Abstract
As health systems seek to incentivize physicians to deliver high-value care, the relationship between physician compensation and health care delivery is an important knowledge gap. To examine physician compensation nationally and its relationship with care delivery, we examined 2012-2015 cross-sectional data on ambulatory primary care physician visits from the National Ambulatory Medical Care Survey. Among 175 762 office visits with 3826 primary care physicians, 15.4% of primary care physicians reported salary-based, 4.5% productivity-based, and 12.9% “mixed” compensation, while 61.4% were practice owners. After adjustment, delivery of out-of-visit/office care was more common for practice owners and “mixed” compensation primary care physicians, while there was little association between compensation type and rates of high- or low-value care delivery. Despite early health reform efforts, the overall landscape of physician compensation has remained strongly tethered to fee-for-service. The lack of consistent association between compensation and care delivery raises questions about the potential impact of payment reform on individual physicians’ behavior.
Keywords: physician compensation, quality of care, health care delivery, primary care, payment models
What do we already know about this topic?
Physician compensation has implications for the kind, quality, and quantity of health care provided to patients, and recent payment reforms have attempted to tie physician compensation to measures of quality of care.
How does your research contribute to the field?
We investigate whether compensation affects primary care physicians’ likelihood to provide certain forms of health care that are typically uncompensated, as well as whether their compensation affects their likelihood to provide high quality/low-value forms of care.
What are your research’s implications toward theory, practice, or policy?
Our results indicate that primary care physician compensation is still dominated by productivity-based payment despite the movement toward payment reform and that compensation models have little association with practice patterns.
In an effort to restrain health care cost growth and improve quality of care, the US Department of Health and Human Services has committed to the ambitious goal of tying 90% of all Medicare provider payments to quality or value-based measures by 2018.1 This reflects building momentum across the health care system away from fee-for-service (FFS) as the predominant payment model for physician services, motivated by the widespread belief that FFS promotes wasteful use of health care resources.2,3 One open question in the movement away from FFS, which has largely focused on system-level payment arrangements, is how physician compensation models in primary care, such as salaried vs productivity-based payments, are associated with meaningful differences in behavior. Primary care is central to many payment reforms, including the Comprehensive Primary Care Initiative and Accountable Care Organizations, which base their payments on individuals receiving primary care in an organization to assess performance on quality of care and efficient use of resources.4-6 In light of these changes, we expect that health systems will seek ways of transmitting incentives to front-line physicians, heightening the importance of closing the knowledge gap on the relationship between compensation and health care.
The structure of physician compensation has important implications for health care delivery and spending. The theoretical relationship between physicians’ financial incentives and health care utilization is well founded in the literature.7-9 Empirically, physician compensation in the United States is typically either salaried, where physicians are paid a fixed amount per session or other unit of time or productivity-based, where physicians are compensated based on volume or a share of practice billings, possibly as an owner or part-owner of a practice.10 The most recent evidence on physician compensation is over a decade old, but has showed that productivity-based compensation predominated.10,11 Research suggests that productivity-compensated physicians tend to generate higher annual health care expenditures and higher spending per episode compared with salaried physicians.11,12 However, the relationship between physician compensation model and quality of care is mixed.11,13,14
Beyond cost and quality, physician compensation could also influence how primary care is delivered. Effective primary care entails not only the conventional face-to-face visit between physicians and patients but also out-of-visit care, such as patient follow-up in hospitals or home, care coordination via e-mail, or phone consultations. In a purely FFS model, physicians typically are only compensated for care that occurs during the in-person visit, potentially discouraging out-of-visit care.15 It is possible that primary care physicians (PCPs) under other compensation methods may be more likely to engage in care delivery outside of the office visit, such as patient e-mails or home visits. However, there is little evidence assessing this question.
We analyzed 3 waves of physician office visits from 2012 to 2015 to examine the landscape of physician compensation in the United States in the current era of health reform. We assessed whether patterns of PCP compensation were associated with out-of-visit care patterns, as well as the provision of high- or low-value care. These analyses examining the relationship between physician compensation and patterns of care can provide testable hypotheses about the role of physicians’ financial incentives as payment reform advances.
Data and Methods
Study Population and Data
We used data for 2012 through 2015 from the publicly available National Ambulatory Medical Care Survey (NAMCS), which is administered by the National Center for Health Statistics at the Centers for Disease Control and Prevention. National Ambulatory Medical Care Survey is a nationally representative annual survey of nonfederal physicians in ambulatory settings (except for community health centers and outpatient hospital departments, which are sampled in different surveys). National Ambulatory Medical Care Survey samples a random week of office visits for each of a nationally representative sample of physicians in a multistage, probabilistic survey design, with each observation representing an office visit during a physician’s sampling period. Data collected include not only patient demographics, payer source, patients’ reason for visit, physician diagnosis, and treatment choices at the visit level but also physician practice-level characteristics, such as type of office setting, compensation type, sources of revenue, specialties available, and electronic health records availability. We only included office visits for adults aged 18 years and older and excluded PCPs without available compensation data (5.7% of sample PCPs without data). We defined PCPs as physicians with a specialty of internal medicine, general and family practice (as labeled in NAMCS), or pediatrics. Our analysis used publicly available data and was deemed nonhuman subjects research by the institutional review board at the Harvard T.H. Chan School of Public Health.
