Abstract
Study Objectives:
Studies have shown racial differences in circadian rhythm in African Americans when compared to non-Hispanic whites, and an association between circadian dyssynchrony and depression. We hypothesized that the prevalence of delayed sleep time is greater in African Americans when compared to whites and that delayed sleep time is associated with depression.
Methods:
We analyzed data from the Sleep Heart Health Study (SHHS), a large community-based sample. Delayed sleep time was defined as self-reported weeknight bedtime after midnight. Depression was defined based on participant's response to the question, “In the past 4 weeks have you felt downhearted and blue?” or reported antidepressant use. We performed multivariate linear and logistic regression, adjusting for age, sex, race, body mass index, smoking, apnea-hypopnea index, alcohol use, and caffeine consumption.
Results:
Adjusted weekday bedtime was 15 ± 7 minutes later in African Americans compared to whites (P < .001). Similarly, weekend bedtime was 18 ± 7 minutes later in African Americans compared to whites (P = .025). The prevalence of delayed sleep time was greater in African Americans (33.3%) compared to whites (18.7%; P < .001). After adjusting for confounders, when compared to whites, a greater proportion of African Americans had delayed sleep time (adjusted odds ratio [aOR] 2.03; 95% confidence interval [95% CI] 1.5, 2.4; P < .0001). Depression was independently associated with delayed sleep time after adjustment (aOR 1.4; 95% CI 1.1, 1.7; P = .007).
Conclusions:
African Americans are more likely to have a delayed sleep time compared to whites, and delayed sleep time was independently associated with depression.
Citation:
Bailey O, Combs D, Sans-Fuentes M, Havens CM, Grandner MA, Poongkunran C, Patel S, Berryhill S, Provencio N, Quan SF, Parthasarathy S. Delayed sleep time in African Americans and depression in a community-based population. J Clin Sleep Med. 2019;15(6):857–864.
Keywords: African American, delayed sleep phase, depression, health disparities
BRIEF SUMMARY
Current Knowledge/Study Rationale: Delayed sleep timing is well described in children and adolescents, and is associated with depression and other adverse outcomes, and may be more prevalent in certain ethnic groups. We hypothesized that delayed sleep timing is more common in African Americans, and that it is associated with depression in a community cohort of older adults.
Study Impact: African Americans were twice as likely to have delayed sleep timing compared to whites. African Americans obtained 22 minutes less sleep on weeknights compared to whites, which was related to delayed sleep timing. Additionally, individuals with delayed sleep timing were 40% more likely to have depression.
INTRODUCTION
Delayed sleep time or evening-type circadian preference is the consequence of a delay in the internal circadian clock influenced by behavioral, environmental, or genetic factors.1,2 Delayed sleep time often leads to shortened sleep duration because of social responsibilities in working adult populations.3 Delayed sleep timing may also have deleterious effects on human health including obesity, cancer, heart disease, and depression.4–6 These disorders have a higher prevalence among African Americans,7–9 but it is unknown if delayed sleep time may contribute to this disparity.3,4,10–13 Although the delayed sleep timing and chronotype across race/ethnicity may be an important mechanistic underpinning for health and disease, it should be recognized that they are a product of both circadian and homeostatic factors and not the circadian influences alone.
Experimental studies have shown an association between circadian misalignment and major depression.14 One such study, by Li et al, identified clock gene expression at the time of death in human brains postmortem.15 Participants with known depression were more likely to have circadian misalignment at the time of death compared to those without depression. Other experimental studies have also suggested the presence of racial/ethnic differences in the circadian rhythm of participants with African ancestry when compared to those of European ancestry.16,17 This includes differences in circadian period (tau) in African Americans when compared to non-Hispanic whites (hereafter referred to as whites), and may suggest racial differences in susceptibility to circadian phase shifting.18 In the United Kingdom Biobank study, blacks were more likely to exhibit morning-type sleep behavior than Caucasians.19 However, in the United States the relationship between delayed sleep time and race, as well as the relationship between depression and delayed sleep time by race/ethnicity remains largely unknown.
Our primary aim was to determine whether race is independently associated with delayed sleep time in a large community-based cohort of United States adults in the Sleep Heart Health Study (SHHS). We hypothesized that in the SHHS cohort, the prevalence of delayed sleep time is greater in African Americans when compared to whites. Additionally, we hypothesized that delayed sleep time is associated with an increased risk for depression. Such findings may lead to signifi-cant public health implications and potential advancements in the precision of diagnosing, preventing, and managing depression among African Americans.
METHODS
Study Population
SHHS was a large multicenter community-based prospective cohort study whose original aim was to assess whether sleep-disordered breathing is a risk factor for cardiovascular disease in middle-aged adults.20,21 Participants in SHHS were recruited from ongoing cohorts including the Cardiovascular Health Study, the Framingham Heart Study, the Tucson Epidemio-logic Study of Obstructive Airways Disease, the Strong Heart Study, the Atherosclerosis Risk in Communities Study, and the Health and Environment Cohort Study in Tucson, as well as New York City cohorts.21–25 Participants older than 40 years were included in the study. Exclusion criteria included history of positive airway pressure treatment for sleep apnea, tracheostomy, or use of supplemental oxygen. Participants completed unattended polysomnography, structured health interviews, and sleep questionnaires between December 1995 and January 1998. We analyzed these data from the SHHS to compare the prevalence of delayed sleep time among African Americans to whites, and further examine the relationship between delayed sleep time and depression.
