Abstract
This research presents an analysis of spatial access to both opioid use disorder treatment facilities and emergency medical services in New Hampshire during 2015–2016, a period during which there was a steep increase in unintentional overdoses involving fentanyl. For this research, spatial access was computed using the enhanced two-step floating catchment area model combined with the Huff model to assess access across New Hampshire and give attention to supply-side parameters that can impact spatial access. The model is designed to measure access to healthcare services for opioid use disorder patients offered at treatment centers or from buprenorphine treatment practitioners, as well as from emergency medical services across New Hampshire. A composite index of accessibility is proposed to represent overall access to these different treatment services for opioid use disorder patients. Geospatial determinants of spatial access included street network distances, driving times and distance decay relationships, while other key factors were services availability and population demand. Among the towns with the highest composite access scores, approximately 40% were metropolitan locations while 16% were rural towns. The insights from this research showed that for this period, while the opioid crisis was impacting many towns in New Hampshire, high levels of access to treatment services were not uniform across the state. When comparing the access results with data on the towns of residence for individuals who died from unintentional overdoses involving fentanyl during 2015 and 2016, estimates found that approximately 40% of the towns were not estimated to be in the highest class of access to treatment services at the time. This research provides information for local public health officials to support planning strategies to address opioid use disorder treatment access in high-risk regions.
Keywords: spatial accessibility, opioid use disorder treatment services, emergency medical services, substance use disorder, floating catchment area
1. Introduction
There has been a steep rise in opioid-related deaths in the US since 2010, with numbers of opioid overdose deaths reaching over 47,000 in 20171. The spatial pattern of these overdose deaths shifted from the US west coast in the early 2000s to New England, Appalachia, and the Ohio Valley by 2016 (Jalal et al., 2018; Rossen, Khan, & Warner, 2014; Ruhm, 2017; Stewart, Cao, Hsu, Artigiani, & Wish, 2017). In New England, specifically in Connecticut, Massachusetts and New Hampshire, opioid-related overdoses tripled between 2011 and 2016 (Rudd, Seth, David, & Scholl, 2016), and in New Hampshire, opioid-related emergency department visits increased by 70% between 2011 and 2015 (Daly et al., 2017). Since 2013, the number of overdoses and deaths involving fentanyl have increased significantly to the point where fentanyl is now a major threat to public health, impacting states such as Ohio, West Virginia, New Hampshire, and Rhode Island among others (Ciccarone, 2010; Gladden, Martinez, & Seth, 2016; Marshall et al., 2017; Peterson et al., 2016). Overdoses involving fentanyl have become much more widespread due to the fact that fentanyl contains more powerful chemical analogues than heroin and is cheaper, easier to manufacture, and is difficult to distinguish from other illicit substances (Baldwin et al., 2018; Ciccarone, Ondocsin, & Mars, 2017; Green & Gilbert, 2016; Somerville et al., 2017).
In 2015, increases in fentanyl-related overdose deaths were occurring at a very high rate in New Hampshire, and this spurred a National Drug Early Warning System (NDEWS) HotSpot study in 2016 on unintentional overdoses involving fentanyl. The mission of NIDA-supported NDEWS is to monitor indicators of emerging drugs in the United States. To achieve this mission, NDEWS staff monitor available opioid use indicators and sponsor HotSpot studies to investigate local drug outbreaks. According to NDEWS, while the number of New Hampshire deaths caused by fentanyl was less than 20 per year up to 2013, the number had increased to over 280 in 2015 (Sorg, Wren, Stewart, & Cao, 2017). The New Hampshire study assessed among other factors, the geospatial relationships between the location of drug use, place of residence, and place of death for decedents from drug overdoses in New Hampshire between 01/2015 and 09/2016. The analysis demonstrated that most of the fatal drug overdoses occurred in metropolitan areas (NDEWS, 2017; Sorg et al., 2017).
The rise of use disorders and mortality from opioids including fentanyl, has raised attention on whether these patients are receiving adequate treatment services. The 2016 National Survey on Drug Use and Health (NSDUH) administered by the Substance Abuse and Mental Health Services Administration (SAMHSA) reported that although approximately 21 million people aged 12 or older needed treatment for substance use in 2016, almost 90% of these patients reported that they did not receive professional treatment in the previous 12 months (Substance Abuse and Mental Health Services Administration, 2017). Previous research investigated the risks associated with not receiving timely treatments (e.g., buprenorphine-naloxone, access to methadone clinics and emergency medical services) among individuals with opioid use disorders both in the US and globally (Dodson, Enki Yoo, Martin-Gill, & Roth, 2018; Dunlop et al., 2017; Lo et al., 2018; Yarborough et al., 2016). For example, in the U.S., a study based on outpatient treatment centers in Baltimore found patients traveling more than 4 miles were significantly associated with a shorter length of stay for treatment completion (Beardsley, Wish, Fitzelle, O’Grady, & Arria, 2003). In New York City, a one-mile travel distance was utilized as threshold for analyzing spatial access to syringe exchange programs among drug injectors and a median of 10% of district surface area were within this distance in 2005 (Cooper et al., 2011). A study in Houston, TX found that heroin injectors tended to live closer to treatment facilities, in order to get assistance and reduce injecting (Kao, Torres, Guerrero, Mauldin, & Bordnick, 2014). Other factors that influence behaviors among opioid users include lower socioeconomic levels (and higher crime rates) for neighborhoods (Kwan et al., 2018) and that impede access to opioid treatment programs and impact treatment continuity among drug users (Mennis et al., 2012).
In New Hampshire, there has been a significant increase in treatment demand for patients with opioid use disorders. The number of opioid-related emergency department visits in July 2016 were double the number from February 2016, and treatment admissions associated with heroin and fentanyl significantly exceeded that for prescription opioids (NDEWS Coordinating Center, 2016). In addition to the services from opioid use disorder treatment facilities, receiving treatment from emergency medical service (EMS) providers, especially naloxone administration at the scene is also critically important when an opioid drug overdose occurs (Faul et al., 2015, 2017). In New Hampshire, a low likelihood of receiving interventions from EMS was found in rural locations (Sorg et al., 2017). Enhancing access to both treatment facilities and EMS services including administering naloxone is important for state and local health planning officials and related stakeholders in reducing the impacts associated with opioid use disorder, especially in a state where a significantly high number of deaths from fentanyl poisoning have been identified. However, very few studies have investigated spatial access to more than one type of resource, e.g., treatment facilities and EMS.
Spatial access refers to the geographic barriers that might exist between service suppliers and population demand (Joseph & Phillips, 1984). A standard approach to measure spatial access uses a gravity-based model that considers the spatial interactions between population locations and service locations based on how far patients are willing to travel (Guagliardo, 2004; Kim & Kwan, 2003; Kwan & Hong, 1998). This framework has been widely used in health care studies and is often used to explain impedances in patients’ travel to health care services given the availability of facilities (Cao, Stewart, & Kalil, 2016; Gharani, Stewart, & Ryan, 2015; Ye & Kim, 2014). In this research, we investigate the key factors or determinants of accessibility that include street network distance, driving time, and distance decay, as well as services availability and population demand to provide a measure of access to key treatment resources for New Hampshire. This work involves an analysis of spatial access to opioid use disorder treatment centers and programs, locations of buprenorphine treatment practitioners, and EMS services by town for 2015 – 2016, a key period during the opioid crisis in New Hampshire. We combine accessibility indices to produce a composite index of spatial access that provides an overall pattern of accessibility to key treatments including emergency response services across the state, and compare this result with known locations (towns) of fatal overdoses that involved fentanyl during this period. The findings provide support for local state stakeholders for allocating scarce treatment resources during the national opioid epidemic.
