Abstract
Two dimensional, hierarchical classification models of personality pathology have emerged as alternatives to traditional categorical systems: multi-tiered models with increasing numbers of factors and models that distinguish between a general factor of severity and specific factors reflecting style. Using a large sample (N=840) with a range of psychopathology, we conducted exploratory factor analyses of individual personality disorder criteria to evaluate the validity of these conceptual structures. We estimated an oblique, “unfolding” hierarchy and a bifactor model, then examined correlations between these and multi-method functioning measures to enrich interpretation. Four-factor solutions for each model, reflecting rotations of each other, fit well and equivalently. The resulting structures are consistent with previous empirical work and provide support for each theoretical model.
Keywords: personality pathology, personality traits, hierarchical trait model, bifactor model
1. Introduction
Articulating the underlying structure of personality pathology is not only a theoretical endeavor but an empirical one, and quantitative modeling like factor analysis has advanced this effort (Wright, 2017; Wright & Zimmermann, 2015). These methods have resulted in dimensional models that mitigate shortcomings of categorical classification such as withindiagnosis heterogeneity, excessive overlap between diagnoses, and poor reliability (Trull & Durrett, 2005). Categories fail to reflect the natural structure of psychological phenomena, whereas dimensional models capture more accurately interrelationships between signs and symptoms (Hyman, 2010). From this nosological research, two alternative hierarchical dimensional approaches to conceptualizing personality pathology have emerged: multi-tiered models and those that separate a general factor of severity from specific factors reflecting style (e.g., Hopwood et al., 2011; Wright et al., 2012). Despite general agreement on the universe of content and a common goal to identify sources of shared variance across clinical manifestations, these approaches are distinguished by differences in structure.
1.1. Unfolding Hierarchical Models
In the first articulation, symptoms are hierarchically organized by shared phenotypes into nested domains of increasing specificity, from broad spectra to individual behaviors. Trait expressions within a domain are assumed to be continuously distributed throughout the population. This approach is exemplified by the Hierarchical Taxonomy of Psychopathology (HiTOP) which synthesizes findings across quantitative structural studies and asserts that most psychopathology can be organized hierarchically (Kotov et al., 2017). At the top of the hierarchy, pathology can be separated into broad internalizing and externalizing spectra. Within these two spectra are domains of psychopathology that correspond roughly to the five maladaptive personality traits consistently found in factor analytic studies (i.e., Detachment, Antagonism, Disinhibition, Psychoticism, and Negative Affectivity; Widiger & Simonsen, 2005) thus integrating personality pathology with other psychiatric conditions (Wright & Simms, 2015).
1.2. General and Specific Factor Models
In contrast to hierarchical models that fold degree of severity into the domains, another approach to conceptualizing and modeling personality pathology partitions severity and style (or content) separately, contending that each element provides unique diagnostic information (Tyrer, 2005). This approach, notably instantiated in one operationalization in the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5) Section III Alternative Model for Personality Disorders, emphasizes core deficits in self and interpersonal functioning underlying different clinical manifestations (Bender, Morey & Skodol, 2011; Hopwood et al., 2013; Kernberg, 1984). Several methodological techniques have been applied to test this structure by comparing outcomes predicted by general psychiatric functioning measures (e.g., severity) and trait-specific measures (e.g., style) (Berghuis et al., 2014; Few et al., 2013; Clark & Ro, 2014). Results from some of these studies suggest the presence of a latent continuum of impairment which accounts for prognostic variance across disorders (Hopwood et al, 2011; Livesley, 2006). However, meaningful interpretation of these results has been limited due to overlapping content between measures (e.g., Lack of Empathy, a core interpersonal impairment, and Callousness, a trait). Recently, factor analytic methods that partition general and specific variance as statistically independent dimensions (i.e., bifactor modeling) have been used to address this limitation (Sharp et al., 2015; Williams, Scalco & Simms, 2018; Wright et al., 2016). n studies of personality disorder criteria or diagnoses, the general factor has been interpreted as representing features of core personality functioning whereas the specific factors denote personality style.
1.3. Comparison of Model Approaches
Controversy about structure is fundamentally about how to best conceptualize personality pathology, which is a matter of construct validity. The importance of establishing a useful representation of psychopathology is evident in the literature comparing these dimensional models (e.g. Kim & Eaton, 2015; Brodbeck et al., 2011) and recent debates surrounding PD criteria in the DSM-5. Despite the significance for basic research and clinical assessment, no study to date has directly compared multi-tiered hierarchical and bifactor models of personality pathology using the same sample and same indicators. The nearest attempt was a comparison of non-nested factor models with a bifactor model of PD symptoms reported by Sharp et al. (2015), but these authors reported exclusively on statistical fit and did not include any external correlates, leaving issues of construct validity unaddressed.
1.4. Current Study
This study directly compared these two hierarchical, dimensional approaches to personality pathology classification in a single sample. Specifically, we conducted exploratory factor analyses (EFA) of individual DSM personality disorder criteria and compared solutions that used an oblique rotation to those that used a bifactor rotation. Oblique models were estimated with increasing numbers of factors to evaluate the “unfolding” of the personality pathology hierarchy. e then examined associations between factors that emerged from these models and an array of multi-method, external variables covering interpersonal and general functioning. By holding sample composition and variables constant, the resulting models differed only by the organization of the indicators in relation to one another. We expected both models to achieve adequate statistical fit but to be interpretively distinct. Our aim was to compare the construct validity of each model, but we had no hypotheses regarding the potential advantages of either model.
2. Method
Further information about sample characteristics, informant data, and reliability of measures can be found in supplementary files at: https://osf.io/ej93v/.
2.1. Participants
A total of 840 participants were drawn from five related subsamples corresponding to consecutive iterations of the same parent grant. The overall sample (63% female, 78% white, average age 36 years old) included outpatients with and without personality disorders (n=554) as well as community participants (n=286). Psychiatric patients were recruited from outpatient clinics at UPMC Western Psychiatric Hospital, and the community participants were recruited through advertising, telephone solicitation using random-digit dialing, and mailings to staff and faculty at the University of Pittsburgh. Exclusion criteria were lifetime history of psychotic disorder or any medical condition that compromised the central nervous system. In the fifth subsample, bipolar disorder was also an exclusion criterion.
2.2. Procedure
Participants in each study completed a battery of self-report inventories and clinical interviews. In all but one sample, participants were asked to identify a person who knew them well and would be willing to participate as a collaborative reporter. These informants reported on the participant for two measures used in this study. Not every measure used for external correlations was administered to each of the five samples, so in addition to descriptions, the number of observations for each measure is included.
2.3. Measures
Personality disorder symptoms (n=840).
Individual DSM-IV PD criteria were rated using the “LEAD standard” (Spitzer, 1983). LEAD is an acronym for “Longitudinal, Expert, and All Data” and requires clinicians who have demonstrated reliability to arrive at consensus decisions integrating data from all available sources (including structured diagnostic interviews with participants and collateral reports from other sources such as significant others and other mental health professionals). Data for each participant was reviewed and discussed by at least three research clinicians and a consensus was developed regarding PD criteria and diagnoses. Consensus decisions were not yet available for the fifth subsample (n=260) so ratings determined by the primary clinician using a structured interview (Structured Clinical Interview for DSM-IV Personality) were used instead.
