Abstract
Study Objectives:
To evaluate prevalence of sedative hypnotic medications and their potential indication among active duty service members (ADSM) and non-ADSM receiving care in the Military Health System (MHS).
Methods:
Using a retrospective cohort study design, we extracted data on sedative hypnotic medications (benzodiazepine receptor agonists, benzodiazepines, sedating antidepressants, and melatonin receptor agonist) dispensed from January 2009 to December 2015. Prevalence was defined as ≥ 1 dispensing per patient per year whereas chronic episode was categorized as ≥ 90 days of continuous therapy. Chi square statistics, odds ratios, and 95% confidence intervals were calculated to assess meaningful differences between ADSM and non-ADSM.
Results:
Mean age at dispensing was 33.5 years in ADSM compared to 59.1 years in non-ADSM. Of all drugs dispensed, 79.2% (n = 2.4 million) were to male ADSM compared to 34.5% (11.5 million) to male non-ADSM. Zolpidem and trazodone were the two most frequently used medications, comprising more than 75% of all prescriptions. Age- and sex-adjusted prevalence peaked at 8.1% in 2013 for ADSM and at 4.9% in 2012 for non-ADSM and remained stable thereafter for both groups. Most episodes for ADSM (81.0%) and non-ADSM (65.0%) were acute or intermittent. ADSM were significantly more likely to have a sleep-related diagnosis associated with their episode than non-ADSM (odds ratio 2.35, 95% confidence interval 2.33–2.36), most frequently insomnia.
Conclusions:
ADSM had a 2% to 3% higher adjusted prevalence of sedative hypnotic medications than non-ADSM. The use of sedative hypnotics in the young ADSM population highlights the need for military-appropriate sleep practices and novel interventions to mitigate sleep disturbances and chronic sleep disorders in this population.
Citation:
Thelus Jean R, Hou Y, Masterson J, Kress A, Mysliwiec V. Prescription patterns of sedative hypnotic medications in the Military Health System. J Clin Sleep Med. 2019;15(6):873–879.
Keywords: hypnotics, insomnia, military health population, military personnel, sedatives, sleep disorders
BRIEF SUMMARY
Current Knowledge/Study Rationale: Active duty service members (ADSM) are a unique population that are at high risk for sleep disturbances and the development of insomnia. Recent information on trend of pharmacological intervention that can be used to mitigate these outcomes are scarce.
Study Impact: In a comprehensive multiyear assessment of sedative hypnotic medications dispensed in the Military Healthcare System, ADSM had a consistently higher prevalence of sedative hypnotic prescriptions than non-ADSM. Most prescriptions in ADSM were for acute or intermittent treatment episodes. In this unique population, the high prevalence of sedative hypnotic medications likely correlates with their high rates of sleep disturbances and suggests the need for novel approaches to improve their sleep.
INTRODUCTION
Chronic insomnia is a disorder that affects approximately 10% of adults in the general population.1,2 There have been marked increases in insomnia diagnoses in the military,3,4 with a recent publication by Taylor et al. reporting the prevalence of insomnia in United States Army soldiers at 19.9%.5 Although this proportion is almost twice as high as that of the general population, the Rand report on sleep in the military found that 48.6% of active duty service members (ADSM) reported poor-quality sleep,6 and thus 19.9% is likely a reasonable estimate of insomnia in this population. Reasons for the higher prevalence in the Rand report could be attributed to other conditions such as insufficient sleep, circadian misalignment, military deployments, and the stressful profession.7,8
In ADSM, insufficient sleep and insomnia symptoms are associated with increased risk of mental health disorders, to include posttraumatic stress disorder9,10; other correlates include lower self-rated health and odds of deployment, increased lost work days and health care utilization, and a higher likelihood of early discharge from military service.6,11 Thus, the treatment of insomnia has implications not only on the sleep and duty performance of service members, but their long-term health.
Despite the increased awareness of sleep disturbances in the military, there are few data on the prevalence and patterns of pharmacologic therapy of insomnia in this population. In one military publication, 11.4% of deployed ADSM reported taking a medication for a “sleep problem.”12 Current clinical guidelines are that pharmacologic treatment may result in improved sleep in the short term, but long-term efficacy is unknown.13 Although short-term pharmacologic treatment for insomnia symptoms may be appropriate, the potential serious side effects of sedative hypnotic medications to include complex behaviors,14 cognitive impairment,15 and increased risk of motor vehicle accidents16 could affect an ADSM's military mission.
