Abstract
Study Objectives:
The aims of this study were to examine (1) relationships among implementing a bedtime routine, nighttime awakenings, and nighttime sleep duration in toddlers from low-income, minority families and (2) differences in maternal and household characteristics between mothers who did versus those who did not implement a nightly bedtime routine for their toddler.
Methods:
Data were collected from mothers of toddlers on maternal and household characteristics and toddler sleep, measured using the Children's HealthWatch Survey and the Extended Brief Infant Sleep Questionnaire (BISQ). A path analysis model was tested to investigate whether nighttime awakenings mediated the relation between implementing a bedtime routine and toddlers' nighttime sleep duration. Chi-square tests were conducted to examine differences in maternal and household characteristics (ie, maternal depressive symptoms, food, housing and energy insecurity) between mothers who did versus those who did not implement nightly bedtime routines over the past 2 weeks.
Results:
Implementing a bedtime routine was associated with longer toddler sleep duration through a decrease in nighttime awakenings (β = 5.04, 95% confidence interval = 0.61 to 11.35). More consistent sleep routine implementation was associated with fewer nighttime awakenings and longer sleep duration. Maternal depressive symptoms, housing insecurity, and food insecurity were associated with decreased likelihood of implementing a nightly bedtime routine.
Conclusions:
Maternal depressive symptoms, food insecurity, and household insecurity (factors associated with low socioeconomic status) may be associated with a negative sleep environment and poor toddler sleep quality, potentially because of decreased implementation of bedtime routines.
Commentary:
A commentary on this article appears in this issue on page 821.
Citation:
Covington LB, Rogers VE, Armstrong B, Storr CL, Black MM. Toddler bedtime routines and associations with nighttime sleep duration, and maternal and household factors. J Clin Sleep Med. 2019;15(6):865–871.
Keywords: bedtime routines, low-income, sleep deficiencies, toddlers
BRIEF SUMMARY
Current Knowledge/Study Rationale: Toddlers from minority, low-income families are at increased risk for deficient sleep and related poor health outcomes. Bedtime routines have been associated with improved sleep in toddlers of high-income, highly educated, Caucasian families, and should be examined among toddlers of low-income minority families to better address sleep deficiencies.
Study Impact: Given the key role sleep plays in the growth and development of young children, this study suggests that mothers of toddlers living in low socioeconomic conditions could benefit from strategies to promote bedtime routines and longer nighttime sleep. Broader public health measures are needed to improve screening and treatment of maternal mental health symptoms and to eliminate food and housing insecurity, especially among families with young children.
INTRODUCTION
Sleep is a determinant of well-being and health across the lifespan.1 In childhood, insufficient sleep duration and poor sleep quality are associated with social-emotional problems,2 poor cognitive functioning,3 and obesity.4 Children from low-income black families obtain less nighttime sleep, and have later bedtimes and poorer sleep routines compared to children from Caucasian families with high socioeconomic status (SES).1,5,6 Mechanisms of sleep deficiencies (ie, poor sleep quality and short sleep duration) in minority racial/ethnic and low SES populations are not well understood,7 but include environmental factors such as housing insecurity8 and unsafe neighborhoods,8,9 and social/economic factors such as food insecurity8 and lack of education.9 Toddlerhood is a critical time in the lifespan during which sleep-wake patterns and sleep consolidation are evolving, and bedtime routines are being established.10,11 Thus, a better understanding of maternal, social, and environmental conditions that put toddlers in minority, low-income families at increased risk for deficient sleep and related poor health outcomes may inform interventions to reduce sleep disparities and improve health.12
Implementing a nightly bedtime routine has been shown to improve sleep in toddlers.13 A bedtime routine is a regular set of activities (ie, reading, bath, teeth brushing) that occurs every night prior to bedtime.14 Cross-sectional, longitudinal, and intervention studies have shown associations between implementing a bedtime routine and earlier bedtimes, decreased sleep onset latency, reduced nighttime awakenings and longer sleep duration.15,16 The more nights per week a routine is implemented, the better the duration and quality of sleep.17 Associations between a bedtime routine and better sleep have mainly been examined among children living in high-income, highly educated, Caucasian families.14,18–23 Such associations, and the mechanisms supporting them, need to be investigated among low-income, minority families of toddlers if sleep deficiencies in these populations are to be addressed.
