Abstract
Introduction:
Although prior clinical and population-based studies have demonstrated comorbidity between mood and alcohol use disorders (AUD), there is a paucity of research assessing whether mood disorders predict transition across stages of alcohol involvement.
Method:
Hypothesizing that mood disorders predict transition across sex-specific alcohol involvement stages, we used prospective data from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC), a nationally representative survey of US adults, which included male (n=14,564) and female (n=20,089) participants surveyed in 2001–2 and re-interviewed in 2004–5. Latent class (LCA) and latent transition analyses (LTA) were used to assess patterns of alcohol involvement in the US, and the association of lifetime mood disorders at baseline with transition across stages of alcohol involvement during follow-up.
Results:
A three-class model of AUD criteria was identified (No problems, Moderate problems and Severe problems) for both males and females. Positive cross-sectional associations between mood disorder and problem classes of alcohol involvement were found among both sexes, as were positive longitudinal associations. Propensity score adjustment mitigated the associations of baseline mood disorder with progressive transition for both sexes. However, among females, baseline mood disorder was consistently associated with reduction in remission from Severe to Moderate alcohol problems (aOR=0.30, CI=0.09–0.99, p=0.048) over time.
Discussion:
Our study provides evidence that mood disorders impact transition through stages of alcohol involvement, most strongly associated with hindering remission among females. Findings advance our understanding of these comorbid relationships and have clinical implications for ongoing assessment of drinking patterns among individuals with mood disorders.
Keywords: abuse, alcohol, dependence, depression, mood, risk, latent transition analysis, major depressive disorder
1. Introduction
The co-occurrence of alcohol and mood disorders is well recognized in community and clinical populations (Farell et al., 2001; Frye et al., 2003; Gilman and Abraham, 2001; Grant et al., 2004, 2015; Hasin et al., 2005; Johnson et al., 2007; Kessler et al., 1997; Lai et al., 2012; Ross, 1995; Wang and Patten, 2001). Alcohol disorders are more commonly the initial (primary) condition (Fergusson et al., 2009; Flensborg-Madsen et al., 2009), yet prospective data indicate that these associations can be bidirectional (Briere et al., 2014; Dawson et al., 2010; Flensborg-Madsen et al., 2009; Gilman and Abraham, 2001; Kuo et al., 2006; Needham, 2007; Pacek et al., 2013; Wang and Patten, 2001, 2002). Although comorbid patterns are frequently reported, there has been relatively little assessment of whether mood disorders predict transition across stages of alcohol involvement. Some studies provide evidence that mood conditions have varying associations with different classifications of alcohol outcomes (e.g., incidence as opposed to relapse) (Behrendt et al., 2011; Boschloo et al., 2012; Conway et al., 2016; Crum et al., 2001; Mattisson et al., 2007). However, most prior studies examining alcohol transitions have assessed associations across one stage and/or in one direction (e.g., no drinking to drinking initiation) (Behrendt et al., 2011; Butterworth et al., 2014; Crum et al., 2001; Martins et al., 2011; Sung et al., 2004). With relatively few exceptions (Cook et al., 2014; Windle and Davies, 1999), there has been little assessment of transitions in multiple directions across more than one stage, especially for comorbid relationships.
An individual’s involvement with alcohol may progress through sequential stages, with progressively maladaptive drinking patterns. However, not everyone progresses through stages sequentially. Some individuals may remain chronically at the same stage for years. Others may undergo remission to less involved stages. Evaluating whether mood disorders impact progression to and/or remission from more severe alcohol involvement aids our understanding of possible etiologic mechanisms for this comorbidity, and may identify potential targets for prevention or early intervention, as well as determine at which alcohol stage mood symptoms have the strongest impact.
Hypothesizing that mood disorders increase the probability of transition to more advanced alcohol involvement stages, our principal goals were to examine whether, and at what stages, baseline mood disorders impact transition through increasingly progressive stages of alcohol involvement, and to assess the possibility of progressing to advanced stages directly without passing through an intervening stage (Bucholz et al., 2000). We also sought to examine whether mood disorders were associated with inhibiting remission to less severe alcohol involvement. Our goal was to examine patterns of alcohol involvement across the entire spectrum of drinking behavior in the US, and consequently our study sample included individuals who reported no consumption and/or no alcohol-related problems. Our rationale was that these individuals may have remitted from a prior alcohol disorder, or may transition to problematic drinking, particularly in the context of mood symptomatology. Furthermore, those with more severe behavior may remit to abstinence and/or non-problematic consumption. Because prior studies have found that the impact of comorbidity may differ for males and females (Frye et al., 2003; Kessler et al., 1997; Kuo, et al., 2006; Ross, 1995; Wang and Patten, 2001), all of our analyses were stratified by sex.
2. Methods
2.1. Study sample
The study sample was drawn from waves 1 and 2 of the National Epidemiological Survey on Alcohol and Related Conditions (NESARC), a representative survey of the US adult population. Wave 1 was fielded in 2001–2002 (n=43,093 participants, aged ≥18 years). Of the 39,959 wave 2 eligible participants, a total of 34,653 were re-interviewed in 2004–2005. Ineligible respondents included those deceased, deported, mentally/physically impaired, or on active military duty. Response rates for wave 1 and eligible wave 2 surveys were 81% and 87%, respectively. Additional survey and study design details are described elsewhere (Grant et al., 2004, 2009). Our study sample included 14,564 males and 20,089 females with assessments at both waves, and was weighted to adjust for unequal probabilities of selection to provide nationally representative estimates.
2.2. Measures
Baseline characteristics were assessed using wave 1 data. Mood disorders included the independent diagnoses (major depression, dysthymia, mania, hypomania), and excluded those solely due to substance-induced intoxication and/or withdrawal, or medical illnesses. Diagnoses were based on DSM-IV criteria ascertained from computerized algorithms using data from the Alcohol Use Disorder and Associated Disabilities Interview Schedule–DSM-IV Version (Grant et al., 2003; Ruan et al., 2008). Baseline lifetime mood disorder was the hypothesized predictor of alcohol involvement transition. Because each independent mood disorder, whether 12-month or lifetime, had similar associations with alcohol involvement stages, they were combined to increase precision of estimates. As we have accomplished previously (La Flair et al., 2012, 2013), alcohol involvement was captured via items assessing clinical features of DSM-IV alcohol abuse and dependence, which were operationalized as four abuse and seven dependence criteria. Therefore, alcohol involvement refers to behaviors related to AUD criteria, and not to consumption level. Consistent with the approach adopted in DSM-V and prior latent class analyses (Ehlke et al., 2012; La Flair et al., 2012, 2013; Muthén, 2006), abuse and dependence criteria were not separated.
Potential confounders in the analyses included sex (analyses were sex-stratified), age (18–35, 36–49, ≥50 years; continuous in multivariable analyses), race/ethnicity (non-Hispanic White, non-Hispanic Black, Hispanic, and other), education (≥12 years, <12 years), lifetime illicit drug abuse and/or dependence (heroin, other narcotics, cocaine, cannabis, stimulants, hallucinogens), nicotine dependence, anxiety disorders (generalized anxiety disorder, social phobia, specific phobia, and/or panic disorder), and family history of alcoholism (any first-degree relative reported as “alcoholic or problem drinker”).