2. Methods
2.1. Data
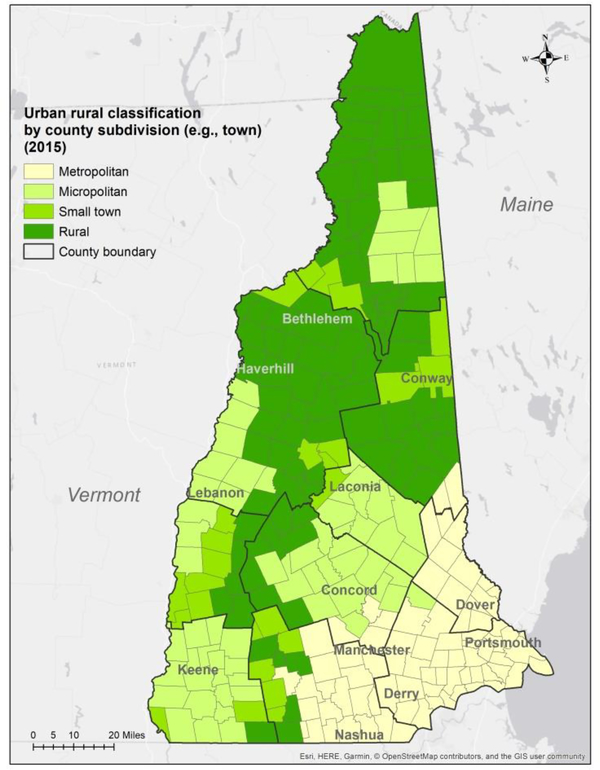
New Hampshire has 10 counties and 259 county subdivisions, including 222 towns, 13 incorporated places, and 24 other spatial entities (including grants, locations, purchases and townships). This state is composed of 120 rural and small towns (population < 10,000), with an overall population in 2015 of 1.3 million (Figure 1). For this research, spatial analyses were undertaken at the granularity of county subdivision (town level), to be consistent with the NDEWS HotSpot study, where the number of overdoses involving fentanyl and possibly other drugs was reported at the same spatial granularity. Details of towns and corresponding demographic data for 2015 obtained from the American Community Survey are listed in Appendix A. The analysis also uses the number of heroin and prescription opioid treatment admissions for New Hampshire during 2015–2016 as reported by the New Hampshire Department of Health and Human Services2. The number of treatment admissions for each town were estimated based on the proportion of town population in each county. In order to investigate spatial access from towns to opioid use disorder treatment centers, this research analyzed locations of 49 treatment centers in the state of New Hampshire from SAMHSA3, released in February 2017. The full list of service settings and treatment types for the centers are listed in Appendix B. In addition, the locations of 125 buprenorphine treatment practitioners were also collected from SAMHSA. In New Hampshire, the cities of Manchester and Nashua designated 16 fire stations as Safe Stations to help fast track patients seeking treatment for opioid use disorders4. The analysis of spatial access to emergency medical services (EMS) was based on data for 172 EMS stations, collected from the State Department of Safety, Division of Fire Standards & Training & Emergency Medical Services5 for fire stations with transport licenses and Yellow pages6 for private EMS services (e.g., American Medical Response in Manchester). These data were accessed in 2017.
Figure 1.
Urban-rural classification for New Hampshire by county subdivision (towns) (n = 259) for 2015.
Another dataset in this research included data on 492 decedents in New Hampshire whose deaths occurred between 01/2015 and 09/2016, and were reported to be from drug poisoning due to fentanyl alone or in combination with other drugs and/or alcohol. Most victims were white, male, and between 20–39 years old (Sorg et al., 2017). Data about these deaths were collected as part of the collaboration between NDEWS New Hampshire HotSpot study researchers and the Office of the Chief Medical Examiner in New Hampshire.
The spatial data for this research included boundaries for 259 county subdivisions (e.g., towns) from TIGER/Line Shapefiles, street network data from OpenStreetMap, population totals for each town, as well as socioeconomic variables from the US Census Bureau’s American Community Survey (ACS)7 for 2015. The urban-rural classification is from USDA’s Rural-Urban Commuting Area (RUCA) Codes8, and were aggregated into 4 categories: metropolitan (urbanized areas of 50,000 and more population), micropolitan (large urban clusters of 10,000 to 49,999 population), small town (small urban clusters of 2,500 to 9,999 population), and rural areas (outside urban areas or urban clusters) (Figure 1).
2.2. Determinants for calculating access to opioid use disorder treatment facilities
For this study, the analysis of spatial access to opioid use disorder treatment facilities includes access to treatment centers, buprenorphine treatment practitioners, and Safe Stations. To calculate spatial access from town centroids to these locations, the enhanced two-step floating catchment area (E2SFCA) model (W. Luo & Qi, 2009) and the Huff model (Huff, 1963) were used together. These models are described in Appendix C. E2SFCA is based on the original two-step floating catchment area (2SFCA) model developed by Luo and Wang (2003) to overcome a limitation in the original 2SFCA model where driving time from an origin to any destination falling into a catchment area is the same regardless of actual distance (i.e., the same driving time threshold is used throughout a catchment). The E2SFCA model captures variable catchment sizes (i.e., variable driving times) using an impedance function between each origin (e.g., centroid of town) and destination (treatment service location) pair based on three key geospatial parameters, including street network distance, driving time and distance decay, for local populations with respect to receiving health care (W. Luo & Whippo, 2012; McGrail, 2012; Schuurman, Bérubé, & Crooks, 2010).
The Huff model (Huff, 1963) has also been applied in human mobility research to investigate place-based accessibility espcially in the context of urban services (Chen et al., 2017; Lu, Shaw, Fang, Zhang, & Yin, 2017). The use of the Huff model with E2SFCA was reported by Luo (2014), where the Huff model was applied to quantify the probability of selecting a health care service site among available services sites, based on the capacity or suitability of each facility. In this study, we used the total number of treatment types reported for each center and practitioner. The benefit of using both models together is that supply side properties are represented based on the different service settings and treatment services available at the treatment centers or practitioner locations.
To compute spatial access from town centroids to EMS service locations, some modifications were made to the E2SFCA. According to a national study on EMS administration of naloxone, the proportion of 911 calls associated with drug overdoses is less than that for other incidents (e.g., stroke and heart attack) (Faul et al., 2015, 2017). For EMS services, there may also be differences in activation times (the time between receiving a 911 call and ambulance dispatch) between urban and rural locations, as well as between volunteer and non-volunteer fire stations, where volunteers may be paged to respond to an emergency and require additional minutes for travel (Carr, Branas, Metlay, Sullivan, & Camargo, 2009). Details of parameter adjustments are displayed in Table 1 in Appendix C.
In order to achieve a measure of spatial access that encompasses the different types of treatment services across the state of New Hampshire during this time period, we created a composite index that reflects all aspects of treatment–non-emergency and emergency–that opioid use disorder patients may require. Details of the computational approach and model modifications are described in Appendix C. All the analyses were implemented using R 3.2.5.