The few studies that have explored bedtime routines in low-income families have found that many families are unable to adhere to them on a nightly basis.24,25 Barriers that can interfere with the nightly implementation of bedtime routines include family stress, parental work hours, lack of time or space, household crowding, and lack of awareness of the association between bedtime routines and sleep onset and quality.6,25 Based on the social-ecological model,26 maternal (ie, educational status, mental health symptoms), social (ie, food insecurity), and environmental factors (ie, housing overcrowding) may contribute to differences in bedtime routine implementation and in sleep quality, and may be a potential point of intervention.1,12 Given the risks for deficient sleep and poor routine adherence among families in low-income circumstances,25 the identification of maternal, social, and environmental barriers associated with implementing a nightly bedtime routine can be useful in informing strategies to protect against deficient sleep.13
The aims of this study were twofold. The first aim was to examine relationships among implementing a bedtime routine, nighttime awakenings, and nighttime sleep duration through a mediation model. We hypothesized that toddlers who had more consistent routine implementation would experience fewer nighttime awakenings and ultimately have longer nighttime sleep duration; specifically, we proposed that nighttime awakenings would mediate the relation between bedtime routine and toddler nighttime sleep duration. Our second aim was to examine differences in maternal and household characteristics among mothers who did versus those who did not implement a nightly bedtime routine for their toddler. We hypothesized that mothers with limited education, depressive symptoms, and living in households with food, housing, and/or energy insecurities were less likely to implement a nightly bedtime routine than mothers without those characteristics.
METHODS
Procedures
Participants were enrolled from the Baltimore recruitment sites of Children's HealthWatch, an ongoing study that monitors the health and well-being of low-income infants and toddlers in the United States. Sites included an inner-city pediatric emergency department and a pediatric primary care clinic. Both sites serve families from urban low-income neighborhoods. This study was approved by the University of Maryland, Baltimore Institutional Review Board. All mothers provided written informed consent prior to data collection. Data were collected between March 2016 and June 2017.
Sample
Biological mothers of toddlers (age 12 to 47 months) were recruited to participate in the study (n = 130). Inclusion criteria for mothers were ability to speak English, reside in the same household as the toddler, and state residency. Mothers of acutely ill or injured toddlers were excluded.
Measures
Mothers completed the Children's HealthWatch survey, which included questions about maternal and household characteristics. Maternal characteristics included current employment (yes/no), marital status (married, single, cohabitation, widowed, separated, or divorced), and education level (some high school or less, high school graduate or GED, technical school or some college, college graduate, Master's level or higher). A 3-item depression screen was administered that has shown a sensitivity of 100%, specificity of 88%, and positive predictive value of 66% compared with the 8-item Rand screening instrument.27 The screen has been successfully used among the Children's HealthWatch sample in previous studies and its positive predictive value has been shown to improve in samples in which depression is prevalent (ie, low-income families).27–30 Mothers screened positive for depressive symptoms if they had a positive response to two of the three items.30
Household characteristics included food, housing, and energy insecurity. Food insecurity was measured by the 18-item US Household Food Security Scale.31,32 This scale has shown high internal consistency reliability with a Cronbach alpha ranging from .86 to .93.32 Households were classified as food insecure if they scored three or more affirmative responses on the 18-item scale, indicating they could not afford adequate nutritious food for active, healthy lives, and that this condition was a result of constrained resources.29,31,32 Housing insecurity was defined as the presence of the following three items: (1) living in a crowded home (> 2 people/bedroom), (2) doubling up (temporarily living with other people for economic reasons), and (3) moving ≥ 2 times per year.33–35 Energy insecurity was defined as a household experiencing at least one of the following conditions within the previous year: a threatened heat/electricity shutoff or refusal to deliver heating fuel, an actual heat/ electricity shutoff or refused delivery of heating fuel, use of the cooking stove as a source of heat, or an unheated/uncooled day because of inability to pay utility bills.29
Mothers also completed the Extended Brief Infant Sleep Questionnaire (BISQ). The BISQ is a measure of infant and toddler sleep and includes questions about daytime and nighttime sleep patterns and sleep-related behaviors over the past 2 weeks.23,36 It has been validated in children 5 to 30 months of age, with high (> 0.82) test–retest reliability.36 Using the BISQ, mothers reported how often they implemented a bedtime routine with their child (never, 1–2 nights/wk, 3–4 nights/ wk, 5–6 nights/wk, every night), and which of 12 activities (bath, TV, dinner/snack, play, brush teeth, read, bottle cuddle, say prayers, rocked run around, listen to music, sing songs, give drink) they implemented prior to bedtime (all applicable items could be checked). Through the BISQ, mothers also indicated if they shared a room or a bed with their toddler (yes/ no for both), the number of toddler nighttime awakenings and the number of times they occurred, and their toddler's usual bedtimes and wake times.
