Abstract
Animal experiments are widely used in preclinical medical research with the goal of disease modeling and exploration of novel therapeutic approaches. In the context of sepsis and septic shock, the translation into clinical practice has been disappointing. Classical animal models of septic shock usually involve one-sex-one-age animal models, mostly in mice or rats, contrasting with the heterogeneous population of septic shock patients. Many other factors limit the reliability of preclinical models and may contribute to preclinical research failure in critical care, including the host specificity of several pathogens, the fact that laboratory animals are raised in pathogen-free facilities and that organ support techniques are either absent or minimal. Advanced animal models have been developed with the aim of improving the clinical translatability of experimental findings. So-called animal ICUs refer to the preclinical investigation of adult or even aged animals of either sex, using—in case of rats and mice—miniaturized equipment allowing for reproducing an ICU environment at a small animal scale and integrating chronic comorbidities to more closely reflect the clinical conditions studied. Strength and limitations of preclinical animal models designed to decipher the mechanisms involved in septic cardiomyopathy are discussed. This article reviews the current status and the challenges of setting up an animal ICU.
Keywords: Animal models, Septic shock
Introduction
Animal experiments are widely used in preclinical medical research for modeling disease and for exploring novel therapeutic approaches. In the context of sepsis and septic shock, the translation into clinical practice has been fairly disappointing [1]. Clearly, models are to mirror key features of the condition to be studied, but, nevertheless, they are not capable of completely replicating all aspects due to inherent simplification. This issue was elegantly summarized by the British statistician George Box: “Essentially, all models are wrong, but some are useful” [2]. Certainly, in the context of sepsis and septic shock, the lacking translation of animal experiments to clinical practice is at least in part due to the complexity of the disease state per se. Moreover, the discrepancy between promising experimental findings and disappointing translation into the clinical setting has also been referred to the inappropriateness of the models used, which ultimately often results in “experimentally induced disturbances that usually diverge from naturally occurring human illness, precluding the replication of disease dynamics and time course” [3]. Moreover, the authors of the latter review stated that “experiments with more advanced supportive care[…], permitting the testing of drugs in a more realistic setting “ should be applied [1]. It is self-evident that this raises the question whether an “animal ICU” is necessary. An “animal ICU” refers to investigation of adult or even aged animals of either sex, eventually with underlying chronic comorbidities and with—in the case of rodents—miniaturized equipment allowing for reproducing an ICU environment, which would ideally integrate standard interventions (including antibiotics, fluids, monitoring) used in the clinical setting of sepsis (see below for details). This discussion is by no means new: Two decades ago, Daniel Traber already highlighted this problem: “Would you as a critical care physician accept data on a septic patient who was not resuscitated? Would you accept data from a drug study on an intensive care patient who was not only not resuscitated with fluid but who did not even have blood pressures and heart rates monitored? If the animals are resuscitated, is the resuscitation to a specific physiologic variable? The pathophysiology and outcome of an unresuscitated, unmonitored, septic patient is certainly different” [4]. The objectives of the present article are (1) to discuss the strengths and limitations of the currently used animal models of sepsis/septic shock, (2) to review the current status and the challenges of setting up an animal ICU and (3) to highlight the relevance of an ICU animal model in the specific example of the septic cardiomyopathy. In this context, this article is complementary to the most recent publications on the “Minimum quality threshold in pre-clinical sepsis studies (MQTIPSS)” initiative of the Wiggers Bernard Conference in Vienna, May 2017 [5–8].
Classical animal models of sepsis/septic shock: strengths and limitations
Do not abandon yet the mouse research ship
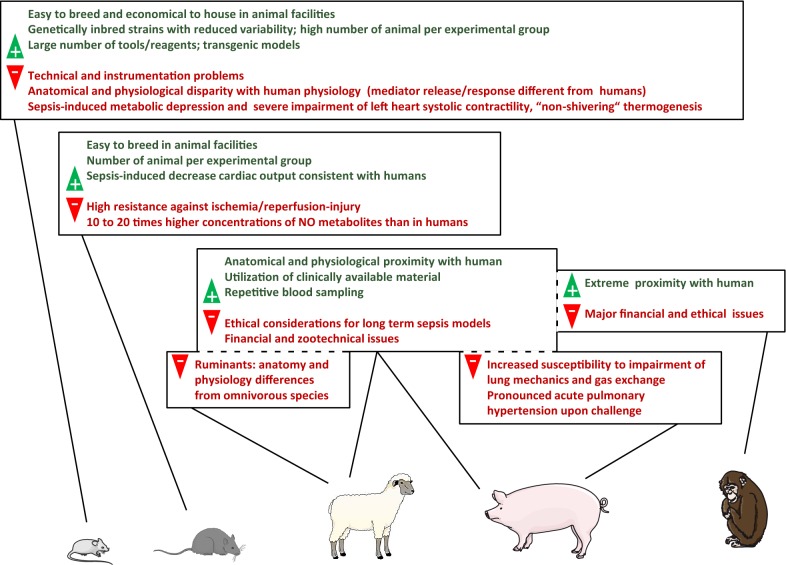
Animal models allow for testing hypotheses generated in patients using intact living systems, so that currently there is no better way to bridge between patients and the laboratory bench. When setting up an animal model, the question that immediately arises is: “Which species should be studied?” Clearly, the most frequently used species is the mouse because of the availability/price of the animals, the accessibility of specific reagents and the development of genetically modified mice. The “pros” and “cons” of the most frequently used mammal species are summarized in Fig. 1. Basic laboratory observations, mechanistic studies or pre-treatment assessment can be performed either by blocking or stimulating key pathways with specific effectors and/or by genetic manipulation, ultimately allowing sophisticated analysis. Gene editing permitted by the CRISPR-Cas9 system now gives the ability to change an organism’s DNA and has recently generated a lot of excitement in the scientific community [9]. There are obvious anatomical and physiological limitations while extrapolating results from a 20–30 g rodent to a 70–80 kg human adult. However, one has to remember that one of the most ground-breaking immunological discoveries was obtained in flies (Drosophila melanogaster): Toll pathway cascade and the subsequent characterization of toll-like receptors have reshaped our understanding of the immune system [10]. Indeed, it is important to keep in mind that even the most simplistic models, in particular mouse models, are potent experimental models for biological questions and/or proof-of-concept studies. A vast amount of researches over the last decades has resulted in the development of numerous examples of valid mouse-to-human translation [11]. These models are the key resource for many biological explorations. The problem of experimental variability can be easily overcome while studying small animals by increasing the sample size, whereas it can hardly be in larger species due to technical and financial concerns. A number of excellent reviews have highlighted interspecies anatomical and physiological differences to help in the selection of appropriate animal models and ensure successful transposition in the clinics [12–16]. Indeed, a major strength of mouse models is to be able to promptly test scientific hypothesis in proof-of-concept studies, whereas the investments in personnel, equipment and consumables to develop advanced animal models can be prohibitive in early stage projects. Indeed, both models (“regular” mice models and advanced animal models) have their own advantages and limitations, but their aims are different and both are needed.
Fig. 1.
“Pros” and “Cons” of experimental models for septic shock research
Why mouse models may poorly mimic human responses
Anatomical and physiological differences are probably the visible tip of the iceberg in terms of barriers to extrapolation from experimental models. Some other gaps are less obvious. First, age- and sex-matched animal models are carefully designed to standardize the confounding factors and to minimize heterogeneity of the results. Indeed, conclusions of experimental research are generally drawn from one-sex-one-age animal models (generally of young age to reduce the cost). In contrast, sepsis affects individuals of all ages, size/weights and sex. This “one size fits all” strategy is understandable in order to reduce animal consumption as recommended by the “3R” principles (“all efforts to replace, reduce, and refine experiments must be undertaken” [17]), but transposing the conclusions to a highly heterogeneous human population is questionable. Similarly, preclinical models cannot reproduce the full complexity of the clinically preexisting health conditions.
