Abstract
Caesarean sections (CS) is the most common lifesaving surgeries for obstructed labour and other emergency obstetrical conditions. The WHO had recommended ideal rate for CS to be between 5% and 15%. The rate higher than 15% indicates overused other than lifesaving. Bangladesh has experienced a dramatic increase in CS delivery from 4% in 2004 to 23% in 2014. This increase is elevated by the several factors including maternal education, maternal request or elective CS, and by the urban richest population. However, little is known about the use CS by the urban poorest population. Therefore, the study aimed to examine and identify the factors associated with CS among the urban disadvantaged section of the population.
A total of 1063 randomly chosen women aged 15–49 years from the population of 121,912 residing five-different slums were interviewed during November–December 2016. CS delivery was considered as outcome variable. Both bivariate and multivariable statistical analyses were carried-out. We performed logistic regression analyses to examine the net-effect of independent variables on outcome variable. Over 25% of total deliveries and 50% of facility-based deliveries were CS. The odds of CS delivery was 3.4-fold greater among better-off women than poorest. Women who had 4 + ANC checks-up during pregnancy had a 2-fold higher odds of CS delivery than women of ANC check-up. In private facilities, 76% of births were delivered as CS, followed by 51% in public facilities and 24% in NGO facilities. The likelihood of CS delivery in private facilities was 9.2-fold greater than NGO facilities after controlling for women socio-demographic, pregnancy and delivery characteristics. Thus, the high use of CS is largely associated with private facility, ANC visits and household wealth. Therefore, the Government of Bangladesh should take immediate actions by designing new policies and regulations to ensure CS for the lifesaving condition, not for financial gain.
Keywords: Caesarean section, Urban slums, Demographic surveillance systems, Maternal pregnancy, Delivery and institutional characteristics, Bangladesh
Highlights
-
•
Half of the facility-based deliveries were delivered as caesarean section (CS).
-
•
Three-fourths of deliveries in private facilities was delivered by CS.
-
•
CS deliveries in private facilities were 9.2-fold greater than CS deliveries in NGO facilities.
-
•
The interaction between wealth and facility type on CS found highly significant.
1. Introduction
Caesarean sections (CS) is lifesaving when vaginal delivery poses a risk to the mother or baby due to obstructed labour, foetal distress or an abnormal position of the baby. According to the recommendation by the World Health Organization (WHO), the acceptable CS rates are 5–15%, and rates outside this range are considered as medically unjustified or unnecessary (Moore, 1985). Though the validity of this threshold has since been questioned, however, a rate below 5% indicates a substantial proportion of women have limited access to surgical obstetric care, and a rate higher than 15% indicates overuse of the procedure other than life-saving reasons (Betrán et al., 2007; Gibbons et al., 2010). Research conducted in many countries found that the high use of CS does not contribute to improved maternal health and pregnancy outcomes (Hannah et al., 2000; Villar et al., 2006). Compare to vaginal delivery, CS delivery is associated with the increased risk of maternal and neonatal mortality and morbidity (Barros et al., 2005; Murphy, Liebling, Verity, Swingler, & Patel, 2001; Villar et al., 2006), the occurrence of preterm birth (Barros et al., 2005; Villar et al., 2006), childhood obesity (Poobalan, Aucott, Gurung, Smith, & Bhattacharya, 2009). However, CS delivery has increased dramatically worldwide during the past two decades, particularly in developing countries like Bangladesh, and has become a major concern for health systems in many countries (Lumbiganon et al., 2010; Souza et al., 2010).
CS delivery in Bangladesh has increased from 4% in 2004 to 23% in 2014. The rate of CS delivery in Bangladesh is much higher compared to neighbouring countries such as India (14%), Pakistan (14%) and Nepal (4%), and developed countries including England (9%), Sweden (8.6%) and Norway (17.1%). The high use of CS and its dramatic increase in the country are considered as a combined effect of several social and institutional factors. Changes in maternal socio-demographic characteristics and institutional professionalism increasing malpractice pressure, and economic growth have led to its increase in the last decade. Studies conducted in South Asian countries, including Bangladesh, have raised concern about the high use of CS, and speculated that the national increase in CS rate could be driven in part by higher CS rates in private facilities whose ultimate goal is to maximize profit (Ajeet & Nandkishore, 2013; Cavallaro et al., 2013; Hoxha et al., 2017). The profit maximizing institutional set-up habitually increases the out-of-pocket (OOP) expenses. It is estimated that 67% of total health expenditure in Bangladesh, is met by household OOP, which is the highest in this region (Bangladesh National Health Accounts., 2015). In 2016, total OOP expenses for CS delivery was USD 453 million averaging USD 552 per case including wage loss where USD 315 million OOP expenses were medically unnecessary or unjustified (Save the Children, 2016). The per capita cost of CS delivery and unnecessary CS delivery are USD 2.83 and USD 1.97 respectively (Save the Children, 2016).