3. Results
3.1. How spatial access to key treatment services varies across New Hampshire
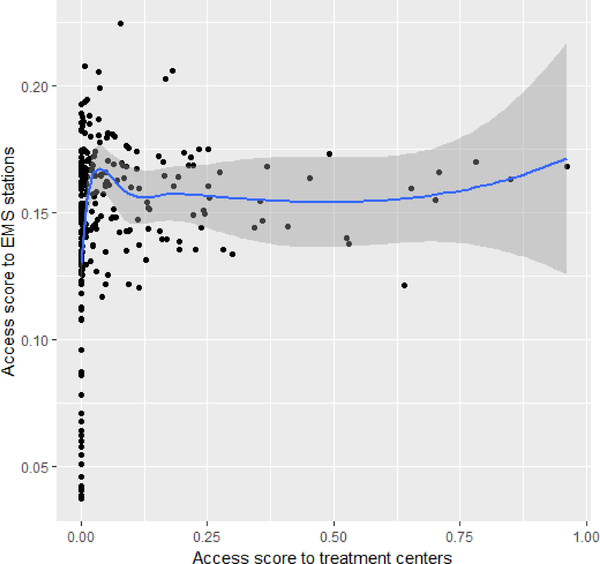
We conducted both separate and combined analyses of spatial accessibility investigating access to treatment centers, buprenorphine treatment practitioner locations, and EMS services in New Hampshire. While the spatial variations across the state meant that no strong relationship held everywhere, when the association between access to treatment centers and access to EMS services was examined using a Pearson’s correlation test, a slightly positive relationship was found with a coefficient of 0.147, p-value 0.017, and t-value 2.402 (CI 95%) (Figure 2). This suggests that in general, where access to treatment centers was higher, access to EMS services also tended to be higher.
Figure 2.
Association between access to opioid use disorder treatment centers and access to EMS services (New Hampshire, 2015 – 2016, n = 259 towns)
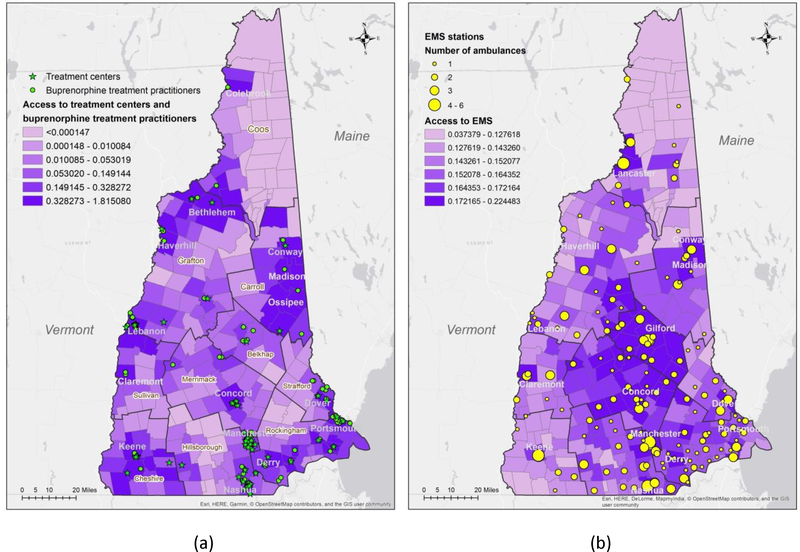
A combined analysis of spatial access to opioid use disorder treatment centers and buprenorphine treatment practitioner locations (referred together as treatment facilities) is shown in Figure 3a. For mapping, a quantile classification was used where each class contains approximately 15% of towns (approximately 45 towns). We found that for access to treatment facilities, towns along the borders of New Hampshire with Vermont, Massachusetts, and Maine including Conway, Portsmouth, Keene, Lebanon and Bethlehem were in the highest class of access scores. The cities of Manchester and Nashua fall into the second highest class of access. In the northern part of the state, certain towns, e.g., Colebrook and Ossipee were examples of rural towns that were also in the highest group of access to treatment facilities. With respect to EMS services, access was found to be high especially in mid-to-southern New Hampshire (e.g., Gilford, Concord, and Manchester) (Figure 3b). Lancaster in Coos County and Conway in Carroll County were other examples of towns that had the highest estimates of access to EMS services.
Figure 3.
Spatial access for New Hampshire, 2015–2016, n=259 towns for (a) treatment facilities (composite access index for treatment centers and buprenorphine treatment practitioners, E2SFCA and Huff model) and (b) EMS (modified E2SFCA model).
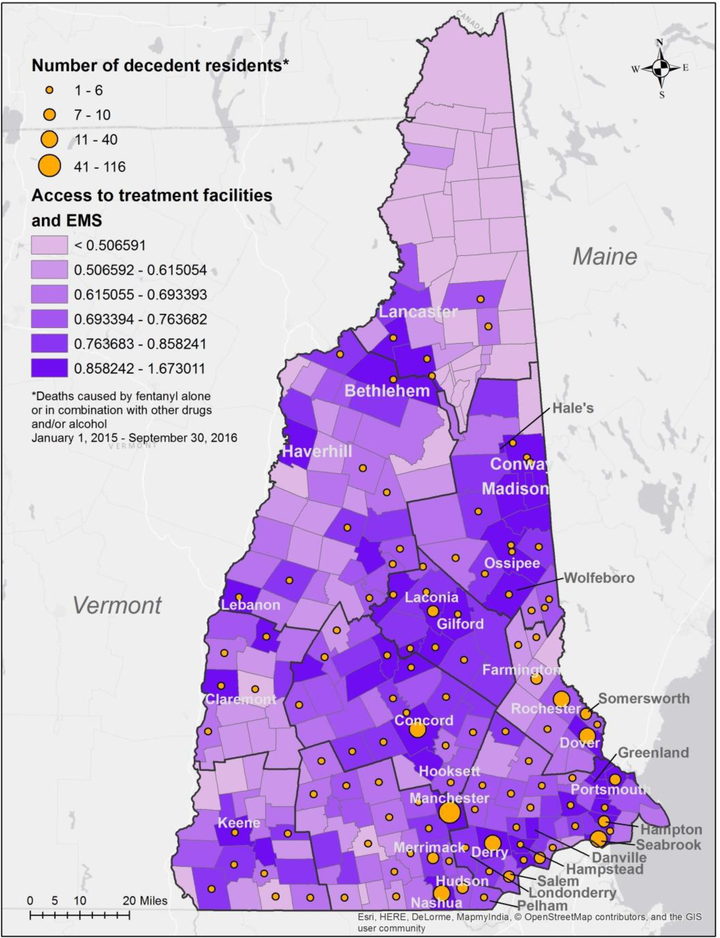
Our results found that access to both service types together (i.e., treatment facilities and EMS services) for this period was estimated to be higher in southern, more populous locations than in northern, remote and less populated areas of the state (Figure 4). The top 5 locations with the highest composite access scores were Hampstead, Keene, Conway, Portsmouth, and Lebanon. For northern rural locations Haverhill and Bethlehem in northern Grafton County, and Whitefield and Carroll in Coos County were found to be in the top class of composite access. Lower composite scores for spatial access during this period were returned for towns in northern Coos County, and towns in Sullivan and Grafton Counties in western New Hampshire, as well as towns in Hillsborough County.
Figure 4.
Composite index of spatial accessibility to treatment facilities and EMS, with towns of residence of decedents from fentanyl overdoses (New Hampshire, 2015–2016, n=259 towns)
3.2. Spatial accessibility and drug poisoning deaths caused by fentanyl or other drugs
The spatial pattern of individual drug poisoning deaths caused by fentanyl alone or in combination with other drugs and/or alcohol between 01/2015 and 09/2016 based on town of residence for 492 decedents (a total of 105 towns) was examined (Figure 4). Natural breaks was applied for categorizing the number of decedent residents in Figure 4. These individuals resided in 112 county subdivisions and villages, with 7 towns (Seabrook, Concord, Dover, Rochester, Derry, Nashua and Manchester) having more than 10 decedent residents each during the period of study. Analysis of the correlation between the estimated number of opioid treatment admissions by town and the number of decedent residents by town returned a strong positive correlation (coeff. 0.894, CI 99.9%).