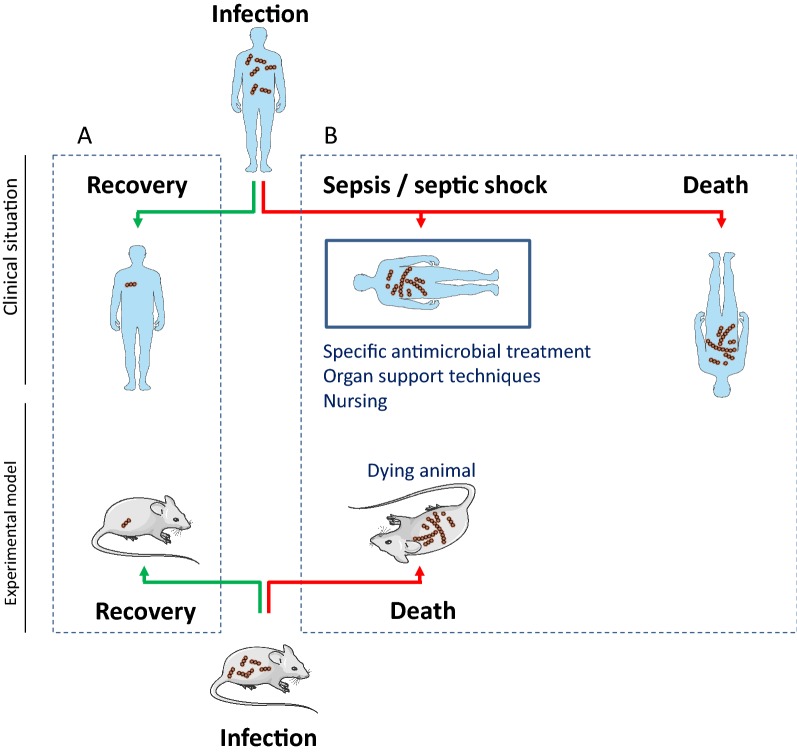
Second, regarding sepsis and host–pathogens interaction, a major problem is the host specificity of most pathogens [18–20]. As an example, mice are not susceptible to infection by human influenza A virus strains. Some of the virus strains must be adapted to be virulent in mice by serial passaging [21]. Similarly, our current understanding of immunology is largely defined in laboratory mice. However, there is growing concern that laboratory mice do not reflect relevant aspects of the human immune system, as laboratory mice have a less complex immune system and live in abnormally hygienic specific pathogen-free barrier facilities [22, 23]. Humans are infected with a variety of acute and chronic pathogens over the course of their lives, and pathogen-driven selection has shaped the immune system of humans. The same is likely true for mice. However, laboratory mice we use for most biomedical studies are bred in ultra-hygienic environments and are kept free of specific pathogens [24]. The immune system of a human adult is probably more closely replicated by mice caught in the wild or purchased in pet stores [22]. Indeed, mice with diverse environmental exposures have more mature immune responses, similar to human adults, whereas laboratory mice have immature or neonate-like immune systems. Moreover, in mouse models the genomic response to endotoxemia, trauma and burns was reported to only poorly mimic that of healthy volunteers and/or patients [25]. It is noteworthy in this context, however, that using the same database other authors came to exactly the opposite conclusion, i.e., that “mouse models greatly mimic human inflammatory diseases” [26]. Third, an animal with a severe infection has two options: rapidly succumb to sepsis or spontaneously recover. A human being with a severe infection has an “intermediate” possibility: surviving (i.e., prolonged critical illness permitted by health care). Severely ill patients are placed in an unphysiological status due to organ support techniques, specific drugs or, in more general terms, all treatments provided in the ICU. There is not a single mechanism at play, in contrast to the initially responsible disease, but a high variety of interplaying mechanisms including effects of all the therapeutic strategies involved. The spectrum of causes or effects is finally difficult to decipher. Because of the level of complexity, animal models incompletely replicate ICU patients. Septic ICU patients are compared with animals infected with lethal dose of microbial agents and killed at a time point defined by the expected survival curve (Fig. 2). Neither the long time course of the human disease nor the complex ICU environment/treatments could be accurately put into the equation.
Fig. 2.
Limits of classical animal models regarding sepsis/septic shock. a Infected animals are powerful models for basic laboratory observations and/or mechanistic studies of host/pathogen interactions. b Animals with a severe infection have two options, curing or dying, while human has an “intermediate” possibility, surviving. ICU patients represent an abnormal situation to an evolutionary view that is difficult to replicate. Infected animals with lethal dose of microbial agents are killed at a defined time point and compared with septic ICU patients. The ICU environment (monitoring, nursing) and treatments (specific antimicrobial treatment, organ support technics) are rarely reproduced in the animal models leading to an uncontrolled mismatch between animal models and “real life” of human care
Advanced animal models comprising full-scale ICU treatment
Do we need the development of miniaturized and sophisticated equipment to study resuscitated rodent models?
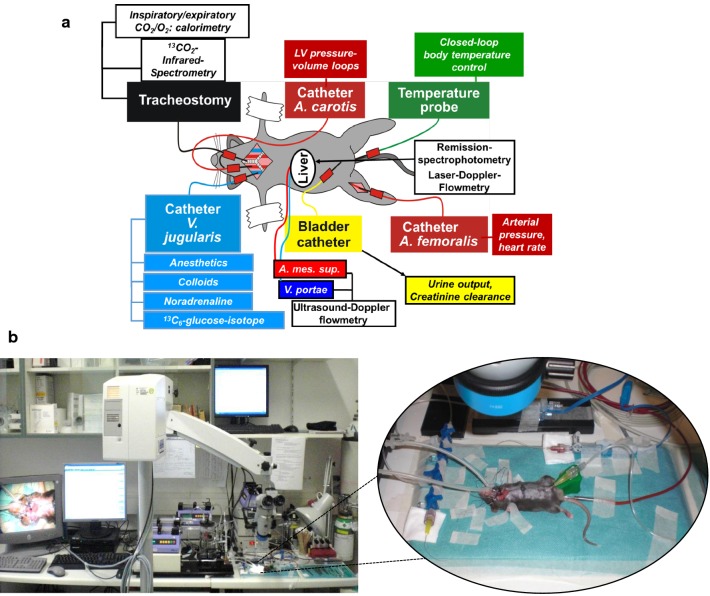
As mentioned above, Angus and van der Poll [1] suggested that experiments with more advanced supportive care would permit the testing of drugs in a more realistic setting. For models of sepsis and septic shock, this would ideally require providing appropriate antimicrobial treatment, hemodynamic monitoring together with adequate fluid resuscitation as well as—if necessary—vasopressor/inotropic support, and eventually (“lung-protective”) mechanical ventilation. Such a strategy of using resuscitated animals indeed increases the chance of successful translation of animal experiments to clinical practice: In fact, already in 2001, Hollenberg et al. demonstrated the impact of standard ICU treatment on mortality of polymicrobial septic shock. Combining fluid resuscitation with antibiotics allowed achieving a 46% survival at 48 h in a murine model of cecal ligation and puncture [27]. In other words, investigating resuscitated animals allowed for approximating mortality rates comparable to the clinical reality rather than studying an otherwise 100% lethal model. This approach also allowed to characterize the role of the inducible isoform of the nitric oxide synthase (iNOS). While 48-h survival did not significantly differ between wild type and iNOS knockout (iNOS−/−) in animals without ICU treatment (0 vs. 13%), iNOS−/− mice showed a markedly improved outcome, as compared with wild-type animals, after administration of antibiotics plus fluid resuscitation (55 vs. 24%) [28]. Moreover, development and miniaturization of sophisticated equipment has allowed for overcoming many technical problems that hindered or even prevented the establishment of ICU procedures in murine experiments (Fig. 3). This is particularly true for mechanical ventilation, which was originally harmful per se due to the lacking availability of appropriate small animal ventilators and/or the use of injurious ventilator settings, in particular as a result of high tidal volumes and/or inadequate positive end-expiratory pressure (PEEP) levels. In contrast, the recently developed small animal mechanical ventilators specifically designed for mice and/or rats allow for implementing “lung-protective” mechanical ventilation with the use of low tidal volumes (6–8 μL/g BW [29], adjustment of PEEP and maximum airway pressures according to gas exchange measurements, thereby following the guidelines of the ARDS Network and/or using the lower and upper inflection points obtained from the determination of pressure–volume curves [30], and inflation hold maneuvers to recruit atelectatic lung regions [31].
Fig. 3.
ICU environment in murine experiments. a Schematic representation of the monitored parameters; b representative illustration of miniaturization of sophisticated equipment used to reproduce the ICU environment in murine experiments; A. carotis, artery carotis; A. mes. sup., artery mesenteric superior; v. portae, vein portae; A. femoralis, artery femoralis
Do we need to study animal models in larger species?