Data Sources
Demographic information, including age, sex, and self-identified race/ethnicity, was derived from the participant's parent cohort. Race and ethnicity were determined by self-identification from demographic questionnaires of the parent cohort. A structured health interview was performed to determine smoking history (pack-years), alcohol use (drinks per week), caffeine consumption (cups of coffee per day) and current medications (presence or absence of antidepressants). We used the question, “in the past 4 weeks have you felt downhearted and blue?” to determine the presence of depression. Participants responded on a 6-point Likert scale ranging from 1 (“all of the time”) to 6 (“none of the time”). Values from 1–3 on the 6-point Likert scale and/or reported use of antidepressant medications (determined by manual review of medication list) were used to define the presence of depression. Participants' weight was measured using a calibrated scale at the time of polysomnography. Participants' height was taken from parent study data obtained within 3 years of the sleep study and used to calculate body mass index (BMI) (kg/m2). Polysomnography was performed in the patient's home using the P Series System (Compumedics, Abbotsford, Victoria, Australia). Polysomnography was scored using standard criteria.26,27 Self-reported bedtime and sleep duration on weekdays and weekends were obtained from the SHHS Sleep Habits Questionnaire. Delayed sleep time was defined as reported time to fall asleep later than midnight on weekdays (which was defined as > 2 hours after socially accepted bedtime of 10:00 pm).
Statistical Analysis
Statistical analysis was performed using SPSS Version 25 (IBM Corp, Armonk, New York, United States). To assess for demographic differences between groups, Pearson χ2 tests were used for categorical variables and linear regression was used for continuous variables. Sleep timing was also evaluated at an hourly interval from 9:00 pm until 4:00 am to compare reported bedtime differences between white and African-American participants at each hour. Binary logistic regression was used to compare the likelihood of delayed sleep time between races, with adjustment for age, sex, BMI, smoking, apnea-hypopnea index, alcohol use, and caffeine consumption. Binary logistic regression was also used to determine the relationship between delayed sleep time and depression, with adjustment for age, sex, BMI, smoking, apnea-hypopnea index, alcohol use, and caffeine consumption. Additionally, we performed linear regression to compare reported sleep timing and duration between races. We adjusted for the same covariates as for the aforementioned logistic regression. We additionally performed moderation analysis to evaluate the potential moderating effects of age and sex on the relationship between race and delayed sleep timing. Moderation analysis was performed using the PROCESS macro for SPSS.28 Finally, given that delayed sleep time is likely to be associated with short sleep duration, we evaluated the relationship between delayed sleep time and depression after stratifying our sample by reported weekday sleep duration of < 7 hours versus ≥ 7 hours. Seven hours was selected to be consistent with prior literature19 on short sleep duration as well as the current American Academy of Sleep Medicine/Sleep Research Society guidelines.29 Results are presented throughout as either mean ± standard deviation, or mean (95% confidence interval [CI]).
We performed sensitivity analysis for the association between delayed sleep time and depression using linear regression (for depression categories ranging from 1 to 6) as well as using logistic regression excluding participants who reported use of antidepressant medications. This approach to sensitivity analysis was selected based on a prior approach to evaluate depression in the Hispanic Community Health Study/Study of Latinos.30 In addition to weekday bedtime, we also evaluated differences in weekend bedtime as well as used a weighted average of weekday and weekend bedtime:
We additionally evaluated midsleep timing as an alternate circadian rhythm marker. Midsleep timing was calculated using the formula derived from the Munich Chronotype Questionnaire.31 Midsleep on free days (MSF) was calculated using the following equation:
Midsleep on free nights corrected for weekend oversleep (MSFsc) was measured using the equation:
 |
RESULTS
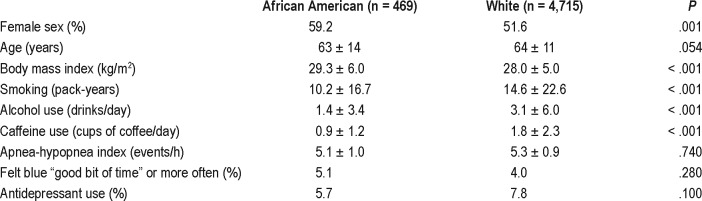
A comparison of the demographic data from African-American and white participants is shown in Table 1. The cohort has a total of 5,184 African-American and white participants with a similar mean age, BMI, and apnea-hypopnea index. Whites had a statistically significant higher mean pack-years smoking history, alcohol use, and caffeine use. There was no significant overall difference in incidence of depressed mood or antidepressant use.
Table 1.
Participant demographics.
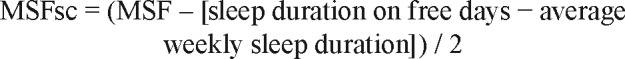
We found that African Americans were more likely to report a later bedtime at all time points after 10:00 pm compared to whites (Figure 1). After adjusting for covariates, weekday self-reported time to fall asleep was 15 ± 7 minutes later in African Americans when compared to whites (P = .03; n = 5,184). Similarly, weekend time to fall asleep was 18 ± 7 minutes later in African Americans when compared to whites (P = .03). The proportion of individuals with delayed sleep time was greater in African Americans (33.3%) when compared to whites (18.7%; P < .0001). After adjusting for covariates, when compared to whites, a greater proportion of African Americans had delayed sleep time (adjusted odds ratio [aOR] 2.03; 95% CI 1.6, 2.6; P < .001; Figure 2).
Figure 1. Weekday bedtime.
Percentage of individuals who report a weekday bedtime later than a given hour between 9:00 PM and 4:00 AM. African Americans (blue) were more likely to report a later bedtime at all time points after 10:00 PM (P < .01 for all) compared to non-Hispanic whites (red). No individuals reported a bedtime later than 4:00 AM.
Figure 2. Delayed sleep onset.
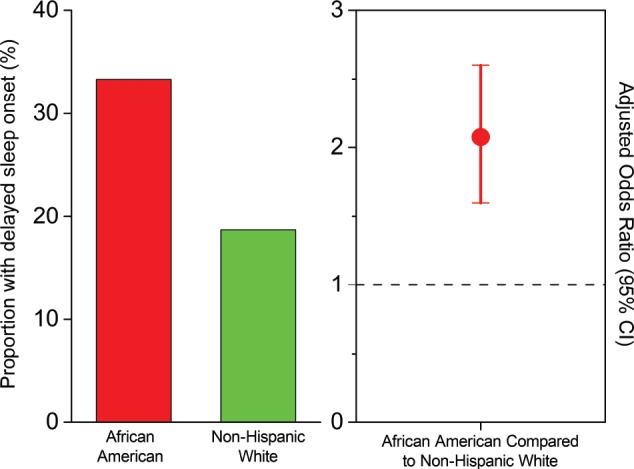
Proportion of individuals with delayed sleep time (sleep time after midnight) are shown for African Americans (red) and non-Hispanic whites (green) in the left panel. In the right panel, the adjusted odds ratio for delayed sleep time in African Americans is shown in comparison to non-Hispanic whites. Note the greater prevalence of delayed sleep time in African Americans.
