Abstract
Rectal prolapse is usually of benign etiology. Rarely, sigmoido-rectal intussusception results from a malignant lead-point. We report the case of a patient with a partially obstructing sigmoid cancer causing a full thickness rectal prolapse requiring surgical intervention. An 82-year-old woman presented with 1 week of rectal bleeding, fecal incontinence, and weight loss. Computed tomography identified sigmoido-rectal intussusception. Colonoscopic biopsy revealed high-grade dysplasia. Magnetic resonance imaging demonstrated a 6-cm mass forming the lead point of the intussusceptum with epiploic appendages seen within the rectal lumen. She underwent laparoscopic low anterior resection with final pathology consistent with T2N0 adenocarcinoma, and recovered well. Among adult patients with rectal prolapse, suspicion for underlying malignancy should prompt a thorough investigation to inform the decision for resection, which may be safely performed by minimally invasive techniques.
Keywords: surgery, gastroenterology/hepatology, oncology, intussusception, cancer, imaging, computed tomography, magnetic resonance imaging, rectal prolapse
Introduction
Intestinal intussusception is rare in adults, accounting for approximately 1% of all bowel obstructions.1 The diagnosis is difficult to establish with history and physical exam findings alone. Prior to the widespread availability of multi-detector computed tomography (CT) and magnetic resonance imaging (MRI), the diagnosis was often made at laparotomy.2 Recognizing and understanding pertinent signs, symptoms, and imaging findings is essential to the early diagnosis and appropriate management of adult intussusception.
Sigmoido-rectal intussusception is a subtype of intestinal intussusception in which an intussusceptum composed of distal sigmoid or rectum prolapses through the anal canal. Rectal prolapse is usually of benign etiology. However, rectal cancer causing a prolapse has been reported.3 We report a unique case in which a partially obstructing sigmoid cancer caused full thickness rectal prolapse requiring surgical intervention.
Case report
An 82-year-old woman presented with 1 week of painless rectal bleeding and fecal incontinence in the context of 10–15 lb weight loss over 6 months and no prior colonoscopy. Her medical history was significant for dementia. Informed consent was provided by her surrogate decision-maker. Her abdomen was soft and non-tender with no appreciable mass. CT of the chest, abdomen, and pelvis demonstrated sigmoido-rectal intussusception with fat stranding in the presacral adipose tissue, without evidence of distant metastasis (Figure 1).
Figure 1.
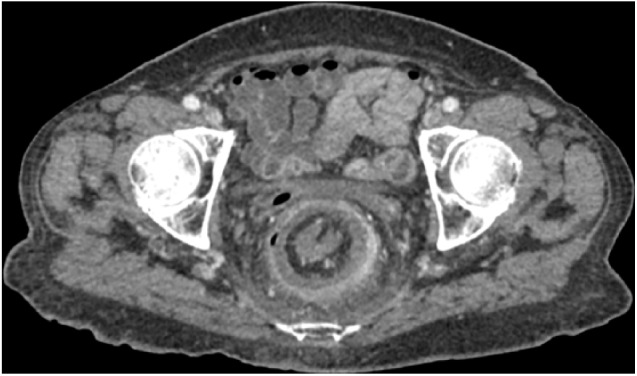
Axial computed tomography image of sigmoido-rectal intussusception with fat stranding in the presacral adipose tissue.
Colonoscopy demonstrated a malignant-appearing obstructing sigmoid tumor telescoping into the rectum (Figure 2). Cold forceps biopsies were superficial, fragmented, and demonstrated high-grade dysplasia. Serum carcinoembryonic antigen was 0.6 ng/mL (ref. 0.0–3.0 ng/mL). MRI of the pelvis demonstrated a 6 cm × 3 cm × 2 cm mass forming the lead point for sigmoido-rectal intussusception with epiploic appendages seen within the rectal lumen and no lymphadenopathy (Figure 3).
Figure 2.
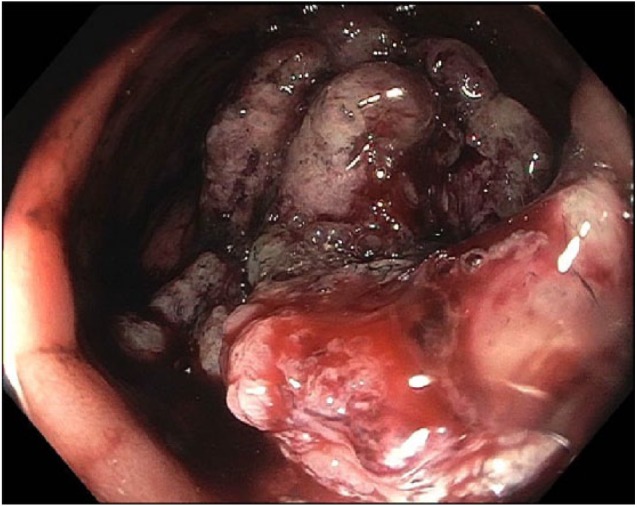
Colonoscopic image of sigmoido-rectal intussusception with epiploic appendages seen within the rectal lumen.