Despite the above-mentioned technical advances, mice as experimental animals present with a major pitfall for translational research, namely due to their fundamentally different metabolic response to stress states resulting from their ability to rapidly reducing “non-shivering thermogenesis” and thereby core temperature [32]. Hence, hypothermia (if not corrected by external means) is a characteristic feature of the murine adaptive response to stress, whereas in larger species as well as in humans it is a mirror of whole body energetic failure (unless therapeutically induced). This problem can be overcome by replacing mice with rats, which, given the size of the individual animals, obviously also alleviates numerous technical and instrumentation problems. Indeed, during sepsis and septic shock, rats were demonstrated to much more closely resemble human beings than mice, in particular with respect to their long-term metabolic and cardiovascular profile [33]. Nevertheless, a word of caution should be left on the translational value of rat experiments, in particular in the context of circulatory shock: Nitric oxide (NO) is referred to as the “final mediator” of vasodilation and impaired vasoconstrictor response in septic shock, and the activity of the inducible isoform of the NO synthase (iNOS) is particularly pronounced in rats, which results in five- to tenfold higher nitrite and/or nitrate blood levels in septic and/or endotoxemic rats when compared to larger species (e.g., swine or sheep) and human beings [34–36]. Moreover, rats show pronounced antioxidant enzyme activity, which, together with the high NO release, makes them particularly resistant against ischemia/reperfusion (I/R) injury [37, 38].
Larger species, in particular when human-sized individual animals are studied, allow for utilizing clinically available material, which obviously facilitates anesthesia and surgical instrumentation, monitoring and the choice of interventional targets. Moreover, the large blood volume permits repetitive blood sampling and titration of readouts according to routinely available biomarkers as well as to physiological target endpoints, as in human. Sheep and swine are the most commonly used larger species, and various physiological parameters are even numerically comparable to the values found in age- and/or sex-matched patients. The “pros” and “cons” of this species are summarized in Fig. 1. As humans, they are monitored and/or vaccinated for specific pathogens and are exposed to an environment rich of microbial exposure. Nevertheless, despite the well-spread and the apparently close similarity of physiological and biological readouts, there are important species-specific differences to keep in mind. For example, sheep are ruminant animals and their gastrointestinal anatomy and physiology markedly differs from the omnivorous species swine, which translates into different kinetics of glucose metabolism. Swine rapidly develop profound acute pulmonary hypertension [39, 40] and are susceptible to impairment of lung mechanics and gas exchange [41, 42]. While in sheep, similar to human beings, measuring the creatinine clearance is an adequate marker of glomerular filtration rate (GFR) [43], this can result in overestimation of GFR in swine due to tubular creatinine secretion [44]. Currently, the mean duration of the ICU stays of patients for septic shock is one to several weeks. In contrast, the maximum duration of stay in an animal ICU is much shorter. Clearly, logistical constraints, in particular due to the required staff, assume major importance, but again, the choice of the species studied plays a major role, in particular with respect to the duration of mechanical ventilation (even without any additional challenge, e.g., circulatory shock and/or hyper-inflammatory conditions). The smaller the animal, the shorter the maximal duration of mechanical ventilation, even with the use of standard clinical ventilator settings to avoid injurious ventilation and, hence, to prevent or at least limit any ventilator-induced lung injury: Whereas the maximal duration of mechanical ventilation in mice and rats is 10–16 [45, 46] and 18–24 h [47, 48], respectively, larger species have been studied during much longer periods of mechanical ventilation, for even up to 48–96 h in sheep [49–52], 54 h in nonhuman primates [53] and 72–104 h in swine [54, 55]. Noteworthily, the limitation concerning one-sex-one-age in mice models (in contrast to the heterogeneous population of septic shock patients) still exists while using larger species.
Do we need to study animals with various age, sex and underlying comorbidities?
It is well established that age, sex and, in particular, chronic comorbidities markedly influence the outcome after sepsis and/or circulatory shock. This notion is also true for preclinical animal experiments, for which the importance of age, sex [56, 57] and/or underlying chronic diseases, including chronic obstructive pulmonary disease (COPD) [30, 58, 59] or cystic fibrosis [60], atherosclerosis [61], cancer [62], diabetes [63, 64] or even “psychological stress” [65], has been demonstrated. Indeed, preexisting coronary artery disease even completely abolished [66, 67] the otherwise promising results obtained in comparable experimental settings in young and healthy animals [68, 69]. Nevertheless, so far, the vast majority of experiments using an animal ICU, in particular when rodents are studied, investigate(d) young and healthy individuals. Clearly, it must be emphasized that since any added comorbidity will aggravate the burden to the animal, integrating comorbidity into the experimental design will necessarily create an ethical dilemma: Is it better to avoid comorbidities to reduce this burden but likely generate less relevant data, or include them expecting that a given comorbid setting might produce novel and translatable findings? [5, 62]. This dilemma obviously is also true for the use of mechanical ventilation, which per se may induce hemodynamic compromise and/or additional lung injury, but most likely will also allow for deeper anesthesia and sedation and thereby alleviate respiratory distress.
Contribution of animal experiments in our current understanding of sepsis: the example of septic cardiomyopathy
Although a precise definition of septic cardiomyopathy is still a matter of debate, cardiac dysfunction occurs in 40–60% of septic shock patients. It is entirely reversible in survivors within 10 days [70], but the presence of sepsis-related cardiac dysfunction is associated with increased short-term mortality [71–74]. Apart from causal treatments (antibiotics, surgical source control) and initial fluid resuscitation, no available treatment has been shown to improve the course of septic cardiomyopathy in humans [75]. As myocardial tissue is not easy to obtain from critically ill patients, only a few studies displayed data on the cellular mechanisms of human septic cardiomyopathy from the left ventricle of patients who died from sepsis [76–79]. To guide the understanding of the main causal mechanisms of human septic cardiomyopathy, most animal studies have used either endotoxin or fecal peritonitis models, with no or only limited resuscitation. Cecal ligation and puncture (CLP) models mimic the chronology of morphological features observed in human septic cardiomyopathy. Early in this model, prior to fluid resuscitation, animals show decreased cardiac output [80] with normal cardiac contractile performances of isolated perfused hearts [81]. At this stage, fluid resuscitation normalizes cardiac output, leading to the so-called hyperdynamic phase of sepsis [82]. Later on, animals that are more likely to die display decreased cardiac output [80] due to cardiac contractile dysfunction (i.e., the “hypodynamic phase of sepsis”) [81]. Conversely to the CLP model, endotoxin models (e.g., using bacterial lipopolysaccharide (LPS)) show very early cardiac contractile dysfunction, skipping the phase of hemodynamic disturbances with maintained cardiac performances [83, 84]. Surviving animals experience total recovery of their cardiac performances within 10 days [85–87]. Unlike endotoxin models, infected animals that mimic the different phases of human septic cardiomyopathy were very useful to analyze the early pathophysiological mechanisms of this syndrome. For example, CLP animals display an early increase in the adrenergic response of the cardiomyocytes, altering calcium sensitivity of cardiac myofibrillar proteins [81, 88–90]. This early mechanism is at least in part responsible for the later attenuation of adrenergic response and septic cardiomyopathy [81, 88–90]. Thus, these CLP-specific data helped researchers to hypothesize that preventing adrenergic stimulation in the early phase of sepsis might prevent cardiomyopathy to occur. Although CLP models are usually fluid-resuscitated, only a minority of the studies used antibiotic regimens [80, 82], and none of them performed complete causal treatments (i.e., both antibiotics administration and surgical source control). Therefore, one might hypothesize that like CLP models with only partial basic resuscitation, CLP models with full causal treatment could bring new significant insights on the pathophysiological mechanisms of septic cardiomyopathy (i.e., still “wrong” but maybe more “useful” models [2]).
Finally, preclinical trials on septic cardiomyopathy yielded conflicting results with poor extrapolation to critically ill patients. Several factors might explain the failure to detect new efficient drugs in this context. First, numerous preclinical experiments were performed on endotoxin models, known to poorly mimic human features of the septic cardiomyopathy [91–100]. Second, like mechanistic studies, although preclinical trials using fecal peritonitis models were usually fluid-resuscitated, none of them combined a causal treatments to the tested drugs [91, 101–108]. Third, only a few studies administered vasoconstrictors to maintain an appropriate systemic blood pressure when testing heart medications with vasodilator properties [107, 108]. Fourth, tested drugs were sometimes administered very early (< H4) [105, 106] after the induction of fecal peritonitis, or even before the insult [91, 92, 109]. All these factors might have favored the beneficial effects of the tested drugs and led to false positive results. Therefore, although sophisticated treatments (e.g., mechanical ventilation) may improve the quality of animal studies in the context of septic cardiomyopathy [110], implementation of the most basic causal treatments should be a prerequisite for future preclinical studies in this field.