Approximately 27% of the towns with decedent residents (29 out of 105 towns) were found to have composite index scores in the highest class (i.e., access to treatment facilities and EMS services) based on our model (Figure 4). These towns accounted for a total of 289 decedents (approximately 60% of the total). Among the 17 towns with highest estimates of opioid treatment admissions, Merrimack, Nashua, Seabrook, Dover, Derry, Laconia, Manchester, Hampton, Concord and Portsmouth had the highest composite access scores. However, seven towns that were associated with higher numbers of opioid treatment admissions (>5) for this period and also higher numbers of decedent residents (>7) had low composite access scores (lowest three classes). These towns include Farmington, Somersworth, Rochester, Salem, Pelham, Hudson, and Hooksett. Towns with fewer than 5 decedent residents (and towns with no decedent residents for this period) were likely to be associated with smaller populations in general. Among this group, while about 15% of these towns were estimated to have high access (e.g., Conway and Bethlehem), approximately 35% were in the lowest two classes of access to both types of treatment services. Towns with lower access were mostly northern and western rural towns.
3.3. Spatial accessibility and urbanization
We also investigated the association between spatial access and towns classified based on urbanization: metropolitan (29.2%), micropolitan (24.6%), small town (10.4%), and rural (35.8%) as per 2015. Among the towns in the highest class of access to treatment facilities, approximately 32.5% were rural towns (Table 1). These towns included Madison and Wolfeboro in Carroll County, and Bethlehem and Haverhill in Grafton County. Seven towns were classified as small towns including Conway and Hale’s (Figure 3a). Thirty-five percent of towns in the highest class of access to EMS were metropolitan while 14% were rural towns. Metropolitan and micropolitan locations represented approximately 70% of the towns with the highest composite index scores (Figure 4). Higher access indices are returned for Manchester, Nashua, Seabrook, and Greenland, as well as for some rural towns such as Haverhill and Bethlehem. This trend between access and urbanization was verified through a Chi-squared test with p<0.01.
Table 1.
Counts and percentage of NH towns estimated to be in the highest class of composite access (treatment facilities, EMS, and both services) by urbanization category
| Metropolitan | Micropolitan | Small town | Rural | |
|---|---|---|---|---|
| Access to treatment facilities | 13 (30.2%) | 9 (20.9%) | 7 (16.3%) | 14 (32.5%) |
| Access to EMS | 15 (34.9%) | 18 (41.9%) | 4 (9.1%) | 6 (13.6%) |
| Access to both services | 17 (39.5%) | 12 (27.9%) | 7 (16.3%) | 7 (16.3%) |
3.4. Spatial accessibility and socioeconomic factors
In addition to urbanization, we also investigated whether there were any associations between the spatial access results and certain socioeconomic variables including median household income, the percentage of residents with employment, and the percentage of residents with a bachelor’s or higher degree (Table 2). The results showed locations with larger populations that were full-time employed, higher median household income and college-educated, were found to have higher access to treatment. Education showed a stronger positive correlation with access to treatment facilities in locations including Portsmouth (close to the University of New Hampshire), Merrimack, Hampton and Lebanon (close to Dartmouth College). Employment was found to have a higher positive association with access to EMS, as well as with composite access scores. Locations with both high values of employment and median household income were mostly in Rockingham and Strafford Counties (including Portsmouth, Hampstead and Derry) and these locations also corresponded with high access to both types of treatment services.
Table 2.
Correlation coefficient between spatial accessibility and median household income (MHI), % of residents with employment (EMP), and % of residents with bachelor’s or higher degree (EDU),
| MHI (p-value) | EMP (p-value) | EDU (p-value) | |
|---|---|---|---|
| Access to treatment facilities | 0.109 (0.075) | 0.122 (0.047)* | 0.207 (0.001)* |
| Access to EMS | 0.570 (<0.001)* | 0.640 (<0.001)* | 0.436 (<0.001)* |
| Composite access | 0.461 (<0.001)* | 0.520 (<0.001)* | 0.430 (<0.001)* |
Statistically significant within 95%CI
4. Discussion
In this research, we investigated the characteristics of spatial access to opioid use disorder treatment services, to both treatment facilities (including buprenorphine treatment practitioner locations), and emergency medical services. We undertook a comprehensive analysis of spatial access using an integration of the E2SFCA model and Huff model for modeling access to treatment facilities, as well as a modified E2SFCA for modeling access to EMS services. The integration of the two models plus the adjustment to the E2SFCA model make this approach for determining spatial accessibility more realistic and provide a better fit for modeling access to opioid use disorder services. Instead of using simple buffer zones to analyze access to treatment services, our models reflect the different patterns of locations of different types of services as well as the role of several key determinants, including street network distance, driving time, distance decay, treatment services availability and population demand.
The results show a marked variation in access to opioid use disorder treatment services across the state with higher access mainly located in the southern part of the State following the trend of where the larger population centers exist. The patterns varied for the different treatment service types. For example, towns along the western border with Vermont and the eastern border with Maine had higher access to opioid use disorder treatment facilities, while central and southern towns had generally higher access to EMS. Certain rural towns, for example, at the border of Merrimack County and Grafton County, with higher access scores for EMS services, may benefit from EMS stations located in nearby larger centers. However, certain locations did not show high access to all treatment resources. For example, for locations with high estimates of opioid treatment admissions, even where the set of services including outpatient, residential, and inpatient services may be available, access may be insufficient.
In general, good spatial access to treatment centers, buprenorphine treatment practitioners, fire stations with Safe Station programs, and EMS stations with multiple service vehicles, plus an optimal road network were the characteristics of locations with high composite spatial access scores. These locations were also associated with higher socioeconomic status. This corresponds to relationships found in previous research by Stahler et al. (2016) and Stein et al. (2015) who both reported higher opioid use associated with groups with lower socioeconomic status. The analysis of urban-rural differences indicated that only approximately 33% of rural towns were in the highest category of access to treatment facilities. This percentage went down to 16% for the highest class of composite access (both treatment facilities and EMS together). For rural towns, there was an overall lower number of treatment centers and buprenorphine treatment practitioners, as well as EMS stations. This finding corresponds to previous research on rural patients and the degree to which they experience lower opportunities for receiving opioid use disorder treatment due to e.g., lack of physicians, current technology, and longer travel distances (Browne et al., 2016; Rosenblatt, Andrilla, Catlin, & Larson, 2015; Sigmon, 2015).
The analyses also showed that certain towns (e.g., Rochester) that were impacted by high numbers of fentanyl deaths between 01/2015 and 09/2016, did not necessarily have high access to all types of treatment services. We found that approximately 40% of decedent individuals during the study period resided in towns that were not estimated to have the highest composite access. This suggests a possible gap in the location of treatment services for patient populations in certain towns during this time. While in some locations (e.g., Manchester), there was estimated to be good access to treatment services, the numbers of treatment admissions and fentanyl deaths were still high. Further investigation is needed to get a clearer understanding of whether other factors may be contributing to impeding access for these individuals. The locations where higher numbers of fentanyl decedents resided, however, varied with respect to access to different treatment services. This indicates that while many of the towns with generally larger estimates of opioid treatment admissions and larger numbers of decedent residents scored high with respect to spatial in access for EMS, they did not also score highly for spatial access to treatment facilities (or vice versa), i.e., they did not have high access to both types of services. These low access zones highlight locations that could be looked at in more detail by local health officials to determine whether additional resources should be planned for these locations.