Figure 3.
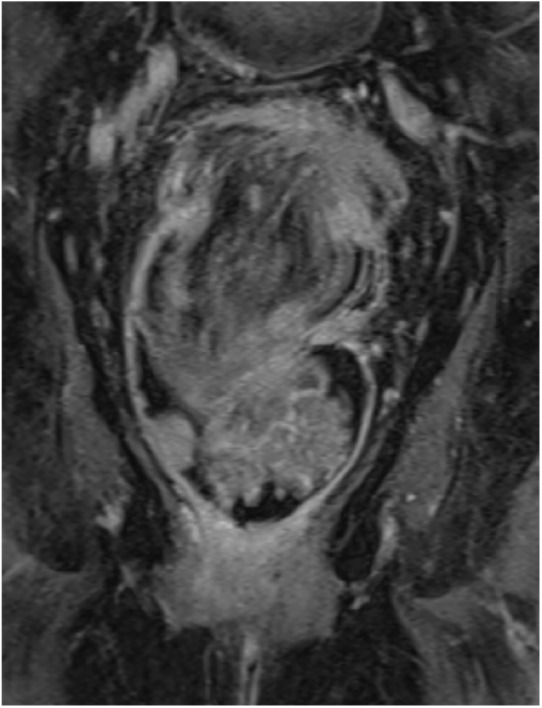
Coronal magnetic resonance image of sigmoido-rectal intussusception with epiploic appendages seen within the rectal lumen.
She underwent a laparoscopic low anterior resection. Intraoperatively, she was found to have a partially obstructed rectosigmoid mass intussuscepting into the rectum. High ligation of the superior mesenteric artery and vein were performed to allow a tension-free primary stapled anastomosis. She recovered well. Final pathology demonstrated a 6.6-cm T2N0 well-differentiated adenocarcinoma with negative margins.
Discussion
Classic descriptions of intestinal intussusception that is not associated with rectal prolapse feature the triad of abdominal pain, palpable abdominal mass, and heme-positive stools. However, this triad is rarely observed in contemporary studies.4 Therefore, early diagnosis often depends on accurate interpretation of imaging findings to avoid discovery at the time of operative exploration.1,2 For pediatric patients, ultrasonography is commonly used as a cost-effective and non-invasive means of identifying a target sign indicating intestinal intussusception. However, its utility is compromised by air within the bowel lumen, which hinders transmission of ultrasonic waves. In addition, it may be difficult to interpret abdominal ultrasound findings in adults with thick abdominal walls and greater distance between the skin and target anatomy. In cases of intussusception leading to rectal prolapse, ultrasonography may be used to assess the anatomical integrity of internal and external sphincter muscles, but other imaging modalities are more effective in assessing the intussusceptum and associated pathology.
CT has emerged as a useful imaging modality for adult intussusception, and is often performed as a primary or secondary assessment of acute and subacute gastrointestinal symptoms of unclear origin, leading to the diagnosis of intussusception in patients with atypical presentations or unreliable history and physical exam findings.5 Similar to ultrasonography, CT may demonstrate a target sign. In addition, CT provides greater detail in illustrating local and regional anatomy, which can inform operative planning.4 In cases of intussusception leading to rectal prolapse, defecating MRI has several advantages over CT.6 The dynamic nature of MR defacography allows accurate assessment of the presence of enterocele, rectocele, and anismus, which are often associated with intussusception.7 In addition, MR defacography allows for global assessment of pelvic floor movements, which can inform operative planning.8
Colonoscopy is an important modality in the diagnosis and management of adult colonic or rectal intussusception with or without rectal prolapse.9,10 This is especially true when patients present with signs and symptoms of large bowel obstruction.11,12 Colonic intussusceptums in adults often represent malignant lead-points. Colonoscopy provides direct visualization of the intussuseptum and associated intraluminal pathology and allows for biopsy and tissue diagnosis. Differentiating between benign and malignant underlying pathology informs decision-making regarding operative resection, an area of controversy.