Several studies conducted in South Asia and other low-middle-income countries reported that the high prevalence of national CS is mainly due to the high use of CS by the urban richest population (Betrán et al., 2007; Cavallaro et al., 2013). These findings are also supported by a recent analysis of 26 South Asian and sub-Saharan African countries, which found that the use of CS was highest among ‘urban rich’ and lowest among the ‘rural poor’ (Betrán et al., 2007). Furthermore, a multi-country study found that the CS rate was substantially higher among the ‘urban richer’ than ‘urban poorer’, and the rate was found to be more than 15% among the richest quintile and fewer than five percent among the poorest quintile (Cavallaro et al., 2013). The trend is not unlikely in Bangladesh.
Several studies have been conducted to identify the knowledge, attitude, prevalence, socio-demographic predictors and determinants of CS delivery in Bangladesh. The finding from these studies showed that the social and community factors, adolescent and late pregnancy, and maternal education and socioeconomic factors have higher influences on CS delivery (Begum et al., 2018; Leone, Padmadas, & Matthews, 2008; Shahabuddin, Delvaux, Utz, Bardají, & De Brouwere, 2016). However, very limited study conducted to assess the socio-demographic and institutional determinants of CS among the urban poorest section of the Bangladeshi population, especially those who are living in slum settlements. Therefore, the objective of this study is the two-fold—first, to examine and identify the factors associated with CS delivery among the socioeconomically disadvantaged section of the urban population using data from a recent survey; and second, to highlight the socio-demographic, institutional and health determinants of CS delivery in urban slums. Findings of the study will help the Government, policymakers and stakeholders for designing evidence-based policies to prevent unnecessary and inappropriate CS deliveries and reduces its consequences on both mother and newborn.
2. Materials and methods
2.1. Study area
The study was conducted in five-different slums of Dhaka (North and South) and Gazipur City Corporation where International Centre for Diarrhoeal Disease Research, Bangladesh (icddr,b) operates a Health and Demographic Surveillance Systems (HDSS) since 2015.1 In the HDSS area, 121,912 people were living in 31,577 slum-households comprising of 10,297 households from the Korail slum, followed by 6,278 households from the Mirpur slum, 2,082 households from the Dhalpur slum, 2,398 households from the Shayampur slum and 10,522 households from the Tongi slum. Several intervention health programmes have been implementing by both the government and non-governmental organizations (NGOs) over the past few decades. For instance, Bangladesh Rural Advanced Committee (BRAC) is providing maternity care to the pregnant and lactating women through the ‘MANOSHI’ programme to ensure better reproductive health outcome (Ahmed et al., 2010). Besides, the general maternal and child healthcare services in these areas have been managed by the Urban Primary Health Care Services Delivery Project (UPHCSDP) since 1998 (Ahmed, Alam, & Iqbal, 2015), an initiative of a public-private partnership with NGOs. And the services have been provided through Comprehensive Reproductive Health Care Centres, Primary Health Care Centres, and Outreach Centres (satellite clinics).
2.3. Study design and data collection
Data for this study were extracted from a cross-sectional survey conducted during November–December 2016 by the icddr,b. To ensure statistical reliable estimates for most of the indicators with 95% confidence interval for women of the two age groups (e.g. 15–24 and 25–49) separately, approximately 1200 women (600 + 600) were required considering 15% of non-response rate. Therefore, a total of 1,200 women of aged 15–49 years and having a child younger than two years were randomly chosen from the HDSS database. Then total sample was distributed to each slum according to their size (i.e., using ‘probability proportional to size’ technique) for taking interview using a structured questionnaire. Data were collected by Computer Assisted Personal Interview (CAPI) using Tablet phone. To ensure the quality of data, a supervisor revisited 5% of the respondents chosen randomly, within two days of data collection by the field worker. Later, the data collector and supervisor together sorted out if there is any inconsistency found in the collected data. However, very few inconsistency (less than 1%) related to typo were reported and solved.
2.4. Measurement of the variables
2.4.1. Dependent variable
The primary outcome in the analysis of this paper was the mode of delivery for the last birth within two years before the survey, self-reported by the mother. The response was categorised as “no” if vaginal delivery regardless of whether instruments were used or not, and “yes” for CS delivery.
2.4.2. Independent variable
Socio-demographic information of women and the characteristics of the facility where birth delivered were considered as independent variables. The variables were chosen based on previous research demonstrating the importance of these factors (Fabri & Murta, 2002; World Health Organization, 2015; Rahman, Shariff, Shafie, Saaid, & Tahir, 2014). These includes type of facility (public, private and non-governmental organization - NGO),2 age at delivery (<24, 24–34 and ≥ 35 years), sex of the child (boy and girl), education (year of schooling: none, 1–5 years, ≥6 years), gestational age (<37 weeks and ≥37 weeks), livebirth order (1, 2–3 and ≥4), antenatal care visit (no visit, 1–3 visits, ≥4 visits), the household's membership with a NGO3 (yes, no), living slum (Shaympur, Korail, Dhalpur, Mirpur and Tongi) and wealth index (poorest, poor and better-off). The wealth index was computed from ownership of a standard set of household items observed by the interviewers using principal components analysis (PCA), with approximately one-third of the households in each category (Filmer & Pritchett, 2001; Howe, Hargreaves, & Huttly, 2008).