2.3. Statistical analyses
We first completed latent class analysis (LCA) on the eleven DSM-IV abuse and dependence criteria. LCA is a data-driven approach that allowed us to characterize patterns of clinical features of AUD observed in our data that may manifest prior to meeting full criteria for AUD or may represent qualitatively different subtypes (e.g., stages). The goal of LCA is to identify the smallest number of latent classes that adequately describe the associations among the clinical features. Information about the class structure is conveyed by the proportion of individuals in each class (latent class prevalences), and the probability of reporting a clinical feature within a class (item probabilities). We fit successive models with increasing numbers of latent classes to determine the most parsimonious model that provided an adequate fit to the data (Nylund et al., 2007). Model selection was based on Akaike’s information criterion (AIC), Bayesian information criterion (BIC) and the sample-size adjusted BIC (a-BIC): global fit indices that combine goodness-of-fit and parsimony. Models with lower values of AIC, BIC and a-BIC are preferred. Because of the large sample size, we have increased power to detect smaller classes, which could result in identification of spurious classes that lack substantive interpretation. Thus, in addition to global fit indices, interpretability and distinguishability of the resultant classes was considered when comparing competing latent class models. Entropy was used to measure the separation of classes, with values approaching 1.0 indicating clearer delineation of classes (Celeux and Soromenho, 1996). To avoid convergence to local maxima, which occurs frequently in LCA, results were based on 10,000 sets of random starting values, each of which was subjected to ten iterations of the estimation procedure. LCA was completed separately for waves 1 and 2 to evaluate alcohol involvement classes at each wave. Based on previous findings of sex differences for AUDs (Grucza et al., 2008; Keyes et al., 2010), models were fit separately for males and females.
Next, we estimated the probability of transitioning between the latent stages of alcohol involvement across the two waves using latent transition analysis (LTA). LTA is an extension of LCA to the longitudinal framework, which expresses change over time in terms of transition probabilities and models the impact of covariates on transitions using a multinomial regression formulation. Transition probabilities reflect the probability of transitioning from a latent stage at wave 1 to another latent stage at wave 2 (Collins and Wugalter, 1992; Reboussin et al., 1998, 1999). Using LTA, we assessed our hypothesis that baseline mood disorder impacted the probability of progressive transition from one alcohol involvement stage to a more advanced stage. Simultaneously, we assessed whether baseline mood disorder was associated with a reduced probability of remission to a less symptomatic alcohol involvement stage.
We utilized the propensity score method of inverse probability of treatment weighting (IPTW) to address potential baseline differences between mood disordered and non-mood disordered participants, which could bias the effect estimates (Curtis et al., 2007; Rubin, 2010; Stuart, 2010). In this technique, first, propensity scores (probability of mood disorder) are computed using a logistic regression model. These scores reflect each participant’s likelihood of having a mood disorder given their sociodemographic and clinical characteristics. The potential confounding baseline sociodemographic and clinical characteristics included in the propensity score model are listed in Table 1. Next, data are weighted by their inverse probability of being in their observed group (those with and without mood disorders). Because the NESARC used a complex sampling design, both LCA and LTA were carried out using Mplus version 7.0 (Muthén and Muthén, 1998–2010) taking into account survey weights, clustering and stratification. The propensity score weights were multiplied by the survey weights and the resulting combined weights were used in the analysis of the association of mood disorder with transitions in alcohol involvement stages (Dugoff et al., 2014). To assess the effectiveness of IPTW in balancing the composition of mood disorder and non-mood disordered groups, we compared characteristics of the group before and after applying the weights (Stuart, 2010). Application of IPTW was deemed successful as the groups were similar with respect to the observed characteristics after using the weights.
Table 1.
Characteristics of the study sample: male (n=14,564) and female (n=20,089) participants by a history of DSM-IV mood disorders at baseline; NESARC, wave 1.
| Characteristics at baseline |
Males |
Females |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total Males | Mood disorder |
Total Females | Mood disorder |
|||||||||||
| Absent | Present | p-valuea | Absent | Present | p-valuea | |||||||||
| N | % | N | % | N | % | N | % | N | % | N | % | |||
| Age (years): | ||||||||||||||
| 18–35 | 4536 | 34.5 | 3695 | 33.4 | 841 | 40.8 | <0.0001 | 6379 | 32.2 | 4707 | 31.2 | 1672 | 35.7 | <0.0001 |
| 36–49 | 4533 | 30.0 | 3751 | 29.6 | 782 | 32.2 | 5716 | 28.7 | 4193 | 27.6 | 1523 | 32.3 | ||
| 50+ | 5495 | 35.5 | 4814 | 37.0 | 681 | 26.9 | 7994 | 39.0 | 6411 | 41.2 | 1583 | 32.0 | ||
| Race/ethnicity: | ||||||||||||||
| White | 9090 | 73.1 | 7489 | 72.1 | 1601 | 78.4 | <0.0001 | 11605 | 72.5 | 8489 | 70.6 | 3116 | 78.6 | <0.0001 |
| Black | 2281 | 9.8 | 2003 | 10.2 | 278 | 8.0 | 4206 | 11.7 | 3438 | 12.6 | 768 | 8.8 | ||
| Hispanic (any race?) | 2718 | 12.3 | 2357 | 12.8 | 361 | 9.1 | 3638 | 10.9 | 2861 | 11.5 | 777 | 9.0 | ||
| Other | 475 | 4.8 | 411 | 4.9 | 64 | 4.5 | 640 | 4.9 | 523 | 5.3 | 117 | 3.6 | ||
| Education (years): | ||||||||||||||
| <12 | 2356 | 14.8 | 2008 | 14.8 | 348 | 14.9 | 0.8367 | 3388 | 14.5 | 2652 | 14.8 | 736 | 13.6 | 0.0009 |
| ≥12 | 12208 | 85.2 | 10252 | 85.2 | 1956 | 85.1 | 16701 | 85.5 | 12659 | 85.2 | 4042 | 86.4 | ||
| Mood disorderb: | ||||||||||||||
| Major depressive disorder | 1798 | 11.8 | 1798 | 77.5 | NA | 4206 | 20.9 | 4206 | 89.0 | NA | ||||
| Dysthymia | 458 | 3.0 | NA | NA | 458 | 19.4 | 1119 | 5.3 | NA | NA | 1119 | 22.5 | ||
| Mania | 462 | 3.1 | 462 | 14.8 | 710 | 3.5 | 710 | 20.4 | ||||||
| Hypomania | 375 | 2.5 | 375 | 16.6 | 481 | 2.2 | 481 | 9.4 | ||||||
| Anxiety disorderb: | ||||||||||||||
| GADc | 418 | 2.8 | 105 | 0.9 | 313 | 13.5 | <0.0001 | 1075 | 5.4 | 269 | 1.5 | 806 | 18.0 | <0.0001 |
| Panic disorder | 496 | 3.3 | 201 | 1.7 | 295 | 12.4 | <0.0001 | 1294 | 6.7 | 481 | 3.4 | 813 | 17.4 | <0.0001 |
| Social phobia | 625 | 4.3 | 313 | 2.6 | 312 | 13.2 | <0.0001 | 1096 | 5.8 | 410 | 2.8 | 686 | 15.5 | <0.0001 |
| Specific phobia | 951 | 6.3 | 582 | 4.5 | 369 | 16.2 | <0.0001 | 2456 | 12.4 | 1365 | 8.7 | 1091 | 24.3 | <0.0001 |
| Non-alcohol drug use disorderb | ||||||||||||||
| Illicit drugsd | 1967 | 13.6 | 1278 | 10.6 | 689 | 30.6 | <0.0001 | 1376 | 7.0 | 672 | 4.4 | 704 | 15.4 | <0.0001 |
| Nicotine | 2731 | 19.6 | 1884 | 16.4 | 847 | 37.5 | <0.0001 | 2965 | 15.4 | 1625 | 11.1 | 1340 | 29.6 | <0.0001 |
| Family history of alcoholism: | ||||||||||||||
| Absent | 10197 | 70.6 | 8923 | 73.2 | 1274 | 55.6 | <0.0001 | 13107 | 66.0 | 10646 | 70.3 | 2461 | 51.9 | <0.0001 |
| Present | 4367 | 29.4 | 3337 | 26.7 | 1030 | 44.4 | 6982 | 34.0 | 4665 | 29.7 | 2317 | 48.1 | ||
Rao-Scott chi-square tests of difference.
