Abstract
Aim:
Biofeedback therapy, whether administered at home or in office settings is effective for dyssynergic defecation (DD). Whether home biofeedback improves quality of life (QOL) and is cost-effective when compared to office biofeedback is unknown.
Methods:
QOL was assessed in 8 domains (SF-36) at baseline and after treatment (3 months), alongside economic evaluation during a RCT comparing home and office biofeedback in patients with DD (Rome III). Costs related to both biofeedback programs were estimated from hospital financial records, study questionnaires and electronic medical records. A conversion algorithm (Brazier) was used to calculate the patient’s QALY (quality-adjusted life years) from SF-36 responses. Cost-effectiveness was expressed as incremental costs per QALY between treatment arms.
Results:
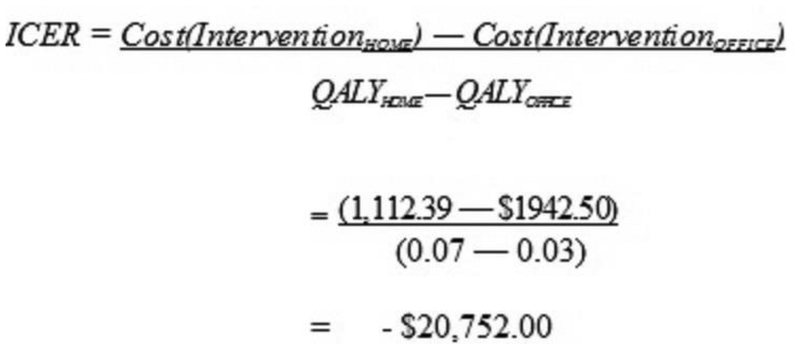
100 patients (96 female, 50 in each treatment arm) with DD participated. Six of 8 QOL domains improved (p<0.05) in office biofeedback, while 4/8 domains improved (p<0.05) in home biofeedback; home was non-inferior to office biofeedback.. The median cost per patient was significantly lower (p<0.01) for home biofeedback $1,112.39 (IQR $826- $1430) than office $1,943 (IQR $1622- $2369) resulting in a cost difference of $830.11 The median QALY gained during the trial was 0.03 for office biofeedback and 0.07 for home biofeedback (p=NS). The incremental cost effectiveness ratio was $20,752.75 in favor of home biofeedback.
Conclusions:
Biofeedback therapy significantly improves QOL in patients with DD regardless of home or office setting. Home biofeedback is a cost-effective treatment option for DD compared to office biofeedback, and offers the potential of treating many more patients in the community.
INTRODUCTION
Chronic constipation affects 15–20% of the population and its prevalence increases with age1,2. There are three recognized heterogeneous and overlapping subtypes: slow-transit constipation (STC), irritable bowel syndrome-constipation predominant (IBS-C) and dyssynergic defecation (DD)3,5. In tertiary care settings, the prevalence of DD among patients with chronic constipation is 40–50%3,6. DD is characterized by the inability of the abdominal, rectal, pelvic floor and anal sphincter muscles to properly coordinate the process of defecation, resulting in a functional anorectal obstruction and difficulty with evacuation3,5,7.
Previous studies have shown that constipated patients generally have decreased quality of life (QOL) and psychosocial dysfunction3,8. When compared to STC, patients with DD have both greater psychological distress and impaired QOL8. Several RCTs have shown that biofeedback therapy improves bowel dysfunction and corrects the underlying pathophysiology in patients with DD9–11. However, whether biofeedback improves QOL in patients with dyssynergic constipation is not known.
Currently, the standard method of administering biofeedback therapy is as an office-based outpatient procedure9–11. Furthermore, it is offered only in a few tertiary care motility centers in the USA and elsewhere or by physiotherapists. There is clearly a dearth of training centers and availability of this treatment, despite the high prevalence of this condition. Consequently, a home-based biofeedback program that can be offered in the community, outside of hospitals and offices may substantially broaden the availability of such a treatment. A recent randomized clinical trial compared the efficacy of home biofeedback against the standard office biofeedback and concluded that these 2 treatment modalities have equivalent effects in improving constipation symptoms, as well as colorectal function12.
In today’s economic climate, especially with rising health care costs, aside from efficacy, treatment modalities must also be able to improve overall quality of life and be cost-effective. This information is important to third-party payors, health economists and policy makers who grapple with difficult decisions in properly allocating limited healthcare resources.