2.5. Statistical analysis
Both bivariate and multivariable statistical analyses were performed to analyse the data. In bivariate techniques, the chi-square test was performed to examine the association between the outcome variable and socio-demographic characteristics of the women. In multivariable analysis, logistic regression analysis was performed to examine net-effect of the independent variables on the outcome variables. We identified maternal education, pregnancy and delivery characteristics potentially associated with CS delivery based on existing literature, especially the WHO multi-country study where they explore these individual association with CS delivery; and how they modified the association between CS delivery and type of delivery facility using adjusted models. In addition to this, few South Asian and Latin American studies have identified a strong association between women's socioeconomic status and CS delivery. Therefore, the interaction effect of births delivered at facilities and women's socioeconomic position was further assessed fitting a logistic regression model with an interaction term to explore if the combined effect of both factors modifies the association with the outcome variables. All analyses were undertaken in STATA software for Windows (STATA/SE version 15.2; StataCorp, 4905 Lakeway Drive, College Station, Texas 77845 USA).
3. Results
3.1. Sample coverage
Of the 1,200 women of childbearing age who gave birth in the preceding two years of the survey selected for the sample, 1,063 were found to be successfully interviewed with a response rate of 88.6%. Rest of the 137 (11.4%) women were unable to interview due to distinct reasons mostly migrated-out from the study areas at the time of interview.
3.2. Socio-demographic characteristics and CS delivery of the study participants
Table 1 shows selected socio-demographic characteristics and CS delivery of 1,063 women aged 15–49 years. More than one-third of the women (34.4%) belong to age group 20–24 years, 28.8% were between 25 and 29 years, and 16.8% were below 20 years. About one-fourth of the women (23.8%) were illiterate, less than half (45.2%) had completed primary education and the rest (31.0%) had more than primary education.
Table 1.
CS delivery among the study participants by selected socio-demographic characteristics.
| Characteristics | No. of women (%) | CS delivery (%) | P-value |
|---|---|---|---|
| Sex of the child | <0.05 | ||
| Boy | 554 (52.1) | 28.5 | |
| Girl | 519 (47.9) | 22.5 | |
| Education | <0.001 | ||
| None | 254 (23.8) | 18.1 | |
| 1–5 years of schooling | 480 (45.2) | 23.8 | |
| ≥6 years of schooling | 329 (31.0) | 34.0 | |
| Age at birth (in years) | 0.352 | ||
| 15-24 | 543 (51.1) | 27.4 | |
| 25-34 | 433 (40.7) | 24.0 | |
| 35-49 | 86 (8.1) | 22.1 | |
| Gestational age | <0.01 | ||
| <37 weeks | 172 (16.2) | 47.1 | |
| ≥37 weeks | 891 (83.8) | 21.4 | |
| Livebirth order | <0.001 | ||
| 1 | 454 (42.7) | 30.8 | |
| 2-3 | 505 (47.5) | 23.0 | |
| ≥4 | 104 (9.8) | 15.4 | |
| ANC visit | <0.001 | ||
| None | 156 (14.7) | 16.0 | |
| 1-3 | 405 (38.1) | 15.8 | |
| ≥4 | 502 (47.2) | 36.5 | |
| NGO membership | <0.05 | ||
| Yes | 429 (40.4) | 28.9 | |
| No | 634 (59.6) | 23.3 | |
| Wealth index | <0.001 | ||
| Poorest | 361 (34.0) | 13.6 | |
| Poor | 352 (33.1) | 22.2 | |
| Better-off | 350 (32.9) | 41.4 | |
| Living slum | <0.001 | ||
| Shaympur | 73 (6.9) | 13.7 | |
| Korail | 316 (29.7) | 13.9 | |
| Dhalpur | 89 (8.4) | 21.4 | |
| Mirpur | 210 (19.8) | 26.7 | |
| Tongi | 375 (35.3) | 38.1 | |
| Number of women | 1,063 (100) | 25.6 |
Note: NGO = Non-governmental organization.
About 26% of the total births were delivered as CS. The CS delivery was significantly associated with women's socio-demographic characteristics. The results revealed that CS delivery was higher among the women who delivered a boy child (28.5%), followed by women with higher education (34.0%), lower gestational age (47.1%) and living in households with highest socioeconomic status (41.4%) compared to their counterparts such as who delivered a girl child (22.5%), lower education (18.1%), higher gestational age (21.4%) and living in households with lowest socioeconomic status (13.6%).
3.3. Multivariable analysis
Table 2 presents both unadjusted and adjusted odds ratio suggesting the magnitude of the association between the women's socio-demographic characteristics and CS delivery. The results from the univariate model showed the significant relationship between CS delivery and socio-demographic factors in each of the models. After adjustment, the influence remained the same for all factors except for education and household's NGO membership. Women's socioeconomic status significantly positively associated with CS delivery. The odds of having CS delivery among the women from better-off households were 3.4-fold greater compared to their counter poorest households. Livebirth order is inversely associated with CS delivery while women with firstborn children (AOR 2.4) had greater odds of having CS delivery. Similarly, women who gave preterm delivery (AOR 3.1) and a boy child (AOR 1.5) were more likely to have CS delivery compared to their counterparts. Moreover, women who had four or more antenatal check-ups during pregnancy are found to have significantly higher odds of having CS delivery compared to those with short of ANC visit (AOR 2.0). There was a significant difference in having CS delivery between the slums. Respondents who resided in the Tongi slum had a 2.8-fold higher odds of CS delivery compared to the respondents residing in Shaympur slum.
