Abstract
Background:
Due to shame and fear of discrimination, individuals in, or seeking, recovery from alcohol and other drug (AOD) problems often struggle with whether, when, and to whom to disclose information regarding their AOD histories and recovery status. This can serve as a barrier to obtaining needed recovery support. Consequently, disclosure may have important implications for recovery trajectories, yet is poorly understood.
Design and Sample:
Cross-sectional, U.S. nationally-representative survey conducted in 2016 among individuals with resolved AOD problems (N=1,987) investigated disclosure comfort and whether disclosure comfort differed by disclosure recipient (i.e., with interpersonal intimacy), time since problem resolution, or primary substance (i.e., alcohol [51%], cannabis [11%], opioids [5%], or “other” [33%]). Predictors of disclosure comfort were also examined. Data were examined using LOWESS analyses, analyses of variance, and regression.
Results:
Overall, longer time since problem resolution was associated with greater disclosure comfort. In general, participants reported greater comfort with disclosure to family and friends, and less comfort with disclosure to co-workers, to first-time acquaintances, in public settings, and in the media, but these effects varied by primary drug with participants who had problems with alcohol and “other” drugs having significantly more disclosure comfort than those who had problems with opioids.
Conclusion:
Dimensions of time since AOD problem resolution, interpersonal intimacy, and primary drug are significantly associated with disclosure comfort. Individuals seeking recovery may benefit from more formal coaching around disclosure, particularly those with primary opioid problems, but further research is needed to determine the desire for and effects of such coaching among those seeking recovery.
Keywords: disclosure, recovery, remission, substance use disorder
1. INTRODUCTION
Disclosure is a key relational process experienced by people who have resolved alcohol and other drug (AOD) problems. People who have resolved AOD problems, including AOD disorders as well as AOD problems that may not meet the threshold for an AOD disorder (e.g., hazardous/harmful alcohol consumption), are often referred to as “being in recovery” (although they may not all identify as being in recovery; Kelly, Abry, Milligan, Bergman, & Hoeppner, 2018). Disclosure of AOD problem resolution involves the sharing of information regarding one’s AOD history, resolution, and/or treatment with others such as family members, friends, co-workers, and acquaintances (Chaudoir & Fisher, 2011). Disclosure represents a gateway to interpersonal interactions that may either support (e.g., through social support) or hinder (e.g., through stigma) recovery (Brewer, 2006; Dobkin, Civita, Paraherakis, & Gill, 2002; Simmonds & Coomber, 2009). People who have resolved AOD problems report struggling with decisions regarding whether to disclose (Earnshaw et al., in press), yet disclosure is currently understudied among people in recovery. Greater understanding of the circumstances under which people feel more or less comfort with disclosing their AOD problem resolution can inform clinical efforts to guide disclosure decisions and processes that may support recovery efforts among this growing population. The current study therefore explores disclosure comfort among a nationally representative sample of U.S. adults who have resolved AOD problems. More specifically, it focuses on whether, when, and to whom people feel comfortable disclosing that they have resolved an AOD problem. Also, given that certain primary drug problems (e.g., heroin, crack cocaine) might be more stigmatized than others (e.g., alcohol), primary drug was examined in relation to disclosure comfort.
Disclosure comfort may vary along several dimensions. People who have resolved an AOD problem in the more distant past, for instance, may be more comfortable with disclosure because they have had more practice with disclosure. The Disclosure Process Model, a framework for understanding disclosure decisions and outcomes among people living with concealable stigmatized identities, includes a feedback loop linking past disclosures with future disclosures (Chaudoir & Fisher, 2011). The model hypothesizes that people who have more positive, accepting disclosures “spiral upwards” toward visibility by feeling increasingly comfortable with disclosure and, in turn, engage in more disclosures. People who have resolved their AOD problem longer ago may also have greater disclosure comfort because they are more likely to have stably resolved their AOD problem and perhaps developed a new and more positive self-image and perspective on their experience, or have developed more self-confidence and self-esteem (Kelly, Greene, & Bergman, 2018).
Characteristics of the disclosure recipient, or the person or group of people to whom an individual is disclosing, may further shape disclosure comfort. Research suggests that there are associations between disclosure frequency with relationship intimacy and closeness (Laurenceau, Barrett, & Pietromonaco, 1998; Manne et al., 2004). The Interpersonal Process Model of Intimacy suggests that disclosure leads to greater relationship intimacy, but also recognizes that greater relationship intimacy may lead to more disclosure (Reis & Shaver, 1988). It is possible that individuals feel greater comfort disclosing their AOD problem resolution in closer or more intimate, trusted, relationships because recipients know them as full people with other identities and characteristics (e.g., mother, athlete), and not merely as people recovering from AOD problems. Indeed, results of qualitative research suggest that people in recovery may feel greater comfort disclosing in more intimate and trusting relationships (Romo, Dinsmore, & Watterson, 2016) such as to friends and family members (Earnshaw et al., in press). People who have resolved AOD problems may also disclose within the contexts of less intimate relationships. They may disclose to employers and coworkers to explain the results of criminal background checks or to request accommodations for treatment (e.g., methadone maintenance therapy; Earnshaw, Smith, & Copenhaver, 2013; Murphy & Irwin, 1992). People with a range of concealable stigmatized characteristics, including histories of AOD problems, additionally disclose in more public settings and the media (Corrigan & Matthews, 2003; Hutchinson et al., 2007; Roose, Fuentes, & Cheema, 2012). People may choose to broadcast a concealable stigmatized identity for several reasons, including to enhance their own power over their identity, educate others about their identity, and reduce stigma associated with their identity (Corrigan & Matthews, 2003; Hutchinson, Mahlalela, & Yukich, 2007). According to the Interpersonal Process Model of Intimacy, individuals may have less comfort disclosing in less intimate relationships and settings, including to co-workers and in public settings or the media.
The type of AOD problem that a person is disclosing may additionally relate to disclosure comfort. In 2016, 15.1 million people in the U.S. were estimated to have an alcohol use disorder, 4.0 million a cannabis use disorder, and 2.1 million an opioid use disorder (Substance Abuse and Mental Health Services Administration, 2017). A study conducted by the World Health Organization in 14 countries found addiction to both alcohol and illicit drugs to be highly stigmatized, with addiction to illicit drugs (e.g., heroin) being more stigmatized than addiction to alcohol (Room, Rehm, Trotter, Paglia, & Üstün, 2001). More specifically, addiction to illicit drugs was the most stigmatized social problem among 18 studied and addiction to alcohol was the fourth most stigmatized. Similarly, people in recovery from heroin report experiencing greater stigma when they disclose than people in recovery from other substances, such as alcohol (Earnshaw et al., in press). It is possible that opioid use disorders are more stigmatized because they are perceived to be particularly perilous (i.e., threatening to the self and others, via overdose and links to infectious disease), disruptive (i.e., interfering with social interactions), and difficult to overcome (Pachankis et al., 2018). Nonetheless, people in recovery from alcohol problems report significant experiences of stigma (e.g., social exclusion) and often choose not to disclose their sobriety (Romo et al., 2016). Taken together, people who have resolved any type of AOD problem may report discomfort surrounding disclosure, yet people who have resolved licit substances (e.g., alcohol) may have slightly greater disclosure comfort than people who have resolved illicit substances.