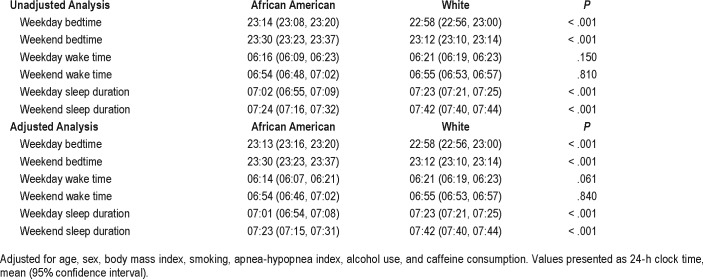
Self-reported time of awakening on weekdays and weekends was not significantly different between African Americans and whites. Weekday wake-up time was 6:14 am for African Americans and 6:21 am for whites (P = .06). Similarly, weekend wake-up time was 6:54 am for African Americans and 6:55 am for whites (P = .84). Weekday sleep duration was shorter by 22 ± 8 minutes in African Americans when compared to whites after adjusting for confounders (P < .001, Table 2). Similarly, the adjusted weekend sleep duration tended to be shorter by 19 ± 8 minutes in African Americans when compared to whites (P = .001). After adjusting for covariates, depression was independently associated with delayed sleep time (aOR 1.3; 95% CI 1.1, 1.7; P = .012).
Table 2.
Sleep timing differences between African Americans and whites.
We found that there was a significant difference in MSF between African Americans and whites in our unadjusted analysis. African Americans had an MSF 10 minutes later than whites (MSF 3:14 am ± 62 minutes compared to MSF 3:04 am ± 83 minutes, P = .006). Adjusted analysis showed similar results, with an African American MSF of 3:13 am (95% CI 3:06, 3:19) compared to a white MSF of 3:04 am (95% CI 3:02, 3:06), P = .01. On evaluation of mid-sleep on free nights corrected for weekend oversleep (MSFsc), a difference was noted between African Americans and whites, but the differences did not reach statistical significance. In the unadjusted analysis, African Americans had an MSFsc of 2:58 am ± 83 minutes compared to a white MSFsc of 2:51 am ± 62 minutes, P = .05. In the adjusted analysis, African Americans had an MSFsc of 2:57 am (95% CI 2:51, 3:03), whereas whites had an MSFsc of 2:51 am (95% CI 2:49, 2:53), P = .08.
Sensitivity analyses confirmed our findings in regard to reported depression. Participants with delayed sleep timing scored 0.14 points worse in their response to the question “in the past 4 weeks have you felt downhearted and blue?” (95% CI 0.04, 0.23, P = .007). We additionally performed logistic regression after excluding participants who reported use of antidepressants. Results were similar to those found during our primary analysis. Subjects with delayed sleep timing were more likely to report depression (aOR 1.60 [95% CI 1.09, 2.36], P = .004; Figure 3).
Figure 3. Relationship between delayed sleep time and depression.
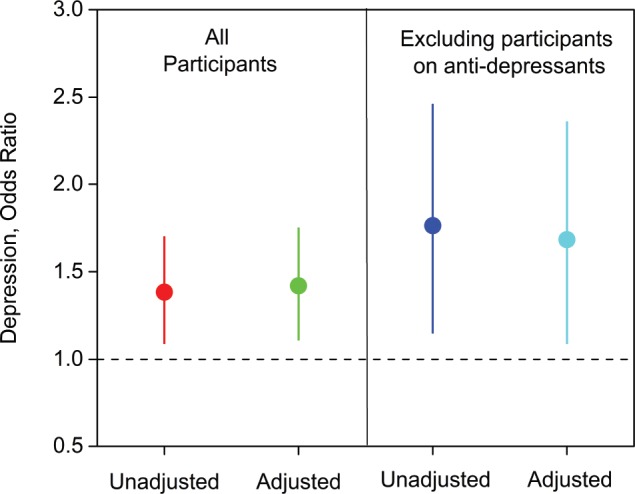
Odds ratios (unadjusted and adjusted) for the relationship between delayed sleep time (sleep time after midnight) and depression are shown for all participants combined (African Americans and non-Hispanic whites; left panel) and after excluding individuals receiving antidepressants (right panel). Individuals without delayed sleep time served as the reference population (dashed horizontal line). Note that the finding of association between delayed sleep time and depression remained after such sensitivity analysis.
We found similar associations for weekend delayed sleep as for weekday delayed sleep. African Americans had an increased odds of delayed sleep time compared to whites. The unadjusted OR was 2.14 (95% CI 1.68, 2.72, P < .001) and the aOR was 2.23 (95% CI 1.75, 2.85, P < .001). Delayed sleep time was again associated with an increased risk of depression. The unadjusted OR was 1.37 (95% CI 1.06, 1.75, P = .014) and the aOR was 1.34 (95% CI 1.04, 1.72, P = .023). Use of a weighted average of weekday and weekend sleep also had similar results. African Americans had an increased odds of delayed sleep time compared to whites. The unadjusted OR was 2.26 (95% CI 1.76, 2.90, P < .001) and the aOR was 2.30 (95% CI 1.78, 2.97, P < .001). Delayed sleep time was again associated with an increased risk of depression. The unadjusted OR was 1.45 (95% CI 1.12, 1.89, P = .005) and the aOR was 1.43 (95% CI 1.10, 1.87, P = .007).