Statistical Analysis
Descriptive statistics were conducted on demographics, sleep variables, and bedtime routine activities. Prior to running the path analytic model to examine mediation, univariate relationships were examined between nighttime sleep duration, nighttime awakenings and toddler demographics, and maternal and household characteristics. The final path analysis model was run using a Poisson distribution to address the count nature of the nighttime awakenings variable.37 Bedtime routines was treated as a continuous variable (ie, number of nights a routine was implemented) and maximum likelihood estimation was used to address missing data. Relative model fit indicators (AIC and BIC) were used to determine the final parsimonious model. Mediation analyses were conducted using 1,000 bootstrapped samples.38 Bootstrapping is a statistical technique that reduces type II errors and does not assume normality for the indirect effect. Significant results are based on the 95% confidence interval not containing zero.38 Following completion of the mediation analyses, chi-square tests were conducted to test for differences in maternal and household characteristics between mothers who implemented a nightly bedtime routine and those who did not, to determine possible barriers to nightly bedtime routine implementation. Data were analyzed using IBM SPSS Statistics, Version 22.0 (IBM Corp, Armonk, New York, United States) and Mplus, Version 8.1 (Muthén & Muthén, Los Angeles, California, United States).
RESULTS
Sample Description
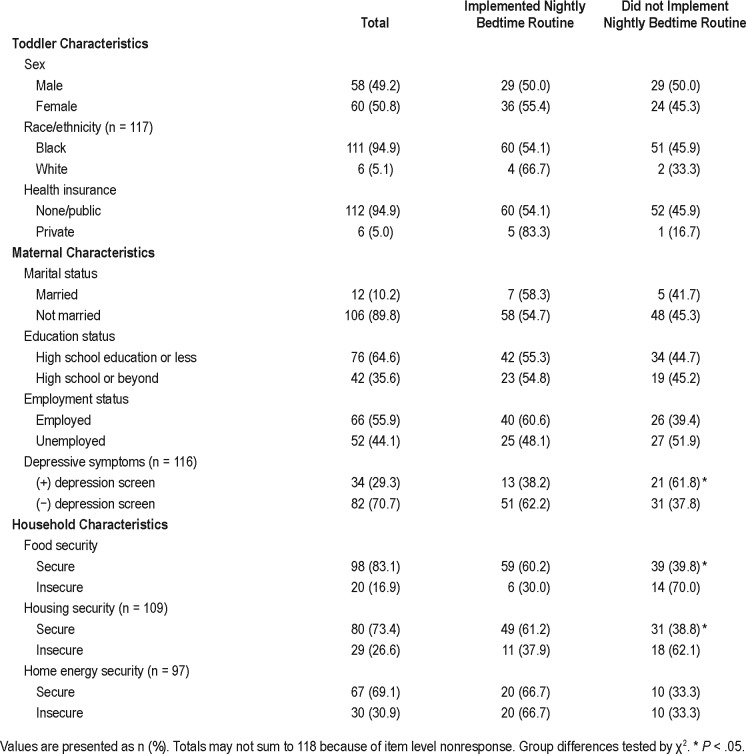
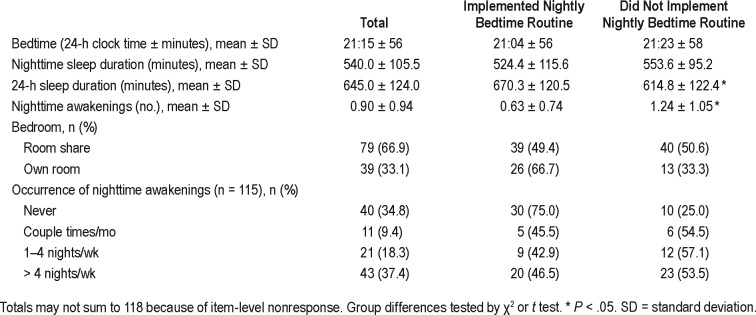
Of the 130 recruited mother-toddler dyads, 9 declined participation in the study, and 3 did not meet inclusion criteria. No participants withdrew from the study. The final sample included 118 mother-toddler dyads. Demographic characteristics of the sample are presented in Table 1. There was less than 5% missing data on all demographic variables, except for energy insecurity (20% missing) and housing insecurity (10% missing). The Little test of MCAR indicated that data were likely missing completely at random χ2(9) = 10.7, P = .30. Maximum likelihood estimation was used to account for missing data. Toddlers were mean age 28.4 months (standard deviation [SD] = 11, range = 12.5 to 47 months) and mothers were mean age 27 years (SD = 5, range = 19 to 44 years). Toddlers' sleep variables are displayed in Table 2, with less than 5% missing data on all sleep variables. Toddlers were reported to sleep an average of 9 hours per night (SD = 1.75 hours, range = 5 to 12 hours) and 10.8 hours per 24-hour period (SD = 2 hours, range = 5 to 16 hours). Almost all mothers reported having a bedtime routine (90%); however, only half (55%) reported implementing a nightly bedtime routine. Taking a bath (74%), watching TV (54%), and having dinner or a snack before bedtime (48%) were the most frequently reported routines.