The high prevalence of insomnia and inherent risk in the military profession underscores the need for a better understanding of sedative hypnotic prescribing in this population. The primary objective of this study was to describe the prevalence and prescription patterns of sedative hypnotics and their potential indications in ADSM. A secondary objective was to assess differences between ADSM and non-ADSM (retirees and family members who receive care in the Military Health System [MHS]). The non-ADSM were used as a reference population to determine if sedative hypnotic prescription patterns were inherent to the MHS or differed between active duty and non-ADSM.
METHODS
Source Data and Population
Patients from the MHS population were included in the study if they had one or more prescriptions dispensed for a sedative hypnotic medication to include: benzodiazepine receptor agonists or BZRAs (eszopiclone, zaleplon, zolpidem); benzodiazepines (estazolam, flurazepam, quazepam, temazepam, triazolam); sedating antidepressants (trazodone, doxepin); and a melatonin receptor agonist (ramelteon) from January 2009 to December 2015. All patients included in the study had to be eligible to receive care within the MHS system in the year prior to their index prescription of sedative hypnotic medications. For ADSM, this included all ADSM in the United States Army, Navy, Air Force, Marines, and Coast Guard along with active National Guard members or Reservists during the respective time periods. For non-ADSM, this primarily included family members of ADSM, retired service members and their family members.17 More detail describing how health care is provided within the MHS is published elsewhere.18,19 Approval for this study was obtained from the Department of the Army, Headquarters, United States Army Medical Research and Materiel Command, Office of Research Protections.
Prescribing Patterns
Information on drug characteristics such as date dispensed, days' supply, and product name as well as demographic characteristics (ADSM or non-ADSM, age, sex, service branch, beneficiary category) were extracted from the MHS pharmacy data transaction system. Characteristics of sedative hypnotic medications were described at the prescription level and percentages were calculated as the proportion of total drugs dispensed. Patient level information such as prevalence of sedative hypnotics and demographic characteristics of patients receiving treatment were calculated based on the number of patients receiving one or more prescriptions divided by the total number of eligible beneficiaries within each year. Patients can be counted in multiple years if they received prescriptions across different years.
To determine continuous duration of therapy, prescriptions dispensed within 30 days of the end of a previous prescription were linked to form a continuous treatment episode. A gap of 31 days or more was used to classify the start of a different treatment episode. After treatment episodes were defined, they were classified as acute, intermittent, or chronic episodes. Acute therapy was defined as episodes lasting fewer than 30 days; intermittent therapy were treatment episodes lasting from 31 to 89 days and chronic therapy was defined as episodes lasting 90 days or more.
Ascertainment of Potential Indication
To assess sleep-related conditions prior to dispensing of sedative hypnotic medications, outpatient records were examined for sleep-related diagnosis codes (Table S3 in the supplemental material) 30 days prior to each treatment episode. Patients with one or more of the relevant codes were classified into four broad categories: insomnia, obstructive sleep apnea, circadian rhythm sleep disorders, and unspecified sleep disturbances. We also combined all categories into any sleep-related conditions to determine the overall number of treatment with at least one sleep-related condition.
Statistical Analysis
Statistical analysis was conducted using SAS software, Version 9.4 (SAS Institute Inc., Cary, North Carolina, United States). Descriptive analysis was used to characterize demographics and prescribing patterns by active duty status and within respective categories. Categorical variables were presented as frequencies and percentages whereas continuous variables were presented as means and standard deviations.
Crude prescribing prevalence was calculated by dividing the number of people with one or more prescriptions by the total number of eligible beneficiaries within respective years. To account for differences in age and sex distribution between ADSM and non-ADSM, we calculated yearly standardized prescribing rates for both groups using the 2010 United States census population as reference.20 Pearson chi-square statistic was used to compare adjusted prevalence by year to determine statistically meaningful differences (defined as P < .05) between the two groups. Additionally, age- and sex-specific as well as adjusted proportions were graphed to visually assess any potential pattern during the study time period.
Proportion of sleep-related diagnosis prior to each episode related to sedative hypnotic medications was calculated as the number of treatments with a relevant diagnosis in the prior 30 days divided by the total number of episodes. To compare differences in documented sleep-related conditions, the odds ratio (OR) of an associated sleep disorder among ADSM was compared to that of non-ADSM. ORs with 95% confidence intervals (CI) were calculated for overall and each specific sleep-related condition.
