Highlights
-
•
Acute aortic abdominal dissection is a rare complication of retroperitoneal laparoscopic paraaortic lymph node dissection.
-
•
Aortic dissection may be part of differential diagnoses in patients with groin and abdominal pain after paraaortic staging.
-
•
Uncomplicated type B aortic abdominal dissection should be managed during the subacute phase.
-
•
Early contrast-enhanced computed tomography should be performed in case of abdominal pain after paraaortic lymphadenectomy.
-
•
Retroperitoneal laparoscopic paraaortic lymph node dissection should be performed at referral cancer centers.
Keywords: Acute aortic dissection, Paraaortic surgical staging, Gynecologic malignancies, Minimally invasive surgery, Surgical complications, Vascular injury
1. Introduction
Paraaortic lymphadenectomy is a surgical procedure commonly used in gynecologic oncology to assess paraaortic lymphatic involvement. Minimally invasive surgery is the preferred approach to perform this surgical staging (Cibula et al., 2018; Uccella et al., 2016; Lu et al., 2016).
Nevertheless, intraoperative and postoperative morbidity has been described in around 8% of these procedures (Leblanc et al., 2016). The most frequent intraoperative complications are vascular injuries, occurring up to 5% of cases. Vascular injuries can be severe complications which can even require conversion to laparotomy when major vessels are involved (Leblanc et al., 2016; Petitnicolas et al., 2017). Ureteral injuries and bowel obstruction are infrequent complications that have also been reported in paraaortic lymphadenectomy (Leblanc et al., 2016). Median and long-term complications associated to aortic staging are mainly lymphocele and lower limb lymphedema, which can occur in approximately 20% and 5% of patients, respectively (Petitnicolas et al., 2017; Frost et al., 2017).
Up to our knowledge there are no cases of acute aortic dissection after laparoscopic paraaortic lymphadenectomy described in the literature. We report the first case of acute aortic abdominal dissection, as a rare complication after retroperitoneal laparoscopic paraaortic lymphadenectomy.
2. Case report
We present the case of a 65-year-old woman with a body mass index of 18.1 kg/m2, and previous history of hyperlipidemia and hypertension treated with Spironolactone and Altizide (25 mg/15 mg per day). She underwent a bilateral adnexectomy and hysterectomy by a median infraumbilical laparotomy outside our hospital for suspicion of uterine sarcoma in preoperative magnetic resonance imaging (Fig. 1). She was referred to our comprehensive cancer center after diagnosis of endometrial carcinosarcoma with a myometrial invasion over 50% in the surgical specimen. After discussion at the tumor board, a laparoscopic surgical staging was recommended.
Fig. 1.
Initial magnetic resonance imaging findings.
Retroperitoneal laparoscopic pelvic and paraaortic lymphadenectomies were performed. The operative time was 160 min and the blood loss was 20 ml. There were no complications during the surgical procedure. At the end of the surgery, we noted a slightly blue coloration of the aorta that was interpreted as an hematoma of the adventitia (Fig. 2). In the recovery room, the patient presented a compromise of dorsiflexion of the right foot as well as a sensory loss of the dorsal surface of the foot. Our first diagnosis was an intraoperative compression of the right external popliteal nerve due to a malposition during surgery. A few hours after the surgery, these symptoms disappeared, and the patient was discharged from hospital at day 1 after surgery. Seven days later, the patient went to the emergency department for stabbing abdominal and bilateral groin pain.
Fig. 2.
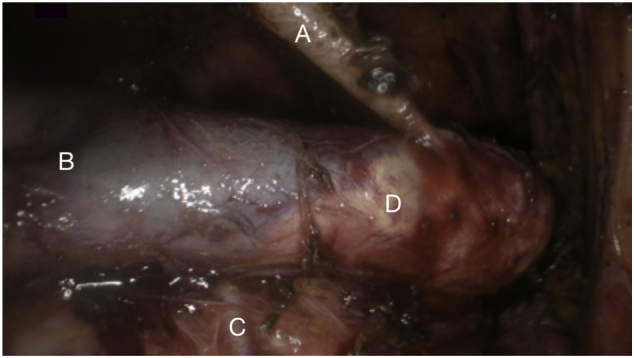
Image after paraaortic lymphadenectomy.
At her admission, blood pressure was 133/80 mmHg, body temperature was 36.7 °C, heart rate was 106 beats/min, respiratory rate was 22 breaths/min, and oxygen saturation was 98% on room air. At clinical examination, she was alert and oriented, without acute distress. Neurologic examination was normal. Bilateral femoral, popliteal, posterior tibial and dorsalis pedis pulses were preserved. There were no abnormalities in electrocardiogram. Laboratory results were unremarkable unless for an increased C-reactive protein of 128.7 mg/l, a decreased hemoglobin of 8.7 g/dl and alteration on hepatic function (gamma-glutamyl transferase 529 UI/l, lactate dehydrogenase 400 UI/l, aspartate aminotransferase 79 UI/l and alanine aminotransferase 113 UI/l).