For the current analyses, individual criteria were dichotomized. Criteria were considered present if rated “probable” or “definite.” Criteria endorsed by less than 5% of the sample were excluded from analyses. As a result, all conduct disorder items, two schizoid items, and one schizotypal item were removed. Criteria for depressive PD and passive-aggressive PD were included to maximize the number of indicators used in factor estimation.1 Though these diagnostic categories are not official diagnoses, the criteria represent meaningful, clinical manifestations of PD (Hopwood et al., 2009; McDermut at al., 2003).
Interpersonal functioning (n=840).
The Inventory of Interpersonal Problems (IIP; Alden et al., 1990) is a self-report measure of interpersonal functioning. Participants rate behavior in terms of problematic excess (i.e. behaviors you do “too much”) or deficiency (i.e. behaviors that are “hard to do”). For this study, IIP scores were summarized by level of dominance and affiliation using weighted means of items corresponding to each axis of interpersonal behavior. Additionally, an overall item average (elevation) was used to represent level of distress. Informants (n=640) completed the IIP re-worded to refer to participant behavior, and the same summary scales were calculated.
Attachment security (n=549)
The Experiences in Close Relationships Scale -- Revised (ECR-R; Fraley et al., 2000) is a self-report questionnaire that assesses adult attachment style. Participants rate statements about their feelings in romantic relationships. The ECR provides a score for level of attachment anxiety and avoidance. Informants (n=221) completed the ECR re-worded to refer to participant behavior in romantic relationships.
Adult Attachment Rating (n=840)
(AAR; Pilkonis et al., 2014) is a clinician-rated measure of attachment style. The AAR includes seven scales, with each corresponding to a prototypical attachment style. Attachment prototypes include three ratings for anxious, ambivalent attachment (excessive dependency, interpersonal ambivalence, and compulsive care-giving), three ratings for avoidant attachment (rigid self-control, defensive separation, and emotional detachment), and one rating for secure attachment.
Personality impairment (n=823).
Alternative Aspects of Personality (AA; Miller et al., 2007) is a clinician-rated measure of degree of impairment due to personality pathology within the domains of subjective distress, intimate relationships, and occupation.
Depression and anxiety (n=840)
The Hamilton Rating Scales for Depression (HRSD; Hamilton 1960) and Anxiety (HARS; Hamilton, 1959) are semi-structured, clinician-rated interviews to measure severity of depression and anxiety symptoms.
General symptomatology (n=840)
The Brief Symptom Inventory (BSI; Derogatis, 1975) is a self-report measure of psychological symptoms. Participants rate level of distress experienced in the past week. For this study, the Global Severity Index was used to assess general symptomatic distress.
Personality traits (n=513)
The NEO Personality Inventory-Revised (NEO-PI-R; Costa & McCrae, 1992) assesses personality traits that correspond to the five-factor model of personality. Participants rate the degree to which items corresponding to the five traits describe them. Ratings are summed to produce scores for neuroticism, extraversion, openness, agreeableness, and conscientiousness.
2.4. Data Analysis
All models were estimated using Mplus Version 8.1 (Muthén & Muthén, 2018). A robust weighted-least-squares estimator (WLSMV) was used with dichotomous individual PD criteria. Model selection in the initial stage of analyses was guided by fit statistics and theoretical coherence of emergent factors. Because of the number of indicators and sample size, chi-square tests of fit were not used, and we relied instead on the root mean squared error of approximation (RMSEA) and the comparative fit index (CFI) to evaluate fit. We considered RMSEA values lower than .05 indicative of excellent fit. A CFI of .90 or greater was considered acceptable. Criterion loadings greater than |.30| were used in factor interpretation in the model estimation step of analyses. Given the large sample size, we de-emphasized statistical significance when examining associations with external variables and relied instead on size of effects. Thus, correlation coefficients greater than |.30| were used in interpretation. WLSMV estimation uses a pairwise-present approach to handling missing data, which assumes that the data were missing completely at random. We believe this assumption was justifiable given that missingness was largely a function of inclusion or exclusion of measures across samples that were otherwise highly similar in composition.
3. Results
For all factor solutions, full factor loading matrices, and model fit comparisons, see supplementary files.
3.1. Unfolding Hierarchical Model
For the first model, we used Goldberg’s (2006) method of hierarchical representation. In this approach, a series of EFAs are estimated beginning with a single-factor model. Then models with an increasing number of factors are estimated with each successive model serving as a level of the hierarchy. Correlations between factor scores across models enable interpretation of factors within and between levels. This unfolding structure has been used to approximate gradation from general to specific factors in personality research, facilitating comparison with previous work.
We estimated a series of oblique, geomin-rotated EFAs with one to twelve factors. An oblique rotation was used because the factors were expected to be correlated, and geomin rotation was chosen to balance factor and variable complexity. Because no a priori assumption regarding number of factors was made, the liberal upper bound was selected to maximize interpretability. Model fit indices improved until seven factors, but the four-factor solution was deemed most interpretable, achieved acceptable fit (RMSEA=.02, CFI=.89), and was used for subsequent analyses.
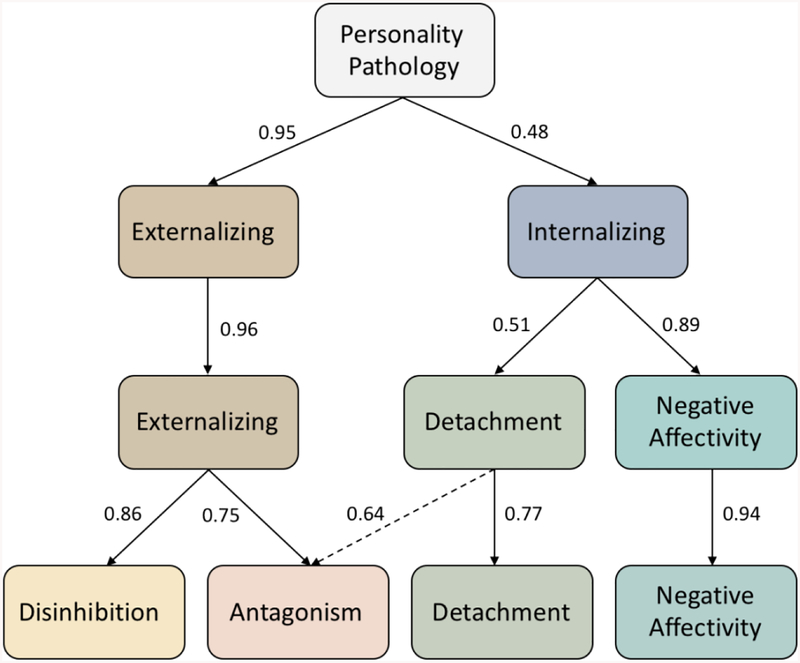
The resulting hierarchical structure is presented in Figure 1. Factor loadings for the lowest level are presented in Table 1. At the highest level of the hierarchy, nearly all PD criteria loaded on a single factor of personality pathology with the exception of obsessive-compulsive criteria, all but one of the schizoid criteria, two avoidant criteria, and two dependent criteria. As expected, the one-factor solution divided into two factors interpreted as Internalizing and Externalizing pathology. Internalizing was marked by schizoid, schizotypal, avoidant, dependent, depressive, and two obsessive-compulsive items, and Externalizing by histrionic, narcissistic, borderline, passive-aggressive, and paranoid items. At the three-factor level, Externalizing remained intact, but Internalizing split into Detachment and Negative Affectivity. The Detachment factor was marked by paranoid, schizoid, schizotypal, and obsessive-compulsive criteria, whereas avoidant, dependent, and depressive items were indicators of Negative Affectivity. Finally, Externalizing divided into Antagonism (which was also correlated with Detachment) and Disinhibition. These two Externalizing factors joined Detachment and Negative Affectivity at the lowest level of the hierarchy. All antisocial, most borderline, some histrionic, and most obsessive-compulsive criteria (with negative loadings) made up the Disinhibition factor, whereas all narcissistic, paranoid (previously loaded on Detachment), passive-aggressive, and some obsessive-compulsive items formed the Antagonism factor. The remaining borderline items loaded on Negative Affectivity, along with dependent, avoidant, and depressive criteria. At this level, half of the histrionic criteria loaded primarily and negatively on the Detachment factor, along with all schizoid and schizotypal items.
