Abstract
Backgroud
The regenerative capacity of the liver is crucial for the host to survive after serious hepatic injuries, tumor resection, or living donor liver transplantation. Panax notoginseng saponins (PNS) have been reported to exert protective effects during organ injuries. The present study aimed to evaluate the effect of PNS on liver regeneration(LR) and on injuries induced by partial hepatectomy (PH).
Methods
We performed 70% partial PH on C57BL/6 J mice treated with or without PNS. LR was estimated by liver weight/body weight, serum alanine aminotransferase (ALT) and aspartate aminotransferase (AST) levels and cell proliferation, and the related cellular signals were analyzed by Western blot.
Results
Different concentrations of PNS promoted hepatocyte proliferation in vitro. Mice in the PNS group showed higher liver/body weight ratios at 2 d and 7 d (P < 0.05) after PH and lower levels of serum ALT and AST (P < 0.05) compared to those of mice in the normal control (NC) group. Histological analysis showed that the expression of proliferating cell nuclear antigen(PCNA) at 2 d and 7 d after PH was significantly higher in the PNS group than in the NC group (P < 0.05). Mechanistically, the AKT/mTOR cell proliferation pathway and AKT/Bad cell survival pathway were activated by PNS, which accelerated hepatocyte proliferation and inhibited apoptosis (P < 0.05).
Conclusions
PNS promoted liver regeneration through activation of PI3K/AKT/mTOR and upregulated the AKT/Bad cell pathways in mice.
Keywords: Panax notoginseng saponins, Liver regeneration, Protein kinase B, Mammalian target of rapamycin
Backgroud
The liver, which has a remarkable regenerative capability, is able to fully regenerate to its original mass, even with less than 30% of its tissue left [1]. This regenerative capacity is crucial for the host to survive after serious hepatic injuries, tumor resection, or living donor liver transplantation. Liver function recovery depends on increased energy production, which is indispensable for restoring liver mass [2]. However, the mechanisms underlying the response of the liver to acute and chronic injury and signaling pathways that are critical for regenerative capacity still require further study.
The traditional Chinese medicinal herb Panax notoginseng(Sanqi), which is known as a hemostatic medicine, has been used to accelerate blood clotting, alleviate swelling and relieve pain for more than a thousand years [3]. Panax notoginseng saponins (PNSs)contains more than 20 dammarane type saponins including ginsenoside Rg1, Rg2, Rb1, Rb2, Rb3, Rc, Rd., Re, Rh, F2 and notoginsenoside R1, R2, R3, R4, R6, Fa, Fc, Fe, etc., among which panax notoginsenoside R1, ginsenoside Rg1, Rd., Re and Rb1 are the major active components [4–6]. More than 200 compounds have been isolated from PNS, including saponins, flavonoids, cyclopeptides, sterols, polyacetylenes, volatile oil, amino acids, and polysaccharides [7]. Various PNS preparations are commercially available and widely applied in pharmaceutical forms, including capsules, injections, and powders [8]. Increasing evidences has indicated that PNS can not only prevent the aggregation of platelets to invigorate the circulation of blood but can also stimulate angiogenesis to repair injured vessels and recover the blood supply for different organs [9]. In addition, PNS prevents cardiomyocyte apoptosis and alleviates oxidative stress-induced damage [10]. PNS protects human umbilical vascular endothelium cell against oxidative damage in vitro [11]. Moreover, PNS has been used in liver diseases. PNS ameliorates liver fibrosis in vivo and vitro [12]. Zhou’s study found that PNS protected liver against hepatotoxicity induced by Triptolide [13]. The protective effect of PNS against liver injuries in mice induced by ethanol has been verified in previous study [14]. Hepatic hemodynamics changed obviously and oxidative stress were increased after partial hepatoectomy (PH) and a quick recover of blood supply and relieved oxidative stress in liver would be beneficial for liver regeneration [15]. It is reasonable to predict that PNS may have protective effects against injuries induced by PH. However, the effect of PNS on the injury induced by PH has never been studied.
The phosphatidylinositol-3-kinase (PI3K)-Protein kinase B(AKT) signaling pathway has long been confirmed as an important pathway regulating cell proliferation. Phosphorylated AKT acts on its downstream targets and participates in the regulation of the cell cycle and growth [16]. It has been reported that PNS activated the PI3K/AKT/mammalian target of rapamycin(mTOR) signaling pathway in anterior cruciate ligament fibroblasts [17]. However, whether the PI3K/AKT signaling pathway in primary hepatocytes is activated upon treatment with PNS is unknown.
The present study examined the effect of PNS on 70% liver resection of liver regeneration (LR) mouse models and studied the underlying mechanism.
Methods
Experimental animals
Male C57BL/6 mice that weighed 19–23 g and were 8–10 weeks of age were purchased from the Experimental Animal Center of Chongqing Medical University (Chongqing, China). Animals were housed in sterile polycarbonate cages with free access to water and food in a specific pathogen-free (SPF) barrier. All animal care and experimental protocols were in compliance with the Animal Management Rules of the Ministry of Health of the People’s Republic of China.
Animal surgery
PNS were purchased from Kunming Pharmaceutical Corporation(China Food and Drug Administration (CFDA) approval number: Z20026438, KPC Pharmaceuticals, Inc., Kunming, China). Seven days before PH, mice were divided into two groups that were administered saline (normal control, NC) or PNS (200 mg/kg, intraperitoneal injection) at 8:00 am everyday [18]. The treatment is maintained during the whole experiment. The same surgical procedure were performed in both NC and PNS group. Before PH, mice were subjected to adequate anesthesia by sodium pentobarbital (50 mg/kg) intraperitoneal injection while the body temperature was sustained by a heating pad at around 36 °C. Two-thirds of the liver (median and left lobes) was removed [19]. All surgeries were performed at 9:00–11:00 AM to rule out the influence of diurnal variations on regeneration. Then, the mice were divided into 3 groups (n = 6 animals per group): PH 2 d, 7 d and sham-operation (sham) groups. The same surgical procedure was performed on the sham groups without conducting PH. The mice were anaesthetized by sodium pentobarbital (50 mg/kg) intraperitoneal injection and sacrificed by cervical dislocation, and the remnant liver tissues were harvested at different time points: 2 and 7 days (s). The regenerative remnant lobe was snap-frozen in liquid nitrogen and stored at − 80 °C for further analysis.