Conclusion
Preclinical models have been widely used with the ultimate goals of improving the underlying mechanisms of the disease and exploring new therapeutic approaches. Simplistic models, in particular mouse models, are potent experimental models for biological questions and/or proof-of-concept studies but failed to bridge the translational gap to the clinic in the setting of septic shock. Using advanced animal models, namely integrating the investigation of adult (and/or aged) animals of either sex in the presence/absence of underlying chronic comorbidities under standardized animal ICU environments, i.e., by integrating as much as possible the standard interventions (including antibiotics, fluids, monitoring) used in the clinical setting of sepsis, will help to overcome the classical limitations of previous experimental studies performed on septic shock and enhance their translational value.
Acknowledgements
Dr. Radermacher received grants from the Deutsche Forschungsgemeinschaft (CRC 1149, GRK 2003) and the German Ministry of Defense
Abbreviations
- CLP
cecal ligation and puncture
- ICU
intensive care unit
Authors’ contributions
AG, SP, NDP and PR drafted the manuscript. All authors read, corrected and approved the final version of the manuscript.
Funding
None.
Availability of data and materials
Not applicable.
Competing interests
None.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Antoine Guillon, Email: antoine.guillon@univ-tours.fr.
Sebastien Preau, Email: seb.preau@gmail.com.
Jérôme Aboab, Email: jerome.aboab@gmail.com.
Eric Azabou, Email: eric.azabou@aphp.fr.
Boris Jung, Email: boris.jung@me.com.
Stein Silva, Email: silvastein@me.com.
Julien Textoris, Email: julien.textoris@biomerieux.com.
Fabrice Uhel, Email: fabrice.uhel@chu-rennes.fr.
Dominique Vodovar, Email: dominique.vodovar@aphp.fr.
Lara Zafrani, Email: lara.zafrani@aphp.fr.
Nicolas de Prost, Phone: + 33 1 49 81 23 94, Email: nicolas.de-prost@aphp.fr.
Peter Radermacher, Email: peter.radermacher@uni-ulm.de.
References
- 1.Angus DC, van der Poll T. Severe sepsis and septic shock. N Engl J Med. 2013;369:840–851. doi: 10.1056/NEJMra1208623. [DOI] [PubMed] [Google Scholar]
- 2.Box GEP. Robustness in the strategy of scientific model building. In: Launer RL, Wilkinson GN, editors. Robustness in statistics. Cambridge: Academic Press; 1979. pp. 201–236. [Google Scholar]
- 3.Marini JJ, Vincent J-L, Annane D. Critical care evidence–new directions. JAMA. 2015;313:893–894. doi: 10.1001/jama.2014.18484. [DOI] [PubMed] [Google Scholar]
- 4.Traber DL. Expired nitric oxide and shock in higher order species. Crit Care Med. 1999;27:255–256. doi: 10.1097/00003246-199902000-00021. [DOI] [PubMed] [Google Scholar]
- 5.Osuchowski MF, Ayala A, Bahrami S, Bauer M, Boros M, Cavaillon J-M, Chaudry IH, Coopersmith CM, Deutschman CS, Drechsler S, Efron P, Frostell C, Fritsch G, Gozdzik W, Hellman J, Huber-Lang M, Inoue S, Knapp S, Kozlov AV, et al. Minimum quality threshold in pre-clinical sepsis studies (MQTiPSS): an international expert consensus initiative for improvement of animal modeling in sepsis. Shock Augusta Ga. 2018;50:377–380. doi: 10.1097/SHK.0000000000001212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zingarelli B, Coopersmith CM, Drechsler S, Efron P, Marshall JC, Moldawer L, Wiersinga WJ, Xiao X, Osuchowski MF, Thiemermann C. Part I: minimum quality threshold in preclinical sepsis studies (MQTiPSS) for study design and humane modeling endpoints. Shock Augusta Ga. 2019;51:10–22. doi: 10.1097/SHK.0000000000001243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Libert C, Ayala A, Bauer M, Cavaillon J-M, Deutschman C, Frostell C, Knapp S, Kozlov AV, Wang P, Osuchowski MF, Remick DG. Part II: minimum quality threshold in preclinical sepsis studies (MQTiPSS) for types of infections and organ dysfunction endpoints. Shock Augusta Ga. 2019;51:23–32. doi: 10.1097/SHK.0000000000001242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hellman J, Bahrami S, Boros M, Chaudry IH, Fritsch G, Gozdzik W, Inoue S, Radermacher P, Singer M, Osuchowski MF, Huber-Lang M. Part III: minimum quality threshold in preclinical sepsis studies (MQTiPSS) for fluid resuscitation and antimicrobial therapy endpoints. Shock Augusta Ga. 2019;51:33–43. doi: 10.1097/SHK.0000000000001209. [DOI] [PubMed] [Google Scholar]
- 9.Ma Y, Zhang L, Huang X. Genome modification by CRISPR/Cas9. FEBS J. 2014;281:5186–5193. doi: 10.1111/febs.13110. [DOI] [PubMed] [Google Scholar]
- 10.Kawai T, Akira S. Toll-like receptors and their crosstalk with other innate receptors in infection and immunity. Immunity. 2011;34:637–650. doi: 10.1016/j.immuni.2011.05.006. [DOI] [PubMed] [Google Scholar]
- 11.Osuchowski MF, Remick DG, Lederer JA, Lang CH, Aasen AO, Aibiki M, Azevedo LC, Bahrami S, Boros M, Cooney R, Cuzzocrea S, Jiang Y, Junger WG, Hirasawa H, Hotchkiss RS, Li X-A, Radermacher P, Redl H, Salomao R, et al. Abandon the mouse research ship? Not just yet! Shock Augusta Ga. 2014;41:463–475. doi: 10.1097/SHK.0000000000000153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Guillon A, Sécher T, Dailey LA, Vecellio L, de Monte M, Si-Tahar M, Diot P, Page CP, Heuzé-Vourc’h N. Insights on animal models to investigate inhalation therapy: relevance for biotherapeutics. Int J Pharm. 2018;536:116–126. doi: 10.1016/j.ijpharm.2017.11.049. [DOI] [PubMed] [Google Scholar]
- 13.Guillon A, Pène F, de Prost N. Pour la commission de la recherche translationnelle de la SRLF. Modèles expérimentaux d’agression pulmonaire aiguë. Méd Intensive Réa. 2018.