These three dimensions of time since problem resolution, level of interpersonal intimacy, and primary substance, may covary with disclosure comfort. Consequently, this study investigated how comfortable people feel disclosing their AOD problem history as a function of time since problem resolution, with respect to different people and levels of public disclosure, and in relation to their primary drug. Based on prior research, we hypothesized that longer time since problem resolution would be associated with greater disclosure comfort. We also hypothesized that greater disclosure comfort would be observed in more intimate or closer relationships, such as with family and friends, than in more distant relationships, such as with first-time acquaintances or in public settings (see Figure 1). Finally, we predicted that people who had resolved problems involving licit substances (e.g., alcohol) would have greater disclosure comfort than people who had resolved problems with illicit and more stigmatized substances (e.g., heroin/opioids). We also explored associations between disclosure comfort with other socio-demographic and relevant clinical characteristics to inform efforts to identify individuals with more or less disclosure comfort. Given that research to date on disclosure among people who have resolved AOD problems has been limited, we did not form hypotheses regarding these associations.
Figure 1.
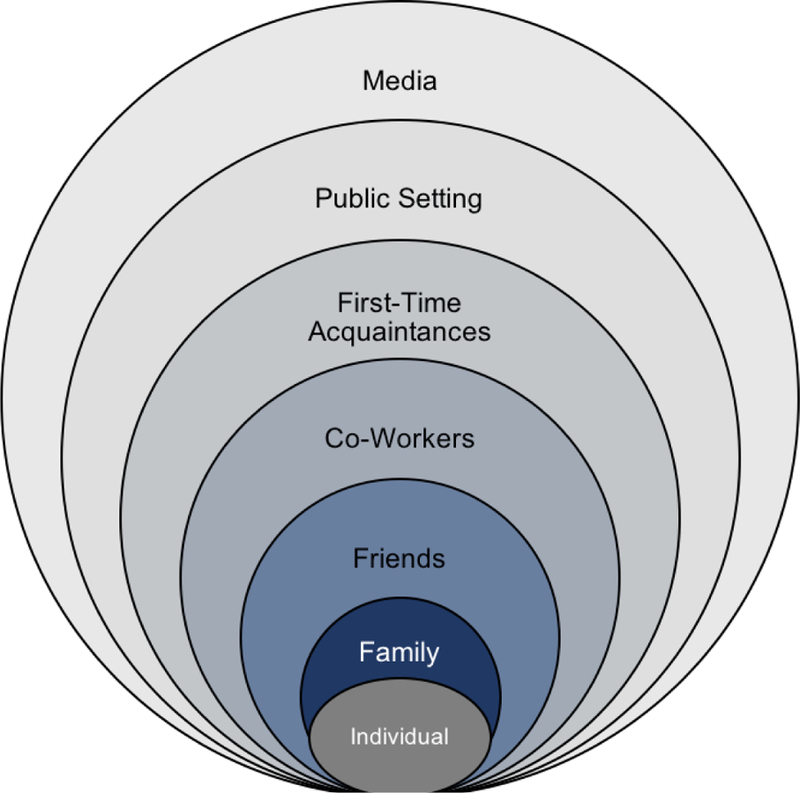
Hypothesized disclosure comfort by level of interpersonal intimacy
Note: Darker colors indicate more hypothesized disclosure comfort
2. MATERIAL AND METHODS
2.1. Participants and Procedures
Data for the current study are drawn from the National Recovery Study (NRS), which is a nationally representative survey of people who have resolved alcohol and drug use problems. To be eligible to participate in the NRS, individuals must have been a noninstitutionalized U.S. citizen, aged 18 years or older, who answered yes to the screening question “Did you used to have a problem with drugs or alcohol, but no longer do?” (Kelly et al. , 2017). Data were collected by the survey company GfK via their KnowledgePanel (GfK, 2013), which is a geo-demographically representative sample of U.S. adults. The KnowledgePanel includes 55,000 adults randomly selected through address-based sampling from 97% of all U.S. households included in the U.S. Postal Service’s Delivery Sequence File. To account for socioeconomic differences in landline telephone use and internet access, GfK provides individuals with a web-enabled computer and free Internet service if necessary. The KnowledgePanel therefore includes individuals from households that have unlisted telephone numbers, do not have landline telephones, use cell phones only, do not have current internet access, and/or do not have devices to access the internet. A representative subset of 38,909 members of the KnowledgePanel were invited by GfK to participate in the NRS. This subset was drawn using a probability proportional to size sampling approach (U.S. Patent No. 7,269,570), which assures that subsamples from a finite panel membership remain a reliable approximation of the entire U.S. population (GfK, 2013).
Of the 38,909 KnowledgePanel members who were contacted, 25,229 responded to the NRS screening question. This response rate of 63.4% is comparable to other nationally representative surveys (Centers for Disease Control and Prevention, 2013; Grant et al., 2015). There were 283 individuals who began the survey but did not complete it, resulting in 2,002 individuals who answered “yes” to the screener question and completed the survey. The current analyses focus on 1,987 participants who responded to the disclosure comfort measure [described below; 15 participants (0.7% of sample) did not respond to this measure]. Median time to completion was 24 minutes (interquartile range = 18–36 minutes). To ensure that the resulting sample represented the US population, differences between the sample and US population were accounted for via sample weights created by Gfk using iterative proportional fitting (Battaglia, Izrael, Hoaglin, & Frankel, 2009). Weights were based on several key variables, including gender, age, race/Hispanic ethnicity, education, census geographical region, household income, home ownership status, and metropolitan area benchmarked to the U.S. Bureau of Census data.
All procedures were approved by the Partners HealthCare Institutional Review Board. Studies using data from the NRS and further detailing these procedures have been previously reported (Kelly et al., 2017, 2018).