Figure 1.
Diagram of hierarchical model. Correlations between superordinate and subordinate factor levels
Table 1.
Factor loadings
| Hierarchical Model | Bifactor Model | |||||||
|---|---|---|---|---|---|---|---|---|
| PD Criteria | Antagon ism |
Detachm ent |
Negative Affectivity |
Disinhi bition |
G | Detachm ent |
Submissi ve−ness |
Disinhibi tion |
| PPD1 Suspects deception | .33 | .30 | .03 | .24 | .50 | .27 | −.05 | .02 |
| PPD2 Doubts of trust | .39 | .23 | .04 | .08 | .44 | .22 | −.01 | −.11 |
| PPD4 Reads hidden meanings | .51 | .10 | .05 | .05 | .52 | .10 | −.04 | −.17 |
| PPD5 Bears grudges | .57 | .13 | .17 | .02 | .60 | .12 | .07 | −.21 |
| PPD6 Perceives attacks | .41 | .10 | .07 | .23 | .57 | .07 | −.05 | −.01 |
| STPD1 Ideas of reference | .42 | .37 | .23 | .21 | .63 | .33 | .14 | −.03 |
| HPD3 Shallow emotion | .49 | −.37 | .07 | .06 | .49 | −.38 | −.08 | −.14 |
| HPD4 Use of appearance | .39 | −.37 | .04 | .20 | .49 | −.39 | −.13 | .00 |
| HPD8 Thinks more intimate | .43 | −.35 | .16 | −.07 | .39 | −.35 | .05 | −.20 |
| NPD1 Grandiosity |
.65 | −.03 | −.33 | .00 | .47 | .00 | −.42 | −.26 |
| NPD2 Fantasies | .63 | −.09 | −.02 | −.05 | .53 | −.08 | −.12 | −.27 |
| NPD3 Believes s/he is special | .67 | −.10 | −.03 | −.09 | .53 | −.09 | −.13 | −.32 |
| NPD4 Needs admiration | .74 | −.28 | .00 | −.12 | .57 | −.27 | −.14 | −.36 |
| NPD5 Entitlement |
.64 | −.17 | −.07 | .09 | .60 | −.17 | −.22 | −.18 |
| NPD7 Lacks empathy | .47 | .03 | −.22 | .21 | .49 | .03 | −.33 | −.04 |
| NPD8 Envy | .6 | −.09 | −.05 | −.01 | .51 | −.08 | −.15 | −.24 |
| NPD9 Arrogant behavior | .73 | .08 | −.36 | −.01 | .52 | .11 | −.44 | −.30 |
| OCPD5 Hoarding |
.33 | .12 | .22 | −.26 | .21 | .17 | .23 | −.31 |
| OCPD6 Reluctant to delegate | .32 | −.02 | .08 | −.24 | .16 | .12 | .08 | −.29 |
| OCPD8 Rigidity |
.57 | .19 | −.05 | −.29 | .31 | .17 | −.04 | −.43 |
| PAPD2 Misunderstood |
.41 | −.06 | .17 | .24 | .60 | −.10 | .01 | .00 |
| PAPD3 Argumentative |
.48 | .04 | .20 | .23 | .68 | .01 | .05 | −.03 |
| PAPD4 Criticizes authority |
.57 | .13 | −.08 | .06 | .54 | .13 | −.16 | −.19 |
| PAPD5 Envy/ resentment | .47 | .01 | .22 | .02 | .52 | .00 | .13 | −.17 |
| PAPD6 Complains |
.53 | −.11 | .23 | .17 | .68 | −.14 | .06 | −.08 |
| DRPD5 Critical towards others | .59 | .29 | −.02 | −.09 | .49 | .29 | −.05 | −.30 |
| PPD7 Suspicions of fidelity |
.15 | .07 | .25 | .30 | .44 | .03 | .13 | .15 |
| STPD2 Odd beliefs | .18 | .26 | −.02 | .31 | .3 | .23 | −.10 | .13 |
| 8 | ||||||||
| HPD2 Sexual behavior | .14 | −.33 | −.13 | .45 | .37 | −.36 | −.31 | .26 |
| NPD6 Exploitative |
.41 | .03 | −.17 | .42 | .59 | .01 | −.33 | .12 |
| ASPD1 Unlawful behavior |
−.26 | .10 | .03 | .88 | 38 | .11 | −.15 | .70 |
| ASPD2 Deceitfulness |
−.07 | .22 | −.12 | .78 | .43 | .02 | −.28 | .54 |
| ASPD3 Impulsivity |
−.25 | .21 | .00 | .76 | .31 | .16 | −.13 | .60 |
| ASPD4 Physical fights | .09 | .10 | −.17 | .71 | .50 | .14 | −.34 | .44 |
| ASPD5 Disregard for safety | −.01 | −.17 | .14 | .51 | .39 | .05 | −.02 | .36 |
| ASPD6 Irresponsibility |
−.20 | .15 | −.08 | .87 | .40 | −.22 | −.25 | .66 |
| ASPD7 Lack of remorse | .11 | .04 | −.24 | .75 | .52 | .08 | −.44 | .46 |
| BPD1 Avoids abandonment | .21 | −.22 | .27 | .32 | .50 | −.26 | .10 | .15 |
| BPD2 Idealization/deval uation |
.19 | −.21 | .32 | .49 | .62 | −.27 | .10 | .27 |
| BPD4 Impulsivity |
−.04 | −.09 | .21 | .74 | .55 | −.17 | −.01 | .52 |
| BPD6 Affect instability | .12 | −.17 | .43 | .52 | .62 | −.24 | .22 | .32 |
| BPD8 Intense anger | .12 | .01 | .25 | .58 | .61 | −.06 | .06 | .35 |
| BPD9 Transient dissociation | .10 | .04 | .39 | .42 | .52 | −.02 | .24 | .25 |
| OCPD1 Orderly |
.34 | .05 | .28 | −.39 | .15 | −.29 | .31 | −.40 |
| OCPD2 Perfectionistic |
.21 | .06 | .29 | −.44 | .01 | .06 | .35 | −.38 |
| OCPD3 Workaholic |
.47 | .11 | −.16 | −.48 | 0.4 | .08 | −.08 | −.51 |
| OCPD4 Inflexible morality |
.42 | .13 | −.02 | −.44 | 0.8 | .17 | .04 | −.46 |
| OCPD7 Miserly |
.24 | .16 | .10 | −.30 | 0.6 | −.01 | .15 | −.30 |
| PAPD1 Resists obligations | .20 | .20 | .09 | .36 | .48 | .16 | −.02 | .16 |
| SZPD1 No desire for intimacy | .27 | .79 | .00 | .04 | .32 | .78 | .05 | −.11 |