Stratification by sleep duration showed that the association between depression and delayed sleep timing was actually greater in participants who slept 7 hours or more compared to short sleepers. Participants with delayed sleep time were much more likely to report a short sleep duration (aOR 3.75, 95% CI 3.21, 4.37, P < .001). Among participants with adequate sleep duration (72% of total sample), delayed sleep time was associated with an aOR of 1.66 (95% CI 1.23, 2.24, P = .001) for depression. Among participants with short sleep (< 7 hours), delayed sleep time was not associated with increased odds of depression (aOR 1.09, 95% CI 0.74, 1.60, P = .68).
Moderation analysis results showed that there was a signifi-cant interaction between age and race for the likelihood of delayed sleep time (P = .003). The graphical results of moderation analysis are presented in Figure 4 and indicate that although the likelihood of delayed sleep time is relatively stable over age in African Americans, there is an age-associated increased likelihood of delayed sleep time in whites. We did not find a significant interaction between sex and race for the likelihood of delayed sleep time (P = .12). We did not find a significant interaction between delayed sleep time and sex or age for the likelihood of depression (P = .20 and P = .29 respectively). Additionally, although delayed sleep time was more common in African Americans, there was no significant interaction between delayed sleep time and race for the likelihood of depression (P = .14). This suggests that there are no racial differences between African Americans and whites in the association of delayed sleep timing with depression.
Figure 4. Delayed sleep time by age.
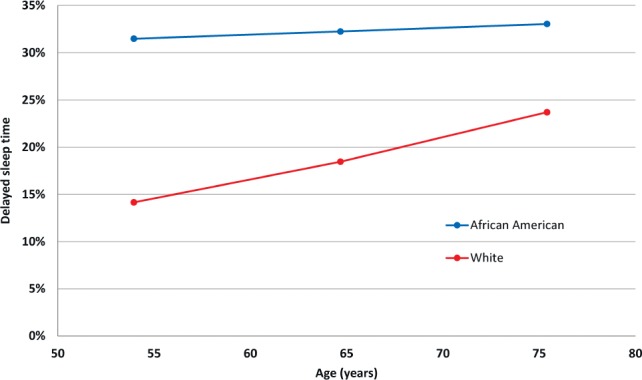
Percentage of individuals with delayed sleep time (sleep time after midnight) are shown for African Americans (blue) and non-Hispanic whites (red) by age. Note that while the likelihood of delayed sleep is time is relative stability over age in African Americans, there is an age-associated increased likelihood of delayed sleep time in whites. Data are presented for mean age and one standard deviation above and below the mean.
Given prior literature showing an association between delayed sleep timing and substance use in younger populations,32,33 we evaluated differences in tobacco, alcohol, and caffeine use in individuals with and without delayed sleep time in this cohort of older adults. Individuals with delayed sleep time had a 15.88 ± 21.55 pack- year history compared to 13.73 ± 24.19 pack-years in individuals without delayed sleep time (P = .009). This was still significant after adjustment for age, sex, and race, 15.19 (95% CI 9.92, 12.52) pack-years compared to 11.22 (95% CI 9.92, 12.52), P = .001. In unad -justed analysis, individuals with delayed sleep time consumed slightly less alcohol compared to those without delayed sleep time, 2.51 ± 5.17 drinks per week compared to 3.05 ± 6.00 drinks per week (P = .009). This was not significant after adjustment for age, sex, and race, 2.32 (95% CI 1.82, 2.81) compared to 2.34 (95% CI 2.00, 2.69) drinks per week, P = .93). Finally, individuals with delayed sleep time consumed slightly less caffeine compared to those without delayed sleep time, 1.59 ± 2.24 cups per day compared to 1.77 ± 2.24 cups per day, P = .023. This was not significant after adjustment for age, sex, and race, 1.42 (95% CI 1.23, 1.61) compared to 1.32 (95% CI 1.20, 1.45) cups per day, P = .411. Please note that the reported differences in delayed sleep time between African Americans and whites as well as the observed association between depression and delayed sleep time in Figure 3 are independent of smoking, alcohol, and caffeine consumption.
DISCUSSION
Sleep and circadian rhythm disorders, including delayed sleep, are associated with poor mental health.4,5,34–39 We found higher rates of delayed sleep time among African-American adults compared to whites in a community-based cohort. The average weekday sleep duration among African Americans was on average 22 minutes shorter than that for whites. Given that weekday bedtime was significantly later in African Americans compared to whites, but there was no difference in weekday wake time, it appears that this disparity in sleep duration is related to delayed sleep timing.
The magnitude of delayed sleep time is worth further discussion. Although the 15- to 19-minute delay in sleep time (on weekdays and weekends, respectively) may seem small, such delays amount to a cumulative 91 to 116 hours over the course of 1 year in the classic epidemiological approach of assessing “cumulative exposure.” Prior studies have shown that a delayed school start intervention in children increased sleep duration of merely 16 to 22 minutes but resulted in improved school performance and decreased daytime sleepiness.40 Moreover, sleep restriction associated with delayed sleep onset of 30 minutes per day over a 5-day period decreased performance on neurocognitive testing, whereas sleep extension of 30 minutes has been shown to improve performance.41 Alternatively, if we examine the data using the proportion of individuals reporting delayed sleep time, after adjusting for confounders, when compared to whites, a greater proportion of African Americans had delayed sleep time (aOR 2.03; 95% CI 1.5, 2.4; P < .0001). Given that African Americans are twice as likely to have delayed sleep timing, if delayed sleep timing is associated with an all-or-none effect, African Americans may be at greater risk for adverse effects associated with delayed sleep timing compared to whites. Furthermore, when we evaluated sleep timing on an hourly basis from 9:00 pm until 4:00 am, we found that African Americans were more likely to report a later bedtime at all time points after 10:00 pm when compared to whites (Figure 2).