Here, we performed a QOL and economic evaluation alongside a randomized controlled trial that compared the efficacy of home biofeedback against the standard office biofeedback in patients with dyssynergic defecation and chronic constipation. The QOL and the cost-effectiveness data were all planned a priori. We tested the following hypotheses: (1) biofeedback will improve QOL in patients with DD; (2) the QOL changes in patients who received home biofeedback will not be equivalent to those who received the standard office biofeedback; and (3) home biofeedback is a more cost-effective alternative to the standard office biofeedback.
METHODS
STUDY DESIGN & PATIENT POPULATION
A consecutive sample of 100 patients who were diagnosed with dyssynergic defecation and seen at a tertiary care center were invited to participate in the study from 2006 to 2010. Dyssynergic defecation was diagnosed when constipated patients (ages 18 to 65 years) satisfied the following Rome III criteria: (1) exhibited dyssynergic pattern on anorectal manometry (ARM), and (2) either prolonged difficulty with expelling a simulated stool (>1 minute), or prolonged delay (>20% marker retention) in colonic transit9,12. Details on the exclusion criteria were previously described12. Patients were then randomized to receive either the standard office biofeedback or the home biofeedback program12. Random numbers generated in advance were placed into sequentially numbered opaque envelopes, sealed, and used for subject assignment. The study was approved by University of Iowa IRB 200209080 and registered in Clinical Trials.gov No. NCT03202771.
Home Biofeedback
Patients in this treatment arm had a baseline visit and 3 brief monthly office visits (total of 4 visits) with a nurse specialist to check up on their progress. The patients were taught how to use the home trainer device on the first visit12. A reusable dual sensor anorectal probe was connected to a handheld pressure monitor (Anatoner, Protech, Hyderabad, India) displaying rectal and anal pressures. The patients were instructed to attempt 15-bearing down maneuvers at least twice daily throughout the study period. With anal relaxation, more lights would illuminate on the LCD display. Fewer lights were associated with paradoxical or increased anal contraction on bearing down. Thus, this device provided patients with instant feedback about their performance.
Office Biofeedback
The standard office biofeedback therapy consisted of biweekly, 1-hour sessions with a nurse specialist/therapist (total of 6 visits) during the 3-month study period9,12. The goals of biofeedback therapy consisted of 3 parts: (1) instructions on diaphragmatic breathing technique to enhance the push effort, (2) improve recto-anal coordination by increasing the intra-abdominal/intra-rectal pressures with synchronized relaxation of the anal sphincters using visual and verbal feedback from manometry, (3) train patients to efficiently pass an artificial stool9,12.
Both treatment groups were also taught proper abdominal muscle coordination exercises to improve the push effort during defecation. Patients were instructed to hold their breaths for 15 seconds and practice this for 20 minutes twice a day.
DATA ASSESSMENT & OUTCOME MEASURES
For this study, we used the SF-36, cost estimation, quality-adjusted life years (QALYs), cost/QALY and incremental cost-effective ratio (ICER) for assessing the outcomes.
Quality of life
The SF-36 is a 36-item, self-reported questionnaire that evaluates 8 domains of physical and mental health-related quality of life: physical functioning (PF), role-physical (RP), bodily pain (BP), general health (GH), vitality (VT), social functioning (SF), role-emotional (RE), and mental health (MH). The 8 domains have proven psychometric properties, reliability and validity8,13.
Cost-effectiveness analysis
Costs
We estimated the costs by using micro-costing analysis, a process that identifies each resource used, measures the quantity of resources used, and applies unit prices to the resources. Cost data was then adjusted to uniformly reflect 2009 levels. Data sources included patients’ medical electronic health records, hospital billing records, and study questionnaires.
We captured costs, from a societal perspective, by incorporating both direct (health care system costs) and indirect costs to the patient (such as patient’s work loss costs due to appointments). We used the equation below to estimate the cost in each treatment arm.
In this equation, each represents, for the ith patient, total costs (TC), outpatient hospital costs (H), physician costs (P), equipment costs (E), home treatment costs (HT), work-loss hours associated with appointments (WL), travel time costs associated with appointments (TT), and transportation costs (T).
