Abstract
Study Objectives:
To examine the risk of hospitalization for motor vehicle accident injury (MVAI) in patients with narcolepsy and the effects of stimulant use on MVAI occurrence in patients with narcolepsy.
Methods:
This is a population-based, retrospective cohort study using Taiwan's National Health Insurance Research Database between 2000 and 2013. We included patients with narcolepsy based on the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes, 347. The case and matched control participants were selected in a ratio of 1:3, and the traffic accident (ICD-9-CM codes: E810–E819) plus injury codes (ICD-9-CM codes: 800.xx–999.xx) due to MVAI following hospitalization were used for the study outcome. The type of injury, causes, intentionality, and the effects of stimulant use on patients with narcolepsy were also assessed.
Results:
A total of 1,316 participants were enrolled, including 329 participants with narcolepsy and 987 participants without narcolepsy. During a 14-year follow-up period, a total of 104 participants had MVAI, of whom 47 (1,559.54 per 100,000 person-years) belonged to the narcolepsy cohort and 57 (556.21 per 100,000 person-years) to the non-narcolepsy cohort. After adjusting for covariates, the risk of hospitalization for MVAI among participants with narcolepsy was still significantly higher than those without narcolepsy (adjusted hazard ratio = 6.725; 95% confidence interval = 4.421–10.231; P < .001). The use of modafinil or methylphenidate, as monotherapy or combined treatment, was associated with a lower risk of MVAI in the narcolepsy cohort.
Conclusions:
Patients with narcolepsy may have a higher risk of hospitalization for MVAI and stimulant use could mitigate such risk.
Citation:
Tzeng NS, Hsing SC, Chung CH, Chang HA, Kao YC, Mao WC, Yang CC, Kuo TB, Chen TY, Chien WC. The risk of hospitalization for motor vehicle accident injury in narcolepsy and the benefits of stimulant use: a nationwide cohort study in Taiwan. J Clin Sleep Med. 2019;15(6):881–889.
Keywords: methylphenidate, modafinil, motor vehicle accident injury, narcolepsy
BRIEF SUMMARY
Current Knowledge/Study Rationale: Narcolepsy is characterized by irresistible daytime sleepiness, and previous studies have demonstrated an association between narcolepsy and motor vehicle accident injury (MVAI). However, direct evidence of the risk of hospitalization for MVAI in narcolepsy is limited for the Asian population. We used a population-based, retrospective cohort study to examine this issue.
Study Impact: The current study demonstrates that patients with narcolepsy had an approximately 6.7-fold increased risk of hospitalization for MVAI when compared to those without narcolepsy. In addition, the use of modafinil or methylphenidate was associated with a lower risk of hospitalization for MVAI in the narcolepsy cohort, either as monotherapy or as combined treatment. Our findings could bring some insights for the regulations of traffic safety.
INTRODUCTION
Motor vehicle accident injury (MVAI) is a major global public health problem and has accounted for mortality, morbidity, and economic loss.1–4 Sleep disorders that result in daytime symptoms have been associated with MVAI in previous research.5–8 One study found that drowsiness increased the risk of near-miss accidents,9 and another showed that drivers with sleep-related near-misses are at an increased risk for MVAI.7
Narcolepsy is characterized by irresistible daytime sleepiness, as well as a sudden loss of muscle tone (cataplexy), sleep-onset or sleep-offset paralysis, and hallucinations.10–12 Previous studies have shown that narcolepsy can be related to MVAI,13,14 and one study showed that patients with sleep apnea and narcolepsy accounted for 71% of all sleep-related automobile accidents.15
The excessive daytime sleepiness of narcolepsy is treated using stimulants such as modafinil and methylphenidate.16–19 Because sleepiness is a significant issue in sleep-related MVAI, it is important to investigate whether patients with narcolepsy can benefit from the use of stimulants in MVAI. Therefore, we used a nationwide population-based registry dataset to investigate the association between narcolepsy and MVAI and the effect that the use of stimulants had on the occurrence of MVAI in patients with narcolepsy.
METHODS
Data Source
The National Health Insurance (NHI) Program was launched in Taiwan in 1995, and as of June 2009, included contracts with 97% of the medical providers with approximately 23 million beneficiaries, or more than 99% of the entire population.20,21 The National Health Insurance Research Database (NHIRD), which contains all the claims data of the beneficiaries, uses the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes to record the diagnoses.22 The details of the program have been documented in previous studies.23–27
The association between participants with narcolepsy and the risk of MVAI was studied using a subset of the NHIRD, the Longitudinal Health Insurance Database, which consists of one million randomly sampled individuals between 2000 and 2013. The Institutional Review Board of the Tri-Service General Hospital approved this study and waived the need for individual written informed consent (IRB No. 1-106-05-169).