2.2. Measures
2.2.1. Socio-Demographics and Clinical Characteristics.
Participants reported their age, gender (male, female), race (White, Non-Hispanic; Black, Non-Hispanic; Other, Non-Hispanic; Hispanic; 2+ Races, Non-Hispanic), sexual orientation (heterosexual, LGBTQ), education (less than high school, high school, some college, bachelor’s degree or more), and current employment status (employed, unemployed). Participants additionally reported whether they had ever been diagnosed with one or more of 16 psychiatric disorders, including anxiety disorders (e.g., generalized anxiety disorder), mood disorders (e.g., major depressive disorder), eating disorders (e.g., anorexia), psychotic disorders (e.g., schizophrenia), and personality disorder, or another psychiatric disorder (specified by participant) (Dennis, Titus, White, Unsicker, & Hodgkins, 2002). Participants also reported whether they were currently involved in the criminal justice system, including awaiting court hearing, on probation, on parole, or other specified.
2.2.2. Substance Use History.
Participants reported which substances they had ever used 10+ times lifetime from a list of 15 from the Global Appraisal of Individual Needs (GAIN-I; Dennis et al., 2002). The substances included: alcohol, marijuana, cocaine, heroin, narcotics other than heroin, methadone, bupenorphine and its formulations, amphetamines, methamphetamine, benzodiazepines, barbituates, hallucinogens, synthetic drugs, inhalents, and stereoids. Participants could additionally specify an other substance. For each substance they indicated they had ever used, participants indicated their age of first use. The substance used at the youngest age was used to indicate the participants’ age at first use. Participants additionally reported whether each substance used was perceived to be a problem for them. This was used to generate a number of problem substances per each participant. Additionally, from the list of substances they identified as being a problem, participants indicated which was their primary drug (or “drug of choice”). These were categorized into four primary substance groups: alcohol, cannabis, opioids, or “other” drug. Participants further indicated whether they had ever in their lifetime been diagnosed with a substance use disorder.
2.2.3. Recovery History and Management.
Participants reported time in years and months since they resolved their substance problem, which was converted into one continuous variable representing years since problem resolution. They also reported the number of “serious attempts” made to resolve their substance use problem before they “overcame” it. Participants reported whether they had utilized recovery support services (state or local recovery community organization, faith-based recovery services, recovery community center, collegiate recovery program/community, recovery high school, and/or sober living environment) and treatment services (inpatient or residential treatment and/or outpatient addiction treatment). They also reported whether they regularly used (i.e., at least once per week) a mutual-help organization (Alcoholics Anonymous, Narcotics Anonymous, Marijuana Anonymous, Cocaine Anonymous, Crystal Methamphetamine Anonymous, SMART Recovery, LifeRing Secular Recovery, Moderation Management, Celebrate Recovery, Women for Sobriety, Secular Organization for Sobriety, other). Participants reported whether they had ever been prescribed a medication to prevent them from drinking alcohol or using opioids. If they responded yes to either item, participants reported lifetime and current use of specific medications from the Form-90, including both generic and brand names (Miller & Del Boca, 1994). Finally, participants were asked whether they were currently abstinent from each substance endorsed for lifetime use. If they reported that they were currently abstinent from each substance, they were coded as “abstinent.” This was measured given that participants may have resolved a problem with one substance but still engage in use of another (e.g., in recovery from opioids but continue to drink alcohol).
2.2.4. Disclosure Comfort.
Items measuring disclosure comfort were included, informed by qualitative findings from Romo, Dinsmore, & Watterson (2016). Findings of this study indicated that people in recovery report a range of comfort with disclosing their recovery status to others. Therefore, participants were asked how comfortable, on a Likert-type scale ranging from 1 = not at all comfortable to 5 = completely comfortable, they felt disclosing their status as someone who has resolved an alcohol or drug use problem. Additionally, Romo and colleagues (2016) found that participants adopted different disclosure strategies for different recipients. Therefore, participants in the present study were asked about their disclosure comfort to a wide range of recipients, including (1) to family, (2) to friends, (3) to co-workers, (4) to someone they are meeting for the first time, (5) in a public setting (e.g., at a community event), and (6) in the media (e.g., a newspaper article). The overall scale had strong internal reliability (α = .90), and therefore an overall disclosure comfort score was created by averaging across all six items. The disclosure variable was normally distributed [skew (SE) = 0.18 (0.06), kurtosis (SE) = −1.01 (0.11)].
2.3. Analyses
First, we characterized the socio-demographics and clinical characteristics of the sample using descriptive statistics. Second, we explored associations between time since problem resolution and disclosure comfort using scatterplots with locally weighted smoothing (LOWESS) lines with a smoothing bandwidth of 0.8 and a uniform kernel function. We examined the association for the first 40 years since problem resolution as well as the first five years specifically, given that the first five years represent a critical time period for recovery during which individuals are at increased risk of relapse (Kelly et al., 2018). We further sought to quantify the association between time since problem resolution and disclosure comfort using regression analysis. Third, we explored mean levels of disclosure comfort to different recipients using a repeated-measures analysis of variance (ANOVA) to test for statistically significant differences in disclosure comfort to different recipients. We additionally visually represented disclosure comfort to different recipients using a stacked bar graph. Fourth, we explored mean levels of disclosure comfort among people reporting different primary substances, including alcohol, cannabis, opioids, or another drug other than cannabis or opioids (e.g., cocaine, amphetamine, methamphetamine, barbiturates, hallucinogens), using ANOVA. We additionally visually represented disclosure comfort among people reporting different primary substances using a stacked bar graph. Finally, we analyzed simultaneous linear regression models to examine the unique independent contributions of socio-demographic and clinical characteristics to disclosure comfort to different recipients. Time since problem resolution and primary substance were included in these analyses to explore the magnitude of their contributions to disclosure comfort after controlling for the effects of each other as well as the socio-demographic and clinical characteristics. Sample weights were applied for all analyses.
3. RESULTS
3.1. Participant Characteristics
Participant characteristics are summarized in Table 1. The average age of participants was 54.20 years (SD=14.34, range=18– 92). Over half (53.3%) of participants identified as male; 75.1% identified as White, Non-Hispanic, 9.7% identified as Hispanic, 9.5% identified as Black, Non-Hispanic, 2.4% identified as an other race, and 3.3% identified as two or more races. The majority of participants (84.1%) identified as heterosexual. There was a wide distribution of educational attainment, with 4.9% of participants reporting less than a high school degree, 17.1% reporting a high school degree, and the remaining reporting some college or more. Approximately half (49.8%) were currently employed, 36.1% had a co-occurring psychiatric disorder, and 3.1% had a history of criminal justice involvement. Slightly over half (58.0%) reported being in recovery from a problem with alcohol, 8.5% from a problem with cannabis, 4.9% from a problem with opioids, and 28.6% from a problem with “other” drugs (e.g., cocaine, amphetamine, methamphetamine, barbiturates, hallucinogens).
Table 1.