Defining Physician Compensation
Our main exposure of interest was the self-reported compensation model for PCPs as defined in NAMCS. Physician compensation was defined by 3 separate questions in the NAMCS survey instrument: (1) physicians’ “overall” compensation type (salaried, productivity-based, or mixed; 9% of physicians self-reported “other,” which we do not examine), where mixed refers to those paid a base salary and a mixture of financial incentives or practice workload share; (2) whether physicians were owners, part owners, or solo practitioners; and (3) questions related to 6 different factors affecting compensation (FACs), including physician productivity, overall practice financial performance, adherence rate to quality measures, patient satisfaction surveys, and practice-level profiling of medical resource use. Because the financial influence of practice ownership might affect the delivery of care in a fundamentally different way than any other type of financial incentives, we focused our analysis on physicians who were employees and not full or partial owners of their practice. We then separated PCPs into 3 categories: employee PCPs compensated via salary, productivity-based, or “mixed” compensation, respectively. As a supplemental analysis, we separately examined physicians who were practice owners (full or partial) stratified by whether or not they were in a solo practice.
To examine the sensitivity of our results to the definition of compensation type, we reproduced our analysis using an alternate version of the compensation exposure variable. Our goal was to define compensation types falling into 2 general categories: purely productivity-based (standard FFS) vs compensation incorporating clinical performance. In the alternate version, we stratified physicians by their stated FACs alone into 2 groups: those that cited practice finances or personal productivity FACs alone (standard FFS model) and those citing any clinical FACs such as patient satisfaction or quality measurement.
Out-of-Visit/Office Care
We examined PCPs’ likelihood of providing nonvisit-based care that is generally uncompensated or undercompensated by insurers relative to physician time (eg, extra time required for home visits or telephone calls, denoted as “out-of-visit care”). These activities were assessed at the individual physician level as binary indicators for whether a physician provided a given out-of-visit/office service in their last “normal week” of care. These measures included whether physicians visited patients in their hospital, home, or nursing home, and whether they performed phone or electronic patient consultations.
Low- and High-Value Care Measures
We used visit-level data to construct a set of low- and high-value care measures that have been used in previous research.16-19 High-value care measures used in this analysis were based on guidelines from the US Preventative Services Task Force and other professional societies. These included counseling for tobacco cessation; weight-loss counseling among obese patients; appropriate care for coronary heart disease, cardiovascular disease, congestive heart failure, depression, and osteoporosis; anticoagulant use for atrial fibrillation; and statin use for diabetic patients (see Table A1 in Online Appendix for detailed definitions).20,21 We based our low-value care measures on published guidelines such as the “Choosing Wisely” initiative,22,23 existing medical literature, and defined them as advanced imaging for sinusitis, low-value screening tests in general medical examinations (GME), and inappropriate opioid or imaging use for lower back pain or headaches.19,24,25 We also estimated a composite measure for any delivery of high- or low-value care, which we constructed by calculating the ratio of the number of low-value (or high-value) services provided in each visit over the total number of low-value (or high-value) services eligible in that visit.16 Some visits were eligible for multiple services, in which case we multiplied visit weights by the number of eligible services, yielding the rate at which low-value (high-value) care was provided over all eligible instances of each measure.
Statistical Analysis
We used weighted cross-tabulations to present our descriptive analyses of compensation types in our sample, examining mutually exclusive survey-weighted frequencies of each of the possible combinations of FACs.
For adjusted analyses, we fitted logistic regression models to estimate the association between physician compensation type (employees with productivity, salaried or mixed compensation), and patterns of care delivery (out-of-visit/office care or low-/high-value care in a visit). Physicians who were solo or nonsolo practice owners were analyzed separately. For each outcome, we presented unadjusted results and subsequently adjusted for patient demographics and practice-level variables, including average age and number of patient chronic conditions, patient sex, race/ethnicity, electronic records usage, rural office setting, practice ownership status, and percentage revenue from Medicare, Medicaid, and private insurers. The adjusted results for our composite measures used the proportion of all eligible visits that had either low- or high-value care delivered as the outcome and was estimated using fractional logistic regression.26
For all analyses, we used robust design-based variance estimators to account for clustering within geographic areas or physicians and NAMCS survey weights to account for survey design and nonresponse. We reported 95% confidence intervals (CIs) for all estimates. All analyses were executed using STATA version 15.