Study Design and Sampled Participants
To undertake this population-based, retrospective cohort study,28 we included participants aged 20 years or older with a diagnosis of narcolepsy, based on the ICD-9-CM code, 347, from January 1, 2000 to December 31, 2013. Each enrolled participant in this study was required to have visited an outpatient clinic at least three times within 1 year of the study duration with the diagnosis code of 347. The exclusion criteria are described as follows: (1) individuals in whom narcolepsy was diagnosed before the cohort entry date, (2) patients who had MVAI-related hospitalization before the cohort entry date, (3) individuals in whom attention deficit hyperactivity disorder had been diagnosed, (4) patients with drug dependence/abuse, (5) individuals younger than 20 years at the cohort entry date, and (6) missing data. The cohort entry date was defined as that of the third diagnosis of narcolepsy within 1 year. Participants were followed until hospitalization for MVAI, withdrawal from the NHI program, or the end of the study. Patients with narcolepsy and the control participants were selected at a 1:3 ratio by the estimated propensity score matching by sex, age, and index year.
Data on the use of modafinil and methylphenidate were collected. The data on the defined daily dosage were obtained from the World Health Organization Collaborating Centre for Drug Statistics Methodology (https://www.whocc.no/), and thus, the estimated proportion of days covered (PDC) recorded as 1% to 50% and 51% to 100% in the 14 years of follow-up.
Major Outcome Measure
The study outcome was hospitalization for MVAI, including the traffic accident (ICD-9-CM codes: E810–E819) plus injury codes (ICD-9-CM codes: 800.xx–999.xx). Evaluation of the severity of the injury was performed using the Injury Severity Score (ISS), and the cutoff point for major trauma defined as scoring ≥ 16.29 The type of injury, causes, intentionality, and the effects of stimulant use on patients with narcolepsy were also assessed. The ICD-9-CM codes are shown in Table S1 in the supplemental material.
Potential Confounders
The covariates included sex; age groups (20–44, 45–64, and ≥ 65 years); monthly income (in New Taiwan Dollars [NT$]; < 18,000, 18,000–34,999, ≥ 35,000); geographical area of residence (Northern, Central, Southern, Eastern Taiwan, and the outer islands); urbanization level of residence (levels 1 to 4); and level of care (medical center, regional, and local hospital). The urbanization level of residence was defined according to the population and various indicators of the level of development. Level 1 was defined as a population of > 1,250,000 and had a specific designation of political, economic, cultural, and metropolitan development. Level 2 was defined as a population between 500,000 and 1,249,999, and as playing an important role in politics, economy, and culture. Urbanization levels 3 and 4 were defined as a population between 149,999 and 499,999, and < 149,999, respectively.30
Comorbidities were assessed using the Charlson Comorbidity Index (CCI), which categorizes the comorbidities using the ICD-9-CM codes, scores each comorbidity category,31–33 and combines all the scores to calculate a single comorbidity score. A score of zero indicates no comorbidities, and higher scores indicate higher comorbidity burdens.21 This study also assessed psychiatric disorders such as anxiety (ICD-9-CM codes 300.X), depressive disorder (ICD-9-CM codes 296.2, 296.3, 300.4, and 311), and the use of antidepressants and benzodiazepine receptor agonists (BZRAs) as covariates. Figure 1 presents a detailed flowchart regarding the participant selection and the study design.
Figure 1. Flowchart regarding the participant selection and the study design.
Statistical Analysis
All statistical analyses were performed using SPSS for Windows, version 22.0 (IBM Corp., Armonk, New York, United States). We used χ2 and t tests to evaluate the distributions of the categorical and continuous variables, respectively, with a Fisher exact test. The multivariate Cox proportional hazards regression analysis was used to determine the risk of hospitalization for MVAI, and the results presented as a hazard ratio (HR) with a 95% CI. HR differs from relative risk (RR), in that RR is cumulative over the entire study, whereas HR makes time implicit and as such, uses data only from when the patient was observed and provides instantaneous risk over the study period. We adjusted for the following potential confounders: sex, age, monthly income, anxiety, depressive disorders, and the usage of antidepressants and BZRAs, CCI scores, urbanization level of the residence, and level of care. According to the multicollinearity between the geographical area and urbanization level of the residence, we chose the urbanization level of the residence for adjustment. The difference in the risk of hospitalization for MVAI, between the study and control groups, was estimated using the Kaplan-Meier method with the log-rank test. A two-tailed value of P < .05 indicated statistical significance.