Table 1.
Sample demographics of mother-toddler dyads (n = 118).
Table 2.
Toddler sleep characteristics (n = 118).
Relationship Between Implementing a Bedtime Routine, Nighttime Awakenings, and Nighttime Sleep Duration
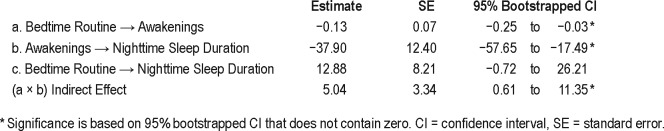
The direct relationship between number of nights implementing a bedtime routine and nighttime sleep duration was not significant (β = 11.8, standard error [SE] = 7.1, P = .10). Mediation was examined, because an association between an independent variable (implementing a bedtime routine) and a dependent variable (nighttime sleep duration) is not a precondition to mediation,38 and prior research has found implementation of a bedtime routine to be associated with decreased nighttime awakenings and increased nighttime sleep duration in toddlers.13 Multiple mediation models were run based on the results of the univariate analyses until the most parsimonious model was achieved (Table 3). Implementing a bedtime routine was directly associated with nighttime awakenings, such that for each additional night a bedtime routine was implemented in a week, the odds of a nighttime awakening was .88 times lower (β = −0.13, SE = 0.07, P = .04). Each nighttime awakening was associated with 38 minutes less nighttime sleep (β = −37.90, SE = 12.40, P = .002). There was a significant indirect effect of nighttime awakenings on the relationship between implementing a bedtime routine and nighttime sleep duration; each extra night of a bedtime routine was associated with 5 extra minutes of sleep via a reduction in nighttime awakenings (β = 5.04, 95% CI = 0.61 to 11.35) (Figure 1).
Table 3.
Regression estimates for mediation model.
Figure 1. The mediating effect of nighttime awakenings on the relation between bedtime routine implementation and nighttime sleep duration in toddlers.
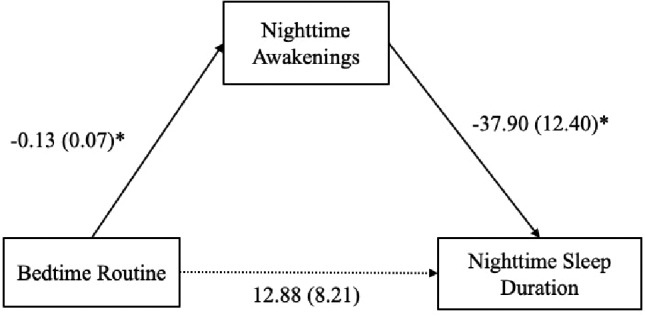
Solid lines indicate significant path, dashed line indicates non-significant path, * P < .05. Indirect effect of bedtime routines on nighttime sleep duration through nighttime awakenings (β = 5.04, 95% confidence interval = 0.61 to 11.35). Analysis is controlled for housing insecurity.
Differences in Implementing a Nightly Bedtime Routine Based on Maternal and Household Characteristics
Maternal and household characteristics by implementing a nightly bedtime routine versus not implementing a nightly bedtime routine are displayed in Table 1. Maternal depressive symptoms was the only maternal characteristic significantly associated with implementing a nightly bedtime routine (χ2(1) = 4.64, P < .05). Of mothers experiencing depressive symptoms, 62% did not implement a nightly bedtime routine. Two household characteristics, food insecurity and housing insecurity, differed significantly by nightly routine (χ2(1) = 6.13, P < .05) and χ2(1) = 4.68, P < .05, respectively). Seventy percent of mothers in food-insecure households and 62% of mothers in housing-insecure households reported not implementing a nightly bedtime routine.
