Abstract
Objective:
A lack of understanding of the causes of attrition in longitudinal studies of older adults may lead to higher attrition rates and bias longitudinal study results. In longitudinal epidemiological studies of Alzheimer’s disease and related dementias, high rates of attrition may cause a systematic underestimation of dementia prevalence and skew the characterization of the disease. This can compromise the generalizability of the study results and any inferences based on the surviving sample may grossly misrepresent the importance of the risk factors for dementia. The National Institute on Aging outlined a National Strategy for Recruitment and Participation in Alzheimer’s Disease Clinical Research to address this problem, providing evidence of the magnitude of this problem.
Method:
To explore predictors of attrition, this study examined the National Alzheimer’s Coordinating Center (NACC) Uniform Data Set; a repository of observations of older adults spanning 11 years, using survival analysis. Four samples were examined: the full sample (n=30,433), the alive subsample excluding those who died (n=24,231), the MRI sample (participants with complete MRI data (n=1,104)), and the alive MRI subsample (participants with MRI data excluding those who died (n=947)).
Results:
Worsening cognitive impairment, neuropsychiatric symptoms, and difficulty with functional activities predicted attrition, as did lower hippocampal volume in the MRI subsample. Questionable co-participant reliability and an informant other than a spouse also increased risk of attrition.
Discussion:
Special considerations exist in recruiting and retaining older adults in longitudinal studies and results of baseline psychological, functional, and cognitive functioning should be used to identify targeted retention strategies.
Keywords: Alzheimer’s disease, attrition, dementia, drop-out, longitudinal study, neuropsychiatric symptoms, hippocampal volume, functional difficulties
Introduction
Attrition is one of the main challenges in longitudinal studies. It refers to the drop out of participants during the course of a study, including drop outs between data collection points or study waves and before the completion of a study [1, 2]. Study participants may miss one wave of a study and return at a later point or may miss one testing point and never return [3]. The latter, which is called terminal attrition, is more common and is the topic of attrition in this paper. Attrition is usually non-random and can threaten the internal and external validity of a study [2, 4, 5]. If attrition creates a difference in group composition and associations between variables of a sample, it poses a threat to internal validity [1]. If attrition causes a change in characteristics of participants in the original sample compared to the subsequent waves, it poses a threat to external validity [1, 2, 6]. These threats to validity are called attrition bias and can change the findings in a study [1]. Therefore, it is important to understand the causes of attrition, especially those that may be preventable, in order to increase the validity and generalizability of empirical studies in different groups.
Attrition could occur due to an array of reasons including refusal for participation, lack of interest, premature withdrawal, failed contact, incompatibility with the research team, or incapability of participation due to illness, injury, or death [2, 4, 7]. Attrition could be higher, and a cause of concern, in studies on specific groups such as the population under investigation in this study, older adults. In longitudinal studies on older adults, high attrition rates due to death is a cause of concern and can create a challenge in exploring the aging process in later stages of life [8–10]. For instance, 38% attrition was reported due to death or mental or physical incapacitation in Feng et al.’s [9] longitudinal study (between 1970-2005) among older adults (mean age at baseline= 64.07, SD= 5.65); close to 22% attrition due to death was reported in the second wave (between 3.3 to 4.2 years after the baseline) and around 26% in the third wave (between 3.7 to 4.4 years after the second wave) of Jacomb et al.’s [10] study among older adults (aged 70 or older at the baseline); and around 20% attrition due to death among older adults (mean age at baseline= 77.9, SD= 6.8) was reported in a 2-year study by Coley et al. [11].
Sociodemographic characteristics of the participants may also influence attrition in longitudinal studies, specifically on older adults. For instance, in the Maastricht Aging Study among adults aged 49 and older at baseline, those who were lost in the three-year follow-up were more often females, had poorer results on neurocognitive tests at baseline, and had lower levels of educational attainment [12]. Similarly, in the study by Jacomb et al. [10] on predictors of older adults’ refusal to participate in a longitudinal study, non-participants were found to have lower years of education and lower cognitive performance scores. Besides gender and education, race and age of older adults are among the socio-demographic characteristics found to be associated with attrition rates in longitudinal studies [13–16].
The literature also supports an association between mental and physical health of older adult participants, specifically adults living with cognitive impairment and dementia, and attrition in longitudinal studies. For example, in Coley et al.’s [11] study on older adults living with mild to moderate Alzheimer disease, institutionalization, loss of autonomy, and increasing caregiver burden were among the major reasons unrelated to mortality that led to sample exit. Similarly, in Tyas et al.’s [17] study on a sample of aging and dementia population, attrition was associated with institutionalization. Moreover, Sliwinski et al. [18] found an association between time to drop out and accelerating memory loss among a sample of older adults. In line with these findings, loss of autonomy, institutionalization, illness, lower level of functioning ability, increased cognitive impairment or low cognitive status, and brain MRI findings indicating higher future risk of dementia (white matter lesion volume and hippocampal volume) are also found to be associated with attrition in longitudinal studies among older adults [11, 13, 15, 19–21].
Additionally, our review of the literature found inconsistent results in previous studies regarding an association between neuropsychiatric symptoms among older adults living with dementia and attrition in longitudinal studies. Steinberg et al [22] found a correlation between neuropsychiatric symptoms such as delusions, hallucinations, agitation/aggression, anxiety, disinhibition, and irritability among a cohort of older adults living with dementia and attrition. Another study among a similar population found neuropsychiatric symptoms of patients who fulfilled total follow-up were similar compared to those individuals who had died or were discontinued from the study [23]. We also retrieved studies suggesting a correlation between attrition and the relationship of the caregiver and older adults. In these studies, drop out was higher among older adult patients cared for by caregiver not related to the patient [11, 19].
A lack of understanding regarding what causes participants to drop out will lead to higher attrition rates, and this can bias the overall results of a study. In large-scale longitudinal epidemiological studies of dementia, high rates of attrition may cause a systematic underestimation of dementia prevalence. This underestimation can compromise the generalizability of the study results. Therefore, any inferences made on the surviving sample may grossly misrepresent the importance of the risk factors for dementia, which may have been identified. In the current study, we aim to expand on the previous studies in the field to better understand potential causes of attrition and magnitude of this problem in longitudinal studies, specifically epidemiological studies of Alzheimer’s disease among older adults. In this context, we utilized the National Alzheimer’s Coordinating Center’s Uniform Data Set to explore three hypotheses informed by the findings of our literature review.
We hypothesized that attrition in our sample is associated with the sociodemographic characteristics of the participants including their sex, age, education, and race. Moreover, we hypothesized that attrition in the sample is correlated with mental health of the participants, specifically their neurological and behavioral status based on: the Clinical Dementia Rating (CDR) global score (0, 0.5, 1, 2, and 3); cognitive status (impaired but not diagnosed with mild cognitive impairment [MCI], diagnosed with MCI, and diagnosed with dementia); depression based on the Geriatric Depression Scale (GDS); and finally, neuropsychiatric symptoms (NPSs, delusion, hallucination, agitation, depression, anxiety, elation, apathy, disinhibition, irritability, motor disturbance, nighttime disturbance, and appetite disturbance) based on the Neuropsychiatric Inventory Questionnaire (NPI-Q). Furthermore, we hypothesized that attrition in the sample is correlated with the physical health of the participants, including functional activity status based on the Functional Assessment Questionnaire (FAQ) or Functional Assessment Scale (FAS) (0-10: normal ability, 11-20: needs assistance, 20-30: dependent) and white matter and hippocampal volumes based on the MRI results. Additionally, we hypothesized that attrition in the sample is associated with co-participant relation (spouse, child, sibling, other relative, friend or someone known, paid caregiver, and others) and reliability defined based on the clinician’s judgment. In order to examine these hypotheses, we used survival analysis [24]. For this analysis, we created subsamples excluding participants who died during data collection, as we expected a major attrition due to death in the utilized dataset based on the reviewed literature.
Method
Data
Data of this study was obtained from the National Alzheimer’s Coordinating Center’s (NACC) Uniform Data Set (UDS), representing the years 2005 to 2016. Four samples were studied based on the obtained data from the NACC UDS: 1) full sample (n=30,433), 2) the alive subsample: a subsample based on the full sample excluding participants who died during the course of the study (n=24,231), 3) the MRI sample: a sample consisted of participants who had MRI information (n=1,104), and 4) the alive MRI subsample: a subsample consisted of participants who had MRI information, excluding those who died (n=947). The specific MRI data of interest in this study were white matter hyperintensities and hippocampal volume [25].
Information in the NACC UDS data set is obtained from 35 Alzheimer’s Disease Centers (ADCs) at a baseline visit and subsequent annual evaluations. At each visit, the data was obtained from the participant, a trusted co-participant (also known as an informant), qualified clinicians (psychometricians, neuropsychologists, neurologists, psychiatrists, internists, and radiologists) and from laboratories, which provide results from blood, cerebrospinal fluid (CSF), and autopsied brain samples. Each participant and their co-participant provided a variety of demographic and social history data, as well as medical history and use of medications in the NACC UDS dataset.
Measures
Death.
Mortality was included as a categorical variable, in which 1 indicated a person had died, and 0 indicated that they are still alive. Based on the death in the sample, we generated two subsamples to review attrition factors unrelated to mortality. Excluding the deaths from the full sample, we generated the alive subsample. Moreover, excluding the deaths from the MRI sample (consisted of participants who had MRI information), we created the alive MRI subsample.
