Dear Editor,
Cancer-associated retinopathy (CAR) is a sight-threatening condition, wherein auto-antibodies are directed against retinal antigens. The rarity and chronicity of the disease complicate its diagnosis and management. The use of intravitreal dexamethasone implants for CAR has not been reported previously. Herein, we report a case of CAR treated over 6 months with immunosuppressive agents followed by intravitreal dexamethasone implants while monitoring plasma autoantibody levels to salvage remnant vision in the last functional eye. Written informed consent was obtained from the patient.
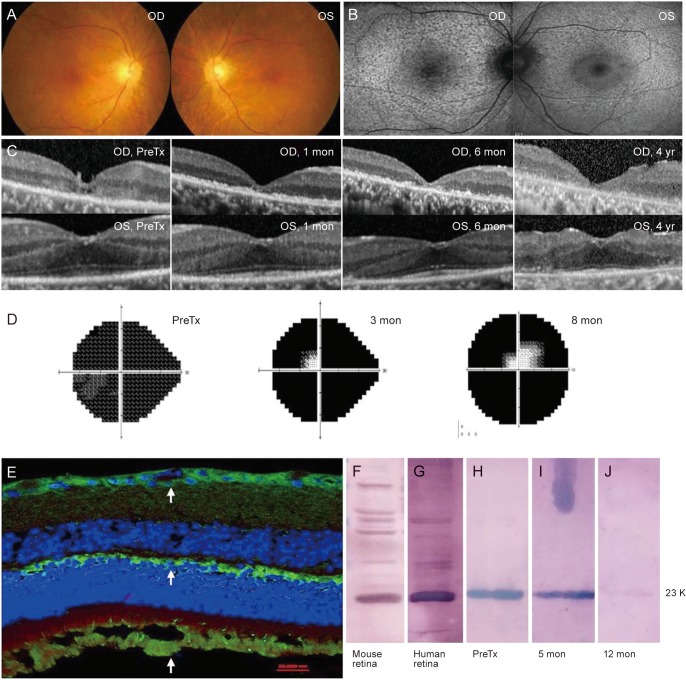
A 64-year-old man was referred for evaluation because of decreased vision in both eyes over 2 months. His best-corrected visual acuity was hand movement in the right eye and 20 / 32 in the left eye. He had no history of diabetes, hypertension, or autoimmune disorder. Slit lamp examination showed trace inflammatory cells in the anterior chambers and vitreous. Fundus examination and fluorescein angiography were unremarkable in both eyes (Fig. 1A). Fundus autofluorescence imaging showed hyperfluorescence in both eyes, except in the macula of the left eye (Fig. 1B). Spectral domain optical coherence tomography (OCT) (Spectralis OCT; Heidelberg Engineering, Heidelberg, Germany) revealed diffuse retinal thinning and photoreceptor disruption in both eyes, with small areas of intact photoreceptors in the central macula of the left eye (Fig. 1C). Humphrey visual field tests demonstrated global constriction in the left eye (Fig. 1D). Full-field electroretinography showed decreased rod and cone responses. Metastatic small-cell lung cancer was detected during systemic workup. With a differential diagnosis of CAR in mind, further tests were performed to reveal the presence of systemic auto-antibodies. Immunofluorescence imaging of a mouse retina treated with the patient's plasma showed antibody deposition on the photoreceptors, photoreceptor cell nuclei, and ganglion cells (Fig. 1E). Western blot analysis demonstrated antibody binding to a 23-kDa antigen of mouse/human retinal lysate in the patient's plasma (Fig. 1F, 1G) [1]. Additionally, the patient's plasma was positive for antigen-antibody reaction when tested with the recombinant protein recoverin (Fig. 1H). Based on diagnosis of CAR, immunosuppressive treatment with oral prednisolone (40 mg/day followed by tapering) and mycophenolate mofetil (1 g/day) was started. One month after treatment, foveal photoreceptor regeneration was observed on OCT. Humphrey perimetry showed a discernible central island at 3 months that was maintained for 8 months in the left eye. The patient's best-corrected visual acuity in the left eye improved to 20 / 16 at 2 months and to 20 / 25 at 6 months. Twelve months after treatment, the plasma anti-recoverin antibody titer had decreased dramatically (Fig. 1I, 1J). Despite the visual improvement, the long-term use of corticosteroid and methotrexate caused adverse events such as weight gain, cataract, and gastrointestinal problems. The patient underwent cataract surgery and received repeated intravitreal injections of dexamethasone implants (Ozurdex, 2 times) and triamcinolone acetonide (MaQaid, 11 times) at intervals of 2 to 4 months. Four years after presentation, a central-island visual field and foveal photoreceptors persisted on OCT of his left eye.