RESULTS
In this study, we enrolled 1,316 participants comprising 329 participants with narcolepsy and 987 participants as the control group. The minimum follow-up duration was 0.01 year and the maximum follow-up period is 13.98 years. (Table S2 in the supplemental material) Table 1 shows the sex, age, monthly insurance premiums, comorbidities, the area of residence, urbanization, and level of care of the patients with narcolepsy and the control participants. When compared to the control patients, the patients with narcolepsy tended to have lower CCI scores, but a higher proportion of anxiety, depressive disorders, and use of antidepressants; they also had a higher ratio of living in urbanization levels 1 or 2, as well as in Northern Taiwan. The Kaplan-Meier analysis showed that the narcolepsy cohort had a significantly higher risk of MVAI (log-rank test < 0.001, Figure 2).
Table 1.
Characteristics of study at the baseline.

Figure 2. Kaplan-Meier for cumulative risk of motor vehicle accident injury among patients with narcolepsy with a log-rank test.

Table 2 shows the Cox regression analysis of factors associated with the risk of hospitalization for MVAI. The crude HR for patients with narcolepsy and hospitalization for MVAI was 6.282 (95% CI 4.198–9.399, P < .001). After adjusting for sex, age, monthly income, anxiety, depressive disorders, the use of antidepressants and BZRAs, CCI scores, urbanization level of the residence, and level of care, the adjusted hazard ratio (aHR) was 6.725 (95% CI 4.421–10.231, P < .001).
Table 2.
Cox regression analysis of factors contributing to MVAI.
Table 3 presents the Cox regression analysis of MVAI type and severity. Overall, after the follow-up period of 14 years, a total of 104 participants had MVAI, with 47 (1,559.54 per 100,000 person-years) from the narcolepsy cohort and 57 (556.21 per 100,000 person-years) from the non-narcolepsy cohort. In assessing the type of injury, patients with narcolepsy had a higher risk of fracture (aHR 1.969, 95% CI 1.294–2.995) and a lower risk of intracranial/internal injury (aHR 0.583, 95% CI 0.383–0.886) than the control group. In addition, patients with narcolepsy were at increased risk of higher scores of ISS, when compared to participants without narcolepsy.
Table 3.
Cox regression analysis of MVAI type and severity.
Table 4 shows that participants with narcolepsy were more likely to be the drivers/riders of motor vehicles, motorcycles, pedal cycles, and other forms of transport when compared to the control group, with an aHR of 40.779, 6.253, 4.078, and 5.580, respectively (all P < .001). However, narcolepsy was not associated with an increased risk of MVAI when the participants were passengers or pedestrians.
Table 4.
Cox regression of vehicle type of MVAI.
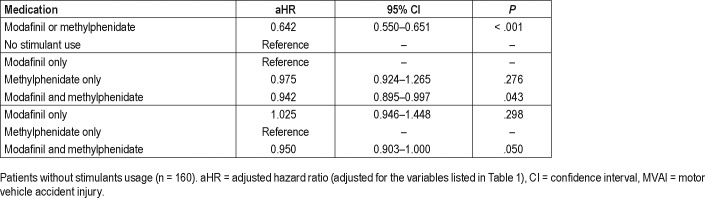
Table 5 presents the effects of stimulant use on the patients with narcolepsy hospitalized for MVAI. The results were consistent whether we investigated the patients with narcolepsy who used modafinil only, methylphenidate only, or a combination of modafinil and methylphenidate. The use of either monotherapy or a combination of modafinil and methylpheni-date was associated with decreased risk of hospitalization for MVAI in patients with narcolepsy. In addition, with either PDC 1% to 50%, or PDC 51% to 100%, the use of these two stimulants was associated with a decreased risk of hospitalization for MVAI in the patients with narcolepsy. Furthermore, a longer PDC of stimulant prescription appeared to reduce risk further, which suggests a dose-response relationship between stimulant use and risk reduction. Finally, patients with narcolepsy using stimulants also saw the benefit of reduced severity scores of MVAI, when compared to the group that did not use stimulants.
Table 5.
Effects of stimulant use on the ISS scores of MVAI in patients with narcolepsy.