Results
Our sample of employee physicians included 35 016 office visits from 1257 PCPs occurring from 2012 to 2015, representing nearly 6.2 billion office visits and 206 465 PCPs nationally with survey weighting. In our weighted sample, 52.7% of PCPs were salaried employees, 11.3% were productivity-based employees, and 36.0% were mixed compensation employees (Tables 1 and 2). There were differences in patient mix across compensation types and ownership status (Table 1 and Table A2 in Online Appendix). For example, salaried PCPs’ patient mix was more racially diverse relative to other compensation types (non-Hispanic whites accounted for 59.9% of patients, vs 78.8% for productivity-based PCPs, 77.3% for mixed compensation PCPs), and they were more likely to be located in the South (41.7% of patients, vs 28.8% for productivity-based PCPs, 33.3% for mixed compensation PCPs, Table 1).
Table 1.
Patient and Physician Characteristics by PCP Compensation Type.
| Salary employee | Productivity employee | Mixed employee | ||||
|---|---|---|---|---|---|---|
| Patient visits (n raw) | 25 270 | 8208 | 24 281 | |||
| Patient visits (n weighted) | 321 403 029 | 65 975 411 | 230 843 894 | |||
| Patient visit characteristics | ||||||
| Age (mean) | 41.4 | (38.9-44.7) | 41.6 | (37.6-45.5) | 41.6 | (38.9-44.3) |
| Female | 61.4% | (0.59-0.64) | 58.6% | (0.55-0.66) | 60.4% | (0.58-0.63) |
| Race/ethnicity | ||||||
| Non-Hispanic white | 59.9% | (0.53-0.67) | 78.8% | (0.74-0.84) | 77.3% | (0.74-0.81) |
| Non-Hispanic black | 13.3% | (0.09-0.17) | 7.6% | (0.05-0.10) | 8.5% | (0.07-0.10) |
| Hispanic | 19.9% | (0.16-0.24) | 9.3% | (0.06-0.12) | 8.4% | (0.07-0.10) |
| Non-Hispanic other | 6.9% | (0.05-0.09) | 4.4% | (0.03-0.06) | 5.8% | (0.04-0.08) |
| Number of chronic diseases | ||||||
| 0 | 43.7% | (0.39-0.49) | 45.0% | (0.39-0.51) | 45.2% | (0.41-0.49) |
| 1 | 22.7% | (0.19-0.30) | 20.0% | (0.17-0.23) | 19.6% | (0.18-0.21) |
| 2 | 14.1% | (0.12-0.16) | 13.6% | (0.12-0.16) | 14.1% | (0.13-0.16) |
| 3 | 10.7% | (0.09-0.12) | 10.9% | (0.09-0.13) | 10.5% | (0.09-0.12) |
| 4+ | 8.8% | (0.07-0.10) | 10.4% | (0.07-0.14) | 10.5% | (0.09-0.12) |
| Region | ||||||
| Northeast | 12.7% | (0.09-0.17) | 8.8% | (0.03-0.15) | 15.2% | (0.10-0.20) |
| Midwest | 16.7% | (0.12-0.22) | 38.6% | (0.27-0.51) | 32.6% | (0.25-0.40) |
| South | 41.7% | (0.32-0.51) | 28.8% | (0.19-0.38) | 33.3% | (0.27-0.40) |
| West | 29.0% | (0.22-0.36) | 23.8% | (0.15-0.33) | 18.9% | (0.14-0.24) |
| Rural visit location | 12.9% | (0.07-0.19) | 11.4% | (0.06-0.17) | 12.8% | (0.09-0.17) |
| Insurance type | ||||||
| Private | 54.2% | (0.50-0.58) | 59.2% | (0.54-0.65) | 59.4% | (0.57-0.62) |
| Medicare | 21.9% | (0.19-0.25) | 24.1% | (0.19-0.29) | 23.4% | (0.21-0.26) |
| Medicaid/Children’s Health Insurance Program | 17.0% | (0.14-0.20) | 10.9% | (0.08-0.14) | 13.1% | (0.10-0.16) |
| Other | 7.0% | (0.05-0.09) | 5.7% | (0.04-0.08) | 4.1% | (0.03-0.05) |
| Practice characteristics | ||||||
| Who owns the practice? | ||||||
| Physician groups | 41.6% | (0.32-0.51) | 28.7% | (0.19-0.38) | 33.0% | (0.26-0.39) |
| Academy/community | 18.0% | (0.13-0.23) | 25.5% | (0.16-0.35) | 32.4% | (0.25-0.40) |
| Insurer/health maintenance organization | 33.5% | (0.26-0.41) | 36.1% | (0.24-0.48) | 29.4% | (0.23-0.35) |
| Capitation revenue | ||||||
| 0%-25% revenue | 53.9% | (0.45-0.63) | 73.5% | (0.64-0.83) | 59.0% | (0.52-0.66) |
| 26%-50% revenue | 3.9% | (0.02-0.06) | 4.9% | (0.00-0.10) | 4.9% | (0.02-0.08) |
| 51%-75% revenue | 7.4% | (0.03-0.12) | 0.0% | (0.00-0.00) | 2.8% | (0.01-0.05) |
| More than 75% revenue | 4.9% | (0.02-0.08) | 0.0% | (0.00-0.00) | 4.0% | (0.01-0.07) |
| Missing | 29.8% | (0.22-0.37) | 21.6% | (0.14-0.30) | 28.8% | (0.23-0.35) |
Note. Table presents estimates of sample demographic characteristics stratified by PCP compensation type; 95% confidence interval in parentheses. PCP = primary care physician.
