Abstract
Objective
To report our operative experience with precision pulse capsulotomy (PPC) for anterior capsulotomy in a paediatric cataract series.
Methods and analysis
This study is a retrospective interventional, descriptive series of consecutive paediatric eyes (≤16 years) undergoing cataract surgery using PPC. Surgical time and the time required to perform PPC was recorded. Any intraoperative and postoperative adverse events were noted. Postoperatively, visual acuity, anterior segment examination and intraocular pressure (IOP) were recorded for all children at day 1, 1 week and 1 month.
Results
21 eyes of 14 patients were included in the study, with the median age at surgery of 6.0 years (IQR; 5-7.75, range=1–16 years). Male to female ratio was 11:3. 13 eyes had lamellar cataract, 3 eyes had total cataract, 2 had posterior subcapsular cataract, 2 had traumatic cataract, while 1 eye had sutural cataract. Median surgical time was 26 min (IQR 21-32) and median PPC time was 75.0 secs (IQR 56-86.5). The anterior capsulotomy was round and complete in most cases, except in one case due to faulty suction. All patients underwent a successful in the bag implantation of intraocular lens with capsulotomy margins overlapping the optic edges in 19 eyes (90%). Median PPC size was 5.54 mm (n=9, IQR 5.39 -5.75) which was slightly larger than expected. None of the cases had any intraoperative or postoperative adverse events with no radial tears of capsulotomy. Postoperatively, the mean final follow-up was 5.71+3.20 weeks.
Conclusion
To conclude PPC can be used as an alternative to manual continuous curvilinear capsulorhexis in paediatric cataract surgery producing round well- centred and strong capsulotomy with an easier learning curve.
Keywords: precision pulse capsulotomy (ppc), pediatric cataract surgery, anterior capsulotomy, technical ease, properties of ppc, size of ppc, infants
Key messages.
What is already known about this subject?
Continuous curvilinear capsulorhexis (CCC) is challenging in paediatric cataract due to its higher elasticity. A new technology called ‘precision pulse capsulotomy’ (PPC) has shown good surgical outcomes in adult cataract producing circular, accurate, strong and well-centred anterior capsulotomy.
What are the new findings?
PPC is a safe, accurate and reliable technology to produce an automated anterior capsulotomy in paediatric cataract.
How might these results change the focus of research or clinical practice?
PPC can be an effective alternative to manual CCC, especially in the hands of beginners/trainees and those with little experience in paediatric cataract. However, further prospective studies are required to understand the long-term outcomes of the procedure.
Introduction
A complete, round and centred capsulotomy is a crucial step in cataract surgery in order to obtain optimum postoperative results. Manual continuous curvilinear capsulorhexis (CCC) has been considered the gold standard for capsulotomy but has a steep learning curve and difficult to perform in certain situations like paediatric cataract, thick fibrotic plaque on anterior capsule, intumescent cataract, small pupils and corneal opacity, even for experienced surgeons.
Paediatric lens capsule is known to be more elastic and tear-resistant than adult lens capsule, offering significant resistance to the shearing forces applied during manual CCC.1 2 It has been reported that the completion rate for paediatric capsulorhexis was only 67% in the hands of trainees,3 and ranging from 47% to 90% in the hands of experienced surgeons depending on the different operating conditions such as type of viscoelastic device (VED) used during the surgery or the type of cataract, thus showing that in unfavourable conditions it is difficult to perform a good, complete manual CCC in children, even for experienced surgeons.4 Several modifications have been used to achieve a good capsulorhexis in children like two incision push pull technique, vitrectorhexis, diathermy, Fugo plasma blade and femtosecond laser. In view of automating capsulotomy, a new technology called precision pulse capsulotomy (PPC) was developed which consistently produced circular, accurate, strong and well-centred capsulotomy in animal and human cadaveric eyes,5 6 and good clinical outcomes in adult eyes operated for senile cataract.7 8 However, this technology has not yet been applied in paediatric cataract. The aim of this study is to report our operative experience in using PPC for anterior capsulotomy in paediatric cataract surgery.
