Abstract
Objective:
We assessed whether provider sitting influenced patient satisfaction in an academic emergency department (ED) and if education and/or environmental manipulation could nudge providers to sit.
Methods:
This was a prospective, controlled pre–post trial of provider sitting and its influence on patient satisfaction within 2 urban, academic EDs. A 12-item survey was administered to a convenience sample of patients to assess for care satisfaction before, during, and after study interventions. Study interventions included (a) placement of branded folding seats and (b) an educational campaign. Only the intervention ED received folding seats. The primary outcome examined the influence of provider sitting on patient satisfaction. A secondary outcome examined the frequency of provider sitting.
Results:
During the entire study period, 2827 patients were surveyed; 63% were female and 65% were between the ages of 26 and 65. Sitting at any point during an ED encounter improved responses to satisfaction questions (polite [67% vs 59%], cared [64% vs 54%], listened [60% vs 52%], informed [57% vs 47%], time [56% vs 45%], P < .0001 for all measures). The odds of provider sitting increased 30% when a seat was placed in the room (odds ratio [OR] = 1.3, 95% confidence interval [CI]: 1.1-1.5). No change in provider sitting was observed in the control ED (OR = 1.0, 95% CI: 0.8-1.2).
Conclusions:
Placing a seat in a patient’s room nudges providers to sit during an ED encounter. Education alone did not influence provider behavior. Sitting down resulted in significantly higher patient satisfaction scores during an ED visit.
Keywords: clinician-patient relationship, communication, emergency medicine, patient satisfaction, quality improvement
Introduction
The physician–patient relationship is fundamentally built upon verbal and nonverbal communication and is an important component for any medical encounter (1,2). Effective communication can be challenging during the provider–patient interaction, particularly in an emergency department (ED) setting (3 –5). Patient dissatisfaction with ED encounters is frequently related to poor communication (2).
Nonverbal cues such as provider posture (sitting versus standing) during ambulatory and inpatient encounters increases the patient’s perceived length of time spent by the physician which may improve provider–patient communication and ultimately patient satisfaction (6 –9).
Additionally, physician communication positively correlates with patient adherence to treatment recommendations and affects patient experience with overall hospital care (10,11). Patient experience is currently assessed using consumer-based satisfaction surveys and is a quality measure for the Value Based Reimbursement Program through the Center for Medicare and Medicaid Services (CMS) (12).
The effect of provider posture during an ED encounter has not been well studied. The primary objective of this study was to characterize the association between provider posture (sitting versus standing) and patient satisfaction. A secondary objective was to test whether education and/or environmental manipulation through placement of colorful, institution-branded folding seats changes provider behavior. We hypothesized that by altering the environment in which health-care professionals practice, we could change provider behavior, facilitate better communication, and positively influence patient satisfaction.
Methods
This was a prospective, controlled, pre–post trial within 2 urban, academic EDs within a single health system. The project was reviewed and approved as a quality improvement study by the University’s institutional review board. Patients were approached by trained research assistant (RAs) for verbal consent if they were 18 years or older, had a Glasgow Coma Score of 15, and were being discharged from the ED to home. Patients were excluded if they had dementia, acute psychosis, or clinical intoxication.
The intervention ED site was a large tertiary care ED with approximately 62 000 annual adult visits, and the control ED was a level-1 trauma center with 47 000 annual visits. Most emergency medicine attending physicians and all emergency medicine residents practice at both sites.
Intervention
Study interventions included (a) placement of institution-branded folding seats and (b) an educational campaign to highlight the importance of good communication. White folding seats were branded with a colorful institution logo and project slogan, “Grab a Seat,” and hung on hooks within eyesight in each patient room (Figure 1). The educational campaign included production of a 4-minute video (https://vimeo.com/162120595) that was disseminated to house staff, attending physicians, nurses, and advanced practice providers (APPs) through e-mail and in-person presentation by a study member. In order to study the benefit of a visual cue (the branded folding seats) on health-care workers, we exposed both EDs to the educational video whereas only the intervention ED received the folding seats.
Figure 1.