Table 2.
Factors Affecting Compensation (FACs).
| Salary employee | Productivity employee | Mixed employee | |
|---|---|---|---|
| Physicians (n raw) | 590 | 172 | 495 |
| Physicians (n weighted) | 108 847 | 23 307 | 74 311 |
| Practice finances | 50.6% (0.44-0.57) | 41.8% (0.31-0.53) | 56.1% (0.49-0.62) |
| Personal productivity | 55.9% (0.49-0.62) | 85.9% (0.79-0.93) | 87.1% (0.83-0.91) |
| Patient satisfaction | 25.3% (0.20-0.31) | 19.4% (0.12-0.26) | 38.2% (0.32-0.44) |
| Quality measures | 22.1% (0.17-0.27) | 36.1% (0.25-0.48) | 46.1% (0.40-0.52) |
| Practice profiling | 12.3% (0.08-0.16) | 7.7% (0.03-0.13) | 21.5% (0.17-0.26) |
Note. χ2 P value for differences in FACs across compensation types is 0.00 at the 95% confidence interval. Physicians could check more than 1 FAC in the survey, thus these totals are not mutually exclusive.
The most common FACs were personal productivity and practice finances, which was consistent across compensation types. However, productivity-based and mixed compensation employees were more likely to cite productivity-based FACs relative to salaried employee PCPs (85.9%, 87.1% vs 55.9%, respectively, P < .001; Table 2). Fewer PCPs reported having compensation based on clinical performance measures. Of these, the most frequently cited FAC was quality measures among mixed compensation PCPs (46.1%; 95% CI = 40.0%-52.0%), which was significantly less likely among salaried PCPs (22.1%, 95% CI = 20.0-31.0). Owner/solo practitioners reported lower rates of these clinical FACs relative to other compensation types (Table A3 in Online Appendix). Fewer than 5% of physicians exclusively cited clinical performance FACs and none of the productivity or financial FACs.
Rates of out-of-visit/office care delivery had a mixed association with compensation type. For example, productivity-based employees were less likely than mixed employees to use phone consults (52.4% vs 38.0% for owners vs productivity-based employees, respectively, adjusted OR [aOR] = 2.50, 95% CI = 1.18-5.30, Table 3), though not for nursing home visits (17.1% vs 8.7%, aOR = 0.34, 95% CI = 0.12-0.93). Physician owners had high rates of hospital visits and phone consults relative to productivity-based employees (Table A4 in Online Appendix).
Table 3.
Out-of-Visit/Office Care by Primary Care Physician Ownership and Compensation Type.
| Percentage (95% CI) |
Unadjusted OR (95% CI) |
Adjusted OR (95% CI) |
|
|---|---|---|---|
| Home visits | |||
| Productivity employee | 3.6 (0.02-0.08) | — | — |
| Salary employee | 4.3 (0.04-0.09) | 1.22 (0.40-3.72) | 0.72 (0.18-2.91) |
| Mixed employee | 2.6 (0.01-0.05) | 0.73 (0.26-2.03) | 0.46 (0.11-1.91) |
| Nursing house visits | |||
| Productivity employee | 17.1 (0.11-0.26) | — | — |
| Salary employee | 8.1 (0.05-0.12) | 0.43* (0.21-0.86) | 0.34* (0.12-0.93) |
| Mixed employee | 8.7 (0.06-0.12) | 0.46* (0.25-0.87) | 0.45 (0.19-1.08) |
| Hospital visits | |||
| Productivity employee | 30.5 (0.22-0.40) | — | — |
| Salary employee | 32.1 (0.26-0.38) | 1.07 (0.65-1.77) | 1.01 (0.47-2.15) |
| Mixed employee | 37.2 (0.32-0.43) | 1.35 (0.82-2.21) | 1.67 (0.91-2.90) |
| Phone consults | |||
| Productivity employee | 38.0 (0.28-0.49) | — | — |
| Salary employee | 51.8 (0.46-0.58) | 1.75* (1.06-2.90) | 1.53 (0.71-3.29) |
| Mixed employee | 52.4 (0.46-0.59) | 1.79* (1.08-2.99) | 2.50* (1.18-5.30) |
| E-mail consults | |||
| Productivity employee | 14.6 (0.09-0.23) | — | — |
| Salary employee | 22.9 (0.18-0.28) | 1.73 (0.91-2.28) | 2.19 (0.96-4.97) |
| Mixed employee | 30.9 (0.25-0.37) | 2.62† (1.38-4.97) | 2.37* (1.04-5.35) |
| Observations (raw/weighed) | 7595/623 039 | ||
Note. Adjusted model uses productivity-based employee physicians as reference category. Adjusters are patient demographics, such as racial/ethnic, urban/rural, age, gender and number of chronic conditions, as well as practice-level characteristics including percentage of revenue from Medicare, Medicaid and private insurance, revenue subject to capitation, and electronic health records availability. OR = odds ratio; CI = confidence interval.