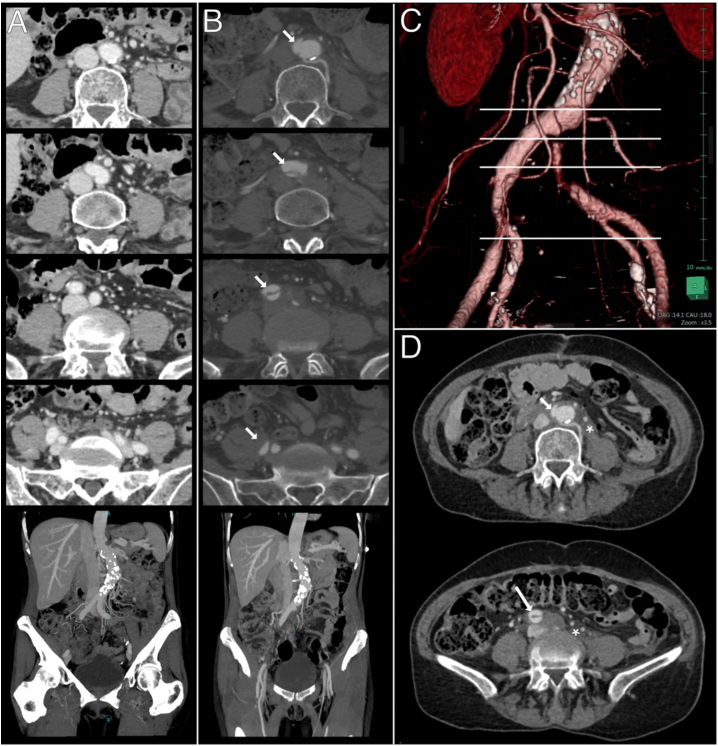
A contrast-enhanced thoraco-abdomino-pelvic computed tomography was performed, revealing an aortic dissection of the infrarenal abdominal aorta (Stanford type B). The entry tear was located 2 cm above the iliac bifurcation, and the dissection reached the initial portion of the right external iliac artery. It was associated with a dynamic obstruction of the left primitive iliac artery with a subsequent thrombosis. Thrombosis of the distal portion of the false lumen was responsible for 50% stenosis of the ostium of the right external iliac artery. Total distal reperfusion was present, for both sides (Fig. 3).
Fig. 3.
Pre and post-operative CT findings.
Antihypertensive treatment was optimized in order to control blood pressure, and anticoagulant therapy was established to treat the thrombosis. One week after the diagnosis, endovascular graft exclusion (EVGE) surgery of bilateral primitive and right external iliac arteries was performed under general anesthesia to cover the primary entry tear and re-expand true lumen of the arteries with guidance by digital subtraction angiography. Two self-expandable covered stents were deployed using the kissing stent technique.
Her pain symptoms improved progressively, and her hepatic function was normalized. We did not find any suitable explanation for the elevation of the hepatic enzymes. She was discharged from hospital six days after EVGE. She was followed in the outpatient clinic of the cardiovascular department six weeks after the EVGE. She was doing well physically and did not present any complaint of abdominal or groin pain. Final histopathology showed paraaortic supramesenteric lymph node involvement (two metastatic lymph nodes) while pelvic lymph nodes were negative, corresponding to IIIC2 International Federation of Gynecology and Obstetrics stage. She received adjuvant concomitant chemoradiotherapy extended to paraaortic field plus adjuvant chemotherapy following PORTEC 3 study protocol (De Boer et al., 2016). In the 6-month follow-up, she was free from her endometrial disease and completely asymptomatic regarding the vascular complication.
3. Discussion
Retroperitoneal approach to perform paraaortic lymph node dissection was firstly described for surgical staging of advanced cervical cancer (Vasilev, 1995; Dargent et al., 2000). Even if some complications such as massive bleeding and conversion to laparotomy due to vascular injury, bowel obstruction, ureteral injury, lymphocele and lymphedema have been described; multiple studies have stated that it has an acceptable morbidity and it currently remains a standard of care for aortic lymphatic assessment (Köhler et al., 2015; Leblanc et al., 2007; Leblanc et al., 2016; Gouy et al., 2013).
