Abstract
Mitogen-activated protein kinase kinase kinase 3 (MAP3K3), a member of the serine/threonine protein kinase family, is ubiquitously expressed and acts as an oncogene. However, the expression and exact molecular mechanism of MAP3K3 in ovarian carcinoma (OC) remain unclear. Here, we found that MAP3K3 protein was highly expressed in 70.5% of high-grade serous ovarian carcinoma (HGSOC) samples. MAP3K3 overexpression was significantly associated with the FIGO stage and chemotherapy response. Additionally, MAP3K3 overexpression was associated with reduced disease-free survival and overall survival. In vitro experiments showed that MAP3K3 overexpression promoted cell proliferation, inhibited apoptosis, and enhanced the migration and invasion of OC cells. Moreover, in vivo tumourigenesis experiments confirmed that silencing MAP3K3 significantly reduced the growth rate and volume of transplanted tumours in nude mice. Drug sensitivity experiments demonstrated that differential expression of MAP3K3 in OC cell lines correlates with chemotherapy resistance. Functionally, the MAP3K3 gene regulated the malignant biological behaviour of OC cells by mediating NF-κB signalling pathways, affecting the downstream epithelial-mesenchymal transition and cytoskeletal protein expression. Our results unveiled the role of MAP3K3 in mediating NF-κB signalling to promote the proliferation, invasion, migration, and chemotherapeutic resistance of OC cells, highlighting a potential new therapeutic and prognostic target.
Subject terms: Prognostic markers, Ovarian cancer, Oncogenes
Introduction
Ovarian carcinoma (OC) is one of the most common malignancies of the female genital organs, ranking eighth in the incidence and mortality of all female cancers worldwide1, with the highest mortality rate in gynaecological cancers in Western countries. Due to the lack of early clinical symptoms and biomarkers for diagnosis, most of them were diagnosed as late stages2. Current treatments mainly include chemotherapy and cytoreductive surgery3. There was no significant improvement in the overall survival rate of patients, mainly due to unclear pathogenesis and lack of targeted therapy. Therefore, there is an urgent need to find molecular markers and elucidate the molecular mechanisms related to the occurrence of OC.
Mitogen-activated protein kinase kinase kinase 3 (MAP3K3), also known as mitogen-activated protein kinase/extracellular signal-regulated kinase kinase kinase 3 (MAP3K3/MEKK3), belongs to the MAP3K family of serine/threonine kinases, and its dysregulated expression plays a vital role in the occurrence, invasion, and metastasis of several types of cancers, including OC, breast cancer, kidney cancer, and oesophageal cancer4–7. However, the molecular mechanism and role of MAP3K3 in OC development and progression have not yet been fully elucidated. Previously8, we found that MAP3K3 was highly expressed in OC tissues and cell lines, including serous ovarian carcinoma (SOC), mucinous ovarian carcinoma, endometrioid ovarian carcinoma, and clear cell ovarian carcinoma, and positively correlated with the poor prognosis of patients. To validate these results and eliminate the influence of confounding factors, we focused only on MAP3K3 function in high-grade serous ovarian carcinoma (HGSOC).
We determined the MAP3K3 expression in 105 tissue samples collected from patients diagnosed with HGSOC and in SOC cell lines and evaluated the correlation with clinical characteristics. We further aimed to elucidate the underlying mechanism by determining the effect of MAP3K3 on the nuclear factor-kappa B (NF-κB) signalling pathway, since several reports have shown that MAP3K3 was highly expressed endogenously in OC cells with persistent activation of the NF-κB signalling pathway9,10. Moreover, we evaluated the effect of MAP3K3 overexpression and silencing on the epithelial-mesenchymal transition (EMT) and expression of cytoskeletal proteins, and their effects on the growth, invasion behaviour, and chemotherapeutic resistance of OC cells. Finally, we studied the effect of MAP3K3 on tumour growth in vivo using a nude mouse model with silenced MAP3K3. These results can provide new insights into the oncogenic mechanisms in OC. Specifically, we hypothesised that MAP3K3 is an oncogene involved in OC by continuously activating the NF-κB signalling pathway, causing EMT and promoting invasion and metastasis. Thus, MAP3K3 might emerge as a new molecular target for the prognosis or treatment of OC.
Results
MAP3K3 was overexpressed in HGSOC tissues and associated with patient survival
TMA and immunohistochemical staining showed that all 105 HGSOC samples were positive for MAP3K3 expression, which was mainly localised in the cytoplasm. MAP3K3 overexpression (immunohistochemical score ≥100) was detected in 74 (70.5%) of the 105 HGSOC cases and 11 (35.5%) of the 31 normal samples. The expression level of MAP3K3 in HGSOC tissues was significantly higher than that in the normal fallopian tube epithelium (P < 0.05; Table 1).
Table 1.
Profiles of MAP3K3 expression in HGSOC and fallopian tube.
| n | MAP3K3 expression | χ2 | P | ||
|---|---|---|---|---|---|
| Overexpression (%) | Low expression (%) | ||||
| High-Grade Serous ovarian cancer | 105 | 74 (70.5) | 31 (29.5) | 12.504 | 0.000** |
| Fallopian tube | 31 | 11 (35.5) | 20 (64.5) | ||
The correlations of MAP3K3 protein expression with clinical-pathological parameters in the 105 HGSOC patients are summarised in Table 2. MAP3K3 overexpression was associated with FIGO stage III + IV (P = 0.003) and chemotherapeutic response (P = 0.049). No significant correlations were observed between MAP3K3 expression and other factors such as age (≤50 years vs > 50 years) and ascites (P > 0.05).
Table 2.
Correlation of MAP3K3 Expression with Clinicopathological Parameters in HGSOC Patients.
| Characteristics | N (105) | MAP3K3 expression | |||
|---|---|---|---|---|---|
| Overexpression | Low expression | χ2 | P | ||
| Age | |||||
| > 50 | 65 | 47 (72.3) | 18 (27.7) | 0.275 | 0.600 |
| ≤50 | 40 | 27 (67.5) | 13 (32.5) | ||
| FIGO stage | |||||
| I + II | 33 | 16 (48.5) | 17 (51.5) | 9.063 | 0.003** |
| III + IV | 39 | 32 (82.1) | 7 (17.9) | ||
| Unknown | 33 | ||||
| Ascites | |||||
| Yes | 45 | 31 (68.9) | 14 (31.1) | 0.835 | 0.361 |
| No | 16 | 9 (56.2) | 7 (43.8) | ||
| Unknown | 44 | ||||
| Chemotherapy response | |||||
| Sensitive | 39 | 20 (51.3) | 19 (48.7) | 3.892 | 0.049* |
| Partially sensitive | 12 | 10 (83.3) | 2 (16.7) | ||
| Unknown response | 54 | ||||
Abbreviations: HGSOC, High-Grade serous ovarian carcinoma.
