. Continuous data were analyzed by matched-paired t-tests. Alpha was set at 0.05. The primary outcome parameter was the overall mean difference between ONSD measurements with the cervical collar on and off. Multiple linear regression was performed to examine the relationship between variables and the primary outcome parameter.
Results:
There were 30 participants enrolled in the study. Overall mean ONSD for participants without the collar was 0.365 ± 0.071 cm and with the collar was 0.392 ± 0.081 cm. The mean change in ONSD for participants with and without the collar was 0.026 ± 0.064 cm (95% confidence interval of difference: 0.015–0.038; P < 0.001). Multiple regression analysis did not identify any variables associated with the variation in ONSD observed for collar versus noncollar.
Conclusions:
We confirmed that ONSD does vary by a measurable amount with placement of a rigid cervical collar on healthy volunteers when assessed by ultrasound.
Keywords: Bedside testing, optic nerve sheath diameter, trauma, ultrasound
INTRODUCTION
Cervical collars have been the standard of practice in the care of trauma patients through emergency medical services for many years. Multiple studies and case series have suggested that the use of cervical collars for spinal immobilization elevates intracranial pressure (ICP), a potentially devastating effect of a theoretically life-preserving intervention.[1,2,3,4,5,6] Other studies and case series have demonstrated variable effects or have suggested that the tightness of the collar is the main influence upon ICP elevation through the mechanism of venous obstruction.[7,8] These studies have either looked directly at ICP or at a surrogate measurement, such as jugular venous distention.
Point-of-care ultrasound (POCUS) has increasingly become more available, though not yet ubiquitous, in emergency departments (EDs) and increasingly important to the specialty of emergency medicine.[9,10,11] POCUS has become the standard of care for evaluating trauma patients with the focused assessment with sonography for trauma examination, and its value beyond this application is many and expanding.[12] Much research has been done regarding POCUS in the ED including its accuracy and impact on efficiency.[13,14,15,16,17] The number of residency programs that offer fellowships in emergency ultrasound has grown and has, therefore, increased the number of ultrasound fellowship-trained emergency physicians and residency-graduated emergency physicians comfortable for performing POCUS.[12] In recent years with the promulgation of ultrasound, it has become evident that POCUS may be used to measure optic nerve sheath diameter (ONSD), which serves as a reliable marker for elevated ICP when ONSD is increased.[18,19,20,21,22]
Millions of cervical collars are placed annually during the care of trauma patients.[23] The benefits of the cervical collars are not known, and they are potentially negative in regard to such things as time to extraction, transport times to the hospital, as well as their influence upon ICP.[23,24,25] The use of POCUS may help guide the risk–benefit analysis of cervical collars when POCUS is utilized to measure ONSD and thus ICP in the trauma patient.
When we initially conceived the study, we hypothesized that the ONSD would increase when a person is wearing a rigid cervical collar for spinal immobilization versus when she/he is not wearing a cervical collar. ONSD has been shown to correlate with ICP; therefore, this study aimed to imply that cervical collars increase ICP and that ocular ultrasound can rapidly assess ICP through the measurement of ONSD. During our study period, two similar, small studies were published providing some evidence for our hypothesis. Thus, we additionally sought to validate the results of these studies in an independent data.[26,27]
METHODS
Study design
This study was a prospective, crossover study in healthy volunteers to assess the difference between ONSD for participants with and without a cervical collar in place.
Study setting
Thirty healthy individuals were enrolled at a Level II trauma center in Corpus Christi, Texas, USA. The protocol was developed and subsequently approved by the CHRISTUS Health Internal Review Board on August 2, 2017. The study was conducted over two separate didactic sessions in September of 2017.
