Abstract
A 27-year-old pregnant female underwent cesarean section due to preeclampsia. Two days after the delivery, she presented with acute onset of blurred vision in the left eye. Optical coherence tomography (OCT) revealed characteristic findings of acute macular neuroretinopathy (AMN) in both eyes. During the follow-up, her vision improved gradually, but outer nuclear layer thinning with disruption of ellipsoid zone was identified from OCT. OCT angiography was arranged and revealed both vascular defect in superficial and deep vascular plexus, which correlated with previous AMN lesions in both eyes. Subsequent microvascular change in AMN was found to involve both superficial and deep vascular plexus, which is different from the current consensus that AMN mainly involved deep vascular plexus. By using the OCT angiography, we can better visualize the detail retinal vascular structure and may identify the real mechanism in this rare retinal disorder.
Keywords: Acute macular neuroretinopathy, optical coherence tomography angiography, preeclampsia, pregnant
Introduction
Acute macular neuroretinopathy (AMN) is a rare retinal disorder firstly described by Bos and Deutman in 1975.[1] It usually presented as acute onset of paracentral scotoma, with the unique fundus findings of reddish brown wedge-shaped or petalloid lesions located at parafoveal area. With the development of spectral domain optical coherence tomography (SD-OCT), Sarraf et al.[2] further categorized the lesions into two types according to the layer involved either above or below the outer plexiform layer (OPL). Type 1 AMN, now known as paracentral acute middle maculopathy (PAMM), refers to hyperreflective bands in the OPL/inner nuclear layer (INL), whereas type 2 AMN, the classic AMN, refers to hyperreflective bands in the OPL/outer nuclear layer (ONL) with disruption of the ellipsoid zone (EZ). It was recently proposed that these two lesion types should be considered distinct entities.[3] PAMM lesions reflect superficial or intermediate capillary plexus occlusion, whereas AMN lesions are caused by deep capillary plexus ischemia.[4]
OCT angiography is a novel imaging modality, which facilitates visualization of retinal vascular flow and detection of vascular defect after the ischemia insult. Here, we report a case of AMN with typical SD-OCT finding and analyzed the subsequent microvascular change by using OCT angiography.
Case Report
A 27-year-old pregnant female at gestational age 39 weeks received cesarean section due to preeclampsia and prolonged labor. Two days after the delivery, she complained of sudden blurred vision with scotoma in her left eye. The best-corrected visual acuity was 20/20 in the right eye and 20/60 in the left eye. The anterior segment examination was unremarkable. Fundus examination revealed bilateral grayish lesions at parafoveal region and more prominent in the left eye [Figure 1]. SD-OCT showed a hyperreflective band located at the ONL level with disruption of underlying EZ [Figure 2a and 2b]. Fluorescein angiography and indocyanine green angiography were all unremarkable. AMN was diagnosed according to the characteristic OCT findings. One month later, the patient's visual acuity improved to 20/40 in her left eye. SD-OCT revealed resolution of previous band-like lesion but left with subsequent ONL thinning and EZ loss [Figure 2c and 2d]. OCT angiography was arranged and showed both vascular defect found at superficial capillary plexus (SCP) and deep capillary plexus (DCP), which were congruent to AMN lesions [Figure 3 and 4].
Figure 1.
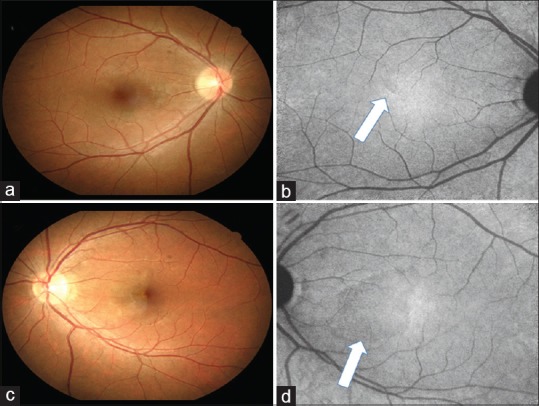
Color fundus photograph and near-infrared reflectance images of the right eye (a and b) and the left eye (c and d). Lesions (arrows) are prominent in the left eye and can be better visualized from near-infrared reflectance images
Figure 2.