Hospital costs: By using the hospital billing records, we were able to estimate the cost to the hospital per office biofeedback visit. We also considered the patient’s age into our calculation. If they were ≥ 65 years old, the hospital costs were based on the prevailing Medicare reimbursement rate. Otherwise, the patients are assigned a private insurance rate. Since there were 6 office biofeedback visits, this value was multiplied by 6, to arrive at total hospital outpatient costs. In contrast, home biofeedback was a new biofeedback modality and not associated with any billable ICD-9 CM codes. The average nurse wage per hour (2007 Bureau of Labor & Statistics) was $ 30.69. Since the nurse would spend 15 minutes with the patient per visit (in the home biofeedback arm) to check device function, answer patient questions and adjust parameters of the device, it would incur a nursing cost of $7.68 per visit. Since there were 4 visits in the home biofeedback arm, this would lead to an estimated amount of $30.69 for hospital costs.
Physician costs: A similar methodology was applied to estimate the physician costs for office biofeedback using an outpatient ICD-9 CM code, multiplied by 6 visits. This was assigned a value of $90 per visit. In biofeedback centers that are supervised by a gastroenterologist or physician, in addition to the hospital costs, a physician charge is assigned to the treatment for providing assistance to the nurse with biofeedback treatment, meeting patient, interpretation of manometry findings and generation of report.
Equipment costs: Since equipment cost for office biofeedback is currently bundled with hospital outpatient costs, this variable was assigned a $0 value for the office biofeedback arm. In contrast, the home biofeedback incurred total costs of $244.00, including rental fees for the home biofeedback device and the costs of the disposable anorectal probes.
Home treatment costs: The home biofeedback group was asked to practice 15 bearing-down maneuvers at home at least twice per day and use the home trainer device. Using the stool diary that informed us on how much time the patient spent with the home device, we calculated the total time practiced at home with the patient’s salary per hour multiplied by 0.5 (0.5 was deemed to be a reasonable discounted cost) since patient practiced these maneuvers when they are off work i.e. early morning or at night.
Loss of work salary due to appointments: This variable was calculated by multiplying the patient’s salary per hour with the number of visits and time spent in these appointments. In the office biofeedback, there were 6 visits and the time spent was 2.25 hours. In contrast, the home biofeedback had 4 visits and time spent on these visits was 1.75 hours. The hours spent in these appointments were increased in both groups to account for parking their cars, checking-in, and time spent waiting to be seen by the nurse therapist. However, the home biofeedback group had a shorter appointment time (30 minutes shorter) when compared to the office biofeedback group since the latter group spent time undergoing biofeedback sessions in the office, whereas the home group was a quick check of any performance related issues and adjusting parameters on home device.
Travel time costs: Patient’s home address (taken from hospital medical records) was designated as point A and hospital address as point B. We then obtained the time spent driving from home to the hospital from MapQuest (www.mapquest.com), multiplied by 2 (round trip), the number of sessions and the patients’ salary per hour (SPH).
Transportation costs: To calculate for transportation costs, the round trip miles traveled between the patient’s home and the hospital was obtained from MapQuest (www.mapquest.com). This value was then multiplied by 0.35 (standard reimbursement rate) and the number of trips the patient made during the 3-month period of participation with the study.
Of note, the salary per hour (SPH) was taken from the Bureau of Labor and Statistics website (2007 dollars) using the patient’s job description as documented in their electronic medical record and their state of residence.
QALYs, Costs/QALY and ICER
Health economists have developed numerous algorithms that convert existing health related outcome data to quality-adjusted life years (QALY) for use in cost-effectiveness analysis14–17. Model 10 is a conversion algorithm that uses SF-36 v.1 and v.2 data to SF-6D classification, assigning a value weight to the measured health-related outcome. This results to a utility index value of 0 to 1. A zero value pertains to death while 1 refers to full health. The conversion algorithm was originally derived from a large community sample representative of the UK national population developed by Brazier et al18. The model 10 utility conversion was executed through SAS statistical software. The converted SF-36 patient responses were used as the denominator for the cost-effectiveness equation.
DATA ANALYSIS
Descriptive statistics were computed for all variables including means, standard deviations, medians with Q1 and Q3 for continuous variables and frequencies for categorical variables. T-test for Wilcoxon-rank sum test were used to compare groups depending on the distribution of the data. Chi-square tests were performed to test statistical differences in frequency.
QOL analysis
We used intention-to-treat analysis in the evaluation of QOL data (n=100). All patients had a baseline SF-36. In case of patients who dropped out, the baseline QOL data was forwarded as the end-of-treatment QOL values (last observation carried forward).