Isolation of primary hepatocytes and cell culture
Primary hepatocytes were isolated according to a method introduced by Edwards M et al. [20]. Briefly, under adequate anesthesia, the inferior vena cava (IVC) was exposed. The IVC was infused with buffer 1 (Ca2+- and Mg2+-free Hanks balanced salt solution (HBSS)) after it was blocked just below the heart. The infusion was changed to buffer 2 (Ca2 + − and Mg2 + −containing HBSS to a final concentration of 0.08 U/mL) and the perfusion was continued for approximately 8–10 min after perfusing buffer 1 for 8 min (5 mL/min). The liver was then placed in a 100-mm cell-culture plate for further hepatocyte isolation. Finally, 1 mL (5 × 106 hepatocytes/mL) of the suspension was dispensed into each well of 12-well culture plates and incubated at 37 °C with 5% CO2 for later use. Hypoxia was simulated according to the study design by Hong et al. [21]. Hepatocytes were preincubated with 10 μM LY294002 for 1 h and were then treated with PNS (0.12 mg/ml) for 24 h. Six hours after the addition of PNS (0.12 mg/ml), the cells were subjected to hypoxia for 24 h.
Cell viability
Primary mouse hepatocytes (6 × 103 cells/well) were treated with a variety of concentrations of PNS for 24 h in 96-well plates. Cell viability was determined by a Cell Counting Kit-8 (MCE, Prod# HY-K0301) according to the company’s protocol. The absorbance at 450 nm was measured by a microplate reader (xMark™ Microplate Absorbance Spectrophotometer, BIO-RAD). Values represent the mean ± SD of at least three independent experiments [22].
Liver function
Serum was isolated from whole blood by centrifuging (5000 rpm, 20 mins) at room temperature after coagulation. An automatic biochemical meter (CX7, Beckman Coulter, USA) was used to detect serum alanine aminotransferase (ALT) and aspartate transaminase (AST) levels.
TUNEL staining
Briefly, the paraffin-embedded tissue sections were deparaffinized and dehydrated. A portion of 50 μl of TUNEL reaction mixture was added to tissue sections. Then, on each slide, 50 μl of conversion agent (POD) and 50–100 μl of substrate solution were added successively, and slides were incubated for 10 min at room temperature. Slides were then dehydrated, cleared and mounted for confocal microscopy observation. A positive signal was defined as the presence of distinct fluorescence staining within the nuclei 4′,6-diamidino-2-phenylindole (DAPI).
Immunohistochemistry staining
All tissues were fixed in 4% paraformaldehyde for 36 h immediately after surgical resection and were embedded in paraffin. The tissue sections (5 μm) were heated, dewaxed and rehydrated by immersion in dimethylbenzene and a graded ethanol series. For immunohistochemistry, an antigen-retrieval technique consisting of heating in a citrate water bath was performed before dewaxing and rehydration. Endogenous peroxidase activity was blocked by incubation with 3% hydrogen peroxide, and nonspecific binding was blocked using 5% bovine serum albumin (BSA) at room temperature. Finally, specimens were incubated overnight with antibodies against PCNA (CST, Prod# 13110S, 1:200), and the sections were stained with diaminobezidin(DAB) the next day.
Ethynyl-2′-deoxyuridine cell proliferation assays
Cell proliferation was assessed by the incorporation of 5-ethynyl-2′-deoxyuridine (Cell-Light™ EdU In Vitro Imaging Kit, Prod# C10310, RiboBio Co) into DNA according to the manufacturer’s instructions. Briefly, hepatocytes were administered with PNS as described, and EdU was added to the culture at a concentration of 100 nmol/L. According to the standard formaldehyde fixation protocol, the cells were permeabilized, fixed and incubated with the reaction cocktail for 30 min. The images of stained cells were captured by fluorescence microscopy. Values represent the mean ± SD of at least three independent experiments.
Western blotting
Total proteins were extracted from mouse liver and primary hepatocytes by RIPA Buffer (Abcam, Prod# ab156034) containing a protease inhibitor cocktail (Beyotime, Prod# P1005). A BCA Protein Assay Kit (CST, Prod#7780) was used to quantify the protein concentration in the supernatant, and lysates were then mixed and heated with Sample Loading Buffer (Beyotime, Prod# P0015A) at 100 °C for 10 min. Samples were separated by SDS-PAGE gels of different concentrations and were then transferred to a 0.2 μm PVDF membrane (ROCHE, Prod# 03010040001). The membranes were blocked with 5% nonfat milk (Bio-Rad, USA) for 60 min at room temperature and incubated overnight at 4 °C with primary antibodies against PI3K antibodies (cat. no. ab32089; 1:1000; Abcam Inc.); p-PI3K antibodies (cat. no. 4228; 1:1000; CST Inc.); AKT (cat. no. ab38449; 1:1000 dilution; Abcam Inc.); p-AKT (cat. no. ab38449; 1:1000; Abcam Inc.); mTOR (cat. no. ab2732; 1:1000; Abcam Inc.); mTOR (cat. no. ab109268; 1:1000; Abcam Inc.) GADPH (cat. no. ab8245; 1:1000 Abcam Inc.); Bad (cat. no. ab32445; 1:1000 Abcam Inc.); and p-Bad (cat. no. ab129192; 1:1000 Abcam Inc.), which was followed by incubation with horseradish peroxidase-conjugated secondary antibodies (ZSGB-BIO, Inc., China). Membranes were washed three times, incubated with HRP-conjugated secondary antibodies (ABclonal, Prod# AS003, AS014) at a dilution of 1:8000 for 60 min the next day and detected by a ChemiDoc™ system (Bio-Rad, USA) via Western-Bright ECL kit (Advansta, USA). β-actin was analyzed as a loading control.