Table 6 shows the effects of stimulant use on MVAI in patients with narcolepsy. The use of modafinil or methylpheni-date in patients with narcolepsy reduced MVAI by 35.8%. The use of both modafinil and methylphenidate together reduced MVAI more than modafinil or methylphenidate alone (aHR 0.942, 95% CI 0.895–0.997).
Table 6.
Effects of stimulant use on MVAI in patients with narcolepsy.
DISCUSSION
Using a population-based, retrospective cohort study designed with large sample size and 14-year follow-up duration, the current study demonstrates that patients with narcolepsy had approximately a 6.7-fold risk of hospitalization for MVAI when compared with the control participants. Furthermore, patients with narcolepsy who received modafinil and methylphenidate, either as monotherapy or combination therapy, had a decreased risk of hospitalization for MVAI.
The relationship between sleep disorders and automobile accidents is an important issue, and our findings are consistent with those of several previous studies.13–15,34,35 Decades ago, Bartels and Kusakcioglu13 and Grubb14 reported that narcolepsy was a possible cause of automobile accidents. Aldrich reviewed the data on sleep-related accidents and compared 70 control patients and 424 participants, and the proportion of patients with sleep-related accidents was highest in patients with narcolepsy.15 Findley et al. enrolled 62 participants with sleep apnea and 10 participants with narcolepsy and found that patients with sleep apnea or narcolepsy had impaired vigilance with a higher automobile accident rate.35 Liu et al. recently used data from a naturalistic driving study and found that drivers with narcolepsy are at significantly higher risk of a crash or near-crash events.34
This study also echoed the benefits of stimulant use on safe driving seen in the results of previous studies.36,37 Gurtman et al. found that modafinil has some benefits concerning an objective driving performance under the conditions of an overnight period of sleep loss.36 Philip et al. further designed a randomized, double-blind placebo-controlled crossover trial of 13 participants with narcolepsy and 14 participants with idiopathic hypersomnia and found that modafinil improved their driving performance.37
In this study, we have several noteworthy findings. First, the patients with narcolepsy had a 6.725-fold increased risk of hospitalization for MVAI when compared to the control participants. Excessive daytime sleepiness and cataplexy are the main symptoms of narcolepsy, and these symptoms are highly associated with MVAI. Many previous studies have investigated the relationship between sleep-related characteristics and automobile accidents, and daytime sleepiness is one of the significant factors.7,9,38 The evidence of a relationship between cataplexy and MVAI is limited, but the causal relationship is reasonable. Cataplexy is a transient episode of muscle weakness, as it can easily induce dangerous driving.
Second, we investigated the type of injury resulting in hospitalization for MVAI and found that patients with narcolepsy had higher risks of fractures and fewer intracranial and internal injuries compared with those without narcolepsy, and 38 of the 47 events were classified as “other and unspecified effects of external causes.” An explanation for these findings is that patients with narcolepsy and MVAI might have more complicated injuries that are not easy to classify as a single type of injury, so clinicians use the phrase “other and unspecified effects of external causes” to define the injuries. Thus, the coding of “other and unspecified effects of external causes” might underestimate the occurrence of other types of injuries, including intracranial and internal injury.
Third, we found that patients with narcolepsy had a higher risk of hospitalization for MVAI when they were the drivers of different types of vehicles, but not passengers. The significantly increased adjusted HRs were found in all the subgroups of the motor vehicle, motorcycle, and the pedal cycle. Unlike many of the developed countries, motorcycles remain popular and commonly used in Taiwan, as with many other Asian countries with a high population density.39 There are many vital issues concerning motorcycle-related injuries studied in Taiwan,40,41 but none of them evaluate the issue of narcolepsy. We found that patients with narcolepsy had an approximately sixfold increased risk of hospitalization for MVAI when they were motorcyclists. Further, drivers of motor vehicles with narcolepsy had a much higher risk than motorcyclists and pedal cyclists in hospitalization for MVAI (aHR 40.779 versus 6.253 and 4.078). Our findings suggest that patients with narcolepsy should carefully consider their risk whether they are a rider or driver, regardless of transportation category.