P < .01. *P < .05.
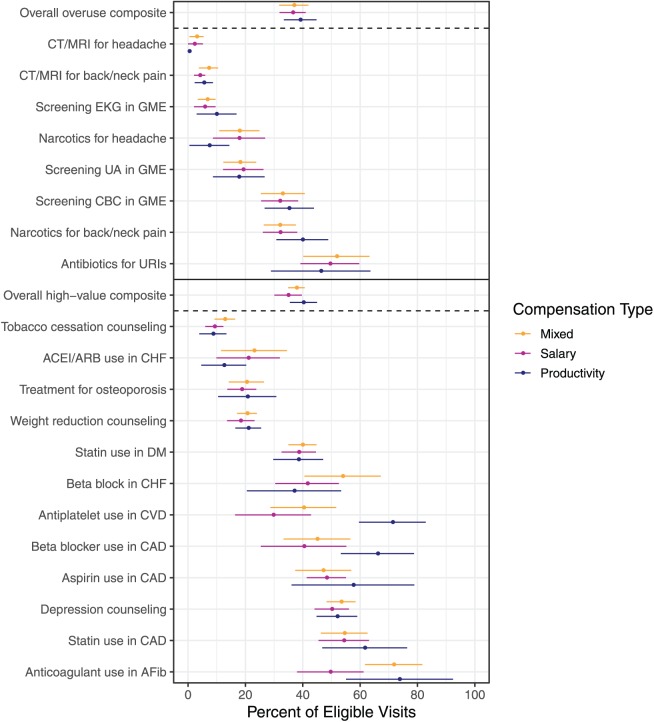
Examining the delivery of high- or low-value care across different compensation models, unadjusted estimates showed comparable effects across salary types and ownership with some exceptions (Figure 1 and Table A5 in Online Appendix). There was no clear pattern in quality toward 1 model vs another and some quality measures had low sample sizes. In adjusted estimates, there was no difference in the rate of high-value care delivery for salaried employees (aOR = 1.07; 95% CI = 0.75-1.54) or mixed compensation employees (aOR = 1.01; 95% CI = 0.74-1.38) relative to productivity-based employee PCPs (Table 4). There was similarly no meaningful difference in composite rates of low-value care delivery by productivity-based employee PCPs vs salaried (aOR = 0.82; 95% CI = 0.59-1.12) or mixed employee PCPs (aOR = 0.94; 95% CI = 0.70-1.27; Table 4).
Figure 1.
Overuse and quality measures by primary care physician compensation type.
Note. All points and error bars indicate unadjusted survey weighted estimates with corresponding 95% confidence intervals. The estimates are colored according to compensation type (dark blue is productivity, purple is salary and orange is mixed). All estimates are survey-weighted proportions accounting for NAMCS sample design. Low- and high-value care composites calculated at the visit level as the proportion of low- or high-value services delivered at a visit. To account for visits qualifying for more services than others, survey weights were multiplied by the number of eligible low- or high-value measures. CT = computed tomography; MRI = magnetic resonance imaging; GME = general medical examination; UA = urinalysis; CBC = complete blood count; URI = upper respiratory tract infection; ACE = angiotensin-converting enzyme inhibitor, ARB = angiotensin receptor blocker; CHF = congestive heart failure; DM = diabetes mellitus; CVD = cerebrovascular disease; CAD = coronary artery disease; AF = atrial fibrillation; CI = confidence interval; EKG = electrocardiogram.
Table 4.