Sociodemographic characteristics.
To test our first hypothesis, we measured the associations between attrition and socio-demographic characteristics of the participants. These characteristics include sex, age, number of years of education, and race. Age and number of years of education (continuous from 0-36 years, where 12 years = high school / GED, 16 = Bachelor’s degree, 18 = master’s degree, 20 = doctorate) were continuous variables, and sex and race (white non-Hispanic [reference group], black non-Hispanic, Hispanic, other) were categorical.
Mental and physical health.
To test our second hypothesis, we measured the associations between attrition and physical and mental health of the participants in our sample. Participants were assessed using a variety of rating scales for mental and physical health, including the Clinical Dementia Rating scale [26], an adapted version of the Functional Activities Questionnaire [27], and the Neuropsychiatric Inventory Questionnaire [28]. Radiologists and pathologists at some ADCs voluntarily provide data from MRIs, and amyloid PET scans, which NACC stores in a repository. At the discretion of the individual ADCs, laboratory and imaging tests are obtained from participants to aid in diagnostic determinations and provide information about medical illnesses when completing UDS forms. Clinicians obtain data from psychometric, medical, neurological, and psychiatric evaluations as well as diagnostic information. A diagnosis regarding cognitive status is often determined by a group of two or more clinicians, neuropsychologists, or the examining physician [25].
The first mental health-related predictor for attrition in this study was the CDR global score. The CDR takes into account six domains, which are scored individually based on the co-participant report and neurological and behavioral exam of the participants. The six domains include memory, orientation, judgment and problem-solving, community affairs, home and hobbies, and personal care [26, 29]. Each domain is rated based on the participant’s cognitive (not physical) ability to function in these areas. Once an individual score is derived in each domain, an algorithm can be used to compute the global score [29]. The overall score of the CDR pertains to a certain cognitive status such that 0 = normal, 0.5 = very mild dementia, 1 = mild dementia, 2 = moderate dementia, and 3 = severe dementia. Therefore, this predictor in this study was a categorical variable with four categories (CDR global score equal to 0 [reference group], 0.5, 1, 2, and 3).
The second mental health-related predictor for attrition in this study was cognitive status. Physicians and neuropsychologists at individual ADCs diagnosed the cognitive status of the participants based on the guidelines set forth by McKhann et al. [30] through a consensus diagnosis process, or by a single clinician. Cognitive status in this study was a categorical variable with four categories: normal cognition (reference group) impaired but not diagnosed with MCI, diagnosed with MCI, and diagnosed with dementia.
Depression was the third mental health-related predictor for attrition in this study. This predictor was based on the total score of the short version of the GDS[31]. The short version of the GDS is a 15-item self-report questionnaire with yes or no answers. Answering yes to 10 of the questions in the short version of the GDS indicates the presence of depression while answering no to the other five is indicative of depression. Therefore, depression in this study was a categorical variable separating depressed adults from others (reference group).
Moreover, in this study, we reviewed the participants’ NPSs as the fourth mental health-related predictor for attrition. In the utilized dataset for this study, NPSs were assessed using the NPI-Q [28]. This questionnaire assesses presence or absence of a problematic behavior in 12 categories based on an interview with co-participants: delusion, hallucination, agitation, depression, anxiety, elation, apathy, disinhibition, irritability, motor disturbance, nighttime disturbance, and appetite disturbance.
Functional activity status of older adults was a physical health-related predictor for attrition. This predictor was defined based on the FAQ or FAS measures. The FAQ was designed based on the Functional Activities Questionnaire [27], which later was adapted to FAS in the UDS version 3. The FAS is a 10-item tool assessing difficulty or a need for help in conducting daily activities based on the co-participant report. The 10 items of the questionnaire include paying bills; assembling records and business affairs; shopping alone for home goods or clothes; playing a game of skill or working on hobbies; heating water or making coffee; preparing a balanced meal; tracking current events; following and understanding a TV program, magazine or book; and traveling, driving, or taking public transportation. Each item could be scored from 0 to 3. Score 3 indicates that the individual is completely dependent on someone else for that task; 2 shows that the person has difficulty in conducting the task but can do it by him or herself; 1 indicates that the individual needs assistance; and 0 shows normal ability. In this study, functional activity is a categorical variable based on the total score of the FAS (0-10: normal ability [reference group]; 11-20: needs assistance; 20-30: dependent). Furthermore, we reviewed the participants’ MRI results, specifically their white matter and hippocampal volumes as another physical health-related predictor for attrition in this study. Both of these predictors were continuous variables.
Co-participant relation and reliability.
We also included information regarding the co-participant’s relationship to the participant as a predictor for attrition, given that a co-participant is required to participate in NACC studies. The assumption was that the co-participant would provide reminders for appointments, travel assistance, and potentially motivation to attend. The co-participant as a predictor in this study was a categorical variable and included the spouse (reference group); child; sibling; other relative; friend, neighbor, or some known through family, friends, work or community; paid caregiver, health care provider, or clinician; and others. Moreover, the reliability of the co-participant was included in this study as a predictor for attrition, and this categorical variable was based on the clinician’s judgment.
Data Analysis
In the analyses, a failure event was defined as a participant’s exit from the study. An exit was defined as the participant’s last visit occurring at least three years before the last survey observation in 2016. The rationale for constraining the analytic sample in this fashion first started as a calculation of the intervals between any two consecutive visits for the same person. We estimated (calculated) that for 99% of people, the likelihood of their return visit following their last visit was less than one percent, especially if someone did not attend a study visit or observation for three years. While the participants had the opportunity for additional visits, the fact that they did not return for a follow-up visit means their exit was the result of circumstances unrelated to lack of additional opportunities for follow-up observations (such as a study ending) or death. Right censoring was used to account for participants whose last visit occurred during the last three years of collected information, as their visits or attrition may occur in future visits but are unaccounted for at the present. Time zero was equal to the participant’s first observation (visit number 1), and time was measured in visits. There was a range of 1 to 10 visits for all counted participants. Outcomes are displayed as hazard ratios. The statistical program STATA [32] was utilized for the analyses, and a p-value < 0.05 was considered statistically significant.
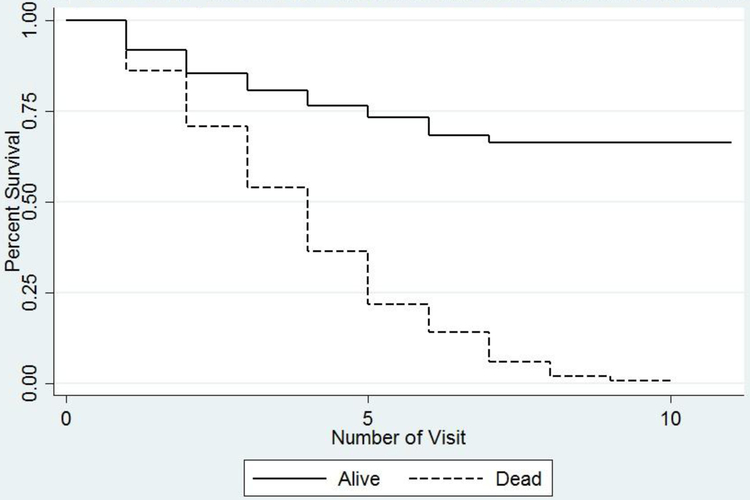
Univariate analysis was conducted to determine frequencies and distributions of values within all variables across each sample and subsample including male sex, age, education, race, CDR scores, cognitive status, depression, NPSs, FAQ or FAS score, MRI indicator including white matter and hippocampal volumes, relationship with informant, and reliability of informant. Baseline survival function was determined using log-rank tests for categorical variables and examined through inspection of Kaplan-Meier plots (see Figures 1 and 2 for Kaplan-Meier plots of the full sample and the MRI sample). Visual inspection of Kaplan–Meier plots were consistent with log-rank tests. Only variables which demonstrated significantly different survival curves among participants were used in the Cox survival analyses. The relationship of selected continuous variables was examined relative to the outcome variable using the Cox proportional hazards model [33]. Cox survival analyses were performed for exploration of the effects of the main variables on attrition in the full sample, alive subsample, MRI sample, and alive MRI subsample. Covariates, which were found to be statistically significant in Table 2, were used to predict the hazard ratio of a failure event (exit from the survey). Regression modeling included simultaneous control of multiple predictors, including male sex, age, education, race, CDR global score, cognitive status, depression, incidence of NPSs, FAQ/FAS score, white matter hyperintensities, hippocampal volume, relationship with co-participant, and reliability of co-participant was conducted. An additional subsample analysis was conducted on the alive subsample, which excluded participants who died (n= 24,231), the MRI sample: a group of participants who also had complete UDS and MRI data (n=1,104), and the alive MRI subsample (n=974). For the analysis with the MRI sample and alive MRI subsample, MRI indicators, such as white matter hyperintensity and hippocampal volume, were also included.
Figure 1.
Kaplan Meier survival curve for the full sample
Figure 2.