Participant Socio-Demographic and Clinical Characteristics (n=1987)
| % (n) | M (SD), Range | |
|---|---|---|
| Socio-Demographics | ||
| Age | 54.20 (14.34), 18–92 | |
| Gender | ||
| Male | 53.3 (1061) | |
| Female | 46.6 (926) | |
| Race/Ethnicity | ||
| White, Non-Hispanic | 75.1 (1492) | |
| Black, Non-Hispanic | 9.5 (188) | |
| Other, Non-Hispanic | 2.4 (48) | |
| Hispanic | 9.7 (193) | |
| 2+ Races, Non-Hispanic | 3.3 (66) | |
| Sexual Orientation | ||
| Heterosexual | 84.1 (1672) | |
| LGBTQ | 15.9 (315) | |
| Education | ||
| Less than High School | 4.9 (98) | |
| High School | 17.1 (340) | |
| Some College | 45.8 (911) | |
| Bachelor’s Degree or More | 32.1 (638) | |
| Employment Status | ||
| Employed | 49.8 (990) | |
| Unemployed | 50.2 (997) | |
| Co-Occurring Psychiatric Disorder | 36.1 (713) | |
| Criminal Justice Involvement | 3.1 (61) | |
| Substance Use History | ||
| Substance of Choice | ||
| Alcohol | 58.0 (1153) | |
| Cannabis | 8.5 (168) | |
| Opioids | 4.9 (97) | |
| Other | 28.6 (569) | |
| Number of Problem Substances | 1.49 (1.29), 1–15 | |
| Age of First Use | 15.02 (4.91), 1–63 | |
| SUD Diagnosis | 19.0 (375) | |
| Recovery History and Management | ||
| Years Since Problem Resolution | 15.10 (12.41), 0–69 | |
| Resolution Attempts | 4.50 (11.40), 0–100 | |
| Recovery Support Service Utilization | 19.3 (382) | |
| Treatment Utilization | 26.2 (517) | |
| Mutual-Help Organization Regular Use | 38.1 (752) | |
| Alcohol Medication (Current + Lifetime) | 5.1 (102) | |
| Opioid Medication (Current + Lifetime) | 3.3 (65) | |
| Abstinence | 56.7 (1126) | |
3.2. Time Since Problem Resolution
Scatterplots with locally weighted scatterplot and smoothing (LOWESS) lines representing the association between time since problem resolution and disclosure comfort are displayed in Figure 2. The first graph spans the first five years since problem resolution, and suggests that participants gain little in disclosure comfort during this period. The second graph spans the first 40 years since problem resolution, and suggests that disclosure comfort increases over this longer time horizon.
Figure 2.
Scatterplots with locally weighted smoothing (LOWESS) lines depicting association between years since problem resolution and disclosure comfort
An additional regression analysis was conducted to characterize the association between years since problem resolution and disclosure comfort. Linear, quadratic, and cubic effects of change were modeled by including years since problem resolution, years since problem resolution squared, and years since problem resolution cubed sequentially in a hierarchical linear regression model predicting disclosure comfort. Results suggested that the linear effect of years since problem resolution accounted for 5.8% of the variance in disclosure comfort (R2=0.058, p<0.001), and adding the quadratic effect of years since problem resolution accounted for an additional 0.4% of the variance (R2 change=0.004, p=0.004). Adding the cubic effect of years since problem resolution accounted for no additional variance in disclosure comfort (R2 change=0.001, p=0.407), and the cubic effect of years since problem resolution was not significant [B(SE)=−0.001(0.001), p=0.407]. The second step of the model including the linear and quadratic effects of years since problem resolution was therefore interpreted. The intercept for this step was 2.593 (SE=0.049) and the linear effect of years since problem resolution was 0.044 (SE=0.006, p<0.001), indicating that participants with zero years of recovery were predicted to have an average disclosure comfort score of 2.593 and gained 0.044 points on the disclosure comfort scale for each additional year since problem resolution. The quadratic effect of years since problem resolution was negative [B(SE)=−0.001(0.001), p=0.004], suggesting that the rate of increase in disclosure comfort slightly slows with additional years since problem resolution.
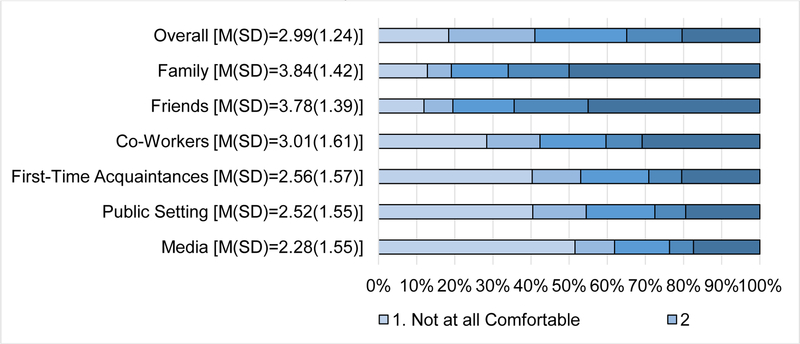
3.3. Disclosure Recipient
The percentages of participants with varying levels of disclosure comfort to different recipients, as well as the means and standard deviations of disclosure comfort to different recipients, are displayed in Figure 3. The mean score for disclosure comfort, averaged across all participants and recipient types, was 2.99 (SD=1.24), reflecting the midpoint of the disclosure comfort scale. Additionally, overall disclosure comfort was approximately equally distributed across comfort levels, indicating that there were similar percentages of participants with low, moderate, and high disclosure comfort in the sample. The bar graph suggests that disclosure comfort decreased with less closeness to recipients such that participants were most comfortable disclosing to family and friends and least comfortable disclosing in the media. For example, approximately 50% of participants reported that they were completely comfortable disclosing to family whereas approximately 50% reported that they were not at all comfortable disclosing in the media.
Figure 3.
Stacked bar graph indicating percentages of participants with varying levels of disclosure comfort to different disclosure recipients
Results of a repeated-measures ANOVA confirmed statistically significant mean differences in disclosure comfort to different recipients, with a large effect size [F(1,1805)=1697.221, p<0.001,ηp2=0.485]. Post-hoc pairwise comparisons with LSD adjustments suggested that differences in disclosure comfort to various types of recipients were all statistically significant (ps<0.001) with two exceptions: Differences in disclosure comfort to family and friends [MDiff (SE)=0.041(0.023), p=0.081], as well as to first-time acquaintances and in public settings [MDiff (SE)=0.043(0.022), p=0.058] were only marginally statistically significant.