Overuse and Quality Measures by PCP Ownership and Compensation Type—Adjusted Results.
| High-value composite | Low-value composite | |||
|---|---|---|---|---|
| (n raw) | 16 071 | 18 451 | ||
| (n weighted) | 343 345 160 | 365 902 345 | ||
| Unadjusted OR (95% CI) | Adjusted OR (95% CI) | Unadjusted OR (95% CI) | Adjusted OR (95% CI) | |
| Productivity employee | Ref | Ref | Ref | Ref |
| — | — | — | — | |
| Salary employee | 0.89 | 1.07 | 0.79 | 0.82 |
| (0.66-1.22) | (0.75-1.54) | (0.60-1.06) | (0.59-1.12) | |
| Mixed compensation employee | 0.91 | 1.01 | 0.90 | 0.94 |
| (0.66-1.26) | (0.74-1.38) | (0.71-1.14) | (0.70-1.27) | |
Note. Results are odds ratios and 95% CIs in parentheses. Compensation reference group is productivity-based employee PCPs. Full adjusted results are given in Table A3 in Online Appendix. Low- and high-value care composites calculated at the visit level as the proportion of low- or high-value services delivered at a visit. To account for visits qualifying for more services than others, survey weights were multiplied by the number of eligible low- or high-value measures. PCP = primary care physician; OR = odds ratio; CI = confidence interval.
Examining our alternate definition of compensation type, there were differences in the delivery of out-of-visit/office care. After adjustment, physicians with only productivity-based FACs reported higher rates of home visits and lower rates of e-mail consults vs physicians with any clinical performance FACs (Table A6 in Online Appendix). As with our main analysis, there was no significant association between our alternate compensation definition and the delivery of high-/low-value care measures (Table A7 in Online Appendix).
Discussion
In this analysis of a nationally representative sample of PCPs from 2012 to 2015, we found little evidence that physician compensation type was systematically associated with differences in the quality of care and mixed associations with the delivery of out-of-visit care. The minimal association between quality and compensation held across multiple measures of high- and low-value care and with an alternate definition of compensation model. Although this is a cross-sectional study that should not be interpreted as causal, the lack of an association between quality and compensation is consistent with the mixed and largely disappointing impact of “pay for performance” programs on quality of care.27,28
We also found that despite early health reform efforts, as of 2015, the overall landscape of physician compensation has remained strongly tethered to FFS. Productivity- and practice-level financial factors dominated clinical factors such as patient satisfaction and quality benchmarks where performance-based payments were reported. This is largely unchanged from prior survey data which found that 82% of PCPs in 1994 and 88% in 2005 were either owners or paid based on productivity or a mix of productivity and salary.12,13 These results are also consistent with a large multistate qualitative study of health care payment models and physician practice performed in 2014, within the time frame of our sample.29 This study found that incentives from new payment models were not translated into individual physician compensation in their sample, and that even in practices with significant involvement in alternative payment models, there was significant pressure to increase financial productivity.29
Our findings on the relationship between out-of-visit/office care and compensation model were mixed. Although typically uncompensated or undercompensated, these forms of care are deemed essential elements of effective primary care.30 Although we hypothesized that employee salaried PCPs would have higher rates of participation in these types of care relative to other PCPs, our results are inconsistent with this hypothesis. Salaried physicians were somewhat more likely to deliver certain types of care, such as phone or e-mail consults, vs productivity-based physicians, but these associations were not significant after adjustment. The most consistent patterns were for “mixed” compensation PCPs, who were more likely to deliver phone and e-mail consults than productivity-based PCPs, though not all of these associations were significant after adjustment. These results might reflect that institutional and practice-level factors are more important for the delivery of out-of-visit/office care than compensation strategy.
At first glance, the lack of relationship between compensation and low-value care or some forms of out-of-visit/office care could be viewed as inconsistent with a positive relationship between FFS and overuse. However, we do not interpret this analysis as contradicting this relationship. Physicians may describe their compensation as “salaried” with or without performance-based factors in their compensation, but they may still operate in a largely FFS culture.29 Most salaried physicians reported that their practices received little revenue from capitated contracts, suggesting that at the practice level, FFS payments remain an important factor. Therefore, it is possible that classifying physician compensation as “salary” or “productivity” based is too imprecise to accurately capture truly distinct payment models, explaining the lack of consistent contrast between these physician groups.