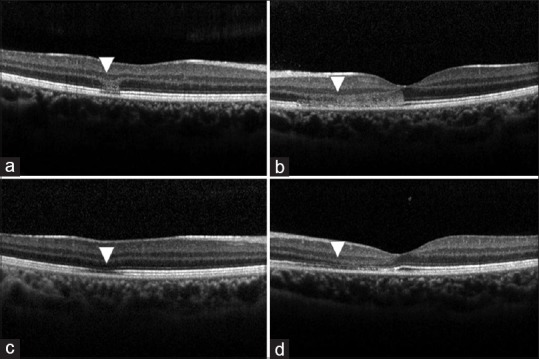
Spectral-domain optical coherence tomography images of the right eye (a and c) and the left eye (b and d). Both a and b revealed characteristic hyperreflective band in the region of outer nuclear layer and outer plexiform layer (arrowheads). After 1 month, spectral-domain optical coherence tomography images of bilateral eyes (c and d) revealed resolution of the previous band lesions but showed thinning of outer nuclear layer and disruption of ellipsoid zone (arrowheads)
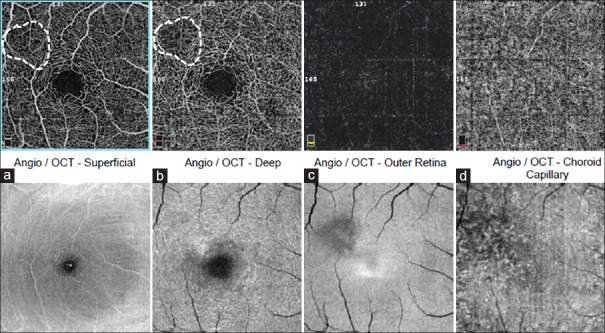
Figure 3.
Optical coherence tomography angiography and en face optical coherence tomography of the right eye. (a) Superficial capillary plexus; (b) deep retinal capillary plexus; (c) outer retina and (d) choroid capillary. Both vascular density in superficial capillary plexus and deep capillary plexus were lower at the area correlated precisely to the en face optical coherence tomography of ellipsoid loss and acute macular neuroretinopathy lesions
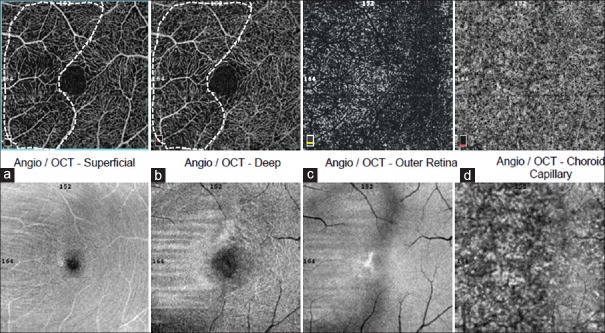
Figure 4.
Optical coherence tomography angiography and en face optical coherence tomography of the left eye. (a) Superficial capillary plexus; (b) deep retinal capillary plexus; (c) outer retina and (d) choroid capillary. Note the lesion was prominent in the left eye and similarly the vascular defects both in superficial capillary plexus and deep capillary plexus are correlated to the lesions identified from en face optical coherence tomography
Discussion
AMN is a relatively uncommon retinal disorder condition that has been previously reported to be associated with various condition, including oral contraceptives, heavy caffeine consumption, epinephrine or ephedrine therapy, viral and flu-like illnesses, and hypovolemic shock.[1,4,5] Recent associations also include sympathomimetic drugs, dengue fever, and systemic lupus erythematosus.[6,7,8] In this study, we reported a preeclampsia female who received cesarean section and developed AMN 2 days after the delivery. Although the lesions in our case were more grayish lesions, which are different from the typical red wedge-shaped lesions found in the original description,[1] SD-OCT has shown the characteristic of deep retinal changes and confirmed the diagnosis.
AMN in pregnant women after delivery was previously reported with 2 women underwent cesarean section, and 1 woman received spontaneous delivery.[9,10] AMN in eclampsia was also reported previously,[11] but the causative mechanism was not clarified. The pathogenesis of AMN is recently recognized as a microvascular etiology with a possible DCP ischemia. Therefore, we can assume the hypoperfusion in retinal circulation related with preeclampsia and postpartum hypotension to be contributive in AMN development in our patient.
By using OCT angiography, the microvascular structure and deep retinal vascular circulation can be better visualized. We confirmed the deep capillary vascular defects found from OCT angiography in our case after 1 month. Interestingly, the vascular defects were also identified at SCP, which is believed to be mainly affected in PAMM. In previous studies, OCT angiography findings in AMN were reported only as deep retinal capillary plexus perfusion defect[12] or choriocapillaris nonperfusion.[13]
So far, there has been no AMN patient whose ischemia layer was found to involve both DCP and SCP on OCT angiography. Since OCT angiography instrument assumes the SCP to be uniformly thick from the perifoveal area across the foveal avascular zone, the assumption is incorrect in true histology correlation.[14] Therefore, the SCP layer segmented may include a variable amount of the DCP surrounding the foveal center and the amount varies between individuals. Besides, OCT angiography in choroid or deep capillaries is recently being questioned of potential image-related artifacts.[15] Nevertheless, the area of vascular defect both in SCP and DCP is clearly visualized and strongly compatible to the lesions noted from fundus and OCT examinations in our case. Therefore, we assumed that the ischemia insult in AMN not only takes place in deep capillaries but in superficial vascular layer as well The other possibility lies in that vascular defect developed in superficial layer may be a secondary phenomenon after the retinal ischemia. Since we only followed OCT angiography 1 month after the diagnosis, the serial OCT angiography at different timing is further needed to clarify this possibility in future studies.