Methods
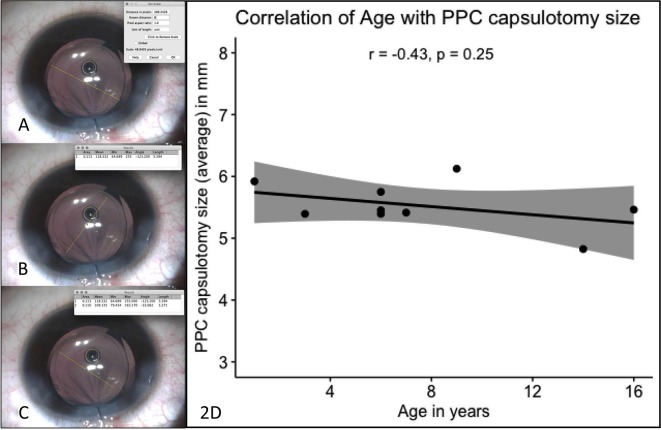
This study is a retrospective analysis of consecutive paediatric eyes (≤16 years of age) undergoing cataract surgery using PPC technology for anterior capsulotomy. An informed consent was taken from the guardians of patients for the surgical procedure after explaining its possible advantages and disadvantages. The study was conducted between March 2017 and September 2017, at two tertiary eye care centres in south India and adhered to the tenets declaration of Helsinki. All patients underwent a thorough preoperative evaluation, including a detailed history, age appropriate methods of vision assessment, anterior and posterior segment examinations. Corneal diameter, axial length and keratometry were measured for all patients. All patients underwent a similar surgical technique (described later) by one of the three experienced paediatric cataract surgeons (figure 1). Any intraoperative adverse events were noted. Total surgical time from patient records and time required to perform PPC starting from entering the probe to its withdrawal from the anterior chamber (AC), was recorded using the surgical video, if available. After intraocular lens (IOL) implantation, completing primary posterior capsulorhexis and clearing the VEDs completely from the AC, the size of capsulotomy was measured using IOL optic size (6 mm) as a reference to set the pixel scale of the image using an open source image J software (Fiji software)9 and then comparing it to the PPC size in two meridians; along the haptic of the IOL and perpendicular to the haptics of the IOL (figure 2) and their average was considered for further analysis.
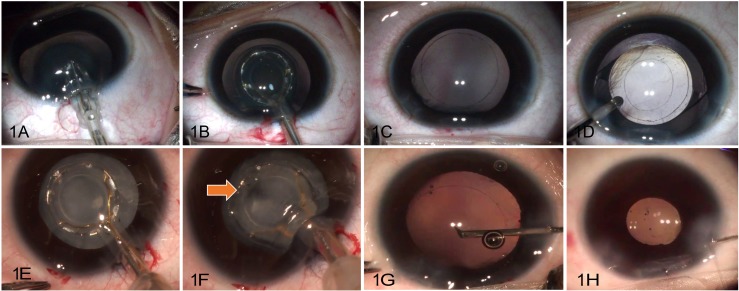
Figure 1.
PPC in lamellar cataract (A–D) and total intumescent cataract (E to H): PPC probe is collapsed and inserted into AC (A), followed by reopening, centration (B, E) and application of suction. A series of nanoelectrical pulse wave forms are delivered (F) and the probe is withdrawn from AC forming a round centred capsulotomy (C), facilitating in the bag IOL implantation (D and H). The instantaneous 360° creation of round regular capsulotomy with simultaneous suction of the liquefied cortex (F, arrow) prevents radial tears. AC, anterior chamber; IOL, intraocular lens; PPC, precision pulse capsulotomy.
Figure 2.
Measurement of size of PPC capsulotomy using image J software. Using the known size of the diameter of IOL optic (6 mm), the scale for the image is set (A). Measurement of diameter of PPC capsulotomy along the IOL haptic (B, length 1) and perpendicular to the IOL haptic (C, length 2) done using the set scale and average of the two diameter. No significant correlation was found between the age of the patients and capsulotomy size (p=0.25, CI (5% and 95%) shown as the shaded region) (D). IOL, intraocular lens; PPC, precision pulse capsulotomy.
Postoperatively, vision assessment, anterior segment examination and IOP were recorded for all children at day 1, 1 week and 1 month. The centration, size and configuration of the anterior capsulotomy were recorded clinically.
PPC device
The device named Zepto (Mynosys, California) consists of console powering a disposable probe, its tip containing a ring made up of nitinol which is a superelastic shape memory alloy. This ring can be easily collapsed and inserted through a minimum of 2.2 mm corneal incision,10 which reopens once inserted into the AC, regaining its original shape. It is surrounded by silicon cup which applies gentle suction to appose the anterior capsule to the inferior surface of nitinol ring. A rapid series of electrical nanopulses are delivered through the nitinol ring, resulting in vapourisation of water molecules trapped between the nitinol ring and the lens capsule, causing instantaneous 360° mechanical cleavage of the stretched capsule without cauterising any tissue.10
Surgical technique
Under all aseptic precautions, two side ports were made at 10 and 2 o’ clock and a 3.2 mm clear corneal wound was constructed superiorly. The capsulotomy ring of the PPC probe was collapsed by sliding the button on the hand-piece and entered through the main wound (figure 1). Once the ring was inside the AC, the sliding button was pulled back with the thumb to open the collapsed ring. After positioning the capsulotomy ring, suction was applied by an unsterile assistant operating the console and small air bubbles were seen moving towards the main wound due to the clearing of VEDs between the suction ring and the anterior capsule. Once this movement ceases, the suction is considered to be complete and nanopulses are delivered with a total duration of 4 ms. Suction was relieved, the ring was pulled out through the main wound with the cut anterior lens capsule either adhered to the capsulotomy ring or remained freely floating in the AC which was easily removed using forceps. The routine steps of lens aspiration, IOL implantation and primary posterior capsulotomy with anterior vitrectomy (if indicated) were performed. Corneal wounds were sutured appropriately.