Table 2.
Unadjusted and adjusted measures of association for CS delivery.
| Characteristics | Crude OR (95% CI) | P-value | Adjusted OR (95% CI) | P-value |
|---|---|---|---|---|
| Sex of child | 0.027 | 0.014 | ||
| Boy | 1 | 1 | ||
| Girl | 1.4 (1.0–1.8) | 1.5 (1.1–2.0) | ||
| Education | <0.001 | 0.984 | ||
| None | 1 | 1 | ||
| 1–5 years of schooling | 1.4 (1.0–2.1) | 1.0 (0.7–1.5) | ||
| ≥6 years of schooling | 2.3 (1.6–3.5) | 1.1 (0.6–1.7) | ||
| Gestational age | 0.005 | <0.001 | ||
| ≥37 weeks | 1 | 1 | ||
| <37 weeks | 3.3 (2.3–4.6) | 3.1 (2.1–4.5) | ||
| Livebirth order | <0.001 | <0.001 | ||
| ≥4 | 1 | 1 | ||
| 2-3 | 1.6 (0.9–2.9) | 1.4 (0.8–2.7) | ||
| 1 | 2.5 (1.4–4.3) | 2.4 (1.3–4.6) | ||
| ANC visit | <0.001 | <0.001 | ||
| None | 1 | 1 | ||
| 1-3 | 1.0 (0.6–1.6) | 0.9 (0.5–1.6) | ||
| ≥4 | 3.0 (1.9–4.8) | 2.0 (1.2–3.3) | ||
| NGO membership | 0.042 | 0.896 | ||
| No | 1 | 1 | ||
| Yes | 1.3 (1.0–1.8) | 1.0 (0.7–1.4) | ||
| Wealth index | <0.001 | <0.001 | ||
| Poorest | 1 | 1 | ||
| Poor | 1.8 (1.2–2.7) | 1.6 (1.1–2.5) | ||
| Better off | 4.5 (3.1–6.5) | 3.4 (2.2–5.2) | ||
| Living slum | <0.001 | <0.001 | ||
| Shaympur | 1 | 1 | ||
| Korail | 1.0 (0.5–2.1) | 1.3 (0.6–2.8) | ||
| Dhalpur | 1.7 (0.8–3.9) | 1.0 (0.4–2.6) | ||
| Mirpur | 2.3 (1.1–4.8) | 1.6 (0.7–3.5) | ||
| Tongi | 3.9 (1.9–7.8) | 2.8 (1.3–5.8) |
3.4. Pregnancy delivery by type of facilities
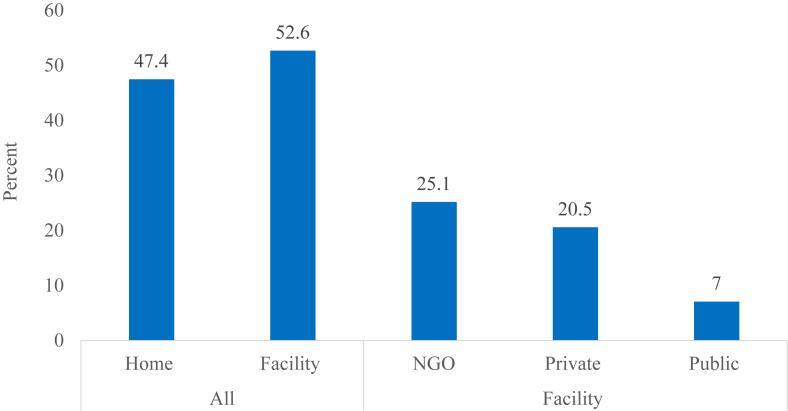
Fig. 1 shows the distribution of pregnancy delivery by the type of facilities. Slightly more than 50% of the births were delivered in health facilities within public (7.0%), private (20.5%) and NGO (25.1%) facilities as compared to home delivery (47.4%).
Fig. 1.
Pregnancy outcome by place of delivery.
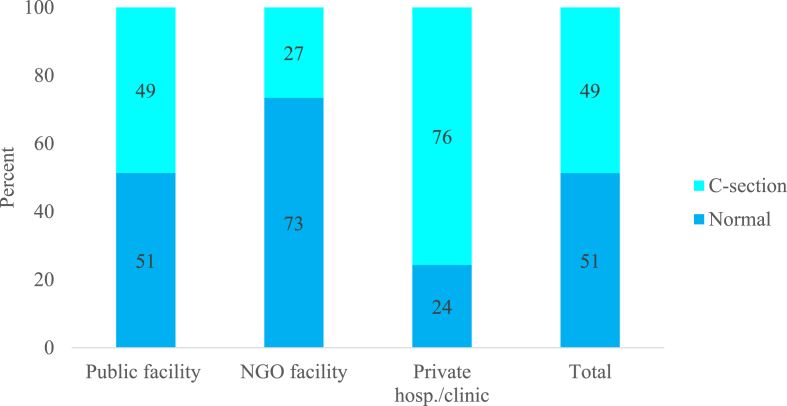
Fig. 2 presents the distribution of CS delivery among the women who gave birth in a facility. Among the total sample (1,063), a total of 559 births were delivered at the facilities. Almost 50% of the facility-based deliveries were delivered as CS delivery. Of the facilities, the private facilities were dominated by producing the highest CS delivery where three in four births were delivered as CS. While the NGO facility produces the lowest CS delivery, where one in four births was delivered as CS. Almost equal proportions of births were delivered as CS in the public health facilities.