Liver/body weight ratio
The liver/body weight ratio, also known as the liver regeneration index, was calculated by the equation: A/B, in which A stands for liver weight after regeneration, while B stands for body weight.
Annexin V-FITC/PI staining
We detected apoptosis in primary mouse hepatocytes by flow cytometry (FCM) using Annexin V-FITC/PI double staining. The cells were harvested and washed with PBS and incubated in binding buffer containing Annexin V-FITC and PI for 15 min at 37 °C in the dark. Cells were then analyzed using FCM (FACS CantoTM, BD, CA, USA). FlowJo software version 7.6.1 (Ashland, OR, USA) was used to count the number of apoptotic cells per sample.
Statistical analysis
All values are expressed as mean ± SD. Data were analyzed using an unpaired two-tailed Student’s t-test or one-way analysis of variance with a post-hoc test. SPSS 22.0 software was applied in all statistical analyses. A P value less than 0.05 was required for results to be considered statistically significant.
Results
PNS promoted primary mouse hepatocyte proliferation in a dose-dependent manner and activated the PI3K/AKT/mTOR signaling pathway in primary mouse hepatocytes
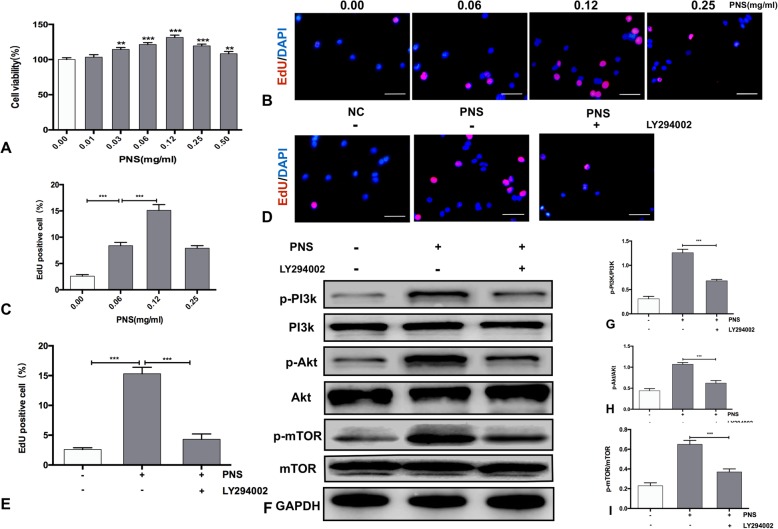
To test the effect of PNS on primary mouse hepatocytes, primary mouse hepatocytes were treated with PNS at concentrations ranging from 0.01 to 0.50 mg/ml for 24 h. PNS gradually increased primary mouse hepatocyte proliferation in a dose-dependent manner, peaking at 0.12 mg/ml. Then, the proliferative effect of PNS decreased with increasing PNS concentrations above 0.12 mg/ml (P < 0.05) (Fig. 1A). These results were similar to that of the EdU assay, in which the proliferative effect of PNS peaked at the 0.12 mg/ml treatment with 15.3% EdU-positive hepatocytes (Fig. 1B-C).
Fig. 1.
PNS promoted primary mouse hepatocyte proliferation via the PI3K/AKT/mTOR signaling pathway. The primary mouse hepatocytes were treated with a range of concentrations of PNS for 24 h. Cells were preincubated with or without 10 μM LY294002 for 1 h and were then treated with 0.12 mg/ml PNS for 24 h. (a) The cell viability was determined by CCK-8 Kits. (b) Primary mouse hepatocytes were pretreated with 0.00, 0.06, 0.12 and 0.25 mg/ml PNS for 24 h and EdU (pink) staining was measured (magnification: × 400, Scale bars represent 50 μm). (c) Quantification of EdU-positive cells. (d) Representative immunofluorescent images of primary mouse hepatocyte proliferation measured by EdU staining (magnification: × 400, Scale bars represent 50 μm). (e) Quantification of EdU-positive cells. (f) Total and phosphorylated protein levels of PI3K, AKT and mTOR in primary mouse hepatocytes. Values represent the mean ± SEM of 3 independent experiments. (g)(h)(i) Bar graph shows the quantification of total and phosphorylated protein levels of PI3K, AKT and mTOR. Values represent the mean ± SD of at least three independent experiments. **P < 0.01, *** P < 0.001
To examine whether PNS could activate AKT/mTOR in primary mouse hepatocytes, we added the PI3K/AKT inhibitor LY294002 to PNS-treated hepatocytes. The EdU staining showed that the proliferative effect of PNS was inhibited by LY294002 (P < 0.05) (Fig. 1D-E). The phosphorylated and total protein levels of PI3K, AKT, and mTOR were examined in hepatocytes treated with 0.12 mg/ml PNS with or without LY294002 by Western blotting. The results showed that PNS increased the phosphorylation of PI3K, AKT, and mTOR in primary mouse hepatocytes, and this effect was blocked by LY294002 (P < 0.05) (Fig. 1F-I).