RESULTS
Demographic and Medication Characteristics
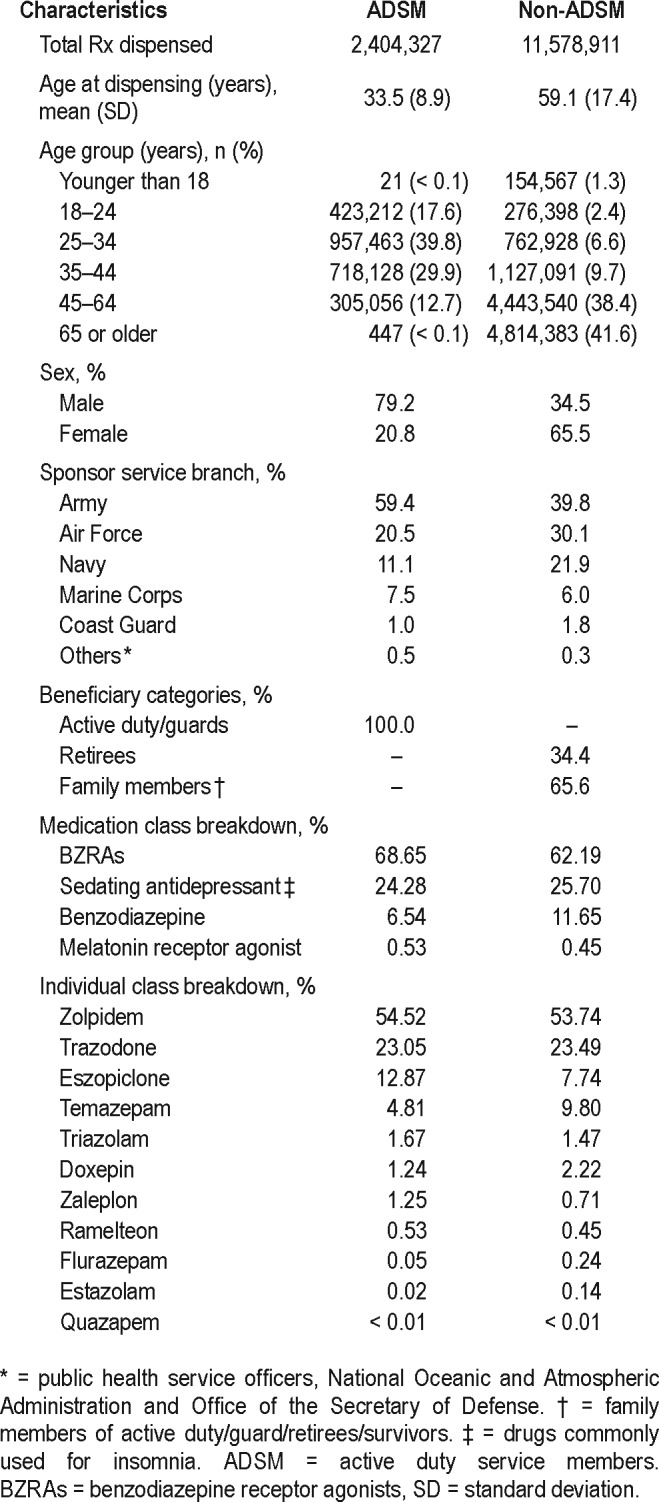
A total of 13.98 million prescriptions were dispensed during the study period; most prescriptions were dispensed to non-ADSM. The age and sex dispensing patterns were consistent with the underlying population distribution of ADSM and non-ADSM.21 Specifically, average age at dispensing was substantially lower for ADSM (33.5 years) when compared to that of non-ADSM (59.1 years); over 80% of all medications were dispensed to ADSM younger than 45 years whereas about the same amount were dispensed to non-ADSM older than 45 years. Most prescriptions for sedative hypnotics among ADSM were dispensed to males (79.2%), whereas in non-ADSM most (65.5%) were dispensed to females. Proportion of medications dispensed by branch of service was highest for Army followed by Air Force and Navy in both groups. Among non-ADSM, 34.4% of the population were retirees indicating that they had previously served in the military (Table 1). Regarding specific medications, zolpidem (∼54%) and trazodone (∼23%), the two most dispensed medications, consistently made up over 75% of all sedative hypnotic medications dispensed.
Table 1.
Demographic characteristics of those receiving sedative hypnotic medications by active duty status from 2009 to 2015.
Trends in Prescribing Prevalence
The average number of prescriptions per ADSM increased from 2.1 prescriptions in 2009 to 3.1 in 2014. For non-ADSM, these numbers were significantly higher (P < .001) but the overall trend was very similar (Table S1 in the supplemental material). Crude prevalence of ADSM receiving more than one prescription for sedative hypnotic medications increased from 5.2% in 2009 to 7.1% in 2012 and declined to 5.9% in 2015. For non-ADSM the crude proportion peaked at 5.1% in 2012 and declined to 4.86 in 2015 (Figure S1 in the supplemental material).
