Abstract
We report the case of a 43-year-old African American man with a history of hypertension and chronic kidney disease presenting with hypertensive emergency and bulbar paralysis in a descending fashion, which ultimately led to acute respiratory failure. He ingested pufferfish liver during the preceding 4 hours prior to presentation, as well as canned foods and cocaine over the prior 3 days. He had a complicated hospital course requiring intubation and mechanical ventilation, as well as the development of acute respiratory distress syndrome and acute renal failure requiring haemodialysis. This case exemplifies the classic manifestations of tetrodotoxin poisoning with some unique overlapping features, in the setting of an interesting social history.
Keywords: toxicology, drugs: respiratory system, mechanical ventilation, drugs: CNS (not psychiatric), neuromuscular disease
Background
Pufferfish, also known as ‘fugu’, is a delicacy in Japan, however, its consumption possesses life-threatening risks secondary to the effects of tetrodotoxin (TTX), which is primarily concentrated in the liver and ovaries.1 2 It must be meticulously prepared by specially-trained chefs in order to avoid its poisoning effects.2 Acute pufferfish poisoning presents with a descending paralysis that may ultimately lead to respiratory failure and death.2 3 There is no antidote for TTX, thus, treatment is purely symptomatic.2 4 Although pufferfish consumption is uncommon in South Florida, there are means of obtaining it, such as underground markets and fishing; thus, it is important to be aware of the clinical presentation after ingestion. Our particular case is exciting because in addition to consuming pufferfish, our patient also ingested canned food and cocaine, which made the differential diagnoses more broad and interesting.
Case presentation
A 43-year-old African American man with history of hypertension (HTN) and chronic kidney disease presented with vomiting, abdominal pain, bilateral leg numbness, difficulty speaking and weakness. He had associated chest pain, which was tearing in nature. Four hours prior to presentation, he ingested pufferfish liver. He reported ingesting canned food and cocaine 3 days prior. The patient’s grandmother, who consumed a smaller portion of the same pufferfish, also presented to our institution with dizziness and lower extremity weakness. His home medications were nifedipine and hydralazine. Social history was notable for occasional cocaine ingestion, however, he denied alcohol or tobacco use. Family history was unremarkable. Surgical history was negative. He had no known allergies. Vital signs were notable for an elevated blood pressure of 268/164 mm Hg, with no fever or tachycardia. Physical exam was pertinent for confusion and somnolence, as well as garbled speech, decreased muscle strength on all extremities and absent reflexes bilaterally.
Investigations
Labs were notable for potassium of 2.8 mmol/L and creatinine of 3.2 mg/dL. Urine toxicology was positive for cocaine. Admission chest radiograph, CT angiogram of the chest, abdomen and pelvis were negative for acute pathology. A CT of the brain and CT angiogram of the head and neck were also negative for acute intracranial findings. An MRI of the brain ruled out stroke and did not show evidence of hypertensive encephalopathy. Transthoracic echocardiogram revealed a preserved ejection fraction, no regional wall motion abnormalities and a thickened left ventricle wall. Neither nerve conduction study nor electromyography were performed.
Differential diagnosis
Acute cerebrovascular accident
Hypertensive encephalopathy
Acute aortic dissection
Cocaine intoxication
Food-borne botulism
Pufferfish poisoning
Guillain-Barré Syndrome
Treatment
The hypertensive emergency on presentation was initially treated with nicardipine and nitroglycerin drips. Soon after presentation, the patient acutely decompensated and was intubated for airway protection. The local poison control centre was contacted and activated charcoal was administered. Since food-borne botulism was considered in the differential diagnosis, botulinum antitoxin was given. A 5 mg dose of intravenous neostigmine was administered, as previous cases reports have documented successful outcomes of pufferfish poisoning with this practice.5 The patient was transferred to the Intensive Care Unit (ICU) for further management.