Fig. 2.
Percentage of CS delivery by type of facility.
Table 3 presents unadjusted and adjusted measures of association between type of delivery facility and CS delivery. After controlling for maternal socio-demographic characteristics, the odds of CS delivery found to be significantly higher in public (AOR: 3.3) and private (AOR: 9.2) facilities compared CS delivery in NGO facilities.
Table 3.
Unadjusted and adjusted measures of association for type of facility and women's socio-demographic characteristics with CS delivery.
| Crude OR (95% CI) | P-value | Adjusted ORa (95% CI) | P-value | |
|---|---|---|---|---|
| Facility | <0.001 | <0.001 | ||
| NGO | 1 | 1 | ||
| Public | 2.6 (1.5–4.4) | 3.3 (1.8–6.0) | ||
| Private | 8.6 (5.7–12.9) | 9.2 (5.7–14.6) |
All results adjusted for sex of child, mother's education, gestational age, birth order, ANC visits and household NGO membership, living slum and wealth index.
Further, the interaction effect between type of facility and socioeconomic status was assessed controlling for the effects of women's socio-demographic characteristics (Table 4). The results suggest that all higher-level combination of interaction between type of facility and socioeconomic status has significantly higher odds of having CS delivery. More specifically, women with increasing socioeconomic status delivered at public or private facilities are significantly higher chance of having CS delivery compared to their counterpart. For instance, the odds of having CS delivery among the women from better-off households and delivered births in private facilities were 21-fold greater compared to women from poorest households and delivered births in NGO facilities. The influence of private facility for CS delivery was found to be too high. For instance, even for the women from the poorest family who delivered at a private facility, the odds of having CS delivery is 22 times of their counterpart.
Table 4.
Interactionon effect of type of delivery facility and women's socioeconomic status.
| Interactions | n | AOR (95% CI) a | P-valueb |
|---|---|---|---|
| NGO facility * poorest | 77 | 1 | <0.001 |
| NGO facility * poor | 89 | 1.8 (0.7–4.4) | |
| NGO facility * better-off | 101 | 4.0 (1.7–9.9) | |
| Public facility * poorest | 27 | 4.0 (1.3–12.2) | |
| Public facility * poor | 25 | 5.3 (1.6–17.3) | |
| Public facility * better-off | 22 | 16.1 (4.7–55.5) | |
| Private facility * poorest | 40 | 22.2 (7.7–64.1) | |
| Private facility * poor | 67 | 19.8 (7.7–50.6) | |
| Private facility * better-off | 111 | 20.9 (8.5–51.5) |
AOR, Adjusted Odds Ratio.
All results adjusted for sex of child, mother's education, gestational age, birth order, ANC visits and household NGO membership and living slum.
p Value from −2 log-likelihood test comparing nested models with and without interaction terms.
4. Discussion
While the facts and figures on CS delivery among such disadvantaged population are limited, the paper focused on examining the prevalence and factors associated with CS delivery among urban slum population in Bangladesh with an aim to provide some guidelines for policymakers to reduce unnecessary CS delivery. Findings suggest that the rate of caesarean delivery among a socioeconomically disadvantaged section of the urban population is nearly two-fold the WHO's recommended rate of 5–15% and slightly higher than the national rate (23%) reported in 2014 (BDHS, 2016). Moreover, findings of the study revealed that women living in households with higher socioeconomic status, those who took at least four ANC visits during pregnancy, delivered birth at private facilities, delivered birth for the first time and delivered a boy child are more likely to have CS delivery than their corresponding counterparts. In addition to this, CS deliveries were significantly higher among who gave birth at facilities where one in every two births was reported as CS delivery. Of them, private facilities dominated strongly, where 73% of the total deliveries were taken place using CS which is four-fold higher than CS delivery at NGO facilities. This means that CS delivery is markedly high among the urban marginalized population when they visit a facility own by a private entrepreneur may have their tendency of profit maximization.
The result is consistent with many other studies conducted in similar settings (Hopkins, 2000; Neuman et al., 2014; Potter et al., 2001). Therefore, it is not unlikely that profit-motivated private hospitals/clinics have contributed to the recent high rates of caesarean births in the country. There are several plausible explanations for the high rates in the private facilities: lack of quality control in hospitals, financial incentive and poor ethical standards. The profit-motivated institutional setting has often provided a hidden or overt financial incentive to encourage such intervention (Chatterjee and Laxminarayan, 2013). This is an important issue for health systems of Bangladesh not only because of associated short-and long-term health risks but also health expenditures related to the increasing costs of caesarean births. Furthermore, due to the absence of a strong quality control system, there are the possibilities that hospitals/clinics may look forward to making more profits. On the other hand, in public facilities, almost 50% of the total births were reported to be delivered as CS. The high rates of CS in public facilities are likely to be complicated delivery referrals that could not be managed by the private or NGO facilities and hence referred to the public facilities (Andaleeb, 2000). In general, public facilities are the referral centres in Bangladesh to manage all complicated maternal and neonatal cases (Ahmed et al., 2015; Andaleeb, 2000).