Kaplan Meier survival curve for the MRI sample
Table 2:
Bivariate Analysis of Predictors and Covariates
| Full Sample | Alive Subsample (dropped those died) |
MRI Sample | Alive MRI Subsample (dropped those died) |
|||||
|---|---|---|---|---|---|---|---|---|
| Sample Size | 30,433 | 24,231 | 1,104 | 947 | ||||
| t or χ2 | p- value |
t or χ2 | p- value |
t or χ2a |
p-value | t or χ2a | p-value | |
| Died | 3502.87 | 0.0000 | N/A | N/A | 279.05 | 0.0000 | N/A | N/A |
| Male | 36.48 | 0.0000 | 1.21 | 0.2705 | 1.69 | 0.1934 | 0.04 | 0.8499 |
| Age | −26.05 | 0.0000 | −10.70 | 0.0000 | −10.84 | 0.0000 | −6.33 | 0.0000 |
| Education (Years) | 29.73 | 0.0000 | 30.63 | 0.0000 | 9.29 | 0.0000 | 7.75 | 0.0000 |
| Race | ||||||||
| White Non-Hispanic | 65.48 | 0.0000 | 219.30 | 0.0000 | 23.32 | 0.0000 | 33.74 | 0.0000 |
| Black Non-Hispanic | 4.74 | 0.0295 | 36.10 | 0.0000 | 17.33 | 0.0000 | 19.55 | 0.0000 |
| Hispanic | 74.66 | 0.0000 | 165.25 | 0.0000 | 10.03 | 0.0015 | 14.16 | 0.0002 |
| Other | 10.33 | 0.0013 | 31.03 | 0.0000 | 0.69 | 0.4073 | 0.02 | 0.8979 |
| CDR score | ||||||||
| CDRGLOB=0 | 2912.47 | 0.0000 | 1611.33 | 0.0000 | 114.03 | 0.0000 | 59.60 | 0.0000 |
| CDRGLOB=0.5 | 65.09 | 0.0000 | 206.33 | 0.0000 | 37.60 | 0.0000 | 36.52 | |
| CDRGLOB=1 | 964.08 | 0.0000 | 594.41 | 0.0000 | 43.92 | 0.0000 | 9.97 | 0.0016 |
| CDRGLOB=2 | 1226.38 | 0.0000 | 602.18 | 0.0000 | 14.98 | 0.0001 | 5.69 | 0.0171 |
| CDRGLOB=3 | 1179.69 | 0.0000 | 171.00 | 0.0000 | 60.11 | 0.0000 | 11.08 | 0.0009 |
| Cognitive Status | ||||||||
| Normal Cognition | 2816.63 | 0.0000 | 1542.86 | 0.0000 | 120.47 | 0.0000 | 58.67 | 0.0000 |
| Impaired but not MCI | 28.25 | 0.0000 | 3.08 | 0.0790 | 1.65 | 0.1989 | 2.39 | 0.1223 |
| MCI | 7.18 | 0.0000 | 75.36 | 0.0000 | 27.32 | 0.0000 | 25.93 | 0.0000 |
| Dementia | 3302.90 | 0.0000 | 1458.77 | 0.0000 | 82.80 | 0.0000 | 18.40 | 0.0000 |
| Depression | 189.92 | 0.0000 | 157.08 | 0.0000 | 1.46 | 0.2269 | 1.18 | 0.2782 |
| NPSs | ||||||||
| Delusion | 917.13 | 0.0000 | 516.75 | 0.0000 | 29.68 | 0.0000 | 12.13 | 0.0005 |
| Hallucination | 710.92 | 0.0000 | 304.04 | 0.0000 | 20.03 | 0.0000 | 10.82 | 0.0010 |
| Agitation | 891.85 | 0.0000 | 441.07 | 0.0000 | 31.23 | 0.0000 | 13.14 | 0.0003 |
| Depression | 546.92 | 0.0000 | 347.03 | 0.0000 | 17.04 | 0.0000 | 8.76 | 0.0031 |
| Anxiety | 529.01 | 0.0000 | 215.95 | 0.0000 | 8.66 | 0.0033 | 0.68 | 0.4085 |
| Elation | 97.36 | 0.0000 | 37.75 | 0.0000 | 2.36 | 0.1248 | 1.51 | 0.2195 |
| Apathy | 1309.52 | 0.0000 | 545.26 | 0.0000 | 14.31 | 0.0002 | 2.91 | 0.0881 |
| Disinhibition | 501.64 | 0.0000 | 187.34 | 0.0000 | 46.26 | 0.0000 | 22.42 | 0.0000 |
| Irritability | 493.18 | 0.0000 | 261.54 | 0.0000 | 18.41 | 0.0000 | 8.33 | 0.0039 |
| Motor Disturbance | 900.50 | 0.0000 | 326.03 | 0.0000 | 14.14 | 0.0002 | 4.03 | 0.0448 |
| Night Time Disturbance | 396.88 | 0.0000 | 158.10 | 0.0000 | 7.48 | 0.0062 | 1.13 | 0.2872 |
| Appetite Disturbance | 619.03 | 0.0000 | 230.89 | 0.0000 | 39.14 | 0.0000 | 20.92 | 0.0000 |
| FAQ or FAS | ||||||||
| 0-10 | 3106.62 | 0.0000 | 1228.11 | 0.0000 | 93.95 | 0.0000 | 29.46 | 0.0000 |
| 11-20 | 654.10 | 0.0000 | 432.66 | 0.0000 | 42.19 | 0.0000 | 16.09 | 0.0001 |
| 21-30 | 2439.25 | 0.0000 | 772.71 | 0.0000 | 51.46 | 0.0000 | 13.35 | 0.0003 |
| MRI Indicator | ||||||||
| White Matter* | N/A | N/A | N/A | N/A | −9.90 | 0.0000 | −6.50 | 0.0000 |
| Hippocampal Volume* | N/A | N/A | N/A | N/A | 9.62 | 0.0000 | 6.31 | 0.0000 |
| Co-Participant Relationship to Subject | ||||||||
| Spouse, Partner or Companion | 24.47 | 0.0000 | 57.37 | 0.0000 | 6.16 | 0.0131 | 11.41 | 0.0007 |
| Child | 134.64 | 0.0000 | 105.40 | 0.0000 | 15.30 | 0.0001 | 11.89 | 0.0006 |
| Sibling | 6.49 | 0.0108 | 0.05 | 0.8257 | 2.48 | 0.1153 | 0.66 | 0.4167 |
| Other Relative | 9.03 | 0.0027 | 14.17 | 0.0002 | 6.62 | 0.0101 | 8.69 | 0.0032 |
| Friend, Neighbor, or Someone Known | 111.81 | 0.0000 | 32.05 | 0.0000 | 5.51 | 0.0189 | 1.38 | 0.2397 |
| Paid Caregiver or Health Care Provider | 43.07 | 0.0000 | 25.60 | 0.0000 | 0.55 | 0.4596 | 0.60 | 0.4401 |
| Other | 0.02 | 0.8770 | 0.83 | 0.3636 | 0.71 | 0.3985 | 2.94 | 0.0865 |
| Co-Participant Reliability | 0.13 | 0.7182 | 1.05 | 0.3046 | 6.17 | 0.0130 | 8.99 | 0.0027 |
Indicates means and standard deviations presented
Individual ADCs not only employ their own individual recruitment protocols but also use a variety of means to obtain follow-up observations from participants. In 2002, the ADC Clinical Task Force was established by the National Institute on Aging to standardize the data collection procedures and participant evaluations across each of the ADCs. In doing so, they also created an annual schedule of follow-up [34], though the methods to encourage follow-up remain individualized to each ADC. The differing recruitment methods and study protocols at each ADC were adjusted as a center specific fixed effect (only 3 centers had complete MRI information, so we adjust for 3 fixed effects with this subsample). Huber–White-corrected standard errors are used to adjust for clustering at the center level.
Results
Participants in the Full Sample
The minimum number of visits for all included participants was 1 and the maximum was 11 (mean = 3; median=3.26). There were 20,256 exits (failures) by the end of the observation period among NACC participants with complete information on variables we used for the analysis. Among all exits, 10,640 participants dropped out after the first visit, and 6,202 participants exited the survey due to the event of death. For the full sample, there were 5,577 failures among individuals with normal cognition, 819 failures among individuals deemed impaired not MCI, 4,319 failures for those with MCI, and 9541 failures for those with dementia. Among the 1,174 individuals with complete MRI information, there were 431 total failures, 152 of which were among those with normal cognition at baseline, 30 among those deemed impaired not MCI, 143 with MCI, and 106 failures for those with dementia. For the full sample, around 44% of the sample was male, the mean age of participants at visit one was 72.60 years (SD: 10.38), and the mean years of education was 14.91 (SD=3.52). The majority of the full sample was White (around 76%), around 14% were Black non-Hispanic, seven percent of the sample reported Hispanic origin, and around three percent were from other ethnic groups. Almost 37% of the sample had a normal CDR score, and near 36% of participants were diagnosed with normal cognition. Around four percent of the sample were diagnosed with impaired cognition but not MCI, around 21% with MCI, and around 38% with dementia. Close to 19% of the sample had depression based on the GDS, and three percent to 29% had at least one neuropsychiatric symptom. Over 71% of participants were determined to have a FAQ or FAS score lower than 10, indicating few difficulties with functional performance, while about 15% of participants had a score between 11-20, signifying a need for some level of assistance in conducting daily activities. Moreover, around 13% of the full sample had a FAQ or FAS score between 21 and 30, which indicates a high level of dependence in conducting daily activities. In the full sample, over 56% of co-participants were the spouses of the participants, over 24% were their children, and the remaining co-participants were comprised of siblings, friends, caregivers, or had other relations with the participants (see Table 1).