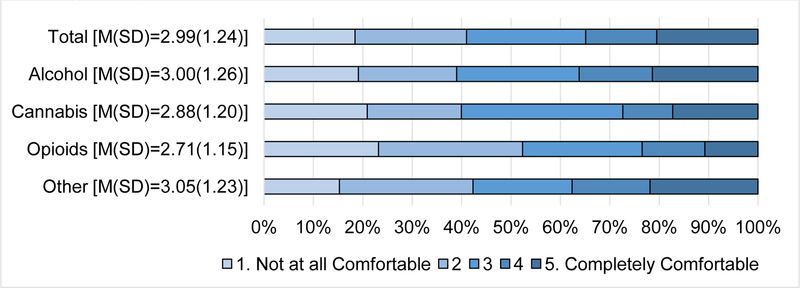
3.4. Primary Substance
The percentages of participants with varying levels of disclosure comfort by different primary substances, as well as the means and standard deviations of disclosure comfort to different recipients, are displayed in Figure 4. This bar graph suggests that participants in the “other” drugs category had the most disclosure comfort, with the largest percentage of participants reporting that they were completely comfortable with disclosure and the smallest percentage reporting that they were not at all comfortable. They appeared to be followed by participants who used alcohol and participants who used cannabis. Participants who used opioids had the lowest disclosure comfort, with the smallest percentage reporting that they were completely comfortable with disclosure and the largest percentage reporting that they were not at all comfortable with disclosure.
Figure 4.
Bar graph indicating percentages of participants with varying levels of disclosure comfort by primary substance
Results of an ANOVA confirmed statistically significant mean differences in disclosure comfort by primary substance, but with a small effect size [F(3,1830)=2.633, p=0.048,ηp2=0.004]. Post-hoc comparisons with LSD adjustments confirmed that participants in the “other” category reported greater disclosure comfort than participants who used opioids [MDiff (SE)=0.330(0.132), p=0.012]. Additionally, participants who used alcohol reported greater disclosure comfort than participants who used opioids [MDiff (SE)=0.279(0.129), p=0.030]. All other group differences by primary substance were not statistically significant.
3.5. Other Socio-Demographic and Clinical Characteristics
Results of simultaneous linear regression analyses examining socio-demographic and clinical characteristics as predictors of disclosure comfort are included in Table 2. Dummy codes representing primary alcohol, cannabis, and “other” drug use were entered into the regression to enable comparisons between participants who primarily used these substances and those who primarily used opioids. Age and age at first use were centered to facilitate meaningful interpretation of intercepts. Because simultaneous regression analyses were used, all associations between predictors and disclosure comfort reported below are dependent upon all of the other covariates included in the regression analyses.
Table 2.
Simultaneous linear regression analyses predicating disclosure comfort from socio-demographic and clinical characteristics, B (SE)
| Overall | Family | Friends | Co-Workers | First-Time Acquaintances | Public Setting | Media | |
|---|---|---|---|---|---|---|---|
| Intercept | 2.06 (0.36)** | 2.06 (0.41)** | 2.85 (0.40)** | 1.71 (0.47)** | 1.96 (0.47)** | 2.04 (0.46)** | 1.75 (0.48)** |
| Socio-Demographics | |||||||
| Age | 0.01 (0.01)** | 0.02 (0.01)** | 0.02 (0.01)** | 0.02 (0.01)** | 0.02 (0.01)** | 0.02 (0.01)** | 0.01 (0.01)* |
| Gender: Male | 0.13 (0.06)* | 0.09 (0.07) | −0.06 (0.06) | 0.29 (0.07)** | 0.19 (0.07)** | 0.15 (0.07)* | 0.12 (0.08) |
| Race: White, Non-Hispanic | −0.04 (0.06) | 0.01 (0.07) | 0.05 (0.07) | 0.07 (0.08) | −0.01 (0.08) | −0.15 (0.07)* | −0.17 (0.08)* |
| Sexual Orientation: Heterosexual | 0.04 (0.08) | 0.09 (0.07) | −0.09 (0.09) | 0.01 (0.10) | 0.04 (0.10) | 0.04 (0.10) | 0.13 (0.10) |
| Education: Some College or More | −0.19 (0.06)** | −0.21 (0.06)** | −0.15 (0.06)* | −0.41 (0.07)** | −0.41 (0.07)** | −0.11 (0.07) | −0.09 (0.07) |
| Employment Status: Employed | 0.01 (0.06) | 0.12 (0.07)+ | 0.02 (0.07) | 0.06 (0.08) | −0.10 (0.08) | 0.01 (0.08) | −0.05 (0.08) |
| Co-Occurring Psychiatric Disorder | −0.07 (0.06) | −0.11 (0.07) | −0.15 (0.07)* | −0.03 (0.08) | −0.08 (0.08) | 0.01 (0.08) | −0.07 (0.08) |
| Criminal Justice Involvement | −0.09 (0.15) | −0.03 (0.17) | 0.05 (0.16) | −0.01 (0.19) | −0.08 (0.19) | −0.25 (0.19) | −0.24 (0.19) |
| Substance Use History | |||||||
| Primary Substance | |||||||
| Alcohol | 0.15 (0.13) | 0.11 (0.15) | 0.02 (0.15) | 0.22 (0.17) | 0.34 (0.17)* | 0.08 (0.17) | 0.12 (0.17) |
| Cannabis | 0.25 (0.15)+ | 0.33 (0.17)* | 0.32 (0.17)* | 0.28 (0.19) | 0.33 (0.19)+ | 0.10 (0.19) | 0.15 (0.19) |
| Other | 0.28 (0.13)* | 0.16 (0.15) | 0.28 (0.15)+ | 0.18 (0.17) | 0.48 (0.17)** | 0.29 (0.17)+ | 0.28 (0.17) |
| Number of Problem Substances | 0.04 (0.02)* | 0.01 (0.02) | 0.05 (0.02)* | 0.03 (0.03) | 0.05 (0.03)+ | 0.05 (0.03)* | 0.06 (0.03)* |
| Age of First Use | −0.02 (0.01)** | −0.01 (0.01) | −0.02 (0.01)** | −0.02 (0.01)** | −0.02 (0.01)** | −0.02 (0.01)* | −0.01 (0.01) |
| SUD Diagnosis | 0.07 (0.08) | 0.11 (0.09) | −0.04 (0.09) | 0.18 (0.11)+ | 0.09 (0.11) | 0.08 (0.10) | 0.01 (0.01) |
| Recovery History and Management | |||||||
| Years Since Problem Resolution | 0.01 (0.01)** | 0.01 (0.01)** | 0.01 (0.01)** | 0.02 (0.01)** | 0.01 (0.01)** | 0.02 (0.01)** | 0.02 (0.01)** |
| Resolution Attempts | 0.01 (0.01)* | 0.01 (0.01) | 0.01 (0.01) | 0.01 (0.01)+ | 0.01 (0.01) | 0.01 (0.01)** | 0.01 (0.01)** |
| Recovery Support Service Utilization | 0.17 (0.08)* | 0.07 (0.09) | 0.01 (0.08) | 0.10 (0.10) | 0.18 (0.10)+ | 0.35 (0.10)** | 0.33 (0.10)** |
| Treatment Utilization | −0.03 (0.08) | 0.29 (0.08)** | 0.24 (0.08)** | −0.16 (0.10) | −0.19 (0.10)* | −0.17 (0.10)+ | -0.18 (0.10)+ |
| Mutual-Help Organization Regular Use | 0.12 (0.07)+ | 0.34 (0.08)** | 0.23 (0.08)** | 0.10 (0.09) | −0.02 (0.09) | 0.01 (0.09) | 0.05 (0.09) |
| Alcohol Medication (Current + Lifetime) | 0.08 (0.13) | 0.23 (0.14) | 0.23 (0.14) | 0.20 (0.16) | −0.10 (0.16) | −0.05 (0.16) | −0.02 (0.17) |
| Opioid Medication (Current + Lifetime) | 0.05 (0.14) | 0.29 (0.16)+ | 0.01 (0.16) | 0.08 (0.18) | 0.01 (0.18) | −0.06 (0.18) | −0.05 (0.18) |
| Abstinence | 0.38 (0.06)** | 0.35 (0.06)** | 0.31 (0.06)** | 0.42 (0.07)** | 0.44 (0.07)** | 0.43 (0.07)** | 0.33 (0.07)** |
| Adjusted R2 Total | 0.12** | 0.13** | 0.11** | 0.12** | 0.08** | 0.09** | 0.06** |
Note:
p≤0.10
p≤0.05
p≤0.01
VIF all below 2, indicating multicollinearity not affecting analyses.