The wealthiest people who have a higher ability to pay for the surgery, which is found to be an important determinant of CS delivery in exiting literature (Neuman et al., 2014). Our findings also support the results of earlier studies conducted in South Asia including Bangladesh and sub-Saharan Africa (Cavallaro et al., 2013; Kamal, Curtis, Hasan, & Jamil, 2016). There are several reasons that could explain why better off are undergoing CS. The first is that people with higher socioeconomic status choose a private hospital because of getting comparatively better care by the highly paid nurses and doctors where the frequency of CS is very much high. Secondly, poorer households cannot afford the surgery and extra costs associated with CS delivery. Additionally, the better-off are more likely to be aware of their existing illness, and this knowledge may prompt them and doctors to consider CS delivery.
A positive association between the use of antenatal care (ANC) services and the CS has substantial public health implication. ANC visits are viewed as an essential measure for a complication-free normal pregnancy. It has been suggested that these visits were used by the healthcare provider to motivate women to undergo a CS. Besides this, in Bangladesh, there is evidence to suggest that women consider an ultrasound to be an integral part of an ANC check-up. At the time of providing ANC, private facilities, in general, are better equipped to provide ultrasound services than public or NGO facilities. Therefore, it is a common practice of Bangladeshi healthcare provider to inform the women whether they are having a boy or girl child (Kamal et al., 2016; National Institute of Population Research and Training (NIPORT)). The technological ability to reveal the sex of the baby might influence the women or their family to invest more or be more cautious about the pregnancy for cultural reasons, which in turn increased their willingness for CS delivery. Our study findings are likewise supported this statement.
Results from this study confirm that the high interaction between women's socioeconomic status and CS delivery in a private facility. Women from the poorest households who gave birth in private facilities had about five-fold higher odds of CS delivery compared to women from better-off households who gave birth at NGO facilities. This indicates, in private facilities, there could have been unnecessary and inappropriate CS delivery practices may be for profit-motivated reasons. Thus, CS is far more than the necessary-level to keep maternal and neonatal mortality rates low. However, there is a slow decrease in the maternal mortality rate (MMR) and neonatal mortality rate (NMR) in the last one-decade despite a very sharp increase in the CS rate. If most of the CS surgeries in Bangladesh were used for emergency cases, the MMR/NMR rate would be decreased very quickly. Unfortunately, many women, who require CS surgeries, do not have access to it. Thus, it is necessary for the government to hold hospitals and clinics accountable for performing CS delivery without sound medical reasons.
The evidence generated from this study also showed that living slum has substantial linkages in relation to the high of CS. Women of Tongi and Mirpur have a much higher likelihood of undergoing a CS delivery. The plausible reasons could be the greater availability of health facilities and healthcare professionals. Many public and private facilities, as well as NGO facilities, are operating health-related activities in these two slums.
To understand circumstances and reasons for the CS, it is crucial to cross-check women's care received with exit interviews, observation of care and feedback from both patients and healthcare professionals. There are, however, few suggestions from the current findings to propose testing both demand and supply side needs to be aimed at enhancing women awareness about the adverse health outcome relating to CS. Alongside health economic analyses to identify optimal use and wastage of resources with the CS delivery, and other potential use of resources for maternity care during and after pregnancy are essential.
The strength of this study is data from a Health and Demographic Surveillance System in the INDEPTH Network which is considered to be the very high quality because of its real-time monitoring. However, there are some limitations of this study. First, we do not have data about maternal complication during pregnancy which could be essential to identify the actual needs of CS. Second, the data are cross-sectional in nature. Therefore, no causal relationship could be identified, and it is not possible to generalise the findings to the country/slum population as a whole. Third, women partners education also has a noteworthy role whether a woman decided to undergo a CS delivery, nevertheless, we don't have the data regarding women spouse education. Considering these limitations, we believed that our study could be a novel way of understanding the reasons why the CS rate in Bangladesh increasing in recent times.
5. Conclusion
Nearly 50 percent of facility-based births were delivered through CS among a socioeconomically disadvantaged section of the urban population. Our results confirmed that the high use of CS among the urban marginalized is mainly associated with births delivered at private facilities; whereas the number of ANC visits, household's socioeconomic position and preterm birth are partially associated with it. Therefore, the high CS delivery rates in Bangladesh might not translate to better birth outcomes. Thus, it is essentials to take immediate action from the Government of Bangladesh by designing new policies and regulations to ensure that CS is only carried out when necessary at a medical standpoint, not for financial gain. Based on the study results, intervention could be designed to reduce CS deliveries by focusing more on the social and institutional factors rather than maternal characteristics.