- 14.Laffey JG, Kavanagh BP. Fifty years of research in ARDS. Insight into acute respiratory distress syndrome. From models to patients. Am J Respir Crit Care Med. 2017;196:18–28. doi: 10.1164/rccm.201612-2415CI. [DOI] [PubMed] [Google Scholar]
- 15.Tremblay LN, Slutsky AS. Ventilator-induced lung injury: from the bench to the bedside. Intensive Care Med. 2006;32:24–33. doi: 10.1007/s00134-005-2817-8. [DOI] [PubMed] [Google Scholar]
- 16.Ware LB. Modeling human lung disease in animals. Am J Physiol Lung Cell Mol Physiol. 2008;294:L149–L150. doi: 10.1152/ajplung.00472.2007. [DOI] [PubMed] [Google Scholar]
- 17.Russell WMS, Burch RL. The principles of humane experimental technique. London: Methuen; 1959. p. 238. [Google Scholar]
- 18.Bean AGD, Baker ML, Stewart CR, Cowled C, Deffrasnes C, Wang L-F, Lowenthal JW. Studying immunity to zoonotic diseases in the natural host—keeping it real. Nat Rev Immunol. 2013;13:851–861. doi: 10.1038/nri3551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bouvier NM. Animal models for influenza virus transmission studies: a historical perspective. Curr Opin Virol. 2015;13:101–108. doi: 10.1016/j.coviro.2015.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wolfe ND, Dunavan CP, Diamond J. Origins of major human infectious diseases. Nature. 2007;447:279–283. doi: 10.1038/nature05775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hocke AC, Suttorp N, Hippenstiel S. Human lung ex vivo infection models. Cell Tissue Res. 2017;367:511–524. doi: 10.1007/s00441-016-2546-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Beura LK, Hamilton SE, Bi K, Schenkel JM, Odumade OA, Casey KA, Thompson EA, Fraser KA, Rosato PC, Filali-Mouhim A, Sekaly RP, Jenkins MK, Vezys V, Haining WN, Jameson SC, Masopust D. Normalizing the environment recapitulates adult human immune traits in laboratory mice. Nature. 2016;532:512–516. doi: 10.1038/nature17655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Graham DM. A walk on the wild side. Lab Anim. 2017;46:423–427. doi: 10.1038/laban.1372. [DOI] [PubMed] [Google Scholar]
- 24.Tao L, Reese TA. Making mouse models that reflect human immune responses. Trends Immunol. 2017;38:181–193. doi: 10.1016/j.it.2016.12.007. [DOI] [PubMed] [Google Scholar]
- 25.Seok J, Warren HS, Cuenca AG, Mindrinos MN, Baker HV, Xu W, Richards DR, McDonald-Smith GP, Gao H, Hennessy L, Finnerty CC, López CM, Honari S, Moore EE, Minei JP, Cuschieri J, Bankey PE, Johnson JL, Sperry J, et al. Genomic responses in mouse models poorly mimic human inflammatory diseases. Proc Natl Acad Sci USA. 2013;110:3507–3512. doi: 10.1073/pnas.1222878110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Takao K, Miyakawa T. Genomic responses in mouse models greatly mimic human inflammatory diseases. Proc Natl Acad Sci USA. 2015;112:1167–1172. doi: 10.1073/pnas.1401965111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hollenberg SM, Dumasius A, Easington C, Colilla SA, Neumann A, Parrillo JE. Characterization of a hyperdynamic murine model of resuscitated sepsis using echocardiography. Am J Respir Crit Care Med. 2001;164:891–895. doi: 10.1164/ajrccm.164.5.2010073. [DOI] [PubMed] [Google Scholar]
- 28.Hollenberg SM, Broussard M, Osman J, Parrillo JE. Increased microvascular reactivity and improved mortality in septic mice lacking inducible nitric oxide synthase. Circ Res. 2000;86:774–778. doi: 10.1161/01.RES.86.7.774. [DOI] [PubMed] [Google Scholar]
- 29.Wagner F, Scheuerle A, Weber S, Stahl B, McCook O, Knöferl MW, Huber-Lang M, Seitz DH, Thomas J, Asfar P, Szabó C, Möller P, Gebhard F, Georgieff M, Calzia E, Radermacher P, Wagner K. Cardiopulmonary, histologic, and inflammatory effects of intravenous Na2S after blunt chest trauma-induced lung contusion in mice. J Trauma. 2011;71:1659–1667. doi: 10.1097/TA.0b013e318228842e. [DOI] [PubMed] [Google Scholar]
- 30.Hartmann C, Gröger M, Noirhomme J-P, Scheuerle A, Möller P, Wachter U, Huber-Lang M, Nussbaum B, Jung B, Merz T, McCook O, Kress S, Stahl B, Calzia E, Georgieff M, Radermacher P, Wepler M. In-depth characterization of the effects of cigarette smoke exposure on the acute trauma response and hemorrhage in mice. Shock Augusta Ga. 2019;51:68–77. doi: 10.1097/SHK.0000000000001115. [DOI] [PubMed] [Google Scholar]
- 31.Reiss LK, Kowallik A, Uhlig S. Recurrent recruitment manoeuvres improve lung mechanics and minimize lung injury during mechanical ventilation of healthy mice. PLoS ONE. 2011;6:e24527. doi: 10.1371/journal.pone.0024527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Radermacher P, Haouzi P. A mouse is not a rat is not a man: species-specific metabolic responses to sepsis—a nail in the coffin of murine models for critical care research? Intensive Care Med Exp. 2013;1:26. doi: 10.1186/2197-425X-1-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zolfaghari PS, Pinto BB, Dyson A, Singer M. The metabolic phenotype of rodent sepsis: cause for concern? Intensive Care Med Exp. 2013;1:25. doi: 10.1186/2197-425X-1-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mehta S, Javeshghani D, Datta P, Levy RD, Magder S. Porcine endotoxemic shock is associated with increased expired nitric oxide. Crit Care Med. 1999;27:385–393. doi: 10.1097/00003246-199902000-00047. [DOI] [PubMed] [Google Scholar]
- 35.Sharma AC, Motew SJ, Farias S, Alden KJ, Bosmann HB, Law WR, Ferguson JL. Sepsis alters myocardial and plasma concentrations of endothelin and nitric oxide in rats. J Mol Cell Cardiol. 1997;29:1469–1477. doi: 10.1006/jmcc.1997.0386. [DOI] [PubMed] [Google Scholar]
- 36.Tracey WR, Tse J, Carter G. Lipopolysaccharide-induced changes in plasma nitrite and nitrate concentrations in rats and mice: pharmacological evaluation of nitric oxide synthase inhibitors. J Pharmacol Exp Ther. 1995;272:1011–1015. [PubMed] [Google Scholar]
- 37.Godin DV, Garnett ME. Species-related variations in tissue antioxidant status–I. Differences in antioxidant enzyme profiles. Comp Biochem Physiol B. 1992;103:737–742. doi: 10.1016/0305-0491(92)90399-C. [DOI] [PubMed] [Google Scholar]
- 38.Godin DV, Garnett ME. Species-related variations in tissue antioxidant status–II. Differences in susceptibility to oxidative challenge. Comp Biochem Physiol B. 1992;103:743–748. doi: 10.1016/0305-0491(92)90400-L. [DOI] [PubMed] [Google Scholar]
- 39.Porta F, Takala J, Weikert C, Bracht H, Kolarova A, Lauterburg BH, Borotto E, Jakob SM. Effects of prolonged endotoxemia on liver, skeletal muscle and kidney mitochondrial function. Crit Care Lond Engl. 2006;10:R118. doi: 10.1186/cc5013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tucker A, McMurtry IF, Reeves JT, Alexander AF, Will DH, Grover RF. Lung vascular smooth muscle as a determinant of pulmonary hypertension at high altitude. Am J Physiol. 1975;228:762–767. doi: 10.1152/ajplegacy.1975.228.3.762. [DOI] [PubMed] [Google Scholar]
- 41.Kuriyama T, Latham LP, Horwitz LD, Reeves JT, Wagner WW. Role of collateral ventilation in ventilation-perfusion balance. J Appl Physiol. 1984;56:1500–1506. doi: 10.1152/jappl.1984.56.6.1500. [DOI] [PubMed] [Google Scholar]
- 42.Hedenstierna G, Hammond M, Mathieu-Costello O, Wagner PD. Functional lung unit in the pig. Respir Physiol. 2000;120:139–149. doi: 10.1016/S0034-5687(00)00099-2. [DOI] [PubMed] [Google Scholar]