Statistical analysis
This study is mainly a descriptive study. The mean and SD for parametric data and median with IQR for non-parametric data were calculated using Microsoft excel 2016. Mann-Whitney test and Spearman correlation was applied for non-parametric data using the open-source R software and R studio.
Patient and public involvement statement
The details of the study and the outcome measures were explained to the guardian/parents including the advantages and disadvantages of PPC based on available literature. Guardians were given a choice to opt for a new automated technology called precision pulse capsulotomy or the conventional manual CCC. All patients who opted for PPC were included in the study. The outcomes of the procedure and the results of the study have been shared with the patients.
Results
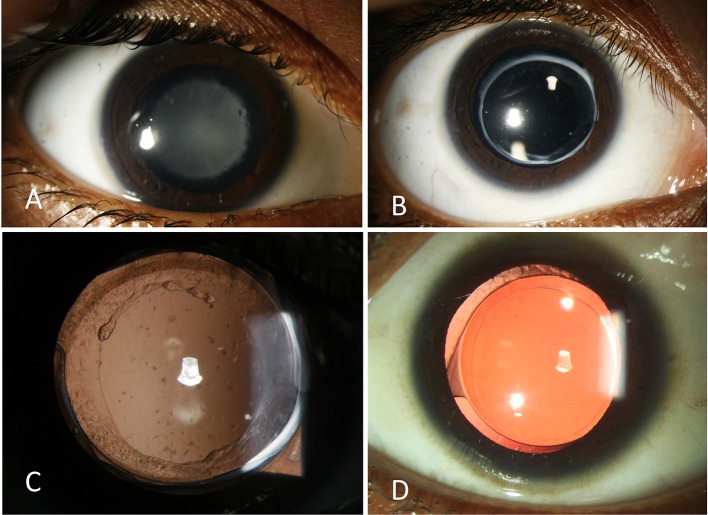
Twenty-one eyes of 14 patients were included in the study, of which, 12 eyes were right and 9 were left. The median age at the time of surgery was 6 years (range=1–16 years) (table 1). Male to female ratio was 11:3. Median preoperative visual acuity was 1.00 LogMAR unit. Morphology of cataract, axial lengths, AC depth and morphology, corneal diameter, pupillary dilation, surgical time and PPC time has been explained in table 1. Dispersive VEDs were used in three eyes while cohesive VEDs in remaining 18 eyes, based on the surgeon’s preference and economic considerations. PPC achieved complete capsulotomy in 20 cases (95%) with one case failing due to faulty suction. A second attempt in this eye after changing the PPC probe was successful with a complete, round and well-centred capsulotomy. All eyes had round and regular capsulotomy with multiple fine capsular tags and irregularities at its edges visible intraoperatively. Capsulotomy margin overlapped the IOL optic 360° 19 eyes (90%) (figure 3) except in two cases in which, one case had mild inferior decentration of the capsulotomy, while the other had larger capsulotomy size. All eyes underwent lens aspiration with a successful in the bag implantation of acrylic foldable hydrophobic IOL. Seventeen eyes had additional primary posterior capsulotomy with anterior vitrectomy. None of the eyes had any intraoperative or postoperative complication with no radial tears. Surgical video was available for 15 eyes, out of which PPC size was measured in 9 eyes while the remaining 6 eyes had either insufficient dilation or distortion of view due to air bubbles in AC at the end of surgery. Median anterior capsulotomy size was 5.45 mm (n=9; along the haptic 5.57 mm; opposite to the haptics 5.47 mm) ranging from 4.82 to 6.12 mm. We did not find any significant correlation between the age of the patient and the size of the PPC capsulotomy (p=0.25) (figure 2).
Table 1.