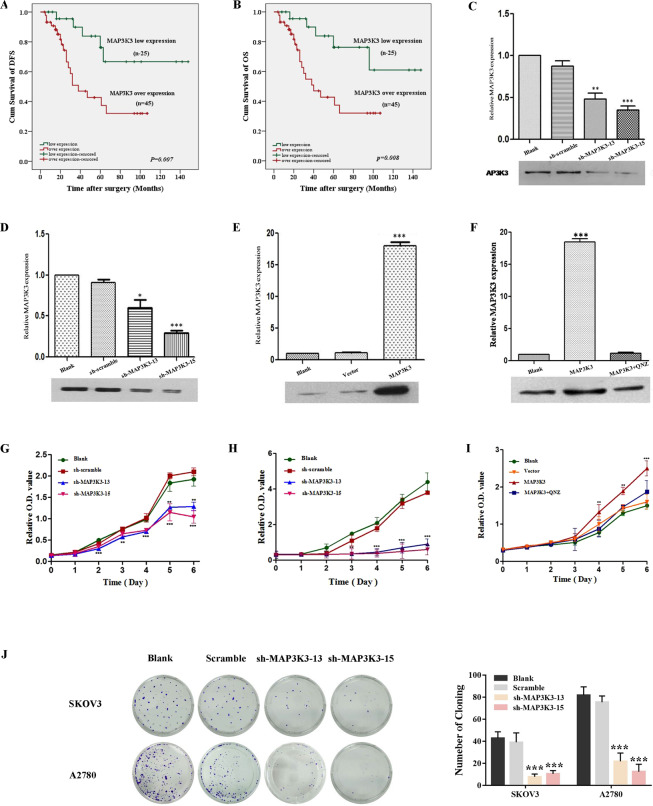
Furthermore, Kaplan-Meier survival analysis suggested that patients with MAP3K3 overexpression had a significantly shorter disease-free survival (DFS) time and overall survival (OS) time than those with low expression (P = 0.007, P = 0.008; Fig. 1A,B). Univariate analysis based on Cox regression models also showed that FIGO stage and chemotherapeutic response may be risk factors affecting HGSOC patients. In addition, multivariate analysis suggested that FIGO stage was an independent risk factor affecting the prognosis of HGSOC patients (Table 3). Collectively, these data indicated that MAP3K3 was overexpressed in HGSOC tissues and associated with patient survival.
Figure 1.
MAP3K3 was positively correlated with survival in HGSOC patients and affected human OC cell proliferation. Patients with MAP3K3 overexpression had shorter disease-free survival (A) and overall survival (B) than those with low MAP3K3 expression (P = 0.007, P = 0.008, respectively). The expression of MAP3K3 protein was detected by transfecting scramble and sh-MAP3K3 in SKOV3 (C) and A2780 (D) cells, and the protein expression of MAP3K3 was detected by transfecting MAP3K3 (E) and MAP3K3 + QNZ (F) in OV2008 cells. The CCK-8 assay (G,H) was used to detect cell proliferation, and a colony formation assay (J) was used to detect the colony forming ability of SKOV3 and A2780 cells. Effect of the overexpression of MAP3K3 and blocking the NF-κB signalling pathway (MAP3K3 + QNZ) in OV2008 cells on proliferation (I). Repeated three independent experiments, *means p < 0.05, **means p < 0.01, ***means p < 0.001.
Table 3.
Univariate and multivariate analyses of the associations between HGSOC Patient Risk Factors.
| Univariate | Multivariate | |||||
|---|---|---|---|---|---|---|
| HR | 95% CI | P | HR | 95% CI | P | |
| MAP3K3 (low vs overexpression) | 1.001 | 0.997–1.004 | 0.655 | 0.998 | 0.990–1.007 | 0.699 |
| Age (≤50 y vs > 50 y) | 0.999 | 0.960–1.038 | 0.947 | 1.020 | 0.932–1.115 | 1.020 |
| FIGO stage (I-II vs III-IV) | 1.931 | 1.197–3.115 | 0.007** | 3.918 | 1.096–13.999 | 0.036* |
| Ascites (no vs yes) | 1.094 | 0.349–3.432 | 0.878 | 1.247 | 0.100–15.532 | 0.864 |
| Chemotherapy response (sensitive vs partial) | 7.788 | 2.572–23.578 | 0.000*** | 13.129 | 0.899–191.787 | 0.060 |
Abbreviations: HR, hazard ratio; CI, confidence interval.
MAP3K3 affected human OC cell proliferation and migration in vitro
The protein and mRNA expression levels of MAP3K3 in OC cells had been detected in our previous study8. Our previous study showed that MAP3K3 were higher in the SOC cell lines than in control 293T cells. Compared with HeyA8, OVCA433, and OV2008 cells, MAP3K3 was relatively more highly expressed in SKOV3, A2780, and C13 cells.
CCK-8 proliferation assays showed that reducing MAP3K3 expression significantly inhibited the cell growth and proliferation of SKOV3 and A2780 cells, whereas MAP3K3 overexpression significantly promoted the proliferation of OV2008 cells (Fig. 1G–I). Moreover, the colony formation assays suggested that silencing MAP3K3 expression attenuated the colony-forming ability of SKOV3 and A2780 cells (Fig. 1J). Transwell migration and invasion assays and the wound-healing assay showed that silencing MAP3K3 expression attenuated the migration, invasion, and motility of SKOV3 and A2780 cells, while MAP3K3 overexpression of OV2008 cells had the opposite effects (Fig. 2A–F). Flow cytometry showed that silencing MAP3K3 promoted the apoptosis of SKOV3 and A2780 cells, whereas MAP3K3 overexpression inhibited the ability of OV2008 apoptosis (Fig. 2G–I).
Figure 2.
MAP3K3 affected human OC cell migration and apoptosis in vitro. Transwell migration and invasion experiment (A,B), cell scratch wound-healing assays (D,E), and flow cytometry (G,H) to detect the effect of MAP3K3 expression on biological function in SKOV3 and A2780 cells. Effect of MAP3K3 overexpression and blocking the NF-κB signalling pathway (MAP3K3 + QNZ) in OV2008 cells on cell migration and invasion (C), cell motility (F), and cell apoptosis (I). Repeated three independent experiments, *means p < 0.05, **means p < 0.01, ***means p < 0.001.
MAP3K3 promoted tumour growth of OC cells in vivo
To evaluate the effect of MAP3K3 expression on tumour growth in vivo, the established SKOV3/sh-MAP3K3, SKOV3/sh-Control, A2780/sh-MAP3K3, and A2780/sh-Control cell lines were injected subcutaneously into the left armpit of nude mice. Xenograft tumours of SKOV3 cells developed at the injection site after 14 days, whereas xenograft tumours of A2780 and OV2008 cells developed after 5 days. During a growth period of 21–28 days, primary tumours derived from SKOV3/sh-MAP3K3 (Fig. 3A,D) and A2780/sh-MAP3K3 cells grew significantly more slowly and were smaller than those derived from control cells (Fig. 3B,F). Primary tumours of OV2008/MAP3K3 cells were larger than those derived from control cells (Fig. 3C,H). Moreover, the weights of the xenograft tumours of the SKOV3/sh-MAP3K3 and A2780/sh-MAP3K3 groups were significantly lower than that of the control group (Fig. 3E–G), whereas contrasting results were observed in the OV2008/MAP3K3 group (Fig. 3I).
Figure 3.