Conclusion
We report an AMN case with subsequent microvascular change, which involves in both superficial and deep vascular plexus. It is relatively uncommon from the current consensus that vascular insult in AMN mainly involves the deep vascular plexus. By using OCT angiography, we can better visualize the detail retinal vascular structure and may extend our understanding to this disease, but further studies are needed in the future.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
The authors declare that there are no conflicts of interests of this paper.
References
- 1.Bos PJ, Deutman AF. Acute macular neuroretinopathy. Am J Ophthalmol. 1975;80:573–84. doi: 10.1016/0002-9394(75)90387-6. [DOI] [PubMed] [Google Scholar]
- 2.Sarraf D, Rahimy E, Fawzi AA, Sohn E, Barbazetto I, Zacks DN, et al. Paracentral acute middle maculopathy: A new variant of acute macular neuroretinopathy associated with retinal capillary ischemia. JAMA Ophthalmol. 2013;131:1275–87. doi: 10.1001/jamaophthalmol.2013.4056. [DOI] [PubMed] [Google Scholar]
- 3.Rahimy E, Kuehlewein L, Sadda SR, Sarraf D. Paracentral acute middle maculopathy: What we knew then and what we know now. Retina. 2015;35:1921–30. doi: 10.1097/IAE.0000000000000785. [DOI] [PubMed] [Google Scholar]
- 4.Yu S, Pang CE, Gong Y, Freund KB, Yannuzzi LA, Rahimy E, et al. The spectrum of superficial and deep capillary ischemia in retinal artery occlusion. Am J Ophthalmol. 2015;159:53–630. doi: 10.1016/j.ajo.2014.09.027. [DOI] [PubMed] [Google Scholar]
- 5.Kerrison JB, Pollock SC, Biousse V, Newman NJ. Coffee and doughnut maculopathy: A cause of acute central ring scotomas. Br J Ophthalmol. 2000;84:158–64. doi: 10.1136/bjo.84.2.158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Leys M, Van Slycken S, Koller J, Van de Sompel W. Acute macular neuroretinopathy after shock. Bull Soc Belge Ophtalmol. 1991;241:95–104. [PubMed] [Google Scholar]
- 7.Munk MR, Jampol LM, Cunha Souza E, de Andrade GC, Esmaili DD, Sarraf D, et al. New associations of classic acute macular neuroretinopathy. Br J Ophthalmol. 2016;100:389–94. doi: 10.1136/bjophthalmol-2015-306845. [DOI] [PubMed] [Google Scholar]
- 8.Lee DH, Lee SC, Kim M. Acute macular neuroretinopathy associated with systemic lupus erythematosus. Lupus. 2016;25:431–5. doi: 10.1177/0961203315619494. [DOI] [PubMed] [Google Scholar]
- 9.Turbeville SD, Cowan LD, Gass JD. Acute macular neuroretinopathy: A review of the literature. Surv Ophthalmol. 2003;48:1–11. doi: 10.1016/s0039-6257(02)00398-3. [DOI] [PubMed] [Google Scholar]
- 10.Aziz HA, Kheir WJ, Young RC, Isom RF, Dubovy SR. Acute macular neuroretinopathy: A case report and review of the literature, 2002-2012. Ophthalmic Surg Lasers Imaging Retina. 2015;46:114–24. doi: 10.3928/23258160-20150101-23. [DOI] [PubMed] [Google Scholar]
- 11.Vance SK, Spaide RF, Freund KB, Wiznia R, Cooney MJ. Outer retinal abnormalities in acute macular neuroretinopathy. Retina. 2011;31:441–5. doi: 10.1097/IAE.0b013e3181fe54fa. [DOI] [PubMed] [Google Scholar]
- 12.Pecen PE, Smith AG, Ehlers JP. Optical coherence tomography angiography of acute macular neuroretinopathy and paracentral acute middle maculopathy. JAMA Ophthalmol. 2015;133:1478–80. doi: 10.1001/jamaophthalmol.2015.4100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Thanos A, Faia LJ, Yonekawa Y, Randhawa S. Optical coherence tomographic angiography in acute macular neuroretinopathy. JAMA Ophthalmol. 2016;134:1310–4. doi: 10.1001/jamaophthalmol.2016.3513. [DOI] [PubMed] [Google Scholar]
- 14.Spaide RF, Curcio CA. Evaluation of segmentation of the superficial and deep vascular layers of the retina by optical coherence tomography angiography instruments in normal eyes. JAMA Ophthalmol. 2017;135:259–62. doi: 10.1001/jamaophthalmol.2016.5327. [DOI] [PubMed] [Google Scholar]
- 15.Ashraf M, Goldstein D, Fawzi A. Optical coherence tomography angiography: Potential artifacts in acute macular neuroretinopathy. JAMA Ophthalmol. 2017;135:675–6. doi: 10.1001/jamaophthalmol.2017.0918. [DOI] [PubMed] [Google Scholar]