Diagnostic categories are not mutually exclusive.
GAD, generalized anxiety disorder.
Includes lifetime history of abuse and/or dependence on non-alcohol substances: heroin, other opioids, cocaine, cannabis, stimulants, and/or hallucinogens.
3. Results
Table 1 includes the frequency distribution of baseline characteristics for our study sample by sex. Approximately 31% of study participants were in the 18–35 year age range, 30% in the 36–49 range, and 39% were 50 years or older. Most were White with at least a high school education. Lifetime major depressive disorder was present in 21% of females and 12% of males; 9% of males and 11% of females had another mood disorder. A greater proportion of females reported family history of alcoholism, and met criteria for anxiety disorders. More males had illicit drug use disorder and nicotine dependence. Those with mood disorders were more likely to be younger, White, have an anxiety or drug use disorder, and have a family history of alcoholism. Females with mood disorders also were more likely to have less education, although the magnitude of these differences was minimal.
3.1. Latent class analyses
We chose a three-class model for each sex, based on data from the fit indices and overall interpretability of the models. As shown in Table 2, for females, the fit indices and entropy generally favored a three-class model for waves 1 and 2. For males, the fit indices and entropy initially suggested a four-class model, similar to prior LCA (Muthén, 2006). A five-class solution did not converge. In the four-class solution, prevalence of the fourth class was relatively low (0.7% at wave 1, 0.8% at wave 2), and the two moderate/middle classes had similar profiles with no distinguishing items between them, limiting clinical interpretability. Consequently, the more parsimonious and interpretable three-class model was used in the LTA for males.
Table 2.
Fit statistics for latent class models of alcohol involvement by sex and NESARC wave.
| No. of Classes | AICa | BICb | a-BICc | Entropyd | |
|---|---|---|---|---|---|
| Males Wave 1 | |||||
| 1 | 63030 | 63113 | 63078 | 1.00 | |
| 2 | 48914 | 49088 | 49015 | 0.94 | |
| 3 | 47538 | 47804 | 47692 | 0.90 | |
| 4 | 47374 | 47731 | 47582 | 0.88 | |
| Males Wave 2 | |||||
| 1 | 68159 | 58243 | 68207 | 1.00 | |
| 2 | 53588 | 53762 | 53689 | 0.90 | |
| 3 | 51651 | 51916 | 51805 | 0.88 | |
| 4 | 51370 | 51726 | 51577 | 0.86 | |
| Females Wave 1 | |||||
| 1 | 50097 | 50184 | 50149 | 1.00 | |
| 2 | 39013 | 39195 | 39122 | 0.95 | |
| 3 | 38002 | 38279 | 38168 | 0.94 | |
| 4 | 37957 | 38328 | 38179 | 0.90 | |
| Females Wave 2 | |||||
| 1 | 52331 | 52417 | 52383 | 1.00 | |
| 2 | 40722 | 40904 | 40831 | 0.94 | |
| 3 | 39586 | 39683 | 39751 | 0.92 | |
| 4 | 39444 | 39816 | 39666 | 0.92 |
AIC: Akaike’s Information Criterion. Lower values represent better fit.
BIC: Bayesian Information Criterion. Lower values represent better fit.
a-BIC: sample-size adjusted Bayesian Information Criterion. Lower values represent better fit.
Values closer to 1 indicated better separation of classes
The alcohol involvement item probabilities for the three classes at waves 1 and 2 are presented in Figure 1A (males) and 1B (females). These classes reflect increasing alcohol involvement stages. Most individuals were categorized into a No problem class, experiencing few clinical criteria: prevalence estimates among females were 92% (wave 1) and 90% (wave 2); among males, they were 86% (wave 1) and 80% (wave 2). A second or Moderate problem class was also similar across the sexes and was characterized by drinking in hazardous situations, problems cutting down consumption, drinking in larger amounts and experiencing tolerance and withdrawal symptoms: estimated prevalence among females was 7% (wave 1), and 9% (wave 2), with a slightly higher prevalence among males (12% at wave 1, 17% at wave 2). The third or Severe problem class, again was similar for females and males, with higher item probabilities than the Moderate class in addition to other drinking-related criteria: role failure and social problems, giving up activities, greater time spent getting alcohol, physical and psychiatric problems. Severe class prevalence estimates were lowest overall, but were lower among females (1.0% (wave 1), 1.1% (wave 2)), compared with males (2.5% (wave 1), 2.8% (wave 2)). Although small differences in item probabilities existed between the waves, the overall qualitative interpretations of the three classes across waves did not change. Therefore, measurement invariance was imposed across waves to ensure that the mean of the latent classes was held constant.
Figure 1.
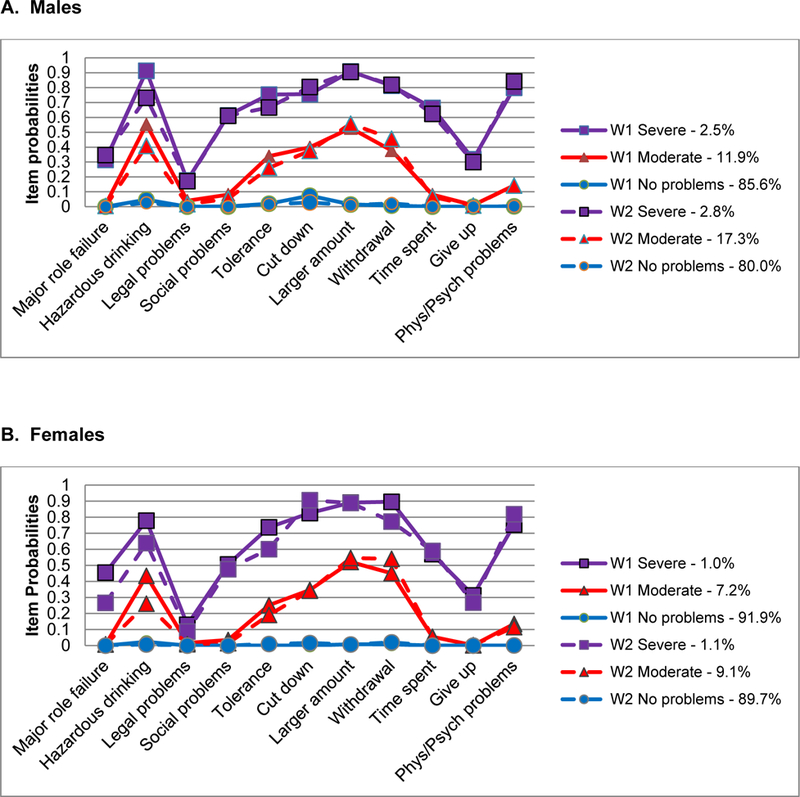
Alcohol involvement item probabilities and class prevalence estimates from the three class model for A) males (n=14,564) and B) females (n=20,089) based on latent class analyses of data from the NESARC, waves 1 and 2.
In supplementary analyses, to confirm that sex-stratified analyses were appropriate, we tested whether the structure of the 3-class model varied for males and females. Measurement invariant testing suggested that pooling data for men and women would lead to a significantly worse model fit (likelihood difference test statistic=276.84, p<0.001, and 182.25, p<0.001 for waves 1 and 2, respectively). To identify the AUD criteria within a class that were driving the sex differences, we tested the invariance of each latent class indicator for each wave. We found 12 of the 33 indicators were significantly different at p<0.05 for wave 1, and 9 were significantly different at wave 2 (see Appendix). For example, males had significantly higher conditional probabilities for drinking in physically hazardous situations, and development of tolerance.