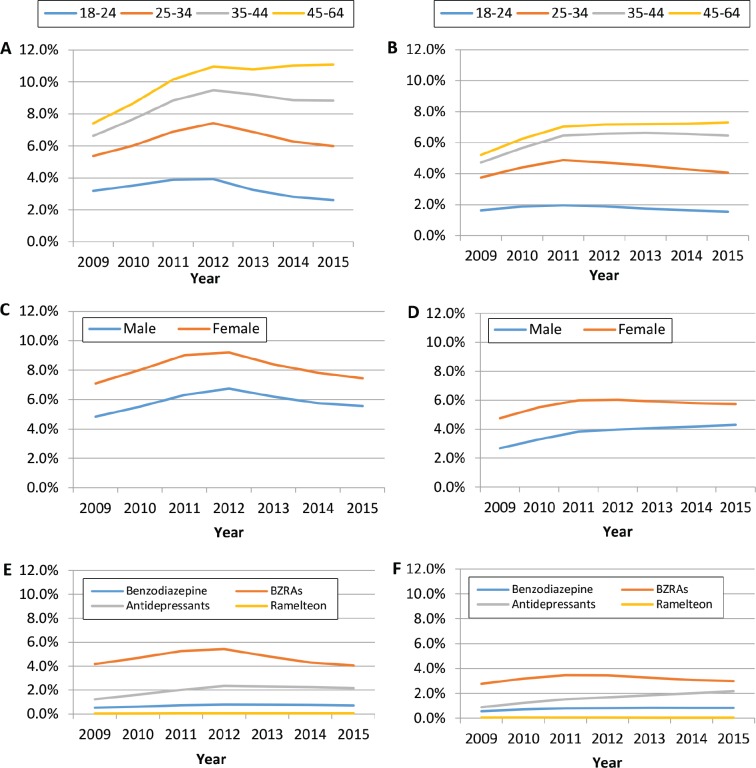
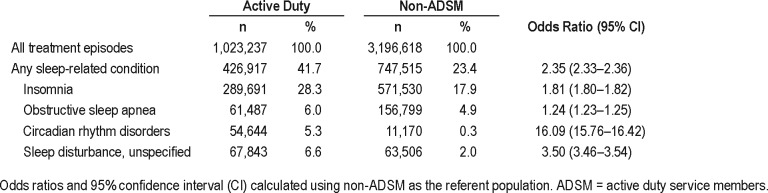
Age- and sex-specific prevalence was consistently higher for ADSM compared to non-ADSM; the greatest difference in prevalence by age was in the oldest age group (45–64 years) (Figure 1, panels A–D). After adjusting for age and sex, prevalence of sedative hypnotic medications peaked at 8.1% in 2013 for ADSM but remained relatively consistent with the crude patterns for non-ADSM. After 2013, rates of sedative hypnotic medications in both ADSM and non-ADSM remained relatively constant (Figure 2). At every time point, ADSM has significantly higher (P < .001) age- and sex-adjusted rates than non-ADSM.
Figure 1. Age- and sex-specific prevalence for sedative hypnotic medications from 2009 to 2015.
(A) ADSM by age, (B) non-ADSM by age, (C) ADSM by sex, (D) non-ADSM by sex, (E) ADSM by classes, and (F) non-ADSM by classes.
Figure 2. Age- and sex-adjusted rates of sedative hypnotic medications in ADSM and non-ADSM from 2009 to 2015.
* Significant at P < .001. ADSM = active duty service members.
Consistent with overall dispensing, prevalence of BZRAs (the largest class of medication) decreased for both ADSM and non-ADSM whereas the prevalence of antidepressants (second largest) remained relatively stable (2%) for ADSM after 2012 and continuously increased among non-ADSM (Figure 1, panels E and F). Prevalence of benzodiazepines and ramelteon, which had much lower prescription rates, remained relatively unchanged for both groups across the study period.