Outcome and follow-up
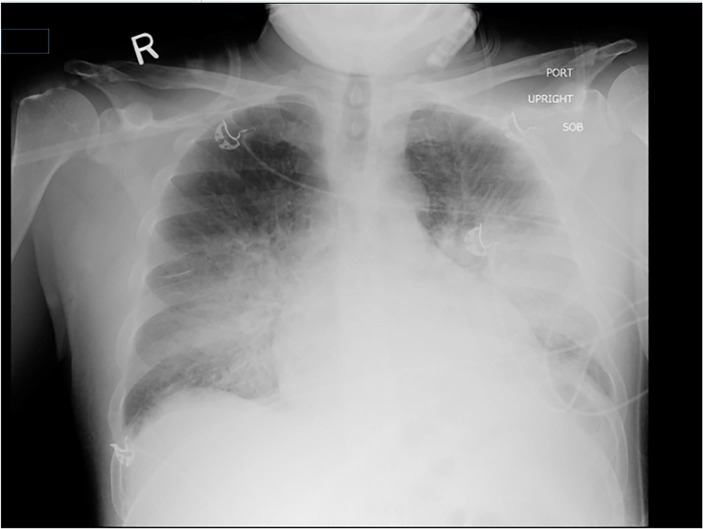
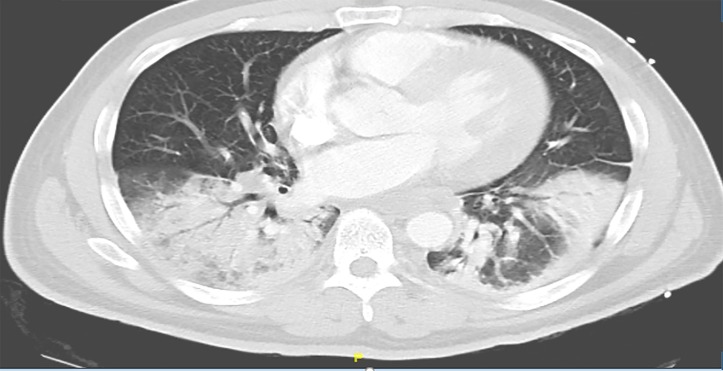
After approximately 24 hours, the patient regained muscle strength and was successfully extubated. However, over the proceeding 24 hours, the patient acutely decompensated and had to be re-intubated. Repeat chest radiograph revealed bilateral alveolar infiltrates (figure 1). Repeat CT chest was consistent with multi-lobar pneumonia and air bronchograms (figure 2). Hospital course was complicated by the development of acute respiratory distress syndrome, in the setting of a possible aspiration event during the episode of bulbar paralysis and subsequent intubation, resulting in the use of prolonged mechanical ventilation and paralytics. Sputum cultures obtained on admission were positive for pan-sensitive Streptococcus pneumoniae, for which intravenous ceftriaxone was initiated. Although the patient’s initial clinical picture was not consistent with community acquired pneumonia, and the isolation of S. pneumoniae in the sputum may have represented a coloniser, the patient was empirically treated, given his severity of illness. The patient’s kidney function continued to worsen and he eventually became anuric, necessitating the initiation of intermittent haemodialysis. Eventually, the patient’s respiratory failure resolved, however, renal function did not recover and the patient remains dialysis-dependent today. The patient’s grandmother endured a much more benign clinical course and did not require ICU management.
Figure 1.
Chest radiograph demonstrating bilateral alveolar infiltrates compatible with acute respiratory distress syndrome.
Figure 2.
CT angiography of the chest revealing multi-lobar pneumonia and air bronchograms.
Discussion
In Japan, where pufferfish or ‘fugu’ is a food delicacy, approximately 50 cases of pufferfish intoxication result in death each year.1 The lethality of pufferfish is attributed to TTX, which is primarily concentrated in the liver and gonads.2 TTX is 1200 times more toxic than cyanide, with the minimal lethal dose in humans being only 2–3 mg.2 3 TTX exerts its paralytic effects by inhibiting voltage-gated sodium channels.2 3 The onset of symptoms is typically 30 min to 6 hours after ingestion.2 4 The most common manifestations of intoxication are tingling sensation, perioral numbness, dizziness, limb weakness, nausea and vomiting, however, respiratory failure and death may occur.2–4 Naturally, aspiration of gastric contents due to compromised airway protection is a common complication, as was the likely case with our patient. The typical haemodynamic presentation is that of hypotension and bradycardia.2 4 Paradoxically, our patient presented with hypertensive emergency, which can be attributed to concomitant cocaine ingestion, in the setting of a history of underlying HTN.
TTX is dose-dependent, as was evident with our patient and his grandmother.2 4 The toxin is heat-stable and has no antidote, therefore, management of intoxication is symptomatic.2 4 Activated charcoal can be administered and gastric lavage may be performed, but these practices are only effective within 60 min of ingestion.4 6 Prior case studies have reported the use of neostigmine to reverse paralytic effects, which we administered to our patient; however, the current literature is insufficient to provide evidence for or against its use.5 7 If intoxication does not result in death, symptoms usually recover within 24 hours, as was the case with our patient.2
Previous outbreaks of pufferfish intoxication have been documented, primarily in countries where resources are scarce and the knowledge about pufferfish consumption is limited.
