Abstract
Background/Purpose
Obstructive sleep apnea syndrome (OSAS) is a common form of sleep disorder. Lateral cephalograms and cone-beam computed tomography (CBCT) have been used for evaluation. However, it is lack of position comparison for these two assessments. Therefore, this study was aimed to evaluate the difference of upper airway measurements taken from lateral cephalograms in upright position and CBCT in supine position.
Material and methods
This retrospective study enrolled patients with lateral cephalograms and CBCT images due to diagnostic necessity. The anterior-posterior distance of most constricted area in pharynx (PASmin) and the distance from mandibular plane to hyoid bone (MP-H) were identified and measured from 21 normal subjects without obstructive sleep apnea (9 males and 12 females, mean age 21.2 years). A paired data were measured from lateral cephalograms taken in upright position and lateral cephalometric images derived from CBCT taken in supine position. Both images were taken within two months. All data were analyzed statistically.
Results
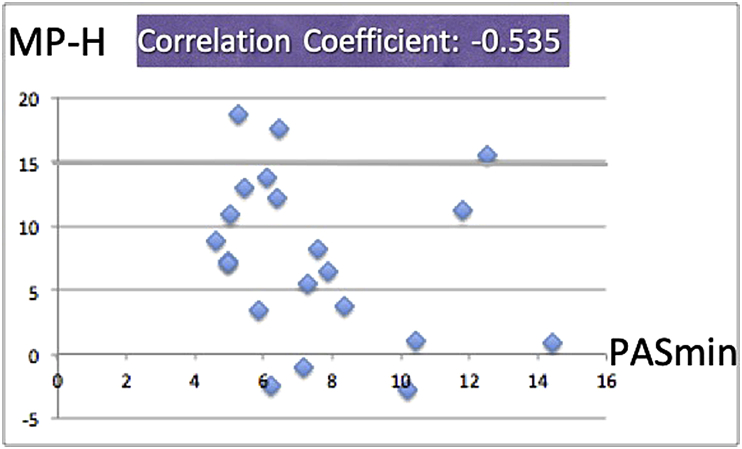
No significant difference was identified in intra-examiner reliability (P > 0.05). PASmin measured from lateral cephalograms in upright position was larger than that taken from CBCT derived cephalometric images, but without statistical significant difference (P = 0.073). Significant difference of MP-H length was identified between two different image taking methods (P = 0.000), and the measurement was significantly larger in cephalograms taken from upright position. No correlations were found among the variables (Body Mass Index (BMI), age, gender) in this study. The only two variables correlated were PASmin and MP-H, and they were negatively correlated (r = −0.535).
Conclusion
The anterior-posterior distance of most constricted area in pharynx (PASmin) and distance of mandibular plane to hyoid bone (MP-H) can be influenced due to change of body position.
Keywords: Upper airway, CBCT, Cephalogram
Introduction
Lateral cephalograms was first proposed for application on patients with obstructive sleep apnea syndrome (OSAS) in 1972 by Cosman et al.,1 lateral cephalograms then became a popular tool for evaluating the site of obstruction and severity in patients with OSAS since Guilleminault et al. published their research.2
Sleep-disordered breathing affects 24% of middle-aged man in Wisconsin,3 14.4% of Chinese men in Hong Kong, and 27% and 16% middle-aged Korean men and women, respectively. OSAS is a common form of sleep-disordered breathing which is characterized by repetitive episodes of partial or complete upper airway obstruction which induces sleep fragmentation and other symptoms.4 It has been postulated that sleep posture influences these events because patients with the syndrome may have increased respiratory difficulty when sleeping in the supine position. OSAS is equally common among middle-aged white and Hong-Kong Chinese populations with a minimum prevalence of 4%. There is also an association between OSAS and heart failure, ischemic heart disease, cardiac arrhythmia, and sudden cardiac death.5 It has been reported that the 5- year survival rate of OSAS patients whose apnea index is more than 20 is about 84%.6 These findings clearly showed that OSAS is a serious condition with major health-related consequences and that early screening on patients with OSAS is important. One overnight polysomnography in a sleep laboratory is accepted as the gold standard for diagnosis of OSAS now.7 Although the diagnostic superiority of polysomnography is without questions, however, it is regarded as both time-consuming and expensive. Thus, this lateral cephalometric method remains a practical preliminary screening tool for OSAS.8 Also, intraoral appliances have been accepted as a noninvasive treatment modalities by many sleep physicians.9 The role of orthodontists to use cephalogram as a preliminary diagnostic tool becomes more important.