Demographic, preoperative, intraoperative and postoperative characteristics of all patients
| Sl no. | Preoperative | Intraoperative | Postoperative | ||||||||||||||
| Age (years) | Sex | Study eye | BCVA logMAR | Anterior segment | Morphology of cataract | AL (mm) | AC depth (mm) | WTW (mm) | Surgical time (min) | PPC time (s) | PPC size (average) (mm) | Centration | Pupillary dilatation | Duration of F/U (weeks) | BCVA | Visual axis (VA) | |
| 1 | 6 | F | OD | 0.5 | Normal | Lamellar | 18.85 | 3.52 | 11.58 | 26 | 92 | NA | Well centred | Good | 12 | 0.3 | Clear VA |
| OS | 0.5 | Normal | Lamellar | 18.71 | 3.59 | 10.67 | 28 | 133 | NA | Inferiorly decentred* | Moderate | 0.3 | Clear VA | ||||
| 2 | 7 | M | OD | 0.6 | Normal | Lamellar | 22.75 | 3.17 | 12.07 | 27 | 72 | 5.41 | Well centred | Good | 8 | 0.3 | Clear VA |
| OS | 0.5 | Normal | Lamellar | 22.73 | 3.21 | 12.4 | 40 | NA | NA | Well centred | Good | 0.3 | Clear VA | ||||
| 3 | 6 | M | OD | 1.2 | Normal | Lamellar | 24.17 | 3.91 | 11.39 | 24 | 79 | 5.33 | Well centred | Good | 8 | 0.7 | Clear VA |
| OS | 1 | Normal | Lamellar | 23.13 | 3.9 | NA | 40 | NA | 5.75 | Well centred | Good | 0.9 | Clear VA | ||||
| 4 | 1 | M | OD | 1.4 | Normal | Lamellar | 19.36 | NA | 11 | 37 | 79 | 5.92 | Well centred | Good | 4 | 1.4 | Clear VA |
| OS | 1.4 | Normal | Lamellar | 20.18 | NA | 11 | 27 | 52 | NA | Well centred | Good | 1.4 | Clear VA | ||||
| 5 | 9 | F | OD | 2.1 | Normal | Lamellar | 19.47 | NA | NA | 32 | 90 | 6.12 | Well centred* | Good | 12 | 2.1 | Clear VA |
| 6 | 8 | M | OD | 2.1 | Normal | Lamellar | 24.26 | NA | NA | 33 | 130 | NA | Well centred | Good | 1 | 2.1 | Clear VA |
| 7 | 5 | M | OS | 1.6 | Normal | Total/intumescent | 24.75 | 3.8 | 12.26 | 30 | NA | NA | Well centred | Good | 4 | 1.1 | Clear VA |
| 8 | 3 | M | OD | 1.1 | Normal | Lamellar | 22.11 | NA | 11 | 18 | 71 | NA | Well centred | Moderate | 6 | 0.7 | Clear VA |
| OS | 2.1 | Normal | Total/intumescent | 22.12 | NA | 11 | 21 | 45 | 5.39 | Well centred | Good | 0.7 | Clear VA | ||||
| 9 | 14 | F | OD | 0.4 | Normal | Y-shaped sutural | 22.7 | 3.92 | 12.6 | 20 | 36 | 4.82 | Well centred | Good | 4 | 0.3 | Clear VA |
| 10 | 6 | M | OS | 0.5 | Linear full thickness corneal scar—paracentral | Dense PSC—traumatic | 22.82 | 2.96 | 12 | 23 | NA | NA | Well centred | Good | 4 | 0.2 | Clear VA |
| 11 | 16 | M | OD | 0.4 | Normal | PSC | 23.49 | 4.19 | 13.12 | 15 | 60 | 5.46 | Well centred | Good | 4 | 0 | Clear VA |
| OS | 0.2 | Normal | PSC | 23.52 | 4.13 | 13.53 | 16 | NA | NA | Well centred | Good | 0 | Clear VA | ||||
| 12 | 5 | M | OD | 2.1 | AC inflammation, white fluffy cortex, mild corneal oedema, thick anterior capsular plaque, posterior synechiae (released intraoperatively) | Traumatic total/intumescent cataract | 22.21 | 3.88 | 11.57 | 47 | NA | NA | Well centred | Moderate | 4 | 0.2 | Clear VA |
| 13 | 5 | M | OD | 2.1 | Normal | Total/intumescent | 22.07 | 2.52 | NA | 12 | 41 | NA | Well centred | Good | 5 | 1 | Clear VA |
| 14 | 6 | M | OD | 0.4 | Normal | Lamellar | 21.17 | 3.33 | 11.58 | 25 | 83 | 5.45 | Well centred | Good | 4 | 0.4 | Clear VA |
| OS | 0.5 | Normal | Lamellar | 21.08 | 3.26 | 11.26 | 25 | 75 | NA | Well centred | Good | 0.4 | Clear VA | ||||
| Med | 6 | 1 | NA | NA | 22.21 | 3.59 | 11.58 | 26 | 75 | 5.45 | NA | NA | 4 | 0.4 | NA | ||
| IQR | 5–7.75 | 0.5–1.6 | NA | NA | 21.08–23.13 | 3.23–3.90 | 11–12.26 | 21 to 32 | 56–86.5 | 5.39–5.75 | NA | NA | 4–7.5 | 0.3–1 | NA | ||
*Not overlapping the optic of the IOL 360°.