Since the QOL data showed improvement from baseline, a one-sided t-test was used to assess within-group statistical significance. In addition, a two-way one-sided t-test (TOST) analysis was used to compare whether the results of home biofeedback group were non-inferior to office biofeedback group.. We used a pre-established delta threshold for each QOL domain. The delta threshold was dependent on the number and psychometric properties of the questions pertaining to each QOL domain. Because of the variable psychometric properties and scores of role physical and role emotional domains, delta thresholds of 25 and 33 score units were used for these domains, and 10 score units for all other domains to be considered statistically significant. If the delta thresholds were not reached, the null hypothesis was rejected and the home biofeedback was deemed non-inferior to office biofeedback on a particular QOL domain.
Cost and cost-effectiveness analyses
In contrast to the QOL analysis, the cost and cost-effectiveness analyses required complete stool diaries and questionnaires to adequately track down cost. For these reasons, we used data from 81 patients who completed the study (17 drop-outs, and another 2 patients with incomplete stool diaries/questionnaires were excluded).
Due to the skewed distribution of the cost and QALY data, Wilcoxon-rank sum test were used to evaluate for statistical significance. An alpha value of at least 0.05 was considered statistically significant. All analyses were performed using SAS Version 9.1 for Windows (Cary, NC). Cost effectiveness analysis used Treeage ® Data 4.0 software, that supports an overlay of probabilistic decision analysis, cost estimation, Monte Carlo simulation models, and sensitivity analyses.
RESULTS
Patient Demographics, baseline symptoms and colorectal function
The study enrolled 100 subjects, 50 (f/m=50/0) were randomized to the Home biofeedback therapy and 50 (f/m=46/4) to the Office biofeedback treatment arm. Table 1 shows that the 2 groups were well matched in terms of mean age, duration of constipation symptoms and baseline symptoms, and that there were no differences. These patients had significant and bothersome constipation at baseline as revealed by the very few complete spontaneous bowel movements (CSBMs) per week, low bowel satisfaction visual analog scores (VAS), harder stools as revealed by the low stool consistency scores (Bristol stool form scale) and higher percentage of patients reporting a feeling of incomplete evacuation. They also had comparable rates of abnormal colonic transit study and abnormally prolonged mean balloon expulsion time (Table 1). On average, patients spent 45–60 minutes for an office-based biofeedback treatment session and 25–30 minutes for each home biofeedback treatment session.
Table 1.
Patient demographics, baseline symptoms and colorectal function, ROM= radiopaque markers
| Demographic Data |
Office Biofeedback (n=50) | Home Biofeedback (n=50) |
|---|---|---|
| Age, years (Mean ± SD) | 42.4 ± 15.4 | 37.1 ± 11.9 |
| Duration of constipation, years (Mean) | 15 | 12 |
| Subjective Measures | ||
| CSBMs per Week, mean (SEM) | 1.2 (0.3) | 0.68 (0.17) |
| Bowel Satisfaction VAS (0–100), mean (SEM) | 18.4 (2.9) | 16.3 (2.4) |
| Stool Consistency (Bristol, 1–7), mean (SEM) | 3.2 (0.2) | 3.4 (0.15) |
| % Stools with Incomplete Evacuation | 76% | 70% |
| Objective Parameters | ||
| % ROM Mean Retention | 45% | 50% |
| Balloon Expulsion Time (Seconds), Mean ± SEM) | 60 ± 11 | 70 ± 12 |
Quality of Life (QOL)
The QOL domains improved significantly from baseline in both the office and home biofeedback treatment arms (Table 2). Six of 8 domains in the office biofeedback group and 4 of 8 domains in the home biofeedback group respectively were significantly higher emphasizing the degree of improvement observed in these patients following biofeedback therapy. It is worth emphasizing that biofeedback, in both the office and home settings, did not cause worsening of QOL in any of the domains, when compared to baseline values. For between group comparisons (Table 3), the TOST analysis with a predefined delta bound threshold revealed that both treatment arms have similar effects in improving QOL, and that the home biofeedback was non-inferior to office biofeedback treatment..
Table 2.