Fig. 1. Summary of clinical and diagnostic features. (A) Color fundus photography showing no apparent abnormalities. (B) Fundus autofluorescence image shows abnormal hyper-autofluorescence in both eyes except the macula of the left eye (OS). (C) Initial spectral domain optical coherence tomography revealing photoreceptor disruption around the fovea more severe in the right eye (OD) than OS. Serial optical coherence tomography images revealed regeneration of the foveal photoreceptor layer after treatment OS and the re-established photoreceptor layer gradually deteriorated during 4 years of follow-up. (D) Initial visual field test revealing global constriction OS. On follow-up 24-2 and 10-2 Humphrey visual field tests OS 3 and 8 months after treatment, a central island of visual field appeared and persisted for 8 months. (E) Immunofluorescence imaging of the mouse retina treated with the patient plasma shows the autoantibody deposition (arrows) on the photoreceptors, photoreceptor cell nuclei, and ganglion cells (green, anti-human IgG Fc Ab; red, peanut agglutinin; blue, DAPI). (F,G) On Western blot analysis, retinal lysate treated with patient plasma was positive for the antibody reaction with a 30 kDa retinal protein (F, mouse retinal lysate; G, human retinal lysate). (H) Patient plasma was positive for the antibody reaction with 23 kDa of the recombinant recoverin protein. (I,J) During the course of treatment, decrease in the titer of anti-recoverin autoantibody was observed (I, 5 months; J, 12 months after treatment, respectively). PreTx = pretreatment.
The etiology of CAR has been established as autoimmune activities of anti-retinal antibodies that react with photoreceptor outer segments and retinal ganglion cells [2]. Numerous immuno-modulatory therapies have been introduced to reduce CAR-related visual loss [3]. However, systemic corticosteroids and other immuno-modulatory therapies have shown limited success in preventing further vision loss and reducing circulating auto-antibodies levels [2,3,4]. Moreover, long-term use of systemic steroids and immunosuppressive agents can produce undesirable side effects. Therefore, local treatment with repeated or sustained-release corticosteroid agents could be a good alternative. Repeated use of intravitreal dexamethasone implants in eyes with non-infectious uveitis was associated with improved intraocular inflammation with tolerable side effects [5]. Similar pathogenic mechanisms between non-infectious uveitis and CAR indicate that the efficacy of repeated intravitreal dexamethasone implants and triamcinolone in non-infectious uveitis can be expected in CAR. In this case report, serial quantification of the plasma anti-recoverin autoantibody titer showed a marked decrease after 12 months of treatment. The reason for the decrease in the plasma autoantibody titer is speculated to be successful cancer treatment or systemic immunosuppressive therapy. Considering the good long-term treatment response, intravitreal dexamethasone implant and triamcinolone with monitoring of serum autoantibody titer may be useful when deciding the treatment regimen for CAR patients.
Acknowledgements
This study was supported by the National Research Foundation (NRF) grant (2016R1D1A1B03934724) and the NRF Bio & Medical Technology Development Program (2018M3A9B5021319) funded by the Korean government (MSIP and MSIT). The funding organization had no role in the design or conduct of this study.
Footnotes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
References
- 1.Forooghian F, Macdonald IM, Heckenlively JR, et al. The need for standardization of antiretinal antibody detection and measurement. Am J Ophthalmol. 2008;146:489–495. doi: 10.1016/j.ajo.2008.05.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Khan N, Huang JJ, Foster CS. Cancer associated retinopathy (CAR): an autoimmune-mediated paraneoplastic syndrome. Semin Ophthalmol. 2006;21:135–141. doi: 10.1080/08820530500350662. [DOI] [PubMed] [Google Scholar]
- 3.Grewal DS, Fishman GA, Jampol LM. Autoimmune retinopathy and antiretinal antibodies: a review. Retina. 2014;34:827–845. doi: 10.1097/IAE.0000000000000119. [DOI] [PubMed] [Google Scholar]
- 4.Kamei M, Fujitomi Y, Kondo Y, et al. Cancer-associated retinopathy after surgery for breast cancer: a case report and review of the literature. Surg Case Rep. 2018;4:10. doi: 10.1186/s40792-018-0418-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pohlmann D, Vom Brocke GA, Winterhalter S, et al. Dexamethasone inserts in noninfectious uveitis: a single-center experience. Ophthalmology. 2018;125:1088–1099. doi: 10.1016/j.ophtha.2017.12.038. [DOI] [PubMed] [Google Scholar]