AC, anterior segment;AL, axial length;BCVA, best-corrected visual acuity in LogMAR;F, female;M, male;Med, median; NA, not available/not applicable; PPC, precision pulse capsulotomy;PSC, posterior subcapsular cataract;VA, visual axis;WTW, white to white corneal diameter.
Figure 3.
Preoperative (A) and 3-month postoperative (B,C) slit lamp images showing round, complete capsulotomy overlapping the IOL optic, while (D) shows similar image in another case. IOL, intraocular lens.
Postoperatively, the median final follow-up was 4 weeks and final median best-corrected visual acuity improved to 0.40 LogMAR units (table 1). Mean IOP at the last follow-up was 16.5±3.16 mm Hg.
Special situations
Traumatic cataract
Case 1: A 5-year-old boy presented with total traumatic cataract and traumatic uveitis with posterior synechiae following a blunt trauma to the right eye. Topical steroids and mydriatics were started preoperatively until the inflammation reduced. Intraoperatively, synechiae were released using a spatula and a thick anterior capsular plaque (central 3 mm) was noted. The PPC probe with its silicone cuff was carefully manoeuvred below the pupillary margins to avoid any iris tissue entrapment. The probe was centred, suction was applied and the pulse was delivered, instantaneously creating a complete, round, well-centred capsulotomy. The liquefied cortex was aspirated simultaneously leaving behind a small lens nucleus. PPC probe was gently removed from AC followed by lens aspiration, successful implantation of IOL and primary posterior capsulotomy with anterior vitrectomy. As the pupil was not well dilated, it was difficult to judge the size of capsulotomy but it appeared to be larger than expected.
Case 2: A 6-year-old boy presented with traumatic posterior subcapsular cataract and partial thickness corneal scar in the left eye after projectile (fire cracker) injury. Corneal scar was linear, paracentral and covered more than 3 clock hours resulting in significant distortion of the view for capsulotomy. Intraoperatively, the pupil was well-dilated, hence the PPC probe was comfortably manoeuvred and centred. A round, complete and well-centred capsulotomy was obtained with a successful IOL implantation and posterior capsulotomy.
Intumescent/Total cataract
PPC was successfully performed in three eyes with total intumescent cataract (figure 1F–J). Anterior capsule was not stained before performing the capsulotomy. The insertion of PPC probe into AC and centration was achieved with ease along with successful application of suction and pulse waveform was delivered. The capsulotomy was created instantaneously and the liquefied cortex was aspirated due to the applied suction simultaneously, leaving behind a soft nucleus. The capsulotomy was complete with no radial tears and was strong enough to continue with the lens aspiration, in the bag implantation of IOL along with posterior capsulotomy.
Discussion
Ease of performing PPC
A good anterior capsulotomy is of utmost importance with regard to IOL implantation, long-term stability, centration and optical quality. The higher elasticity of the paediatric lens capsule poses a significant challenge for the surgeons and results in a difficult learning curve for manual CCC. On the other hand, PPC was technically easier to perform and had a fast learning curve. The PPC probe was effortlessly entered and snuggled out of the AC through a 3.2 mm clear corneal incision without damaging the corneal wound or touching the endothelium. The suction held the capsule well except for one case. Since the time taken to perform PPC was very small, it did not increase the surgical time than expected.
In case of small pupils, the probe was carefully manoeuvred under the iris edges, using only VEDs for moderate dilation of the pupil. Waltz et al also demonstrated that PPC can be performed in spite of small pupils upto 4 mm in size in adults with or without the use of iris hooks.7 In the current study, PPC was successfully performed in three cases of intumescent cataract and one traumatic cataract in spite of anterior capsular fibrosis and posterior synechiae. The instantaneous 360° creation of capsulotomy and simultaneous aspiration of liquefied cortex prevents any inadvertent tears or Argentinian flag sign in these cases.7 Although the sample size is too small to draw conclusions regarding the safety and efficacy of PPC in small pupils, traumatic and intumescent cataracts, we report favourable initial outcomes in such cases, but further evidence with a larger sample is necessary.
Centration of the PPC probe was achieved based on the surgeon’s experience and was challenging in the initial two eyes with mild inferior decentration due to the learning curve of the surgeon considering the difficult thumb-up holding position of the PPC probe, which is not usual for cataract surgeons. In children, the procedure is performed under general anaesthesia and it is difficult to centre the probe based on patients’ fixation as described in adults.7 The use of Purkinje images has been suggested as a guide to judge the centration of PPC probe.7 Future studies can also be planned using other tools such as ray-tracing for better centration of the PPC.