Effects of (A) Office Biofeedback therapy on QOL domains (n=45), and (B) Home Biofeedback on QOL domains (n=38).
| QOL Domains | Baseline | 3 months | Difference ± SEDiff | P |
|---|---|---|---|---|
| Role Emotional | 68.8 | 82.7 | 13.9 ± 4.7 | 0.005 |
| Mental Health | 67.2 | 72.2 | 4.8 ± 2.1 | 0.015 |
| Social Functioning | 53.3 | 59.8 | 6.6 ± 2.5 | 0.005 |
| Role Physical | 52.0 | 59.7 | 7.8 ± 3.9 | 0.03 |
| Vitality | 43.6 | 50.0 | 6.4 ± 2.5 | 0.005 |
| Bodily Pain | 54.2 | 60.5 | 6.4 ± 2.6 | 0.01 |
| Physical Functioning | 79.6 | 82.1 | 2.6 ± 1.6 | 0.065 |
| General Health | 52.8 | 53.4 | 0.6 ± 1.9 | 0.38 |
| QOL Domains | Baseline | 3 months | Difference ± SEDiff | P |
| Role Emotional | 69.7 | 77.6 | 7.9 ± 2.9 | 0.005 |
| Mental Health | 69.1 | 70.7 | 1.6 ± 1.9 | 0.20 |
| Social Functioning | 58.1 | 60.8 | 2.7 ± 2.3 | 0.12 |
| Role Physical | 60.2 | 71.1 | 10.9 ± 4.9 | 0.015 |
| Vitality | 42.4 | 46.4 | 3.9 ± 2.1 | 0.03 |
| Bodily Pain | 56.8 | 62.4 | 5.6 ± 2.8 | 0.025 |
| Physical Functioning | 82.8 | 85.9 | 3.1 ± 2.1 | 0.075 |
| General Health | 57.0 | 58.0 | 1.0 ± 1.8 | 0.29 |
Table 3.
Office vs. home biofeedback non-inferiority analysis
| QOL Domains | TOST Comparisons | Delta Bound | P value |
|---|---|---|---|
| Role Emotional | −6 (−15.2 to 3.2) | 33 | <0.01 |
| Mental Health | −3.2 (−8 to 1.6) | 10 | 0.01 |
| Social Functioning | −3.9 (−9.6 to 1.8) | 10 | 0.04 |
| Role Physical | −3.1 (−7.4 to 13.7) | 25 | <0.01 |
| Vitality | −2.4 (−7.8 to 3) | 10 | 0.01 |
| Bodily Pain | −0.7 (−7.1 to 5.7) | 10 | 0.01 |
| Physical Functioning | 0.5 (−3.9 to 4.9) | 10 | <0.01 |
| General Health | 0.4 (−3.9 to 4.7) | 10 | 0.01 |
A p-value of <0.05 is considered statistically equivalent
Cost and Cost-effectiveness analysis
From a societal perspective, we found that the home biofeedback incurred a cost of $1112.39 (Q1 $825.59, Q3 $1429.99) and the office biofeedback incurred a cost of $1842.50 (Q1 $1621.70, Q3 $2369), (Table 4). This amounted to a statistically significant cost difference of $830.11 (Q1 $791.11, Q3 $939.90) in favor of the home biofeedback group being less costly. Table 5 outlined the costs incurred per treatment group, QALYs at baseline and 3 months after treatment, QALY change score between 2 time periods, and the average cost ratio per treatment group. The estimated average cost-utility ratios for both office biofeedback ($64,750) and home biofeedback ($15,891.29) fell well within the accepted cost-effective parameters of less than $100,000 per QALY. This meant that both treatment options are independently cost-effective.
Table 4.
Summary of treatment costs in each treatment arm
| Type of costs | Office Biofeedback (n=44) |
Home Biofeedback (n=37) |
||
|---|---|---|---|---|
| Computation | Cost (median, IQR) |
Computation | Cost (median, IQR) |
|
| Hospital costs | 6 sessions x HC per session | $732.78 | 4 sessions x HC per session | $30.69 |
| Physician costs | 6 sessions x PC per session | $625.50 | 4 sessions x PC per session | $90.00 |
| Equipment costs | 0 | $0 | $280 = $100 (device) + 1.5 x $120/probe | $244.00 |
| Home treatment | 0 | $0 | SPH* (estimated data) x 0.5 | $185.80 ($112.30, $325.20) |
| Loss of salary due to appointments | 2.25 hrs x 6 sessions x SPH | $134.73 ($101.79, $357.21) | 1.75 hrs. x 4 sessions x SPH | $142.20 ($79.17, $402.50) |
| Travel time costs | Roundtrip distance x 6 sessions x SPH | $132.50 ($56.60, $345.60) | Roundtrip distance x 4 sessions x SPH | $149.40 ($71.50, $276) |
| Transportation costs | Roundtrip distance x 6 sessions x 0.35 | $203.70 ($48.50, $424) | Roundtrip distance x 4 sessions x 0.35 | $179.20 ($78.10, $259.80) |
| Total costs* | $1942.50 ($1621.70, $2369) | $1112.39($825.59$1429.99 | ||
P value (total costs): <0.001. SPH = salary per hour, taken from the Bureau of labor and statistics (2007) using patient’s job description and state of residence; HC = hospital costs; andPC = physician costs
Table 5.