A photo of the folding seat used in this study. Chairs were hung on the wall within eye sight of the provider. Stools were labeled with the project logo.
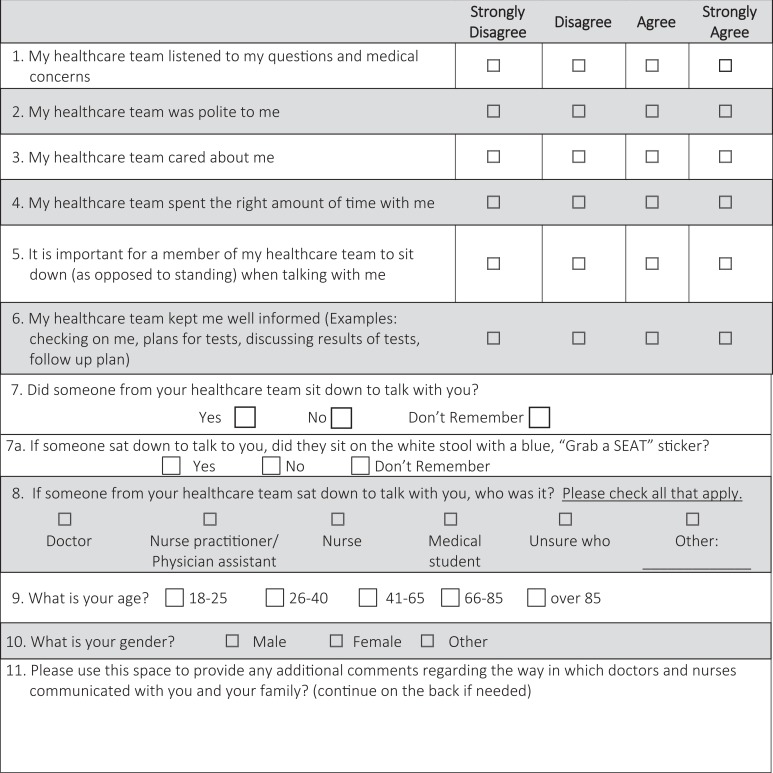
Patients marked for discharge to home from the ED were eligible for enrollment. A convenience sample was obtained by trained RAs who enrolled patients between 7 am and 12 am, 7 days a week during the 10-month study period. The RAs administered a 12-item survey instrument that was designed by the authors and members of our hospital’s Patient and Family Advisory Council after review of prior patient satisfaction-based tools and approved by our hospital’s patient experience team to ensure compliance with CMS regulations (8,13). Patients were surveyed on a 4-point Likert scale (strongly disagree, disagree, agree, and strongly agree) assessing the patient’s perception of how well providers kept them informed, spent enough time with them, and whether they felt the provider listened, cared, was polite, and important for the provider to sit down. The survey also assessed if any health-care member sat down with the patient and, if so, who (doctor, APP, nurse, medical student, unsure, other; Appendix A). Providers in both EDs were blinded to data collection.
The survey was pilot tested and administered to patients at both EDs for 3 months prior to intervention to obtain baseline satisfaction scores and provider sitting behavior. The survey was then withheld as both interventions were introduced over a 4-week period followed by another 4-week washout period for providers to acclimate to the new seats in the clinical environment. During the 3-month intervention period, the survey included an additional question at the intervention ED for patients to report whether the provider used the folding seat to sit. The folding seats were then removed from the intervention ED and patients at both study sites were surveyed for an additional 3 months postintervention.
Measures
For the primary objective, the influence of provider posture on patient satisfaction was captured by calculating the frequency at which patients “strongly agreed” to each of the satisfaction questions. This method of analysis is used in similar studies and consumer-based health-care surveys (8,11,12). The secondary objective was to determine whether either intervention (education alone or education and environmental manipulation), as measured by patient response to whether a provider sat down, increased provider sitting.