Properties of PPC capsulotomy
Different techniques have been designed to overcome the difficulties in manual CCC with modest success, such as the two incision push pull technique, that may sometimes result in incomplete capsulotomies with residual tags while vitrectorhexis and diathermy capsulotomies may not be as strong as manual CCC.11 12 PPC produced strong, round, well-centred (95%) and complete capsulotomies (95%) in the current study with no radial tears. Although current technologies like femtosecond capsulotomy have shown promising results in children,13 a few reports of tearing of its capsulotomy edges while dialling the IOL in adults have questioned its strength and integrity.14–16 In animal and human cadaveric eye studies, PPC capsulotomy edge tear strength was found to be three times greater compared with a femtosecond laser capsulotomy and four times higher compared with the manual CCC, which is considered as a gold standard.6 Scanning electron microscopy (SEM) studies of PPC on human cadaveric eyes demonstrated eversion of the anatomical edge of capsulotomy resulting in a smooth continuous functional edge which may explain its higher strength in spite of irregularities seen in the anatomical edge.5 However, an SEM study on surgical cases with radial capsular tears demonstrated a defect and split in the PPC edge with a corresponding focal tag. This led to the hypothesis that these focal tags and frayed collagen fibres, possibly due to dissipated thermal energy, may be the potential point of weakness compared with the smooth edges of manual CCC.8 17
Although initial clinical results of PPC in senile cataracts reported a 100% efficacy with all cases achieving complete capsulotomies without any adverse events,7 later studies have found higher rates of incomplete capsulotomies (72% completion rate), radial tears of its edges (4%)18 19 and structural irregularities with focal tags which have created doubts about the efficacy and strength of PPC.17 Even though the dispersive VEDs may play a vital role in preventing the dissemination of energy to endothelium, a possibility of its incomplete clearance between the nitinol ring and the lens capsule resulting in inadequate apposition, along with their undetermined electrical and thermal conductivity have been postulated to adversely affect the cleavage of the lens capsule. As a result, Mynosys now recommends use of VEDs of 300 000 mPas viscosity or less.18 A soft-shell technique using cohesive VEDs for the capsule and dispersive VEDs for coating the endothelium20 appears to be a reasonable option which can be explored in future studies. Recently, an improved version of PPC with better nitinol ring morphology for more uniform conduction, improved device suction and updated VED recommendations, improved completion rate to 96% but the anterior capsule tears remained high at 4% with irregular edges seen on electron microscopy in adults. All the tears were found to be subincisional, possibly due to persistent focal energy effect or variable suction across the capsule.8 In the current study, we found a 95% completion rate with one failed case using a dispersive VED due to faulty suction with no energy being delivered to the capsule. We did not witness any complication or adverse event intraoperatively as well as postoperatively with no radial tears in spite of irregularities and tags at the PPC edges, possibly due to stronger paediatric lens capsule. Although these tags did not cause any adverse event in our study, one needs to be careful not to engage or pull them during intraoperative instrumentation which may result in tearing of the capsulotomy edge.
PPC has been reported to create capsulotomies in the range of 5.1–5.3 mm in size, in human adult cadaveric eyes (PPC probe size 5.2 mm).5 Rabbit eyes having higher lens capsular elasticity were found to have larger PPC capsulotomy diameter compared with human eyes.5 Similarly, the higher elasticity of paediatric lens capsule might have resulted in slightly larger PPC capsulotomy size than expected (median PPC size=5.45 mm, IQR=5.39–5.75 mm, range=4.82–6.12 mm). Since no adult control group was included in this study, this variability in PPC size could be due to the different measuring techniques used in the two studies (image J software in the current series compared with direct measurement in the human cadaveric eyes). In view of smaller eyes in infants, it is desirable to use a smaller probe size which is currently being developed by Mynosys. It was noticed that a 11-month-old baby had larger PPC size (5.92 mm), possibly due to very high elasticity of an infant lens capsule; however, the efficacy of PPC in infant eyes needs further evaluation. We did not find any association between PPC size and the age of the patient unlike in femtosecond capsulotomy which has shown a significant negative correlation between age of the child and capsulotomy size.13 However, femtosecond laser capsulotomy size can be customised based on the patients’ requirements.
Theoretical safety concerns regarding PPC
Ocular tissue safety is maintained by the silicon cup insulating the nitinol ring, protecting the ocular tissues from the extremely brief electrical nanopulses. Since the cutting of the lens capsule is caused by mechanical cleavage without any cauterisation,10 a minimal rise of 1–2°C in temperature of AC has been noted in animal and human cadaveric eyes, which is not clinically significant.5 They also showed that there was no difference in the amount of morphological endothelial cell damage, corneal transparency, AC cells and flare and posterior capsular opacification (PCO) in the postoperative period between the PPC and the manual CCC groups.5 Although we did not find any significant, unexpected change in corneal transparency, AC reaction or amount of PCO, larger studies with corneal endothelial cell count and morphology are needed to comment on the safety of this technology.