Study subjects
We recruited 30 volunteers from a group of emergency medicine residents, faculty of the residency program, and rotating medical students. Individuals had to be generally healthy, between the ages of 18 and 65 years, and willing and able to volunteer for this study to be included. Exclusion criteria included inability to consent, inability to lay flat on a bed or table for 15 min in duration, a history of glaucoma, globe injury, lens implant, or recent refractive surgery (within the past 60 days). In addition, volunteers were excluded if there was a history of stroke, elevated ICP, uncontrolled hypertension, or carotid artery disease. In view of the fact that volunteers in this study were primarily resident physicians from our own department, an independent counseling session was provided before the request for participation to avoid any perception of coercion in this study. All volunteers were verbally consented to take part in the study. No remuneration was provided for participation.
Measurements
Volunteers had an ONSD measurement done while wearing and while not wearing a cervical collar. They were randomized to either have ONSD measured first without cervical collar or initially with cervical collar. A rigid, “no-neck” cervical collar of appropriate size was used for the purposes of this study. The collars were Ossur Patriot® collars which offer total cervical arch support, universal size, ventilation openings to reduce heat and moisture, and multiheight adjustment. Each collar was placed in a similar manner by a single investigator. A period of 10 min elapsed between collar placement or removal and the second measurement. Two sonographers with either registered diagnostic medical sonographer (RDMS) qualifications or ultrasound fellowship training performed ONSD measurements upon each volunteer in both the eyes. Figure 1 illustrates the ultrasound image and specific areas of measurement to obtain ONSD. Each sonographer was blinded to the results of the other sonographer. The volunteer was supine for at least 5 min before the first set of measurements and remained so during the subsequent 10 min before the second set of measurements. Measurements were done while the patient was flat without any head elevation. The measurement of the ONSD was in the transverse plane and was measured 3 mm behind the globe. The optic nerve sheath was defined as the anechoic column visualized in the retrobulbar space, its diameter measured as the inside the hyperechoic dura mater.
Figure 1.
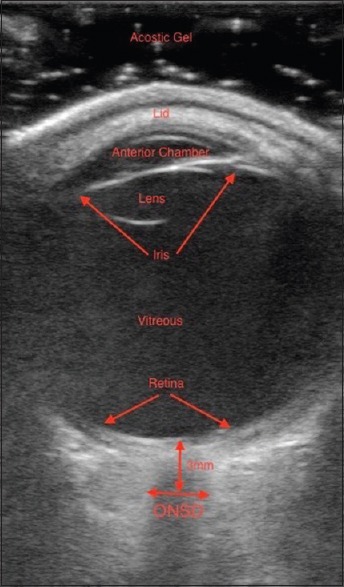
Optic nerve sheath diameter measurement
Statistical analysis
Data from the 30 volunteers were obtained from the sonographers and recorded by a single study author. Data collected included the participant's age and gender as well as the ONSD other both the eyes, from two sonographers, with and without a cervical collar in place. Continuous data were presented as mean ± standard deviation and were analyzed by paired t-tests. Alpha was set at 0.05. Confidence intervals (CIs) were calculated for mean difference between ONSD changes. The primary outcome parameter was the overall mean difference between cervical collars on ONSD. Multiple linear regression was performed to examine the relationship between variables and the primary outcome parameter.
RESULTS
In total, 240 separate measurements of ONSD were recorded on thirty volunteers. The volunteers ranged in age from 25 to 50 years and had a mean age of 29.7 years ± 4.57. Thirty percent of our participants were female. The average ONSD with a cervical collar in place was 0.392 ± 0.081 cm, whereas the average ONSD without a cervical collar placed was 0.365 ± 0.071 cm. The mean change in ONSD for participants with and without the collar was 0.026 ± 0.064 cm (95% CI of difference: 0.015–0.038; P < 0.001) [Figure 2], and these differences with the collar placement were essentially the same for each eye.
Figure 2.