Regarding disclosure comfort across all disclosure recipients, participants who were older, male, and had less than a college education reported more overall disclosure comfort, controlling for all other socio-demographic and clinical characteristics. Additionally, participants who used “other” drugs reported greater overall disclosure comfort than those who used opioids. Participants who had a higher number of problem substances, were younger when they first used substances, had more time since problem resolution, had more resolution attempts, had used recovery support services, and were abstinent had more overall disclosure comfort.
Table 2 also includes covariates of disclosure comfort to specific disclosure recipients. Participants who were older, had more years since problem resolution, and who were abstinent consistently reported greater disclosure comfort to all disclosure recipients, controlling for all other socio-demographic and clinical characteristics. Other covariates of disclosure comfort varied by disclosure recipient. Some similarities were observed in covariates of disclosure comfort to family and friends, to co-workers and first-time acquaintances, and in public settings and the media. Participants with less than a college education and participants who had utilized treatment and mutual-help organizations reported more disclosure comfort to family and friends. Participants reporting cannabis had more disclosure comfort to family and friends than participants reporting opioids. Participants without a co-occurring psychiatric disorder, who used more problem substances, and were younger when they first used substances also had more disclosure comfort to friends specifically.
Regarding disclosure to co-workers and first-time acquaintances, participants who were men, had less than a college education, and were younger when they first used substances reported more disclosure comfort, controlling for all other socio-demographic and clinical characteristics. In addition, participants reporting alcohol and “other” drugs had more disclosure comfort to first-time acquaintances than participants reporting opioids, and participants who had not utilized treatment had more disclosure comfort to first-time acquaintances. Regarding disclosure in public settings and in the media, participants who were people of color, reporting more problem substances, who had more resolution attempts, and had utilized recovery support services reported greater comfort. Additionally, participants who were male and were younger when they first used substances reported greater disclosure comfort in public settings.
4. DISCUSSION
This study examined disclosure comfort among a nationally representative sample of U.S. adults who have resolved an AOD problem. As hypothesized, results suggest that disclosure comfort is related to three dimensions: time since problem resolution, closeness of relationship, and primary drug. That is, disclosure comfort increases over time and differs by disclosure recipient and primary drug. Participants initiating recovery had low to moderate disclosure comfort, which appeared to increase only slightly over the first five years since problem resolution. Disclosure comfort continues to gradually but steadily increase over the next 40 years but remains at a moderate level. As theorized by the Disclosure Process Model, it is plausible that some individuals who have been in recovery longer have accrued positive experiences with disclosure that, in turn, result in slightly more disclosure comfort over time (Chaudoir & Fisher, 2011). It is also possible that individuals who have been in recovery longer are more likely to have stably resolved their AOD problem and perhaps developed a new and more positive perspective on their experience. These individuals may also be more likely to perceive AOD problems as treatable health conditions, which is associated with lower stigma (McGinty, Goldman, Pescosolido, & Barry, 2015). Indeed, participants with other indicators of successfully resolving their AOD problem, including being abstinent and having used recovery services, also had greater disclosure comfort. Participants who have been in recovery for longer may also have developed more self-confidence and self-esteem (Kelly et al, 2018), resulting in greater disclosure comfort. Nonetheless, participants who had resolved their AOD problem a long time ago (i.e., 40 years) reached only moderate levels of disclosure comfort. It is possible that fear of discrimination and other barriers to disclosure persist long after AOD problems have been resolved (Vilsaint et al, in press).
In support of the Interpersonal Process Model of Intimacy (Reis & Shaver, 1988), participants on average reported the most comfort disclosing in more intimate relationships, including to family and friends, and the least comfort disclosing in less intimate relationships and settings, including in the media. Relationship closeness had a large effect size in disclosure comfort, underscoring the importance of closeness in disclosure. Greater trust and perceived safety in disclosure to those closest may mediate this observation. It is likely also that people who have resolved an AOD problem may receive more benefits from disclosing to this innermost circle as these individuals also have the greatest motivation and capacity to assist them in their recovery. In short, they care more. In other words, there may be different goals in disclosing to family and friends than in disclosing in more public settings and in the media with obtaining recovery support related to the former, and giving/sharing recovery support related to the latter. It is important to note, however, that there was variability in disclosure comfort to different sources with at least some participants reporting being not at all comfortable and others reporting being completely comfortable disclosing to each type of disclosure recipient.
Participants who had resolved problems with opioids generally reported lower disclosure comfort than participants who had resolved problems with alcohol and drugs other than cannabis. People who had resolved problems with opioids may represent a particularly vulnerable group, potentially experiencing and fearing greater stigma than people who have resolved other AOD problems while having less access to recovery capital and experiencing lower quality of life, particularly in the initial years of recovery (Earnshaw et al., in press; Kelly et al., 2018). We hypothesized that people who had resolved problems with illicit drugs would report lower disclosure comfort than people who had resolved problems with licit drugs. Yet, people who had resolved problems with drugs other than opioids and cannabis (e.g., cocaine, methamphetamine, hallucinogens), which are often illicit, reported higher disclosure comfort. It is possible that some of these drugs were prescribed (e.g., benzodiazepines) and therefore were licit. It is also possible that stigma associated with these drugs is weaker than stigma associated with opioids, leading to greater comfort with disclosure. Notably, the effect size of primary drug on disclosure comfort was small, suggesting it may play a more minor role in disclosure comfort than other characteristics of the disclosure process (e.g., relationship closeness). Additionally, there was also variability in disclosure comfort across substance types with some participants reporting being not at all comfortable and others reporting being completely comfortable disclosing within each substance type. Future research should be conducted to better understand nuances of stigma and disclosure comfort associated with different types of drugs and substances.