Table 1:
Demographic Overview of Sample and Predictor Variables
| Full Sample | Alive Subsample (dropped those died) |
p-value | MRI Sample | Alive MRI Subsample (dropped those died) |
p-value | |
|---|---|---|---|---|---|---|
| Sample Size | 30,433 | 24,231 | 1,104 | 947 | ||
| Died | 20.38% | 0.00% | p<0.001 | 14.22% | 0.00% | p<0.001 |
| Male | 43.63% | 40.99% | p<0.001 | 40.67% | 39.07% | p = 0.008 |
| Age* | 72.60 [10.38] | 71.57 [10.03] | p<0.001 | 72.01 [10.83] | 70.76 [10.80] | p<0.001 |
| Education (Years)* | 14.91 [3.52] | 14.96 [3.52] | p<0.001 | 14.59 [3.52] | 14.83 [3.54] | p<0.001 |
| Race | ||||||
| White Non-Hispanic | 75.88% | 73.53% | p<0.001 | 72.19% | 73.71% | p = 0.006 |
| Black Non-Hispanic | 13.79% | 14.98% | p<0.001 | 14.67% | 13.62% | p = 0.015 |
| Hispanic | 7.10% | 7.80% | p<0.001 | 10.60% | 9.93% | p = 0.075 |
| Other | 3.22% | 3.69% | p<0.001 | 2.54% | 2.75% | p = 0.277 |
| CDR score | ||||||
| CDRGLOB=0 | 36.77% | 42.04% | p<0.001 | 55.80% | 60.72% | p<0.001 |
| CDRGLOB=0.5 | 36.50% | 37.97% | p<0.001 | 34.15% | 32.52% | p = 0.005 |
| CDRGLOB=1 | 17.34% | 14.55% | p<0.001 | 8.88% | 6.34% | p<0.001 |
| CDRGLOB=2 | 6.35% | 4.28% | p<0.001 | 0.82% | 0.32% | p<0.001 |
| CDRGLOB=3 | 3.04% | 1.16% | p<0.001 | 0.36% | 0.11% | p<0.001 |
| Cognitive Status | ||||||
| Normal Cognition | 36.35% | 41.57% | p<0.001 | 58.51% | 64.10% | p<0.001 |
| Impaired but not MCI | 4.38% | 4.89% | p<0.001 | 3.89% | 3.48% | p = 0.084 |
| MCI | 21.20% | 22.74% | p<0.001 | 23.64% | 22.18% | p = 0.005 |
| Dementia | 38.07% | 30.80% | p<0.001 | 13.95% | 10.24% | p<0.001 |
| Depression | 18.57% | 18.30% | p = 0.015 | 6.79% | 6.55% | p = 0.424 |
| NPSs | ||||||
| Delusion | 8.23% | 6.70% | p<0.001 | 3.89% | 2.96% | p<0.001 |
| Hallucination | 4.68% | 3.36% | p<0.001 | 1.54% | 1.16% | p = 0.012 |
| Agitation | 21.02% | 18.56% | p<0.001 | 14.76% | 13.20% | p<0.001 |
| Depression | 29.00% | 27.48% | p<0.001 | 23.46% | 22.28% | p = 0.023 |
| Anxiety | 25.01% | 22.79% | p<0.001 | 17.84% | 16.37% | p = 0.002 |
| Elation | 3.47% | 3.09% | p<0.001 | 1.90% | 1.80% | p = 0.523 |
| Apathy | 24.84% | 20.76% | p<0.001 | 13.41% | 11.83% | p<0.001 |
| Disinhibition | 13.15% | 11.15% | p<0.001 | 8.42% | 6.86% | p<0.001 |
| Irritability | 27.39% | 25.46% | p<0.001 | 19.57% | 17.85% | p<0.001 |
| Motor Disturbance | 11.74% | 9.19% | p<0.001 | 5.43% | 4.22% | p<0.001 |
| Night Time Disturbance | 22.21% | 20.37% | p<0.001 | 14.76% | 13.41% | p = 0.002 |
| Appetite Disturbance | 17.49% | 15.22% | p<0.001 | 10.33% | 8.87% | p<0.001 |
| FAQ or FAS | ||||||
| 0-10 | 71.46% | 78.65% | p<0.001 | 87.14% | 90.92% | p<0.001 |
| 11-20 | 15.07% | 13.11% | p<0.001 | 8.51% | 6.55% | p<0.001 |
| 21-30 | 13.47% | 8.24% | p<0.001 | 4.35% | 2.53% | p<0.001 |
| MRI Indicator | ||||||
| White Matter | 8.28 [12.52] | 6.90 [10.77] | p<0.001 | |||
| Hippocampal Volume | 6.12 [0.91] | 6.21 [0.87] | p<0.001 | |||
| Co-Participant Relationship | ||||||
| Spouse/Partner | 56.29% | 55.56% | p<0.001 | 55.62% | 55.97% | p = 0.565 |
| Child | 24.59% | 23.75% | p<0.001 | 24.37% | 22.70% | p = 0.002 |
| Sibling | 4.19% | 4.71% | p<0.001 | 5.80% | 6.34% | p = 0.060 |
| Other Relative | 3.58% | 3.66% | p = 0.165 | 3.53% | 3.48% | p = 0.832 |
| Friend, Neighbor, or Someone Known | 8.90% | 9.98% | p<0.001 | 9.33% | 10.03% | p = 0.049 |
| Paid Caregiver | 0.82% | 0.72% | p<0.001 | 0.27% | 0.21% | p = 0.343 |
| Other | 1.62% | 1.63% | p = 0.851 | 1.09% | 1.27% | p = 0.156 |
| Co-Participant Reliability | 3.28% | 3.26% | p = 0.654 | 2.54% | 2.32% | p = 0.269 |
Indicates means and standard deviations presented
Participants in the Alive Subsample
Participants in the alive subsample (attrition for reasons other than death) were significantly different from participants in the full sample in relation to demographic variables and mental and physical health (see p-values reported in Table 1). Participants in this subsample were slightly more likely to be female, younger, and more educated. They were also more likely to be Black non-Hispanic or Hispanic compared to the participants of the full sample. Participants in the alive subsample were more likely to have a lower CDR score (demonstrating normal neurological and behavioral status), and normal cognition compared to the participants of the full sample. Moreover, participants in this subsample were slightly less likely to have depression and any of the 12 denoted neuropsychiatric symptoms in the NIQ. Additionally, participants in this subsample were more likely to have a FAQ or FAS score between 11-20 indicating a lower level of dependence in daily activities. Co-participants in this subsample were slightly less likely to be the spouses or partner or children of the participants and slightly more likely to be paid caregivers compared to the full sample (see Table 1).
Participants in the MRI Sample
Participants in the MRI sample were more likely to be female and less likely to be White non-Hispanic compared to the participants of the full sample and alive subsample. The average age of the participants in the MRI sample was slightly lower than the full sample and higher than the alive subsample. Moreover, the average years of education of the participants in this subsample was slightly lower than the full sample and the alive subsample. Participants in this subsample were more likely to have normal neurological and behavioral status based on the CDR, and normal cognition based on the diagnosis of the clinicians compared to the full sample and the alive subsample. Moreover, participants in the MRI sample were less likely to have depression and all 12 neuropsychiatric symptoms indicated in the NIQ. They also had better functional ability in daily activities compared to the participants in the full sample and the alive subsample. Co-participants in this subsample were slightly more likely to be the spouses or partners of the participants and less likely to be paid caregivers (see Table 1).
Participants in the Alive MRI Subsample
Compared to those in the MRI sample, participants in the alive MRI subsample were more likely to be female, had a lower average mean age at the baseline, had higher average years of education and were more likely to be White non-Hispanic. Participants in this subsample were more likely to have normal neurological and behavioral status, and normal cognition compared to the MRI sample. Moreover, participants in this subsample were less likely to be depressed or have any neuropsychiatric symptoms based on the NPI-Q compared to the participants in the MRI sample. Participants in the alive MRI subsample were more likely to have lower scores in FAQ or FAS, indicating higher levels of independence in daily activities compared to the participants of the MRI sample. Participants in this subsample had lower white matter hyperintensities (6.90 vs 8.28, p <0.001) and higher hippocampal volume (6.21 vs 6.12, p <0.001) compared to those in the MRI sample. Co-participants in this subsample were more likely to be spouses or partners of the participants or paid caregivers compared to the MRI sample. Percentages, means, and standard deviations (where applicable) for the full sample and subsamples are displayed in Table 1.