Moreover, this is the first community-based study that has found an association between delayed sleep time and depression in older adults (older than 40 years). We found a 40% increased risk of depression being associated with delayed sleep time. Such findings are novel considering that prior research has been limited to adolescents and young adults.42–44 In younger working adults, delayed sleep time has been associated with depressive symptoms.45 We found that participants with delayed sleep time were 3.75 times more likely to report short sleep duration, less than 7 hours. Short sleep duration is well known to be associated with increased risk of depression.39,46,47 However, in our sample, the association between depression and delayed sleep timing was greater in individuals obtaining sufficient sleep. This suggests that short sleep is not mediating the relationship between delayed sleep time and depression, and supports our hypothesis that delayed sleep time is independently associated with increased risk of depression. These disparities in the prevalence of delayed sleep time among African Americans carry profound implications for mental health in at-risk populations in the United States.48
Malone et al. have reported a prior study derived from the United Kingdom Biobank cohort compared differences in morning-evening type sleep preference and sleep duration in Black participants compared to white participants and found that black participants reported more morning preference when compared to white participants.19 A subsequent study with detailed propensity score matching for other confounding social and environmental characteristics confirmed this finding of morning preference and short sleep duration in black participants compared to white participants.49 Similar to our findings, black participants in this cohort were more likely to report short sleep duration. However, although circadian preference was assessed, actual sleep timing was not assessed. Given that social constraints such as child care and job schedule may affect sleep timing, it is possible that African Americans may have a morning circadian preference, but choose a delayed bedtime as a consequence of these social constraints. Murray and colleagues noted that 43% of individuals in their study had “noncircadian” delayed sleep phase disorder.50 Such individuals had typical phase angles between dim light melatonin onset (DLMO) and bedtime, and thus were not experiencing circadian misalignment as typically defined. Eastman and colleagues found a shorter tau in African Americans than whites, and such a finding would be consistent with an earlier circadian phase and sleep timing.16 Considering such information, the phase angle between DLMO (which occurs earlier in African Americans) and delayed sleep time is much larger and may conceivably impose greater adverse effects of phase dyssynchrony. Notably, the tendency toward having a delayed sleep time may be transgenerational, with Hasler and colleagues reporting later bedtimes in African American than white participants in an adolescent sample, suggesting that the tendency toward delayed sleep timing may begin early in life.33
Differences in sleep timing among the African diaspora suggests that racial/ethnic differences in sleep may be contributing to disparities in depression and other health outcomes.16,18,51 Such findings need to be further explored to uncover the underlying factors responsible for these disparities in sleep timing and depression. Contributing biological, environmental, psychosocial, and cultural factors52 must be identified in order to design interventions that can improve the diagnosis, prevention, and treatment of depression in at-risk populations where these disparities exist.7,18,53,54 Additionally, future studies should investigate particular circadian and gene environment interactions that may be driving the effect of sleep timing on disparities in depression, obesity, heart disease, and cancer in African Americans.4–6
There are limitations to our study. We defined depression as reported use of antidepressants, or self-reported depressed mood based on a single question. Use of a validated depression screening questionnaire such as the Beck Depression inventory would be preferable.55 However, given the paucity of cohort studies with sleep data available, this single question approach has been used previously.56 Moreover, we believe that our findings have value considering that the relationship between delayed sleep time and race in the context of depression measured in the same cohort has not been previously reported in a large community-based population. Additionally, although we provide information on midsleep differences, information on use of alarm clocks to wake up in the morning was not collected as a part of the SHHS. Given that alarm clock use advances calculated midsleep timing by leading to an earlier wake time than circadian preference would predict, midsleep timing results in this cohort may not be an accurate reflection of true midsleep timing. Finally, although we showed that delayed sleep time is more common in African Americans, and delayed sleep time is associated with depression; we did not find any differences in the relationship between delayed sleep time and depression between African Americans and whites. This may be because there are no such differences, but may alternately be due to sample size limitations. The SHHS was not designed to study ethnicity-related sleep disparities or depression. More specifically, the SHHS depended on race/ethnicity distribution in the community-based population and population-level prevalence of depression, leading to fewer individuals who are African American and suffer from depression. Future studies that enrich their cohorts with enrichment of both African Americans and individuals with depression are needed. Further, there is an important distinction between race as a primary factor versus a marker of interest within the context of sociocultural, environmental, and other factors that were not measured in our archival study. Therefore, we caution the reader to interpret our findings within the context of such considerations. We would like to note that although the mechanistic aspects for the reasons for delayed sleep time (sociocultural versus genetic, etc.) may be uncertain, the SHHS is a large, community-based, multicenter, observational epidemiological cohort that is representative of the population and hence has generalizable findings that are of value when considered within the context of the aforementioned limitations.
CONCLUSIONS
Our results show that race is associated with delayed sleep time in a large, community-based cohort of adults. African Americans were more likely to experience delayed sleep time and short sleep duration when compared to whites. Additionally, we found that delayed sleep time was independently associated with depression. These findings required further investigation of the underlying biological and psychosocial factors responsible for this disparity in sleep timing and the association with depression.
DISCLOSURE STATEMENT
All authors have seen and approved this manuscript. The study was funded by the National Institutes of Health (National Heart, Lung, and Blood Institute [NHLBI]). The sponsor was involved in oversight of human subject safety through an independent Data Safety Monitoring Board (DSMB), and had nonvoting representation in the steering committee that approved this manuscript submission. This work was supported by National Heart, Lung, and Blood Institute cooperative agreements U01HL53940 (University of Washington), U01HL53941 (Boston University), U01HL53938 (University of Arizona), U01HL53916 (University of California, Davis), U01HL53934 (University of Minnesota), U01HL53931 (New York University), U01HL53937 and U01HL64360 (Johns Hopkins University), U01HL63463 (Case Western Reserve University), U01HL63429 (Missouri Breaks Research). This work was also supported by the National Institutes of Health Grants (HL138377 and HL126140 to S.P). Patient-Centered Outcomes Research Institute contract (IHS-1306-2505; EAIN 3394-UOA; and PPRND-1507-31666 to S.P); the American Sleep Medicine Foundation (ASMF 150-JF-16 to D.C.) and a University of Arizona Health Sciences Career Development Award to D.C. The statements in this manuscript are solely the responsibility of the author and do not necessarily represent the views of PCORI, its Board of Governors or Methodology Committee. Conflicts of Interest: Dr. Parthasarathy reports grants from ASMF (169-SR-17), NIH/NHLBI (HL13877), grants from Patient Centered Outcomes Research Institute (IHS-1306-2505, EAIN #3394-UoA, PPRND-1507-31666), grants from US Department of Defense, grants from NIH/NCI (1R21CA184920), grants from Johrei Institute, personal fees from American Academy of Sleep Medicine, personal fees from UpToDate Inc., grants from Younes Sleep Technologies, Ltd., grants from Niveus Medical Inc., personal fees from Vapotherm, Inc., personal fees from Merck, Inc., grants from Philips Respironics, Inc., personal fees from Philips Respironics, Inc., personal fees from Bayer, Inc. outside the submitted work; In addition, Dr. Parthasarathy has a patent UA 14-018 U.S.S.N. 61/884,654; PTAS 502570970 (Home breathing device) issued. Dr. Quan reports grant support from the NIA (AG009975), NHLBI (HL117995), NIDDK (DK110528), consults for Jazz Pharmaceuticals and Best Doctors, and receives a stipend from the American Academy of Sleep Medicine. The remaining authors do not have any conflicts of interest to disclose.