Statistical Analysis
Survey questions and patient demographics were summarized using frequencies and percentages for categorical variables and means with standard deviations for continuous variables. To determine the differences in patient satisfaction when a provider sat down, answers to survey questions were dichotomized based on response. Since more than half of patients strongly agreed to all survey questions, we compared “strongly agree” to the other 3 categories. χ2 test was used to compare differences in patient satisfaction when a provider sat down versus did not sit regardless of period. Additionally, an overall satisfaction score (range 5-20) was developed combining 5 of the questions (provider was polite, cared, listened, kept well informed, and spent enough time) to examine overall satisfaction rather than the individual components. To determine the differences in satisfaction score over time, separate 2-way analyses of variance were performed by hospital with the 2 factors being study: period and sitting behavior. To determine the differences in sitting, pre-, during, and postintervention, logistic regression adjusting for patient satisfaction score and hospital was employed. All analyses were performed using SAS statistical software (Version 9.4, SAS Institute, Cary, North Carolina).
Results
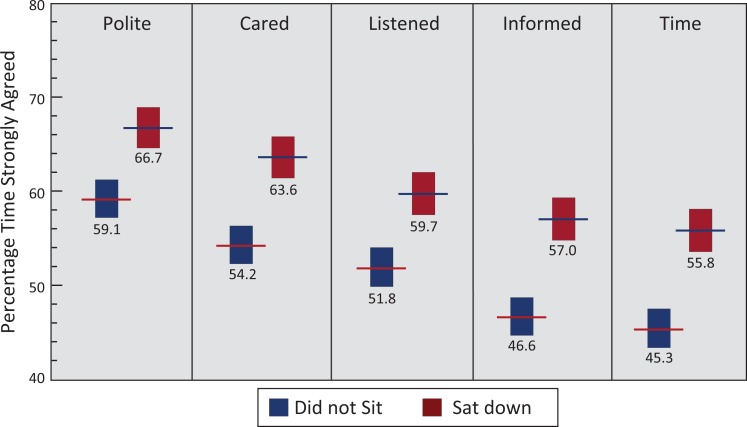
During the entire study period, 2827 patients were surveyed at both study sites; 65% at the intervention ED and 45% at the control. Similar numbers of surveys were obtained during each study phase: preintervention (1087), intervention (874), postintervention (866). Between both sites, 63% were female and 65% were between the ages of 26 and 65 (Table 1). Compared to the control ED, survey respondents at the intervention ED were significantly more likely to be female (66% vs 58%; P < .0001) and were more likely to be younger (age 18-40; 61% vs 43%; P < .0001). Incomplete surveys (n = 86) were discarded, leaving 2741 responses for final analysis. Regardless of hospital site, provider sitting at any point during an ED encounter as opposed to standing improved responses to satisfaction questions (polite [67% vs 59%], cared [64% vs 54%], listened [60% vs 52%], informed [57% vs 47%], time [56% vs 45%]; P < .0001 for all measures, Figure 2). Despite the improvement in satisfaction when a provider sat down, only 13% of patients strongly agreed that it is important for a provider to sit during an ED encounter.
Table 1.
Characteristics of Patients Enrolled During the Study Period.
| Demographics | Both EDs | Intervention ED | Control ED | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | % | Pre | Study | Post | Total | % | Pre | Study | Post | Total | % | |
| Total | 2827 | 840 | 501 | 433 | 1774 | 62.8 | 247 | 373 | 433 | 1053 | 37.2 | |
| Age | ||||||||||||
| 18-25 | 654 | 23.1 | 246 | 133 | 116 | 495 | 27.9 | 30 | 72 | 57 | 159 | 15.1 |
| 26-40 | 872 | 30.8 | 265 | 170 | 147 | 582 | 32.8 | 63 | 101 | 126 | 290 | 27.5 |
| 41-65 | 968 | 34.2 | 259 | 141 | 129 | 529 | 29.8 | 112 | 145 | 182 | 439 | 41.7 |
| 66-85 | 305 | 10.8 | 66 | 52 | 36 | 154 | 8.7 | 37 | 53 | 61 | 151 | 14.3 |
| 86+ | 28 | 1.0 | 4 | 5 | 5 | 14 | 0.8 | 5 | 2 | 7 | 14 | 1.3 |
| Sex | ||||||||||||
| Female | 1777 | 62.9 | 580 | 316 | 270 | 1166 | 65.7 | 141 | 224 | 246 | 611 | 58.0 |
Abbreviation: ED, emergency department.