Other socio-demographic and clinical characteristics that were consistently associated with disclosure comfort included age and abstinence. Participants who were older were more comfortable with disclosure, even after controlling for years since problem resolution. As has been suggested in the racism literature (Gee, Walsemann, & Brondolo, 2012), it is possible that resilience to stigma changes across the lifespan. People may therefore become more resilient and therefore more comfortable with disclosing histories of AOD problems as they become older; in short, they don’t care as much what other people think. Moreover, participants who were abstinent were more comfortable with disclosure. Disclosure recipients may more readily believe that individuals have successfully resolved AOD problems if they are fully abstinent, leading individuals in recovery to feel more comfort with disclosure. An individual who has resolved a problem with opioids, but continues to drink alcohol, may experience greater stigma from others regarding their continued substance use and therefore feel less comfortable disclosing that they formerly had a problem with opioids. Several other socio-demographic (e.g., gender, race/ethnicity, sexual orientation, education) and clinical (e.g., number of problem substances, age of first use, resolution attempts, treatment utilization) characteristics were associated with disclosure comfort. Future research should continue to identify which individuals feel greater comfort with disclosure and why.
4.1. Strengths, Limitations, and Future Directions
This is the first known study to examine disclosure among a nationally representative sample of U.S. adults who have resolved AOD problems. Disclosure represents a gateway to relational processes that may support or hinder recovery efforts, and yet has been understudied among people in recovery. Unlike studies that focus on individuals recruited from treatment or recovery services, who are often in the early stages of recovery and/or recovering from a limited group of substances, this sampling strategy enabled us to examine covariates of disclosure comfort among individuals with a wide range of time since problem resolution and histories with different problem substances.
The current study focused on disclosure comfort, not on actual disclosure behavior. Future research should examine the role of disclosure comfort in actual disclosure behavior to determine the extent to which comfort with disclosure leads to more disclosures as well as how such disclosure may help diminish shame and fear of discrimination. Future research may also examine covariates of disclosure behaviors. The current study was cross-sectional, and therefore conclusions regarding causal associations between variables cannot be made. Moreover, it is possible that some of the trends observed in the analyses of associations between time in recovery and disclosure comfort could be due to cohort effects. Future longitudinal research that follows people who have resolved AOD problems over time can clarify potentially causal associations and trajectories of disclosure over time. Longitudinal research could also inform understanding of whether relationship intimacy leads to greater disclosure, and/or disclosure leads to greater relationship intimacy among people in recovery. This study documents variability in disclosure comfort but does not provide insight into why disclosure comfort varies. Future research should continue to examine why people who have resolved AOD problems report varying disclosure comfort depending on when, to whom, and what they disclose.
4.2. Conclusions
AOD problems are highly stigmatized in the U.S. and worldwide (Room et al., 2001), and many people do not feel comfortable disclosing their AOD recovery to others despite sometimes years and decades of stable recovery. Disclosure may enhance recovery if it leads to greater social support from others, or hinder recovery if it leads to discrimination. Future research is needed to continue to understand the role of disclosure and related interpersonal processes in recovery trajectories. If found that aspects of disclosure processes are associated with recovery, it will become important to develop interventions that help people make decisions regarding whether, when, and to whom to disclose their AOD history and/or recovery status and to develop skills to disclose in effective ways. Ultimately, a greater focus on disclosure within research and treatment may support the recovery efforts of the millions of U.S. adults who have experienced an AOD problem.
HIGHLIGHTS.
Research on disclosure may inform efforts to support people in recovery.
Disclosure comfort increases with time, yet only reaches a moderate level.
Individuals are most comfortable disclosing in close relationships.
Individuals recovering from opioid problems have the least disclosure comfort.
Acknowledgments
Role of Funding Sources: This work was supported by the National Institute on Drug Abuse (NIDA; K01DA042881, VAE) and National Institute on Alcohol Abuse and Alcoholism (NIAAA; K23AA025707, BGB; K24AA022136, JFK) and by an anonymous donation to the MGH Recovery Research Institute. Funders were not involved in the study design; collection, analysis, or interpretation of the data; write up of the report; or decision to submit the article for publication. The content is solely the responsibility of the authors and does not necessarily represent the official views of its funders.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declarations of Interest: None. The authors declare that they have no competing interests. They alone are responsible for the content and writing of the paper.
REFERENCES
- Battaglia MP, Izrael D, Hoaglin DC, & Frankel MR (2009). Practical considerations in raking survey data. Survey Practice, 2(5), 1–37. https://doi.org/http://surveypractice.org/2009/06/29/raking-survey-data/ [Google Scholar]
- Brewer MK (2006). The contextual factors that foster and hinder the process of recovery for alcohol dependent women. Journal of Addictions Nursing, 17(3), 175–180. [Google Scholar]
- Centers for Disease Control and Prevention (CDC), National Center for Health Statistics (NCHS) (2013). Unweighted Response Rates for the National Health and Nutrition Examination Survey (NHANES) 2011–2012 CDC National Center for Health Statistics, Hyattsville, MD: Available at: https://www.cdc.gov/nchs/nhanes/response_rates_cps.htm. Accessed November 30, 2017. [Google Scholar]
- Chaudoir S, & Fisher JD (2011). The Disclsoure Process Model: Understanding disclosure decision-making and post-disclosure outcomes among people living with a concealable stigmatized identity. Psychological Bulletin, 136(2), 236–256. 10.1037/a0018193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corrigan P, & Matthews A (2003). Stigma and disclosure: Implications for coming out of the closet. Journal of Mental Health, 12(3), 235–248. [Google Scholar]
- Dennis M, Titus J, White M, Unsickler J, Hodgkins D (2002). Global Appraisal of Individual Needs (GAIN): Administration Guide for the GAIN and Related Measures Chestnut Health Systems, Bloomington, IL: Available at: https://chestnut.app.box.com/v/GAIN-I-Materials/file/63671257181. Accessed November 30, 2017. [Google Scholar]
- Dobkin PL, Civita M De, Paraherakis A, & Gill K (2002). The role of functional social support in treatment retention and outcomes among outpatient adult substance abusers. Addiction, 97(3), 347–356. [DOI] [PubMed] [Google Scholar]
- Earnshaw VA, Bogart LM, Menino DD, Kelly JF, Chaudoir SR, Reed NM, & Levy S (in press). Disclosure, stigma, and social support among young people receiving treatment for substance use disorders and their caregivers: A qualitative analysis. International Journal of Mental Health and Addiction 10.1007/s11469-018-9930-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Earnshaw V, Smith L, & Copenhaver M (2013). Drug addiction stigma in the context of methadone maintenance therapy: An investigation into understudied sources of stigma. International Journal of Mental Health and Addiction, 11(1), 110–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gee GC, Walsemann KM, & Brondolo E (2012). A life course perspective on how racism may be related to health inequities. American Journal of Public Health, 102, 967–974. 10.2105/AJPH.2012.300666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- GfK. (2013). KnowledgePanel design summary Available at: http://www.Knowledgenetworks.Com/Knpanel/Docs/Knowledgepanel(R)-Design-Summary-Description.pdf. Accessed August 8, 2018.