PNS promoted liver regeneration and activated the PI3K/AKT/mTOR signaling pathway in vivo
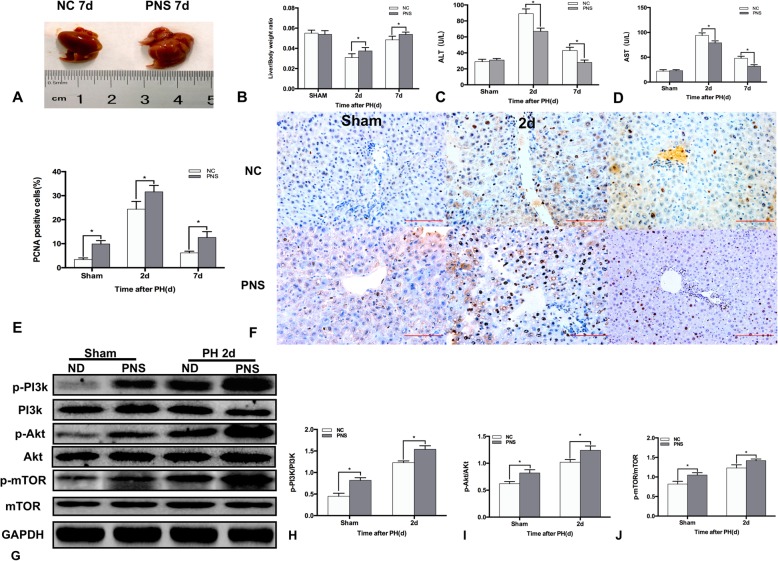
We determined whether PNS caused a proliferative effect in hepatocytes in vivo. The regenerated liver was larger 7 d after PH with PNS treatment (Fig. 2A). The liver/body weight ratios were higher at both 2 d and 7 d after PH with PNS treatment (P < 0.05) (Fig. 2B). The ALT and AST levels in serum are widely used biochemical markers for hepatic function. The serum ALT and AST levels were lower at both 2 d and 7 d after PH with PNS treatment (P < 0.05) (Fig. 2C-D). The PCNA staining showed that the proliferation of hepatocytes in vivo was higher in PNS group with or without PH (P < 0.05) (Fig. 2E-F). Western blotting showed that the phosphorylated protein levels of PI3K, AKT, and mTOR were higher in mice with PNS treatment than those of NC mice (P < 0.05) (Fig. 2G-J).
Fig. 2.
PNS activated the PI3K/AKT/mTOR signaling pathway during LR in vivo. C57BL/6 J mice were administered PNS 7 days before PH. (a) The regenerated liver in mice treated with or without PNS 7 days after PH. (b) Quantification of the relative ratio of liver weight/body weight in mice treated with or without PNS at 2 d and 7 d after PH. Serum concentrations of ALT (c) and AST (d) at 2 d and 7 d after PH. (e) Quantification of PCNA-positive cells in mice treated with or without PNS at 2 d and 7 d after PH. (f) Representative liver sections stained with PCNA in mice treated with or without PNS at 2 d and 7 d after PH (original magnification: × 200, scale bars represent 100 μm). (g) Total and phosphorylated protein levels of PI3k, AKT and mTOR in mice treated with or without PNS at 2 d after PH. (H)(I)(J) Bar graph shows the quantification of the total and phosphorylated protein levels of PI3k, AKT and mTOR. Values represent the mean ± SD of at least three independent experiments. * P<0.05
PNS inhibited hepatocellular apoptosis during LR in mice through AKT/bad signaling
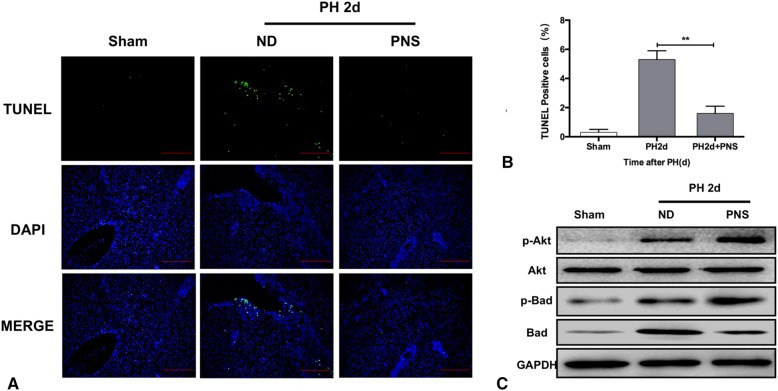
We determined whether PNS had an extra protective effect during LR. The TUNEL staining showed that cellular apoptosis was inhibited in mice with PNS treatment (P < 0.05) (Fig. 3A-B). The phosphorylated protein levels of AKT and Bad increased in PNS group (P < 0.05) (Fig. 3C).
Fig. 3.
PNS inhibited cellular apoptosis during LR in vivo via the AKT/Bad pathway. (a) Representative liver sections stained by TUNEL in mice treated with or without PNS at 2 d after PH. (b) Quantification of TUNEL-positive cells in mice treated with or without PNS at 2 d after PH. (c) Total and phosphorylated protein levels of AKT and Bad in mice treated with or without PNS at 2 d after PH. Values represent the mean ± SD of at least three independent experiments; ** P<0.01
PNS alleviated hypoxia-induced hepatocellular apoptosis through AKT/bad signaling in vitro
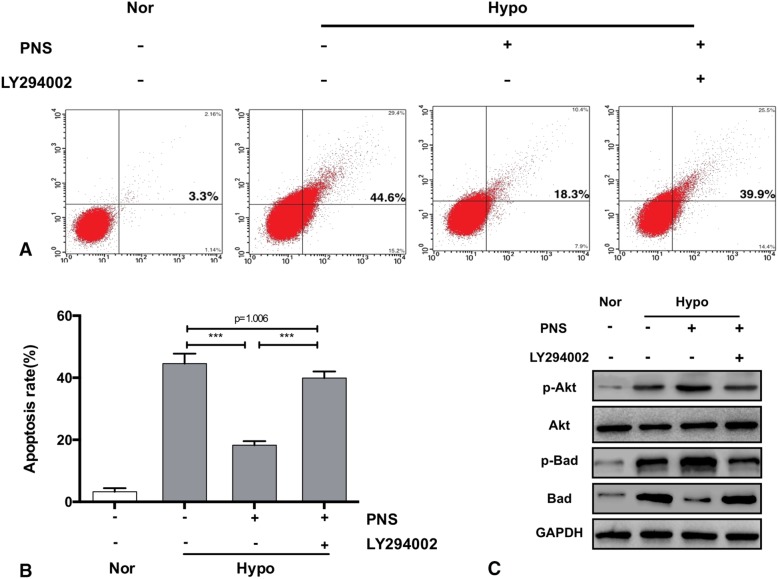
Annexin V/PI staining showed that the hypoxia-induced apoptosis rate decreased in primary hepatocytes treated with PNS comparing to that of hepatocytes without PNS treatment. However, LY294002 blocked the inhibitory effect of PNS on apoptosis induced by hypoxia in hepatocytes (Fig. 4A-C). These results indicated that the protective effect of PNS on hepatocytes involved the activation of PI3K/AKT/Bad pathways.