5. Limitations
Data limitations are often noted in health-related studies. In this research, data on the number of beds and physicians were unavailable. Psychosocial therapies and counseling services were not part of this analysis, and so are not included as service settings that represent the varying capacities of opioid use disorder treatment centers. This could result in underestimations relating to treatment centers and less variation among centers in general. Potential overestimation of access to buprenorphine treatment practitioners may exist due to over-counting of possibly waivered physicians from the SAMHSA dataset (Huhn & Dunn, 2017). When analyzing access to EMS, we retrieved the number of emergency transport vehicles based on publicly accessible data sources. However, the numbers were estimated for most private ambulance stations based on spot checking across the state and therefore could be underestimated. And while the spatial extent of this research is the state of New Hampshire, and the treatment centers, buprenorphine treatment physicians, and EMS stations are within the state boundary, there could be a potential underestimation of access for towns near the state’s boundary due to possible access for these residents receiving treatment outside the state.
The treatment admission data this research used were reported by county, and were estimated to town level based on the proportion of population in each town. There could be underestimation in low populated locations and overestimation in more highly populated places. The opioid treatment admissions data do not include Medicaid and private-insured individuals. These limitations could be possibly improved by further sensitivity analysis.
6. Conclusions
Enhancing access to treatment services is an important step for local public health officials as they work to reduce the risks and impacts from high numbers of individuals suffering with opioid use disorders. The contribution of this research is that we have designed an approach to measure spatial access to opioid use disorder treatment services in relation to both treatment facilities and emergency medical services in New Hampshire, a state hit particularly hard by the opioid crisis. This study provides a detailed investigation of the degree to which access to treatment for opioid use disorder patients varied across the state during 2015–2016. The results from this research identified locations where there is mismatch between access to treatment services and impacts from fentanyl overdoses.
The unique insights from investigating spatial access for both treatment facilities and EMS together provides information that local health stakeholders (e.g., opioid use disorder treatment service planners and healthcare professionals) can use for decision support and could provide further strategies to improve treatment access in at-risk regions, for example, for locating additional treatment services. This analysis could be beneficial to other states currently being impacted by the opioid crisis where geographical insights could identify gaps in services that may impact different population groups.
Future research could include extending the types of facilities to include for example, psychosocial and counseling facilities that could be used by patients. In addition, insurance providers and waiting time for patients to access treatment, as well as the locations of police stations that are reported to possibly serve as deterrents to treatment access are additional factors that could contribute to impeding access and could be future determinants in the model.
Acknowledgments
Research reported in this publication was supported by the National Institute on Drug Abuse of the National Institutes of Health under Award Number U01DA038360, awarded to the Center for Substance Abuse Research (CESAR) at the University of Maryland, College Park. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Appendix A9
| County (Population 2015) | Belknap (60,424) | Carroll (47,853) | Cheshire (77,342) | Coos (34,562) | Grafton (89,415) | Hillsborough (404,151) | Merrimack (448,153) | Strafford (125,396) | Sullivan (42,600) | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Towns | Alton | Albany | Alstead | Atkinson and | Jefferson | Alexandria | Landaff | Amherst | Allenstown | Hopkinton | Barrington | Acworth |
| Barnstead | Bartlett | Chesterfield | Gilmanton | Kilkenny | Ashland | Lebanon | Antrim | Andover | Kensington | Dover | Charlestown | |
| Belmont | Brookfield | Dublin | Academy | Lancaster | Bath | Lincoln | Bedford | Atkinson | Kingston | Durham | Claremont | |
| Center Harbor | Chatham | Fitzwilliam | Beans grant | Low and | Benton | Lisbon | Bennington | Auburn | Londonderry | Farmington | Cornish | |
| Gilford | Conway | Gilsum | Beans purchase | Burbanks | Bethlehem | Littleton | Brookline | Boscawen | Loudon | Lee | Croydon | |
| Gilmanton | Eaton | Harrisville | Berlin | Martins | Bridgewater | Livermore | Deering | Bow | New Castle | Madbury | Goshen | |
| Laconia | Effingham | Hinsdale | Cambridge | Milan | Bristol | Lyman | Francestown | Bradford | New London | Middleton | Grantham | |
| Meredith | Freedom | Jaffrey | Carroll | Mlllsfield | Campton | Lyme | Goffstown | Brentwood | Newbury | Milton | Langdon | |
| New Hampton | Hale's | Keene | Chandlers | Northumberland | Canaan | Monroe | Greenfield | Candia | Newfields | New Durham | Lempster | |
| Sanbornton | Hart's Location | Marlborough | Clarksville | Odell | Dorchester | Orange | Greenville | Canterbury | Newington | Rochester | Newport | |
| Tilton | Jackson | Marlow | Colebrook | Pinkhams | Easton | Orford | Hancock | Chester | Newmarket | Rollinsford | Plainfield | |
| Madison | Nelson | Columbia | Pittsburg | Ellsworth | Piermont | Hillsborough | Chichester | Newton | Somersworth | Springfield | ||
| Moultonborough | Richmond | Crawfords | Randolph | Enfield | Plymouth | Hollis | Concord | North Hampton | Strafford | Sunapee | ||
| Ossipee | Rlndge | Cutts | Sargents | Franconia | Rumney | Hudson | Danbury | Northfield | Unity | |||
| Sandwich | Roxbury | Dalton | Second College | Grafton | Sugar Hill | Litchfield | Danville | Northwood | Washington | |||
| Tamworth | Stoddard | Dlxs | Shelburne | Groton | Thornton | Lyndeborough | Deerfield | Nottingham | ||||
| Tuftonboro | Sullivan | Dixville | Stark | Hanover | Warren | Manchester | Derry | Pembroke | ||||
| Wakefield | Surry | Dummer | Stewartstown | Haverhill | Waterville | Mason | Dunbarton | Pittsfield | ||||
| Wolfeboro | Swanzey | Errol | Stratford | Hebron | Valley | Merrimack | East | Plaistow | ||||
| Troy | Ervings | Success | Holderness | Wentworth | Milford | Kingston | Portsmouth | |||||
| Walpole | Gorham | Thompson and | Woodstock | Mont Vernon | Epplng | Raymond | ||||||
| Westmoreland | Greens | Meserves | Nashua | Epsom | Rye | |||||||
| Winchester | Hadleys | Wentworth | New Boston | Exeter | Salem | |||||||
| Whitefield | New Ipswich | Franklin | Salisbury | |||||||||
| Pelham | Fremont | Sandown | ||||||||||
| Peterborough | Greenland | Seabrook | ||||||||||
| Sharon | Hampstead | South Hampton | ||||||||||
| Temple | Hampton | Stratham | ||||||||||
| Weare | Hampton | Sutton | ||||||||||
| Wilton | Falls | Warner | ||||||||||
| Windsor | Henniker | Webster | ||||||||||
| Hill | Wilmot | |||||||||||
| Hooksett | Windham | |||||||||||
Appendix B10
| List of service settings | List of service types |
|---|---|
| Hospital inpatient | substance abuse treatment |
| Residential | detoxification |
| Outpatient | methadone maintenance |
| Short-term residential | methadone maintenance for predetermined time |
| Long-term residential | methadone detoxification |
| Residential detoxification | buprenorphine maintenance |
| Outpatient detoxification | buprenorphine maintenance for predetermined time |
| Outpatient methadone/buprenorphine or naltrexone | buprenorphine detoxification |
| Outpatient day treatment or partial hospitalization | relapse prevention from naltrexone |
| Intensive outpatient treatment | buprenorphine used in treatment |
| Regularoutpatient treatment | naltrexone (oral) |
| Hospital inpatient detoxification | vivitrol (injectable naltrexone) |
| Hospital inpatient treatment | methadone |
| do not use medication for opioid addiction | |
| accepts clients on opioid medication | |
| prescribe/administer buprenorphine and/or naltrexone | |
| all clients in opioid treatment program | |
| SAMHSA-certified Opioid Treatment Program |
Appendix C
Access to treatment facilities
The approach for the E2SFCA is expressed as follows (Eqs C1 and C2) while the parameters for this study will be explained together with the integration of the Huff model for Eqs (C4) and (C5).