Aortic dissection is a life-threatening condition with a high mortality rate. It arises from a tear in the aortic intima and exposes medial layer to pulsatile blood flow, which progressively separate the aortic wall layers creating a false lumen (Gawinecka et al., 2017). Long-term hypertension, old age, arteriosclerosis, dyslipidemia, and potential iatrogenic procedures such as cardiac catheterization or aortic cross-clamping during aortic surgery, have been identified as risk factors for aortic dissection (Elsayed et al., 2017). Our patient had a long-term hypertension treated with dual antihypertensive therapy. Hypertension is the most important risk factor for aortic dissection, present in about 80% of the patients presenting this condition (Gawinecka et al., 2017). Moreover, as noted in Fig. 2, the patient had atheromatous aortic plaques. Arteriosclerosis is known to be more common in patients with type B dissection, which was the case of our patient (Gawinecka et al., 2017). We hypothesize that the presence of multiple risk factors in our patient -age, hypertension and arteriosclerosis- added to a direct insult to the aorta such as paraaortic lymphadenectomy could have led to traumatize aortic intima and cause an aortic dissection.
Retrospective evaluation of this case suggests that the aortic dissection probably occurred during the surgery, which could explain the slightly blue coloration of the aorta at the end of the surgery. The immediate postoperative symptoms of the right foot could probably be explained by a transient ischemia. An immediate postoperative contrast-enhanced computed tomography could have permitted an earlier diagnosis. Fortunately, our patient presented an uncomplicated type B aortic dissection, which could be managed with elective surgery. In uncomplicated aortic dissections, it is recommended to perform the surgical repair during the subacute phase, as it has been demonstrated that those performed in the acute phase have a higher complication rate. Furthermore, aortic plasticity, or capacity of favorable remodeling, seems to be preserved through subacute phase (Alfson and Ham, 2017).
In conclusion, even if severe complications of paraaortic laparoscopic staging are rare, they can be life-threatening for the patients. Aortic dissection has to be considered as a potential complication after paraaortic lymphadenectomy. It should be part of the differential diagnoses in patients with high-risk factors presenting intense abdominal and groin pain after retroperitoneal laparoscopic paraaortic lymphadenectomy, and a contrast-enhanced computed tomography with an arterial acquisition has to be performed in case of suspicion. Failure to diagnose an acute dissection and delay of specific treatment could lead to a fatal patient outcome. Consequently, this kind of procedures should be performed at referral centers.
Patient consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Disclosure
The authors have no financial disclosures.
Contribution
Martina Aida Angeles: Conceptualization, data curation, methodology, writing-original draft.
Olivier Meyrignac: Conceptualization, data curation, methodology, imaging processing, writing-original draft.
Carlos Martínez-Gómez: Conceptualization, data curation, methodology, writing-original draft.
Amel Daboussi: Conceptualization, project administration, methodology writing - review.
Jean Segal: Conceptualization, data curation, methodology, writing-original draft.
Mathilde Del: Conceptualization, data curation, methodology, writing-original draft.
Gwénaël Ferron: Conceptualization, project administration, methodology writing - review.
Alejandra Martinez: Conceptualization, project administration, methodology writing - review.
Acknowledgements
Martina Aida Angeles acknowledges the grant support from ”la Caixa” Foundation, Barcelona (Spain).
References
- Alfson D.B., Ham S.W. Type B aortic dissections current guidelines for treatment. Cardiol. Clin. 2017;35:387–410. doi: 10.1016/j.ccl.2017.03.007. [DOI] [PubMed] [Google Scholar]
- Cibula D., Pötter R., Planchamp F., Avall-Lundqvist E., Fischerova D., Haie Meder C., Köhler C., Landoni F., Lax S., Lindegaard J.C., Mahantshetty U., Mathevet P., McCluggage W.G., McCormack M., Naik R., Nout R., Pignata S., Ponce J., Querleu D., Raspagliesi F., Rodolakis A., Tamussino K., Wimberger P., Raspollini M.R. The European Society of Gynaecological Oncology/European Society for Radiotherapy and Oncology/European Society of Pathology guidelines for the management of patients with cervical cancer. Int. J. Gynecol. Cancer. 2018;28:641–655. doi: 10.1097/IGC.0000000000001216. [DOI] [PubMed] [Google Scholar]