| SZPD2 Solitary activities | .11 | .76 | .02 | .02 | .17 | .75 | .10 | −.06 |
| SZPD3 No interest in sex | .17 | .39 | .11 | −.24 | .06 | .40 | .19 | −.24 |
| SZPD5 Lacks friends | .04 | .85 | −.04 | .18 | .20 | .83 | .03 | .07 |
| SZPD7 Emotional coldness |
.01 | .69 | −.11 | .04 | .04 | .68 | −.02 | .00 |
| STPD4 Odd thinking | .40 | .56 | .09 | −.07 | .38 | .55 | .11 | −.23 |
| STPD5 Suspiciousness |
.21 | .61 | −.01 | .33 | .45 | .58 | −.05 | .12 |
| STPD6 Constricted affect |
.09 | .71 | .01 | .15 | .24 | .69 | .05 | .04 |
| STPD7 Odd behavior | .10 | .73 | .07 | .19 | .2 | .70 | .10 | .06 |
| .9 | ||||||||
| STPD9 Social anxiety | .15 | .57 | .17 | .05 | .27 | .54 | .20 | −.05 |
| HPD1 Center of attention | .49 | −.53 | −.09 | .08 | .43 | −.52 | −.25 | −.12 |
| HPD6 Theatricality |
.26 | −.42 | .24 | .07 | .35 | −.44 | .10 | −.04 |
| HPD7 Easily suggestible | .16 | −.45 | .49 | .08 | .36 | −.48 | .34 | .02 |
| BPD3 Identity disturbance | .31 | −.13 | .37 | .31 | .63 | −.18 | .18 | .10 |
| BPD5 Suicidal behavior | .02 | −.16 | .53 | .35 | .43 | −.23 | .37 | .24 |
| BPD7 Chronic emptiness | .13 | −.02 | .57 | .34 | .57 | −.09 | .41 | .19 |
| AVPD1 Avoids social work | −.08 | .41 | .57 | −.02 | .16 | .37 | .60 | .01 |
| AVPD2 Must be liked | −.06 | .30 | .69 | −.06 | .19 | .25 | .70 | −.02 |
| AVPD3 Intimacy restraint |
−.01 | .34 | .47 | −.12 | .11 | .31 | .51 | −.09 |
| AVPD4 Fears rejection | −.09 | .20 | .8 | −.06 | .20 | .14 | .79 | .00 |
| AVPD5 Socially inhibited |
−.23 | .37 | .63 | −.15 | .05 | .33 | .71 | −.02 |
| AVPD6 Views self as inept | −.14 | .27 | .74 | −.02 | .16 | .21 | .75 | .04 |
| AVPD7 Avoids risk | −.01 | .30 | .52 | −.09 | .15 | .26 | .54 | −.06 |
| DNPD1 Reassurance |
−.02 | −.12 | .58 | .04 | .2 | −.16 | .51 | .05 |
| 2 | ||||||||
| DNPD2 Avoids responsibility | .05 | −.26 | .49 | .03 | .24 | −.29 | .40 | .02 |
| DNPD3 Difficulty disagreeing |
−.08 | −.01 | .56 | −.29 | .05 | −.03 | .60 | −.16 |
| DNPD4 Can’t self-initiate | .07 | −.12 | .51 | .00 | .25 | −.16 | .44 | −.02 |
| DNPD5 Seeks nurturance | −.01 | −.16 | .39 | −.10 | .07 | −.18 | .36 | −.05 |
| DNPD6 Discomfort alone |
.24 | −.31 | .47 | .03 | .41 | −.34 | .34 | −.06 |
| DNPD7 Seeks relationships | .24 | −.28 | .33 | .26 | .50 | −.32 | .16 | .10 |
| DNPD8 Fear of being left | .23 | −.25 | .51 | .10 | .45 | −.29 | .37 | −.01 |
| PAPD7 Hostile defiance | .22 | .05 | .34 | .05 | .37 | .03 | .27 | −.05 |
| DRPD1 Gloomy mood | .15 | .31 | .58 | .10 | .45 | .25 | .52 | .00 |
| DRPD2 Worthlessness |
−.15 | .13 | .77 | −.01 | .17 | .07 | .75 | .06 |
| DRPD3 Critical toward self | −.06 | .08 | .60 | −.27 | .00 | .06 | .64 | −.15 |
| DRPD4 Brooding |
.15 | .10 | .46 | −.23 | .16 | .09 | .48 | −.21 |
| DRPD6 Pessimistic |
.08 | .39 | .50 | .07 | .34 | .29 | .48 | .01 |
| DRPD7 Prone to guilt | −.17 | .05 | .56 | −.21 | .0 | .34 | .60 | −.07 |
| .8 | ||||||||
Primary loadings over >|.30| are bolded and underlined. ASPD=antisocial; AVPD=avoidant;
BPD=borderline; DNPD=dependent; DRPD=depressive; HPD=histrionic; NPD=narcissistic;
PAPD=passive-aggressive; PPD=paranoid; STPD=schizotypal; SZPD=schizoid.
3.2. Bifactor Model
We used a bifactor rotation method for EFA with the same PD criteria. In this approach, each indicator was allowed to load onto a specific factor and an orthogonal general factor which partitioned each indicator’s shared and specific variance. To remain consistent across models, we estimated a series of bifactor EFAs with one to twelve specific factors using a bifactor geomin (with orthogonal specific factors) rotation. Models beyond three specific factors included factors with few primary PD criteria loadings, suggesting over-extraction. For subsequent analyses, a model with three specific factors was selected for both interpretability and acceptable model fit statistics. The RMSEA and CFI were identical to the unfolding factor solution because the same number of factors was retained (general and three specific factors); the models differ only in rotation. Additionally, alternative fit indices recommended for evaluating bifactor models (Rodriguez et al., 2016) indicated a well-defined general factor that explained 86% of the common variance in the model with good reliability (ω=.83).