In recent years, Cone-beam computed tomography (CBCT) was highly recommended as a better imaging modality in dental and maxillofacial diagnosis, by visualization and image processing on a 1:1 scale and with a considerably degree of lower radiation dose compared to medial computed tomography (medial CT).10,11
Previous studies showed that postural effect should be taken into account when assessing upper airway structure.12 And there were studies proved that there are some noticeable differences in upper airway structure between lateral cephalograms taken under two different positions in terms of upright and supine positions.13 Also, there were studies comparing upright cephalogram and upright CBCT in upper airway evaluation, too.14,15 However, to our knowledge, research comparing lateral cephalogram taken under upright position and CBCT taken under supine position for upper airway evaluation remains lacking. This study was aimed to obtain further information in upper airway anterior-posterior distance evaluation by comparing lateral cephalograms and CBCT under upright and supine postures respectively.
Materials and methods
A sample of 94 Taiwanese adult subjects who had upright lateral cephalograms and supine CBCT images due to orthodontic diagnosis necessities were chosen from the data bank at the department of orthodontics at Veterans General Hospital, Taipei, Taiwan. We obtained these data retrospectively. From this parent sample, 21 subjects (9 males and 12 females, 15–37 year old, mean age 21.2 ± years) who met the following criteria were included in this study:
-
•
Subjects revealed no subjective symptoms suggestive of OSAS.
-
•
Subjects had lateral cephalogram taken in the upright position.
-
•
Subjects had CBCT image taken in the supine position.
-
•
These images were taken within 2 months.
-
•
Subjects who are older than 15 year old.
CBCT were obtained using NewTom 5G (QR s.r.l., Verona, Italy). The scanning parameters were 1–20 mA, 110 kV, 0.3 mm focal spot, field of view 18 cm × 16 cm, and voxel size from 150 to 250 μm according to the manual instruction. All patients bit in centric occlusion, and were instructed not to swallow, and had their heads oriented so that their midsagittal planes were positioned perpendicular, with the Frankfurt plane perpendicular to the floor. The images were imported into Simplant O&O software (for Intel X86, Platform V3.0.0.59) for standardization for the purpose of setting nature head position. Then the reconstructed lateral cephalograms were obtained.
The lateral cephalograms were acquired with Sirona Orthophos XG5 DS CEPH under condition of 60–90 kv, 3–16 mA (Sirona Dental System GmbH, Bensheim, Germany). A Cephalostat ensured natural head positioning, and the central beam was aimed at the left side of the face with a 10 percent standardized magnification. All patients bited in centric occlusion and instructed not to swallow. All cephalograms were processed and imported into PiViewSTAR (INFINITT Co. Ltd., Seoul, Korea) software, and manually adjusted of brightness and contrast.
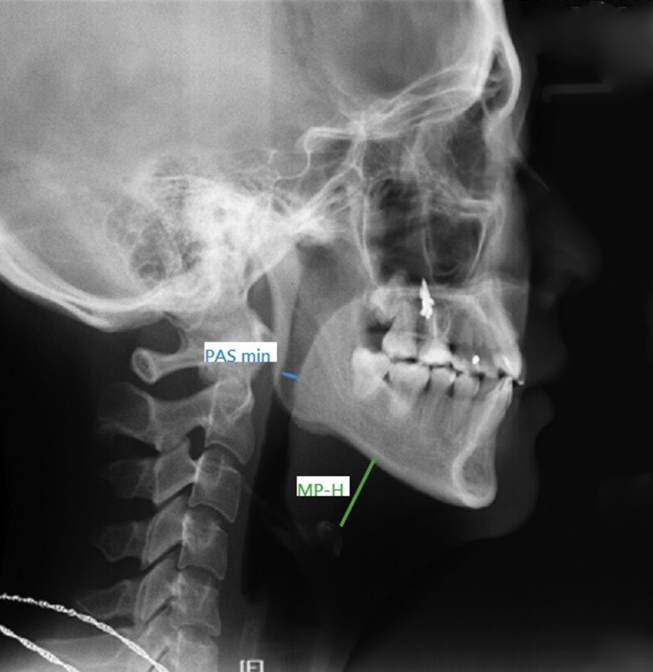
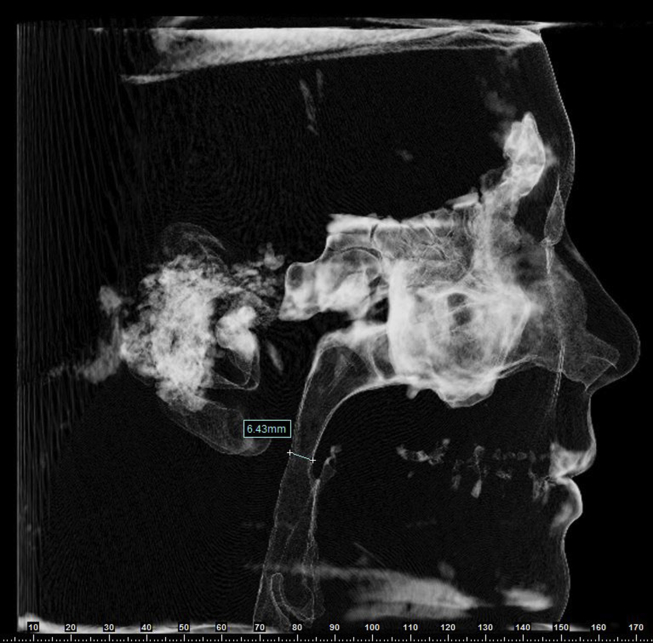
The following two pre-established measurements were marked and measured on the sagittal view of lateral cephalograms (Fig. 1) and CBCT derived from lateral cephalograms (Figure 2, Figure 3) respectively:
Figure 1.