| (C1) |
| (C2) |
The Huff model (Huff, 1963) has also been applied in human mobility research to investigate place-based accessibility espcially in the context of urban services (Chen et al., 2017; Lu et al., 2017). The use of the Huff model with E2SFCA was reported by Luo (2014), where the Huff model was applied to quantify the probability of selecting a health care service site among available services sites, based on the capacity or suitability of each facility:
| (C3) |
The advantage of using both models together is that supply side properties are represented based on the different service settings and treatment services available at the treatment locations. In equation (C3), Cj or Cs denotes the total number of treatment types that each center, doctor’s office, or fire station (Safe Station) is able to provide. As a result, the model for computing spatial accessibility to opioid use disorder treatment services (ATi) is as follows:
| (C4) |
| (C5) |
where Sj refers to the number of service settings (e.g., inpatient treatment) in each opioid use disorder treatment center, Safe Station Program, or buprenorphine treatment practitioner locations. Pk denotes population of heroin and prescription opioid treatment admissions in each town that falls into the catchment area dr of each treatment center j. In this study, we consider this number as the population of opioid use disorder patients. The access score ATi of each town is computed based on the sum of treatment service-treatment admission ratio Rj of each service site that falls into the catchment area dr of each town centroid j. The catchment area dr is defined by an impedance function. A Gaussian function is used for the impedance function (t) capturing the smoothing that fits best with the distance decay effects assumed for this analysis. Gaussian weights are computed as:
| (C6) |
| (C7) |
For the Gaussian function, tij represents the travel time for driving between each town centroid i and opioid use disorder treatment center j. The travel times were calculated using an Origin-Destination matrix based on OpenStreetMap (Package osrm in R 3.2.5). m and n represent the indices of time adjustments and weights applied due to different travel scenarios. To consider the difference between actual and estimated driving times in different locations across the State, we undertook tests using Google Maps at different times of the day. Based on the fact that rural roads in New Hampshire have fewer vehicles and lower populations we multiplied 1.1, 1.3, 1.3, 1.4 to the estimated travel times to represent travel in rural, small town, micropolitan and metropolitan towns respectively (Carr et al., 2009). However, accounting for a longer travel time for patients residing in rural locations, we set different driving time thresholds (i.e., maximum driving time for patients) for rural, small town, micropolitan, and metropolitan. To identify the impedance coefficient for each urban-rural category, we tested actual driving times for these categories using Google maps. The values of β vary based on whether the catchment areas cover rural or urban towns. In this research, for travel to treatment locations, 45 min was set as an accessible driving time threshold for rural locations, 35 minutes for small town, 30 minutes for micropolitan, and 25 minutes for metropolitan towns (Table C1). The values of β are determined when Gaussian function f(tij) approaches 0 (e.g., 0.01 as threshold for this study) at 45, 35, 30 and 25 of each subzone (Cao, Stewart, & Kalil, 2016; Wan, Zhan, Zou, & Chow, 2012). This impedance function was applied in both the E2SFCA and Huff models in this analysis.
Spatial accessibility to buprenorphine treatment practitioners (ABi) was computed using E2SFCA (equation (C1) and (C2)) since these locations offered only a single type of service. In this analysis, all the service sites are weighted equally, with one physician at each location. The remaining computation follows the approach for computing spatial accessibility to treatment centers, adopting Gaussian weights for the impedance function and distinguishing rural, small town, micropolitan and metropolitan using 45 min, 35 min, 30 min and 25 minutes as driving time thresholds for each population center respectively.
Table C1.
Summary of distance decay function parameters and driving time adjustments (New Hampshire, 2015–2016, n = 259 towns)
| Driving time threshold for Gaussian function (min) | Impedance coefficient in Gaussian function | Driving time threshold for Inverse Power function (min) | Impedance coefficient in Inverse Power function | m (Eq.C7) for tij and tiu | n (Eq.C7) for tiu (min) | |
|---|---|---|---|---|---|---|
| Urban-rural classification | ||||||
| Rural | 45 | 440 | 20 | 1.54 | 1.1 | 3 |
| Small town | 35 | 270 | 18 | 1.6 | 1.3 | 2 |
| Micropolitan | 30 | 200 | 15 | 1.7 | 1.3 | 2 |
| Metropolitan | 25 | 135 | 13 | 1.8 | 1.4 | 1.5 |
| EMS station type | ||||||
| Volunteer | -- | -- | -- | -- | -- | 3 |
| Non-volunteer | -- | -- | -- | -- | -- | 0 |
Access to emergency medical services (EMS)
To estimate access to EMS specifically for opioid use disorder, we subtracted the demand ratio for nonopioid EMS sevices (e.g., cardiac or trauma services) from the demand ratio for opioid use-related EMS services for the first step of E2SFCA:
| (C8) |
| (C9) |
where Eu refers to the number of emergency transport vehicles (i.e., ambulances) for each EMS station u. Pk(non–opioid) denotes population that town total population subtracting heroin and prescription opioid treatment admissions in each town. This represents the population for other, non-opioid patients who utilized EMS services. In equation (C8), the original ratio possibly overestimates the number of opioid use disorder patients accessing EMS services and therefore, the current Ru represented an effective ratio of EMS-opioid use disorder patients. The final AEi measures spatial accessibility to EMS specifically for opioid use disorder patients. The impedance function (tiu) for this analysis applied an inverse power function tiu−α to represent the distance decay effects for emergency service scenarios.
Previous research has reported that the national average emergency response time in the U.S. is 15 min 19 sec11. In this analysis, 20 min was set as an access threshold for emergency transport vehicles’ driving time responding to rural calls, and this threshold is gradually reduced for small towns and micropolitan towns, and reduced further to 13 min for metropolitan towns (possibly conservative for some urban EMS response times that may in fact be much faster). The values of the impedance coefficient were determined when the inverse power function reaches 0.01 for each category.