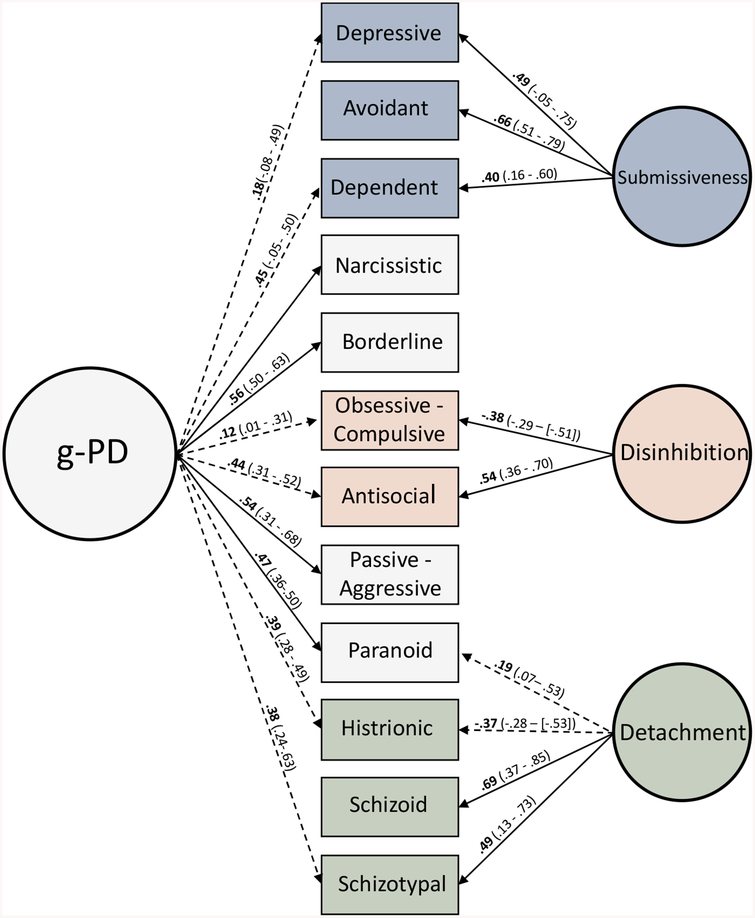
Factor loadings from the final bifactor model are presented in Table 1, and the structure is depicted in Figure 2. The general factor consisted of all borderline, narcissistic, and passive-aggressive items, and all but one paranoid criterion. It also included some loadings of schizotypal, histrionic, dependent, depressive, and antisocial criteria. In this model, a specific Antagonism factor was not found as all criteria that formed this factor in the unfolding model were included in the general factor. The specific factors were interpreted as Detachment, Disinhibition, and Submissiveness. Similar to the unfolding model, schizoid, schizotypal, and histrionic (negatively loaded) items formed a Detachment factor. Disinhibition was marked by all antisocial criteria and negative loadings of all but one obsessive-compulsive items; it no longer included any borderline items. Submissiveness resembled Negative Affectivity in the unfolding model, with all avoidant, dependent, and depressive criteria, but without any borderline items, which loaded exclusively on the general factor in this model.
Figure 2.
Diagram of bifactor model. Observed variables refer to all indicators associated with that PD, not individual criteria. Only criteria loadings >|.30| are used for interpretation. Solid lines indicate primary loadings for half or more of criteria. Dashed lines indicate primary loadings for less than half of criteria. Bolded values are average loadings for each PD, range of loadings in parenthesis.
3.3. Factor Similarity
To facilitate direct, statistical comparison between factors in each model, we calculated congruence coefficients for those factors composed of comparable PD criteria. The degree of similarity between factors was used to aid interpretation of points of convergence and divergence between each model. As they are approximating the same constructs, we expected the overall structural elements in each model to have substantial overlap, but to also differ in ways indicative of conceptual differences between the two approaches. The Detachment factors were the most similar (rc=.97), followed by Submissiveness in the bifactor with Negative Affectivity in the unfolding model (rc=.94), whereas the Disinhibition factors were less similar (rc=.85). Despite sharing many of the same criteria, the general factor in the bifactor model was fairly distinct from Antagonism in the unfolding model (rc=.78).
3.4. Correlations Between Factors and Measures of Functioning
In the second stage of analyses, we used exploratory structural equation modeling to examine correlations between the factors from both models and measures of general psychiatric functioning, attachment style, interpersonal distress, and personality to validate and enrich factor interpretation. All correlations are provided in Table 2.
Table 2.
Correlations Between Factors and External Variables
| Hierarchical Model | Bi-factor Model | |||||||
|---|---|---|---|---|---|---|---|---|
| Variable | Antagoni sm |
Detachm ent |
Negative Affectivi ty |
Disinhibiti on |
Gener al |
Detachm ent |
Submissiven ess |
Disinhibiti on |
| IIP Dominance | .20 | −.19 | −.49 | .33 | .18 | −.12 | −.60 | .09 |
| IIP Affiliation | −.12 | −.44 | −.02 | −.17 | −.17 | −.44 | .02 | −.12 |
| IIP Elevation | .29 | .12 | .63 | .21 | .42 | .05 | .51 | .06 |
| IIP Dominance * |
.15 | −.18 | −.31 | .16 | −.04 | −.08 | −.38 | .07 |
| IIP Affiliation * |
−.08 | −.45 | −.02 | −.05 | −.15 | −.45 | −.01 | −.06 |
| IIP Elevation* | .10 | −.05 | .38 | .33 | .32 | −.21 | .24 | .34 |
| ECR Attachment Anxiety |
.06 | −.09 | .32 | .21 | .20 | −.14 | .25 | .19 |
| ECR Attachment Avoidance |
.04 | .04 | .28 | .17 | .17 | .01 | .23 | .19 |
| ECR Attachment Anxiety* |
.21 | −.04 | .48 | .37 | .40 | −.11 | .33 | .25 |
| ECR Attachment Avoidance* |
−.03 | .25 | .17 | −.16 | −.03 | .26 | .26 | −.10 |
| AAR Excessive Dependency |
.10 | −.35 | .43 | .11 | .21 | −.45 | .31 | .02 |
| AAR Interpersonal Ambivalence |
.35 | −.25 | .29 | .60 | .55 | −.31 | −.01 | .28 |
| AAR Rigid Self-Control | .19 | .16 | −.04 | −.52 | −.12 | .18 | .06 | −.65 |
| AAR Defensive Separation |
.25 | .32 | −.05 | .09 | .21 | .34 | −.10 | −.09 |
| AAR Emotional Detachment |
.39 | .05 | −.10 | .63 | .51 | .09 | −.36 | .27 |
| AAR Compulsive Care-giving |
−.08 | −.19 | .04 | −.20 | −.15 | −.20 | .09 | −.15 |
| AAR Secure | −.32 | −.32 | −.42 | −.54 | −.60 | −.23 | −.21 | −.37 |
| AA Subjective | .00 | .06 | .42 | .35 | .25 | .00 | .35 | .41 |
| Distress | ||||||||
| AA Intimate Relationships | −.02 | .12 | .21 | .42 | .22 | .09 | .15 | .48 |
| AA Occupational |
.06 | .15 | .20 | .54 | .32 | .13 | .10 | .54 |
| BSI Global | .22 | −.14 | .43 | .33 | .39 | −.21 | .29 | .19 |
| HRSD Depression |
.23 | −.09 | .48 | .38 | −.15 | .33 | .23 | |
| HARS Anxiety |
.23 | −.11 | .44 | .36 | .40 | −.16 | .29 | .21 |
| NEO-PI Neuroticism |
.31 | .00 | .66 | .17 | .48 | −.08 | .48 | .04 |
| NEO-PI Extraversion |
.00 | −.36 | −.29 | −.03 | −.09 | −.29 | −.32 | −.13 |
| NEO-PI Openness |
−.07 | −.09 | .10 | −.19 | −.07 | −.13 | .14 | −.16 |
| NEO-PI Agreeableness |
−.15 | −.21 | .08 | −.30 | −.16 | −.25 | .14 | −.26 |
| NEO-PI Conscientious ness |
.20 | −.19 | −.10 | −.20 | .07 | −.12 | −.18 | −.40 |
Bolded, underlined correlations >|.30|,
=informant report.