- 43.Nawaz M, Shah BH. Renal clearance of endogenous creatinine and urea in sheep during summer and winter. Res Vet Sci. 1984;36:220–224. doi: 10.1016/S0034-5288(18)31983-0. [DOI] [PubMed] [Google Scholar]
- 44.Wendt M, Waldmann KH, Bickhardt K. Comparative studies of the clearance of inulin and creatinine in swine. Zentralbl Veterinarmed A. 1990;37:752–759. doi: 10.1111/j.1439-0442.1990.tb00969.x. [DOI] [PubMed] [Google Scholar]
- 45.Hegeman MA, Hemmes SNT, Kuipers MT, Bos LDJ, Jongsma G, Roelofs JJTH, van der Sluijs KF, Juffermans NP, Vroom MB, Schultz MJ. The extent of ventilator-induced lung injury in mice partly depends on duration of mechanical ventilation. Crit Care Res Pract. 2013;2013:435236. doi: 10.1155/2013/435236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Helmerhorst HJF, Schouten LRA, Wagenaar GTM, Juffermans NP, Roelofs JJTH, Schultz MJ, de Jonge E, van Westerloo DJ. Hyperoxia provokes a time- and dose-dependent inflammatory response in mechanically ventilated mice, irrespective of tidal volumes. Intensive Care Med Exp. 2017;5:27. doi: 10.1186/s40635-017-0142-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kroon AA, Wang J, Post M. Alterations in expression of elastogenic and angiogenic genes by different conditions of mechanical ventilation in newborn rat lung. Am J Physiol Lung Cell Mol Physiol. 2015;308:L639–L649. doi: 10.1152/ajplung.00293.2014. [DOI] [PubMed] [Google Scholar]
- 48.Lindqvist J, van den Berg M, van der Pijl R, Hooijman PE, Beishuizen A, Elshof J, de Waard M, Girbes A, Spoelstra-de Man A, Shi Z-H, van den Brom C, Bogaards S, Shen S, Strom J, Granzier H, Kole J, Musters RJP, Paul MA, Heunks LMA, et al. Positive end-expiratory pressure ventilation induces longitudinal atrophy in diaphragm fibers. Am J Respir Crit Care Med. 2018;198:472–485. doi: 10.1164/rccm.201709-1917OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Esechie A, Enkhbaatar P, Traber DL, Jonkam C, Lange M, Hamahata A, Djukom C, Whorton EB, Hawkins HK, Traber LD, Szabo C. Beneficial effect of a hydrogen sulphide donor (sodium sulphide) in an ovine model of burn- and smoke-induced acute lung injury. Br J Pharmacol. 2009;158:1442–1453. doi: 10.1111/j.1476-5381.2009.00411.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Chemonges S, Shekar K, Tung J-P, Dunster KR, Diab S, Platts D, Watts RP, Gregory SD, Foley S, Simonova G, McDonald C, Hayes R, Bellpart J, Timms D, Chew M, Fung YL, Toon M, Maybauer MO, Fraser JF. Optimal management of the critically ill: anaesthesia, monitoring, data capture, and point-of-care technological practices in ovine models of critical care. Biomed Res Int. 2014;2014:468309. doi: 10.1155/2014/468309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Yaghouby F, Daluwatte C, Fukuda S, Nelson C, Salsbury J, Kinsky M, Kramer GC, Strauss DG, Enkhbaatar P, Scully CG. Progression and variability of physiologic deterioration in an ovine model of lung infection sepsis. J Appl Physiol Bethesda Md. 1985;123:172–181. doi: 10.1152/japplphysiol.00122.2017. [DOI] [PubMed] [Google Scholar]
- 52.Kolobow T, Moretti MP, Fumagalli R, Mascheroni D, Prato P, Chen V, Joris M. Severe impairment in lung function induced by high peak airway pressure during mechanical ventilation. An experimental study. Am Rev Respir Dis. 1987;135:312–315. doi: 10.1164/arrd.1987.135.2.312. [DOI] [PubMed] [Google Scholar]
- 53.Guillon A, Pardessus J, Lhommet P, Parent C, Respaud R, Marchand D, Montharu J, De Monte M, Janiak P, Boixel C, Audat H, Huille S, Guillot E, Heuze-Vourc’h N. Exploring the fate of inhaled monoclonal antibody in the lung parenchyma by microdialysis. mAbs. 2019;11:297–304. doi: 10.1080/19420862.2018.1556081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Bogdanski R, Blobner M, Becker I, Hänel F, Fink H, Kochs E. Cerebral histopathology following portal venous infusion of bacteria in a chronic porcine model. Anesthesiology. 2000;93:793–804. doi: 10.1097/00000542-200009000-00029. [DOI] [PubMed] [Google Scholar]
- 55.Horst K, Simon TP, Pfeifer R, Teuben M, Almahmoud K, Zhi Q, Santos SA, Wembers CC, Leonhardt S, Heussen N, Störmann P, Auner B, Relja B, Marzi I, Haug AT, van Griensven M, Kalbitz M, Huber-Lang M, Tolba R, et al. Characterization of blunt chest trauma in a long-term porcine model of severe multiple trauma. Sci Rep. 2016;6:39659. doi: 10.1038/srep39659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Drechsler S, Weixelbaumer K, Raeven P, Jafarmadar M, Khadem A, van Griensven M, Bahrami S, Osuchowski MF. Relationship between age/gender-induced survival changes and the magnitude of inflammatory activation and organ dysfunction in post-traumatic sepsis. PLoS ONE. 2012;7:e51457. doi: 10.1371/journal.pone.0051457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Checchia PA, Schierding W, Polpitiya A, Dixon D, Macmillan S, Muenzer J, Stromberg P, Coopersmith CM, Buchman TG, Cobb JP. Myocardial transcriptional profiles in a murine model of sepsis: evidence for the importance of age. Pediatr Crit Care Med J Soc Crit Care Med World Fed Pediatr Intensive Crit Care Soc. 2008;9:530–535. doi: 10.1097/PCC.0b013e3181849a2f. [DOI] [PubMed] [Google Scholar]
- 58.Guillon A, Jouan Y, Brea D, Gueugnon F, Dalloneau E, Baranek T, Henry C, Morello E, Renauld J-C, Pichavant M, Gosset P, Courty Y, Diot P, Si-Tahar M. Neutrophil proteases alter the interleukin-22-receptor-dependent lung antimicrobial defence. Eur Respir J. 2015;46:771–782. doi: 10.1183/09031936.00215114. [DOI] [PubMed] [Google Scholar]
- 59.Kemmler J, Bindl R, McCook O, Wagner F, Gröger M, Wagner K, Scheuerle A, Radermacher P, Ignatius A. Exposure to 100% oxygen abolishes the impairment of fracture healing after thoracic trauma. PLoS ONE. 2015;10:e0131194. doi: 10.1371/journal.pone.0131194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Guillon A, Chevaleyre C, Barc C, Berri M, Adriaensen H, Lecompte F, Villemagne T, Pezant J, Delaunay R, Moënne-Loccoz J, Berthon P, Bähr A, Wolf E, Klymiuk N, Attucci S, Ramphal R, Sarradin P, Buzoni-Gatel D, Si-Tahar M, et al. Computed tomography (CT) scanning facilitates early identification of neonatal cystic fibrosis piglets. PLoS ONE. 2015;10:e0143459. doi: 10.1371/journal.pone.0143459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hartmann C, Loconte M, Antonucci E, Holzhauser M, Hölle T, Katzsch D, Merz T, McCook O, Wachter U, Vogt JA, Hoffmann A, Wepler M, Gröger M, Matejovic M, Calzia E, Georgieff M, Asfar P, Radermacher P, Nussbaum BL. Effects of hyperoxia during resuscitation from hemorrhagic shock in swine with preexisting coronary artery disease. Crit Care Med. 2017;45:e1270–e1279. doi: 10.1097/CCM.0000000000002767. [DOI] [PubMed] [Google Scholar]
- 62.Guillon A, Montharu J, Cormier B, Vecellio L, Diot P, de Monte M. New insights into the pathophysiology of aspiration pneumonia. Br J Anaesth. 2011;106:608–609. doi: 10.1093/bja/aer053. [DOI] [PubMed] [Google Scholar]
- 63.Collino M, Benetti E, Miglio G, Castiglia S, Rosa AC, Aragno M, Thiemermann C, Fantozzi R. Peroxisome proliferator-activated receptor β/δ agonism protects the kidney against ischemia/reperfusion injury in diabetic rats. Free Radic Biol Med. 2011;50:345–353. doi: 10.1016/j.freeradbiomed.2010.10.710. [DOI] [PubMed] [Google Scholar]