Fig. 4.
PNS inhibited hypoxia-induced cellular apoptosis via the AKT/Bad pathway in vitro. Primary mouse hepatocytes were preincubated with or without 10 μM LY294002 for 1 h and were then treated with 0.12 mg/ml PNS for 6 h before being subjected to hypoxia for 24 h. (a) The effect of a PI3K inhibitor on the protective activity of PNS against hypoxia-induced apoptosis in primary mouse hepatocytes was determined using Annexin V/PI staining by flow cytometry. (b) Quantification of (a). (c) Total and phosphorylated protein levels of AKT and Bad in primary mouse hepatocytes. Values represent the mean ± SD of at least three independent experiments; *** P<0.001
Discussion
PNS is a species of the genus Panax and have extensive pharmacological activities in the treatment of various diseases, such as cardiovascular, nervous and anticancer, anti-atherosclerotic and other biological activities [23]. PNS are active components with different dammarane-type saponins [5]. Notoginsenoside R1 is a unique component in PNS, which contributed to the amelioration of myocardial cells apoptosis and myocardial ischemia/reperfusion injury via inhibiting the activation of TAK1/NF-κB pathways [24]. Additionally, Notoginsenoside R1 exerts protective effects through the enhancement of beta-amyloid protein degradation and maybe is a potential candidate for AD treatment [25]. For the effective treatment of cerebrovascular diseases and improves the cognitive and sensorimotor deficits, Ginsenoside Rb1 as also a major active component in PNS has the function on the modulation of the AKT/mTOR signaling pathway and down-regulation of caspase-3 in rats subjected to phototrombic stroke [26]. It was indicated that the ginsenoside Rh4 could trigger apoptosis by activating the ROS/JNK/p53 pathway in colorectal cancer cells [27]. In general, these components of PNS have various biological effects, such as antioxidant, anti-inflammatory, antiaging, neuroprotective, and anti-apoptosis and this prompted us to investigate the overall effects of PNS on LR and explore related molecular mechanisms. In the current study, we demonstrated that administration of PNS can promote LR and improve liver function after PH in mice through PI3K/AKT/mTOR pathway, thus such protective mechanism might mainly be induced by Ginsenoside Rb1. In our study, the results demonstrated that PNS at concentrations varying from 0.03 to 0.5 mg/ml promoted cell proliferation, which peaked at a concentration of 0.12 mg/ml in primary mouse hepatocytes; thus, we chose this concentration (0.12 mg/ml) for further study.
During LR, organisms developed complex protective mechanisms to survive in a challenging environment. Stress response proteins and pathways were involved in these mechanisms, including membrane transporters, protein chaperones, antioxidant enzymes, growth factors, and signaling pathways and transcriptional factors [28]. PI3K/AKT has long been considered a major pathway that promotes cell proliferation and prevents cellular apoptosis [29]. AKT phosphorylation initiates the expression of proteins involved in regulating proliferation and apoptosis in cells [30]. Cell apoptosis and survival, protein synthesis, and autophagy were regulated by phosphorylated mTOR, which was initiated by AKT [31]. In A KT knockout mice, LR was severely impaired and mortality increased due to the impairment of the proliferative capacity of hepatocytes [32, 33]. In our study, the results showed that PNS at a concentration of 0.12 mg/ml significantly increased the expression level of phosphorylated PI3K, AKT and mTOR. Administration of LY294002 blocked the proliferative effect of PNS and the PI3K/AKT/mTOR pathway, suggesting that PNS promoted cell proliferation in primary hepatocytes through the PI3K/AKT/mTOR pathway. In vivo, the results showed that PNS promoted LR. The regenerated remnant was larger than that of the NC group at 7 days after PH. The circulating levels of ALT and AST decreased with PNS treatment, indicating that PNS ameliorated liver injury induced by PH [34]. PCNA staining showed that PNS administration promoted cellular proliferation in regenerated liver. In our study, the phosphorylated levels of PI3K, AKT and mTOR increased at 2 days after PH, which is in accordance with a previous study [35], and the PI3K/AKT/mTOR pathway was elevated with administration of PNS.
TUNEL staining showed that apoptosis of hepatocytes increased at 2 days after PH, which is consistent with a previous study [36]. PNS significantly relieved cellular apoptosis after PH. Bad has been confirmed to be a downstream target of AKT in preventing cellular apoptosis [37]. Bad, which is a member of the Bcl-2 family, is able to combine with antiapoptotic Bcl-2 or Bcl-xL to form a complex that promotes apoptosis [38]. Previous studies have suggested that phosphorylation of Bad by AKT resulted in cell survival [39]. In our study, the results showed that p-Bad increased while Bad decreased after PNS administration. In vitro, we cultured primary hepatocytes in a hypoxic incubator to simulate the hypoxic state that hepatocytes undergo during LR. A previous study showed that AKT/Bad was activated during hypoxia [40]. Our results showed that PNS ameliorated the cellular apoptosis induced by hypoxia, and the AKT/Bad pathway was activated. However, these effects of PNS could be abolished by treatment with LY294002. In summary, the antiapoptotic effects of PNS during hypoxia were related to the activation of the AKT/Bad cell survival pathway.
Conclusions
The present study verified that PNS promoted hepatocyte proliferation during LR and protected hepatocytes against PH-induced apoptosis through the initiation of the PI3K/AKT/mTOR pathway and the PI3K/AKT/Bad pathway (as summarized in Fig. 5). The main findings of this study provided direct experimental evidence that PNS treatment could be a new approach to promote the regenerative capacity of the liver and accelerate the recovery of liver function in patients who have suffered from hepatic injuries caused by major hepatectomy.
Fig. 5.