Figure 2.
Emergency department respondents who “strongly agreed” with each of the 5 quality measures assessed on the discharge survey based on provider sitting. Responses are aggregated from both emergency departments during the entire study period (n = 2741), P < .0001 for each comparison.
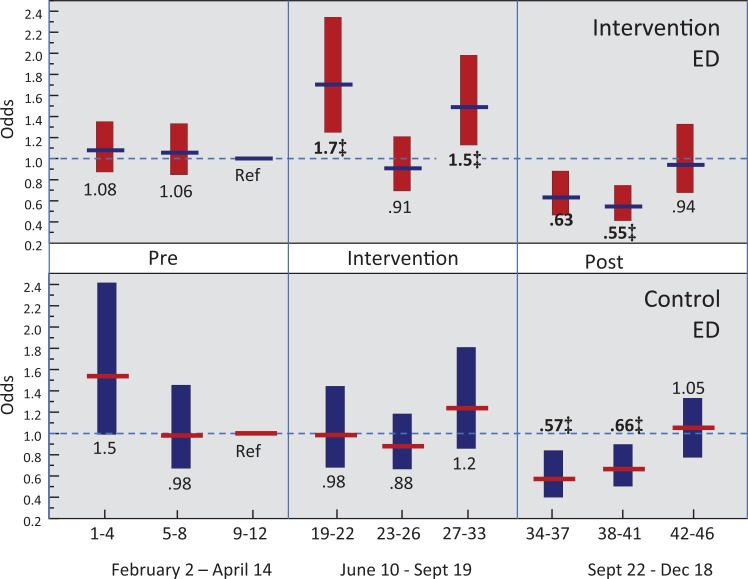
Patients were surveyed to identify provider (physician, APP, nurse) sitting behavior. During the entire study period, at least 1 provider sat down 40% of the time at the intervention site compared to 44% at the control. If only 1 provider sat down, it was more likely to be a physician as opposed to an APP or nurse (Table 2). After implementation of the folding seats and educational video at the intervention site, the odds of sitting by a physician or APP increased by 30% (odds ratio [OR] = 1.3, 95% confidence interval [CI]: 1.1-1.5) adjusted for patient satisfaction. There was no difference in physician and APP sitting at the control site (OR = 1.0, 95% CI: 0.8-1.2). Additionally, removal of the folding seat at the intervention site resulted in a significant decrease in physician and APP sitting across both study sites followed by return to the preintervention baseline (Figure 3).
Table 2.
Characteristics of Provider Type Who Sat Down During a Clinical Encounter as Reported by Patient Survey Responses.
| Provider | Intervention ED | Control ED | ||||
|---|---|---|---|---|---|---|
| Pre (%) | Study (%) | Post (%) | Pre (%) | Study (%) | Post (%) | |
| Total (MD, APP, Nurse) | 477 (57) | 290 (58) | 184 (42) | 173 (70) | 201 (54) | 212 (49) |
| MD | 211 (25) | 159 (32) | 79 (18) | 87 (35) | 110 (30) | 113 (26) |
| APP | 97 (11) | 53 (11) | 56 (13) | 27 (11) | 24 (6) | 14 (3) |
| Nurse | 169 (20) | 78 (16) | 49 (11) | 64 (26) | 67 (18) | 85 (19) |
Abbreviations: APP, advanced practice providers; ED, emergency department; MD, (Attending, Resident).
Figure 3.
Sitting during each period of the study (pre-, during, and postintervention). Multivariate logistic regression adjusted for patient satisfaction score (5-20). All comparisons use reference period 9 to 12 weeks before intervention. Ref indicates reference; ‡ = statistical significance.