Acknowledgments
This research protocol was funded by the Government of the People’s Republic of Bangladesh and Embassy of Sweden with the technical support from Asian Development Bank and UNFPA. icddr,b acknowledges with gratitude the commitment of Government of People's Republic of Bangladesh and Embassy of Sweden, technical support from Asian Development Bank and UNFPA to its research effort. We also acknowledge Mokbul Sharif, Shahinur Islam, Nargis Akter for filed implementation and data management.
Footnotes
A slum is a cluster of compact settlements of 5 or more households which generally grow very unsystematically and haphazardly on government and private vacant land, are prone to adverse environmental hazards and exposures (BBS 2015).
The Government or public facility is operated by the state ownership to provide comprehensive health services through Ministry of Health and Family Welfare through district hospitals at district level, Upazila Health Complex at subdistrict level, Union Health and Family Welfare Centre at Union level and Community Clinic at ward level. The private facility consists of the formal sector which provides both western and traditional services through a range of facilities from hospitals to clinics, laboratories and drug stores; and the informal sector. The formal sector is concentrated in urban areas, and the informal sector is the principal provider in rural areas. The NGOs facility is operating by the donor agencies with the partnerships between the Government in the areas of financing, planning, service delivery, capacity building, and monitoring and evaluation (Bangladesh Health Systems Review., 2015).
The household belongs to any activities with any of non-governmental organization, for instance, access to micro-credit or micro-finance, insurance coverage or any social transfer or health services programmes.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ssmph.2019.100415.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Ahmed S.M., Alam B.B., Iqbal A. Bangladesh Health Systems Review. 2015;5(3) 2015. [Google Scholar]
- Ahmed S.M., Hossain A., Khan M.A., Mridha M.K., Alam A., Choudhury N. Using formative research to develop MNCH programme in urban slums in Bangladesh: Experiences from MANOSHI, BRAC. BMC Public Health. 2010;10(1):663. doi: 10.1186/1471-2458-10-663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ajeet S., Nandkishore K. The boom in unnecessary caesarean surgeries is jeopardizing women's health. Health Care for Women International. 2013;34(6):513–521. doi: 10.1080/07399332.2012.721416. [DOI] [PubMed] [Google Scholar]
- Andaleeb S.S. Public and private hospitals in Bangladesh: Service quality and predictors of hospital choice. Health Policy and Planning. 2000;15(1):95–102. doi: 10.1093/heapol/15.1.95. [DOI] [PubMed] [Google Scholar]
- Barros F.C., Victora C.G., Barros A.J., Santos I.S., Albernaz E., Matijasevich A. The challenge of reducing neonatal mortality in middle-income countries: Findings from three Brazilian birth cohorts in 1982, 1993, and 2004. The Lancet. 2005;365(9462):847–854. doi: 10.1016/S0140-6736(05)71042-4. [DOI] [PubMed] [Google Scholar]
- BDHS . National Institute of Population Research and Training (NIPPORT); 2016. Report of the Bangladesh health and demographic survey 2014. Dhaka, Bangladesh Bangladesh. [Google Scholar]
- Begum T., Ellis C., Sarker M., Rostoker J.F., Rahman A., Anwar I. A qualitative study to explore the attitudes of women and obstetricians towards caesarean delivery in rural Bangladesh. BMC Pregnancy and Childbirth. 2018;18(1):368. doi: 10.1186/s12884-018-1993-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Betrán A.P., Merialdi M., Lauer J.A., Bing‐Shun W., Thomas J., Van Look P. Rates of caesarean section: Analysis of global, regional and national estimates. Paediatric & Perinatal Epidemiology. 2007;21(2):98–113. doi: 10.1111/j.1365-3016.2007.00786.x. [DOI] [PubMed] [Google Scholar]
- Cavallaro F.L., Cresswell J.A., França G.V., Victora C.G., Barros A.J., Ronsmans C. Trends in caesarean delivery by country and wealth quintile: Cross-sectional surveys in southern Asia and sub-saharan Africa. Bulletin of the World Health Organization. 2013;91(12):914–922D. doi: 10.2471/BLT.13.117598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chatterjee S., Laxminarayan R. Costs of surgical procedures in Indian hospitals. BMJ Open. 2013;3 doi: 10.1136/bmjopen-2013-002844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fabri R., Murta E. Socioeconomic factors and cesarean section rates. International Journal of Gynecology & Obstetrics. 2002;76(1):87–88. doi: 10.1016/s0020-7292(01)00544-6. [DOI] [PubMed] [Google Scholar]
- Filmer D., Pritchett L.H. Estimating wealth effects without expenditure data—or tears: An application to educational enrollments in states of India. Demography. 2001;38(1):115–132. doi: 10.1353/dem.2001.0003. [DOI] [PubMed] [Google Scholar]
- Gibbons L., Belizán J.M., Lauer J.A., Betrán A.P., Merialdi M., Althabe F. The global numbers and costs of additionally needed and unnecessary caesarean sections performed per year: Overuse as a barrier to universal coverage. World Health Report. 2010;30:1–31. [Google Scholar]