- 64.Dupuy V, Mayeur N, Buléon M, Jaafar A, Al Saati T, Schaak S, Praddaude F, Minville V, Tack I. Type 2 diabetes mellitus in mice aggravates the renal impact of hemorrhagic shock. Shock Augusta Ga. 2012;38:351–355. doi: 10.1097/SHK.0b013e318268810f. [DOI] [PubMed] [Google Scholar]
- 65.Langgartner D, Wachter U, Hartmann C, Gröger M, Vogt J, Merz T, McCook O, Fink M, Kress S, Georgieff M, Kunze JF, Radermacher PL, Reber SO, Wepler M. Effects of psychosocial stress on subsequent hemorrhagic shock and resuscitation in male mice. Shock Augusta Ga. 2018. [DOI] [PubMed]
- 66.Wepler M, Hafner S, Scheuerle A, Reize M, Gröger M, Wagner F, Simon F, Matallo J, Gottschalch F, Seifritz A, Stahl B, Matejovic M, Kapoor A, Möller P, Calzia E, Georgieff M, Wachter U, Vogt JA, Thiemermann C, et al. Effects of the PPAR-β/δ agonist GW0742 during resuscitated porcine septic shock. Intensive Care Med Exp. 2013;1:28. doi: 10.1186/2197-425X-1-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Matějková Š, Scheuerle A, Wagner F, McCook O, Matallo J, Gröger M, Seifritz A, Stahl B, Vcelar B, Calzia E, Georgieff M, Möller P, Schelzig H, Radermacher P, Simon F. Carbamylated erythropoietin-FC fusion protein and recombinant human erythropoietin during porcine kidney ischemia/reperfusion injury. Intensive Care Med. 2013;39:497–510. doi: 10.1007/s00134-012-2766-y. [DOI] [PubMed] [Google Scholar]
- 68.Simon F, Scheuerle A, Gröger M, Vcelar B, McCook O, Möller P, Georgieff M, Calzia E, Radermacher P, Schelzig H. Comparison of carbamylated erythropoietin-FC fusion protein and recombinant human erythropoietin during porcine aortic balloon occlusion-induced spinal cord ischemia/reperfusion injury. Intensive Care Med. 2011;37:1525–1533. doi: 10.1007/s00134-011-2303-4. [DOI] [PubMed] [Google Scholar]
- 69.Kapoor A, Shintani Y, Collino M, Osuchowski MF, Busch D, Patel NSA, Sepodes B, Castiglia S, Fantozzi R, Bishop-Bailey D, Mota-Filipe H, Yaqoob MM, Suzuki K, Bahrami S, Desvergne B, Mitchell JA, Thiemermann C. Protective role of peroxisome proliferator-activated receptor-β/δ in septic shock. Am J Respir Crit Care Med. 2010;182:1506–1515. doi: 10.1164/rccm.201002-0240OC. [DOI] [PubMed] [Google Scholar]
- 70.Vieillard-Baron A. Septic cardiomyopathy. Ann. Intensive Care. 2011;1:6. doi: 10.1186/2110-5820-1-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Charpentier J, Luyt C-E, Fulla Y, Vinsonneau C, Cariou A, Grabar S, Dhainaut J-F, Mira J-P, Chiche J-D. Brain natriuretic peptide: a marker of myocardial dysfunction and prognosis during severe sepsis. Crit Care Med. 2004;32:660–665. doi: 10.1097/01.CCM.0000114827.93410.D8. [DOI] [PubMed] [Google Scholar]
- 72.Sanfilippo F, Corredor C, Arcadipane A, Landesberg G, Vieillard-Baron A, Cecconi M, Fletcher N. Tissue Doppler assessment of diastolic function and relationship with mortality in critically ill septic patients: a systematic review and meta-analysis. Br J Anaesth. 2017;119:583–594. doi: 10.1093/bja/aex254. [DOI] [PubMed] [Google Scholar]
- 73.Sanfilippo F, Corredor C, Fletcher N, Tritapepe L, Lorini FL, Arcadipane A, Vieillard-Baron A, Cecconi M. Left ventricular systolic function evaluated by strain echocardiography and relationship with mortality in patients with severe sepsis or septic shock: a systematic review and meta-analysis. Crit Care Lond Engl. 2018;22:183. doi: 10.1186/s13054-018-2113-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Landesberg G, Jaffe AS, Gilon D, Levin PD, Goodman S, Abu-Baih A, Beeri R, Weissman C, Sprung CL, Landesberg A. Troponin elevation in severe sepsis and septic shock: the role of left ventricular diastolic dysfunction and right ventricular dilatation. Crit Care Med. 2014;42:790–800. doi: 10.1097/CCM.0000000000000107. [DOI] [PubMed] [Google Scholar]
- 75.Walley KR. Sepsis-induced myocardial dysfunction. Curr Opin Crit Care. 2018;24:292–299. doi: 10.1097/MCC.0000000000000507. [DOI] [PubMed] [Google Scholar]
- 76.Hotchkiss RS, Swanson PE, Freeman BD, Tinsley KW, Cobb JP, Matuschak GM, Buchman TG, Karl IE. Apoptotic cell death in patients with sepsis, shock, and multiple organ dysfunction. Crit Care Med. 1999;27:1230–1251. doi: 10.1097/00003246-199907000-00002. [DOI] [PubMed] [Google Scholar]
- 77.Takasu O, Gaut JP, Watanabe E, To K, Fagley RE, Sato B, Jarman S, Efimov IR, Janks DL, Srivastava A, Bhayani SB, Drewry A, Swanson PE, Hotchkiss RS. Mechanisms of cardiac and renal dysfunction in patients dying of sepsis. Am J Respir Crit Care Med. 2013;187:509–517. doi: 10.1164/rccm.201211-1983OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Matkovich SJ, Al Khiami B, Efimov IR, Evans S, Vader J, Jain A, Brownstein BH, Hotchkiss RS, Mann DL. Widespread down-regulation of cardiac mitochondrial and sarcomeric genes in patients with sepsis. Crit Care Med. 2017;45:407–414. doi: 10.1097/CCM.0000000000002207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Rossi MA, Celes MRN, Prado CM, Saggioro FP. Myocardial structural changes in long-term human severe sepsis/septic shock may be responsible for cardiac dysfunction. Shock Augusta Ga. 2007;27:10–18. doi: 10.1097/01.shk.0000235141.05528.47. [DOI] [PubMed] [Google Scholar]
- 80.Zanotti Cavazzoni SL, Guglielmi M, Parrillo JE, Walker T, Dellinger RP, Hollenberg SM. Ventricular dilation is associated with improved cardiovascular performance and survival in sepsis. Chest. 2010;138:848–855. doi: 10.1378/chest.09-1086. [DOI] [PubMed] [Google Scholar]
- 81.Wu LL, Tang C, Liu MS. Altered phosphorylation and calcium sensitivity of cardiac myofibrillar proteins during sepsis. Am J Physiol Regul Integr Comp Physiol. 2001;281:R408–R416. doi: 10.1152/ajpregu.2001.281.2.R408. [DOI] [PubMed] [Google Scholar]
- 82.Hollenberg SM, Dumasius A, Easington C, Colilla SA, Neumann A, Parrillo JE. Characterization of a hyperdynamic murine model of resuscitated sepsis using echocardiography. Am J Respir Crit Care Med. 2001;164:891–895. doi: 10.1164/ajrccm.164.5.2010073. [DOI] [PubMed] [Google Scholar]
- 83.Preau S, Delguste F, Yu Y, Remy-Jouet I, Richard V, Saulnier F, Boulanger E, Neviere R. Endotoxemia engages the RhoA kinase pathway to impair cardiac function by altering cytoskeleton, mitochondrial fission, and autophagy. Antioxid Redox Signal. 2016;24:529–542. doi: 10.1089/ars.2015.6421. [DOI] [PubMed] [Google Scholar]
- 84.Nevière R, Fauvel H, Chopin C, Formstecher P, Marchetti P. Caspase inhibition prevents cardiac dysfunction and heart apoptosis in a rat model of sepsis. Am J Respir Crit Care Med. 2001;163:218–225. doi: 10.1164/ajrccm.163.1.2003109. [DOI] [PubMed] [Google Scholar]
- 85.Natanson C, Danner RL, Fink MP, MacVittie TJ, Walker RI, Conklin JJ, Parrillo JE. Cardiovascular performance with E. coli challenges in a canine model of human sepsis. Am J Physiol. 1988;254:H558–H569. doi: 10.1152/ajpheart.1988.254.3.H558. [DOI] [PubMed] [Google Scholar]
- 86.Parrillo JE, Parker MM, Natanson C, Suffredini AF, Danner RL, Cunnion RE, Ognibene FP. Septic shock in humans. Advances in the understanding of pathogenesis, cardiovascular dysfunction, and therapy. Ann Intern Med. 1990;113:227–242. doi: 10.7326/0003-4819-113-3-227. [DOI] [PubMed] [Google Scholar]