The sagittal view of lateral cephalograms.
Figure 2.
The sagittal view of lateral cephalograms derived from cone-beam computed tomography (CBCT).
Figure 3.
The sagittal view of skull coincident to the sagittal view of Fig. 2.
Minimum of Pharyngeal airway space (PASmin): The most constricted anterior-posterior distance of upper airway, from which a line was traced perpendicular from the posterior wall of the pharynx extending to the anterior wall of the pharynx.
Mandibular plane to hyoid bone (MP-H): Linear distance along perpendicular from the most upper anterior point of hyoid bone to mandibular plane.
All measurements of lateral cephalograms and CBCT derived lateral cephalograms were performed by a single investigator. Magnification differences between cephalostats were calibrated before data analysis.
We also collected data of age, gender, Body Mass Index (BMI), skeletal pattern of each sample (Table 1).
Table 1.
All demographic data and measurements of the 21 subjects.
| No | Skeletal pattern | Age (y/o) | Gender 1: male 2: female |
BMI | PASm CBCT1 |
PASm Ceph1 |
PAS CBCT2 |
PASm Ceph2 |
MPH CBCT1 |
MPH Ceph1 |
MPH CBCT2 |
MPH Ceph2 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 29 | 1 | 24.48 | 10.24 | 14.78 | 10.44 | 14.18 | 0.88 | 9.77 | 1.1 | 8.53 |
| 2 | 2 | 34 | 2 | 19.53 | 10.2 | 12.12 | 10.19 | 11.66 | −2.44 | 4.79 | −2.82 | 4.45 |
| 3 | 3 | 19 | 1 | 22.49 | 14.18 | 16.11 | 14.44 | 16.87 | 0.36 | 5.12 | 0.91 | 5.59 |
| 4 | 2 | 17 | 1 | 18.551 | 11.48 | 9.07 | 11.82 | 8.54 | 11.02 | 16.77 | 11.23 | 17.48 |
| 5 | 2 | 37 | 2 | 18.73 | 7.13 | 7.09 | 7.16 | 6.71 | −2.46 | 10.55 | −0.97 | 10.79 |
| 6 | 3 | 31 | 1 | 22.72 | 7.9 | 6.81 | 7.86 | 7.07 | 6.65 | 10.96 | 6.47 | 10.1 |
| 7 | 2 | 17 | 2 | 24.44 | 7.02 | 7.71 | 7.26 | 8.1 | 5.89 | 15.11 | 5.44 | 14.8 |
| 8 | 3 | 20 | 2 | 18.04 | 8.58 | 7.33 | 8.36 | 7.53 | 3.56 | 8.02 | 3.67 | 11.4 |
| 9 | 2 | 19 | 1 | 20.56 | 5 | 5.37 | 4.96 | 4.67 | 7.92 | 10.76 | 7.17 | 11.13 |
| 10 | 3 | 25 | 1 | 17.91 | 4.04 | 7.61 | 4.59 | 7.16 | 8.77 | 15.04 | 8.77 | 15.69 |
| 11 | 1 | 14 | 2 | 20.9 | 6.06 | 9.01 | 6.23 | 8.06 | −2.35 | 7.91 | −2.53 | 5.35 |
| 12 | 3 | 27 | 2 | 33.59 | 6.37 | 10.43 | 6.37 | 9.27 | 11.6 | 9.52 | 12.15 | 9.03 |
| 13 | 1 | 17 | 1 | 20.42 | 12.39 | 13.14 | 12.5 | 13.09 | 15.23 | 18.12 | 15.52 | 19.17 |
| 14 | 3 | 24 | 1 | 21.7 | 5.18 | 8.57 | 5.05 | 8.01 | 10.95 | 13.17 | 10.87 | 14.18 |
| 15 | 2 | 27 | 2 | 18.21 | 6.6 | 4.84 | 6.47 | 4.67 | 18.16 | 23.91 | 17.51 | 25.4 |