DISCUSSION
There are two primary findings from this investigation. First, the indirect relationship between implementing a bedtime routine and longer sleep duration among toddlers occurred through having fewer nighttime awakenings. Second, maternal depressive symptoms, housing insecurity, and food insecurity were associated with decreased implementation of a nightly bedtime routine among mothers of toddlers. These findings extend prior research conducted primarily among toddlers in Caucasian families with high SES15 by finding similar associations and identifying a potential mechanism for the relationship between bedtime routine implementation and longer sleep duration, among toddlers in low-income families. Bedtime routines help toddlers calm down at night and create a nurturing, repetitive pattern that signals sleep and relaxation in young children.13 The calming and nurturing nature of a bedtime routine may help toddlers with sleep consolidation, possibly explaining the mechanism linking bedtime routines with reduced nighttime awakenings.13
As other studies have shown, nightly bedtime routines have been associated with earlier bedtimes, fewer number and duration of nighttime awakenings, longer nighttime sleep, and more total sleep in 24 hours, compared to bedtime routines implemented less regularly.17,18,21 Such positive effects have been seen in as few as 3 consecutive nights of a routine.14 If nightly routines begin in toddlerhood, better sleep may persist through childhood.17 Identifying factors related to implementing a nightly bedtime routine is pressing among low-income families who are less likely to do so as a result of barriers they may face regarding routines.25
In comparison, Hale et al. 200925 found that mothers who were Hispanic or black were less likely to implement a consistent bedtime routine, compared with mothers who were Caucasian, even after adjusting for maternal education, family structure, and other household characteristics.25 The present study extends those of Hale et al. 200925 by finding a relationship between maternal depressive symptoms and implementation of a nightly bedtime routine, with a higher proportion of mothers reporting depressive symptoms not implementing a nightly routine.
Our study also examined relationships between household characteristics and toddlers' sleep environment. Food, housing, and energy insecurity have all been associated with poor health outcomes in toddlers of low-income families, making it plausible for these household characteristics to have a similar relationship with sleep health.34,35,39 These findings add to the literature by suggesting that factors associated with low SES (presence of maternal depressive symptoms, food insecurity, and household insecurity) may negatively relate to toddlers' sleep environment and be associated with poor sleep quality due to decreased likelihood of implementing a nightly bedtime routine.
Implementing a consistent bedtime routine has also been associated with health benefits that extend beyond sleep outcomes. Several studies have found an association between nightly bedtime routines and improved emotional behavioral regulation and child mood.13 For example, reading at bedtime has been associated with positive cognitive outcomes and language development in young childhood,40 and hygiene routines such as taking a bath and brushing teeth can directly protect young children from illness.41,42 Such positive health outcomes associated with bedtime routine implementation may be particularly beneficial to at-risk, impoverished families. Implementing healthy nightly routines may serve as a defense against the stresses families face on a daily basis and foster positive health outcomes.13
Limitations
The findings of this study should be considered in light of its limitations. Analyses were based on maternal report of toddler sleep using the BISQ. Prior research has found that mothers often overestimate toddler sleep duration and underestimate their number of awakenings at night.43,44 We also lacked the ability to measure day-to-day sleep variability. Using the BISQ, mothers reported their toddler's average sleep duration, quality, and routines based on the past 2 weeks. There is no way of knowing whether these reports of sleep were typical for the toddler, or how much their day-to-day sleep patterns might vary. Moreover, it is unclear which specific routines, if any, are associated with decreased nighttime awakenings or increased sleep duration among this low-income population. Such relationships were explored and no signification associations were found. It is possible that the specific routine may not be as important as the consistency of the routine, or more likely, significant associations were not detected because the study was underpowered. Based on a Monte Carlo power simulation with our results, we had 49% power to detect a signifi-cant effect, if one existed. Future studies should examine these associations with a larger sample size to ensure that significant effects, if they exist, can be detected. In regard to the Children's HealthWatch survey, housing characteristics and maternal characteristics, such as depressive symptoms, have been related to children's health indicators, but may be subject to reporting bias.35 Additionally, our findings have limited generalizability to toddlers in general, given the sample was almost entirely low-income and black children.