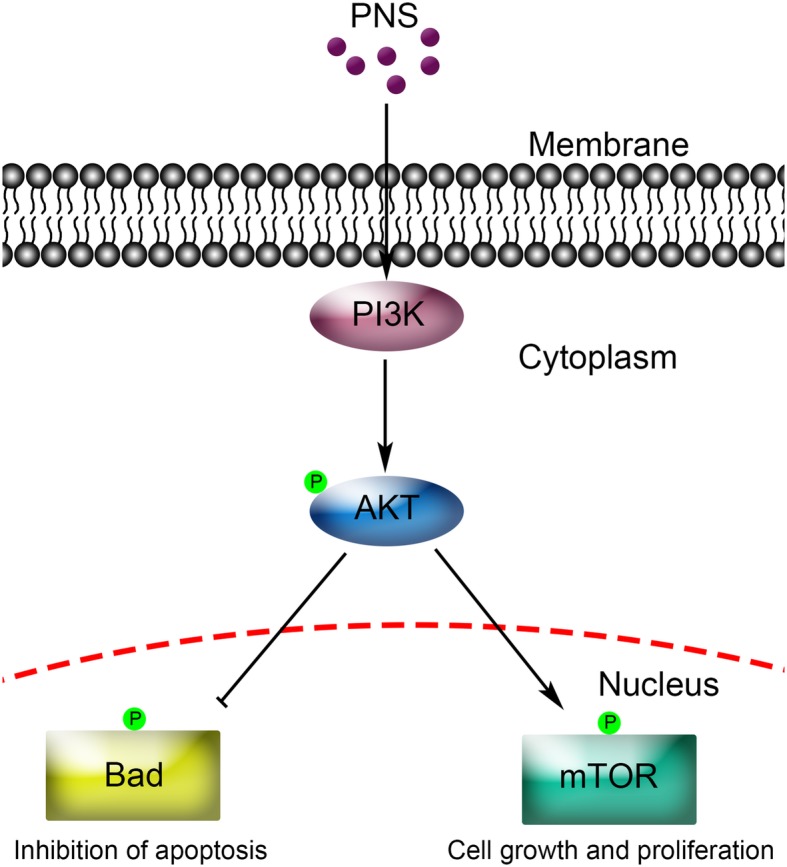
A schematic model of upregulated PI3K/AKT/ mTOR cell proliferation pathway and upregulated AKT/Bad cell survival pathway by PNS in primary mouse hepatocytes
Acknowledgements
Not applicable.
Abbreviations
- AKT
Protein kinase B
- ALT
Anine aminotransferase
- AST
Aspartate transaminase
- BSA
Bovine serum albumin
- DAB
diaminobezidin 3
- DAPI
4′,6-diamidino-2-phenylindole
- EdU
5-ethynyl-2′-deoxyuridine
- HBSS
Hanks balanced salt solution
- IVC
Inferior vena cava
- LR
Liver regeneration
- mTOR
Mammalian target of rapamycin
- NC
Normal control
- PCNA
Proliferating cell nuclear antigen
- PH
Partial hepatectomy
- PI3K
Phosphatidylinositol-3-kinase
- PNS
Panax notoginseng saponins
- SPF
Specific pathogen free
Authors’ contributions
YFC and WH designed the study and supervised the project; ZH and BH carried out most of the experimental work; WMH conducted the molecular cloning experiments; WJ conducted part of the animal experiments; MMY analyzed the data; ZH, BH and GJP wrote the manuscript; YFC and WH approved the final version of manuscript. All authors read and approved the final manuscript.
Funding
This study was supported by grants from the National Natural Science Foundation of China (NSFC: No.81670599; awarded to GJP and No. 81570569; awarded to MMY) administered by the the National Natural Science Fund Committee. Both funds facilitate the design of the study and collection of data.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
Ethical reviews of animal experiment were approved by the ethics committee of the Second Affiliated Hospital of Chongqing Medical university and all animals’ care and experimental protocols were in line with the Animal Management Rules of the Ministry of Health of the People’s Republic of China.
Consent for publication
Not applicable.
Competing interests
All of the authors declare that there are no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Hua Zhong, Hao Wu and He Bai contributed equally to this work.
References
- 1.Mukherjee S, Chellappa K, Moffitt A, Ndungu J, Dellinger RW, Davis JG, Agarwal B, Baur JA. Nicotinamide adenine dinucleotide biosynthesis promotes liver regeneration. Hepatology. 2017;65(2):616–630. doi: 10.1002/hep.28912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Michalopoulos GK. Liver regeneration. J Cell Physiol. 2007;213(2):286–300. doi: 10.1002/jcp.21172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lee MR, Yun BS, Sung CK. Comparative study of white and steamed black Panax ginseng, P. quinquefolium, and P. notoginseng on cholinesterase inhibitory and Antioxidative activity. J Ginseng Res. 2012;36(1):93–101. doi: 10.5142/jgr.2012.36.1.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gu CZ, Lv JJ, Zhang XX, Qiao YJ, Yan H, Li Y, Wang D, Zhu HT, Luo HR, Yang CR, et al. Triterpenoids with promoting effects on the differentiation of PC12 cells from the steamed roots of Panax notoginseng. J Nat Prod. 2015;78(8):1829–1840. doi: 10.1021/acs.jnatprod.5b00027. [DOI] [PubMed] [Google Scholar]
- 5.Wang N, Wang L, Qi L, Lu X. Construct a gene-to-metabolite network to screen the key genes of triterpene saponin biosynthetic pathway in Panax notoginseng. Biotechnol Appl Biochem. 2018;65(2):119–127. doi: 10.1002/bab.1580. [DOI] [PubMed] [Google Scholar]
- 6.Li X, Wang G, Sun J, Hao H, Xiong Y, Yan B, Zheng Y, Sheng L. Pharmacokinetic and absolute bioavailability study of total panax notoginsenoside, a typical multiple constituent traditional chinese medicine (TCM) in rats. Biol Pharm Bull. 2007;30(5):847–851. doi: 10.1248/bpb.30.847. [DOI] [PubMed] [Google Scholar]
- 7.Xu C, Weiwei W, Wang B, Zhang T, Cui X, Pu Y, Li N. Analytical methods and biological activities of Panax notoginseng saponins: recent trends. J Ethnopharmacol. 2019. [DOI] [PubMed]
- 8.Gui Q, Yang Y, Ying S, Zhang M. Xueshuantong improves cerebral blood perfusion in elderly patients with lacunar infarction. Neural Regen Res. 2013;8(9):792–801. doi: 10.3969/j.issn.1673-5374.2013.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shen K, Ji L, Gong C, Ma Y, Yang L, Fan Y, Hou M, Wang Z. Notoginsenoside Ft1 promotes angiogenesis via HIF-1alpha mediated VEGF secretion and the regulation of PI3K/AKT and Raf/MEK/ERK signaling pathways. Biochem Pharmacol. 2012;84(6):784–792. doi: 10.1016/j.bcp.2012.05.024. [DOI] [PubMed] [Google Scholar]