Fourth, we found that patients with narcolepsy were at particularly high risk for serious (ISS ≥ 16) MVAI over minor injuries (ISS < 16) (aHR 4.894 versus 8.760). The high risk for more severe MVAI could be related to impaired vigilance that is known to occur in narcolepsy.35
Finally, we found that stimulants such as modafinil and methylphenidate could decrease the risk of hospitalization for MVAI in patients with narcolepsy. Modafinil and methylphenidate are frequently used in patients with narcolepsy and are beneficial for the symptoms of daytime sleepiness,16,42,43 which is the leading cause of MVAI. Some previous clinical studies have also confirmed that the use of modafinil can improve the driving performance in patients with hypersomnia and individuals with sleep deprivation.36,37 Our study has further provided some critical information for this issue. We found that the use of stimulants in patients with narcolepsy could reduce the likelihood of MVAI of all severities. Additionally, the combined use of modafinil and methylphenidate may be superior to either medication alone. A longer PDC of stimulant prescription appeared to reduce risk further, which suggests a dose-response relationship between stimulant use and risk reduction. Clinicians should be vigilant in assessing the need for stimulant therapy for patients with narcolepsy.
Current policy in Taiwan suggests that medical specialists should carefully evaluate patients with narcolepsy before the test for a driving license, but these individuals are not prohibited from driving. Many countries including Canada, the United Kingdom, and some states of the United States have specific guidelines regarding the fitness of patients with narcolepsy for driving.44 According to one review, regulations governing mandatory reporting of sleep disorders to traffic authorities are frequently inconsistent with scientific knowledge relating sleepiness to driving.45 Our results could bring some insights into this issue.
In the current study, we demonstrated a higher concentration of patients with narcolepsy in Northern Taiwan, more highly urbanized areas, and centers marked by a higher level of medical care. This is likely because most sleep centers are located in Northern Taiwan, which is more highly urbanized. From the statistics of the Taiwan Society of Sleep Medicine, among the 20 sleep centers in Taiwan, 40 % (8/20) are in Northern Taiwan, and 60% (12/20) are located in medical centers.46 Another notable finding was the low prevalence of anxiety and depression at study entry, which was higher in patients with narcolepsy than in control participants (Table 1); however, when the whole study period was considered, anxiety and depression increased to 20% and was similar between patients with narcolepsy and control participants (Table S3 in the supplemental material).
This study has several limitations. First, the diagnosis of narcolepsy was obtained based on the ICD-9-CM codes instead of validated structural diagnostic instruments. In addition, the ICD-9-CM does not differentiate between type 1 and type 2 narcolepsy. These data may be less accurate in the enrolled participants. For instance, patients with idiopathic hypersomnia, severe sleep apnea, sleep deprivation, and circadian rhythm disorders might be recorded as patients with narcolepsy. However, the National Health Insurance Administration in Taiwan has made every effort to verify the exactness of the diagnoses in the database. Additionally, to further ensure accuracy, we only enrolled participants with at least three outpatient clinic visits that were coded with a diagnosis of narcolepsy. Because narcolepsy is a rare disorder, it is still worth using this nationwide population-based, retrospective cohort study to provide information for such an important issue. Second, the use of stimulants was assessed based on the prescription records, but the medication compliance and the rate of refills were unknown. However, we compared the different PDC of stimulant use to minimize the effect of this limitation. In addition, only modafinil and methylphenidate have been licensed to treat narcolepsy in Taiwan. The effects of other medications such as sodium oxybate were not able to be evaluated in our study. Third, several important un-measured confounding factors may have affected the results. For example, it is important to evaluate where and how the MVAI happened and the lifestyle of the patients with narcolepsy, as drinking coffee or napping routines are not able to be assessed by the NHIRD. Fourth, some of the results may have error grouping because of the coding preference from clinicians. For example, the subgroup analysis in Table 3 found that the rate of “others” groups is higher than other subgroups in both types of injury and vehicle use. The error grouping may lead to underestimation of the results in other subgroups. Finally, the results may or may not be generalizable to contexts outside Taiwan. The rush- hour traffic conditions and the high proportion of motorcycle usage are unique in a high population density country such as Taiwan, and further verification of the generalizability of our results to other countries is needed.
CONCLUSIONS
This study found a significantly higher risk of hospitalization for MVAI in patients with narcolepsy, and the use of stimulants such as modafinil and methylphenidate could reduce the risk of MVAI. If the association reflects a causal effect, these findings strongly suggest that clinicians should inform the patients about the risk of MVAI and the benefits of stimulant use to those with narcolepsy.
DISCLOSURE STATEMENT
This study was performed in the Tri-Service General Hospital, Taipei, Taiwan. All authors have seen and approved this manuscript. This work was supported by the Tri-Service General Hospital Research Foundation (TSGH-C106-104, TSGH-C107-004, TSGH-C107-106, TSGH-C108-003, TSGH-C108-151) and the Medical Affairs Bureau, Ministry of Defense of Taiwan (MAB-107-084). The authors report no conflicts of interest.