There are also limitations to the mediation analysis. The relationship between having a bedtime routine and toddler nighttime sleep duration was not direct, but was mediated through nighttime awakenings. However, it is not uncommon for an absence of a direct relationship in a mediation model.38 Given the cross-sectional nature of surveys, causal relationships cannot be identified.33,35
Finally, all study participants were low-income, meaning that the role of poverty could not be examined. It is possible that poverty is driving the underlying mechanisms of relationships identified in this study. Future research is needed to examine the role of poverty to develop tailored programs and interventions surrounding sleep duration and quality in toddlers of low-income families.12
Clinical Implications
The results of this study have major clinical implications. During infancy, providers can strategize with families on how to implement a nightly bedtime routine into their schedule.13 The American Academy of Pediatrics recommends that providers ask families about toddler sleep duration and bedtime routine implementation at yearly check-ups.45 These questions could address the time prior to bedtime, the frequency that bedtime routines are implemented, and barriers to implementation. Low SES families may face multiple barriers to nightly routine implementation, such as overcrowded households,6 and parents working multiple jobs or shiftwork. As we found, only 55% of families with a bedtime routine implemented it every night. Providers can help families identify tailored routines that can be adapted in their family environment, such as an abbreviated routine for parents who work late.13 Helping families incorporate nightly bedtime routines into their schedules can be emphasized by multiple health care providers, including dentists, lactation consultants, pediatric psychologists, and preschool and daycare systems.13
Future Research
Future studies are needed to better understand sleep deficiencies among toddlers and to consider effects of the multifactorial components of SES, including maternal and household characteristics. Such characteristics need to be considered when counseling families regarding nightly bedtime routines. A dose-dependent bedtime routine intervention17 could be examined to determine the benefits of a nightly bedtime routine compared to a routine implemented less often among low-income families. Additionally, future research could examine how specific components of bedtime routines contribute to decreased awakenings and longer sleep duration as they may be just as important as how often the routine is being implemented.22,46 Objective measures of sleep such as actigraphy can eliminate the potential inaccuracies of relying on caregiver report.43 Longitudinal study designs would allow for the examination of potential causal pathways and mechanisms contributing to sleep definciencies.12 Ultimately, identifying specific routines that are feasible to implement nightly in poor sleep environments, and that best predict decreased awakenings and increased sleep duration, will not only further support the relationships identified in this study, but will also potentially lead to better sleep outcomes in this underresourced population.
DISCLOSURE STATEMENT
This study was conducted at University of Maryland Medical Center. All authors have reviewed and approved this manuscript. Data collection was supported in part by funding through Children's HealthWatch donors, which are listed at http://www.childrenshealthwatch.org. The authors report no conflicts of interest.
ABBREVIATIONS
- BISQ
Extended Brief Infant Sleep Questionnaire
- SES
socioeconomic status
REFERENCES
- 1.El-Sheikh M, Bagley EJ, Keiley M, Elmore-Staton L, Chen E, Buckhalt JA. Economic adversity and children's sleep problems: Multiple indicators and moderation effects. Health Psychol. 2013;32(8):849–859. doi: 10.1037/a0030413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hysing M, Sivertsen B, Garthus-Niegel S, Eberhard-Gran M. Pediatric sleep problems and social-emotional problems. A population-based study. Infant Behav Dev. 2016;42:111–118. doi: 10.1016/j.infbeh.2015.12.005. [DOI] [PubMed] [Google Scholar]
- 3.Turnball K, Reid GJ, Morton JB. Behavioral sleep problems and their potential impact on developing executive function in children. Sleep. 2013;36(7):1077–1084. doi: 10.5665/sleep.2814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Miller MA, Kruisbring M, Wallace J, Ji C, Cappucino FP. Sleep duration and incidence of obesity in infants, children and adolescents: a systematic review and meta-analysis of prospective studies. Sleep. 2018;41(4) doi: 10.1093/sleep/zsy018. [DOI] [PubMed] [Google Scholar]