Pattern of Treatment and Sleep-Related Diagnosis
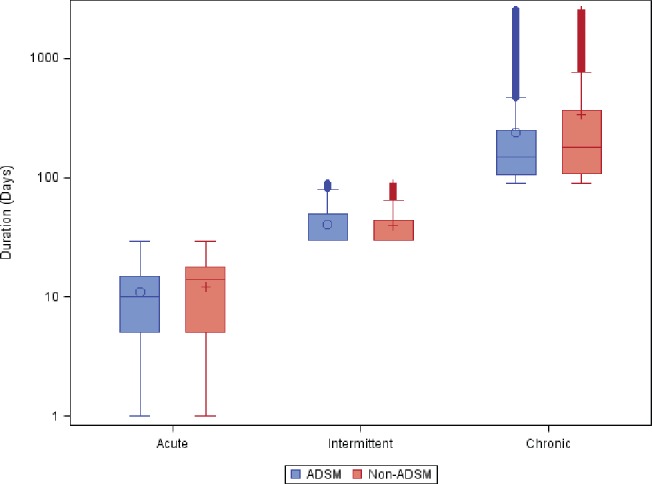
ADSM received 1.02 million sedative hypnotic episodes whereas non-ADSM received 3.2 million episodes during the study period. Most episodes for ADSM (81.0%) and non-ADSM (65%) were acute or intermittent. (Table S2 in the supplemental material). Average duration of treatment for acute (11 days for ADSM and 12 days for non-ADSM) and intermittent episodes (40 days for ADSM and 39 days for non-ADSM) were similar for both groups. For chronic use, duration of treatment in ADSM was markedly shorter (241 days) than non-ADSM (340 days) (Figure 3). When stratified by age group, proportion of episodes that were chronic increased with age, irrespective of active duty or non-active duty status but the increase by age group was more pronounced among non-ADSM.
Figure 3. Duration of sleep medication by type of therapy.
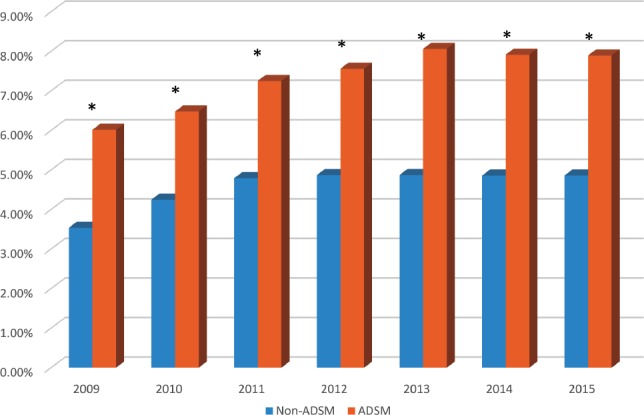
Overall, 42% of ADSM and 23% of non-ADSM had a sleep disorder diagnosis associated with their treatment episode. For ADSM the most frequent associated diagnosis was insomnia in 28.3%, followed by obstructive sleep apnea in 6.0%, circadian rhythm disorders in 5.3%, and unspecified sleep disturbance in 6.6% of all episodes. Specifically, ADSM were more than twice as likely to have a sleep-related diagnosis as non-ADSM (OR 2.35, 95% CI 2.33–2.36) (Table 2). The difference in associated diagnoses was most pronounced for circadian rhythm disorders where ADSM had greater than a 16-fold higher odds (OR 16.09, 95% CI 15.76–16.42) of a circadian rhythm disorder compared to non-ADSM. There was no significant change in the associated diagnoses between ADSM and non-ADSM when we assessed the difference by acute, intermittent and chronic episodes.
Table 2.
Pattern of sleep-related diagnosis prior to treatment episodes by active duty status.
DISCUSSION
The primary finding of our study is that ADSM have a higher prevalence of sedative hypnotic prescriptions than a corresponding cohort of non-ADSM even after accounting for age and sex differences among the two groups. This finding is consistent with the higher prevalence of sleep disturbances6 and insomnia5 reported in ADSM than non-ADSM. Although the overall prevalence of sedative hypnotic medications was higher for ADSM, they were less likely to have chronic episodes when compared to non-ADSM who were almost twice as likely to have chronic treatment.22 Most notably, more than 80% of sedative hypnotic episodes in ADSM were acute or intermittent. To our knowledge, this study is the first to document such differences in prescribing patterns in ADSM, a population that is often exposed to increased occupational risks.
Several factors that may explain the higher proportion of acute and intermittent episodes related to sedative hypnotic medications in ADSM include: insomnia symptoms secondary to stress from military duties and/or work environment (ie, field training exercise, deployment), circadian misalignment from shift work, 24-hour duty or jetlag6,23,24 The higher proportion of sleep disorder diagnoses associated with episodes related to sedative hypnotic medications for ADSM than non-ADSM provide some support for this association; specifically, the higher odds of circadian rhythm disorder in ADSM.
Despite potential short-term indications for pharmacologic therapy for transient sleep disturbances or insomnia symptoms, the higher prevalence of sedative hypnotic medications is concerning. Specifically, ADSM are relatively young with a mean age of 33.5 years and have recurrent sleep disturbances because of the nature of their military duties. Prior research has found that individuals using sleep aids for insomnia are likely to continue using them.25 Thus, there is the potential for recurrent or long-term sleep medications usage in ADSM. Another important consideration is that in individuals who have insomnia symptoms of a short-term or transient nature, chronic insomnia appears more likely to develop.26 Our study did not evaluate the outcomes of military personnel who received acute or intermittent treatment episodes. However, the high prevalence of insomnia5 in the military suggests more robust treatment options (ie, behavioral therapies) for this common sleep disorder are required.