- 10.Zhang EY, Gao B, Shi HL, Huang LF, Yang L, Wu XJ, Wang ZT. 20(S)-Protopanaxadiol enhances angiogenesis via HIF-1alpha-mediated VEGF secretion by activating p70S6 kinase and benefits wound healing in genetically diabetic mice. Exp Mol Med. 2017;49(10):e387. doi: 10.1038/emm.2017.151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chen SC, Cheng JJ, Hsieh MH, Chu YL, Kao PF, Cheng TH, Chan P. Molecular mechanism of the inhibitory effect of trilinolein on endothelin-1-induced hypertrophy of cultured neonatal rat cardiomyocytes. Planta Med. 2005;71(6):525–529. doi: 10.1055/s-2005-864153. [DOI] [PubMed] [Google Scholar]
- 12.Hui J, Gao J, Wang Y, Zhang J, Han Y, Wei L, Liu X, Wu J. Panax notoginseng saponins ameliorates experimental hepatic fibrosis and hepatic stellate cell proliferation by inhibiting the Jak2/ Stat3 pathways. J Tradit Chin Med. 2016;36(2):217–224. doi: 10.1016/S0254-6272(16)30030-9. [DOI] [PubMed] [Google Scholar]
- 13.Zhou L, Zhou C, Feng Z, Liu Z, Zhu H, Zhou X. Triptolide-induced hepatotoxicity can be alleviated when combined with Panax notoginseng saponins and Catapol. J Ethnopharmacol. 2018;214:232–239. doi: 10.1016/j.jep.2017.12.033. [DOI] [PubMed] [Google Scholar]
- 14.Ding RB, Tian K, Cao YW, Bao JL, Wang M, He C, Hu Y, Su H, Wan JB. Protective effect of panax notoginseng saponins on acute ethanol-induced liver injury is associated with ameliorating hepatic lipid accumulation and reducing ethanol-mediated oxidative stress. J Agric Food Chem. 2015;63(9):2413–2422. doi: 10.1021/jf502990n. [DOI] [PubMed] [Google Scholar]
- 15.Audebert C, Bekheit M, Bucur P, Vibert E, Vignon-Clementel IE. Partial hepatectomy hemodynamics changes: experimental data explained by closed-loop lumped modeling. J Biomech. 2017;50:202–208. doi: 10.1016/j.jbiomech.2016.11.037. [DOI] [PubMed] [Google Scholar]
- 16.Choi SC, Kim SJ, Choi JH, Park CY, Shim WJ, Lim DS. Fibroblast growth factor-2 and -4 promote the proliferation of bone marrow mesenchymal stem cells by the activation of the PI3K-AKT and ERK1/2 signaling pathways. Stem Cells Dev. 2008;17(4):725–736. doi: 10.1089/scd.2007.0230. [DOI] [PubMed] [Google Scholar]
- 17.Yu L, Xie J, Xin N, Wang Z. Panax notoginseng saponins promote wound repair of anterior cruciate ligament through phosphorylation of PI3K, AKT and ERK. Int J Clin Exp Pathol. 2015;8(1):441–449. [PMC free article] [PubMed] [Google Scholar]
- 18.Yang CY, Wang J, Zhao Y, Shen L, Jiang X, Xie ZG, Liang N, Zhang L, Chen ZH. Anti-diabetic effects of Panax notoginseng saponins and its major anti-hyperglycemic components. J Ethnopharmacol. 2010;130(2):231–236. doi: 10.1016/j.jep.2010.04.039. [DOI] [PubMed] [Google Scholar]
- 19.Mitchell C, Willenbring H. A reproducible and well-tolerated method for 2/3 partial hepatectomy in mice. Nat Protoc. 2008;3(7):1167–1170. doi: 10.1038/nprot.2008.80. [DOI] [PubMed] [Google Scholar]
- 20.Edwards M, Houseman L, Phillips IR, Shephard EA. Isolation of mouse hepatocytes. Methods Mol Biol. 2013;987:283–293. doi: 10.1007/978-1-62703-321-3_24. [DOI] [PubMed] [Google Scholar]
- 21.Hong S, Lee JE, Kim CY, Seong GJ. Agmatine protects retinal ganglion cells from hypoxia-induced apoptosis in transformed rat retinal ganglion cell line. BMC Neurosci. 2007;8:81. doi: 10.1186/1471-2202-8-81. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 22.Mosmann T. Rapid colorimetric assay for cellular growth and survival: application to proliferation and cytotoxicity assays. J Immunol Methods. 1983;65(1–2):55–63. doi: 10.1016/0022-1759(83)90303-4. [DOI] [PubMed] [Google Scholar]
- 23.Zhang M, Guan Y, Xu J, Qin J, Li C, Ma X, Zhang Z, Zhang B, Tang J. Evaluating the protective mechanism of panax notoginseng saponins against oxidative stress damage by quantifying the biomechanical properties of single cell. Anal Chim Acta. 2019;1048:186–193. doi: 10.1016/j.aca.2018.10.030. [DOI] [PubMed] [Google Scholar]
- 24.Ge ZR, Xu MC, Huang YU, Zhang CJ, Lin JE, Ruan CW. Cardioprotective effect of notoginsenoside R1 in a rabbit lung remote ischemic postconditioning model via activation of the TGF-beta1/TAK1 signaling pathway. Exp Ther Med. 2016;11(6):2341–2348. doi: 10.3892/etm.2016.3222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Li Z, Li H, Zhao C, Lv C, Zhong C, Xin W, Zhang W. Protective effect of Notoginsenoside R1 on an APP/PS1 mouse model of Alzheimer's disease by up-regulating insulin degrading enzyme and inhibiting Abeta accumulation. CNS Neurol Disord Drug Targets. 2015;14(3):360–369. doi: 10.2174/1871527314666150225141521. [DOI] [PubMed] [Google Scholar]