ACKNOWLEDGMENTS
The authors thank Ming-Chieh Tsai for preparing this manuscript. Author contributions: NST contributed to the study design and wrote the manuscript; HAC, YCK, WCM, SCH, CHY, and BJK contributed to manuscript preparation, editing, and revision; CHC and WCC contributed to interpretation of the results and statistical analysis of the study; TYC and WCC contributed to the study design, supervision of the work, and manuscript preparation.
ABBREVIATIONS
- BZRA
benzodiazepine receptor agonists
- CCI
Charlson Comorbidity Index
- ICD-9-CM
International Classification of Diseases, Ninth Revision, Clinical Modification
- ISS
Injury Severity Score
- MVAI
motor vehicle accident injury
- NHI
National Health Insurance
- NHIRD
National Health Insurance Research Database
- PDC
proportion of days covered
REFERENCES
- 1.Craig A, Tran Y, Guest R, et al. Psychological impact of injuries sustained in motor vehicle crashes: systematic review and meta-analysis. BMJ Open. 2016;6(9):e011993. doi: 10.1136/bmjopen-2016-011993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jiang B, Liang S, Peng ZR, et al. Transport and public health in China: the road to a healthy future. Lancet. 2017;390(10104):1781–1791. doi: 10.1016/S0140-6736(17)31958-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Karkee R, Lee AH. Epidemiology of road traffic injuries in Nepal, 2001-2013: systematic review and secondary data analysis. BMJ Open. 2016;6(4):e010757. doi: 10.1136/bmjopen-2015-010757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vecino-Ortiz AI, Jafri A, Hyder AA. Effective interventions for unintentional injuries: a systematic review and mortality impact assessment among the poorest billion. Lancet Glob Health. 2018;6(5):e523–e534. doi: 10.1016/S2214-109X(18)30107-4. [DOI] [PubMed] [Google Scholar]
- 5.Gupta R, Pandi-Perumal SR, Almeneessier AS, BaHammam AS. Hypersomnolence and traffic safety. Sleep Med Clin. 2017;12(3):489–499. doi: 10.1016/j.jsmc.2017.03.018. [DOI] [PubMed] [Google Scholar]
- 6.Pizza F, Jaussent I, Lopez R, et al. Car crashes and central disorders of hypersomnolence: a French study. PloS One. 2015;10(6):e0129386. doi: 10.1371/journal.pone.0129386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Powell NB, Schechtman KB, Riley RW, Guilleminault C, Chiang RP, Weaver EM. Sleepy driver near-misses may predict accident risks. Sleep. 2007;30(3):331–342. doi: 10.1093/sleep/30.3.331. [DOI] [PubMed] [Google Scholar]
- 8.Smolensky MH, Di Milia L, Ohayon MM, Philip P. Sleep disorders, medical conditions, and road accident risk. Accid Anal Prev. 2011;43(2):533–548. doi: 10.1016/j.aap.2009.12.004. [DOI] [PubMed] [Google Scholar]
- 9.Quera Salva MA, Barbot F, Hartley S, et al. Sleep disorders, sleepiness, and near-miss accidents among long-distance highway drivers in the summertime. Sleep Med. 2014;15(1):23–26. doi: 10.1016/j.sleep.2013.06.018. [DOI] [PubMed] [Google Scholar]
- 10.Murray TJ, Foley A. Narcolepsy. Can Med Assoc J. 1974;110(1):63–66. [PMC free article] [PubMed] [Google Scholar]
- 11.Zeman A, Britton T, Douglas N, et al. Narcolepsy and excessive daytime sleepiness. BMJ. 2004;329(7468):724–728. doi: 10.1136/bmj.329.7468.724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dauvilliers Y, Arnulf I, Mignot E. Narcolepsy with cataplexy. Lancet. 2007;369(9560):499–511. doi: 10.1016/S0140-6736(07)60237-2. [DOI] [PubMed] [Google Scholar]
- 13.Bartels EC, Kusakcioglu O. Narcolepsy: a possible cause of automobile accidents. Lahey Clin Found Bull. 1965;14(1):21–26. [PubMed] [Google Scholar]
- 14.Grubb TC. Narcolepsy and highway accidents. JAMA. 1969;209(11):1720. [PubMed] [Google Scholar]