ACKNOWLEDGMENTS
The authors are indebted to the Sleep Heart Health Study (SHHS) participants who contributed their time to this study. The authors are grateful for diligent work performed by the technical staff at the clinical sites for collecting the data. The authors are thankful to the reading center for analyzing and coding the sleep studies. DC, SQ and SP had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. SHHS acknowledges the Atherosclerosis Risk in Communities Study, the Cardiovascular Health Study, the Framingham Heart Study, the Cornell/Mt. Sinai Worksite and Hypertension Studies, the Strong Heart Study, the Tucson Epidemiologic Study of Airways Obstructive Diseases (TESAOD), and the Tucson Health and Environment Study for allowing their cohort members to be part of the SHHS and for sharing such data for the purposes of this study. SHHS is particularly grateful to the members of these cohorts who agreed to participate in SHHS as well. SHHS further recognizes all the investigators and staff who have contributed to its success. A list of SHHS investigators, staff, and their participating institutions is available on the SHHS website (www.jhsph.edu/shhs).
ABBREVIATIONS
- aOR
adjusted odds ratio
- BMI
body mass index
- MSF
midsleep on free days
- MSFsc
midsleep on free nights corrected for weekend oversleep
- SHHS
Sleep Heart Health Study
REFERENCES
- 1.Marodi L. [Nobel Prize for the discoveries of genetic mechanisms controlling the circadian rythm] Orv Hetil. 2018;159(6):239. doi: 10.1556/650.2018.HO2590. [DOI] [PubMed] [Google Scholar]
- 2.Friborg O, Bjorvatn B, Amponsah B, Pallesen S. Associations between seasonal variations in day length (photoperiod), sleep timing, sleep quality and mood: a comparison between Ghana (5 degrees) and Norway (69 degrees) J Sleep Res. 2012;21(2):176–184. doi: 10.1111/j.1365-2869.2011.00982.x. [DOI] [PubMed] [Google Scholar]
- 3.Grandner MA, Hale L, Moore M, Patel NP. Mortality associated with short sleep duration: the evidence, the possible mechanisms, and the future. Sleep Med Rev. 2010;14(3):191–203. doi: 10.1016/j.smrv.2009.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wong PM, Hasler BP, Kamarck TW, Muldoon MF, Manuck SB. Social jetlag, chronotype, and cardiometabolic risk. J Clin Endocrinol Metab. 2015;100(12):4612–4620. doi: 10.1210/jc.2015-2923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ford DE, Kamerow DB. Epidemiologic study of sleep disturbances and psychiatric disorders. An opportunity for prevention? JAMA. 1989;262(11):1479–1484. doi: 10.1001/jama.262.11.1479. [DOI] [PubMed] [Google Scholar]
- 6.Van Laake LW, Lüscher TF, Young ME. The circadian clock in cardiovascular regulation and disease: lessons from the Nobel Prize in Physiology or Medicine 2017. Eur Heart J. 2018;39(24):2326–2329. doi: 10.1093/eurheartj/ehx775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Adenekan B, Pandey A, McKenzie S, Zizi F, Casimir GJ, Jean-Louis G. Sleep in America: role of racial/ethnic differences. Sleep Med Rev. 2013;17(4):255–262. doi: 10.1016/j.smrv.2012.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Singh GK, Daus GP, Allender M, et al. Social determinants of health in the United States: addressing major health inequality trends for the nation, 1935-2016. Int J MCH AIDS. 2017;6(2):139–164. doi: 10.21106/ijma.236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Polednak AP. Racial differences in mortality from obesity-related chronic diseases in US women diagnosed with breast cancer. Ethn Dis. 2004;14(4):463–468. [PubMed] [Google Scholar]
- 10.Fernandez-Mendoza J, He F, LaGrotte C, Vgontzas AN, Liao D, Bixler EO. Impact of the metabolic syndrome on mortality is modified by objective short sleep duration. J Am Heart Assoc. 2017;6(5):e005479. doi: 10.1161/JAHA.117.005479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fernandez-Mendoza J, He F, Vgontzas AN, Liao D, Bixler EO. Objective short sleep duration modifies the relationship between hypertension and all-cause mortality. J Hypertens. 2017;35(4):830–836. doi: 10.1097/HJH.0000000000001253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Heslop P, Smith GD, Metcalfe C, Macleod J, Hart C. Sleep duration and mortality: The effect of short or long sleep duration on cardiovascular and all-cause mortality in working men and women. Sleep Med. 2002;3(4):305–314. doi: 10.1016/s1389-9457(02)00016-3. [DOI] [PubMed] [Google Scholar]
- 13.Gottlieb DJ, Punjabi NM, Newman AB, et al. Association of sleep time with diabetes mellitus and impaired glucose tolerance. Arch Intern Med. 2005;165(8):863–867. doi: 10.1001/archinte.165.8.863. [DOI] [PubMed] [Google Scholar]
- 14.Etain B, Dumaine A, Bellivier F, et al. Genetic and functional abnormalities of the melatonin biosynthesis pathway in patients with bipolar disorder. Hum Mol Genet. 2012;21(18):4030–4037. doi: 10.1093/hmg/dds227. [DOI] [PubMed] [Google Scholar]