- Hannah M.E., Hannah W.J., Hewson S.A., Hodnett E.D., Saigal S., Willan A.R. Planned caesarean section versus planned vaginal birth for breech presentation at term: A randomised multicentre trial. The Lancet. 2000;356(9239):1375–1383. doi: 10.1016/s0140-6736(00)02840-3. [DOI] [PubMed] [Google Scholar]
- Hopkins K. Are Brazilian women really choosing to deliver by cesarean? Social Science & Medicine. 2000;51(5):725–740. doi: 10.1016/s0277-9536(99)00480-3. [DOI] [PubMed] [Google Scholar]
- Howe L.D., Hargreaves J.R., Huttly S.R. Issues in the construction of wealth indices for the measurement of socio-economic position in low-income countries. Emerging Themes in Epidemiology. 2008;5(1):3. doi: 10.1186/1742-7622-5-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoxha I., Syrogiannouli L., Luta X., Tal K., Goodman D.C., da Costa B.R. Caesarean sections and for-profit status of hospitals: Systematic review and meta-analysis. BMJ open. 2017;7(2) doi: 10.1136/bmjopen-2016-013670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kamal N., Curtis S., Hasan M.S., Jamil K. Trends in equity in use of maternal health services in urban and rural Bangladesh. International Journal for Equity in Health. 2016;15(1):27. doi: 10.1186/s12939-016-0311-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leone T., Padmadas S.S., Matthews Z. Community factors affecting rising caesarean section rates in developing countries: An analysis of six countries. Social Science & Medicine. 2008;67(8):1236–1246. doi: 10.1016/j.socscimed.2008.06.032. [DOI] [PubMed] [Google Scholar]
- Lumbiganon P., Laopaiboon M., Gülmezoglu A.M., Souza J.P., Taneepanichskul S., Ruyan P. Method of delivery and pregnancy outcomes in Asia: The WHO global survey on maternal and perinatal health 2007–08. The Lancet. 2010;375(9713):490–499. doi: 10.1016/S0140-6736(09)61870-5. [DOI] [PubMed] [Google Scholar]
- Moore B. Appropriate technology for birth. The Lancet. 1985;326(8458):787. [Google Scholar]
- Murphy D.J., Liebling R.E., Verity L., Swingler R., Patel R. Early maternal and neonatal morbidity associated with operative delivery in second stage of labour: A cohort study. The Lancet. 2001;358(9289):1203–1207. doi: 10.1016/S0140-6736(01)06341-3. [DOI] [PubMed] [Google Scholar]
- National Institute of Population Research and Training (NIPORT), reportICF international Bangladesh health facility survey 2014 final report Dhaka, Bangladesh Ministry of Health and Family Welfare.
- Neuman M., Alcock G., Azad K., Kuddus A., Osrin D., More N.S. Prevalence and determinants of caesarean section in private and public health facilities in underserved South Asian communities: Cross-sectional analysis of data from Bangladesh, India and Nepal. BMJ Open. 2014;4(12) doi: 10.1136/bmjopen-2014-005982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poobalan A.S., Aucott L.S., Gurung T., Smith W.C.S., Bhattacharya S. Obesity as an independent risk factor for elective and emergency caesarean delivery in nulliparous women–systematic review and meta‐analysis of cohort studies. Obesity Reviews. 2009;10(1):28–35. doi: 10.1111/j.1467-789X.2008.00537.x. [DOI] [PubMed] [Google Scholar]
- Potter J.E., Berquó E., Perpétuo I.H., Leal O.F., Hopkins K., Souza M.R. Unwanted caesarean sections among public and private patients in Brazil: Prospective study. BMJ. 2001;323(7322):1155–1158. doi: 10.1136/bmj.323.7322.1155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahman M., Shariff A.A., Shafie A., Saaid R., Tahir R.M. Determinants of caesarean risk factor in northern region of Bangladesh: A multivariate analysis. Iranian Journal of Public Health. 2014;43(1):16. [PMC free article] [PubMed] [Google Scholar]
- Save the Children . Save the Children; Dhaka, Bangladesh: 2016. Statistical analysis of cesarean sections in Bangladesh in 2016. [Google Scholar]
- Shahabuddin A.S.M., Delvaux T., Utz B., Bardají A., De Brouwere V. Determinants and trends in health facility-based deliveries and caesarean sections among married adolescent girls in Bangladesh. BMJ Open. 2016;6(9) doi: 10.1136/bmjopen-2016-012424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Souza J.P., Gülmezoglu A., Lumbiganon P., Laopaiboon M., Carroli G., Fawole B. Caesarean section without medical indications is associated with an increased risk of adverse short-term maternal outcomes: The 2004-2008 WHO global survey on maternal and perinatal health. BMC Medicine. 2010;8(1):71. doi: 10.1186/1741-7015-8-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Villar J., Valladares E., Wojdyla D., Zavaleta N., Carroli G., Velazco A. Caesarean delivery rates and pregnancy outcomes: The 2005 WHO global survey on maternal and perinatal health in Latin America. The Lancet. 2006;367(9525):1819–1829. doi: 10.1016/S0140-6736(06)68704-7. [DOI] [PubMed] [Google Scholar]
- World Health Organization . 2015. WHO recommendations on interventions to improve preterm birth outcomes. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.