3.2. Latent transition analyses
We first examined the overall estimated probabilities of transitioning between the three classes across waves (Figure 2), adjusting for sampling weights. The highest stability was seen for those without problems: 93% of females and 90% of males in the No problem stage at baseline remained in this stage at follow-up. Notably, 65% of females and 56% of males in the Severe stage at baseline reported fewer alcohol criteria at follow-up (remitting to Moderate or No problems stages). A low proportion of females (0.8%) skipped an intervening stage, and transitioned from No problems to Severe problems. For males, 9% transitioned from Moderate to Severe stages compared with 1% that transitioned from No problems to Severe. Although there was greater probability for symptom improvement than symptom progression, males were less likely to recover than females. A greater proportion of males in the Severe (44%) stage remained at that stage without symptom improvement compared with 35% of females. A greater proportion of females in the Moderate stage remitted to No problems compared to males (35% and 24%, respectively).
Figure 2.
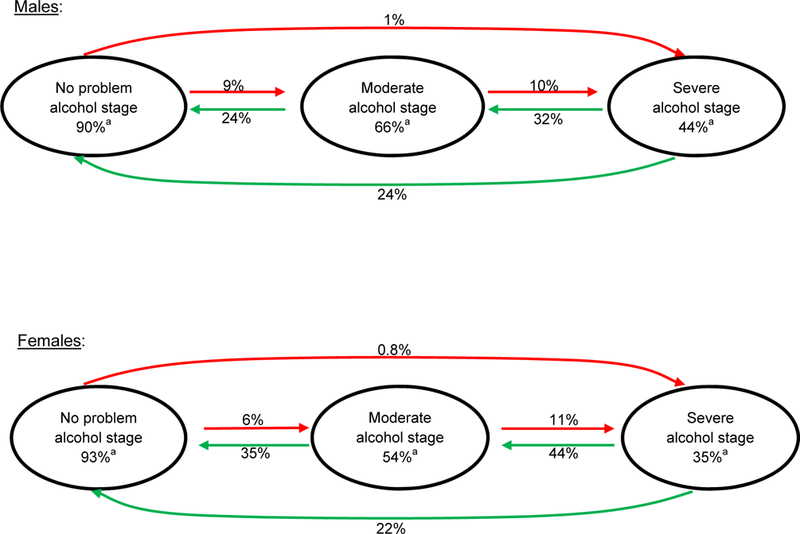
Probability of transitioning across stages of alcohol involvement during follow-up for males (n=14,564) and females (n=20,089); data from NESARC, waves 1 and 2; data adjusted by sampling weights.
a Percentages in the circles represent the proportion of individuals at a specific alcohol involvement stage at baseline that remained in the same stage at follow-up. For example, 90% of males in the No problem stage remained at that stage.
Second, we examined the cross-sectional association of lifetime mood disorder at baseline with baseline alcohol involvement stages (Table 3), with and without adjustment using the method of propensity score weighting. Findings were similar among men and women: mood disorder was significantly associated with both Moderate and Severe stages, relative to the No problem stage. These findings remained significant after adjustment for potential confounding except for the association of mood disorder and the Moderate stage among males.
Table 3.
Cross-sectional association of lifetime mood disorders at baseline with alcohol involvement stages among males and females at baseline; NESARC, wave 1.
| Alcohol involvement stage | Mood disordera | |
|---|---|---|
| Unadjusted ORb (95% CI)c, p-value | Propensity Score Adjustedd ORb (95% CI)c, p-value | |
| Males | ||
| Severe | 5.89 (4.42–7.85), <0.001 | 2.58 (1.75, 3.81), <0.001 |
| Moderate | 2.05 (1.72–2.45), <0.001 | 1.13 (0.92, 1.39), 0.250 |
| No problems | Reference | |
| Females | ||
| Severe | 5.82 (4.00–8.49), <0.001 | 1.96 (1.27–3.06), 0.001 |
| Moderate | 2.20 (1.88–2.58), <0.001 | 1.32 (1.10–1.59), 0.003 |
| No problems | Reference | |
Mood disorder includes a lifetime diagnosis of DSM-IV major depressive disorder, dysthymia, mania, or hypomania at the time of the baseline interview.
OR, odds ratio.
95% CI, confidence interval.
Propensity score models include age, race-ethnicity, educational level, family history of alcoholism, and the history of lifetime anxiety, nicotine, and non-alcohol drug use disorders.
Third, we assessed the longitudinal associations between mood disorders and transitioning across alcohol stages. The odds ratios presented in Table 4 correspond to the odds of transitioning between alcohol involvement stages from wave 1 to 2 relative to staying at the same stage for those with and without a mood disorder. In unadjusted analyses, we found positive progressive longitudinal associations from Moderate to Severe stages among males and No Problems to Moderate stages among females, and a negative association with remission from Severe to Moderate involvement among females. After adjustment for potential confounders using propensity score weighting, among females, mood disorder was associated with elevated odds for movement from the No problems to Severe stage at follow-up, but was not statistically significant (adjusted odds ratio (aOR)=2.16, 95% confidence interval (CI)=0.81–5.76, p=0.123). Similarly, among males in adjusted models, baseline mood disorder was associated with an almost two-fold increased odds of transitioning from Moderate to Severe stage relative to males who remained at the Moderate stage (aOR=1.73, CI=0.82–3.66, p=0.153), but was not statistically significant. There was no evidence that mood disorder increased the probability of progression from No problems to Moderate problems for either sex. Among females, mood disorder was negatively associated with remission. Women with a mood disorder history and Severe problems at baseline were significantly less likely to transition to Moderate problems during follow-up (aOR=0.30, CI=0.09, 0.99 p=0.048) relative to women without a mood disorder. Mood disorders had no appreciable associations with remission transitions among males.
Table 4.
The association of lifetime mood disorder at baseline with transitions in alcohol involvement stage at follow-up by sex; data are from the NESARC, waves 1 and 2.
| Transition direction | Mood Disorders with Transitions in Alcohol Involvement Stages | |||
|---|---|---|---|---|
| Males | Females | |||
| Unadjusted ORa (95% CI)b, p-value | Propensity Score Adjustedc ORa (95% CI)b, p-value | Unadjusted ORa (95% CI)b, p-value | Propensity Score Adjusteda ORa (95% CI)b, p-value | |
| Progression | ||||
| No Problems to Moderate | 0.91 (0.67, 1.24) p=0.569 | 0.73 (0.51, 1.04) p=0.084 | 1.34 (1.06, 1.69) p=0.015 | 0.85 (0.65, 1.11) p=0.243 |
| No Problems to Severe | 1.20 (0.52, 2.74) p=0.669 | 0.89 (0.26, 3.08) p=0.851 | 1.39 (0.67, 2.91) p=0.376 | 2.16 (0.81, 5.76) p=0.123 |
| Moderate to Severe | 2.08 (1.26, 3.42) p=0.004 | 1.73 (0.82, 3.66) p=0.153 | 1.25 (0.77, 2.05) p=0.368 | 1.23 (0.66, 2.30) p=0.508 |
| Remission | ||||
| Moderate to No Problems | 1.39 (0.91, 2.13) p=0.127 | 1.45 (0.89, 2.35) p=0.132 | 1.36 (0.90, 2.04) p=0.148 | 0.90 (0.57, 1.40) p=0.625 |
| Severe to No Problems | 0.85 (0.45, 1.62) p=0.633 | 0.74 (0.27, 2.02) p=0.560 | 0.64 (0.28, 1.47) p=0.293 | 0.52 (0.12, 2.18) p=0.367 |
| Severe to Moderate | 1.51 (0.75, 3.03) p=0.251 | 1.54 (0.54, 4.40) p=0.417 | 0.43 (0.19, 0.98) p=0.045 | 0.30 (0.09, 0.99) p=0.048 |
OR, odds ratio. Odds ratios represent the odds of a mood disorder being associated with transitioning between the specific alcohol involvement stages relative to the odds of staying in the same stage.