MAP3K3 promoted the tumour growth of OC cells in vivo. Tumour volumes and weights of SKOV3 (A,D,E) and A2780 (B,F,G) cells with knockdown of MAP3K3 were decreased. Tumour volumes and weights of OV2008 (C,H,I) cells overexpressing MAP3K3 were increased. Compared to the respective control group at each time point; n = 10. Representative photographs of haematoxylin and eosin, MAP3K3, WT-1, Ki-67, BCL-2, BAX, E-cadherin, and vimentin immunohistochemistry staining of the primary tumour tissues from nude mice, with original magnification × 200 (J). Western blot analysis of the expression levels of MAP3K3, BCL-2, BAX, E-cadherin, vimentin, p-p65, and p65 in the primary tumour tissues (sh-Control and sh-MAP3K3 in SKOV3 cells) from nude mice (K). β-actin was used as an internal control.
Immunohistochemical staining showed that the sh-MAP3K3 groups of mice derived from SKOV3 cells expressed lower levels of MAP3K3 and had a lower cell proliferation index (as shown by Ki-67 staining) than the control group. Additionally, the expression level of the apoptosis-related factor BCL-2 in the MAP3K3 knockdown groups was lower than that of the control group, whereas the expression level of the anti-apoptotic factor BAX showed a reversed pattern. The expression level of the epithelial marker E-cadherin was also higher in the MAP3K3 knockdown groups than in the control group, and the expression level of the mesenchymal marker vimentin was slightly lower than that of the control group. The SOC marker WT-1 was expressed in both groups (Fig. 3J). Western blot analysis of the xenografts showed that MAP3K3 and BCL-2 expression in the sh-MAP3K3 group was lower than that in the control group, whereas the BAX expression was higher than that of the control group (Fig. 3K).
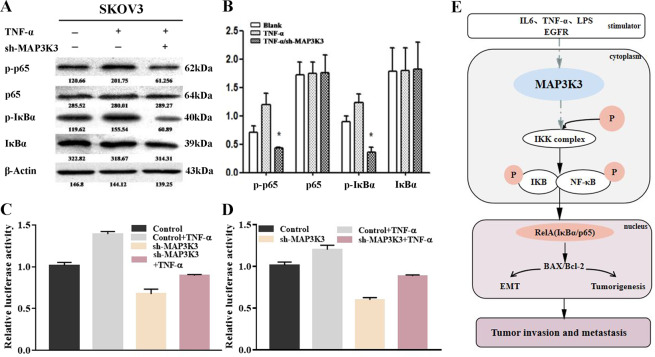
MAP3K3 regulates the activity of the NF-κB signalling pathway
We next explored the possible mechanism by which MAP3K3 promotes the migration and invasion of OC cells. After transfecting the NF-κB signalling pathway-activating factor TNF-α in SKOV3 cells and SKOV3/sh-MAP3K3 cells, we detected the expression of essential proteins of the NF-κB signalling pathway. p-p65 and p-IκBα expression levels were significantly upregulated after TNF-α stimulation of SKOV3 cells, while p65 and IκBα expression remained unchanged, demonstrating that TNF-α can effectively activate the NF-κB signalling pathway. After knockdown of MAP3K3 in SKOV3 cells, p-p65 and p-IκBα expressions were downregulated, and p65 and IκBα expressions were still unchanged, indicating that silencing MAP3K3 can inhibit activation of the NF-κB signalling pathway via TNF-α (Fig. 4A,B).
Figure 4.
Effect of MAP3K3 on the NF-κB signalling pathway. (A,B) Western blot to detect the inhibitory effect of MAP3K3 on NF-κB signalling in SKOV3 cells through different treatments of TNF-α (without/adding TNF-α/adding TNF-α + sh-MAP3K3). Detection of NF-κB signalling pathways in different cell treatment groups (Control/TNF-a/sh-MAP3K3/sh-MAP3K3 + TNF-a) in SKOV3 cells (C) and A2780 cells (D) by the luciferase reporter assay. Summary diagram showing cooperation between MAP3K3 and NF-κB-EMT signalling-related protein expression in OC (E).
The luciferase reporter assay conducted in SKOV3 and A2780 cells confirmed that the NF-κB signalling pathway was activated after the addition of TNF-α. After knockdown of MAP3K3, the activity of the NF-κB signalling pathway was significantly decreased. However, after the addition of TNF-α to SKOV3/sh-MAP3K3 cells, the activity of the NF-κB signalling pathway was restored (Fig. 4C,D).
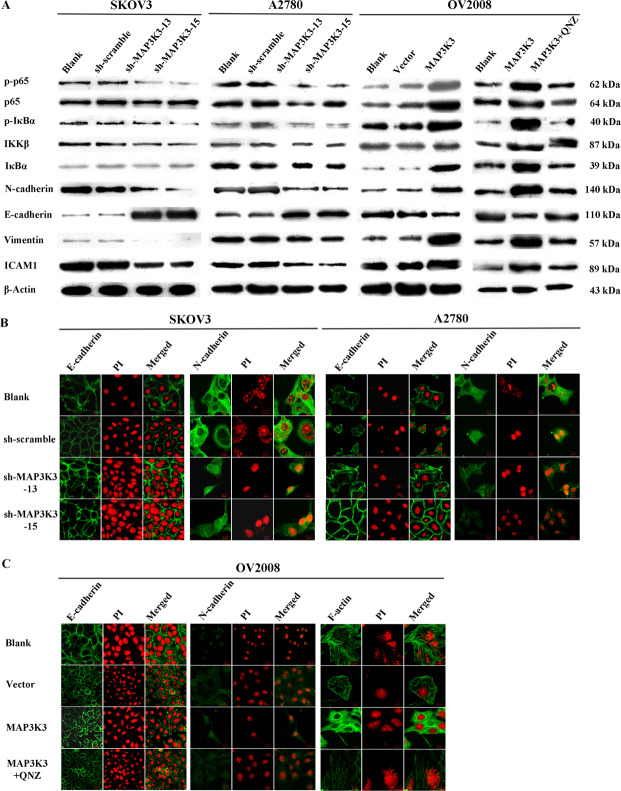
MAP3K3 affects NF-κB pathway activity and expression of EMT-related and cytoskeletal proteins
Western blot analysis showed that the expression levels of the NF-κB signalling pathway activity marker proteins p-p65 and p-IκBα were significantly downregulated in SKOV3/sh-MAP3K3 and A2780/sh-MAP3K3 cells compared to those of the control. The p65, IKKβ, and IκBα protein levels remained unchanged, whereas the expression of EMT markers N-cadherin, vimentin, and ICAM1 were downregulated, and E-cadherin expression was upregulated. After transient transfection of MAP3K3 in OV2008 cells, p-p65 and p-IκBα expression levels were significantly upregulated, and the expression levels of p65, IKKβ, and IκBα remained unchanged. N-cadherin, vimentin, and ICAM1 expression was upregulated, and that of E-cadherin was downregulated. After transfection of the MAP3K3 overexpression plasmid in OV2008 cells, the signal pathway activity was blocked using the specific NF-κB signalling pathway inhibitor QNZ, and the results of protein expression were reversed (Fig. 5A).
Figure 5.