- 15.Aldrich MS. Automobile accidents in patients with sleep disorders. Sleep. 1989;12(6):487–494. doi: 10.1093/sleep/12.6.487. [DOI] [PubMed] [Google Scholar]
- 16.Barateau L, Lopez R, Dauvilliers Y. Treatment options for narcolepsy. CNS Drugs. 2016;30(5):369–379. doi: 10.1007/s40263-016-0337-4. [DOI] [PubMed] [Google Scholar]
- 17.Barateau L, Lopez R, Dauvilliers Y. Management of narcolepsy. Curr Treat Options Neurol. 2016;18(10):43. doi: 10.1007/s11940-016-0429-y. [DOI] [PubMed] [Google Scholar]
- 18.Kallweit U, Bassetti CL. Pharmacological management of narcolepsy with and without cataplexy. Expert Opin Pharmacother. 2017;18(8):809–817. doi: 10.1080/14656566.2017.1323877. [DOI] [PubMed] [Google Scholar]
- 19.Swick TJ. Treatment paradigms for cataplexy in narcolepsy: past, present, and future. Nat Sci Sleep. 2015;7:159–169. doi: 10.2147/NSS.S92140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ho Chan WS. Taiwan's healthcare report 2010. EPMA J. 2010;1(4):563–585. doi: 10.1007/s13167-010-0056-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Needham DM, Scales DC, Laupacis A, Pronovost PJ. A systematic review of the Charlson comorbidity index using Canadian administrative databases: a perspective on risk adjustment in critical care research. J Crit Care. 2005;20(1):12–19. doi: 10.1016/j.jcrc.2004.09.007. [DOI] [PubMed] [Google Scholar]
- 22.Chinese Hospital Association. ICD-9-CM English-Chinese Dictionary. Taipei, Taiwan: Chinese Hospital Association Press; 2000. [Google Scholar]
- 23.Tzeng NS, Hsu YH, Ho SY, et al. Is schizophrenia associated with an increased risk of chronic kidney disease? A nationwide matched-cohort study. BMJ Open. 2015;5(1):e006777. doi: 10.1136/bmjopen-2014-006777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yang CW, Tzeng NS, Yin YJ, et al. Angiotensin receptor blockers decrease the risk of major adverse cardiovascular events in patients with end-stage renal disease on maintenance dialysis: a nationwide matched-cohort study. PloS One. 2015;10(10):e0140633. doi: 10.1371/journal.pone.0140633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tzeng NS, Chung CH, Yeh CB, et al. Are chronic periodontitis and gingivitis associated with dementia? A nationwide, retrospective, matched-cohort study in Taiwan. Neuroepidemiology. 2016;47(2):82–93. doi: 10.1159/000449166. [DOI] [PubMed] [Google Scholar]
- 26.Chen TY, Winkelman JW, Mao WC, Liu CL, Hsu CY, Wu CS. The use of benzodiazepine receptor agonists and the risk of hospitalization for pneumonia: a nationwide population-based nested case-control study. Chest. 2018;153(1):161–171. doi: 10.1016/j.chest.2017.07.030. [DOI] [PubMed] [Google Scholar]
- 27.Sheu JJ, Lee HC, Lin HC, Kao LT, Chung SD. A 5-year follow-up study on the relationship between obstructive sleep apnea and Parkinson disease. J Clin Sleep Med. 2015;11(12):1403–1408. doi: 10.5664/jcsm.5274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sedgwick P. Retrospective cohort studies: advantages and disadvantages. BMJ. 2014;348:g1072. doi: 10.1136/bmj.g2979. [DOI] [PubMed] [Google Scholar]
- 29.Copes WS, Champion HR, Sacco WJ, Lawnick MM, Keast SL, Bain LW. The Injury Severity Score revisited. J Trauma. 1988;28(1):69–77. doi: 10.1097/00005373-198801000-00010. [DOI] [PubMed] [Google Scholar]
- 30.Chang CY, Chen WL, Liou YF, et al. Increased risk of major depression in the three years following a femoral neck fracture--a national population-based follow-up study. PloS One. 2014;9(3):e89867. doi: 10.1371/journal.pone.0089867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Randomised trial of plasma exchange, intravenous immunoglobulin, and combined treatments in Guillain-Barre syndrome. Plasma Exchange/Sandoglobulin Guillain-Barré Syndrome Trial Group. Lancet. 1997;349(9047):225–230. [PubMed] [Google Scholar]