- 26.Yan YT, Li SD, Li C, Xiong YX, Lu XH, Zhou XF, Yang LQ, Pu LJ, Luo HY. Panax notoginsenoside saponins Rb1 regulates the expressions of AKT/ mTOR/PTEN signals in the hippocampus after focal cerebral ischemia in rats. Behav Brain Res. 2018;345:83–92. doi: 10.1016/j.bbr.2018.02.037. [DOI] [PubMed] [Google Scholar]
- 27.Wu Q, Deng J, Fan D, Duan Z, Zhu C, Fu R, Wang S. Ginsenoside Rh4 induces apoptosis and autophagic cell death through activation of the ROS/JNK/p53 pathway in colorectal cancer cells. Biochem Pharmacol. 2018;148:64–74. doi: 10.1016/j.bcp.2017.12.004. [DOI] [PubMed] [Google Scholar]
- 28.Arumugam TV, Gleichmann M, Tang SC, Mattson MP. Hormesis/preconditioning mechanisms, the nervous system and aging. Ageing Res Rev. 2006;5(2):165–178. doi: 10.1016/j.arr.2006.03.003. [DOI] [PubMed] [Google Scholar]
- 29.Brunet A, Datta SR, Greenberg ME. Transcription-dependent and -independent control of neuronal survival by the PI3K-AKT signaling pathway. Curr Opin Neurobiol. 2001;11(3):297–305. doi: 10.1016/S0959-4388(00)00211-7. [DOI] [PubMed] [Google Scholar]
- 30.Ming M, Feng L, Shea CR, Soltani K, Zhao B, Han W, Smart RC, Trempus CS, He YY. PTEN positively regulates UVB-induced DNA damage repair. Cancer Res. 2011;71(15):5287–5295. doi: 10.1158/0008-5472.CAN-10-4614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nguyen-Tu MS, da Silva Xavier G, Leclerc I, Rutter GA. Transcription factor-7-like 2 (TCF7L2) gene acts downstream of the Lkb1/Stk11 kinase to control mTOR signaling, beta cell growth, and insulin secretion. J Biol Chem. 2018;293(36):14178–14189. doi: 10.1074/jbc.RA118.003613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lee MY, Luciano AK, Ackah E, Rodriguez-Vita J, Bancroft TA, Eichmann A, Simons M, Kyriakides TR, Morales-Ruiz M, Sessa WC. Endothelial AKT1 mediates angiogenesis by phosphorylating multiple angiogenic substrates. Proc Natl Acad Sci U S A. 2014;111(35):12865–12870. doi: 10.1073/pnas.1408472111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Moris D, Vernadakis S, Papalampros A, Vailas M, Dimitrokallis N, Petrou A, Dimitroulis D. Mechanistic insights of rapid liver regeneration after associating liver partition and portal vein ligation for stage hepatectomy. World J Gastroenterol. 2016;22(33):7613–7624. doi: 10.3748/wjg.v22.i33.7613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fan JS, Liu DN, Huang G, Xu ZZ, Jia Y, Zhang HG, Li XH, He FT. Panax notoginseng saponins attenuate atherosclerosis via reciprocal regulation of lipid metabolism and inflammation by inducing liver X receptor alpha expression. J Ethnopharmacol. 2012;142(3):732–738. doi: 10.1016/j.jep.2012.05.053. [DOI] [PubMed] [Google Scholar]
- 35.Araujo TG, de Oliveira AG, Tobar N, Saad MJ, Moreira LR, Reis ER, Nicola EM, de Jorge GL, dos Tartaro RR, Boin IF, et al. Liver regeneration following partial hepatectomy is improved by enhancing the HGF/met axis and AKT and Erk pathways after low-power laser irradiation in rats. Lasers Med Sci. 2013;28(6):1511–1517. doi: 10.1007/s10103-013-1264-y. [DOI] [PubMed] [Google Scholar]
- 36.Borowiak M, Garratt AN, Wustefeld T, Strehle M, Trautwein C, Birchmeier C. Met provides essential signals for liver regeneration. Proc Natl Acad Sci U S A. 2004;101(29):10608–10613. doi: 10.1073/pnas.0403412101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Datta SR, Dudek H, Tao X, Masters S, Fu H, Gotoh Y, Greenberg ME. AKT phosphorylation of BAD couples survival signals to the cell-intrinsic death machinery. Cell. 1997;91(2):231–241. doi: 10.1016/S0092-8674(00)80405-5. [DOI] [PubMed] [Google Scholar]
- 38.Zhang H, Xiong Z, Wang J, Zhang S, Lei L, Yang L, Zhang Z. Glucagon-like peptide-1 protects cardiomyocytes from advanced oxidation protein product-induced apoptosis via the PI3K/AKT/bad signaling pathway. Mol Med Rep. 2016;13(2):1593–1601. doi: 10.3892/mmr.2015.4724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tang B, Tang F, Wang Z, Qi G, Liang X, Li B, Yuan S, Liu J, Yu S, He S. Upregulation of AKT/NF-kappaB-regulated inflammation and AKT/bad-related apoptosis signaling pathway involved in hepatic carcinoma process: suppression by carnosic acid nanoparticle. Int J Nanomedicine. 2016;11:6401–6420. doi: 10.2147/IJN.S101285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Yang X, Wei A, Liu Y, He G, Zhou Z, Yu Z. IGF-1 protects retinal ganglion cells from hypoxia-induced apoptosis by activating the Erk-1/2 and AKT pathways. Mol Vis. 2013;19:1901–1912. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.