MAP3K3 affects NF-κB pathway activity and expression of EMT-related and cytoskeletal proteins. (A) Western blot analysis of the effect of MAP3K3 expression on the expression of key proteins of the NF-κB signalling pathway and EMT-related proteins in SKOV3 cells (Blank, sh-scramble, sh-MAP3K3-13, sh-MAP3K3-15), A2780 cells (Blank, sh-scramble, sh-MAP3K3-13 and sh-MAP3K3-15) and OV2008 (Blank, vector, MAP3K3 and MAP3K3 + QNZ). (B) Immunofluorescence assay to detect the effect of knockdown of MAP3K3 on EMT-related proteins in SKOV3 and A2780 cells. (C) Overexpression of MAP3K3 and/or blocking of NF-κB signalling pathway altered the expression levels of E-cadherin and N-cadherin in OV2008 cells.
Immunofluorescence experiments showed that knocking down MAP3K3 in SKOV3 and A2780 cells resulted in more substantial expression of epithelial markers, while the expression of the mesenchymal marker N-cadherin decreased (Fig. 5B); MAP3K3 overexpression showed the opposite result in OV2008 cells. The transfection of MAP3K3 in OV2008 cells resulted in significantly reduced expression of the cytoskeletal protein F-actin, which consequently loosened the cell structure. After transfection of MAP3K3 and the NF-κB signalling pathway inhibitor QNZ, F-actin expression in OV2008 cells was increased (Fig. 5C). These results suggest that MAP3K3 affects EMT by regulating the expression of cytoskeletal proteins such as F-actin, which promotes the conversion of OC cell morphology into mesenchymal cells, to weaken adhesion between cells.
Overall, these data indicated that MAP3K3 activities the NF-κB signalling pathway, causing EMT and promoting the invasion and metastasis of OC (Fig. 4E).
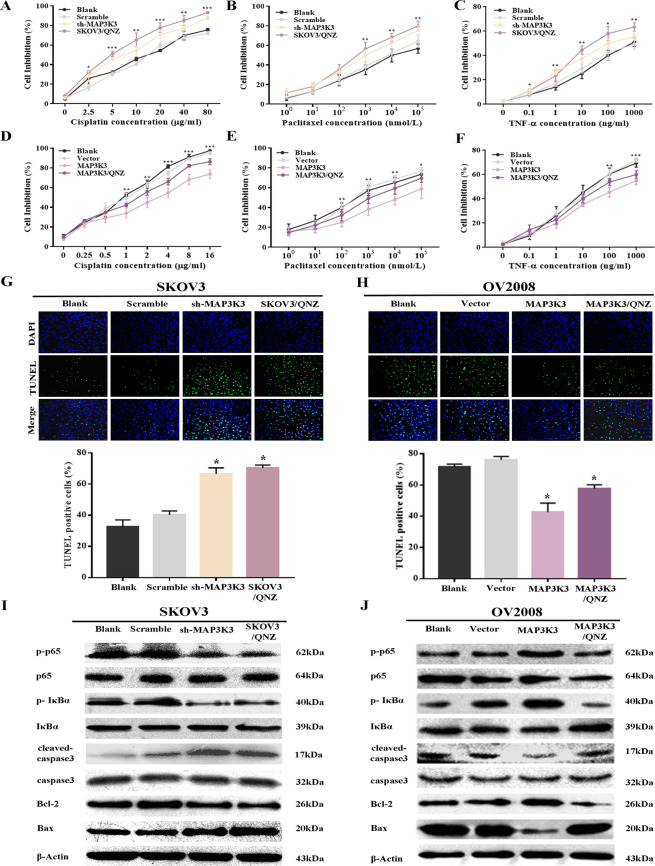
MAP3K3 contributed to chemotherapeutic resistance
The MTT assay showed that cisplatin inhibited the growth of SKOV3 cells. Knockdown of MAP3K3 expression or inhibition of the NF-κB signalling pathway in SKOV3 cells enhanced the ability of cisplatin to inhibit cell growth and the sensitivity of SKOV3 cells to cisplatin (Fig. 6A). MAP3K3 overexpression weakened the sensitivity of OV2008 cells to cisplatin, and blocking the NF-κB signalling pathway reversed this effect (Fig. 6D). Experiments with other common chemotherapeutic drugs such as paclitaxel and TNF-α showed the same results as above (Fig. 6B,C,E,F). The above results indicate that MAP3K3 promotes chemoresistance and thus weakens the inhibitory effects of chemotherapy drugs on tumour growth.
Figure 6.
Relationship between MAP3K3 and chemotherapeutic sensitivity. (A–C) MTT assay to detect the effect of knocking down MAP3K3 expression in SKOV3 cells or blocking the NF-κB pathway (SKOV3/QNZ) on the sensitivity to cisplatin (A), paclitaxel (B), and TNF-α (C). (D–F) MTT assay to detect the effect of overexpression of MAP3K3 and/or blocking of NF-κB pathway (MAP3K3/QNZ) on the sensitivity to cisplatin (D), paclitaxel (E), and TNF-α (F). (G,H) TUNEL assay to detect the cell apoptosis of four groups of cells induced by cisplatin in SKOV3 (G) and OV2008 (H) cells. Blue: nucleus; green: apoptotic cells. (I,J) Western blot to detect the effect of MAP3K3 on the NF-κB pathway and apoptosis-related proteins in SKOV3 (I, Blank, Scramble, sh-MAP3K3, Blank/QNZ) and OV2008 (J, Blank, Vector, MAP3K3 and MAP3K3/QNZ) cells. Repeated three independent experiments, *means p < 0.05, **means p < 0.01, ***means p < 0.001.
The TUNEL assay further showed that after knocking down MAP3K3 expression or inhibiting the NF-κB signalling pathway, the numbers of apoptotic cells in the SKOV3/sh-MAP3K3 and SKOV3/QNZ groups significantly increased (Fig. 6G). MAP3K3 overexpression in OV2008 cells showed a significantly decreased number of apoptotic cells. After MAP3K3 overexpression and NF-κB signalling pathway inhibition, the number of MAP3K3/QNZ apoptotic cells significantly increased, reaching a higher level than that of the OV2008/MAP3K3 group (Fig. 6H).
Treatment of the four groups of SKOV3 cells with a final concentration of 15 µg/ml cisplatin downregulated the expression of the critical factors of the NF-κB signalling pathway, p-p65 and p-IκBα, whereas the total protein expression of p65 and IκBα was unchanged. Thus, the activity of the NF-κB signal pathway was decreased. Expression of the anti-apoptotic protein BCL-2 was downregulated, and the expressions of pro-apoptotic proteins cleaved-caspase3 and BAX were upregulated (Fig. 6I). The four groups of cells treated with cisplatin at a final concentration of 1 µg/ml showed an opposite trend, and the activity of the NF-κB signalling pathway was enhanced to resist apoptosis. After MAP3K3 overexpression in OV2008 cells and simultaneous inhibition of the NF-κB signalling pathway by QNZ, the expression patterns of these proteins were reversed compared to those of the OV2008/MAP3K3 group (Fig. 6J). These results suggest that MAP3K3 activates downstream anti-apoptotic proteins via the NF-κB signalling pathway, inhibits the expression of pro-apoptotic proteins, and thus prevents the induction of apoptosis of OC cells by cisplatin.