95% CI, confidence interval.
Propensity score models include age, race-ethnicity, educational level, family history of alcoholism, and the history of lifetime anxiety, nicotine dependence, and non-alcohol drug use disorders.
4. Discussion
There is a relative paucity of prior studies that have examined transition patterns across stages of alcohol involvement in the general population. Bypassing the limitations inherent in defining individuals in the community as having or not having an AUD, we aimed to provide a broader understanding of the spectrum of alcohol involvement in the US, by assessing classes of criteria used to define an AUD. In addition, our goal was to provide information on transition patterns of drinking behavior among the entire national sample including those who report no drinking or no alcohol-related problems, hypothesizing that these individuals may transition to more problematic behavior, and those in more severe stages may remit to abstinence or non-problematic consumption.
Three classes of alcohol involvement were identified both for men and women. Most individuals fall within the No problems class, and the majority of these individuals remain in this class over time. This class structure is similar to LCA of AUD symptoms using other samples (Mancha et al., 2012; Swift et al., 2016). Consistent with our a priori hypotheses, having a mood disorder diagnosis at baseline, was associated with the problem classes of alcohol involvement. Mood disorder was strongly associated with the cross-sectional alcohol stages, and with some sex-specific longitudinal transitions across stages. The association of mood disorders with the progressive transition through worsening stages of alcohol involvement was mitigated once propensity score adjustment was completed. However, among women, mood disorders continued to have a strong independent association with inhibiting remission from Severe to Moderate problems even after controlling for confounding.
Associations of mood symptoms with alcohol disorders have been reported repeatedly in prior investigations (Blanco et al., 2010; Boschloo et al., 2012; Cranford et al., 2011; Edwards et al., 2011; Grant et al., 2003, 2004; Kessler et al., 1997; Marmorstein, 2009; Prisciandaro et al., 2012; Young-Wolff et al., 2009). However, with few exceptions (e.g, McBride et al., 2014), there has been relatively little assessment of mood conditions with specific transitions through alcohol involvement stages. One advantage of the methodology used in this report is the simultaneous assessment of the direction and magnitude of transitions across empirically-derived stages of alcohol involvement and our ability to examine the associations of mood disorder with stage-specific transitions. Although in cross sectional analyses, mood disorders continued to be associated with alcohol stages after controlling for confounding among both men and women, this was not found in the progressive longitudinal transitions. While an initial association was found in unadjusted models in the longitudinal transition from moderate to severe problems for men and from no problems to moderate problems for women, confounding characteristics (such as substance use involvement) explained these associations. Furthermore, it is likely that adults who initially are without drinking problems or those within a more moderate stage of alcohol involvement are more able to cope with the mood symptoms and therefore less likely to transition to more severe problematic drinking as a result of mood symptoms. Also, the cross-sectional comorbid associations well documented in prior literature may be plausibly explained by the reverse directional pathway (alcohol problems causing the development or worsening of mood symptoms) as has been found in some prior studies (Fergusson et al., 2009; Flensborg-Madsen et al., 2009). These potential etiological mechanisms need to be assessed in future investigations.
An additional important finding from the current report was the longitudinal association between baseline mood disorders and the inhibition of remission of alcohol-related problems among women. A number of prior reports indicate that individuals with comorbid disorders, compared to those with a single diagnosis, have more severe prognostic outcomes such as higher relapse rates, greater risk for treatment dropout and more severe symptoms (Britton et al., 2015; Curran et al., 2000; Driessen et al., 2001; Greenfield et al., 1998; Prisciandaro et al., 2012; van Zaane et al., 2010). This highlights the importance of recognizing maladaptive drinking behavior among patients with mood disorders, and educating patients about risks of consuming alcohol, such as might occur if used as a mechanism for self-medicating mood symptoms (Bolton et al., 2009; Crum et al., 2013; Khantzian, 1990). In this report, the negative association of mood disorder with alcohol problem remission was only found for women. Women may be more vulnerable to the comorbid presence of mood symptoms and problematic drinking behavior. Some prior studies report stronger comorbid associations among women (Husky et al., 2008; Kessler et al., 1997; Ross, 1995). Furthermore, mood symptom severity or duration may be greater among females, given the higher prevalence of depressive disorders among women in general (Van de Velde et al., 2010; Weissman et al., 1996). Dawson and colleagues found that internalizing psychopathology was significantly more prevalent among women with lifetime alcohol dependence than was found for men (Dawson et al., 2010). Service utilization and treatment outcome also may differ by sex for those with comorbid conditions (Chen et al., 2013; Dawson et al., 2010; Farren et al., 2011), which may reflect differences in mental health care access, presence of refractory symptoms or limited response to available treatment.
The findings of this report should be considered in the context of potential limitations. First, we were unable to adjust for all possible confounding characteristics. For example, alcohol expectancies may motivate drinking behavior (Hasking et al., 2011; Jones et al., 2001; Smith, 1994), and be affected by mood state (Demmel et al., 2006; Catanzaro and Laurent, 2004). Second, although the dataset is the largest prospective population-based US survey that provides detailed alcohol and psychiatric symptom data needed for the analyses, multiple transition patterns are assessed and power is limited to evaluate some associations, including those for specific mood diagnoses. Additionally, there were relatively few transitions during the follow-up interval. Whether three years is sufficient time to assess all transitions will need further exploration in samples with longer follow-up. Third, although health services data was gathered, information on the extent and timing of service utilization related to comorbid symptoms was not available to assess potential treatment response. Furthermore, treatment utilization was limited: 34.5% of females and almost half of males (46.5%) with mood disorders reported no mood or alcohol treatment during follow-up. Inclusion of this treatment variable, as a covariate in the propensity score adjusted regression model, did not appreciably alter the estimates presented in this report. Lastly, due to limitations in prevalence, lifetime mood disorder was used. This strategy may make it more difficult to interpret the temporal relationships with the alcohol stages. However, similar associations with alcohol stages were found for both lifetime and 12-month diagnoses. Furthermore, approximately half of those with lifetime mood disorder at baseline also met criteria for 12-month mood disorder.
Notwithstanding these limitations, the current report provides new information regarding the potential impact of mood disorders on the progression and remission of alcohol-related problems. Mood disorders may have significant effects on the probability of transitioning through alcohol stages, particularly on remission from severe problems among women. The findings emphasize the importance of ongoing assessments of drinking patterns among individuals with mood disorders, the evaluation of mood symptoms among individuals with drinking problems, as well as the need to educate patients with mood disorders about the risks of maladaptive drinking behaviors and provide alternative coping strategies. Further research will be needed to explore transition patterns over longer intervals given that an interval of approximately three years may not be sufficient to reveal all transition patterns. In addition, it will be necessary to explore the etiological mechanisms for the sex-specific findings, and the role of health service use in accelerating or diminishing the pace of transitions.
Acknowledgements:
The analyses and preparation of this project were supported by grants from the National Institute on Alcohol Abuse and Alcoholism (AA016346), and the National Institute on Drug Abuse (DA030460). Preparation of this paper also was supported by a Johns Hopkins School of Medicine Clinician Scientist Award (AA), and by a T32 (DA007292) (NK, KT) from the National Institute on Drug Abuse. Dr. Mojtabai has received consulting fees and research funding from Bristol-Myers Squibb and Ludbeck pharmaceuticals. Other authors report no conflicts of interest. Dr. Rosa M. Crum had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Drs. Kerry Green and Beth Reboussin performed the statistical analyses for this study.
Appendix.