- 15.Li JZ, Bunney BG, Meng F, et al. Circadian patterns of gene expression in the human brain and disruption in major depressive disorder. Proc Natl Acad Sci U S A. 2013;110(24):9950–9955. doi: 10.1073/pnas.1305814110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Eastman CI, Suh C, Tomaka VA, Crowley SJ. Circadian rhythm phase shifts and endogenous free-running circadian period differ between African-Americans and European-Americans. Sci Rep. 2015;5:8381. doi: 10.1038/srep08381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Paech GM, Crowley SJ, Eastman CI. Sleep and cognitive performance of African-Americans and European-Americans before and during circadian misalignment produced by an abrupt 9-h delay in the sleep/wake schedule. PLoS One. 2017;12(10):e0186843. doi: 10.1371/journal.pone.0186843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Grandner MA, Williams NJ, Knutson KL, Roberts D, Jean-Louis G. Sleep disparity, race/ethnicity, and socioeconomic position. Sleep Med. 2016;18:7–18. doi: 10.1016/j.sleep.2015.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Malone SK, Patterson F, Lu Y, Lozano A, Hanlon A. Ethnic differences in sleep duration and morning-evening type in a population sample. Chronobiol Int. 2016;33(1):10–21. doi: 10.3109/07420528.2015.1107729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fried LP, Borhani NO, Enright P, et al. The Cardiovascular Health Study: design and rationale. Ann Epidemiol. 1991;1(3):263–276. doi: 10.1016/1047-2797(91)90005-w. [DOI] [PubMed] [Google Scholar]
- 21.Dawber TR, Kannel WB, Lyell LP. An approach to longitudinal studies in a community: the Framingham Study. Ann N Y Acad Sci. 1963;107:539–556. doi: 10.1111/j.1749-6632.1963.tb13299.x. [DOI] [PubMed] [Google Scholar]
- 22.Petit E, Milano G, Lévi F, Thyss A, Bailleul F, Schneider M. Circadian rhythm-varying plasma concentration of 5-fluorouracil during a five-day continuous venous infusion at a constant rate in cancer patients. Cancer Res. 1988;48(6):1676–1679. [PubMed] [Google Scholar]
- 23.Lebowitz MD, Knudson RJ, Burrows B. Tucson epidemiologic study of obstructive lung diseases. I: Methodology and prevalence of disease. Am J Epidemiol. 1975;102(2):137–152. doi: 10.1093/oxfordjournals.aje.a112141. [DOI] [PubMed] [Google Scholar]
- 24.Rhoades DA, Welty TK, Wang W, et al. Aging and the prevalence of cardiovascular disease risk factors in older American Indians: the Strong Heart Study. J Am Geriatr Soc. 2007;55(1):87–94. doi: 10.1111/j.1532-5415.2006.01018.x. [DOI] [PubMed] [Google Scholar]
- 25.The Atherosclerosis Risk in Communities (ARIC) Study: design and objectives. The ARIC investigators. Am J Epidemiol. 1989;129(4):687–702. [PubMed] [Google Scholar]
- 26.Wideman L, Calkins SD, Janssen JA, et al. Rationale, design and methods for the RIGHT Track Health Study: pathways from childhood self-regulation to cardiovascular risk in adolescence. BMC Public Health. 2016;16:459. doi: 10.1186/s12889-016-3133-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Quan SF, Howard BV, Iber C, et al. The Sleep Heart Health Study: design, rationale, and methods. Sleep. 1997;20(12):1077–1085. [PubMed] [Google Scholar]
- 28.Hayes AF, Rockwood NJ. Regression-based statistical mediation and moderation analysis in clinical research: observations, recommendations, and implementation. Behav Res Ther. 2017;98:39–57. doi: 10.1016/j.brat.2016.11.001. [DOI] [PubMed] [Google Scholar]
- 29.Watson NF, Badr MS, Belenky G, et al. Recommended amount of sleep for a healthy adult: a joint consensus statement of the American Academy of Sleep Medicine and Sleep Research Society. Sleep. 2015;38(6):843–844. doi: 10.5665/sleep.4716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dunn EC, Sofer T, Wang MJ, et al. Genome-wide association study of depressive symptoms in the Hispanic Community Health Study/Study of Latinos. J Psychiatr Res. 2018;99:167–176. doi: 10.1016/j.jpsychires.2017.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Roenneberg T, Wirz-Justice A, Merrow M. Life between clocks: daily temporal patterns of human chronotypes. J Biol Rhythms. 2003;18(1):80–90. doi: 10.1177/0748730402239679. [DOI] [PubMed] [Google Scholar]
- 32.Hasler BP, Clark DB. Circadian misalignment, reward-related brain function, and adolescent alcohol involvement. Alcohol Clin Exp Res. 2013;37(4):558–565. doi: 10.1111/acer.12003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hasler BP, Franzen PL, de Zambotti M, et al. Eveningness and later sleep timing are associated with greater risk for alcohol and marijuana use in adolescence: initial findings from the National Consortium on Alcohol and Neurodevelopment in Adolescence study. Alcohol Clin Exp Res. 2017;41(6):1154–1165. doi: 10.1111/acer.13401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Haus EL, Smolensky MH. Shift work and cancer risk: potential mechanistic roles of circadian disruption, light at night, and sleep deprivation. Sleep Med Rev. 2013;17(4):273–284. doi: 10.1016/j.smrv.2012.08.003. [DOI] [PubMed] [Google Scholar]
- 35.Cole HV, Owusu-Dabo E, Iwelunmor J, et al. Sleep duration is associated with increased risk for cardiovascular outcomes: a pilot study in a sample of community dwelling adults in Ghana. Sleep Med. 2017;34:118–125. doi: 10.1016/j.sleep.2017.03.008. [DOI] [PubMed] [Google Scholar]