Average cost ratio per treatment group
| Treatment Group | Costs/Group | QALY Baseline (median, Q1, Q3) | QALY 3 months (median, Q1, Q3) | QALY change score (median, Q1, Q3) | Average Ratio ($/QALY) |
|---|---|---|---|---|---|
| Office biofeedback | $1942.50 | 0.70 (0.59, 0.84) |
0.74 (0.59, 0.89) |
0.03 (−0.01, 0.07) |
$64,750.00 |
| Home biofeedback | $1112.39 | 0.73 (0.63, 0.84) |
0.78 (0.66, 0.89) |
0.07 (0, 0.10) |
$15,891.29 |
The incremental cost-effectiveness ratio (ICER, Figure 1), resulted in a negative cost-effectiveness ratio for the home biofeedback group, indication a strong “dominance” over the office biofeedback alternative as a more effective and cost-saving program.
Figure 1.
Incremental cost-effectiveness ratios (ICER)
DISCUSSION
Biofeedback therapy is now recommended as the first line treatment for patients with chronic constipation and dyssynergic defecation, and is endorsed by the American and European Societies of Neurogastroenterology and Motility11 and the American College of Gastroenterology19 and the American Gastroenterology Association5. Also, in a previous report, we demonstrated that patients with dyssynergic defecation and those with slow transit constipation have significant impairment of both QOL and psychosocial function8. However, a lack of availability, both trained personnel and centers, the need for multiple hospital visits and insurance hurdles from claims that biofeedback treatment is experimental and has not been proven to improve patient’s quality of life or is cost effective has prevented broader usage of this therapy in clinical practice. In a recent randomized controlled trial, we reported that home biofeedback can be as effective as office biofeedback therapy in improving symptoms of chronic constipation, and in correcting dyssynergic defecation12. Approximately 70%, of patients receiving either treatment were considered responders12.
This prospective randomized comparisons of QOL domains and cost effectiveness were conducted alongside the RCT to rigorously examine if biofeedback therapy influences the QOL in patients with dyssynergic defecation, what are the costs associated with biofeedback treatment, and if there are any differences in the QOL domains or costs if the treatment was administered in a home setting versus an office setting. Here, we first of all confirmed previous findings that patients with dyssynergic defecation have significantly impaired QOL8 and that several domains are affected. Furthermore, this study shows that biofeedback therapy has a significant impact in improving several of the QOL domains. Also, our study reveals that the new home biofeedback program has equivalent gains in QOL and was non-inferior to the standard office biofeedback treatment. Significantly, we found that the following domains, role emotional, role physical, vitality and bodily pain domains significantly improved in patients receiving both the office and home biofeedback therapy. Additionally we found that the mental health and social functioning domains significantly improved in the office biofeedback group. Although there were trends towards improvement in each one of the remaining QOL parameters, the ITT analysis showed no significant difference.
Our next objective was to examine the costs associated with each treatment modality. Using standard metrics of cost-assessment from a societal perspective and using conservative cost estimates based on centers for medical services rate in 2009 when the studies were completed, we showed that the average cost for 6 sessions of office biofeedback therapy was $1942.50. Comparatively, the cost for home biofeedback therapy including a loaner cost for equipment and disposable probe was $1112.39, i.e a savings of $830.11. for home biofeedback therapy. Furthermore, office and home biofeedback cost/QALY values fell within the accepted parameters of less than $100,000/QALY, suggesting that these 2 treatment modalities were independently cost-effective. Next, we calculated the incremental cost effectiveness ratio (ICER) to better understand and determine the cost savings if any. We found that the home biofeedback treatment showed a strong dominance as a more effective and cost-saving treatment modality for dyssynergic defecation with an ICER of $21,525 in favor of this treatment. These findings indicate that the overall biofeedback therapy is inexpensive whether administered at home or in an office setting but home biofeedback is a more cost-effective method of delivering this treatment.