- 5.Jones HD, Ball H. Exploring socioeconomic differences in bedtime behaviours and sleep duration in English preschool children. Infant Child Dev. 2014;23(5):518–531. doi: 10.1002/icd.1848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bagley E, Kelly R, Buckhalt JA, El-Sheikh M. What keeps low-SES children from sleeping well: The role of presleep worries and sleep environment. Sleep Med. 2015;16(4):496–502. doi: 10.1016/j.sleep.2014.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Laposky AD, Cauter EV, Diez-Roux AV. Reducing health disparities: The role of sleep deficiency and sleep disorders. Sleep Med. 2016;18:3–6. doi: 10.1016/j.sleep.2015.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Grandner MA, Williams NJ, Knutson KL, Roberts D, Jean-Louis G. Sleep disparity, race/ethnicity, and socioeconomic position. Sleep Med. 2016;18:7–18. doi: 10.1016/j.sleep.2015.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fuller-Rowell TE, Curties DS, El-Sheikh M, Chae DH, Boylon JM, Ryff CD. Racial disparities in sleep: the role of neighborhood disadvantage. Sleep Med. 2016;27–28:1–8. doi: 10.1016/j.sleep.2016.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yu X, Sadeh A, Simon LH, Mindell JA, Li AM. Parental behaviors and sleep/wake patterns of infants and toddlers in Hong Kong, China. World J Pediatr. 2017;13(5):496–502. doi: 10.1007/s12519-017-0025-6. [DOI] [PubMed] [Google Scholar]
- 11.Bonuck KA, Blank A, True-Felt B, Chervin R. Promoting sleep health among families of young children in head start: Protocol for a social-ecological approach. Prev Chronic Dis. 2016;13(E121):1–8. doi: 10.5888/pcd13.160144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Guglielmo D, Gazmararian JA, Chung J, Rogers AE, Hale L. Racial/ethnic disparities in US school-aged children and adolescents: a review of the literature. Sleep Health. 2018;4(1):68–80. doi: 10.1016/j.sleh.2017.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mindell JA, Williamson AA. Benefits of a bedtime routine in young children: Sleep, development and beyond. Sleep Med Rev. 2018;40:93–108. doi: 10.1016/j.smrv.2017.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mindell JA, Leichman ES, Lee C, Williamson AA, Walters RM. Implementation of a nightly bedtime routine: how quickly do things improve? Infant Behav Dev. 2017;49:220–227. doi: 10.1016/j.infbeh.2017.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mindell JA, Williamson AA. Benefits of a bedtime routine in young children: Sleep, development and beyond. Sleep Med Rev. 2017:1–16. doi: 10.1016/j.smrv.2017.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Allen SL, Howlett MD, Coulombe JA, Corkum PV. ABCs of SLEEPING: a review of the evidence behind pediatric sleep practice recommendations. Sleep Med Rev. 2016;29:1–14. doi: 10.1016/j.smrv.2015.08.006. [DOI] [PubMed] [Google Scholar]
- 17.Mindell JA, Li AM, Sadeh A, Kwon R, Goh DYT. Bedtime routines for young children: A dose-dependent association with sleep outcomes. Sleep. 2015;38(5):717–722. doi: 10.5665/sleep.4662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mindell JA, Telofski LS, Wiegand B, Kurtz ES. A nightly bedtime routine: Impact on sleep in young children and maternal mood. Sleep. 2009;32(5):599–606. doi: 10.1093/sleep/32.5.599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mindell JA, Leichman ES, Puzino K, Walters R, Bullar B. Parental concerns about infant and toddler sleep assessed by a mobile app. Behav Sleep Med. 2015;13(5):359–374. doi: 10.1080/15402002.2014.905475. [DOI] [PubMed] [Google Scholar]
- 20.Mindell JA, Du Mond CE, Sadeh A, Telofski LS, Kulkarni N, Gunn E. Efficacy of an internet-based intervention for infant and toddler sleep disturbances. Sleep. 2011;34(4):451–458. doi: 10.1093/sleep/34.4.451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mindell JA, Du Mond C, Sadeh A, Telofski LS, Kulkarni N, Gunn E. Long-term efficacy of an internet-based intervention for infant and toddler sleep disturbances: one year follow-up. J Clin Sleep Med. 2011;7(5):507–511. doi: 10.5664/JCSM.1320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Staples AD, Bates JE, Petersen IT. Bedtime routines in early childhood: Prevalence, consistency and associations with nighttime sleep. Monogr Soc Res Child Dev. 2015;80(1):141–159. doi: 10.1111/mono.12149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sadeh A, Mindell JA, Luedtke K, Wiegand B. Sleep and sleep ecology in the first 3 years: a web-based study. J Sleep Res. 2009;18(1):60–73. doi: 10.1111/j.1365-2869.2008.00699.x. [DOI] [PubMed] [Google Scholar]
- 24.Yoo J, Slack KS, Holl JL. The impact of health-promoting behaviors on low-income children's health: a risk and resilience perspective. Health Soc Work. 2010;34(2):133–143. doi: 10.1093/hsw/35.2.133. [DOI] [PubMed] [Google Scholar]