Discussion
MAP3K3 plays an essential role in the development of early embryonic cardiovascular systems, endothelial cell proliferation, apoptosis, myocyte formation, and various inflammatory and immune responses11,12. Recently, abnormal amplification of MAP3K3 has attracted widespread attention, and MAP3K3 overexpression has been shown to play a cancer-promoting role in different types, such as oesophageal squamous cell carcinoma, non-small cell lung cancer, pancreatic cancer, hepatocellular carcinoma, and renal clear cell carcinoma13–17. However, He et al.7 reported that MAP3K3 overexpression in primary lung adenocarcinoma was positively correlated with good patient prognosis and negatively correlated with lung adenocarcinoma cell invasion and metastasis. MAP3K3 was also found to inhibit Hedgehog pathway-dependent medulloblastoma by inhibiting GLI1 function18. These contrasting results suggest that different tumour microenvironments play different roles in inducing MAP3K3. Here, we clarify the role of MAP3K3 overexpression in OC.
Currently, the reasons for overexpression of MAP3K3 are MAP3K3 amplification, RAS gene mutation, and the regulation of epigenetics. The genetic background of ovarian cancer is similar to that of breast cancer. Fan et al.4 found the amplification rate of MAP3K3 was only 21.5%, so the overexpression of MAP3K3 protein in some OC tissues may be due to its high copy amplification. In addition, the tissues and cell lines used in our experiments were high-grade serous ovarian carcinoma. The common molecular abnormalities in high-grade serous ovarian carcinoma included mutations of the RAS gene. Mutation of the upstream RAS gene directly leads to mitogen-activated protein kinase (MAPK) cascade activation. Our previous study19 found that the mutation rate of KRAS in serous ovarian carcinoma was only 8.6%, so the mutation of RAS gene also caused the overexpression of MAP3K3 in some ovarian carcinomas. A growing body of epigenetics shows that especially non-coding RNAs can exert powerful gene regulation and are widely involved in many biological processes such as chromatin recombination, transcriptional gene expression, and post-transcriptional regulation20,21. Therefore, the regulation of non-coding RNA aroused our interest, and we hypothesized that overexpression of MAP3K3 in ovarian carcinoma may be related to gene amplification, RAS gene mutation, and the regulation of epigenetics.
Excessive activation of the NF-κB signalling pathway has been widely detected in various malignancies and is involved in the regulation of many downstream transcription factors associated with malignant behaviour22–24. Similar to the findings of Samanta et al.9,10, we found that MAP3K3 was highly expressed in OC tissues and cells with persistent activation of the NF-κB signalling pathway. NF-κB activation in cells is under tight control. MAP3K3 is a crucial regulatory kinase that activates the NF-κB signalling pathway induced by TNF-α, IL-1, and LPS. The transcription factor complex RelA (IκBα/p65) is the most extensive and potent classical NF-κB activation pathway25,26. The regulatory mechanism of MAP3K3 may be mainly through the direct phosphorylation and activation of the IκB kinase (IKK), resulting in the phosphorylation and degradation of IκBα, the release of RelA that binds to IκBα, and activation of anti-apoptotic genes due to RelA nuclear entry9,27–29. Consistently, we found that MAP3K3 downregulation inhibited NF-κB signalling pathway activation by TNF-α, and downregulated p-p65 and p-IκBα (activator protein of the NF-κB signalling pathway) expression, suggesting that MAP3K3 is involved in the IκBα/p65 (RelA)-dependent pathway in OC cells to promote sustained NF-κB signalling pathway activation.
Studies in a variety of tumours have confirmed that activation of the NF-κB signalling pathway may lead to upregulation of transcription factors such as Twist and Snail, with subsequent EMT30,31. Downregulated MAP3K3 expression reduced the expression of markers of mesenchymal tissue but increased the epithelial marker E-cadherin. Thus, MAP3K3 appears to be a regulatory kinase of the NF-κB signalling pathway, and could promote OC invasion and metastasis via continuous activation of the NF-κB signalling pathway to induce EMT in OC. Theoretically, silencing MAP3K3 may block its downstream signalling pathway and reverse the malignant phenotype of OC.
Indeed, inhibiting MAP3K3 expression decreased activation of the NF-κB signalling pathway, resulting in significant reduction of the proliferation of OC cells and their resistance to apoptosis. Previous studies have confirmed that NF-κB promotes tumour cell proliferation by directly initiating transcription and promoting cyclin expression by binding to promoters of the live cyclins Cyclin D1, D2, D3 and c-Myc32,33. NF-κB can also inhibit cell death programs and DNA damage-induced apoptosis by activating the transcription and expression of BCL-2, inhibitor of apoptosis proteins family members, and the anti-apoptotic factor XIAP34–36. Thus, MAP3K3-mediated activation of the NF-κB signalling pathway may also induce the sustained proliferation and anti-apoptosis of OC cells by modulating these factors.
The MAPK and NF-κB signalling pathways are the central pathways mediating EMT37, and MAP3K3 is the key kinase in these two signalling pathways. The first step in cell movement is the protrusion of the cell’s front end, and F-actin is one of the main factors affecting this process. The polymerisation of F-actin can promote the formation of cell neurites38. While MAP3K3 overexpression resulted in upregulation of mesenchymal markers and downregulation of epithelial markers, we also detected a significant decrease in the expression of the cytoskeletal protein F-actin, which was upregulated after silencing MAP3K3. This suggests that decreased F-actin aggregation was associated with MAP3K3 overexpression and NF-κB signalling pathway activation, which may further promote cell morphological changes, migration, and invasion, although the specific mechanism remains to be further studied.
Methods
Specimens and patient data
We collected tumour tissue samples from 105 HGSOC patients and 31 normal oviduct tissues from healthy women visiting the Department of Pathology, Shihezi University School of Medicine from 1980 to 2017. The specimens were formalin-fixed, paraffin-embedded, and stained with haematoxylin and eosin using standard procedures. All subjects provided informed consent, and the study was approved and supervised by the Research Ethics Committee of the First Affiliated Hospital of Shihezi University School of Medicine. All experiments were performed in accordance with the Helsinki Declaration ethical guidelines.
Histopathological assessment was independently performed by two pathologists under a microscope. No patient received chemotherapy or radiotherapy before surgery. Owing to the longer duration of some cases, we were unable to collect complete clinical information for all the patients. Details of patients are provided in the Supplementary Table 1 (Table S1). As of December 5, 2017, 70 patients were followed up by an interview in the clinic or by telephone; there were 24 deaths, and 46 patients were still alive.
Tissue microarray (TMA) construction and immunohistochemistry
TMAs, histological and immunohistochemical staining of the tissue sections were performed as described previously8,39. Immunohistochemistry results were evaluated independently by two pathologists with a semi-quantitative scoring method based on staining intensity as follows40: the percentage of positive cells (range, 0–100%) was multiplied by the staining intensity score (1, buff; 2, yellow; and 3, brown). Scores ≥100 were classified as overexpression, whereas those <100 were classified as low expression.