Our findings show an initial increase from 2009 to 2012 in prevalence of sedative hypnotic medications in both ADSM and non-ADSM followed by continual decline in age- and sex-specific prevalence in ADSM, except in the 45- to 64-year-old age group. The initial increased prevalence of sedative hypnotics, for both ADSM and non-ASDM, is consistent with two previous studies that assessed sleep medication usage utilizing National Health and Nutrition Examination Survey data.27,28 Specifically, both studies reported an increasing prevalence of sleep medication usage in 2010 and 2012; however, to our knowledge there are no large population-based studies since 2012 on prescribing patterns of sedative hypnotic medications.28
Our finding of decrease in prevalence of BZRAs corresponded to the US Food and Drug Administration drug safety communication regarding the risk of zolpidem as well as eszoplicone.20,21 Additionally, in the MHS, an online training requirement for providers on this topic might have also contributed to the more pronounced decline in ADSM. Furthermore, a recent guideline from the American Academy of Sleep Medicine on the pharmacologic treatment of chronic insomnia reported only weak recommendations for using eszopiclone, zolpidem, and temazepam to treat insomnia and weak recommendations for not using trazodone.29 As zolpidem and trazo-done were the two most frequently dispensed medications in our population, the effects of this guideline on future clinical practice merits further investigation.
Overall, non-ADSM military health care beneficiaries had a prevalence of sedative hypnotic medications lower than ADSM but comparable to the general United States population.22 Thus, providers in the MHS are not necessarily more likely to prescribe pharmacologic therapy than civilian health care providers. This finding further substantiates multiple reports that disturbed sleep and insomnia are more prevalent in ADSM.5,6,10 Our study also found that women30 and older patients31 (who have higher rates of insomnia symptoms) in both ADSM and non-ADSM, had a higher prevalence of sleep medication usage. This finding of higher rates of sedative hypnotic medications in these two groups is consistent with prior reports.32 Regarding older patients, previous studies have reported more frequent and longer duration of sleep medication exposure in this age group and in those with various comorbid disorders.6 In the military, ADSM in the 45- to 64-year-old age group are likely senior leaders whose decisions carry substantial ramifications. The effect of sleep medications on their cognitive performance is unknown but requires further study.
Our findings are limited in that we did not specifically assess medication use nor did we restrict dispensing of the various medications by sleep indication; instead, we focused on the overall burden of dispensing in the MHS. We also did not assess over-the-counter medication or prescriptions that could have been obtained outside of the MHS for beneficiaries with other health insurance. Additionally, medications that were dispensed from military treatment facilities in deployed locations were not accessible as part of the extracted data. Thus, our prevalence of sedative hypnotic medications is likely an underestimation, especially as it pertains to ADSM.
Including all use of sedative hypnotics, irrespective of indication, likely resulted in some misclassification of patients who may be receiving these medications for reasons other than sleep disturbances. We tried to mitigate these occurrences by removing drugs that are predominantly used for other indications and rarely used for sleep disturbances as well as assessing sleep-related diagnosis prior to the start of an episode. Although fewer than 50% of all episodes in our study had a documented sleep-related diagnosis, patients may be receiving treatment for multiple conditions and indications that are not often documented at each encounter, potentially resulting in misclassification of sleep disorders.33 Additional practices in coding variations at MTFs versus non-MTFs may have resulted in differential coding for ADSM and non-ADSM, as ADSM are more closely monitored for conditions and treatments related to readiness. Irrespective of these limitations, our findings are insightful in that they provide additional context to the higher utilization often reported among ADSM—specifically, the need to further address acute use and focus on alternative treatment such as cognitive behavioral therapy for insomnia (CBTi) among the smaller subset of patients with chronic use.
In the military, it is understandable that there are many factors that contribute to sleep disturbances. Our findings showed a higher prevalence in ADSM with respect to non-ADSM, though primarily acute treatment. The effect of sedative hypnotic medications prescribing on duty performance and long-term health is currently unknown but requires further study. Notably, with the ongoing implementation of CBTi in the MHS, we expect a continued stabilization or a potential downward trend in prevalence of sedative hypnotics. However, without directed research to optimize the sleep of ADSM, they will remain at increased risk for disturbed sleep and chronic sleep disorders.