One of the most notable outbreaks occurred in Bangladesh in 2008, where 95 people in three different districts consumed pufferfish and 14 of them died.8 Although most reported cases of pufferfish poisoning have occurred in Asia, cases have been noted in other temperate areas of the world, as pufferfish thrive in warm waters. In 2013, in Reunion Island (surrounded by the Indian Ocean), a family of 12 was hospitalised after pufferfish intoxication.9 In 2014, two individuals in Minneapolis, Minnesota were hospitalised after ingesting dried pufferfish purchased from a street vendor.3
Pufferfish consumption is not commonly seen in the United States; however, both consumers and healthcare professionals should be aware of its particular life-threatening clinical manifestations, as well as differential diagnoses. Although TTX is extremely potent and poisonous, it has the potential to play a beneficial role in the non-edible form. The potent paralytic and analgesic effects of TTX pose promising treatment options in the pain relief and cosmetic industries.2 In China, it is currently used as an analgesic for terminally-ill patients; while in Japan, it has been applied for neuralgia and rheumatism.6 Much remains to be investigated regarding this powerful and paralysing toxin before it is commercially used. For now, we will forewarn the public to refrain from consuming the deadly delicacy known as ‘fugu’.
Learning points.
Pufferfish consumption is potentially lethal as a result of tetrodotoxin (TTX), which is mostly concentrated in the liver and gonads.
Pufferfish intoxication commonly presents as a descending paralysis with perioral tingling, nausea, vomiting, weakness and dizziness.
TTX causes paralysis by inhibiting voltage-gated sodium channels.
Symptoms typically present 30 min to 6 hours after consumption.
There is no antidote for tetrodotoxin, hence, management is supportive.
Footnotes
Contributors: PA is the main author of the manuscript. RD reviewed pertinent literature and helped with the draft of the original article. FH and GF helped revising the draft and produce the final manuscript submitted for publication.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Obtained.
References
- 1. Centers for Disease Control and Prevention (CDC. Tetrodotoxin poisoning associated with eating puffer fish transported from Japan--California, 1996. MMWR. Morbidity and mortality weekly report. 1996;45:389. [PubMed] [Google Scholar]
- 2. Lago J, Rodríguez LP, Blanco L, et al. Tetrodotoxin, an extremely potent marine neurotoxin: distribution, toxicity, origin and therapeutical uses. Mar Drugs 2015;13:6384–406. 10.3390/md13106384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Taken A. Tetrodotoxin poisoning outbreak from imported dried puffer fish. Minneapolis, Minnesota, 2014. [PubMed] [Google Scholar]
- 4. Bane V, Lehane M, Dikshit M, et al. Tetrodotoxin: chemistry, toxicity, source, distribution and detection. Toxins 2014;6:693–755. 10.3390/toxins6020693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Chowdhury FR, Nazmul Ahasan HA, Mamunur Rashid AK, et al. Tetrodotoxin poisoning: a clinical analysis, role of neostigmine and short-term outcome of 53 cases. Singapore Med J 2007;48:830–3. [PubMed] [Google Scholar]
- 6. Noguchi T, Arakawa O. Tetrodotoxin--distribution and accumulation in aquatic organisms, and cases of human intoxication. Mar Drugs 2008;6:220–42. 10.3390/md6020220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Liu SH, Tseng CY, Lin CC. Is neostigmine effective in severe pufferfish-associated tetrodotoxin poisoning? Clin Toxicol 2015;53:13–21. 10.3109/15563650.2014.980581 [DOI] [PubMed] [Google Scholar]
- 8. Homaira N, Rahman M, Luby SP, et al. Multiple outbreaks of puffer fish intoxication in Bangladesh, 2008. Am J Trop Med Hyg 2010;83:440–4. 10.4269/ajtmh.2010.10-0168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Puech B, Batsalle B, Roget P, et al. Family tetrodotoxin poisoning in Reunion Island (Southwest Indian Ocean) following the consumption of Lagocephalus sceleratus (Pufferfish). Bulletin de la Société de pathologie exotique 2014;107:79–84. 10.1007/s13149-014-0340-2 [DOI] [PubMed] [Google Scholar]