Cell lines and culture conditions
SKOV3 (a highly metastatic SOC cell line), HeyA8 (a human SOC cell line), and 293T (a human embryonic kidney epithelial cell line) cells were purchased from the Chinese Academy of Sciences Type Culture Collection (Shanghai, China). OVCA433 (a human SOC cell line) and A2780 (a low metastatic potential cell line) cells were generously provided by Dr Gang Chen (Department of Gynecology and Obstetrics, Tongji Hospital of Huazhong University of Science and Technology). OV2008 (sensitive to cisplatin) and C13* (cisplatin-resistant line derived from OV2008 cells) cells were obtained from Prof Benjamin K. Tsang (Ottawa Health Research Institute, Ottawa, Canada)41. The cells were cultured in RPMI-1640 (Gibco, Life Technologies, Shanghai, China) medium supplemented with 10% heat-inactivated foetal bovine serum (Biological Industries, Kibbutz Beit Haemek, Israel) at 37 °C in a constant temperature and humidified incubator containing 5% CO2.
Expression plasmids and stably transfected cell lines
To study the effect of MAP3K3 on the OC cell lines SKOV3, A2780, and OV2008, four cell lines showing stable low MAP3K3 expression were established: SKOV3/sh-MAP3K3-13, SKOV3/sh-MAP3K3-15, A2780/sh-MAP3K3-13, and A2780/sh-MAP3K3-15, respectively. Additionally, the MAP3K3 transient overexpression cell lines OV2008/MAP3K3 and OV2008/MAP3K3 + QNZ (EVP4593, Selleck, USA) were established.
Details on MAP3K3 expression vector construction, short hairpin RNA (shRNA) expression vectors (sh-MAP3K3) and control (sh-Control), and cell line construction methods are provided in the Supplementary Information.
The human MAP3K3 expression vector pBabe-MAP3K3-WT-V5-His (MAP3K3), short hairpin RNA (shRNA) expression vectors specific to MAP3K3 p-super-shRNA-MAP3K3-13 (sh-MAP3K3-13) and p-super-shRNA-MAP3K3-15 (sh-MAP3K3-15), and random sequence interference expression vector p-super-shRNA-Scramble (sh-scramble) were generous gifts from Prof Jianhua Yang (Baylor College of Medicine, TX, Houston, USA). The retroviral expression vector for MAP3K3 shRNA was constructed by subcloning sh-MAP3K3 into the pSIH1-H1-copGFP vector in our lab.
Western blot analysis
Western blot analysis was performed as described previously8. Cells were incubated with the primary antibodies at a dilution of 1:1000 against MAP3K3 (ab40756), and E-cadherin (ab76055) obtained from Abcam; and with antibodies against N-cadherin (#13116), p-p65 (#3033), p-IκBa (#9246), IKKa (#2682), IKKβ (#2684), ICAM1 (#4915), vimentin (#5741), and p65 (#6956) obtained from Cell Signaling Technology (Danvers, MA, USA). The antibodies against β-actin (1:1000 dilution), F-actin (1:100 dilution), and fluorescein isothiocyanate-conjugated goat anti-rabbit IgG-H&L (1:10000 dilution) were obtained from ZSGB-BIO. MAP3K3 protein levels were detected using a secondary antibody conjugated to horseradish peroxidase. The protein signals were detected with an enhanced chemiluminescence kit (Thermo, Waltham, MA, USA). β-Actin was used as a loading control. All images were obtained by GEL-DOC2000 Imager (Bio-Rad, USA) and processed by its built-in software (Image Lab).
Immunofluorescence
Immunofluorescence analysis was performed as described previously8,42. Cells were incubated with the antibodies against MAP3K3 (1:50 dilution), E-cadherin (1:100 dilution), and N-cadherin (1:100 dilution).
Dual-luciferase reporter gene assay
The cells were seeded in 48-well plates (300 µl/well) and grown for 18–24 h. Transfection solution A was diluted in serum-free Opti-MEM with NF-κB-Luc and Renilla (50 µl). Solution B was diluted in serum-free medium Opti-MEM Liposomes Lipofectamine 2000 Reagent (50 µl, Invitrogen, USA) for 5 min. The cells were then transfected with solutions A and B and cultured for 48 h. Gene activity was detected with a luciferase reporter assay using Dual Luciferase Reporter Assay Kit (Promega, USA) according to the manufacturer’s instructions. The activity of Renilla luciferase was used as a control. The relative light unit (RLU) was detected by the GloMax 96 microplate luminometer. The activation intensity of the reporter gene was then calculated as the ratio of the RLU of firefly luciferase to that of Renilla luciferase.
Proliferation assay
SKOV3, A2780, and OV2008 cells were incubated and transfected with the different treatments as described above for 48 h, and the Cell Counting Kit-8 (CCK-8) assay was performed to construct the cell growth curve. The optical density (OD) value was determined by measuring absorbance at 450 nm with a microplate reader at the same time every day until the sixth day from the beginning of cell attachment. The daily OD values of each group of cells were used to draw the cell growth curve.
Apoptosis detection with flow cytometry
The Annexin V/FITC Apoptosis Kit (Lianke Biological, Hangzhou, China) was used to detect the apoptosis rate of treated transfected cells, which was quantified with a FACSCalibur flow cytometer (Becton-Dickinson, USA) using CellQuest software.
Colony formation assays
A cell suspension (400 μl/well) and 2 ml medium were added to a six-well plate. After visualising the colonies at 10–14 days of culture, the plates were washed, fixed, and stained (Crystal Violet Staining Solution, Beyotime, China). The number of colonies with more than 50 cells in a low-magnification visual field was counted, and the following formula was used to calculate the colony formation rate: clone formation rate = (number of clones/seeded cells) × 100%.
Wound-healing assay
The cells were seeded in six-well plates and cultured until full confluence was reached. Uniform scratches were made in the centre of the wells. The plates were washed and cultured in serum-free RPMI1640 medium without a penicillin-streptomycin mixture. Scratches were observed every 0 h, 12 h, 24 h, and 48 h. Statistical analysis of the areas before and after healing was conducted using the IPP statistical software.
Transwell migration and invasion assays
Transwell migration and invasion assays were performed as described previously43. The migration and invasion abilities of OC cells with the different treatments were measured using Boyden chambers (8-mm pore size; Thermo Fisher Scientific, USA).
Chemoresistance assay
SKOV3 and OV2008 cells of different treatment groups were incubated with various concentrations of cisplatin (Sigma-Aldrich, USA), paclitaxel, and tumour necrosis factor-alpha (TNF-α) for 48 h based on a previously reported cisplatin concentration gradient9,10. The 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyl tetrazolium bromide (MTT) assay was then performed to determine the cell inhibition ratio. The terminal deoxynucleotidyl transferase-mediated dUTP nick end labelling (TUNEL) assay was used to detect the degree of cell apoptosis using the One Step TUNEL Apoptosis Assay Kit (Beyotime, China) according to the manufacturer’s protocol.