Male-female invariance testing for the 3-class model of NESARC wave 1 and wave 2 alcohol use disorder criteria: conditional probabilities and p-values.
| Wave 1 | Wave 2 | |||||
|---|---|---|---|---|---|---|
| No Problems Class | Males | Females | p | Males | Females | p |
| Major Role Failure | 0.000 | 0.000 | 1.000 | 0.000 | 0.000 | 1.000 |
| Physically Hazardous | 0.047 | 0.024 | 0.000 | 0.026 | 0.007 | 0.000 |
| Legal Problems | 0.000 | 0.000 | 0.614 | 0.000 | 0.000 | 0.363 |
| Social/Interpersonal Problems | 0.001 | 0.000 | 0.542 | 0.000 | 0.000 | 1.000 |
| Tolerance | 0.012 | 0.006 | 0.001 | 0.016 | 0.010 | 0.013 |
| Unsuccessful Efforts to Cut Down | 0.074 | 0.029 | 0.000 | 0.028 | 0.016 | 0.001 |
| Larger Amount/Longer Periods | 0.015 | 0.008 | 0.006 | 0.010 | 0.007 | 0.202 |
| Withdrawal | 0.007 | 0.007 | 0.711 | 0.022 | 0.020 | 1.000 |
| Great Deal of Time Spent | 0.000 | 0.000 | 0.198 | 0.000 | 0.000 | 1.000 |
| Giving Up/Reducing Activities | 0.000 | 0.000 | 0.212 | 0.000 | 0.000 | 1.000 |
| Physical/Psychological Problem | 0.002 | 0.000 | 0.153 | 0.003 | 0.001 | 0.069 |
| Moderate Class | Males | Females | p | Males | Females | p |
| Major Role Failure | 0.013 | 0.007 | 0.382 | 0.005 | 0.008 | 1.000 |
| Physically Hazardous | 0.553 | 0.435 | 0.000 | 0.409 | 0.261 | 0.000 |
| Legal Problems | 0.040 | 0.017 | 0.013 | 0.017 | 0.009 | 0.115 |
| Social/Interpersonal Problems | 0.081 | 0.035 | 0.000 | 0.053 | 0.015 | 0.001 |
| Tolerance | 0.339 | 0.252 | 0.002 | 0.261 | 0.191 | 0.001 |
| Unsuccessful Efforts to Cut Down | 0.399 | 0.347 | 0.087 | 0.375 | 0.342 | 0.250 |
| Larger Amount/Longer Periods | 0.528 | 0.521 | 0.867 | 0.558 | 0.546 | 0.706 |
| Withdrawal | 0.378 | 0.451 | 0.026 | 0.457 | 0.541 | 0.002 |
| Great Deal of Time Spent | 0.081 | 0.055 | 0.111 | 0.065 | 0.053 | 0.322 |
| Giving Up/Reducing Activities | 0.010 | 0.001 | 0.024 | 0.008 | 0.003 | 0.164 |
| Physical/Psychological Problem | 0.143 | 0.135 | 0.728 | 0.142 | 0.115 | 0.229 |
| Severe Class | Males | Females | p | Males | Females | p |
| Major Role Failure | 0.314 | 0.455 | 0.038 | 0.347 | 0.266 | 0.191 |
| Physically Hazardous | 0.913 | 0.779 | 0.004 | 0.732 | 0.639 | 0.107 |
| Legal Problems | 0.176 | 0.130 | 0.270 | 0.171 | 0.088 | 0.020 |
| Social/Interpersonal Problems | 0.614 | 0.506 | 0.172 | 0.611 | 0.476 | 1.000 |
| Tolerance | 0.753 | 0.737 | 0.810 | 0.667 | 0.601 | 0.333 |
| Unsuccessful Efforts to Cut Down | 0.756 | 0.826 | 0.252 | 0.805 | 0.906 | 0.040 |
| Larger Amount/Longer Periods | 0.909 | 0.891 | 0.666 | 0.906 | 0.889 | 0.658 |
| Withdrawal | 0.813 | 0.896 | 0.084 | 0.819 | 0.773 | 0.329 |
| Great Deal of Time Spent | 0.664 | 0.570 | 0.198 | 0.624 | 0.590 | 0.624 |
| Giving Up/Reducing Activities | 0.319 | 0.313 | 0.917 | 0.300 | 0.268 | 0.671 |
| Physical/Psychological Problem | 0.799 | 0.754 | 1.000 | 0.842 | 0.819 | 0.716 |
References
- Briere FN, Rohde P, Seeley JR, Klein D, Lewinsohn PM, 2014. Comorbidity between major depression and alcohol use disorder from adolescence to adulthood. Compr. Psychiatry 55, 526–533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Behrendt S, Beesdo-Baum K, Zimmermann P, Höfler M, Perkonigg A, Bühringer G, Lieb R, Wittchen HU, 2011. The role of mental disorders in the risk and speed of transition to alcohol use disorders among community youth. Psychol. Med 41, 1073–1085. [DOI] [PubMed] [Google Scholar]
- Blanco C, Okuda M, Markowitz JC, Liu SM, Grant BF, Hasin DS, 2010. The epidemiology of chronic major depressive disorder and dysthymic disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions. J. Clin. Psychiatry 71, 1645–1656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bolton JM, Robinson J, Sareen J, 2009. Self-medication of mood disorders with alcohol and drugs in the National Epidemiologic Survey on Alcohol and Related Conditions. J. Affect. Disord 115, 367–375. [DOI] [PubMed] [Google Scholar]
- Boschloo L, Vogelzangs N, van den Brink W, Smit JH, Veltman DJ, Beekman AT, Penninx BW, 2012. Alcohol use disorders and the course of depressive and anxiety disorders. Br. J. Psychiatry 200, 476–484. [DOI] [PubMed] [Google Scholar]
- Britton PC, Stephens B, Wu J, Kane C, Gallegos A, Ashrafioun L, Tu X, Conner KR, 2015. Comorbid depression and alcohol use disorders and prospective risk for suicide attempt in the year following inpatient hospitalization. J. Affect. Disord 187, 151–155. [DOI] [PubMed] [Google Scholar]
- Bucholz KK, Heath AC, Madden PA, 2000. Transitions in drinking in adolescent females: evidence from the Missouri adolescent female twin study. Alcohol. Clin. Exp. Res 24, 914–923. [PubMed] [Google Scholar]
- Butterworth P, Slade T, Degenhardt L, 2014. Factors associated with the timing and onset of cannabis use and cannabis use disorder: Results from the 2007 Australian National Survey of Mental Health and Well-Being. Drug Alcohol Rev 33, 555–564. [DOI] [PubMed] [Google Scholar]
- Catanzaro SJ, Laurent J, 2004. Perceived family support, negative mood regulation expectancies, coping, and adolescent alcohol use: evidence of mediation and moderation effects. Addict. Behav 29, 1779–1797. [DOI] [PubMed] [Google Scholar]
- Celeux G, Soromenho G, 1996. An entropy criterion for assessing the number of clusters in a mixture model. J. Classification 13, 195–212. [Google Scholar]
- Chen LY, Strain EC, Crum RM, Mojtabai R, 2013. Gender differences in substance abuse treatment and barriers to care among persons with substance use disorders with and without comorbid major depression. J. Addict. Med 7, 325–334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins LM, Wugalter SE, 1992. Latent class models for stage-sequential dynamic latent variables. Multivariate Behav. Res 27, 131–137. [Google Scholar]
- Conway KP, Swendsen J, Husky MM, He J-P, Merikangas KR, 2016. Association of lifetime mental disorders and subsequent alcohol and illicit drug use: results from the National Comorbidity Survey–Adolescent Supplement. J. Am. Acad. Child Adolesc. Psychiatry 55, 280–288. [DOI] [PubMed] [Google Scholar]
- Cook EC, Pflieger JC, Connell AM, Connell CM, 2015. Do specific transitional patterns of antisocial behavior during adolescence increase risk for problems in young adulthood? J. Abnorm. Child Psychol 43(1), 95–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cranford JA, Nolen-Hoeksema S, Zucker RA, 2011. Alcohol involvement as a function of co-occurring alcohol use disorders and major depressive episode: Evidence from the National Epidemiologic Survey on Alcohol and Related Conditions. Drug Alcohol Depend 117(2–3), 145–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crum RM, Brown C, Liang KY, Eaton WW, 2001. The association of depression and problem drinking: analyses from the Baltimore ECA follow-up study. Epidemiologic Catchment Area. Addict. Behav 26, 765–773. [DOI] [PubMed] [Google Scholar]