This study has several limitations. First, our analysis is cross-sectional and observational in nature, precluding the establishment of causality between physician compensation models and patterns of care delivery explored above. Selection concerns are also important: PCPs might self-select into practices or compensation arrangements based on factors that are correlated with our outcomes. In addition, we perform many hypothesis tests in this analysis without correction for multiple testing, but our results should be regarded as exploratory and our interpretation focuses on broader patterns beyond individual significant results. A second issue is that our measure of physician compensation type is self-reported, subject to recall or measurement error. However, a physician’s perceived compensation type and reported set of FACs is arguably a more accurate reflection of the incentives under which they provide care. Despite this, we are unable to assess the magnitude of heterogeneity or error in self-reported compensation type, so these analyses should be viewed as exploratory. In addition, our compensation measures are binary and can have overlapping profiles with FACs, limiting our ability to stratify by intensity of each factor that affects compensation and provide more precise estimates. Therefore, we were unable to examine or quantify the impact of financial incentives of varying magnitude, which is an important research question to address in the future. Another issue is that NAMCS, as any survey, is subject to sampling and measurement error.31 We addressed this concern by pooling 3 years of NAMCS data and using several measures for each outcome of interest. Another issue is that NAMCS is nationally representative of community-based independent physician practices but does not sample hospital outpatient departments or community health centers (as of 2012, the first year of our data). Therefore, our results may not generalize to physicians employed by hospitals working in outpatient departments or community health centers. Finally, our quality/overuse measures lack comprehensive exclusion criteria given that a patient’s full clinical history is unavailable. However, we do not expect systematic differences in this lack of information between our PCP and patient subgroups.
Spurred by Medicare policy changes and demonstration projects, payment reform continues to unfold across the United States. Although these efforts were underway during our study period, we did not observe a meaningful shift away from purely productivity-based compensation. However, there were few differences between practice patterns of physicians with different self-reported compensation. The lack of consistent association between compensation and care delivery suggests that payment reform might have an attenuated impact for individual physicians. It remains to be seen how compensation and financial incentives for individual physicians will evolve as alternative payment models and value-based purchasing programs take root and mature.
Supplemental Material
Supplemental material, Online_appendix for The Association Between Primary Care Physician Compensation and Patterns of Care Delivery, 2012-2015 by Adrian Garcia Mosqueira, Meredith Rosenthal and Michael L. Barnett in INQUIRY: The Journal of Health Care Organization, Provision, and Financing
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported by The National Science Foundation Graduate Research Fellowship (AGM).
Supplemental Material: Supplemental material for this article is available online.
ORCID iDs: Adrian Garcia Mosqueira  https://orcid.org/0000-0001-8210-2489
https://orcid.org/0000-0001-8210-2489
Michael L. Barnett  https://orcid.org/0000-0002-4884-6609
https://orcid.org/0000-0002-4884-6609
References
- 1. Burwell SM. Setting value-based payment goals—HHS efforts to improve US health care. N Engl J Med. 2015;372(10):897-899. [DOI] [PubMed] [Google Scholar]
- 2. Fisher ES, Bynum JP, Skinner JS. Slowing the growth of health care costs—lessons from regional variation. N Engl J Med. 2009;360(9):849-852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Fisher E, Goodman D, Skinner J, Bronner K. Health care spending, quality and outcomes: more isn’t always better. Dartmouth Inst Heal Policy Clin Pract Dartmouth, New Hampsh. 2009;27: 1-6. [PubMed] [Google Scholar]
- 4. Doherty RB. Goodbye, sustainable growth rate—hello, merit-based incentive payment system. Ann Intern Med. 2015;163(2):138-139. [DOI] [PubMed] [Google Scholar]
- 5. McWilliams JM, Hatfield LA, Chernew ME, Landon BE, Schwartz AL. Early performance of accountable care organizations in Medicare. N Engl J Med. 2016;374(24):2357-2366. doi: 10.1056/NEJMsa1600142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Peikes D, Dale S, Ghosh A, et al. The comprehensive primary care initiative: effects on spending, quality, patients, and physicians. Health Aff (Millwood). 2018;37(6):890-899. doi: 10.1377/hlthaff.2017.1678. [DOI] [PubMed] [Google Scholar]
- 7. McGuire TG. Physician agency. Handb Heal Econ. 2000;1:461-536. [Google Scholar]
- 8. Clemens J, Gottlieb JD. Do physicians’ financial incentives affect medical treatment and patient health. Am Econ Rev. 2014;104(4):1320-1349. doi: 10.1257/aer.104.4.1320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Gruber J, Owings M. Physician financial incentives and cesarean section delivery. Rand J Econ. 1996:99-123. [PubMed] [Google Scholar]