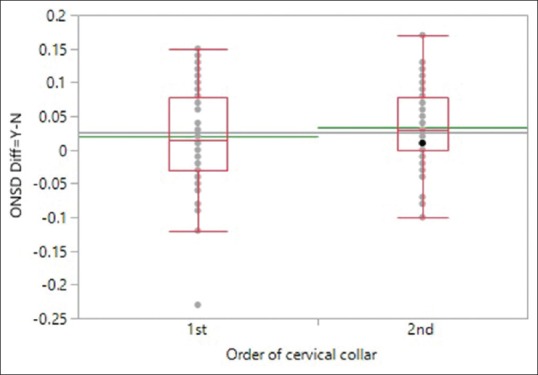
Order of the cervical collar
There were no significant differences for the mean change in ONSD irrespective of the order in which the collar was placed on ( first 0.20 ± 0.071 cm vs. second 0.033 ± 0.055 cm; P = 0.26). The mean difference between measurements by each examiner was 0.019 ± 0.073 cm. Multiple regression analysis did not identify any participant variables associated with the variation in ONSD observed for collar versus noncollar.
DISCUSSION
Two recent studies demonstrated that cervical collar placement was associated with increased ONSD. Maissan et al. conducted a prospective, blinded, crossover study of 45 healthy volunteers. Multiple measurements with and without cervical collars were recorded, and wearing a cervical collar was associated with increased ONSD. Unique to Maissan's study was the effort given in an attempt to blind the sonographers to each volunteer's collar status. A curtain was placed over each patient in a manner that allowed sonographers access to assess the ONSD while obstructing their view of the volunteer's neck. Before measurements, the Velcro straps of the cervical collar were opened and closed regardless of whether it was on the participant's neck, creating auditory ambiguity of the participant's collar status. Although this may not have been a perfect double-blinding process, it is good practice methodologically.
Woster et al.'s study was a prospective cohort study of 20 healthy volunteers. Baseline ONSD was measured and then ONSD was recorded both 5 and 20 min after cervical collar placement. Similar to the findings in the aforementioned study, cervical collars were noted to be associated with an increase ONSD. Woster's study took care not only to investigate whether an increase in ONSD associated with the placement of a cervical collar would be present but also whether or not this change in ONSD would be persistent or transient. In the study, the increase in ONSD that was noted with collar placement persisted for at least 15 min after the first measurement after collar placement.
While both of these studies were well designed and conducted, our study is novel for evaluating whether the order of placement of the cervical collar would be associated with a change in the diameter of the optic nerve sheath. Our study demonstrated that the change in ONSD with placement of a cervical collar appeared to be irrespective of the order in which the collar was placed or the time in which the patient was supine. Further, our multiple regression analysis found that gender, age, and timing of cervical collar placement were not significantly associated with changes in mean ONSD diameter.
Limitations
Our study has several limitations that warrant discussion. First of all, the study group was small, and yet, we did confirm an association between cervical collar placement and an increase in ONSD that had been observed in other reports. One of the unique aspects of the Maissan et al. study was the fact that the sonographers were blinded to the volunteers' collar status. We did not blind sonographers to participants' collar status in this manner; thus, there is a potential for bias in ONSD measurements from this perspective. In addition, another methodological concern within our study design was the fact that two sonographers comprised the role of Sonographer B. While we recorded measurements of two sonographers for each eye, for each patient, both with and without cervical collar placed, Sonographer A remained the same while two RDMS-qualified sonographers took turns making the measurements of Sonographer B. While we do not believe this significantly impacted the primary outcome of the study, it does limit our ability to assess for interobserver agreement.
Finally, another limitation of our study as well as the recent similar studies is that we performed ONSD measurements on healthy volunteers. The true utility of this modality would be to understand its accuracy in measuring ONSD and how this measurement could be utilized in the setting of evaluating ED patients with potential increases in ICP. We believe this provides a clear direction for future studies in this area of interest. We are currently developing protocols to compare ONSD measurements in uninjured patients against those with head injury and invasive monitoring devices where the ICP is known.