- 87.Natanson C, Fink MP, Ballantyne HK, MacVittie TJ, Conklin JJ, Parrillo JE. Gram-negative bacteremia produces both severe systolic and diastolic cardiac dysfunction in a canine model that simulates human septic shock. J Clin Invest. 1986;78:259–270. doi: 10.1172/JCI112559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Tang C, Liu MS. Initial externalization followed by internalization of beta-adrenergic receptors in rat heart during sepsis. Am J Physiol. 1996;270:R254–R263. doi: 10.1152/ajpregu.1996.270.1.R254. [DOI] [PubMed] [Google Scholar]
- 89.Tang C, Yang J, Wu LL, Dong LW, Liu MS. Phosphorylation of beta-adrenergic receptor leads to its redistribution in rat heart during sepsis. Am J Physiol. 1998;274:R1078–R1086. doi: 10.1152/ajpregu.1998.274.4.R1078. [DOI] [PubMed] [Google Scholar]
- 90.Wu L-L, Yang S-L, Yang R-C, Hsu H-K, Hsu C, Dong L-W, Liu M-S. G protein and adenylate cyclase complex-mediated signal transduction in the rat heart during sepsis. Shock Augusta Ga. 2003;19:533–537. doi: 10.1097/01.shk.0000055816.40894.cd. [DOI] [PubMed] [Google Scholar]
- 91.Sanfilippo F, Santonocito C, Morelli A, Foex P. Beta-blocker use in severe sepsis and septic shock: a systematic review. Curr Med Res Opin. 2015;31:1817–1825. doi: 10.1185/03007995.2015.1062357. [DOI] [PubMed] [Google Scholar]
- 92.Pinto BB, Rehberg S, Ertmer C, Westphal M. Role of levosimendan in sepsis and septic shock. Curr Opin Anaesthesiol. 2008;21:168–177. doi: 10.1097/ACO.0b013e3282f43c56. [DOI] [PubMed] [Google Scholar]
- 93.Chagnon F, Coquerel D, Salvail D, Marsault E, Dumaine R, Auger-Messier M, Sarret P, Lesur O. Apelin compared with dobutamine exerts cardioprotection and extends survival in a rat model of endotoxin-induced myocardial dysfunction. Crit Care Med. 2017;45:e391–e398. doi: 10.1097/CCM.0000000000002097. [DOI] [PubMed] [Google Scholar]
- 94.Coquerel D, Chagnon F, Sainsily X, Dumont L, Murza A, Côté J, Dumaine R, Sarret P, Marsault É, Salvail D, Auger-Messier M, Lesur O. ELABELA improves cardio-renal outcome in fatal experimental septic shock. Crit Care Med. 2017;45:e1139–e1148. doi: 10.1097/CCM.0000000000002639. [DOI] [PubMed] [Google Scholar]
- 95.Cunha-Goncalves D, Perez-de-Sa V, Larsson A, Thörne J, Blomquist S. Inotropic support during experimental endotoxemic shock: part II. A comparison of levosimendan with dobutamine. Anesth Analg. 2009;109:1576–1583. doi: 10.1213/ane.0b013e3181af40e0. [DOI] [PubMed] [Google Scholar]
- 96.Cunha-Goncalves D, Perez-de-Sa V, Grins E, Dahm PL, Thörne J, Blomquist S. Inotropic support during experimental endotoxemic shock: part I. The effects of levosimendan on splanchnic perfusion. Anesth Analg. 2009;109:1568–1575. doi: 10.1213/ane.0b013e3181af3fe3. [DOI] [PubMed] [Google Scholar]
- 97.Beebe DS, Belani KG, Tuohy SE, Sweeney MF, Gillingham K, Komanduri V, Palahniuk RJ. Is dantrolene safe to administer in sepsis? The effect of dantrolene after endotoxin administration in dogs and rats. Anesth Analg. 1991;73:289–294. doi: 10.1213/00000539-199109000-00011. [DOI] [PubMed] [Google Scholar]
- 98.Wei X, Meng X, Yuan Y, Shen F, Li C, Yang J. Quercetin exerts cardiovascular protective effects in LPS-induced dysfunction in vivo by regulating inflammatory cytokine expression, NF-κB phosphorylation, and caspase activity. Mol Cell Biochem. 2018;446:43–52. doi: 10.1007/s11010-018-3271-6. [DOI] [PubMed] [Google Scholar]
- 99.Zhang N, Feng H, Liao H-H, Chen S, Yang Z, Deng W, Tang Q-Z. Myricetin attenuated LPS induced cardiac injury in vivo and in vitro. Phytother Res PTR. 2018;32:459–470. doi: 10.1002/ptr.5989. [DOI] [PubMed] [Google Scholar]
- 100.Wagner S, Schürmann S, Hein S, Schüttler J, Friedrich O. Septic cardiomyopathy in rat LPS-induced endotoxemia: relative contribution of cellular diastolic Ca(2 +) removal pathways, myofibrillar biomechanics properties and action of the cardiotonic drug levosimendan. Basic Res Cardiol. 2015;110:507. doi: 10.1007/s00395-015-0507-4. [DOI] [PubMed] [Google Scholar]
- 101.Cameron EM, Zhuang J, Menconi MJ, Phipps R, Fink MP. Dantrolene, an inhibitor of intracellular calcium release, fails to increase survival in a rat model of intra-abdominal sepsis. Crit Care Med. 1996;24:1537–1542. doi: 10.1097/00003246-199609000-00018. [DOI] [PubMed] [Google Scholar]
- 102.Fries M, Ince C, Rossaint R, Bleilevens C, Bickenbach J, Rex S, Mik EG. Levosimendan but not norepinephrine improves microvascular oxygenation during experimental septic shock. Crit Care Med. 2008;36:1886–1891. doi: 10.1097/CCM.0b013e31817cede9. [DOI] [PubMed] [Google Scholar]
- 103.Zausig YA, Geilfus D, Missler G, Sinner B, Graf BM, Zink W. Direct cardiac effects of dobutamine, dopamine, epinephrine, and levosimendan in isolated septic rat hearts. Shock Augusta Ga. 2010;34:269–274. doi: 10.1097/SHK.0b013e3181cd877b. [DOI] [PubMed] [Google Scholar]
- 104.Wang X, Ma S, Liu Y, Xu W, Li Z. Effects and mechanism analysis of combined infusion by levosimendan and vasopressin on acute lung injury in rats septic shock. Cell Biochem Biophys. 2014;70:1639–1645. doi: 10.1007/s12013-014-0107-1. [DOI] [PubMed] [Google Scholar]
- 105.Tsao C-M, Li K-Y, Chen S-J, Ka S-M, Liaw W-J, Huang H-C, Wu C-C. Levosimendan attenuates multiple organ injury and improves survival in peritonitis-induced septic shock: studies in a rat model. Crit Care Lond Engl. 2014;18:652. doi: 10.1186/s13054-014-0652-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Celes MRN, Malvestio LM, Suadicani SO, Prado CM, Figueiredo MJ, Campos EC, Freitas ACS, Spray DC, Tanowitz HB, da Silva JS, Rossi MA. Disruption of calcium homeostasis in cardiomyocytes underlies cardiac structural and functional changes in severe sepsis. PLoS ONE. 2013;8:e68809. doi: 10.1371/journal.pone.0068809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Rehberg S, Ertmer C, Vincent J-L, Spiegel H-U, Köhler G, Erren M, Lange M, Morelli A, Seisel J, Su F, Van Aken H, Traber DL, Westphal M. Effects of combined arginine vasopressin and levosimendan on organ function in ovine septic shock. Crit Care Med. 2010;38:2016–2023. doi: 10.1097/CCM.0b013e3181ef4694. [DOI] [PubMed] [Google Scholar]
- 108.Ji M, Li R, Li G, Fan Y, Dong L, Yang J, Peng YG, Wu J. Effects of combined levosimendan and vasopressin on pulmonary function in porcine septic shock. Inflammation. 2012;35:871–880. doi: 10.1007/s10753-011-9388-3. [DOI] [PubMed] [Google Scholar]
- 109.García-Septien J, Lorente JA, Delgado MA, de Paula M, Nin N, Moscoso A, Sánchez-Ferrer A, Perez-Vizcaino F, Esteban A. Levosimendan increases portal blood flow and attenuates intestinal intramucosal acidosis in experimental septic shock. Shock Augusta Ga. 2010;34:275–280. doi: 10.1097/SHK.0b013e3181cd8c5b. [DOI] [PubMed] [Google Scholar]
- 110.Cherpanath TGV, Smeding L, Hirsch A, Lagrand WK, Schultz MJ, Groeneveld ABJ. Low tidal volume ventilation ameliorates left ventricular dysfunction in mechanically ventilated rats following LPS-induced lung injury. BMC Anesthesiol. 2015;15:140. doi: 10.1186/s12871-015-0123-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.