There was no case with preoperative or postoperative zonular weakness/dialysis in the current series. Waltz et al performed a successful PPC on a case with traumatic zonular dialysis of six clock hour with a dense cataract.7 The PPC edges were reported to be strong enough to be held by iris hooks and withstand phacoemulsification stress. No extra zonular movement or stress was found while performing PPC on human cadaveric eyes.5 In paediatric cataract, the additional force required to perform manual CCC may cause additional stress to the existing zonules in a case with zonular weakness, thus making PPC a favourable alternative in such cases.
Specific advantages and disadvantages of PPC in paediatric cataract surgery
Femtosecond capsulotomy is also considered a good automated alternative to manual CCC in paediatric cataract surgery, but it poses some unique challenges such as logistic issues of moving a child from femtosecond room to the cataract theatre under general anaesthesia. Other issues with femtosecond laser include the tremendous rise in IOP on docking the eye, small pupils and corneal opacities hampering the formation of a complete capsulotomy and the extremely high cost of the technology, all of which can be solved using PPC.
The PPC console is smaller than femtosecond laser-assisted cataract surgery unit and can be readily incorporated in an operating theatre. Although the PPC technology is cheaper than that of femtosecond, the disposable probes indeed add to the cost of the surgery. The use of PPC in smaller infant eyes with the current size probe should be cautioned. A smaller size of PPC probe, may add better overlapping of the capsulotomy edges over the IOL with better centration and easier manoeuvring in the AC of smaller eyes. Femtosecond laser has also been shown to be safe and effective in paediatric cataract and can be used to create primary posterior capsulotomy, which is not advisable using PPC as there is no preclinical or clinical evidence about the safety and efficacy of its use in posterior capsulotomy. Since the posterior capsule is concave in shape unlike the flat anterior capsule and is situated very posteriorly, it may be difficult to induce adequate suction. Also, the suction applied may induce traction on the vitreous base with a theoretical possibility of vitreous loss or engaging vitreous into the suction cup possibly leading to retinal tears and detachment. Moreover, with the current size of the PPC probe, it is not possible to guide it under an anterior capsulotomy of 5 mm.
Limitations of this study are the small sample size and a very small subset of data for capsulotomy size (n=9) for our analysis. Only short-term results have been reported since the purpose of the study is to present the operative results; nonetheless, it is a significant limitation. Endothelial cell count with morphology and macular thickness could have added valuable quantitative information regarding the safety of PPC.
To conclude, PPC appears to be a safe, precise and accurate automated technology to obtain a round, well-centred and strong capsulotomy in paediatric cataract surgery within a short follow-up. This procedure may be even more helpful in the hands of beginners and those with little experience in paediatric cataract surgery, empowering them to contribute a greater share in eradicating needless childhood blindness. However, clinical randomised studies comparing its outcomes in paediatric and adult cataracts are needed to evaluate the PPC induced changes in corneal endothelium, AC and posterior segment; size, strength and morphology of the capsulotomy; adverse events; long-term outcomes with the incidence of capsular phimosis and PCO formation rates, against that of femtosecond and manual capsulotomy. While it works very well for intumescent lens, its suitability for capsulotomy in infants needs further validation since it was found that PPC produced a larger capsulotomy in an infant in our study.
Acknowledgments
We thank photography and communication department of LVPEI, Hyderabad
Footnotes
Presented at: Part of this work has been presented at International Strabismological Association(ISA) and American Association for Pediatric Ophthalmology and Strabismus(AAPOS) joint meeting, 18–22 March 2018, Washington DC, USA and World Society for Paediatric Ophthalmology & Strabismus (WSPOS) Subspecialty Day, September 2018, Vienna.
Contributors: PC and RK planned the study. PC was involved in data collection, statistical analysis and drafting of manuscript. RK, AB and VW revised the manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Commissioned; externally peer reviewed.