- 25.Hale L, Berger LM, LeBourgeois MK, Brooks-Gunn J. Social and demographic predictors of preschoolers' bedtime routines. J Dev Behav Pediatr. 2009;30(5):394–402. doi: 10.1097/DBP.0b013e3181ba0e64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bronfenbrenner U. Ecological systems theory. In: Vasta R, editor. Six Theories of Child Development: Revised Formulations and Current Issues. London, England: Jessica Kingsley Publishers; 1992. pp. 187–249. [Google Scholar]
- 27.Kemper KJ, Babonis TR. Screening for maternal depression in pediatric clinics. Am J Dis Child. 1992;146(7):876–878. doi: 10.1001/archpedi.1992.02160190108031. [DOI] [PubMed] [Google Scholar]
- 28.Black MM, Quigg AM, Cook J, et al. WIC participation and attenuation of stress-related health risks of household food insecurity and caregiver depressive symptoms. Arch Pediatr Adolesc Med. 2012;166(5):444–451. doi: 10.1001/archpediatrics.2012.1. [DOI] [PubMed] [Google Scholar]
- 29.Chilton M, Black MM, Berkowitz C, et al. Food insecurity and risk of poor health among US-Born children of immigrants. Am J Public Health. 2009;99(3):556–562. doi: 10.2105/AJPH.2008.144394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Casey P, Goolsby S, Berkowitz C, et al. Maternal depression, changing public assistance, food security and child health status. Pediatrics. 2004;113(2):298–304. doi: 10.1542/peds.113.2.298. [DOI] [PubMed] [Google Scholar]
- 31.Bickel G, Nord M, Price C, Hamilton W, Cook J. Guide to Measuring Household Food Security, Revised 2000. Alexandria, VA: U.S. Department of Agriculture, Food and Nutrition Service; 2000. [Google Scholar]
- 32.Nord M, Andrews M, Carlson S. Household Food Security in the United States, 2007: Economic Research Report. Washington, DC: United States Department of Agriculture, Economic Research Service; 2008. Economic Research Report Number 66. [Google Scholar]
- 33.Joyce K, Breen A, Ettinger de Cuba S, et al. Household hardships, public programs, and their associations with the health and development of very young children: insights from Children's HealthWatch. J Appl Res Child. 2012;3(1) [Google Scholar]
- 34.Cutts DB, Meyers AF, Black MM, et al. US housing insecurity and the health of very young children. Am J Public Health. 2011;101(8):1508–1514. doi: 10.2105/AJPH.2011.300139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sandel M, Sheward R, Ettinger De Cuba S, et al. Unstable housing and caregiver and child health in renter families. Pediatrics. 2018;141(2):e20172199. doi: 10.1542/peds.2017-2199. [DOI] [PubMed] [Google Scholar]
- 36.Sadeh A. A brief screening questionnaire for infant sleep problems: validation and findings for an internet sample. Pediatrics. 2004;113(6):e570–e577. doi: 10.1542/peds.113.6.e570. [DOI] [PubMed] [Google Scholar]
- 37.Muthén LK, Muthén BO. MPlus User's Guide. 8th ed. Los Angeles, CA: Muthén & Muthén; 1998–2010. [Google Scholar]
- 38.Hayes AF. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. New York, NY: Guilford Press; 2013. [Google Scholar]
- 39.Frank DA, Casey PH, Black MM, et al. Cumulative hardship and wellness of low-income young children: Multisite surveillance study. Pediatrics. 2010;125(5):e1115–e1123. doi: 10.1542/peds.2009-1078. [DOI] [PubMed] [Google Scholar]
- 40.Zuckerman B, Khandekar A. Reach out and read: evidence based approach to promoting early child development. Curr Opin Pediatr. 2010;22(4):539–544. doi: 10.1097/MOP.0b013e32833a4673. [DOI] [PubMed] [Google Scholar]
- 41.Blume-Peytavi U, Hauser M, Stamatas GN, Pathirana D, Bartels NG. Skin care practices for newborns and infants: review of the clinical evidence for best practices. Pediatr Dermatol. 2012;29(1):1–14. doi: 10.1111/j.1525-1470.2011.01594.x. [DOI] [PubMed] [Google Scholar]
- 42.Tinanoff N, Reisine S. Update on early childhood caries since the surgeon general's report. Acad Pediatr. 2009;9(6):396–403. doi: 10.1016/j.acap.2009.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mindell JA, Meltzer LJ, Carskadon MA, Chervin RD. Developmental aspects of sleep hygiene: findings from the 2004 National Sleep Foundation Sleep in America poll. Sleep Med. 2009;10(7):771–779. doi: 10.1016/j.sleep.2008.07.016. [DOI] [PubMed] [Google Scholar]
- 44.Mindell JA, Sadeh A, Wiegand B, How TH, Goh DY. Cross-cultural differences in infant and toddler sleep. Sleep Med. 2010;11(3):274–280. doi: 10.1016/j.sleep.2009.04.012. [DOI] [PubMed] [Google Scholar]
- 45.Ersu R, Boran P, Akın Y, Bozaykut A, Ay P, Sami A. Effectiveness of a sleep education program for pediatricians. Pediatr Int. 2016;59(3):280–285. doi: 10.1111/ped.13147. [DOI] [PubMed] [Google Scholar]
- 46.Hale L, Berger LM, LeBourgeois MK, Brooks-Gunn J. A longitudinal study of preschoolers' language-based bedtime routines, sleep duration, and well-being. J Fam Psychol. 2011;25(3):423–433. doi: 10.1037/a0023564. [DOI] [PMC free article] [PubMed] [Google Scholar]