- 10. Landon BE, Reschovsky JD, Pham HH, Kitsantas P, Wojtuskiak J, Hadley J. Creating a parsimonious typology of physician financial incentives. Health Serv Outcomes Res Methodol. 2009;9(4):213-233. doi: 10.1007/s10742-010-0057-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Landon BE, O’Malley AJ, McKellar MR, Reschovsky JD, Hadley J. Physician compensation strategies and quality of care for Medicare beneficiaries. Am J Manag Care. 2014;20(10):804-811. [PMC free article] [PubMed] [Google Scholar]
- 12. Landon BE, Reschovsky JD, O’Malley AJ, Pham HH, Hadley J. The relationship between physician compensation strategies and the intensity of care delivered to Medicare beneficiaries. Health Serv Res. 2011;46(6, pt 1):1863-1882. doi: 10.1111/j.1475-6773.2011.01294.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Conrad DA, Maynard C, Cheadle A, et al. Primary care physician compensation method in medical groups: does it influence the use and cost of health services for enrollees in managed care organizations. JAMA. 1998;279(11):853-858. [DOI] [PubMed] [Google Scholar]
- 14. Rosenthal MB, Dudley RA. Pay-for-performance: will the latest payment trend improve care. JAMA. 2007;297(7):740-744. doi: 10.1001/jama.297.7.740. [DOI] [PubMed] [Google Scholar]
- 15. Berenson RA, Rich EC. US approaches to physician payment: the deconstruction of primary care. J Gen Intern Med. 2010;25(6):613-618. doi: 10.1007/s11606-010-1295-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Barnett ML, Linder JA, Clark CR, Sommers BD. Low-value medical services in the safety-net population. JAMA Intern Med. 2017;177(6):829-837. doi: 10.1001/jamainternmed.2017.0401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Barnett ML, Linder JA. Antibiotic prescribing for adults with acute bronchitis in the United States, 1996-2010. JAMA. 2014;311(19):2020-2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Barnett ML, Linder JA. Antibiotic prescribing to adults with sore throat in the United States, 1997-2010. JAMA Intern Med. 2014;174(1):138-140. doi: 10.1001/jamainternmed.2013.11673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Mehrotra A, Zaslavsky AM, Ayanian JZ. Preventive health examinations and preventive gynecological examinations in the United States. Arch Intern Med. 2007;167(17):1876-1883. doi: 10.1001/archinte.167.17.1876. [DOI] [PubMed] [Google Scholar]
- 20. Edwards ST, Mafi JN, Landon BE. Trends and quality of care in outpatient visits to generalist and specialist physicians delivering primary care in the United States, 1997–2010. J Gen Intern Med. 2014;29(6):947-955. doi: 10.1007/s11606-014-2808-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Linder JA, Ma J, Bates DW, Middleton B, Stafford RS. Electronic health record use and the quality of ambulatory care in the United States. Arch Intern Med. 2007;167(13):1400-1405. doi: 10.1001/archinte.167.13.1400. [DOI] [PubMed] [Google Scholar]
- 22. Cassel CK, Guest JA. Choosing wisely: helping physicians and patients make smart decisions about their care. JAMA. 2012;307(17):1801-1802. doi: 10.1001/jama.2012.476. [DOI] [PubMed] [Google Scholar]
- 23. Rao VM, Levin DC. The overuse of diagnostic imaging and the Choosing Wisely initiative. Ann Intern Med. 2012;157(8):574-576. doi: 10.7326/0003-4819-157-8-201210160-00535. [DOI] [PubMed] [Google Scholar]
- 24. Mafi JN, McCarthy EP, Davis RB, Landon BE. Worsening trends in the management and treatment of back pain. JAMA Intern Med. 2013;173(17):1573-1581. doi: 10.1001/jamainternmed.2013.8992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Schwartz AL, Landon BE, Elshaug AG, Chernew ME, McWilliams JM. Measuring low-value care in Medicare. JAMA Intern Med. 2014;174(7):1067-1076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Papke LE, Wooldridge J. Econometric methods for fractional response variables with an application to 401 (k) plan participation rates. J Appl Econometrics. 1996;11:619-632. [Google Scholar]
- 27. VanHerck P, DeSmedt D, Annemans L, Remmen R, Rosenthal MB, Sermeus W. Systematic review: effects, design choices, and context of pay-for-performance in health care. BMC Health Serv Res. 2010;10:247. doi: 10.1186/1472-6963-10-247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Mendelson A, Kondo K, Damberg C, et al. The effects of pay-for-performance programs on health, health care use, and processes of care: a systematic review. Ann Intern Med. 2017;166(5):341-353. doi: 10.7326/M16-1881. [DOI] [PubMed] [Google Scholar]
- 29. Friedberg MW, Chen PG, White C, et al. Effects of health care payment models on physician practice in the United States. Rand Health Q. 2015;5(1):8. [PMC free article] [PubMed] [Google Scholar]
- 30. American Academy of Family Physicians. Joint principles of the Patient-Centered Medical Home. Del Med J. 2008;80(1):21. [PubMed] [Google Scholar]
- 31. Gilchrist VJ, Stange KC, Flocke SA, McCord G, Bourguet C. A comparison of the National Ambulatory Medical Care Survey (NAMCS) measurement approach with direct observation of outpatient visits. Med Care. 2004;42(3):276-280. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, Online_appendix for The Association Between Primary Care Physician Compensation and Patterns of Care Delivery, 2012-2015 by Adrian Garcia Mosqueira, Meredith Rosenthal and Michael L. Barnett in INQUIRY: The Journal of Health Care Organization, Provision, and Financing