Home biofeedback also offers the advantage of treating more patients with dyssynergic defecation, since this can be done in the community, outside of hospitals and offices. The disadvantage is that at present there is no commercially available device for home biofeedback training for constipation, although several devices are available for fecal incontinence (In Tone MV®, Milwaukee, WI). A recent comparative study showed that a commercially available home trainer for fecal incontinence was as effective as office biofeedback20. We are working with potential vendors to further refine our prototype device that has been patented21 and used in this clinical research study for commercial use.
A potential limitation of the home biofeedback system could be that it may require more visits, and more time each visit, especially in community practice, offsetting its cost benefits. However, with advances in tele-monitoring and bluetooth technology and voice activated systems, we anticipate that the costs for home biofeedback may be actually lower, as these patients can be monitored from home and adjustments to treatment plan and device can be performed remotely. Another limitation of our study was that most subjects enrolled were women. However, based on our clinical experience we believe that our results are equally applicable to men, but this aspect needs further validation.
In conclusion, our study shows that constipation with dyssynergic defecation is associated with profound negative effects on QOL, and that biofeedback therapy significantly improves these QOL domains restoring the patient’s health. These improvements occurred irrespective of whether the patients received biofeedback treatment in a home or office setting, and home biofeedback was non-inferior to office biofeedback treatment. From a cost perspective, home biofeedback is significantly more cost-effective and should be the preferred approach for managing these patients. Such an approach could broaden the availability of this treatment modality to the millions in the community. Because, we found that home biofeedback is non-inferior to office biofeedback but less costly, it seems reasonable to consider a tiered approach where home biofeedback is offered first and if patients have refractory symptoms theycould be given the option of office-based biofeedback therapy.
Study Highlights:
- What is current knowledge:
- Dyssynergic defecation affects 1/3rd of patients with chronic constipation and significantly affects quality of life. Biofeedback therapy is effective in improving bowel symptoms and correcting dyssynergia.
- Whether biofeedback therapy improves quality of life in patients with dyssynergic defecation is not known. Also whether home biofeedback therapy is cost-effective when compared to office biofeedback therapy is unclear.
- What is New Here:
- Biofeedback therapy significantly improves quality of life in patients with dyssynergic defecation irrespective of whether the treatment is administered at home or in an office setting.
- Home biofeedback therapy is more cost-effective than office-based biofeedback therapy for patients with dyssynergic defecation.
Acknowledgement:
This work was supported by NIH grant RO1 DK 57100–05 and grant RR00059 from the General Clinical Research Centers program, National Center for Research Resources. The study was conducted at the University of Iowa and data analysis and manuscript writing was completed at Augusta University and University of Iowa. Grant Support: Dr. Satish Rao is supported by NIH grant R01 DK 57100–05. Portions of this work was presented at the American College of Gastroenterology Meeting in San Diego, California on October 2009, Am J Gastroenterol 2009; 1308:5488 and at the Digestive Disease Week Meeting Chicago, Illinois on May 2011, Gastroenterology 2011;224:552.. We thank Mr. Kice Brown and Dr. B. Zimmerman for support with statistical analysis and QALY measures.
Footnotes
Conflicts of Interest: All authors declare no conflicts of interests with this study. Dr. Rao holds a patent No US8758387B2 for the anatoner system that includes the home biofeedback device probe and software used for this study.
ClinicalTrials.gov: Registered at Clinical trials.gov no NCT03202771.