DISCLOSURE STATEMENT
All authors have seen and approved the final version of this manuscript. The authors report no conflicts of interest.
ABBREVIATIONS
- ADSM
active duty service members
- BZRA
benzodiazepine receptor agonist
- MHS
Military Health System
REFERENCES
- 1.National Institutes of Health. Sleep; National Institutes of Health State of the Science Conference statement on Manifestations and Management of Chronic Insomnia in Adults; June 13-15, 2005; 2005. pp. 1049–1057. [DOI] [PubMed] [Google Scholar]
- 2.Morin CM. Cognitive behavioral therapy for chronic insomnia: state of the science versus current clinical practices. Ann Intern Med. 2015;163(3):236–237. doi: 10.7326/M15-1246. [DOI] [PubMed] [Google Scholar]
- 3.Caldwell JA, Knapik JJ, Lieberman HR. Trends and factors associated with insomnia and sleep apnea in all United States military service members from 2005 to 2014. J Sleep Res. 2017;26(5):665–670. doi: 10.1111/jsr.12543. [DOI] [PubMed] [Google Scholar]
- 4.Lewis PE, Emasealu OV, Rohrbeck P, Hu Z. Risk of type II diabetes and hypertension associated with chronic insomnia among active component, U.S. Armed Forces, 1998-2013. MSMR. 2014;21(10):6–13. [PubMed] [Google Scholar]
- 5.Taylor DJ, Pruiksma KE, Hale WJ, et al. Prevalence, correlates, and predictors of insomnia in the US Army prior to deployment. Sleep. 2016;39(10):1795–1806. doi: 10.5665/sleep.6156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Troxel WM, Shih RA, Pedersen ER, et al. Sleep in the Military: promoting healthy sleep among U.S. Servicemembers. Rand Health Q. 2015;5(2):19. [PMC free article] [PubMed] [Google Scholar]
- 7.Luxton DD, Greenburg D, Ryan J, Niven A, Wheeler G, Mysliwiec V. Prevalence and impact of short sleep duration in redeployed OIF soldiers. Sleep. 2011;34(9):1189–1195. doi: 10.5665/SLEEP.1236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Seelig AD, Jacobson IG, Smith B, et al. Sleep patterns before, during, and after deployment to Iraq and Afghanistan. Sleep. 2010;33(12):1615–1622. doi: 10.1093/sleep/33.12.1615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gehrman P, Seelig AD, Jacobson IG, et al. Predeployment sleep duration and insomnia symptoms as risk factors for new-onset mental health disorders following military deployment. Sleep. 2013;36(7):1009–1018. doi: 10.5665/sleep.2798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McLay RN, Klam WP, Volkert SL. Insomnia is the most commonly reported symptom and predicts other symptoms of post-traumatic stress disorder in U.S. service members returning from military deployments. Mil Med. 2010;175(10):759–762. doi: 10.7205/milmed-d-10-00193. [DOI] [PubMed] [Google Scholar]
- 11.Seelig AD, Jacobson IG, Donoho CJ, Trone DW, Crum-Cianflone NF, Balkin TJ. Sleep and health resilience metrics in a large military cohort. Sleep. 2016;39(5):1111–1120. doi: 10.5665/sleep.5766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mental Health Advisory Team 9 (MHAT 9) Operation Enduring Freedom (OEF) 2013 Afghanistan. Homeland Security Digital Library website [PDF] [Accessed May 3, 2019]. https://www.hsdl.org/?abstract&did = 750301. Published October 10, 2013.