- 36.Combs D, Goodwin JL, Quan SF, Morgan WJ, Shetty S, Parthasarathy S. Insomnia, health-related quality of life and health outcomes in children: a seven year longitudinal cohort. Sci Rep. 2016;6:27921. doi: 10.1038/srep27921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Quan SF, Combs D, Parthasarathy S. Impact of sleep duration and weekend oversleep on body weight and blood pressure in adolescents. Southwest J Pulm Crit Care. 2018;16(1):31–41. doi: 10.13175/swjpcc150-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Seixas AA, Nunes JV, Airhihenbuwa CO, et al. Linking emotional distress to unhealthy sleep duration: analysis of the 2009 National Health Interview Survey. Neuropsychiatr Dis Treat. 2015;11:2425–2430. doi: 10.2147/NDT.S77909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lippman S, Gardener H, Rundek T, et al. Short sleep is associated with more depressive symptoms in a multi-ethnic cohort of older adults. Sleep Med. 2017;40:58–62. doi: 10.1016/j.sleep.2017.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Li S, Arguelles L, Jiang F, et al. Sleep, school performance, and a school-based intervention among school-aged children: a sleep series study in China. PloS One. 2013;8(7):e67928. doi: 10.1371/journal.pone.0067928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sadeh A, Gruber R, Raviv A. The effects of sleep restriction and extension on school-age children: what a difference an hour makes. Child Dev. 2003;74(2):444–455. doi: 10.1111/1467-8624.7402008. [DOI] [PubMed] [Google Scholar]
- 42.Saxvig IW, Pallesen S, Wilhelmsen-Langeland A, Molde H, Bjorvatn B. Prevalence and correlates of delayed sleep phase in high school students. Sleep Med. 2012;13(2):193–199. doi: 10.1016/j.sleep.2011.10.024. [DOI] [PubMed] [Google Scholar]
- 43.Asaoka S, Komada Y, Aritake S, Morita Y, Fukuda K, Inoue Y. Effect of delayed sleep phase during university life on the daytime functioning in work life after graduation. Sleep Med. 2014;15(9):1155–1158. doi: 10.1016/j.sleep.2014.05.017. [DOI] [PubMed] [Google Scholar]
- 44.Combs D, Goodwin JL, Quan SF, Morgan WJ, Parthasarathy S. Longitudinal differences in sleep duration in Hispanic and Caucasian children. Sleep Med. 2016;18:61–66. doi: 10.1016/j.sleep.2015.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sakamoto N, Nanri A, Kochi T, et al. Bedtime and sleep duration in relation to depressive symptoms among Japanese workers. J Occup Health. 2013;55(6):479–486. doi: 10.1539/joh.13-0074-oa. [DOI] [PubMed] [Google Scholar]
- 46.Alcantara C, Biggs ML, Davidson KW, et al. Sleep disturbances and depression in the Multi-Ethnic Study of Atherosclerosis. Sleep. 2016;39(4):915–925. doi: 10.5665/sleep.5654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Stamatakis KA, Kaplan GA, Roberts RE. Short sleep duration across income, education, and race/ethnic groups: population prevalence and growing disparities during 34 years of follow-up. Ann Epidemiol. 2007;17(12):948–955. doi: 10.1016/j.annepidem.2007.07.096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Moussavi S, Chatterji S, Verdes E, Tandon A, Patel V, Ustun B. Depression, chronic diseases, and decrements in health: results from the World Health Surveys. Lancet. 2007;370(9590):851–858. doi: 10.1016/S0140-6736(07)61415-9. [DOI] [PubMed] [Google Scholar]
- 49.Malone SK, Patterson F, Lozano A, Hanlon A. Differences in morning-evening type and sleep duration between Black and White adults: results from a propensity-matched UK Biobank sample. Chronobiol Int. 2017;34(6):740–752. doi: 10.1080/07420528.2017.1317639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Murray JM, Sletten TL, Magee M, et al. Prevalence of circadian misalignment and its association with depressive symptoms in delayed sleep phase disorder. Sleep. 2017;40(1) doi: 10.1093/sleep/zsw002. [DOI] [PubMed] [Google Scholar]
- 51.Seixas AA, Auguste E, Butler M, et al. Differences in short and long sleep durations between blacks and whites attributed to emotional distress: analysis of the National Health Interview Survey in the United States. Sleep Health. 2017;3(1):28–34. doi: 10.1016/j.sleh.2016.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Williams NJ, Grandner MA, Wallace DM, et al. Social and behavioral predictors of insufficient sleep among African Americans and Caucasians. Sleep Med. 2016;18:103–107. doi: 10.1016/j.sleep.2015.02.533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hill TD, Trinh HN, Wen M, Hale L. Perceived neighborhood safety and sleep quality: a global analysis of six countries. Sleep Med. 2016;18:56–60. doi: 10.1016/j.sleep.2014.12.003. [DOI] [PubMed] [Google Scholar]
- 54.Fung CH, Veasey SC. Research priorities in the area of sleep/circadian rhythm and aging research: commentary on “Report and Research Agenda of the American Geriatrics Society and National Institute on Aging Bedside-to-Bench Conference on Sleep, Circadian Rhythms, and Aging: New Avenues for Improving Brain Health, Physical Health, and Functioning”. Sleep. 2017;40(5) doi: 10.1093/sleep/zsx065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Beck AT, Steer RA, Ball R, Ranieri W. Comparison of Beck Depression Inventories -IA and -II in psychiatric outpatients. J Pers Assess. 1996;67(3):588–597. doi: 10.1207/s15327752jpa6703_13. [DOI] [PubMed] [Google Scholar]
- 56.Parthasarathy S, Vasquez MM, Halonen M, et al. Persistent insomnia is associated with mortality risk. Am J Med. 2015;128(3):268.e2–275.e2. doi: 10.1016/j.amjmed.2014.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]