IIP=Inventory of Interpersonal Problems (self, informant report), ECR=Experiences in Close Relationships (self, informant report), AAR=Adult Attachment Rating (clinician report), AA=Alternative Aspects of Personality Disorder (clinician report), BSI=Brief Symptom Inventory (self-report), HRSD=Hamilton Rating Scale for Depression (clinician report), HARS=Hamilton Rating Scale for Anxiety (clinician report), NEO-PI=NEO Personality Inventory (self-report).
In the oblique four-factor model, Detachment was distinguished by low extraversion, low affiliation, avoidant attachment, and lack of subjective distress or clinician-rated impairment. Antagonism was marked by attachment insecurity and neuroticism, but was otherwise uncorrelated with general or interpersonal distress or clinician-rated impairment. Unlike the previous two factors, Disinhibition and Negative Affect were associated more strongly with subjective distress. Disinhibition was also correlated with informant and clinician ratings of interpersonal impairment and attachment insecurity, but not self-reported interpersonal distress. Disinhibition was also marked by general psychiatric symptoms across self and clinician ratings. Negative Affectivity was distinguished by correlations with general psychiatric symptoms, anxious and dependent attachment styles, submissiveness, and interpersonal distress.
In the bifactor model, the general factor was associated with informant and clinician ratings of attachment insecurity, interpersonal distress, and general psychiatric symptoms. For the specific factors, correlations with Detachment in this model were nearly identical to those from the oblique model, with the exception of less attachment insecurity. Disinhibition was not associated with attachment insecurity, interpersonal distress, or internalizing symptoms, unlike the oblique model, but was marked primarily by clinician and informant ratings of impairment and low constraint (negative correlations with conscientiousness and rigid, controlling attachment style). As expected, Submissiveness was distinguished by low dominance as well as interpersonal distress, anxious and dependent attachment styles, and internalizing symptoms. Submissiveness resembled the Negative Affectivity factor in the oblique model but was more strongly correlated with low dominance and less strongly correlated with general psychiatric distress.
4. Discussion
This study used factor analysis to investigate competing dimensional structures for personality pathology. Using individual PD criteria from a large sample, we estimated an unfolding hierarchical model with four factors at the lowest level and a bifactor model with a general factor and three specific factors. Both were determined to be good-fitting models; indeed, they had identical fit statistics. Correlations between the factors in the two models and measures of functioning revealed easily interpretable associations, further supporting construct validity for both models.
4.1. Interpretation of Hierarchical and Bifactor Models
As hypothesized, each modeling approach produced interpretively distinct structures consistent with other work. Before discussing each model in greater detail, some overall points of comparison should be made. Though both models included analogous factors, the pattern of associations with external variables and factor congruence coefficients suggest that the factors are not isomorphic. Specifically, Detachment, Negative Affect/Submissiveness, and Disinhibition to a somewhat lesser degree, appear to be relatively coherent pathological styles that, after accounting for shared variance with general personality pathology, differ mainly by severity (i.e., are less strongly correlated with indicators of dysfunction). In contrast, Antagonism can be conceptualized as a unique domain or as features common to all forms of personality pathology.
As replicated across studies of personality and psychopathology broadly, we found the general factor in the hierarchical model divided into Internalizing and Externalizing pathology. Unlike corresponding PD models using self-reported data (Wright et al., 2012; Wright & Simms, 2014), the Externalizing factor in this model was more strongly correlated with the initial general factor than was Internalizing pathology. Morey, Krueger, and Skodol (2014) estimated an unfolding hierarchical model using clinician-rated PD criteria and found results similar to the current study with an Externalizing factor at the second level most strongly correlated with the general factor.
Systematic discrepancies between informant and self-reported impairment are evident in our results, which included measures from multiple reporting sources. In nearly all cases that sources differed, informant and clinician ratings were more strongly associated with our dimensions than participant self-reports. It is possible that problematic interpersonal behavior experienced by others may be underreported by the individuals emitting those behaviors.
Additionally, because the sample used in the current study is arguably the most comprehensive to date in terms of number of PD indicators included in analyses, our findings support the view that personality pathology is best characterized by interpersonal conflict and antagonism.
A related consideration when contextualizing our findings with other studies is the impact of method variance. For instance, compared to much of the literature, we find relatively modest correlations between factors derived from clinician PD ratings and self-reported personality. Meta-analytic reviews demonstrate a clear relationship between basic personality and PD, but also show that cross-method associations attenuate these effects (Saulsman & Page, 2004). For the purpose of construct validation, it is less critical that our effect sizes replicate exactly those of others—rather, it is more important that general patterns of associations are similar. That the models in this study are broadly consistent with previous work, despite the number of cross-method comparisons, makes these results all the more compelling.
At the lowest level of the hierarchy in the unfolding model, the four-factor solution resembles that of other pathological trait models which converge on variants of Extraversion-Introversion, Antagonism-Agreeableness, Impulsivity-Constraint, and Emotional Dysregulation-Stability (Widiger & Simonsen, 2005). Up to the four-factor level, our results closely map the structure found in other studies using Goldberg’s method with PD criteria (Wright et al., 2012; Morey et al., 2014). In contrast to the five maladaptive traits included in some measurement models, a Psychoticism/Thought Disorder dimension did not emerge in our data even when more than four factors were extracted. However, this result was not surprising given our sampling frame—participants with a lifetime history of psychotic symptoms were excluded—coupled with the level of severity required to reach a clinical threshold with psychoticism items.
The bifactor model in this study can also be interpreted in the context of other, similar models to draw substantive conclusions. The saturation of the general PD factor with borderline criteria may be the most robust finding across studies (Sharp et al., 2015; Williams et al., 2015, Wright et al., 2016), including the current one. This finding has been interpreted previously to suggest that borderline features represent fundamental disturbances in self-definition and interpersonal relatedness underlying all personality pathology rather than a discrete subtype of PD (Sharp et al., 2015). Furthermore, in this study, a specific Antagonism factor did not appear in the bifactor model; rather, virtually all the criteria that comprised Antagonism in the hierarchical model were included in the general factor, and the remaining specific factors differed between models mainly by strength of association with measures of functioning. Taken together, these findings are consistent with the continuum of severity proposed for personality dysfunction by some theorists (Kernberg, 1984; Bender et al., 2011). It is possible that antagonistic PD features were overrepresented in this sample given certain recruitment goals, which in turn could affect interpretation of the general factor. However, similar bifactor model results have been found across different clinical populations, and similar hierarchical models have been found using non-clinical samples (e.g., Wright et al., 2012).