Given the high incidence of underlying malignancy in adult intussusceptums, many advocate for routine resection.1 This seems prudent for older patients with higher likelihood of underlying malignancy and in cases in which the bowel wall is compromised, increasing the potential morbidity of operative reduction without resection. When intussusception is caused by a malignant lead-point, reduction prior to resection may promote intraluminal seeding and venous embolization.13 For colonic intussusceptums in adults, which are likely to represent malignant lead-points, resection should be performed without prior reduction.14 A laparoscopic approach appears to be safe and effective.3,5,15 The weight of evidence suggests that the role for operative reduction without resection is limited to younger patients with small bowel intussusception, low likelihood of underlying malignancy, and healthy-appearing tissues.4
Conclusion
When adult patients present with rectal prolapse of unclear etiology, the presence underlying malignancy should be investigated with a thorough history and physical examination augmented by colonoscopy with consideration of abdominal CT or MR defacography to assess for the presence of associated conditions. When a malignant lead-point is diagnosed or suspected, resection should be performed without prior reduction. Operative resection may be safely and effectively performed with minimally invasive techniques.
Footnotes
Authors’ Note: This work has not been presented at any meetings and has never been submitted elsewhere. A.C.F. and T.J.L. performed the literature review and drafted the manuscript. S.A.T., T.E.R., and A.I. provided critical revisions. All authors approved the final submitted version of the manuscript.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Ethics approval: Our institution does not require ethical approval for reporting individual cases or case series.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Informed consent: Written informed consent was obtained from the patient’s legally authorized representative for the patient’s anonymized information to be published in this article.
ORCID iDs: Tyler J Loftus  https://orcid.org/0000-0001-5354-443X
https://orcid.org/0000-0001-5354-443X
Thomas E Read  https://orcid.org/0000-0003-3760-3748
https://orcid.org/0000-0003-3760-3748
References
- 1. Azar T, Berger DL. Adult intussusception. Ann Surg 1997; 226(2): 134–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Stewardson RH, Bombeck CT, Nyhus LM. Critical operative management of small bowel obstruction. Ann Surg 1978; 187(2): 189–193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Yamamoto R, Mokuno Y, Matsubara H, et al. Laparoscopic low anterior resection for rectal cancer with rectal prolapse: a case report. J Med Case Rep 2018; 12(1): 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Takeuchi K, Tsuzuki Y, Ando T, et al. The diagnosis and treatment of adult intussusception. J Clin Gastroenterol 2003; 36(1): 18–21. [DOI] [PubMed] [Google Scholar]
- 5. Wang N, Cui XY, Liu Y, et al. Adult intussusception: a retrospective review of 41 cases. World J Gastroenterol 2009; 15(26): 3303–3308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Stoker J, Rociu E, Wiersma TG, et al. Imaging of anorectal disease. Br J Surg 2000; 87(1): 10–27. [DOI] [PubMed] [Google Scholar]
- 7. Melchior C, Bridoux V, Touchais O, et al. MRI defaecography in patients with faecal incontinence. Colorectal Dis 2015; 17(3): O62–O19. [DOI] [PubMed] [Google Scholar]
- 8. Dvorkin LS, Hetzer F, Scott SM, et al. Open-magnet MR defaecography compared with evacuation proctography in the diagnosis and management of patients with rectal intussusception. Colorectal Dis 2004; 6(1): 45–53. [DOI] [PubMed] [Google Scholar]
- 9. Rashid Z, Basson MD. Association of rectal prolapse with colorectal cancer. Surgery 1996; 119(1): 51–55. [DOI] [PubMed] [Google Scholar]
- 10. Jones OM, Cunningham C, Lindsey I. The assessment and management of rectal prolapse, rectal intussusception, rectocoele, and enterocoele in adults. BMJ 2011; 342: c7099. [DOI] [PubMed] [Google Scholar]
- 11. Hurwitz LM, Gertler SL. Colonoscopic diagnosis of ileocolic intussusception. Gastrointest Endosc 1986; 32(3): 217–218. [DOI] [PubMed] [Google Scholar]
- 12. Begos DG, Sandor A, Modlin IM. The diagnosis and management of adult intussusception. Am J Surg 1997; 173(2): 88–94. [DOI] [PubMed] [Google Scholar]
- 13. Weilbaecher D, Bolin JA, Hearn D, et al. Intussusception in adults. Review of 160 cases. Am J Surg 1971; 121(5): 531–535. [DOI] [PubMed] [Google Scholar]
- 14. Eisen LK, Cunningham JD, Aufses AH., Jr. Intussusception in adults: institutional review. J Am Coll Surg 1999; 188(4): 390–395. [DOI] [PubMed] [Google Scholar]
- 15. Park KK, Lee SH, Baek SU, et al. Laparoscopic resection for middle and low rectal cancer. J Minim Access Surg 2014; 10(2): 68–71. [DOI] [PMC free article] [PubMed] [Google Scholar]