Deriving a composite index for spatial accessibility
To create the composite index, the first step involved normalizing the two indices for treatment centers and buprenorphine treatment practitioners (ATi and ABi) to a range between 0 and 1, equation (C10) (Abuzied, Yuan, Ibrahim, Kaiser, & Saleem, 2016; Ye & Kim, 2014). The normalized indices ATi and ABi were summed to compute composite index ATBi Through normalization, the original distribution of access scores of each type of treatment can be maintained. For the second step, both ATBi and AEi were normalized to the range between 0 and 1 following equation (C10), and summed up to get an overall accessibility score (Eq. C11).
| (C10) |
| (C11) |
Determine composite spatial access to treatment and EMS services in New Hampshire Significant variation was found in composite access across New Hampshire for 2015–2016 Approximately 40% of towns with highest composite access are metropolitan locations Some locations with high access to treatment facilities do not score highly for access to EMS
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Abuzied S, Yuan M, Ibrahim S, Kaiser M, & Saleem T (2016). Geospatial risk assessment of flash floods in Nuweiba area, Egypt. Journal of Arid Environments, 133, 54–72. 10.1016/j.jaridenv.2016.06.004 [DOI] [Google Scholar]
- Baldwin N, Gray R, Goel A, Wood E, Buxton JA, & Rieb LM (2018). Fentanyl and heroin contained in seized illicit drugs and overdose-related deaths in British Columbia, Canada: An observational analysis. Drug and Alcohol Dependence, 185(December 2017), 322–327. 10.1016/j.drugalcdep.2017.12.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beardsley K, Wish ED, Fitzelle DB, O’Grady K, & Arria AM (2003). Distance traveled to outpatient drug treatment and client retention. Journal of Substance Abuse Treatment, 25(4), 279–285. 10.1016/S0740-5472(03)00188-0 [DOI] [PubMed] [Google Scholar]
- Browne T, Priester MA, Clone S, Iachini A, Dehart D, & Hock R (2016). Barriers and Facilitators to Substance Use Treatment in the Rural South : A Qualitative Study. Journal of Rural Health, 32, 92–101. 10.1111/jrh.12129 [DOI] [PubMed] [Google Scholar]
- Cao Y, Stewart K, & Kalil R (2016). Geographic patterns of end-stage renal disease and kidney transplants in the Midwestern United States. Applied Geography, 71, 133–143. 10.1016/j.apgeog.2016.05.001 [DOI] [Google Scholar]
- Carr BG, Branas CC, Metlay JP, Sullivan AF, & Camargo CA (2009). Access to Emergency Care in the United States. Annals of Emergency Medicine, 54(2), 261–269. 10.1016/j.annemergmed.2008.11.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen BY, Yuan H, Li Q, Wang D, Shaw S, Chen P, & Lam WHK (2017). Measuring place-based accessibility under travel time uncertainty. International Journal of Geographical Information Science, 31(4), 783–804. 10.1080/13658816.2016.1238919 [DOI] [Google Scholar]
- Ciccarone D (2010). Heroin in brown, black and white: structural factors and medical consequences in the US heroin market. International Journal of Digital Earth, 20(3), 277–282. 10.1016/j.drugpo.2008.08.003.Heroin [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ciccarone D, Ondocsin J, & Mars SG (2017). Heroin uncertainties: Exploring users’ perceptions of fentanyl-adulterated and -substituted ‘heroin.’ International Journal of Drug Policy, 46, 146–155. 10.1016/j.drugpo.2017.06.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper HLF, Des Jarlais DC, Ross Z, Tempalski B, Bossak B, & Friedman SR (2011). Spatial access to syringe exchange programs and pharmacies selling over-the-counter syringes as predictors of drug injectors’ use of sterile syringes. American Journal of Public Health, 101(6), 1118–1125. 10.2105/AJPH.2009.184580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daly ER, Dufault K, Swenson DJ, Lakevicius P, Metcalf E, & Chan BP (2017). Use of Emergency Department Data to Monitor and Respond to an Increase in Opioid Overdoses in New Hampshire, 2011–2015. Public Health Reports (Washington, D.C. : 1974), 132(1), 73S–79S. 10.1177/0033354917707934 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dodson ZM, Enki Yoo E-H, Martin-Gill C, & Roth R (2018). Spatial Methods to Enhance Public Health Surveillance and Resource Deployment in the Opioid Epidemic. American Journal of Public Health, e1–e6. 10.2105/AJPH.2018.304524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunlop AJ, Brown AL, Oldmeadow C, Harris A, Gill A, Sadler C, … Lintzeris N (2017). Effectiveness and cost-effectiveness of unsupervised buprenorphine-naloxone for the treatment of heroin dependence in a randomized waitlist controlled trial. Drug and Alcohol Dependence, 174, 181–191. 10.1016/j.drugalcdep.2017.01.016 [DOI] [PubMed] [Google Scholar]
- Faul M, Dailey MW, Sugerman DE, Sasser SM, Levy B, & Paulozzi LJ (2015). Disparity in naloxone administration by emergency medical service providers and the burden of drug overdose in US rural communities. American Journal of Public Health, 105, e26–e32. 10.2105/AJPH.2014.302520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faul M, Lurie P, Kinsman JM, Dailey MW, Crabaugh C, & Sasser SM (2017). Multiple Naloxone Administrations Among Emergency Medical Service Providers is Increasing. Prehospital Emergency Care, 21(4), 411–419. 10.1080/10903127.2017.1315203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gharani P, Stewart K, & Ryan GL (2015). An enhanced approach for modeling spatial accessibility for in vitro fertilization services in the rural Midwestern United States. Applied Geography, 64, 12–23. 10.1016/j.apgeog.2015.08.005 [DOI] [Google Scholar]
- Gladden RM, Martinez P, & Seth P (2016). Fentanyl Law Enforcement Submissions and Increases in Synthetic Opioid–Involved Overdose Deaths — 27 States, 2013–2014. MMWR. Morbidity and Mortality Weekly Report, 65(33), 837–843. 10.15585/mmwr.mm6533a2 [DOI] [PubMed] [Google Scholar]
- Green TC, & Gilbert M (2016). Counterfeit Medications and Fentanyl. JAMA Internal Medicine, 176(10), 1555–1557. 10.1001/jamainternmed.2016.4306 [DOI] [PubMed] [Google Scholar]
- Guagliardo MF (2004). Spatial accessibility of primary care: concepts, methods and challenges. International Journal of Health Geographics, 3, 3 10.1186/1476-072X-3-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huff DL (1963). A probabilistic analysis of shopping center trate areas. Land Economics, 39, 81–90. [Google Scholar]
- Huhn AS, & Dunn KE (2017). Why aren’t physicians prescribing more buprenorphine? Journal of Substance Abuse Treatment, 78, 1–7. 10.1016/j.jsat.2017.04.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jalal H, Balmert LC, Roberts MS, Buchanich JM, Zhang K, & Burke DS (2018). Changing dynamics of the drug overdose epidemic in the United States from 1979 through 2016. Science, 361(6408), eaau1184. 10.1126/science.aau1184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joseph AE, & Phillips DR (1984). Accessibility and utilization: geographical perspectives on health care delivery. Sage. [Google Scholar]
- Kao D, Torres LR, Guerrero EG, Mauldin RL, & Bordnick PS (2014). Spatial accessibility of drug treatment facilities and the effects on locus of control, drug use, and service use among heroin-injecting Mexican American men. International Journal of Drug Policy, 25(3), 598–607. 10.1016/j.drugpo.2013.12.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim H, & Kwan M (2003). Space-time accessibility measures : A geocomputational algorithm with a focus on the feasible opportunity set and possible activity duration, 71–91.