Univariate and Multivariate Analyses
Preliminary univariate analysis using the log-rank test for equality of survivor functions in the full samples revealed statistically significant differences (p < 0.001) in the survival curves of those with different mortality statuses, age, years of education, participants who were white non-Hispanic or Hispanic, all levels of CDR global scores, cognitive status, depression, all NPs, all levels of FAQ or FAS scores, and relationships with co-participants, specifically spouses, children, other relatives, and friends/neighbors. Results for the log-rank tests are summarized in Table 2. Regression results are summarized in Table 3. For the full sample and MRI sample (Columns 1 and 3, Table 3), the event of death increased the hazard of exiting the study by about 2 times (Hazard Ratio (HR): 1.92, 95% CI: 1.67-2.19; OR: 2.54, 1.40-4.63; p<0.01, respectively). A higher educational level was associated with lower attrition within the full sample (HR: 0.97, 0.97-0.98), alive subsample (HR: 0.97, 0.96-0.98), MRI sample (HR: 0.97, 0.96-0.99), and the alive MRI subsample (HR: 0.95, 0.93-0.97). Hispanic participants were less likely to exit the study in the full sample (HR: 0.85, 0.76-0.96), and alive subsample (HR: 0.85, 0.72-0.99), compared to White non-Hispanic participants.
Table 3:
Cox Proportional Hazard Ratio Model (Exit as Outcome Variable) (95% robust confidence interval in parentheses)
| Full Sample | Alive Subsample (dropped those died) |
MRI Sample | Alive MRI Subsample (dropped those died) |
|
|---|---|---|---|---|
| Sample Size | 30,433 | 24,231 | 1,104 | 947 |
| Died | 1.92*** (1.67 - 2.19) | 2.54*** (1.40 - 4.63) | ||
| Male | 1.02 (0.98 - 1.07) | 1.01 (0.96 - 1.07) | 1.05 (0.91 - 1.21) | 1.08 (0.90 - 1.31) |
| Age | 1.00 (1.00 - 1.00) | 1.00 (1.00 - 1.00) | 0.99 (0.98 - 1.01) | 0.99 (0.96 - 1.02) |
| Education | 0.97*** (0.97 - 0.98) | 0.97*** (0.96 - 0.98) | 0.97*** (0.96 - 0.99) | 0.95*** (0.93 - 0.97) |
| Race (White Non-Hispanic as Reference) | ||||
| Black Non-Hispanic | 1.11* (1.00 - 1.25) | 1.13* (0.99 - 1.29) | 1.06 (0.73 - 1.53) | 1.03 (0.70 - 1.51) |
| Hispanic | 0.85** (0.76 - 0.96) | 0.85** (0.72 - 0.99) | 1.03 (0.94 - 1.12) | 0.90* (0.79 - 1.01) |
| Other | 1.25** (1.03 - 1.53) | 1.27*** (1.06 - 1.53) | 0.72*** | 0.86 |
| CDR score (CDRGLOB=0 as Reference) | ||||
| CDRGLOB=0.5 | 1.19*** (1.07 - 1.32) | 1.20*** (1.06 - 1.35) | 1.12 (0.89 - 1.43) | 1.16 (0.89 - 1.52) |
| CDRGLOB=1 | 1.27*** (1.13 - 1.43) | 1.28*** (1.10 - 1.48) | 1.12 (0.64 - 1.96) | 0.97 (0.70 - 1.34) |
| CDRGLOB=2 | 1.54*** (1.35 - 1.76) | 1.58*** (1.35 - 1.85) | 1.09 (0.56 - 2.11) | 2.38*** (1.29 - 4.39) |
| CDRGLOB=3 | 1.67*** (1.47 - 1.91) | 1.44*** (1.18 - 1.77) | 2.29*** (1.50 - 3.48) | 2.49** (1.23 - 5.06) |
| Cognitive Status (Normal Cognition as Reference) | ||||
| Impaired but not MCI | 1.23*** (1.05 - 1.42) | 1.21** (1.03 - 1.41) | 1.09 (0.94 - 1.26) | 1.35*** (1.14 - 1.60) |
| MCI | 1.26*** (1.13 - 1.42) | 1.27*** (1.11 - 1.44) | 1.39*** (1.19 - 1.63) | 1.63*** (1.45 - 1.83) |
| Dementia | 1.47*** (1.31 - 1.65) | 1.53***(1.33 - 1.76) | 1.73*** (1.16 - 2.58) | 2.17*** (1.24 - 3.78) |
| NPSs | ||||
| Delusion | 1.03 (0.98 - 1.09) | 1.04 (0.97 - 1.12) | 0.89 (0.76 - 1.04) | 0.95 (0.82 - 1.10) |
| Hallucination | 1.04 (0.98 - 1.10) | 1.04 (0.95 - 1.14) | 1.71*** (1.36 - 2.15) | 1.37 (0.84 - 2.25) |
| Agitation | 1.05** (1.01 - 1.09) | 1.07*** (1.02 - 1.13) | 1.05 (0.86 - 1.27) | 1.09 (0.76 - 1.56) |
| Depression | 1.05*** (1.02 - 1.08) | 1.07*** (1.03 - 1.11) | 1.04 (0.82 - 1.31) | 0.86* (0.73 - 1.02) |
| Anxiety | 1.00 (0.97 - 1.04) | 0.99 (0.94 - 1.05) | 0.90 (0.78 - 1.04) | 0.81 (0.57 - 1.14) |
| Elation | 0.95 (0.89 - 1.03) | 0.97 (0.88 - 1.08) | 0.95 (0.78 - 1.17) | 1.37*** (1.22 - 1.55) |
| Apathy | 1.04** (1.00 - 1.08) | 1.04 (0.99 - 1.09) | 1.15*** (1.09 - 1.22) | 1.16 (0.99 - 1.37) |
| Disinhibition | 0.97* (0.94 - 1.00) | 0.98 (0.92 - 1.04) | 1.14** (1.03 - 1.27) | 1.65*** (1.38 - 1.96) |
| Irritability | 0.98 (0.94 - 1.02) | 0.96 (0.92 - 1.01) | 0.90 (0.78 - 1.06) | 0.82 (0.67 - 1.02) |
| Motor Disturbance | 1.02 (0.97 - 1.07) | 1.01 (0.93 - 1.10) | 0.81*** (0.75 - 0.88) | 0.65*** (0.61 - 0.68) |
| Night Time Disturbance | 1.00 (0.96 - 1.04) | 0.97 (0.93 - 1.02) | 0.95 (0.87 - 1.05) | 0.78** (0.65 - 0.94) |
| Appetite Disturbance | 1.10*** (1.06 - 1.15) | 1.09*** (1.03 - 1.15) | 1.16 (0.92 - 1.47) | 1.43*** (1.11 - 1.84) |
| FAQ or FAS (0-10 as Reference Category) | ||||
| 11-20 | 1.06** (1.00 - 1.11) | 1.05 (0.97 - 1.12) | 1.18*** (1.10 - 1.27) | 1.05* (0.99 - 1.10) |
| 21-30 | 1.10*** (1.02 - 1.18) | 1.13** (1.01 - 1.25) | 1.11 (0.93 - 1.32) | 1.10*** (1.07 - 1.13) |
| MRI Indicator | ||||
| White Matter | 1.00 (1.00 - 1.01) | 1.00 (1.00 - 1.01) | ||
| Hippocampal Volume | 0.92*** (0.89 - 0.94) | 0.96 (0.90 - 1.02) | ||
| Co-Participant Relationship (Spouse as Reference) | ||||
| Child | 1.10*** (1.06 - 1.14) | 1.10*** (1.05 - 1.14) | 1.11 (0.97 - 1.28) | 1.16 (0.95 - 1.41) |
| Sibling | 1.15*** (1.07 - 1.24) | 1.14*** (1.04 - 1.24) | 1.12 (0.74 - 1.70) | 0.93 (0.47 - 1.83) |
| Other Relative | 1.20*** (1.10 - 1.31) | 1.23*** (1.10 - 1.37) | 1.84*** (1.41 - 2.41) | 2.16*** (1.68 - 2.78) |
| Friend, Neighbor, or Someone Known | 1.14*** (1.06 - 1.24) | 1.15*** (1.04 - 1.27) | 0.93 (0.73 - 1.17) | 1.02 (0.77 - 1.36) |
| Paid Caregiver/Health Care Provider | 1.23*** (1.08 - 1.39) | 1.26** (1.03 - 1.54) | 3.07 (0.86 - 11.0) | 8.45** (1.38 - 52.0) |
| Other | 1.19** (1.04 - 1.37) | 1.27** (1.05 - 1.52) | 2.03*** (1.29 - 3.21) | 1.90** (1.16 - 3.14) |
| Reliability of Co-Participant | 1.11* (1.00 - 1.23) | 1.20*** (1.07 - 1.35) | 1.37* (0.98 - 1.92) | 1.88** (1.03 - 3.44) |
Robust 95% confidence intervals are in the parentheses.
p<0.01,
p<0.05,
p<0.1
Worsening CDR score and cognitive status increased the hazard of exiting the study in the full sample (CDR global score of 3 = HR: 1.67, 1.47-1.91) and the alive subsample (CDR global score of 3 = HR: 1.44, 1.18-1.77)). A CDR global score of 3 was also significantly associated with attrition in the MRI sample (HR: 2.29, 1.50-3.48) and the MRI alive subsample (HR: 2.49, 1.23-5.06), p<.01), and a CDR global score of 2 was also associated with attrition in all categories, except the MRI full sample. A number of NPSs also influenced the stability of a person’s study participation. For instance, in the alive subsample if participants had depression (HR: 1.07, 1.03-1.11), exhibited agitation (HR: 1.07, 1.02-1.11, or reported an appetite disturbance (OR: 1.09, 1.03-1.15), they were more likely to exit the study prematurely. In the alive MRI sub sample, a different pattern emerged in which the presence of elation (HR: 1.37, 1.22-1.55, p < .01), disinhibition (HR: 1.65, 1.38-1.96), and an appetite disturbance (HR: 1.43, 1.11-1.84) predicted early attrition. The presence of apathy also led to a higher risk of early attrition in the full sample (HR: 1.04, 1.00-1.08) and in the MRI sample (HR: 1.15, 1.09-1.22). Interesting, the presence of motor disturbance (HR: 0.65, 0.61-0.68) and nighttime disturbance (HR: 0.78, 0.65-0.94) in the alive MRI subsample was associated with a participant staying in the study.