- Dargent D., Ansquer Y., Mathevet P. Technical development and results of left extraperitoneal laparoscopic paraaortic lymphadenectomy for cervical cancer. Gynecol. Oncol. 2000;77:87–92. doi: 10.1006/gyno.1999.5585. [DOI] [PubMed] [Google Scholar]
- De Boer S.M., Powell M.E., Mileshkin L., Katsaros D., Bessette P., Haie-meder C., Ottevanger P.B., Ledermann J.A., Khaw P., Colombo A., Fyles A., Baron M., Kitchener H.C., Nijman H.W., Roussy I.G. Toxicity and quality of life after adjuvant chemoradiotherapy versus radiotherapy alone for women with high-risk endometrial cancer (PORTEC-3): an open-label, multicentre, randomised, phase 3 trial. Lancet Oncol. 2016;17:1114–1126. doi: 10.1016/S1470-2045(16)30120-6. [DOI] [PubMed] [Google Scholar]
- Elsayed R.S., Cohen R.G., Fleischman F., Bowdish M.E. Acute Type A aortic dissection cardiac surgery aortic dissection diagnosis management outcomes. Cardiol. Clin. 2017 doi: 10.1016/j.ccl.2017.03.004. [DOI] [PubMed] [Google Scholar]
- Frost J.A., Webster K.E., Bryant A., Morrison J. Lymphadenectomy for the management of endometrial cancer (review) Cochrane Database Syst. Rev. 2017 doi: 10.1002/14651858.CD007585.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gawinecka J., Schönrath F., Von Eckardstein A. Acute aortic dissection: pathogenesis, risk factors and diagnosis. Swiss Med. Wkly. 2017:1–7. doi: 10.4414/smw.2017.14489. [DOI] [PubMed] [Google Scholar]
- Gouy S., Morice P., Narducci F., Uzan C., Martinez A., Rey A., Bentivegna E., Pautier P., Deandreis D., Querleu D., Haie-Meder C., Leblanc E. Prospective multicenter study evaluating the survival of patients with locally advanced cervical cancer undergoing laparoscopic Para-aortic lymphadenectomy before chemoradiotherapy in the era of positron emission tomography imaging. J. Clin. Oncol. 2013;31:3026–3033. doi: 10.1200/JCO.2012.47.3520. [DOI] [PubMed] [Google Scholar]
- Köhler C., Mustea A., Marnitz S., Schneider A., Chiantera V., Ulrich U., Scharf J., Martus P., Andrade Vieira M., Tsunoda A. Perioperative morbidity and rate of upstaging after laparoscopic staging for patients with locally advanced cervical cancer: results of a prospective randomized trial. Am. J. Obstet. Gynecol. 2015:1–7. doi: 10.1016/j.ajog.2015.05.026. [DOI] [PubMed] [Google Scholar]
- Leblanc E., Narducci F., Frumovitz M., Lesoin A., Castelain B., Baranzelli M.C., Taieb S., Fournier C., Querleu D. Therapeutic value of pretherapeutic extraperitoneal laparoscopic staging of locally advanced cervical carcinoma. Gynecol. Oncol. 2007;105:304–311. doi: 10.1016/j.ygyno.2006.12.012. [DOI] [PubMed] [Google Scholar]
- Leblanc E., Katdare N., Narducci F., Bresson L., Gouy S., Morice Þ.P., Ferron Þ.G., Querleu D., Martinez A. vol. 26. 2016. Should Systematic Infrarenal Para-Aortic Dissection be the Rule in the Pretherapeutic Staging of Primary or Recurrent Locally Advanced Cervix Cancer Patients with a Negative; pp. 169–175. [DOI] [PubMed] [Google Scholar]
- Lu Q., Qu H., Liu C., Wang S., Zhang Z., Zhang Z. Vol. 95. 2016. Comparison of Laparoscopy and Laparotomy in Surgical Staging of Apparent Early Ovarian Cancer; pp. 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petitnicolas C., B H.A., Ghesquie Þ.L., Tresch-bruneel E., Cordoba A., Narducci F., Bresson L. Vol. 27. 2017. Morbidity of Staging Inframesenteric Paraaortic Lymphadenectomy in Locally Advanced Cervical Cancer Compared With Infrarenal Lymphadenectomy; pp. 575–580. [DOI] [PubMed] [Google Scholar]
- Uccella S., Bonzini M., Palomba S., Fanfani F., Malzoni M., Ceccaroni M., Seracchioli R., Ferrero A., Berretta R., Vizza E., Sturla D., Roviglione G., Monterossi G., Casadio P., Volpi E., Mautone D., Corrado G., Bruni F., Scambia G., Ghezzi F. Laparoscopic vs. open treatment of endometrial cancer in the elderly and very elderly: an age-stratified multicenter study on 1606 women. Gynecol. Oncol. 2016;141:211–217. doi: 10.1016/j.ygyno.2016.02.029. [DOI] [PubMed] [Google Scholar]
- Vasilev S.A. A modified incision and technique for total retroperitoneal access and lymph node dissection. Gynecol. Oncol. 1995;56:226–230. doi: 10.1006/gyno.1995.1036. [DOI] [PubMed] [Google Scholar]