It is also notable that two of the specific factors in the bifactor model align with the axes of the interpersonal circumplex (dominance and affiliation), namely Submissiveness (low dominance) and Detachment (low affiliation), which supports the theoretical “interpersonal core” of personality pathology (Hopwood et al., 2013). It has been proposed that extremes in dominance correspond to agentic problems and that extremes in affiliation correspond to difficulties relating to others (Pincus, 2018). One interpretation of the Detachment and Submissiveness factors in this study is that they represent patterns of agentic and affiliative expression (style), whereas the general factor represents pervasiveness of impairment across self and other (severity). In further support of this interpretation, Detachment was correlated with self- and informant-reported problems with affiliation, Submissiveness was correlated with self- and informant-reported problems with dominance, and both were correlated with clinician-rated problems in attachment.
4.2. Implications
We do not present these results as evidence for the superiority of one model over another. Instead, we hope to clarify disagreement between approaches to enable more productive conversation and research surrounding dimensional models of personality pathology. These models are empirically indistinguishable by all model fit statistics, with both fitting the data well. Accordingly, any argument in favor or against either model is not a matter of statistical fit. Both models demonstrate interpretable patterns of correlations with external variables and convergence with established theoretical traditions. Thus, the distinction between these models is conceptual, and each approach has significant but divergent implications for the future of personality pathology research and theory.
An oblique dimensional approach integrates personality pathology into a broader framework of personality and psychopathology. Thus, this approach is valuable for investigation of common processes that cut across clinical syndromes and that may be relevant to etiology, pathogenesis, natural history of disorders, and response to treatment. This conceptualization has been productively operationalized by the HiTOP model and may appeal to proponents of the National Institute of Mental Health’s Research Domain Criteria initiative which seeks to identify transdiagnostic mechanisms grounded in observable behavior and neurobiology. Indeed, there is mounting evidence that factor analytically defined spectra share common genetic variance (Kendler et al., 2011; Dick et al., 2008) and environmental risk factors (Vachon et al., 2015), and that they predict symptom course better than DSM categories (Vollebergh et al., 2001). This approach effectively eliminates personality pathology as a distinct construct and draws attention away from the rich, longstanding literature defining core self and interpersonal dysfunction. By reorganizing and merging those clinical features with other descriptively similar symptoms, there is potential for gains in transdiagnostic assessment, but a loss of focus on foundational understandings of personality pathology.
In contrast, models that organize PD criteria into general and specific factors aim to distinguish personality pathology from other forms of psychopathology and refine our understanding of PDs as distinct clinical phenomena. This approach is especially useful for research concentrated on personality pathology, development of clinical assessments, and identification of mechanisms most relevant to the treatment of PDs. Studies which demonstrate the predictive value of general impairment severity, regardless of stylistic expression, have enhanced efforts to define basic features of personality functioning (Bender et al., 2011; Hopwood et al., 2011; Livesley, 2006). Assessment instruments informed by accurate definition of a continuum of PD severity may improve diagnostic precision and therapeutic outcomes (Berghuis et al., 2014). These models are predicated on the importance of self and interpersonal impairments for understanding personality pathology, whereas factor analytic research from an integrative hierarchical approach does not capture this core. For this reason, general and specific models are less compatible quantitatively and conceptually with broader taxonomic efforts. Such a divergence could represent a lost opportunity for personality pathology research to build on advances made by the growing literature on transdiagnostic features and processes.
Any debate over which dimensional classification model provides the “best fit” will not be resolved by statistical metrics alone—and may largely miss important intellectual and clinical points. Empirical fit is only meaningful in the context of the theoretical model that data are intended to test, and deciding on appropriate theoretical models will, in turn, be guided by this purpose. Is personality pathology best understood in terms of cross-cutting spectra or by fundamental self and interpersonal dysfunction? As we continue to improve taxonomic and diagnostic systems of personality and psychopathology, it is important that the underlying conceptual implications of model selection are carefully considered, because whichever structure is pursued will provide the foundation for subsequent research and theory development.
Highlights.
We estimated an unfolding hierarchical model and bifactor model using personality disorder criteria that showed good and equivalent fit.
Factors from both models were associated with external measures of general psychiatric and interpersonal functioning.
Results support the construct validity of each model approach.
Our study points to the importance of the considering conceptual implications of model selection.
Acknowledgments
This research was supported by a grant from the National Institute of Mental Health (R01 MH056888, PI: Pilkonis). The views contained in the manuscript are those of the authors and not necessarily those of the funding source.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declarations of interest: None.
We estimated the final models without these criteria and correlations with all external variables were nearly identical.
References
- Alden LE, Wiggins JS, & Pincus AL (1990). Construction of circumplex scales for the Inventory of Interpersonal Problems. Journal of Personality Assessment, 55(3–4), 521–536. [DOI] [PubMed] [Google Scholar]
- Berghuis H, Kamphuis JH, & Verheul R (2014). Specific personality traits and general personality dysfunction as predictors of the presence and severity of personality disorders in a clinical sample. Journal of Personality Assessment, 96(4), 410–416. [DOI] [PubMed] [Google Scholar]
- Bender DS, Morey LC, & Skodol AE (2011). Toward a model for assessing level of personality functioning in DSM–5, part I: A review of theory and methods. Journal of Personality Assessment, 93(4), 332–346. [DOI] [PubMed] [Google Scholar]
- Brodbeck J, Abbott RA, Goodyer IM, & Croudace TJ (2011). General and specific components of depression and anxiety in an adolescent population. BMC Psychiatry, 11(1), 191–191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caspi A, Houts RM, Belsky DW, Goldman-Mellor SJ, Harrington H,…Moffitt TE (2014). The p factor: One general psychopathology factor in the structure of psychiatric disorders? Clinical Psychological Science, 2(2), 119–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark LA, & Ro E (2014). Three-pronged assessment and diagnosis of personality disorder and its consequences: Personality functioning, pathological traits, and psychosocial disability. Personality Disorders: Theory, Research, & Treatment, 5(1), 55–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costa PT, & McCrae RR (1992). Normal personality assessment in clinical practice: The NEO personality inventory. Psychological Assessment, 4(1), 5–13. [Google Scholar]