- 32.van den Berg B, Walgaard C, Drenthen J, Fokke C, Jacobs BC, van Doorn PA. Guillain-Barre syndrome: pathogenesis, diagnosis, treatment and prognosis. Nat Rev Neurol. 2014;10(8):469–482. doi: 10.1038/nrneurol.2014.121. [DOI] [PubMed] [Google Scholar]
- 33.Willison HJ, Jacobs BC, van Doorn PA. Guillain-Barre syndrome: surveillance and cost of treatment strategies - Authors' reply. Lancet. 2017;389(10066):253–254. doi: 10.1016/S0140-6736(17)30055-7. [DOI] [PubMed] [Google Scholar]
- 34.Liu SY, Perez MA, Lau N. The impact of sleep disorders on driving safety-findings from the Second Strategic Highway Research Program naturalistic driving study. Sleep. 2018;41(4) doi: 10.1093/sleep/zsy023. [DOI] [PubMed] [Google Scholar]
- 35.Findley L, Unverzagt M, Guchu R, Fabrizio M, Buckner J, Suratt P. Vigilance and automobile accidents in patients with sleep apnea or narcolepsy. Chest. 1995;108(3):619–624. doi: 10.1378/chest.108.3.619. [DOI] [PubMed] [Google Scholar]
- 36.Gurtman CG, Broadbear JH, Redman JR. Effects of modafinil on simulator driving and self-assessment of driving following sleep deprivation. Hum Psychopharmacol. 2008;23(8):681–692. doi: 10.1002/hup.983. [DOI] [PubMed] [Google Scholar]
- 37.Philip P, Chaufton C, Taillard J, et al. Modafinil improves real driving performance in patients with hypersomnia: a randomized double-blind placebo-controlled crossover clinical trial. Sleep. 2014;37(3):483–487. doi: 10.5665/sleep.3480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sunwoo JS, Hwangbo Y, Kim WJ, Chu MK, Yun CH, Yang KI. Sleep characteristics associated with drowsy driving. Sleep Med. 2017;40:4–10. doi: 10.1016/j.sleep.2017.08.020. [DOI] [PubMed] [Google Scholar]
- 39.Chen CF. Personality, safety attitudes and risky driving behaviors--evidence from young Taiwanese motorcyclists. Accid Anal Prev. 2009;41(5):963–968. doi: 10.1016/j.aap.2009.05.013. [DOI] [PubMed] [Google Scholar]
- 40.Chiu WT, Chu SF, Chang CK, Lui TN, Chiang YH. Implementation of a motorcycle helmet law in Taiwan and traffic deaths over 18 years. JAMA. 2011;306(3):267–268. doi: 10.1001/jama.2011.989. [DOI] [PubMed] [Google Scholar]
- 41.Liang CC, Liu HT, Rau CS, Hsu SY, Hsieh HY, Hsieh CH. Motorcycle-related hospitalization of adolescents in a Level I trauma center in southern Taiwan: a cross-sectional study. BMC Pediatr. 2015;15:105. doi: 10.1186/s12887-015-0419-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mitler MM, Harsh J, Hirshkowitz M, Guilleminault C. Long-term efficacy and safety of modafinil (PROVIGIL((R))) for the treatment of excessive daytime sleepiness associated with narcolepsy. Sleep Med. 2000;1(3):231–243. doi: 10.1016/s1389-9457(00)00031-9. [DOI] [PubMed] [Google Scholar]
- 43.Lavault S, Dauvilliers Y, Drouot X, et al. Benefit and risk of modafinil in idiopathic hypersomnia vs. narcolepsy with cataplexy. Sleep Med. 2011;12(6):550–556. doi: 10.1016/j.sleep.2011.03.010. [DOI] [PubMed] [Google Scholar]
- 44.Pakola SJ, Dinges DF, Pack AI. Review of regulations and guidelines for commercial and noncommercial drivers with sleep apnea and narcolepsy. Sleep. 1995;18(9):787–796. doi: 10.1093/sleep/18.9.787. [DOI] [PubMed] [Google Scholar]
- 45.MacLean AW, Davies DR, Thiele K. The hazards and prevention of driving while sleepy. Sleep Med Rev. 2003;7(6):507–521. doi: 10.1016/s1087-0792(03)90004-9. [DOI] [PubMed] [Google Scholar]
- 46.A Brief Introduction of Taiwan Society of Sleep Medicine. Taiwan Society of Sleep Medicine website. [Accessed May 6, 2019]. http://www.tssm.org.tw/English.php?key=English_About.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.