| 16 | 2 | 34 | 2 | 23.32 | 7.69 | 7.32 | 4.95 | 7.35 | 7.6 | 9.41 | 7.1 | 9.79 |
| 17 | 2 | 18 | 2 | 19.84 | 5.59 | 4.08 | 5.46 | 3.75 | 13.11 | 25.24 | 12.88 | 24.87 |
| 18 | 2 | 15 | 2 | 20.83 | 6.04 | 3.74 | 6.08 | 3.44 | 13.48 | 16.27 | 13.78 | 17.56 |
| 19 | 2 | 22 | 1 | 24.5 | 5.09 | 7.9 | 5.26 | 8.75 | 18.78 | 24.52 | 18.61 | 24.16 |
| 20 | 2 | 23 | 2 | 17.15 | 6.19 | 7.06 | 5.86 | 7.55 | 2.93 | 14.31 | 3.45 | 14.64 |
| 21 | 1 | 28 | 2 | 21.98 | 7.64 | 15.28 | 7.59 | 15.67 | 7.92 | 10.14 | 8.21 | 12 |
All collected data are listed in Table 1.
Tests for intraexaminer reliability were performed. During data collection, the examiner obtained and recorded two linear measurements (PASmin and MP-H) from lateral cephalogram which was taken under upright position, and two linear measurements (PASmin and MP-H) from lateral cephalometric images derived from CBCT taken in supine position. Two weeks later, the same investigator repeated the whole procedure. Intraexaminer reliability was calculated with Paired-t test.
The software program Microsoft Excel was used for data collection. Wilcoxon Signed rank test was employed to compare each linear measurement between two methods, and the correlation between age, gender, BMI, skeletal pattern, PASmin and MP-H was analyzed with Spearman correlation. All statistical analyses were performed with the SPSS statistical software package. (Version 20.0, SPSS), 5% level of significance (P < 0.05) was used.
Results
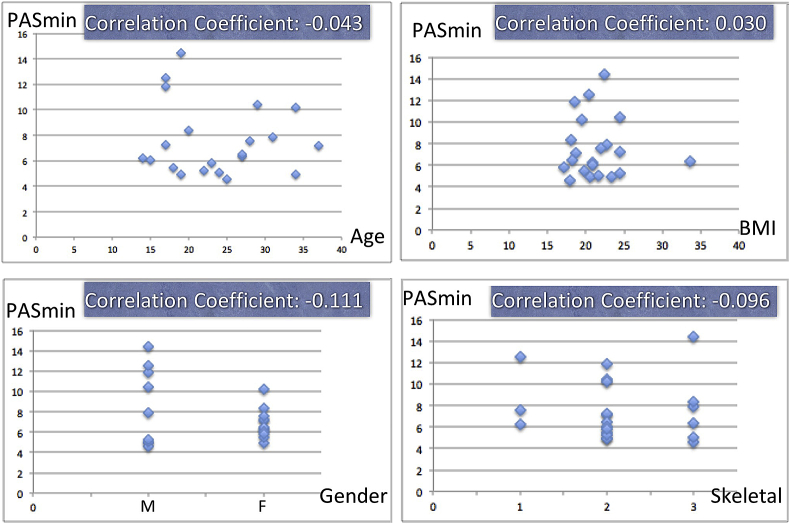
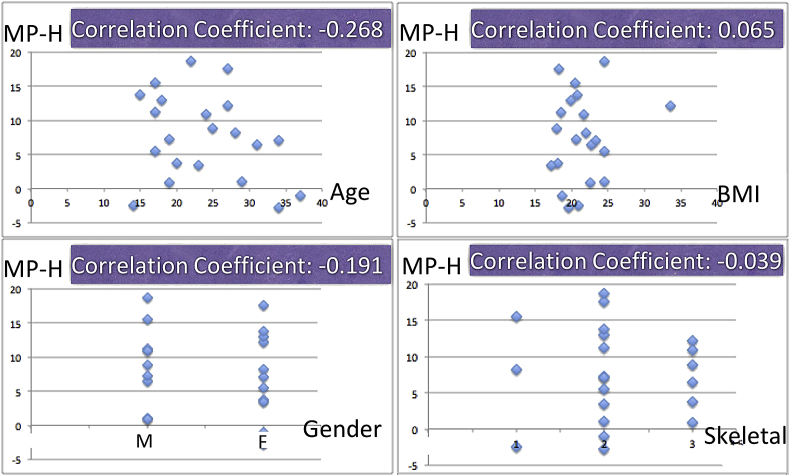
No significant difference could be identified in intraexaminer reliability. Table 1 showed PASmin collected from lateral cephalograms in upright position was larger than that taken from CBCT derived cephalometric images, but without significant difference (P = 0.073) (Table 2). However, there was significant difference of MP-H identified between two different method: the MP-H was significant larger in cephalograms taken in upright position than CBCT derived cephalometric images taken from supine position (P = 0.000) (Table 3). There was no correlations between the variables of age, gender, BMI, skeletal pattern and PASmin or between age, gender, BMI, skeletal pattern and MP-H (Figure 4, Figure 5) (Table 3). The only two variables correlated were PASmin and MP-H, and they were negative correlated (correlation coefficient: - 0.535) (Fig. 6).