- Derogatis LR (1977). SCL-90: Administration, scoring, and procedures manual I. Baltimore: Clinical Psychometrics Research. [Google Scholar]
- Dick DM, Aliev F, Wang JC, Grucza RA, Schuckit M, Kuperman S, …Goate A (2008). Using dimensional models of externalizing psychopathology to aid in gene identification. Archives of General Psychiatry, 65(3), 310–318. [DOI] [PubMed] [Google Scholar]
- Few LR, Miller JD, Rothbaum AO, Meller S, Maples S, Terry J, Collins B, & Mackillop J (2013). Examination of the section III DSM-5 diagnostic system to personality disorders in an outpatient clinical sample. Journal of Abnormal Psychology, 122(4), 1057–1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fraley RC, Waller NG, & Brennan KA (2000). An item response theory analysis of self-report measures of adult attachment. Journal of Personality and Social Psychology, 78(2), 350–365. [DOI] [PubMed] [Google Scholar]
- Goldberg LR (2006). Doing it all Bass-Ackwards: The development of hierarchical factor structures from the top down. Journal of Research in Personality, 40(4), 347–358. [Google Scholar]
- Hamilton M (1960). A rating scale for depression. Journal of Neurology, Neurosurgery, and Psychiatry, 23, 56–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamilton M (1959). The assessment of anxiety states by rating. British Journal of Medical Psychology, 32, 50–55. [DOI] [PubMed] [Google Scholar]
- Hopwood CJ, Morey LC, Markowitz JC, Pinto A, Skodol AE, Gunderson JG, …Sanislow CA(2009). The construct validity of passive-aggressive personality disorder. Psychiatry, 72(3), 256–267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hopwood CJ, Malone JC, Ansell EB, Sanislow CA, Grilo CM,…Morey LC (2011). Personality assessment in DSM–V: Empirical support for rating severity, style, and traits. Journal of Personality Disorders, 25(5), 305–320. [DOI] [PubMed] [Google Scholar]
- Hopwood CJ, Wright AGC, Ansell EB, & Pincus AL (2013). The interpersonal core of personality pathology. Journal of Personality Disorders, 27(3), 271–295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hyman SE (2010). The diagnosis of mental disorders: The problem of reification. Annual Review of Clinical Psychology, 6(1), 155–179. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Aggen SH, Knudsen GP, Røysamb E, Neale MC, & Reichborn-Kjennerud T (2011). The structure of genetic and environmental risk factors for syndromal and subsyndromal common DSM-IV axis I and all axis II disorders. American Journal of Psychiatry, 168(1), 29–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kernberg OF (1984). Severe personality disorders: Psychotherapeutic strategies. New Haven: Yale University Press. [Google Scholar]
- Kim H, & Eaton NR (2015). The hierarchical structure of common mental disorders: Connecting multiple levels of comorbidity, bifactor models, and predictive validity. Journal of Abnormal Psychology, 124(4), 1064–1078. [DOI] [PubMed] [Google Scholar]
- Kotov R, Krueger RF, Watson D, Achenbach TM, Althoff RR, …Zimmerman M (2017). The hierarchical taxonomy of psychopathology (HiTOP): A dimensional alternative to traditional nosologies. Journal of Abnormal Psychology, 126(4), 454–477. [DOI] [PubMed] [Google Scholar]
- Livesley WJ (2006). General assessment of personality disorder (GAPD). Department of Psychiatry, University of British Columbia. [Google Scholar]
- McDermut W, Zimmerman M, & Chelminski I (2003). The construct validity of depressive personality disorder. Journal of Abnormal Psychology, 112(1), 49–6. [PubMed] [Google Scholar]
- Miller JD, Campbell WK, & Pilkonis PA (2007). Narcissistic personality disorder: Relations with distress and functional impairment. Comprehensive Psychiatry, 48(2), 170–177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morey LC, Krueger RF, & Skodol AE (2013). The hierarchical structure of clinician ratings of proposed DSM-5 pathological personality traits. Journal of Abnormal Psychology, 122(3), 836–841. [DOI] [PubMed] [Google Scholar]
- Muthén LK, & Muthén BO (2018). Mplus user’s guide (8th ed.). Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- Pilkonis PA., Kim Y, Yu L, & Morse JQ (2014). Adult attachment ratings (AAR): An item response theory analysis. Journal of Personality Assessment, 96(4), 417–425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pincus AL (2018). An interpersonal perspective on Criterion A of the DSM-5 Alternative Model for Personality Disorders. Current Opinion in Psychiatry, 21, 11–17. [DOI] [PubMed] [Google Scholar]
- Rodriguez A, Reise SP, & Haviland MG (2016). Evaluating bifactor models: Calculating and interpreting statistical indices. Psychological Methods, 21(2), 137–150 [DOI] [PubMed] [Google Scholar]
- Saulsman LM, & Page AC (2004). The five-factor model and personality disorder empirical literature: A meta-analytic review. Clinical Psychology Review, 23(8), 1055–1085. [DOI] [PubMed] [Google Scholar]
- Sharp C, Wright AGC, Fowler JC, Frueh BC, Allen JG, Oldham J, & Clark LA (2015). The structure of personality pathology: Both general (‘g’) and specific (‘s’) factors? Journal of Abnormal Psychology, 124(2), 387–398. [DOI] [PubMed] [Google Scholar]
- Spitzer RL (1983). Psychiatric diagnosis: Are clinicians still necessary? Comprehensive Psychiatry, 24(5), 399–411. [DOI] [PubMed] [Google Scholar]
- Trull TJ, & Durrett CA (2005). Categorical and dimensional models of personality disorder. Annual Review of Clinical Psychology, 1(1), 355–380. [DOI] [PubMed] [Google Scholar]
- Tyrer P (2005). The problem of severity in the classification of personality disorder. Journal of Personality Disorders, 19(3), 309–314. [DOI] [PubMed] [Google Scholar]
- Vachon DD, Krueger RF, Rogosch FA, & Cicchetti D (2015). Assessment of the harmful psychiatric and behavioral effects of different forms of child maltreatment. JAMA Psychiatry, 72(11), 1135–1142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vollebergh WAM, Iedema J, Bijl RV, de Graaf R, Smit F, & Ormel J (2001). The structure and stability of common mental disorders: The NEMESIS study. Archives of General Psychiatry, 58(6), 597–603 [DOI] [PubMed] [Google Scholar]
- Widiger TA, & Simonsen E (2005). Alternative dimensional models of personality disorder: Finding a common ground. Journal of Personality Disorders, 19(2), 110–130. [DOI] [PubMed] [Google Scholar]
- Williams TF, Scalco MD, & Simms LJ (2018). The construct validity of general and specific dimensions of personality pathology. Psychological Medicine, 48(5), 834–848. [DOI] [PubMed] [Google Scholar]
- Wright AGC (2017). The current state and future of factor analysis in personality disorder research. Personality Disorders: Theory, Research, and Treatment, 8(1), 14–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright AGC, Hopwood CJ, Skodol AE, & Morey LC (2016). Longitudinal validation of general and specific structural features of personality pathology. Journal of Abnormal Psychology, 125(8), 1120–1134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright AGC, & Simms LJ (2014). On the structure of personality disorder traits: Conjoint analyses of the CAT-PD, PID-5, and NEO-PI-3 trait models. Personality Disorders: Theory, Research, and Treatment, 5(1), 43–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright AGC, Thomas KM, Hopwood CJ, Markon KE, Pincus AL, & Krueger RF (2012). The hierarchical structure of DSM-5 pathological personality traits. Journal of Abnormal Psychology, 121(4), 951–957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright AGC & Zimmermann J (2015). At the nexus of science and practice: Answering basic clinical questions in personality disorder assessment and diagnosis with quantitative modeling techniques In Huprich S (Ed.), Personality disorders: Toward theoretical and empirical integration in diagnosis and assessment (pp. 109–144). Washington, DC: American Psychological Association. [Google Scholar]