CONCLUSIONS
We found that cervical collar placement is associated with increased ONSD for healthy volunteers. Future studies should evaluate the utility of this modality for assessing patients with head trauma and other conditions that are associated with elevations in ICP.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Davies G, Deakin C, Wilson A. The effect of a rigid collar on intracranial pressure. Injury. 1996;27:647–9. doi: 10.1016/s0020-1383(96)00115-5. [DOI] [PubMed] [Google Scholar]
- 2.Craig GR, Nielsen MS. Rigid cervical collars and intracranial pressure. Intensive Care Med. 1991;17:504–5. doi: 10.1007/BF01690778. [DOI] [PubMed] [Google Scholar]
- 3.Raphael JH, Chotai R. Effects of the cervical collar on cerebrospinal fluid pressure. Anaesthesia. 1994;49:437–9. doi: 10.1111/j.1365-2044.1994.tb03482.x. [DOI] [PubMed] [Google Scholar]
- 4.Kolb JC, Summers RL, Galli RL. Cervical collar-induced changes in intracranial pressure. Am J Emerg Med. 1999;17:135–7. doi: 10.1016/s0735-6757(99)90044-x. [DOI] [PubMed] [Google Scholar]
- 5.Mobbs RJ, Stoodley MA, Fuller J. Effect of cervical hard collar on intracranial pressure after head injury. ANZ J Surg. 2002;72:389–91. doi: 10.1046/j.1445-2197.2002.02462.x. [DOI] [PubMed] [Google Scholar]
- 6.Hunt K, Hallworth S, Smith M. The effects of rigid collar placement on intracranial and cerebral perfusion pressures. Anaesthesia. 2001;56:511–3. doi: 10.1046/j.1365-2044.2001.02053.x. [DOI] [PubMed] [Google Scholar]
- 7.Kuhnigk H, Bomke S, Sefrin P. Effect of external cervical spine immobilization on intracranial pressure. Aktuelle Traumatol. 1993;23:350–3. [PubMed] [Google Scholar]
- 8.Stone MB, Tubridy CM, Curran R. The effect of rigid cervical collars on internal jugular vein dimensions. Acad Emerg Med. 2010;17:100–2. doi: 10.1111/j.1553-2712.2009.00624.x. [DOI] [PubMed] [Google Scholar]
- 9.Talley BE, Ginde AA, Raja AS, Sullivan AF, Espinola JA, Camargo CA, Jr, et al. Variable access to immediate bedside ultrasound in the emergency department. West J Emerg Med. 2011;12:96–9. [PMC free article] [PubMed] [Google Scholar]
- 10.Dean AJ, Breyer MJ, Ku BS, Mills AM, Pines JM. Emergency ultrasound usage among recent emergency medicine residency graduates of a convenience sample of 14 residencies. J Emerg Med. 2010;38:214–20. doi: 10.1016/j.jemermed.2007.12.028. [DOI] [PubMed] [Google Scholar]
- 11.Moore CL, Molina AA, Lin H. Ultrasonography in community emergency departments in the United States: Access to ultrasonography performed by consultants and status of emergency physician-performed ultrasonography. Ann Emerg Med. 2006;47:147–53. doi: 10.1016/j.annemergmed.2005.08.023. [DOI] [PubMed] [Google Scholar]
- 12.Adhikari S, Blaivas M. History, progress, and future of emergency ultrasound. Ultrasound Clin. 2014;9:119–21. [Google Scholar]
- 13.Hasani SA, Fathi M, Daadpey M, Zare MA, Tavakoli N, Abbasi S, et al. Accuracy of bedside emergency physician performed ultrasound in diagnosing different causes of acute abdominal pain: A prospective study. Clin Imaging. 2015;39:476–9. doi: 10.1016/j.clinimag.2015.01.011. [DOI] [PubMed] [Google Scholar]
- 14.Mallin M, Craven P, Ockerse P, Steenblik J, Forbes B, Boehm K, et al. Diagnosis of appendicitis by bedside ultrasound in the ED. Am J Emerg Med. 2015;33:430–2. doi: 10.1016/j.ajem.2014.10.004. [DOI] [PubMed] [Google Scholar]