- Grant BF, Goldstein RB, Saha TD, Patricia Chou S, Jung J, Zhang H, … Hasin DS (2015). Epidemiology of DSM-5 alcohol use disorder results from the national epidemiologic survey on alcohol and related conditions III. JAMA Psychiatry, 72(8), 757–766. 10.1001/jamapsychiatry.2015.0584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hutchinson PL, Mahlalela X, & Yukich J (2007). Mass media, stigma, and disclosure of HIV test results: multilevel analysis in the Eastern Cape, South Africa. AIDS Education & Prevention, 19(6), 489–510. [DOI] [PubMed] [Google Scholar]
- Kelly JF, Abry AW, Milligan CM, Bergman BC, & Hoeppner BB (2018). On being “in recovery”: A national study of prevalence and correlates of adopting or not adopting a recovery identity among individuals resolving drug and alcohol problems. Psychology of Addictive Behaviors, 32(6), 595–604. [DOI] [PubMed] [Google Scholar]
- Kelly JF, Bergman B, Hoeppner BB, Vilsaint C, & White WL (2017). Prevalence and pathways of recovery from drug and alcohol problems in the United States population: Implications for practice, research, and policy. Drug and Alcohol Dependence, 181, 162–169. 10.1016/j.drugalcdep.2017.09.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JF, Greene MC, & Bergman BG (2018). Beyond abstinence: Changes in indices of quality of life with time in recovery in a nationally representative sample of U.S. adults. Alcoholism: Clinical and Experimental Research, 42(4), 770–780. 10.1111/acer.13604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JF, Wakeman SE, & Saitz R (2015). Stop talking “dirty”: Clinicians, language, and quality of care for the leading cause of preventable death in the United States. American Journal of Medicine, 128(1), 8–9. 10.1016/j.amjmed.2014.07.043 [DOI] [PubMed] [Google Scholar]
- Kelly JF, & Westerhoff CM (2010). Does it matter how we refer to individuals with substance-related conditions? A randomized study of two commonly used terms. International Journal of Drug Policy, 21(3), 202–207. 10.1016/j.drugpo.2009.10.010 [DOI] [PubMed] [Google Scholar]
- Laurenceau J, Barrett LF, & Pietromonaco PR (1998). Intimacy as an interpersonal process: The importance of self-disclosure, partner disclosure, and perceived partner responsiveness, 74, 1238–1251. 10.1037//0022-3514.74.5.1238 [DOI] [PubMed] [Google Scholar]
- Manne S, Rini C, Goldstein L, Ostroff J, Fox K, & Grana G (2004). The interpersonal process model of intimacy: The role of self-disclosure, partner disclosure, and partner responsiveness in interactions between breast cancer patients and their partners. Journal of Family Psychology, 18(4), 589–599. 10.1037/0893-3200.18.4.589 [DOI] [PubMed] [Google Scholar]
- McGinty EE, Goldman HH, Pescosolido B, & Barry CL (2015). Portraying mental illness and drug addiction as treatable health conditions: Effects of a randomized experiment on stigma and discrimination. Social Science & Medicine, 126, 73–85. [DOI] [PubMed] [Google Scholar]
- Miller WR, & Del Boca FK (1994). Measurement of drinking behavior using the Form 90 family of instruments. Journal of Studies on Alcohol, 12, 112–118. [DOI] [PubMed] [Google Scholar]
- Murphy S, & Irwin J (1992). “Living with the dirty secret”: Problems of disclosure for methadone maintenance clients. Journal of Psychoactive Drugs, 24(3), 257–264. [DOI] [PubMed] [Google Scholar]
- Pachankis JE, Hatzenbuehler ML, Wang K, Burton CL, Crawford FW, Phelan JC, & Link BG (2018). The burden of stigma on health and well-being: A taxonomy of concealment, course, disruptiveness, aestetics, origin, and peril across 93 stigmas. Personality and Social Psychology Bulletin, 44(4), 451–474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reis HT, & Shaver P (1988). Intimacy as an interpersonal process. Handbook of Personal Relationships, 367–389. 10.1016/0045-7825(81)90049-9 [DOI] [Google Scholar]
- Romo LK, Dinsmore DR, & Watterson TC (2016). “Coming out” as an alcoholic: How former problem drinkers negotiate disclosure of their nondrinking identity. Health Communication, 31(3), 336–345. 10.1080/10410236.2014.954090 [DOI] [PubMed] [Google Scholar]
- Room R, Rehm J, Trotter RT II, Paglia A, & Üstün TB (2001). Cross-cultural views on stigma valuation parity and societal attitudes towards disability. Disability and Culture: Universalism and Diversity, 247–291. [Google Scholar]
- Roose R, Fuentes L, & Cheema M (2012). Messages about methadone and buprenorphine in reality television: A content analysis of Celebrity Rehab with Dr. Drew. Substance Use & Misuse, 47(10), 1117–1124. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration (2017). Key substance use and mental health indicators in the United States: Results from the 2016 National Survey on Drug Use and Health (HHS Publication No. SMA 17–5044, NSDUH Series H-52) Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration; Retrieved from https://www.samhsa.gov/data/. Accessed August 8, 2018. [Google Scholar]
- Simmonds L, & Coomber R (2009). Injecting drug users: A stigmatised and stigmatizing population. International Journal of Drug Policy, 20(2), 121–130. 10.1016/j.drugpo.2007.09.002 [DOI] [PubMed] [Google Scholar]
- Tempalski B, Friedman R, Keem M, Cooper H, & Friedman SR (2007). NIMBY localism and national inequitable exclusion alliances: The case of syringe exchange programs in the United States. Geoforum, 38, 1250–1263. 10.1016/j.geoforum.2007.03.012 [DOI] [PMC free article] [PubMed] [Google Scholar]