Increased difficulty with daily activities measured by a higher FAQ score (between 21 and 30) also increased the hazard of leaving the study in the full sample (HR: 1.10, 1.02-1.19), alive subsample (HR: 1.13, 1.01-1.25), and alive MRI subsample (HR: 1.10, 1.07-1.13). In the MRI sample analyses, where we control for two MRI indicators, lower hippocampal volume was associated with higher likelihood of exiting the survey (HR: 0.92, 0.89-0.94). Moreover, when participants were accompanied by co-participants (informants) other than their spouse, they experienced a statistically significant increased hazard of exiting the study in the full sample (HR: 1.23, 1.08-1.39 for paid caregiver or health care provider) and the alive subsample (HR: 1.26, 1.03-1.54 for paid caregiver or health care provider). The reliability of the co-participants themselves was also significantly associated with early attrition from the study among all participant samples.
Discussion
In this study, univariate analyses showed that attrition could be associated with mortality, age, education, race, CDR score, cognitive status, FAQ or FAS score, and co-participant relation. Moreover, our Cox survival analyses found that attrition could be associated with mortality, education, race, CDR score, cognitive status, some of the NPSs, FAQ or FAS score, and hippocampal volume. However, hazard ratios for attrition between the full sample and the alive subsample were only slightly different, indicating the importance of other associated factors of attritions besides death.
The study results support the existing literature, in which increasing age, NPSs, and cognitive impairment are consistently related to greater rates of attrition [13, 22, 36, 37]. Moreover, an increase in the number of educational years in the full sample and subsamples of this study found to be associated with a reduced likelihood of study drop-out (p < .01). This is in line with previous studies [38, 39], though mixed results are found in the literature. Reinwand et al. [40] most recently examined seven studies with the specific intent of examining the effect of educational level on attrition rates. Their findings point to significantly higher attrition among participants with no education, primary, or lower vocational school attainment compared to those with professional or University education. In these same studies, attrition was significantly higher among those with secondary vocational school or high school education compared to participants with professional or University education. However, there was a lack of association between attrition rates and educational level in four out of seven studies reviewed by Reiwand et al [40]. Though the current study demonstrated that higher educational attainment is associated with a reduced likelihood of attrition, the peer-reviewed literature remains mixed and further studies in a nationally representative sample are needed. In addition, specific information about educational type, quality, field/industry, and even occupation may provide further detail that will elucidate why the literature is mixed and what the predictive educational factor may be with regard to attrition.
In addition to education, the presence of depression significantly increased the hazard of attrition in the full sample (HR: 1.04, 1.00-1.09). This finding is in line with the previous literature in which depression was an independent predictor of attrition, and associated with all other risk factors for attrition [38]. For instance, Beekman et al. [38] reported a 73.6% response rate among those without depression symptoms, and a 63% rate among those with depression (OR: 1.67; 1.36-2.06). In addition, depression, whether prodromal or an independent lifelong risk factor, has been found to increase the hazard of cognitive impairment [41–44], and increasing severity of cognitive impairment is associated with attrition [7, 9, 12, 37].
Moreover, race and ethnicity of the participants was associated with attrition in this study. Although the majority of participants were White, Black non-Hispanic participants were more likely to attrite in both the full sample and the MRI sample. This phenomenon persisted even when excluded participants who died during the course of the study. Meanwhile, Hispanic participants, though less than five percent of the participants in the NACC database, were less likely to attrite compared to white non-Hispanic participants. As such, there are special considerations that researchers should heed when working with older adults of minority backgrounds, though these suggestions can be tailored to the racial, ethnic, and cultural background of the participants given that different groups are experiencing more or less risk of attrition.
The finding, which revealed that reduced hippocampal volume was associated with risk for drop out from the study, was a new finding given that only one previous study examined hippocampal volume in relation to a lack of follow-up for imaging sessions. Though the exact reason for this association requires further study, this finding is likely to be related to the association of hippocampal atrophy to memory and cognitive decline [45–47]. This phenomenon is supported by a previous study in which participants who had poorer results on neurocognitive tests at baseline were more likely to attrite [12]. In this study, in addition to reduced hippocampal volume, we also found a relationship between increased white matter hyperintensities and the attrition rate. These findings are in line with a recent study that evaluated brain MRI measures and study attrition. Glymour et al. [19] found that greater baseline levels of white matter lesion volume increased the likelihood of attrition, and greater declines in hippocampal volume between baseline and follow-up imaging sessions were also related to study drop out.
Limitations
Some additional factors that may influence attrition were not available for examination in the current dataset. For instance, among older adults, beliefs about the advantages of participation in a study have been found to be associated with frequency of participation [15]. Moreover, although this study identifies factors influencing attrition in a large longitudinal database, we did not include the role of frailty or illness, which may require additional individual attention from investigators. Individuals with severe cognitive impairment may not be able to answer researchers’ questions reliably, may be unable to respond to researchers’ attempt at follow-up, and may not be able to keep appointments for follow-up. Income, socioeconomic status, and geographic distance away from the observing ADC, important sociodemographic variables that may influence a participant’s ability to follow-up, were not available for analysis in the NACC data. Future studies conducted on the NACC database should account for the variation in research designs across different Alzheimer’s Disease Centers in the United States, including case series, case-control studies, and even studies which may approximate a cohort study design. In addition, milestone data submitted to NACC by individual ADCs specifies whether the participants are discontinued/dropped from the study and whether they will be followed minimally until autopsy, and thus are not actually discontinued from the study. Even when an autopsy is performed, the information available to NACC may be subject to the time interval within which the individual ADC provides the results. Therefore, using milestone data may result in a different conclusion than applying the 3-year attrition cut point that was developed for the purposes of this study. A particular strength of this study was the large sample size, number of visits, and, even with the known limitations, the ability to validate and expand upon the existing literature base.
Recommendations and Conclusion
Deeg et al. [7] have suggested that there are two different sources of attrition – unmodifiable causes, outside the control of the researcher, and modifiable causes that can be changed by the researcher. Mortality, advancing age, cognitive decline, increased NPSs, limitation in physical ability, and variations in hippocampal volume are unmodifiable and inevitable sources of attrition. Unmodifiable associated factors with attrition should be accounted for in the design of the study. For instance, compensation could be made during recruitment to maintain adequate statistical power after attrition related to these unmodifiable sources. In this context, some researchers oversample individuals at greater risk of dropping out with the hopes that adequate numbers are retained by study completion [13]. This study found that attrition could be associated with modifiable causes such as considerations in working with participants from different racial and ethnic groups and unmodifiable causes such as death in a longitudinal study of older adults. The design of longitudinal studies could be improved so as to minimize attrition by learning lessons from the findings of this and other studies.
For attrition related to unmodifiable causes, strategies such as oversampling individuals at greater risk of attrition and recruiting proxies could be considered. It has been found that including information by proxy respondents, as opposed to excluding proxy information during participant attrition, resulted in a 12% increase in estimated dementia prevalence [49]. For attrition related to modifiable risk factors, targeted strategies may minimize attrition. Andersen and Newman [51] developed a theoretical framework that seeks to explain the effect of individual determinants on medical care usage, which we believe can be applied to a discussion of attrition in health-related studies. In this context, education might be thought of as a “predisposing variable” such that it influences a participant’s attitudes or beliefs about their needs for services or observations. In contrast, depression not only signals a “need-for-care” but it also might be characterized as an enabling factor, which might facilitate, or in this case, hinder the participants’ utilization of services. The importance of these individual factors in study follow-up and completion signals the need for early identification of these attrition risk factors in participants, and the development of procedures to ensure their participation until the study ends.
Researchers can increase retention by (a) gathering sufficient tracking information at baseline, and forging formal and informal working relationships with third parties so as to efficiently enable location of a missing participant [52]; (b) study participants need to receive statements of gratitude for their participation from the research staff, who should thank them for their time and interact with them in a genuine and personal manner [15, 36, 52]; (c) every effort should be made to regularly update participants on the progress of the research project and to provide consistent feedback on individual progress [15, 36], including the use of newer technology such as text messaging [53]; (d) participants should be constantly reminded of the potential real-world impact of the study and the importance of their participation [7, 10, 36]; and (e) flexibility in research design and eliminating barriers to participation by accommodating the needs of the older adults, especially those with limited functional ability, such as providing more accessible locations and time frames for scheduled meetings, providing adequate breaks between testing sessions and abbreviating such session so as to prevent exhaustion [10, 12, 15, 36, 52]. In addition, providing roundtrip transportation to study sites, conducting portions of interviews and observations in natural home and residential settings, and working with staff and administrators at long-term living centers where older adults may reside may address logistical concerns and provide additional support to the older adult participant.