- 15.Shih CH. Effect of emergency physician-performed pelvic sonography on length of stay in the emergency department. Ann Emerg Med. 1997;29:348–51. doi: 10.1016/s0196-0644(97)70346-9. [DOI] [PubMed] [Google Scholar]
- 16.Bertoglio K, Fischetti C. Emergency department versus radiology department pelvic ultrasound and effect on patient length of stay: A randomized control trial. Ann Emerg Med. 2013;62(Suppl):S80. [Google Scholar]
- 17.Bryczkowski C, Morrison D, Donato J, McCoy J. Impact of bedside ultrasound on emergency department length of stay in patients with a suspected peritonsillar abscess: A case series. Ultrasound Med Biol. 2015;41:S125. doi: 10.7759/cureus.32207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Raffiz M, Abdullah JM. Optic nerve sheath diameter measurement: A means of detecting raised ICP in adult traumatic and non-traumatic neurosurgical patients. Am J Emerg Med. 2017;35:150–3. doi: 10.1016/j.ajem.2016.09.044. [DOI] [PubMed] [Google Scholar]
- 19.Padayachy LC, Padayachy V, Galal U, Gray R, Fieggen AG. The relationship between transorbital ultrasound measurement of the optic nerve sheath diameter (ONSD) and invasively measured ICP in children: Part I: Repeatability, observer variability and general analysis. Childs Nerv Syst. 2016;32:1769–78. doi: 10.1007/s00381-016-3067-5. [DOI] [PubMed] [Google Scholar]
- 20.Padayachy LC, Padayachy V, Galal U, Pollock T, Fieggen AG. The relationship between transorbital ultrasound measurement of the optic nerve sheath diameter (ONSD) and invasively measured ICP in children: Part II: Age-related ONSD cut-off values and patency of the anterior fontanelle. Childs Nerv Syst. 2016;32:1779–85. doi: 10.1007/s00381-016-3068-4. [DOI] [PubMed] [Google Scholar]
- 21.Young AM, Guilfoyle MR, Donnelly J, Scoffings D, Fernandes H, Garnett M, et al. Correlating optic nerve sheath diameter with opening intracranial pressure in pediatric traumatic brain injury. Pediatr Res. 2017;81:443–7. doi: 10.1038/pr.2016.165. [DOI] [PubMed] [Google Scholar]
- 22.Komut E, Kozacı N, Sönmez BM, Yılmaz F, Komut S, Yıldırım ZN, et al. Bedside sonographic measurement of optic nerve sheath diameter as a predictor of intracranial pressure in ED. Am J Emerg Med. 2016;34:963–7. doi: 10.1016/j.ajem.2016.02.012. [DOI] [PubMed] [Google Scholar]
- 23.Sundstrøm T, Asbjørnsen H, Habiba S, Sunde GA, Wester K. Prehospital use of cervical collars in trauma patients: A critical review. J Neurotrauma. 2014;31:531–40. doi: 10.1089/neu.2013.3094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vanderlan WB, Tew BE, McSwain NE., Jr Increased risk of death with cervical spine immobilisation in penetrating cervical trauma. Injury. 2009;40:880–3. doi: 10.1016/j.injury.2009.01.011. [DOI] [PubMed] [Google Scholar]
- 25.Haut ER, Kalish BT, Efron DT, Haider AH, Stevens KA, Kieninger AN, et al. Spine immobilization in penetrating trauma: More harm than good? J Trauma. 2010;68:115–20. doi: 10.1097/TA.0b013e3181c9ee58. [DOI] [PubMed] [Google Scholar]
- 26.Maissan IM, Ketelaars R, Vlottes B, Hoeks SE, den Hartog D, Stolker RJ, et al. Increase in intracranial pressure by application of a rigid cervical collar: A pilot study in healthy volunteers. Eur J Emerg Med. 2018;25:e24–8. doi: 10.1097/MEJ.0000000000000490. [DOI] [PubMed] [Google Scholar]
- 27.Woster CM, Zwank MD, Pasquarella JR, Wewerka SS, Anderson JP, Greupner JT, et al. Placement of a cervical collar increases the optic nerve sheath diameter in healthy adults. Am J Emerg Med. 2018;36:430–4. doi: 10.1016/j.ajem.2017.08.051. [DOI] [PubMed] [Google Scholar]