- Crum RM, Mojtabai R, Lazareck S, Bolton JM, Robinson J, Sareen J, Green KM, Stuart EA, La Flair L, Alvanzo AA, Storr CL, 2013. A prospective assessment of reports of drinking to self-medicate mood symptoms with the incidence and persistence of alcohol dependence. JAMA Psychiatry 70, 718–726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curran GM, Flynn HA, Kirchner J, Booth BM, 2000. Depression after alcohol treatment as a risk factor for relapse among male veterans. J. Subst. Abuse Treat 19, 259–265. [DOI] [PubMed] [Google Scholar]
- Curtis LH, Hammill BG, Eisenstein EL, Kramer JM, Anstrom KJ, 2007. Using inverse probability-weighted estimators in comparative effectiveness analyses with observational databases. Med. Care 45, S103–S107. [DOI] [PubMed] [Google Scholar]
- Dawson DA, Goldstein RB, Moss HB, Li TK, Grant BF, 2010. Gender differences in the relationship of internalizing and externalizing psychopathology to alcohol dependence: likelihood, expression and course. Drug Alcohol Depend 112(1–2), 9–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Demmel R, Nicolai J, Gregorzik S, 2006. Alcohol expectancies and current mood state in social drinkers. Addict. Behav 31, 859–867. [DOI] [PubMed] [Google Scholar]
- Driessen M, Meier S, Hill A, Wetterling T, Lange W, Junghanns K, 2001. The course of anxiety, depression and drinking behaviours after completed detoxification in alcoholics with and without comorbid anxiety and depressive disorders. Alcohol Alcohol 36, 249–255. [DOI] [PubMed] [Google Scholar]
- Dugoff EH, Schuler M, Stuart EA, 2014. Generalizing observational study results: applying propensity score methods to complex surveys. Health Serv. Res 49(1), 284–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards AC, Sihvola E, Korhonen T, Pulkkinen L, Moilanen I, Kaprio J, Rose RJ, Dick DM, 2011. Depressive symptoms and alcohol use are genetically and environmentally correlated across adolescence. Behav. Genet 41, 476–487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehlke SJ, Hagman BT, Cohn AM, 2012. Modeling the dimensionality of DSM-IV alcohol use disorder criteria in a nationally representative sample of college students. Subst. Use Misuse 47(10), 1073–1085. [DOI] [PubMed] [Google Scholar]
- Farrell M, Howes S, Bebbington P, Brugha T, Jenkins R, Lewis G, Marsden J, Taylor C, Meltzer H, 2001. Nicotine, alcohol and drug dependence and psychiatric comorbidity. Results of a national household survey. Br. J. Addict 179, 432–437. [DOI] [PubMed] [Google Scholar]
- Farren CK, Snee L, McElroy S, 2011. Gender differences in outcome at 2-year follow-up of treated bipolar and depressed alcoholics. J. Stud. Alcohol Drugs 72(5), 872–880. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Boden JM, Horwood LJ, 2009. Tests of causal links between alcohol abuse or dependence and major depression. Arch. Gen. Psychiatry 66, 260–266. [DOI] [PubMed] [Google Scholar]
- Flensborg-Madsen T, Mortensen EL, Knop J, Becker U, Sher L, Gronbaek M, 2009. Comorbidity and temporal ordering of alcohol use disorders and other psychiatric disorders: results from a Danish register-based study. Compr. Psychiatry 50, 307–314. [DOI] [PubMed] [Google Scholar]
- Frye MA, Altshuler LL, McElroy SL, Suppes T, Keck PE, Denicoff K, Nolen WA, Kupka R, Leverich GS, Pollio C, Grunze H, Walden J, Post RM, 2003. Gender differences in prevalence, risk, and clinical correlates of alcoholism comorbidity in bipolar disorder. Am. J. Psychiatry 160, 883–889. [DOI] [PubMed] [Google Scholar]
- Gilman SE, Abraham HD, 2001. A longitudinal study of the order of onset of alcohol dependence and major depression. Drug Alcohol Depend 63, 277–286. [DOI] [PubMed] [Google Scholar]
- Grant BF, Dawson DA, Stinson FS, Chou PS, Kay W, Pickering R, 2003. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV AUDADIS-IV: reliability of alcohol consumption, tobacco use, family history of depression and psychiatric diagnostic modules in a general population sample. Drug Alcohol Depend 71, 7–16. [DOI] [PubMed] [Google Scholar]
- Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, Pickering RP, Kaplan K, 2004. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch. Gen. Psychiatry 61, 807–816. [DOI] [PubMed] [Google Scholar]
- Grant BF, Goldstein RB, Chou SP, Huang B, Stinson FS, Dawson DA, Saha TD, Smith SM, Pulay AJ, Pickering RP, Ruan WJ, Compton WM, 2009. Sociodemographic and psychopathologic predictors of first incidence of DSM-IV substance use, mood and anxiety disorders: results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. Mol. Psychiatry 14, 1051–1066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Goldstein RB, Saha TD, Chou SP, Jung J, Zhang H, Pickering RP, Ruan WJ, Smith SM, Huang B, Hasin DS, 2015. Epidemiology of DSM-5 alcohol use disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions III. JAMA Psychiatry 72, 757–766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenfield SF, Weiss RD, Muenz LR, Vagge LM, Kelly JF, Bello LR, 1998. The effect of depression on return to drinking: a prospective study. Arch. Gen. Psychiatry 55, 259–265. [DOI] [PubMed] [Google Scholar]
- Grucza RA, Bucholz KK, Rice JP, Bierut LJ, 2008. Secular trends in the lifetime prevalence of alcohol dependence in the United States: a re-evaluation. Alcohol. Clin. Exp. Res 32, 763–770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasking P, Lyvers M, Carlopio C, 2011. The relationship between coping strategies, alcohol expectancies, drinking motives and drinking behaviour. Addict. Behav 36, 479–487. [DOI] [PubMed] [Google Scholar]
- Hasin DS, Goodwin RD, Stinson FS, Grant BF, 2005. Epidemiology of major depressive disorder: results from the National Epidemiologic Survey on Alcoholism and Related Conditions. Arch. Gen. Psychiatry 62, 1097–1106. [DOI] [PubMed] [Google Scholar]
- Husky MM, Mazure CM, Paliwal P, McKee SA, 2008. Gender differences in the comorbidity of smoking behavior and major depression. Drug Alcohol Depend 93, 176–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson ME, Brems C, Mills ME, Fisher DG, 2007. Psychiatric symptomatology among individuals in alcohol detoxification treatment. Addict. Behav 32, 1745–1752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones BT, Corbin W, Fromme K, 2001. A review of expectancy theory and alcohol consumption. Addiction 96, 57–72. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Crum RM, Warner LA, Nelson CB, Schulenberg J, Anthony JC, 1997. The lifetime co-occurrence of DSM-III-R alcohol abuse and dependence with other psychiatric disorders in the National Comorbidity Survey. Arch. Gen. Psychiatry 54, 313–321. [DOI] [PubMed] [Google Scholar]
- Khantzian EJ, 1990. Self-regulation and self-medication factors in alcoholism and the addictions. Similarities and differences. Recent Dev. Alcohol 8, 255–271. [PubMed] [Google Scholar]
- Keyes KM, Martins SS, Blanco C, Hasin DS, 2010. Telescoping and gender differences in alcohol dependence: new evidence from two national surveys. Am. J. Psychiatry 167, 969–976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuo PH, Gardner CO, Kendler KS, Prescott CA, 2006. The temporal relationship of the onsets of alcohol dependence and major depression: using a genetically informative study design. Psychol. Med 36, 1153–1162. [DOI] [PubMed] [Google Scholar]