The literature discussing strategies for retention, specifically in working with older adults is limited, but Dennis and Neese [54] offer six suggestions to efficiently and respectfully recruit and retain culturally diverse older adult participants. First, researchers should be culturally aware and understand the historical abuses of certain populations, such as African Americans in the name of science. Second, researchers should seek relationships with and permission of the formal and informal local leadership. Third, researchers should build trust with participants by making the research process as accessible and inclusive as possible, spend the time to educate participants, and promptly and openly address any conflicts that arise. Fourth, researchers should work in partnership with participants, empowering individuals to work in mutual respect and effort with researchers, not in a situation where the researcher has more choice or power than the participant. Fifth, researchers and staff should recognize the vast in-group differences between people who self-identify in a certain cultural or ethnic group and they should not make assumptions about culture, values, ideas, and norms. Finally, researchers should constantly be aware of their thoughts and actions and engage in self-reflection [54].
The findings of this study provide formative data to help move the field forward in developing sound research designs and retention designs that take into the particular concerns and considerations that arise when developing recruitment and retention plans with older adults that buffer against the risk of attrition.
Acknowledgments:
The NACC database is funded by NIA/NIH Grant U01 AG016976. NACC data are contributed by the NIA-funded ADCs: P30 AG019610 (PI Eric Reiman, MD), P30 AG013846 (PI Neil Kowall, MD), P50 AG008702 (PI Scott Small, MD), P50 AG025688 (PI Allan Levey, MD, PhD), P50 AG047266 (PI Todd Golde, MD, PhD), P30 AG010133 (PI Andrew Saykin, PsyD), P50 AG005146 (PI Marilyn Albert, PhD), P50 AG005134 (PI Bradley Hyman, MD, PhD), P50 AG016574 (PI Ronald Petersen, MD, PhD), P50 AG005138 (PI Mary Sano, PhD), P30 AG008051 (PI Thomas Wisniewski, MD), P30 AG013854 (PI M. Marsel Mesulam, MD), P30 AG008017 (PI Jeffrey Kaye, MD), P30 AG010161 (PI David Bennett, MD), P50 AG047366 (PI Victor Henderson, MD, MS), P30 AG010129 (PI Charles DeCarli, MD), P50 AG016573 (PI Frank LaFerla, PhD), P50 AG005131 (PI James Brewer, MD, PhD), P50 AG023501 (PI Bruce Miller, MD), P30 AG035982 (PI Russell Swerdlow, MD), P30 AG028383 (PI Linda Van Eldik, PhD), P30 AG053760 (PI Henry Paulson, MD, PhD), P30 AG010124 (PI John Trojanowski, MD, PhD), P50 AG005133 (PI Oscar Lopez, MD), P50 AG005142 (PI Helena Chui, MD), P30 AG012300 (PI Roger Rosenberg, MD), P30 AG049638 (PI Suzanne Craft, PhD), P50 AG005136 (PI Thomas Grabowski, MD), P50 AG033514 (PI Sanjay Asthana, MD, FRCP), P50 AG005681 (PI John Morris, MD), P50 AG047270 (PI Stephen Strittmatter, MD, PhD).
Abbreviations:
- AD
Alzheimer’s disease
- ADC
Alzheimer’s disease center
- CSF
cerebrospinal fluid
- FAQ
Functional Activities Questionnaire
- FAS
Functional Assessment Scale
- GDS
Geriatric Depression Scale
- MRI
magnetic resonance imaging
- NACC
National Alzheimer’s Coordinating Center
- NPI-Q
Neuropsychiatric Inventory Questionnaire
- UDS
Uniform Data Set
Footnotes
Conflict of Interest: On behalf of all authors, the corresponding author states that there is no conflict of interest.
Contributor Information
Shanna L. Burke, Florida International University, Robert Stempel College of Public Health and Social Work, School of Social Work, 11200 S.W. 8th Street, AHC5 585, Miami, Florida 33199, 305-348-7462, sburke@fiu.edu.
Tianyan Hu, Florida International University, Robert Stempel College of Public Health and Social Work, Department of Health Policy and Management, 11200 S.W. 8th Street, AHC5-452, Miami, Florida 33199, 3053488416, tihu@fiu.edu.
Mitra Naseh, Florida International University, Robert Stempel College of Public Health and Social Work, School of Social Work, Miami, FL 33199, mahma024@fiu.edu.
Nicole M. Fava, Florida International University, Robert Stempel College of Public Health and Social Work, School of Social Work, 11200 S.W. 8th Street, AHC5- 566, Miami, FL 33199, 305-348-4568, nfava@fiu.edu.
Janice O’Driscoll, Florida International University, Robert Stempel College of Public Health and Social Work, School of Social Work, 11200 S.W. 8th Street, AHC5, Miami, Florida 33199, 305-721-4142, jan.odriscoll@gmail.com.
Daniel Alvarez, Florida International University, Robert Stempel College of Public Health and Social Work, School of Social Work, 11200 S.W. 8th Street, Miami, Florida 33199, dalva042@fiu.edu.
Linda B. Cottler, College of Public Health and Health Professions, Dean's Professor and Chair-Department of Epidemiology, College of Public Health and Health Professions and, College of Medicine, University of Florida, 2004 Mowry Drive, PO Box 100231, Gainesville, FL 32611, 352-273-5468, lcottler@ufl.edu.
Ranjan Duara, Wien Center for Alzheimer’s Disease and Memory Disorders, Mount Sinai Medical Center, Miami Beach FL 33140, Departments of Neurology, University of Florida College of Medicine, Gainesville, FL and Herbert Wertheim, College of Medicine, Florida International University, Miami, duara@msmc.com.
References
- 1.Harrop EN (2014) Follow-up Difficulty and Retention: Evaluating Potential Attrition Bias in a Longitudinal Substance Abuse Treatment Study. PhD Thesis [Google Scholar]
- 2.Miller RB, Wright DW (1995) Detecting and correcting attrition bias in longitudinal family research. J Marriage Fam 921–929 [Google Scholar]
- 3.Dufouil C, Brayne C, Clayton D (2004) Analysis of longitudinal studies with death and drop-out: a case study. Stat Med 23:2215–2226. 10.1002/sim.1821 [DOI] [PubMed] [Google Scholar]
- 4.Boykin DM, London MJ, Orcutt HK (2016) Examining minority attrition among women in longitudinal trauma research. J Trauma Stress 29:26–32 [DOI] [PubMed] [Google Scholar]
- 5.Rubin A, Babbie E (2016) Empowerment series: Essential research methods for social work, 4th ed. Cengage Learning, Boston, MA [Google Scholar]
- 6.White KS, Allen LB, Barlow DH, et al. (2010) Attrition in a multicenter clinical trial for panic disorder. J Nerv Ment Dis 198:665–671 [DOI] [PubMed] [Google Scholar]
- 7.Deeg DJH, van Tilburg T, Smit JH, de Leeuw ED (2002) Attrition in the Longitudinal Aging Study Amsterdam: The effect of differential inclusion in side studies. J Clin Epidemiol 55:319–328. 10.1016/S0895-4356(01)00475-9 [DOI] [PubMed] [Google Scholar]
- 8.Chang C-CH, Yang H-C, Tang G, Ganguli M (2009) Minimizing attrition bias: a longitudinal study of depressive symptoms in an elderly cohort. Int Psychogeriatr 21:869–878 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Feng D, Silverstein M, Giarrusso R, et al. (2006) Attrition of Older Adults in Longitudinal Surveys: Detection and Correction of Sample Selection Bias Using Multigenerational Data. J Gerontol B Psychol Sci Soc Sci 61:S323–S328 [DOI] [PubMed] [Google Scholar]
- 10.Jacomb PA, Jorm AF, Korten AE, et al. (2002) Predictors of refusal to participate: a longitudinal health survey of the elderly in Australia. BMC Public Health 2:1 10.1186/1471-2458-2-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Coley N, Gardette V, Toulza O, et al. (2008) Predictive Factors of Attrition in a Cohort of Alzheimer Disease Patients. Neuroepidemiology 31:69–79. 10.1159/000144087 [DOI] [PubMed] [Google Scholar]
- 12.Van Beijsterveldt CEM, van Boxtel MPJ, Bosma H, et al. (2002) Predictors of attrition in a longitudinal cognitive aging study:: The Maastricht Aging Study (MAAS). J Clin Epidemiol 55:216–223. 10.1016/S0895-4356(01)00473-5 [DOI] [PubMed] [Google Scholar]
- 13.Chatfield MD, Brayne CE, Matthews FE (2005) A systematic literature review of attrition between waves in longitudinal studies in the elderly shows a consistent pattern of dropout between differing studies. J Clin Epidemiol 58:13–19. 10.1016/j.jclinepi.2004.05.006 [DOI] [PubMed] [Google Scholar]
- 14.Kapteyn A, Michaud P-C, Smith J (2006) Effects of Attrition and Non-Response in the Health and Retirement Study. 44 [Google Scholar]
- 15.von Strauss E, Fratiglioni L, Jorm AF, et al. (1998) Attitudes and Participation of the Elderly in Population Surveys: Data from a Longitudinal Study on Aging and Dementia in Stockholm. J Clin Epidemiol 51:181–187. 10.1016/S0895-4356(97)00242-4 [DOI] [PubMed] [Google Scholar]