Tumour growth in severe combined immunodeficient mice
BALB/c-nu nude mice were obtained from the Institute of Laboratory Animal Sciences, the Chinese Academy of Medical Sciences (Beijing, China). All experiments and handling of mice were conducted in accordance with the Animal Management Regulations of the Ministry of Health of China, the Animal Protection and Use Committee of Shihezi University approved the experimental protocol. SKOV3 cells and SKOV3 cells stably expressing low levels of MAP3K3 (3 × 107 cells), A2780 and A2780 cells stably expressing low levels of MAP3K3 (5 × 106 cells), and OV2008 and OV2008 cells stably expressing high levels of MAP3K3 (1 × 107 cells) were implanted subcutaneously into the mice. The mice were euthanised four weeks after injection, and the tumours were excised and weighed, resected, fixed, and embedded in paraffin for histological haematoxylin and eosin staining, immunohistochemistry analysis, and immunoblotting.
Statistical analysis
Statistical analyses were performed using SPSS software (version 13.0; SPSS, Chicago, IL, USA). Pearson χ2 test was used to analyse the associations between the MAP3K3 protein expression levels within the normal fallopian tube and the OC tissues. The Pearson χ2 and Fisher’s exact tests were used to evaluate the significance of the relationship between the MAP3K3 protein expression level and clinicopathological characteristics. The Kaplan-Meier and the log-rank test were used to estimator the differences in overall survival time and disease-free survival time. Univariate and multivariate analyses were performed using the Cox proportional hazards regression method to determine the independent significance of relevant clinical covariates. The other data such as proliferation were evaluated by unpaired Student’s t-tests. A P value < 0.05 was considered statistically significant, *represents P < 0.05, **represents P < 0.01 and ***represents P < 0.001.
Ethics approval and consent to participate
All subjects that contributed tissue specimens for this study provided informed consent, and the study was approved and supervised by the Research Ethics Committee of the First Affiliated Hospital of Shihezi University School of Medicine. All experiments were performed in accordance with the Helsinki Declaration ethical guidelines. All experiments and handling of mice were conducted in accordance the Animal Management Regulations of the Ministry of Health of China, the Animal Protection and Use Committee of Shihezi University approved the experimental protocol. The methods section has included the statement for this effect.
Conclusions
This study established that MAP3K3 overexpression is a prognostic indicator of OC. MAP3K3 appears to regulate the NF-κB signalling pathway, promoting the proliferation, invasion, migration, and chemotherapeutic resistance of OC cells. These results suggest MAP3K3 as a potential candidate target for the development of new therapeutic strategies against OC.
Supplementary information
Acknowledgements
We thank Dr. Gang Chen (Department of Gynecology and Obstetrics, Tongji Hospital of Huazhong University of Science and Technology) for kindly providing cell lines OVCA433 and A2780, Prof. Benjamin K. Tsang (Ottawa Health Research Institute, Ottawa, Canada) for kindly providing cell lines OV2008 and C13*, and Prof. Jianhua Yang (Baylor College of Medicine, TX, Houston, USA) for kindly providing vectors pBabe-MAP3K3-WT-V5-His, p-super-shRNA-MAP3K3-13, p-super-shRNA-MAP3K3-15, and p-super-shRNA-Scramble. This work was funded by the National Natural Science Foundation of China (No. 81660431). No funding or other benefits related to the subject of this article were received from any commercial entity.
Author Contributions
Y.Z. and S.-S.W. performed most of the experimental work; L.T., H.Z. and F.L. obtained H.G.S.O.C. specimens and conducted histological diagnoses; S.-S.W., Z.L. and J.-F.J. helped perform the animal studies; W.-H.L. and S.-L.G. helped with microarray analysis; L.-J.P., W.-J.Z., W.J. and F.L. helped with the design and analysis of the experiments; Y.Z. wrote the manuscript. All authors have read and approved the final manuscript.
Competing Interests
The authors declare no competing interests.
Footnotes
This article has been retracted. Please see the retraction notice for more detail: https://doi.org/10.1038/s41598-025-20904-y
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Change history
9/23/2025
This article has been retracted. Please see the Retraction Notice for more detail: 10.1038/s41598-025-20904-y
Contributor Information
Wei Jia, Email: jiaweipatho@sina.com.
Feng Li, Email: lifeng7855@126.com.
Supplementary information
Supplementary information accompanies this paper at 10.1038/s41598-019-44835-7.
References
- 1.Bray, F. et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin.68, 394–424 (2018). [DOI] [PubMed] [Google Scholar]
- 2.Heintz, A. P. et al. Carcinoma of the ovary. FIGO 26th Annual Report on the Results of Treatment in Gynecological Cancer. International journal of gynaecology and obstetrics: the official organ of the International Federation of Gynaecology and Obstetrics.95(Suppl 1), S161–92 (2006). [DOI] [PubMed] [Google Scholar]
- 3.Bristow, R. E., Tomacruz, R. S., Armstrong, D. K., Trimble, E. L. & Montz, F. J. Survival effect of maximal cytoreductive surgery for advanced ovarian carcinoma during the platinum era: a meta-analysis. J. Clin Oncol.20, 1248–1259 (2002). [DOI] [PubMed] [Google Scholar]
- 4.Fan, Y. et al. Amplification and over-expression of MAP3K3 gene in human breast cancer promotes formation and survival of breast cancer cells. J. Pathol.232, 75–86 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cao, X., Lu, H., Zhang, L., Chen, L. & Gan, M. MEKK3 and survivin expression in cervical cancer: association with clinicopathological factors and prognosis. Asian Pac. J. Cancer Prev.15, 5271–5276 (2014). [DOI] [PubMed] [Google Scholar]
- 6.Hasan, R. et al. Mitogen activated protein kinase kinase kinase 3 (MAP3K3/MEKK3) overexpression is an early event in esophageal tumorigenesis and is a predictor of poor disease prognosis. BMC cancer.14, 2 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.He, Y. et al. MAP3K3 expression in tumor cells and tumor-infiltrating lymphocytes is correlated with favorable patient survival in lung cancer. Sci Rep.5, 11471 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jia, W. et al. MAP3K3 overexpression is associated with poor survival in ovarian carcinoma. Hum. Path.50, 162–169 (2016). [DOI] [PubMed] [Google Scholar]
- 9.Samanta, A., Huang, H., Bast, R. & Liao, W. Overexpression of MEKK3 confers resistance to apoptosis through activation of NFkappaB. J. Biol. Chem.279, 7576–7583 (2004). [DOI] [PubMed] [Google Scholar]