Table 2.
PASmin (minimum of pharyngeal airway spaces) from Ceph and CBCT.
| PASmin | Mean | Median (25th, 75th) | P value |
|---|---|---|---|
| Ceph | 8.6714 | 8.0100 (6.890, 10.465) | 0.073 |
| CBCT | 7.5667 | 6.4700 (5.360, 9.275) |
PASmin: Minimum of Pharyngeal airway space.
Ceph: data collected by cephalogram in upright position.
CT: data collected by CBCT in supine position.
Table 3.
MP-H ( Linear distance along perpendicular from the most upper anterior point of hyoid bone to mandibular plane)from Ceph and CBCT.
| MP-H | Mean | Median (25th, 75th) | P value |
|---|---|---|---|
| Ceph | 13.624 | 12.0000 (9.410, 17.520) | 0.000* |
| CBCT | 7.5486 | 7.170 (2.275, 12.515) |
MP-H: Linear distance along perpendicular from the most upper anterior point of hyoid bone to mandibular plane.
Ceph: data collected by cephalogram in upright position.
CT: data collected by CBCT in supine position.
*p value <0.05 was considered significant.
Figure 4.
Correlation of minimum of pharyngeal airway space (PASmin) with variables of age, gender, Body Mass Index (BMI) and skeletal pattern.
Figure 5.
Correlation of mandibular plane to hyoid bone (MP-H) with variables of age, gender, BMI and skeletal pattern.
Figure 6.
The correlation between PASmin and MP-H.
Discussion
Within the limitation of the study, it can be concluded that with a change of body position from upright to supine, changes in PASmin and MP-H can be identified. PASmin is larger in lateral cephalograms (upright) than CBCT-derived cephalometric images (supine), but without statistical significance (P = 0.073). MP-H is significantly larger in lateral cephalograms (upright) than CBCT-derived cephalometric images (supine) (P = 0.000). The two variables of PASmin and MP-H are negatively correlated (r = −0.535).
OSAS has been proved to show association with systemic disease such as heart failure, ischemic heart disease, cardiac arrhythmia, and sudden cardiac death.5 It has been reported that the 5-year survival rate is about 84% for OSAS patients with apnea index exceeds 20.6 Even more, a significant prevalence of sleep apnea in a middle-aged, nonclinical population (the Wisconsin Sleep Cohort) was noticed in the first population study conducted using inlabs studies of sleep and breathing, and these findings pointed out a potential pronounces and largely undiagnosed effect of sleep-disordered breathing on public health.3 These findings clearly signaled that OSAS is a serious condition with major health-related consequences and that early screening of candidates of patient with OSAS is important. Hence, research related to airway has come into notice. In orthodontic daily practice, cephalometric is a must for clinics. This study intended to evaluate if lateral cephalogram could be an effective first line screening tool for narrow upper airway. Previous study suggested that postural effect should be taken into account while evaluating upper airway, and there was a study researching upper airway difference in lateral cephalogram in upright and supine postures.13 Our study uses CBCT for supine position as representative instead. There are several advantages using supine CBCT. First, CBCT has superior imaging modality, improved condition for visualization, better image manipulation on a 1:1 scale than lateral cephalogram.10 Second, and most importantly, upper airway obstruction during sleep usually occurs in supine position,16 the patterns of anatomic structure of upper airway under supine position should be much more similar to those while OSA occurs.