REFERENCES
- 1.Higgins PD, Johanson JF. Epidemiology of constipation in North America: a systematic review. Am J Gastroenterol 2004;99:750–9. [DOI] [PubMed] [Google Scholar]
- 2.Rao SSC, Camilleri M. Clinical approach to constipation In Yamada’s Text Book of Gastroenterology, 6th Edition, Edited by Podolsky D et al. , Chapter 42, John Wiley & Sons, Ltd. 2016. Pp 757–780. [Google Scholar]
- 3.Rao SSC, Rattanakovit K, Patcharatrakul T. Diagnosis and Management of Chronic Constipation in Adults. Nature Review, Gastroenterology & Hepatology 2016;13:295–305. [DOI] [PubMed] [Google Scholar]
- 4.Mertz H, Naliboff B, Mayer E. Physiology of refractory chronic constipation. Am J Gastroenterol 1999;94:609–15. [DOI] [PubMed] [Google Scholar]
- 5.Bharucha AE, Dorn SD, Lembo A, Pressman A. American Gastroenterological Association medical position statement on constipation. Gastroenterology 2013;144:211–17. [DOI] [PubMed] [Google Scholar]
- 6.Surrenti E, Rath DM, Pemberton JH, Camilleri M. Audit of Constipation in a Tertiary Referral Gastroenterology Practice. Am J Gastroenterol 1995;90:1471–5. [PubMed] [Google Scholar]
- 7.Rao SSC, Welcher KD, Leistikow JS. Obstructive defecation: A failure of rectoanal coordination. Am J Gastroenterol 1998;93:1042–50. [DOI] [PubMed] [Google Scholar]
- 8.Rao SS, Seaton K, Miller MJ, Schulze K, Brown CK, Paulson J, Zimmerman B. Psychological profiles and quality of life differ between patients with dyssynergia and those with slow transit constipation. J Psychosom Res, 2007. October:63(4):441–9. Epub 2007 Aug 1. [DOI] [PubMed] [Google Scholar]
- 9.Rao SS, Seaton K, Miller M, et al. Randomized controlled trial of biofeedback, sham feedback, and standard therapy for dyssynergic defecation. Clin Gastroenterol Hepatol 2007;5:331–8. [DOI] [PubMed] [Google Scholar]
- 10.Chiarioni G, Whitehead WE, Pezza V, Morelli A, Bassotti G. Biofeedback is superior to laxatives for normal transit constipation due to pelvic floor dyssynergia. Gastroenterology 2006;130:657–64. [DOI] [PubMed] [Google Scholar]
- 11.Rao SS, Benninga MA, Bharucha AE, Chiarioni G, Di Lorenzo C, Whitehead WE. ANMS-ESNM position paper and consensus guidelines on biofeedback therapy for anorectal disorders. Neurogastroenterol Motil 2015;27:594–609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rao SSC, Valestin JA, Xiang X, Hamdy S, Bradley CS, Zimmerman BM. Home-based versus office-based biofeedback therapy for constipation with dyssynergic defecation: A randomized controlled trial. Lancet Gastroenterol Hepatol 2018. Published On-line September 17, 2018. S2468–1253:30266–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brazier JE, Harper R, Jones NM, O’Cathain A, Thomas KJ, Usherwood T, Westlake L. Validating the SF-36 health survey questionnaire: new outcome measure for primary care. BMJ 1992. July 18;305:160–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Drummond M, McGuire A. Economic evaluation in health care: merging theory with practice. Oxford University Press, New York, 2001. [Google Scholar]
- 15.Luce BR, Manning WG, Siegel JE, Pipscomb J. Estimating costs in cost-effectiveness analysis gold In: Cost-effectiveness in health and medicine. Russell JE, Siegel E, Weinstein MC (Eds). Oxford University Press, New York, 1996. [Google Scholar]
- 16.Haddix AC, Corso PA, Gorsky RD. Costs In: Prevention effectivess: A guide to decision analysis and economic evaluation. (Eds) Haddix S Teutsch SM and PA Corso. Oxford and New York, Oxford University Press, 2003. pp. 264, ISBN: 0-19-514897-5. [Google Scholar]
- 17.Sloan FA. Valuing health care: Costs, benefits, effectivess of harmaceuticals and other medical technologies. New York: Cambridge University Press, 1995, c1996. 273 p. [Google Scholar]
- 18.Brazier JE, et al. Measuring and valuing health for economic evaluation. 2007. Oxford: Oxford University Press. [Google Scholar]
- 19.Wald A, Bharucha AE, Cosman BC, Whitehead, WE. ACG Clinical Guide: Management of benign anorectal disorders. Am J Gastroenterol 2014;109:1141–1157. [DOI] [PubMed] [Google Scholar]
- 20.Sharma A, Xiang X, Yan Y, et al. Home Biofeedback Therapy Improves Fecal Incontinence Severity and Quality of Life in a Non-Inferiority Randomized Controlled Study. Am J Gastroenterol 2018;113:5246. [Google Scholar]
- 21.Rao SSC, Kumar MNS. Biofeedback training of anal and rectal muscles. Patent No. US 8758387 B2 and US 20130018308; June 24, 2014. [Google Scholar]