- 13.Wilt TJ, MacDonald R, Brasure M, et al. Pharmacologic treatment of insomnia disorder: an evidence report for a clinical practice guideline by the American College of Physicians. Ann Intern Med. 2016;165(2):103–112. doi: 10.7326/M15-1781. [DOI] [PubMed] [Google Scholar]
- 14.Poceta JS. Zolpidem ingestion, automatisms, and sleep driving: a clinical and legal case series. J Clin Sleep Med. 2011;7(6):632–638. doi: 10.5664/jcsm.1468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tannenbaum C, Paquette A, Hilmer S, Holroyd-Leduc J, Carnahan R. A systematic review of amnestic and non-amnestic mild cognitive impairment induced by anticholinergic, antihistamine, GABAergic and opioid drugs. Drugs Aging. 2012;29(8):639–658. doi: 10.1007/BF03262280. [DOI] [PubMed] [Google Scholar]
- 16.Rudisill TM, Zhu M, Kelley GA, Pilkerton C, Rudisill BR. Medication use and the risk of motor vehicle collisions among licensed drivers: A systematic review. Accid Anal Prev. 2016;96:255–270. doi: 10.1016/j.aap.2016.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ford ES, Wheaton AG, Cunningham TJ, Giles WH, Chapman DP, Croft JB. Trends in outpatient visits for insomnia, sleep apnea, and prescriptions for sleep medications among US adults: findings from the National Ambulatory Medical Care survey 1999-2010. Sleep. 2014;37(8):1283–1293. doi: 10.5665/sleep.3914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Meyer TE, Taylor LG, Xie S, et al. Neuropsychiatric events in varenicline and nicotine replacement patch users in the Military Health System. Addiction (Abingdon, England) 2013;108(1):203–210. doi: 10.1111/j.1360-0443.2012.04024.x. [DOI] [PubMed] [Google Scholar]
- 19.Capaldi VF, 2nd, Kim JR, Grillakis AA, Taylor MR, York CM. Insomnia in the military: application and effectiveness of cognitive and pharmacologic therapies. Curr Psychiatry Rep. 2015;17(10):85. doi: 10.1007/s11920-015-0622-9. [DOI] [PubMed] [Google Scholar]
- 20.Howden LM, Meyer JA. Age and Sex Composition: 2010. Washington, DC: U.S. Department of Commerce, Economics and Statistics Administration, U.S. Census Bureau; 2011. [Google Scholar]
- 21.Military OneSource website. 2014 Demographics: Profile of the Military Community [PDF] [Accessed May 3, 2019]. https://www.militaryonesource.mil/reports-and-surveys/demographic-profiles/2014-demographics-report. Published 2014.
- 22.Roth T. Insomnia: definition, prevalence, etiology, and consequences. J Clin Sleep Med. 2007;3(5 Suppl):S7–S10. [PMC free article] [PubMed] [Google Scholar]
- 23.Miller NL, Shattuck LG, Matsangas P. Sleep and fatigue issues in continuous operations: a survey of U.S. Army officers. Behav Sleep Med. 2011;9(1):53–65. doi: 10.1080/15402002.2011.533994. [DOI] [PubMed] [Google Scholar]
- 24.Mysliwiec V, Walter RJ, Collen J, Wesensten N. Military sleep management: an operational imperative. US Army Med Dep J. 2016;(2–16):128–134. [PubMed] [Google Scholar]
- 25.Pillai V, Cheng P, Kalmbach DA, Roehrs T, Roth T, Drake CL. Prevalence and predictors of prescription sleep aid use among individuals with DSM-5 insomnia: the role of hyperarousal. Sleep. 2016;39(4):825–832. doi: 10.5665/sleep.5636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ellis JG, Gehrman P, Espie CA, Riemann D, Perlis ML. Acute insomnia: current conceptualizations and future directions. Sleep Med Rev. 2012;16(1):5–14. doi: 10.1016/j.smrv.2011.02.002. [DOI] [PubMed] [Google Scholar]
- 27.Kantor ED, Rehm CD, Haas JS, Chan AT, Giovannucci EL. Trends in prescription drug use among adults in the United States from 1999-2012. JAMA. 2015;314(17):1818–1831. doi: 10.1001/jama.2015.13766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bertisch SM, Herzig SJ, Winkelman JW, Buettner C. National use of prescription medications for insomnia: NHANES 1999-2010. Sleep. 2014;37(2):343–349. doi: 10.5665/sleep.3410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sateia MJ, Buysse DJ, Krystal AD, Neubauer DN, Heald JL. Clinical practice guideline for the pharmacologic treatment of chronic insomnia in adults: an American Academy of Sleep Medicine clinical practice guideline. J Clin Sleep Med. 2017;13(2):307–349. doi: 10.5664/jcsm.6470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Green MJ, Espie CA, Benzeval M. Social class and gender patterning of insomnia symptoms and psychiatric distress: a 20-year prospective cohort study. BMC Psychiatry. 2014;14:152. doi: 10.1186/1471-244X-14-152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rodriguez JC, Dzierzewski JM, Alessi CA. Sleep problems in the elderly. Med Clin North Am. 2015;99(2):431–439. doi: 10.1016/j.mcna.2014.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pallesen S, Sivertsen B, Nordhus IH, Bjorvatn B. A 10-year trend of insomnia prevalence in the adult Norwegian population. Sleep Med. 2014;15(2):173–179. doi: 10.1016/j.sleep.2013.10.009. [DOI] [PubMed] [Google Scholar]
- 33.Schroeck JL, Ford J, Conway EL, et al. Review of safety and efficacy of sleep medicines in older adults. Clin Ther. 2016;38(11):2340–2372. doi: 10.1016/j.clinthera.2016.09.010. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.