- La Flair LN, Reboussin BA, Storr CL, Letourneau E, Green KM, Mojtabai R, Pacek LR, Alvanzo AA, Cullen B, Crum, R.M., 2013. Childhood abuse and neglect and transitions in stages of alcohol involvement among women: A latent transition analysis approach. Drug Alcohol Depend 132, 491–498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- La Flair LN, Bradshaw CP, Storr CL, Green KM, Alvanzo AA, Crum RM, 2012. Intimate partner violence and patterns of alcohol abuse and dependence criteria among women: a latent class analysis. J. Stud. Alcohol Drugs 73, 351–360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai HM, Sitharthan T, Huang QR, 2012. Exploration of the comorbidity of alcohol use disorders and mental health disorders among inpatients presenting to all hospitals in New South Wales, Australia. Subst. Abus 33, 138–145. [DOI] [PubMed] [Google Scholar]
- Mancha BE, Hulbert A, Latimer WW, 2012. A latent class analysis of alcohol abuse and dependence symptoms among Puerto Rican youth. Subst. Use Misuse 47(4), 429–441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marmorstein NR, 2009. Longitudinal associations between alcohol problems and depressive symptoms: early adolescence through early adulthood. Alcohol. Clin. Exp. Res 33, 49–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martins SS, Gorelick DA, 2011. Conditional substance abuse and dependence by diagnosis of mood or anxiety disorder or schizophrenia in the U.S. population. Drug Alcohol Depend 119, 28–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mattisson C, Bogren M, Horstmann V, Munk-Jorgensen P, Nettelbladt P, 2007. The long-term course of depressive disorders in the Lundby Study. Psychol. Med 37, 883–891. [DOI] [PubMed] [Google Scholar]
- McBride O, Adamson G, Cheng HG, Slade T, 2014. Changes in drinking patterns in the first years after onset: A latent transition analysis of National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) data. Psychol. Addict. Behav 28(3), 696–709. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO, 1998–2010. Mplus Users Guide Version 6, 1998–2010 Muthén and Muthén, Los Angeles, CA. [Google Scholar]
- Muthén B, 2006. Should substance use disorders be considered as categorical or dimensional? Addiction 101 Suppl 1, 6–16. [DOI] [PubMed] [Google Scholar]
- Needham BL, 2007. Gender differences in trajectories of depressive symptomatology and substance use during the transition from adolescence to young adulthood. Soc. Sci. Med 65, 1166–1179. [DOI] [PubMed] [Google Scholar]
- Nylund KL, Asparouhov T, Muthén BO, 2007. Deciding on the number of classes in latent class analysis and growth mixture modeling: A Monte Carlo Simulation study. Struct. Equ, Modeling 14(4), 535–569. [Google Scholar]
- Pacek LR, Martins SS, Crum RM, 2013. The bidirectional relationships between alcohol, cannabis, co-occurring alcohol and cannabis use disorders with major depressive disorder: results from a national sample. J. Affect. Disord 148(2–3), 188–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prisciandaro JJ, DeSantis SM, Chiuzan C, Brown DG, Brady KT, Tolliver BK, 2012. Impact of depressive symptoms on future alcohol use in patients with co-occurring bipolar disorder and alcohol dependence: a prospective analysis in an 8-week randomized controlled trial of acamprosate. Alcohol. Clin. Exp. Res 36, 490–496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reboussin BA, Reboussin DM, Liang KY, Anthony JC, 1998. A latent transition approach for modeling progression of health-risk behavior. Multivariate Behav. Res 33, 457–478. [DOI] [PubMed] [Google Scholar]
- Reboussin BA, Liang KY, Reboussin DM, 1999. Estimating equations for a latent transition model with multiple discrete indicators. Biometrics 55, 839–845. [DOI] [PubMed] [Google Scholar]
- Ross HE, 1995. DSM-III-R alcohol abuse and dependence and psychiatric comorbidity in Ontario: results from the Mental Health Supplement to the Ontario Health Survey. Drug Alcohol Depend 39, 111–128. [DOI] [PubMed] [Google Scholar]
- Ruan WJ, Goldstein RB, Chou SP, Smith SM, Saha TD, Pickering RP, Dawson DA, Huang B, Stinson FS, Grant BF, 2008. The alcohol use disorder and associated disabilities interview schedule-IV AUDADIS-IV: reliability of new psychiatric diagnostic modules and risk factors in a general population sample. Drug Alcohol Depend 92, 27–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubin DB, 2010. Propensity score methods. Am. J. Ophthalmol 149, 7–9. [DOI] [PubMed] [Google Scholar]
- Smith GT, 1994. Psychological expectancy as mediator of vulnerability to alcoholism. Ann. N. Y. Acad. Sci 708, 165–171. [DOI] [PubMed] [Google Scholar]
- Stuart EA, 2010. Matching methods for causal inference: A review and a look forward. Stat. Sci 25, 1–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sung M, Erkanli A, Angold A, Costello EJ, 2004. Effects of age at first substance use and psychiatric comorbidity on the development of substance use disorders. Drug Alcohol Depend 75, 287–299. [DOI] [PubMed] [Google Scholar]
- Swift W, Slade T, Carragher N, Coffey C, Degenhardt L, Hall W, Patton G, 2016. Adolescent predictors of a typology of DSM-5 alcohol use disorder symptoms in young adults derived by latent class analysis using data from an Australian cohort study. J. Stud. Alcohol Drugs 77(5), 757–765. [DOI] [PubMed] [Google Scholar]
- Wang J, Patten SB, 2001. A prospective study of sex-specific effects of major depression on alcohol consumption. Can. J. Psychiatry 46, 422–425. [DOI] [PubMed] [Google Scholar]
- Wang J, Patten SB, 2002. Prospective study of frequent heavy alcohol use and the risk of major depression in the Canadian general population. Depress. Anxiety 15, 42–45. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Bland RC, Canino GJ, Faravelli C, Greenwald S, Hwu HG, Joyce PR, Karam EG, Lee CK, Lellouch J, Lépine JP, Newman SC, Rubio-Stipec M, Wells JE, Wickramaratne PJ, Wittchen H, Yeh EK, 1996. Cross-national epidemiology of major depression and bipolar disorder. JAMA 276, 293–299. [PubMed] [Google Scholar]
- Windle M, Davies PT, 1999. Depression and heavy alcohol use among adolescents: concurrent and prospective relations. Dev. Psychopathol 11, 823–844. [DOI] [PubMed] [Google Scholar]
- Young-Wolff KC, Kendler KS, Sintov ND, Prescott CA, 2009. Mood-related drinking motives mediate the familial association between major depression and alcohol dependence. Alcohol. Clin. Exp. Res 33, 1476–1486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van de Velde S, Bracke P, Levecque K, 2010. Gender differences in depression in 23 European countries. Cross-national variation in the gender gap in depression. Soc. Sci. Med 71, 305–313. [DOI] [PubMed] [Google Scholar]
- van Zaane J, van den Brink W, Draisma S, Smit JH, Nolen WA, 2010. The effect of moderate and excessive alcohol use on the course and outcome of patients with bipolar disorders: a prospective cohort study. J. Clin. Psychiatry 71, 885–893. [DOI] [PubMed] [Google Scholar]