Numbers of measurement modalities have been proposed for airway evaluation.17, 18, 19, 20, 21 However, the presented means are still broad. In our study, we choose two specific measurements for representative, the most constricted linear measurement of upper airway and the linear distance along perpendicular from the most upper anterior point of hyoid bone to mandibular plane. Since increased mandibular plane to hyoid bone distance and decreased width of the posterior airway space were significant predictors of elevations in AHI.22 Also, the activity of muscle groups plays the major role in the maintenance of upper airway patency, especially genioglossus muscle, which is the largest and most powerful upper airway dilator,23 and the hyoid apparatus is also a determinant factor to maintain the patency of the pharyngeal column and thus make respiration possible.24, 25, 26 That's why we choose MP-H as one of our representative measurement, since the hyoid apparatus could almost represent the genioglossus muscle tonicity.
We found that the PASmin, which refers to the most constricted linear dimension of upper airway, is usually at the retropalatal region, which is correlated with results in the previous study.27 Our study showed no significant difference in the distance of most constricted area of pharyngeal space while change of posture in two different methods, which is correlated with previous research by Pae et al. comparing the upper airway structure in upright and supine position of 10 OSA symptom-free control group with cephalograms.13 They pointed out no significant difference of the upper part of the oropharynx while change of postures in symptom-free group, and this is correlated to our study, since the narrowest pharyngeal airway space is in the upperpart of oropharynx in most cases in our study. As for MPH, which refers to the vertical position of hyoid bone relative to the mandibular plane, showed significant difference (P = 0.000) when body posture changes from upright to supine in two different methods in our study. MPH is significant larger when body posture stays upright in lateral cephalogram, meaning hyoid bone is in significant lower position compared with supine position in CBCT. The result is correlated to previous electromyography study by Pae13 and Douglas,16 both showed genioglossus muscle activity increase in supine position in normal subjects. Though increased EMG activity cannot be directly equivalent to muscle shortening, elevation of hyoid bone position while contraction of suprahyoid muscle could be anticipated after all.
Moshiri et al.28 assessed the accuracy of number of cephalometric measurements using dry human skulls, comparing different CBCT reconstructions with lateral cephalograms. They concluded that measurements of two-dimensional reconstructions cephalograms are nearly the actual values and is more accurate than lateral cephalograms for most linear measurements calculated in the sagittal plane. So we use CBCT derived cephalograms to facilitate our study rather than sagittal or axial slices of the raw data of CBCT.
We tried to find correlation between our two measurements and the major risk factors of OSA, which were strongly signaled by populated-based cross sectional and longitudinal studies, including excess body weight, male gender, cranial facial structures and aging.3,17,29, 30, 31 However, there are some limitations in our study, which mainly has to do with our study samples. First, this study used cephalometric and CBCT data from the database of non- OSA patient in department of orthodontics, most of whom are young and not yet middle aged. Second, most of them have BMI in the normal range, so it was hard to show the possible difference of PASmin and MPH in different BMI groups. Moreover, we have limited data sample included in this study, so it was also difficult to present the possible correlation of different groups of gender and skeletal pattern if these patterns are correlated to PASmin and MPH or not. Nevertheless, we assessed soft tissue points formed by projection of shades areas, whether on cephalograms or CBCT, could hamper the accuracy of measurements. Most importantly, our study used cephalometric and CBCT data obtained in waking subjects instead of ones that were asleep, and there might be some difference between these two states.
Nevertheless, we studied patient who is subjectively healthy without any subjective symptoms of sleep-disordered disease. In the future, there should be study investigating is there difference between upright lateral cephalograms and supine CBCT in sleep-disordered patient in order to find out more informations for diagnosing sleep-disordered patients in a preliminary way.
In conclusion, whether from the aspect of cost or convenience, cephlograms remains an important preliminary tool for upper airway evaluation, despite of the popularity of 3D image nowadays. However, based on the results of this study, the two considerable measurements of upper airway change with body posture. Therefore, careful interpretation of upper airway under upright cephalograms is necessary, then one can use cephalograms as the first line diagnostic tool to rule out the candidates of upper airway abnormality, and as a preliminary screening tool to explore the candidates of OSA.
Conflicts of interest
The authors have no conflicts of interest relevant to this article.