- Kwan M, & Hong X (1998). Network-based constraints-oriented choice set formation using GIS. Geographical Systems, 5, 139–162. [Google Scholar]
- Kwan M, Wang J, Tyburski M, Epstein DH, William J, Preston KL, … William J (2018). Uncertainties in the geographic context of health behaviors : a study of substance users ‘ exposure to psychosocial stress using GPS data. International Journal of Geographical Information Science, 00(00), 1–20. 10.1080/13658816.2018.1503276 [DOI] [Google Scholar]
- Lo A, Kerr T, Hayashi K, Milloy M, Nosova E, & Liu Y (2018). Factors associated with methadone maintenance therapy discontinuation among people who inject drugs. Journal of Substance Abuse Treatment, 94(August), 41–46. 10.1016/J.JSAT.2018.08.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu S, Shaw S, Fang Z, Zhang X, & Yin L (2017). Exploring the Effects of Sampling Locations for Calibrating the Huff Model Using Mobile Phone Location Data. Sustainability, 9(159). 10.3390/su9010159 [DOI] [Google Scholar]
- Luo J (2014). Integrating the Huff Model and Floating Catchment Area Methods to Analyze Spatial Access to Healthcare Services. Transactions in GIS, 18(3), 436–448. 10.1111/tgis.12096 [DOI] [Google Scholar]
- Luo W, & Qi Y (2009). An enhanced two-step floating catchment area (E2SFCA) method for measuring spatial accessibility to primary care physicians. Health and Place, 15(4), 1100–1107. 10.1016/j.healthplace.2009.06.002 [DOI] [PubMed] [Google Scholar]
- Luo W, & Wang F (2003). Spatial accessibility to primary care and physician shortage area designation: a case study in Illinois with GIS approaches. In Geographic Information Systems and Health Applications (pp. 260–278). [Google Scholar]
- Luo W, & Whippo T (2012). Variable catchment sizes for the two-step floating catchment area (2SFCA) method. Health and Place, 18(4), 789–795. 10.1016/j.healthplace.2012.04.002 [DOI] [PubMed] [Google Scholar]
- Marshall BDL, Krieger MS, Yedinak JL, Ogera P, Banerjee P, Alexander-Scott NE, … Green TC (2017). Epidemiology of fentanyl-involved drug overdose deaths: A geospatial retrospective study in Rhode Island, USA. International Journal of Drug Policy, 46, 130–135. 10.1016/j.drugpo.2017.05.029 [DOI] [PubMed] [Google Scholar]
- McGrail MR (2012). Spatial accessibility of primary health care utilising the two step floating catchment area method: an assessment of recent improvements. International Journal of Health Geographics, 11(1), 50 10.1186/1476-072X-11-50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mennis J, Stahler GJ, Baron DA, Mennis J, Stahler GJ, Geographic DAB, … Baron DA (2012). Geographic Barriers to Community-Based Psychiatric Treatment for Drug-Dependent Patients. Annals of the Association of American Geographers ISSN:, 12(5), 1093–1103. 10.1080/00045608.2012.657142 [DOI] [Google Scholar]
- NDEWS. (2017). Highlights from the NDEWS New Hampshire HotSpot Study. College Park, MD. [Google Scholar]
- NDEWS Coordinating Center. (2016). New Hampshire HotSpot Report - The Increase in Fentanyl Overdoses.
- Peterson AB, Gladden RM, Delcher C, Spies E, Garcia-Williams A, Wang Y, … Goldberger BA (2016). Increases in Fentanyl-Related Overdose Deaths — Florida and Ohio, 2013–2015. Morbidity and Mortality Weekly Report (MMWR), 65(33), 844–849. [DOI] [PubMed] [Google Scholar]
- Rosenblatt RA, Andrilla CHA, Catlin M, & Larson EH (2015). Geographic and Specialty Distribution of US Physicians Trained to Treat Opioid Use Disorder. Annals of Family Medicine, 13(1), 23–26. 10.1370/afm.1735.INTRODUCTION [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rossen LM, Khan D, & Warner M (2014). Hot spots in mortality from drug poisoning in the United States, 2007–2009. Health and Place, 26, 14–20. 10.1016/j.healthplace.2013.11.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rudd RA, Seth P, David F, & Scholl L (2016). Increases in Drug and Opioid-Involved Overdose Deaths - United States, 2010–2015. Morbidity and Mortality Weekly Report (MMWR), 65, 1445–1452. [DOI] [PubMed] [Google Scholar]
- Ruhm CJ (2017). Geographic Variation in Opioid and Heroin Involved Drug Poisoning Mortality Rates. American Journal of Preventive Medicine, 53(6), 745–753. 10.1016/j.amepre.2017.06.009 [DOI] [PubMed] [Google Scholar]
- Schuurman N, Bérubé M, & Crooks VA (2010). Measuring potential spatial access to primary health care physicians using a modified gravity model. Canadian Geographer / Le Géographe Canadien, 54(1), 29–45. 10.1111/j.1541-0064.2009.00301.x [DOI] [Google Scholar]
- Sigmon S (2015). Access to Treatment for Opioid Dependence in Rural America Challenges and Future Directions. JAMA Psychiatry, 71(4). 10.1001/jamapsychiatry.2013.4450 [DOI] [PubMed] [Google Scholar]
- Somerville NJ, O’Donnell J, Gladden RM, Zibbell JE, Green TC, Younkin M, … Walley AY (2017). Characteristics of Fentanyl Overdose — Massachusetts, 2014–2016. MMWR. Morbidity and Mortality Weekly Report, 66(14), 382–386. 10.15585/mmwr.mm6614a2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sorg MH, Wren JA, Stewart K, & Cao Y (2017). Unintentional Fentanyl Overdoses in New Hampshire: An NDEWS HotSpot Analysis. Retrieved from https://ndews.umd.edu/publications/unintentional-fentanyl-overdoses-new-hampshire-ndewshotspot-analysis%0A
- Stahler GJ, Mennis J, & Ducette JP (2016). Addictive Behaviors Residential and outpatient treatment completion for substance use disorders in the U. S.: Moderation analysis by demographics and drug of choice. Addictive Behaviors, 58, 129–135. 10.1016/j.addbeh.2016.02.030 [DOI] [PubMed] [Google Scholar]
- Stein MD, Anderson BJ, Thurmond P, & Bailey GL (2015). Comparing the life concerns of prescription opioid and heroin users. Journal of Substance Abuse Treatment, 48(1), 43–48. 10.1016/j.jsat.2014.07.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart K, Cao Y, Hsu MH, Artigiani E, & Wish E (2017). Geospatial Analysis of Drug Poisoning Deaths Involving Heroin in the USA, 2000–2014. Journal of Urban Health, 94(4), 572–586. 10.1007/s11524-017-0177-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. (2017). Key Substance Use and Mental Health Indicators in the United States: Results from the 2016 National Survey on Drug Use and Health. Rockville, MD. [Google Scholar]
- Wan N, Zhan FB, Zou B, & Chow E (2012). A relative spatial access assessment approach for analyzing potential spatial access to colorectal cancer services in Texas. Applied Geography, 32(2), 291–299. 10.1016/j.apgeog.2011.05.001 [DOI] [Google Scholar]
- Yarborough BJH, Stumbo SP, McCarty D, Mertens J, Weisner C, & Green CA (2016). Methadone, buprenorphine and preferences for opioid agonist treatment: A qualitative analysis. Drug and Alcohol Dependence, 160, 112–118. 10.1016/j.drugalcdep.2015.12.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ye H, & Kim H (2014). Measuring Spatial Health Disparity Using a Network-Based Accessibility Index Method in a GIS Environment : A Case Study of Hillsborough Measuring Spatial Health Disparity Using a Network-Based Accessibility. International Journal of Geospatial and Environmental Research, 1(1), Article 2. Retrieved from http://dc.uwm.edu/ijger/vol1/iss1/2 [Google Scholar]