References
- 1. Fisher RF. The elastic constants of the human lens. J Physiol 1971;212:147–80. 10.1113/jphysiol.1971.sp009315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Fisher RF. The influence of age on some ocular basement membranes. Eye 1987;1:184–9. 10.1038/eye.1987.35 [DOI] [PubMed] [Google Scholar]
- 3. Muralidhar R, Siddalinga Swamy GS, Vijayalakshmi P. Completion rates of anterior and posterior continuous curvilinear capsulorrhexis in pediatric cataract surgery for surgery performed by trainee surgeons with the use of a low-cost viscoelastic. Indian J Ophthalmol 2012;60:144–6. 10.4103/0301-4738.90492 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Jeng BH, Hoyt CS, McLeod SD. Completion rate of continuous curvilinear capsulorhexis in pediatric cataract surgery using different viscoelastic materials. J Cataract Refract Surg 2004;30:85–8. 10.1016/S0886-3350(03)00669-2 [DOI] [PubMed] [Google Scholar]
- 5. Chang DF, Mamalis N, Werner L. Precision pulse capsulotomy: preclinical safety and performance of a new capsulotomy technology. Ophthalmology 2016;123:255–64. 10.1016/j.ophtha.2015.10.008 [DOI] [PubMed] [Google Scholar]
- 6. Thompson VM, Berdahl JP, Solano JM, et al. . Comparison of manual, femtosecond laser, and precision pulse capsulotomy edge tear strength in paired human cadaver eyes. Ophthalmology 2016;123:265–74. 10.1016/j.ophtha.2015.10.019 [DOI] [PubMed] [Google Scholar]
- 7. Waltz K, Thompson VM, Quesada G. Precision pulse capsulotomy: initial clinical experience in simple and challenging cataract surgery cases. J Cataract Refract Surg 2017;43:606–14. 10.1016/j.jcrs.2017.01.023 [DOI] [PubMed] [Google Scholar]
- 8. Hooshmand J, Abell RG, Allen P, et al. . Intraoperative performance and ultrastructural integrity of human capsulotomies created by the improved precision pulse capsulotomy device. J Cataract Refract Surg 2018;44:1333–5. 10.1016/j.jcrs.2018.07.041 [DOI] [PubMed] [Google Scholar]
- 9. Schindelin J, Arganda-Carreras I, Frise E, et al. . Fiji: an open-source platform for biological-image analysis. Nat Methods 2012;9:676–82. 10.1038/nmeth.2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Chang DF. Zepto precision pulse capsulotomy: a new automated and disposable capsulotomy technology. Indian J Ophthalmol 2017;65:1411–4. 10.4103/ijo.IJO_737_17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Andreo LK, Wilson ME, Apple DJ. Elastic properties and scanning electron microscopic appearance of manual continuous curvilinear capsulorhexis and vitrectorhexis in an animal model of pediatric cataract. J Cataract Refract Surg 1999;25:534–9. 10.1016/S0886-3350(99)80051-0 [DOI] [PubMed] [Google Scholar]
- 12. Luck J, Brahma AK, Noble BA. A comparative study of the elastic properties of continuous tear curvilinear capsulorhexis versus capsulorhexis produced by radiofrequency endodiathermy. Br J Ophthalmol 1994;78:392–6. 10.1136/bjo.78.5.392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Dick HB, Schelenz D, Schultz T. Femtosecond laser-assisted pediatric cataract surgery: Bochum formula. J Cataract Refract Surg 2015;41:821–6. 10.1016/j.jcrs.2014.08.032 [DOI] [PubMed] [Google Scholar]
- 14. Abell RG, Davies PEJ, Phelan D, et al. . Anterior capsulotomy integrity after femtosecond laser-assisted cataract surgery. Ophthalmology 2014;121:17–24. 10.1016/j.ophtha.2013.08.013 [DOI] [PubMed] [Google Scholar]
- 15. Abell RG, Darian-Smith E, Kan JB, et al. . Femtosecond laser-assisted cataract surgery versus standard phacoemulsification cataract surgery: outcomes and safety in more than 4000 cases at a single center. J Cataract Refract Surg 2015;41:47–52. 10.1016/j.jcrs.2014.06.025 [DOI] [PubMed] [Google Scholar]
- 16. Chang JSM, Chen IN, Chan W-M, et al. . Initial evaluation of a femtosecond laser system in cataract surgery. J Cataract Refract Surg 2014;40:29–36. 10.1016/j.jcrs.2013.08.045 [DOI] [PubMed] [Google Scholar]
- 17. Hooshmand J, Abell RG, Goemann K, et al. . Ultrastructural integrity of human Capsulotomies created by a thermal device. Ophthalmology 2018;125:340–4. 10.1016/j.ophtha.2017.09.018 [DOI] [PubMed] [Google Scholar]
- 18. Hooshmand J, Abell RG, Allen P, et al. . Thermal capsulotomy: initial clinical experience, intraoperative performance, safety, and early postoperative outcomes of precision pulse capsulotomy technology. J Cataract Refract Surg 2018;44:355–61. 10.1016/j.jcrs.2017.12.027 [DOI] [PubMed] [Google Scholar]
- 19. Kelkar JA, Mehta HM, Kelkar AS, et al. . Precision pulse capsulotomy in phacoemulsification: clinical experience in Indian eyes. Indian J Ophthalmol 2018;66:1272–7. 10.4103/ijo.IJO_146_18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Arshinoff SA. Dispersive-cohesive viscoelastic soft shell technique. J Cataract Refract Surg 1999;25:167–73. 10.1016/S0886-3350(99)80121-7 [DOI] [PubMed] [Google Scholar]