References
- 1.Cosman B., Crikelair G.F. Mandibular hypoplasia and the late development of glossopharyngeal airway obstruction. Plast Reconstr Surg. 1972;50:573–579. doi: 10.1097/00006534-197212000-00005. [DOI] [PubMed] [Google Scholar]
- 2.Guilleminault C., Riley R., Powell N. Obstructive sleep apnea and abnormal cephalometric measurements. Implications for treatment. Chest. 1984;86:793–794. doi: 10.1378/chest.86.5.793. [DOI] [PubMed] [Google Scholar]
- 3.Young T., Palta M., Dempsey J., Skatrud J., Weber S., Badr S. The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med. 1993;328:1230–1235. doi: 10.1056/NEJM199304293281704. [DOI] [PubMed] [Google Scholar]
- 4.Kimoff R.J. Sleep fragmentation in obstructive sleep apnea. Sleep. 1996;19:S61–S66. doi: 10.1093/sleep/19.suppl_9.s61. [DOI] [PubMed] [Google Scholar]
- 5.Gami A.S., Olson E.J., Shen W.K. Obstructive sleep apnea and the risk of sudden cardiac death: a longitudinal study of 10,701 adults. J Am Coll Cardiol. 2013;62:610–616. doi: 10.1016/j.jacc.2013.04.080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kimura H. Sleep apnea syndrome and its mortality. Nihon Rinsho. 2000;58:1571–1574. [PubMed] [Google Scholar]
- 7.McNicholas W.T. Diagnosis of obstructive sleep apnea in adults. Proc Am Thorac Soc. 2008;5:154–160. doi: 10.1513/pats.200708-118MG. [DOI] [PubMed] [Google Scholar]
- 8.de Berry-Borowiecki B., Kukwa A., Blanks R.H. Cephalometric analysis for diagnosis and treatment of obstructive sleep apnea. Laryngoscope. 1988;98:226–234. doi: 10.1288/00005537-198802000-00021. [DOI] [PubMed] [Google Scholar]
- 9.Marklund M., Verbraecken J., Randerath W. Non-CPAP therapies in obstructive sleep apnoea: mandibular advancement device therapy. Eur Respir J. 2012;39:1241–1247. doi: 10.1183/09031936.00144711. [DOI] [PubMed] [Google Scholar]
- 10.Scarfe W.C., Farman A.G. What is cone-beam CT and how does it work? Dent Clin N Am. 2008;52:707–730. doi: 10.1016/j.cden.2008.05.005. [DOI] [PubMed] [Google Scholar]
- 11.Mozzo P., Procacci C., Tacconi A., Martini P.T., Andreis I.A. A new volumetric CT machine for dental imaging based on the conebeam technique: preliminary results. Eur Radiol. 1998;8:1558–1564. doi: 10.1007/s003300050586. [DOI] [PubMed] [Google Scholar]
- 12.Yildirim N., Fitzpatrick M.F., Whyte K.F., Jalleh R., Wightman A.J., Douglas N.J. The effect of posture on upper airway dimensions in normal subjects and in patients with the sleep apnea/hypopnea syndrome. Am Rev Respir Dis. 1991;144:845–847. doi: 10.1164/ajrccm/144.4.845. [DOI] [PubMed] [Google Scholar]
- 13.Pae E.K., Lowe A.A., Sasaki K., Price C., Tsuchiya M., Fleetham J.A. A cephalometric and electromyographic study of upper airway structures in the upright and supine positions. Am J Orthod Dentofacial Orthop. 1994;106:52–59. doi: 10.1016/S0889-5406(94)70021-4. [DOI] [PubMed] [Google Scholar]
- 14.Feng X., Li G., Qu Z., Liu L., Näsström K., Shi X.Q. Comparative analysis of upper airway volume with lateral cephalograms and cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 2015;147:197–204. doi: 10.1016/j.ajodo.2014.10.025. [DOI] [PubMed] [Google Scholar]
- 15.Vizzotto M.B., Liedke G.S., Delamare E.L., Silveira H.D., Dutra V., Silveira H.E. A comparative study of lateral cephalograms and cone-beam computed tomographic images in upper airway assessment. Eur J Orthod. 2012;34:390–393. doi: 10.1093/ejo/cjr012. [DOI] [PubMed] [Google Scholar]
- 16.Douglas N.J., Jan M.A., Yildirim N., Warren P.M., Drummond G.B. Effect of posture and breathing route on genioglossal electromyogram activity in normal subjects and in patients with the sleep apnea/hypopnea syndrome. Am Rev Respir Dis. 1993;148:1341–1345. doi: 10.1164/ajrccm/148.5.1341. [DOI] [PubMed] [Google Scholar]