- 10.Samanta, A. et al. MEKK3 expression correlates with nuclear factor kappa B activity and with expression of antiapoptotic genes in serous ovarian carcinoma. Cancer.115, 3897–3908 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhou, Z. et al. The cerebral cavernous malformation pathway controls cardiac development via regulation of endocardial MEKK3 signaling and KLF expression. Dev Cell.32, 168–80 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fisher, O. et al. Structure and vascular function of MEKK3-cerebral cavernous malformations 2 complex. Nat Commun.6, 7937 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kumar, A., Chatopadhyay, T., Raziuddin, M. & Ralhan, R. Discovery of deregulation of zinc homeostasis and its associated genes in esophageal squamous cell carcinoma using cDNA microarray. Int. J. Cancer.120, 230–242 (2007). [DOI] [PubMed] [Google Scholar]
- 14.Zhao, L. et al. MiroRNA-188 Acts as Tumor Suppressor in Non-Small-Cell Lung Cancer by Targeting MAP3K3. Mol. Pharm.15, 1682–1689 (2018). [DOI] [PubMed] [Google Scholar]
- 15.Santoro, R. et al. MEKK3 Sustains EMT and Stemness in Pancreatic Cancer by Regulating YAP and TAZ Transcriptional Activity. Anticancer Res.38, 1937–1946 (2018). [DOI] [PubMed] [Google Scholar]
- 16.Chen, Y. et al. Bufalin inhibits migration and invasion in human hepatocellular carcinoma SK-Hep1 cells through the inhibitions of NF-kB and matrix metalloproteinase-2/-9-signaling pathways. Environ Toxicol.30, 74–82 (2015). [DOI] [PubMed] [Google Scholar]
- 17.Chen, Q. et al. Expression and prognostic role of MEKK3 and pERK in patients with renal clear cell carcinoma. Asian Pac. J. Cancer Prev.16, 2495–2499 (2015). [DOI] [PubMed] [Google Scholar]
- 18.Lu, J. et al. MEKK2 and MEKK3 suppress Hedgehog pathway-dependent medulloblastoma by inhibiting GLI1 function. Oncogene. 1 (2018). [DOI] [PMC free article] [PubMed]
- 19.Jia, W. et al. REDD1 and p-AKT over-expression may predict poor prognosis in ovarian cancer. Int. J. Clin. Exp. Pathol.7, 5940–5949 (2014). [PMC free article] [PubMed] [Google Scholar]
- 20.Mattick, J. S. & Makunin, I. V. Non-coding RNA. Human molecular genetics.null, R17–29 (2006). [DOI] [PubMed] [Google Scholar]
- 21.Thomson, D. W. & Dinger, M. E. Endogenous microRNA sponges: evidence and controversy. Nat. Rev. Genet.17, 272–283 (2016). [DOI] [PubMed] [Google Scholar]
- 22.Baud, V. & Karin, M. Is NF-kappaB a good target for cancer therapy? Hopes and pitfalls. Nat. Rev. Drug Discov.8, 33–40 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sasaki, C., Toman, J. & Vageli, D. The In Vitro Effect of Acidic-Pepsin on Nuclear Factor KappaB Activation and Its Related Oncogenic Effect on Normal Human Hypopharyngeal Cells. PLoS ONE.11, e0168269 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yu, L., Li, L., Medeiros, L. & Young, K. NF-κB signaling pathway and its potential as a target for therapy in lymphoid neoplasms. Blood Rev.31, 77–92 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Varfolomeev, E. et al. Cellular inhibitors of apoptosis are global regulators of NF-κB and MAPK activation by members of the TNF family of receptors. Sci. Signal.5, ra22 (2012). [DOI] [PubMed] [Google Scholar]
- 26.DiDonato, J., Hayakawa, M., Rothwarf, D., Zandi, E. & Karin, M. A cytokine-responsive IkappaB kinase that activates the transcription factor NF-kappaB. Nature.388, 548–554 (1997). [DOI] [PubMed] [Google Scholar]
- 27.Yang, J. et al. The essential role of MEKK3 in TNF-induced NF-kappaB activation. Nat. Immunol.2, 620–624 (2001). [DOI] [PubMed] [Google Scholar]
- 28.Huang, Q. et al. Differential regulation of interleukin 1 receptor and Toll-like receptor signaling by MEKK3. Nat. Immunol.5, 98–103 (2004). [DOI] [PubMed] [Google Scholar]
- 29.Abbasi, S., Su, B., Kellems, R., Yang, J. & Xia, Y. The essential role of MEKK3 signaling in angiotensin II-induced calcineurin/nuclear factor of activated T-cells activation. J. Biol. Chem.280, 36737–36746 (2005). [DOI] [PubMed] [Google Scholar]
- 30.Yu, L., Mu, Y., Sa, N., Wang, H. & Xu, W. Tumor necrosis factor α induces epithelial-mesenchymal transition and promotes metastasis via NF-κB signaling pathway-mediated TWIST expression in hypopharyngeal cancer. Oncol Rep.31, 321–327 (2014). [DOI] [PubMed] [Google Scholar]
- 31.Li, C. et al. Epithelial-mesenchymal transition induced by TNF-α requires NF-κB-mediated transcriptional upregulation of Twist1. Cancer Res.72, 1290–1300 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hsia, C., Cheng, S., Owyang, A., Dowdy, S. & Liou, H. c-Rel regulation of the cell cycle in primary mouse B lymphocytes. Int. Immunol.14, 905–916 (2002). [DOI] [PubMed] [Google Scholar]
- 33.Hinz, M. et al. Constitutive NF-kappaB maintains high expression of a characteristic gene network, including CD40, CD86, and a set of antiapoptotic genes in Hodgkin/Reed-Sternberg cells. Blood.97, 2798–2807 (2001). [DOI] [PubMed] [Google Scholar]
- 34.Boise, L. et al. bcl-x, a bcl-2-related gene that functions as a dominant regulator of apoptotic cell death. Cell.74, 597–608 (1993). [DOI] [PubMed] [Google Scholar]
- 35.Karin, M. Nuclear factor-kappaB in cancer development and progression. Nature.441, 431–436 (2006). [DOI] [PubMed] [Google Scholar]
- 36.Tang, G. et al. Inhibition of JNK activation through NF-kappaB target genes. Nature.414, 313–317 (2001). [DOI] [PubMed] [Google Scholar]
- 37.Yin, H. et al. Adenovirus-mediated TIPE2 overexpression inhibits gastric cancer metastasis via reversal of epithelial-mesenchymal transition. Cancer Gene Ther.24, 180–188 (2017). [DOI] [PubMed] [Google Scholar]
- 38.Moscat, J. & Diaz-Meco, M. The atypical protein kinase Cs. Functional specificity mediated by specific protein adapters. EMBO Rep.1, 399–403 (2000). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rimm, D. L. et al. Tissue microarray: a new technology for amplification of tissue resources. Cancer J.7, 24–31 (2001). [PubMed] [Google Scholar]
- 40.Carvalho, S., Milanezi, F., Costa, J. L., Amendoeira, I. & Schmitt, F. PIKing the right isoform: the emergent role of the p110 beta subunit in breast cancer. Virchows Arch.456, 235–243 (2010). [DOI] [PubMed] [Google Scholar]
- 41.Asselin, E., Mills, G. B. & Tsang, B. K. XIAP regulates Akt activity and caspase-3-dependent cleavage during cisplatin-induced apoptosis in human ovarian epithelial cancer cells. Cancer Res.61, 1862–1868 (2001). [PubMed] [Google Scholar]
- 42.Fong, B., Watson, P. H. & Watson, A. J. Mouse preimplantation embryo responses to culture medium osmolarity include increased expression of CCM2 and p38 MAPK activation. BMC Dev. Biol.7, 2 (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kuo, C. L. et al. Gallic acid inhibits migration and invasion of SCC-4 human oral cancer cells through actions of NF-kappaB, Ras and matrix metalloproteinase-2 and -9. Oncol Rep.32, 355–361 (2014). [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.