- 16.Zhivan NA, Ang A, Amaro H, et al. (2012) Ethnic/Race Differences in the Attrition of Older American Survey Respondents: Implications for Health-Related Research. Health Serv Res 47:241–254. 10.1111/j.1475-6773.2011.01322.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tyas SL, Tate RB, Wooldrage K, et al. (2006) Estimating the Incidence of Dementia: The Impact of Adjusting for Subject Attrition Using Health Care Utilization Data. Ann Epidemiol 16:477–484. 10.1016/j.annepidem.2005.09.006 [DOI] [PubMed] [Google Scholar]
- 18.Sliwinski MJ, Hofer SM, Hall C, et al. (2003) Modeling memory decline in older adults: the importance of preclinical dementia, attrition, and chronological age. Psychol Aging 18:658. [DOI] [PubMed] [Google Scholar]
- 19.Glymour MM, Chêne G, Tzourio C, Dufouil C (2012) Brain MRI markers and dropout in a longitudinal study of cognitive aging. Neurology 79:1340–1348. 10.1212/WNL.0b013e31826cd62a [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.O’Connor ML (2010) How does mobility change over time for older adults, and how are changes influenced by cognitive functioning? [Google Scholar]
- 21.Tan JE (2009) Functional abilities and mild cognitive impairment: investigation using the modified Scales of Independent Behavior-Revised. PhD Thesis [DOI] [PubMed] [Google Scholar]
- 22.Steinberg M, Shao H, Zandi P, et al. (2008) Point and 5-year period prevalence of neuropsychiatric symptoms in dementia: the Cache County Study. Int J Geriatr Psychiatry 23:170–7. 10.1002/gps.1858 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Aalten P, de Vugt ME, Jaspers N, et al. (2005) The course of neuropsychiatric symptoms in dementia. Part I: findings from the two-year longitudinal Maasbed study. Int J Geriatr Psychiatry 20:523–30. 10.1002/gps.1316 [DOI] [PubMed] [Google Scholar]
- 24.Kleinbaum D, Klein M (2012) Survival Analysis - A Self-Learning Text, Third. Springer, New York, NY [Google Scholar]
- 25.Beekly DL, Ramos EM, van Belle G, et al. (2004) The National Alzheimer’s Coordinating Center (NACC) Database: an Alzheimer disease database. Alzheimer Dis Assoc Disord 18:270–277 [PubMed] [Google Scholar]
- 26.Morris JC (1993) The Clinical Dementia Rating (CDR): Current version and scoring rules. Neurology 43:2412–2414 [DOI] [PubMed] [Google Scholar]
- 27.Pfeffer RI, Kurosaki TT, Harrah CH, et al. (1982) Measurement of functional activities in older adults in the community. J Gerontol 37:323–329 [DOI] [PubMed] [Google Scholar]
- 28.Cummings JL, Mega M, Gray K, et al. (1994) The Neuropsychiatric Inventory: comprehensive assessment of psychopathology in dementia. Neurology 44:2308–2308 [DOI] [PubMed] [Google Scholar]
- 29.Washington University Alzheimer’s Disease Research Center (1999) Global Clinical Dementia Rating (CDR) Based on CDR Box Scores, https://www.alz.washington.edu/cdrnacc.html. Accessed 21 Apr 2017 [Google Scholar]
- 30.McKhann GM, Knopman DS, Chertkow H, et al. (2011) The diagnosis of dementia due to Alzheimer’s disease: Recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement 7:263–269. 10.1016/j.jalz.2011.03.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yesavage JA, Brink TL, Rose TL, et al. (1982) Development and validation of a geriatric depression screening scale: A preliminary report. J Psychiatr Res 17:37–49. 10.1016/0022-3956(82)90033-4 [DOI] [PubMed] [Google Scholar]
- 32.StataCorp (2015) Stata Statistical Software: Release 14. StataCorp, College Station, TX [Google Scholar]
- 33.Cox DR (1972) Regression Models and Life-Tables. J R Stat Soc Ser B Methodol 34:187–220 [Google Scholar]
- 34.Weintraub S, Salmon D, Mercaldo N, et al. (2009) The Alzheimer’s Disease Centers’ Uniform Data Set (UDS): The Neuropsychological Test Battery. Alzheimer Dis Assoc Disord 23:91–101. 10.1097/WAD.0b013e318191c7dd [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Stang A, Jöckel KH (2004) Studies with low response proportions may be less biased than studies with high response proportions. Am J Epidemiol 159:204–210 [DOI] [PubMed] [Google Scholar]
- 36.Bhamra S, Tinker A, Mein G, et al. (2008) The retention of older people in longitudinal studies: A review of the literature. Qual Ageing Older Adults 9:27–35. 10.1108/14717794200800025 [DOI] [Google Scholar]
- 37.Vega S, Benito-León J, Bermejo-Pareja F, et al. (2010) Several factors influenced attrition in a population-based elderly cohort: Neurological disorders in Central Spain Study. J Clin Epidemiol 63:215–222. 10.1016/j.jclinepi.2009.03.005 [DOI] [PubMed] [Google Scholar]
- 38.Beekman ATF, Penninx BWJH, Deeg DJH, et al. (2002) The impact of depression on the well-being, disability and use of services in older adults: a longitudinal perspective. Acta Psychiatr Scand 105:20–27. 10.1034/j.1600-0447.2002.10078.x [DOI] [PubMed] [Google Scholar]
- 39.Eysenbach G (2005) The Law of Attrition. J Med Internet Res 7:e11 10.2196/jmir.7.1.e11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Reinwand DA, Crutzen R, Elfeddali I, et al. (2015) Impact of Educational Level on Study Attrition and Evaluation of Web-Based Computer-Tailored Interventions: Results From Seven Randomized Controlled Trials. J Med Internet Res 17:e228 10.2196/jmir.4941 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Burke SL, Maramaldi P, Cadet T, Kukull W (2016) Associations between depression, sleep disturbance, and apolipoprotein E in the development of Alzheimer’s disease: dementia. Int Psychogeriatr FirstView:1–16. 10.1017/S1041610216000405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Burke SL, Maramaldi P, Cadet T, Kukull W (2016) Neuropsychiatric symptoms and Apolipoprotein E: Associations with eventual Alzheimer’s disease development. Arch Gerontol Geriatr 65:231–238. 10.1016/j.archger.2016.04.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Butters MA, Young JB, Lopez O, et al. (2008) Pathways linking late-life depression to persistent cognitive impairment and dementia. Dialogues Clin Neurosci 10:345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Caraci F, Copani A, Nicoletti F, Drago F (2010) Depression and Alzheimer’s disease: Neurobiological links and common pharmacological targets. Eur J Pharmacol 626:64–71. 10.1016/j.ejphar.2009.10.022 [DOI] [PubMed] [Google Scholar]
- 45.Duara R, Loewenstein DA, Potter E, et al. (2008) Medial temporal lobe atrophy on MRI scans and the diagnosis of Alzheimer disease. Neurology 71:1986–1992. 10.1212/01.wnl.0000336925.79704.9f [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Price JL (2002) Limbic system. In: Ramachandran V (ed) Encyclopedia of the human brain. Academic Press. [Google Scholar]
- 47.Smith AD (2002) Imaging the progression of Alzheimer pathology through the brain. Proc Natl Acad Sci 99:4135–4137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Deeg DJH (2002) Attrition in longitudinal population studies: Does it affect the generalizability of the findings?: An introduction to the series. J Clin Epidemiol 55:213–215. 10.1016/S0895-4356(01)00472-3 [DOI] [Google Scholar]
- 49.Wu Q, Tchetgen EJT, Osypuk TL, et al. (2013) Combining direct and proxy assessments to reduce attrition bias in a longitudinal study. Alzheimer Dis Assoc Disord 27:207–212. 10.1097/WAD.0b013e31826cfe90 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Cottler LB, Compton WM, Ben-Abdallah A, et al. (1996) Achieving a 96.6 percent follow-up rate in a longitudinal study of drug abusers. Drug Alcohol Depend 41:209–217. 10.1016/0376-8716(96)01254-9 [DOI] [PubMed] [Google Scholar]
- 51.Andersen R, Newman JF (2005) Societal and Individual Determinants of Medical Care Utilization in the United States. Milbank Q 83 10.1111/j.1468-0009.2005.00428.x [DOI] [PubMed] [Google Scholar]
- 52.Ribisl KM, Walton MA, Mowbray CT, et al. (1996) Minimizing participant attrition in panel studies through the use of effective retention and tracking strategies: Review and recommendations. Eval Program Plann 19:1–25. 10.1016/0149-7189(95)00037-2 [DOI] [Google Scholar]
- 53.Varma DS, Hart M, McIntyre DS, et al. (2016) A Research Protocol to Test the Effectiveness of Text Messaging and Reminder Calls to Increase Service Use Referrals in a Community Engagement Program. JMIR Res Protoc 5 10.2196/resprot.5854 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Dennis BP, Neese JB (2000) Recruitment and Retention of African American Elders into Community-Based Research: Lessons Learned. Arch Psychiatr Nurs 14:3–11 [DOI] [PubMed] [Google Scholar]