- 17.Partinen M., Guilleminault C., Quera-Salva M.A., Jamieson A. Obstructive sleep apnea and cephalometric roentgenograms. The role of anatomic upper airway abnormalities in the definition of abnormal breathing during sleep. Chest. 1988;93:1199–1205. doi: 10.1378/chest.93.6.1199. [DOI] [PubMed] [Google Scholar]
- 18.Susarla S.M., Abramson Z.R., Dodson T.B., Kaban L.B. Cephalometric measurement of upper airway length correlates with the presence and severity of obstructive sleep apnea. J Oral Maxillofac Surg. 2010;68:2846–2855. doi: 10.1016/j.joms.2010.06.196. [DOI] [PubMed] [Google Scholar]
- 19.Sonsuwan N., Suchachaisri S., Chaloeykitti L. The relationships between cephalometric parameters and severity of obstructive sleep apnea. Auris Nasus Larynx. 2011;38:83–87. doi: 10.1016/j.anl.2010.04.009. [DOI] [PubMed] [Google Scholar]
- 20.Pracharktam N., Nelson S., Hans M.G. Cephalometric assessment in obstructive sleep apnea. Am J Orthod Dentofacial Orthop. 1996;109:410–419. doi: 10.1016/s0889-5406(96)70123-3. [DOI] [PubMed] [Google Scholar]
- 21.Ping-Ying Chiang R., Lin C.M., Powell N., Chiang Y.C., Tsai Y.J. Systematic analysis of cephalometry in obstructive sleep apnea in Asian children. Laryngoscope. 2012;122:1867–1872. doi: 10.1002/lary.23297. [DOI] [PubMed] [Google Scholar]
- 22.Pracharktam N., Hans M.G., Strohl K.P., Redline S. Upright and supine cephalometric evaluation of obstructive sleep apnea syndrome and snoring subjects. Angle Orthod. 1994;64:63–73. doi: 10.1043/0003-3219(1994)064<0063:UASCEO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 23.Dempsey J.A., Veasey S.C., Morgan B.J., O'Donnell C.P. Pathophysiology of sleep apnea. Physiol Rev. 2010;90:47–112. doi: 10.1152/physrev.00043.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Doual A., Léger J.L., Doual J.M., Hadjiat F. The hyoid bone and vertical dimension. Orthod Fr. 2003;74:333–363. [PubMed] [Google Scholar]
- 25.Van de Graaff W.B., Gottfried S.B., Mitra J., van Lunteren E., Cherniack N.S., Strohl K.P. Respiratory function of hyoid muscles and hyoid arch. J Appl Physiol Respir Environ Exerc Physiol. 1984;57:197–204. doi: 10.1152/jappl.1984.57.1.197. [DOI] [PubMed] [Google Scholar]
- 26.van Lunteren E., Haxhiu M.A., Cherniack N.S. Mechanical function of hyoid muscles during spontaneous breathing in cats. J Appl Physiol (1985) 1987;62:582–590. doi: 10.1152/jappl.1987.62.2.582. [DOI] [PubMed] [Google Scholar]
- 27.Trudo F.J., Gefter W.B., Welch K.C., Gupta K.B., Maislin G., Schwab R.J. State-related changes in upper airway caliber and surrounding softtissue structures in normal subjects. Am J Respir Crit Care Med. 1998;158:1259–1270. doi: 10.1164/ajrccm.158.4.9712063. [DOI] [PubMed] [Google Scholar]
- 28.Moshiri M., Scarfe W.C., Hilgers M.L., Scheetz J.P., Silveira A.M., Farman A.G. Accuracy of linear measurements from imaging plate and lateral cephalometric images derived from cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 2007;132:550–560. doi: 10.1016/j.ajodo.2006.09.046. [DOI] [PubMed] [Google Scholar]
- 29.Dempsey J.A., Skatrud J.B., Jacques A.J. Anatomic determinants of sleep-disordered breathing across the spectrum of clinical and nonclinical male subjects. Chest. 2002;122:840–851. doi: 10.1378/chest.122.3.840. [DOI] [PubMed] [Google Scholar]
- 30.Young T., Finn L., Austin D., Peterson A. Menopausal status and sleep-disordered breathing in the Wisconsin sleep Cohort study. Am J Respir Crit Care Med. 2003;167:1181–1185. doi: 10.1164/rccm.200209-1055OC. [DOI] [PubMed] [Google Scholar]
- 31.Young T., Peppard P.E., Taheri S. Excess weight and sleep-disordered breathing. J Appl Physiol (1985) 2005;99:1592–1599. doi: 10.1152/japplphysiol.00587.2005. [DOI] [PubMed] [Google Scholar]