Discussion
The primary goal of this study was to explore ways in which we can improve communication with our patients through influencing the behavior of our providers. Effective communication relies on both verbal and nonverbal cues. Prior studies in the ambulatory setting suggest that communication, measured by satisfaction surveys, is improved when a provider sits as opposed to stands (7,9). This is the first study to show that provider sitting at any point during the clinical encounter improves patient perception of their care and overall satisfaction in the ED setting. Furthermore, provider sitting was significantly influenced by placement of a colorful, branded folding seat in the clinical environment.
In 2008, Johnson et al studied 224 ED patient encounters and found that provider sitting was associated with an increased perceived length of time that a provider spent with patients; however, that study failed to show a significant benefit in patient satisfaction (13). In our larger, prospective observational study, we found a significant improvement in patient satisfaction when any provider sat down at any point during the clinical ED encounter. Interestingly, a majority of patients felt that provider posture was unimportant, yet the results suggest there is an unconscious patient preference for providers to sit down.
To encourage providers to sit down with patients in the ED, we tested whether education alone or a visual cue of a folding seat in addition to education changed the behavior. Similar to prior studies, we found that educating providers on the importance of sitting had no effect on provider posture (14). We were able to overcome this barrier and improve physician nonverbal communication by “nudging” providers to sit down by providing them with a visual cue—the branded seat—in their clinical environment. Default preferences or “nudges” are a tool utilized in behavioral economics.
Behavioral economics is a field of study that combines economic theory and psychology to investigate the way in which individuals respond to their environment (15 –17). In health care, behavioral economics is utilized in various ways: from addressing the childhood obesity epidemic to changing physician ordering behavior through default options in electronic health records (18,19). In this study, the branded folding seat with the slogan, “Grab a Seat,” served as a “nudge” to visually remind providers to sit down.
We found a statistically significant increase in the number of providers who sat during the intervention period at the intervention ED compared to the control ED. Of the providers who sat down, physicians were more likely to sit than an APP. This may be due to the patient population seen by APPs at our institution, where lower acuity patients are evaluated in a fast track setting. Sitting at the intervention site transiently returned to baseline during the intervention (weeks 23-26) before increasing again. This period spanned July, a time of trainee turnover in our academic health system. Once the seats were removed from the clinical environment, provider sitting significantly decreased across both study sites and eventually returned to the preintervention baseline. Interestingly, this result was observed at both sites. This phenomenon may be explained by the crossover of residents and attending physicians who work at both sites, further illustrating the powerful influence that visual cues can have on providers.
There are several limitations when attempting to attribute one intervention to patient satisfaction, particularly in an ED setting where multiple factors such as time of day, ED census, wait time, and hospital capacity all play a role in the overall patient experience. Further limitations of our study include the use of a convenience sample and survey as a method of data collection. Patients were immediately approached after discharge to minimize recall bias; however, 4% of intervention site and 5% of control site patients did not remember if any provider sat down. To minimize confounder bias, the patient was first asked about satisfaction, then was asked about whether a provider sat down. Patients may have been more willing to participate in the study if they were highly satisfied or highly dissatisfied with their care. Our study did not measure the actual frequency of use of the branded folding seat. Initially, our data collection was set to end 3 months after intervention rollout; however, after 3 seats broke, the study ended early due to safety concerns. We have since found a suitable alternative to the seats.
Conclusions
Using visual cues in the physical environment can nudge providers to sit down during the clinical encounter and improve patient satisfaction. The intervention is simple and can be easily adapted or implemented by other EDs or clinical settings. Future studies are needed to assess which part of the clinical encounter is the most important for providers to sit down. We believe that this relatively inexpensive, simple intervention will lead to improvement in perceived patient care and ED patient satisfaction.
Acknowledgments
The authors would like to thank The Housestaff and Advanced Practice Provider Quality Council at the Hospital of the University of Pennsylvania for their support and funding of this project. Additionally, we acknowledge Oluwabusayo A. Adebusuyi MD MPH, Tariq Ali MD, Jamie Senger CRNP, Kathleen Sindoni, Jeffrey Petty, Anita Mcginn-Natali, and Leonard Schultz for their contributions to the data collection, educational video, and quality improvement activity.
Author Biographies
Clinton J Orloski is a fellow in critical care medicine at the University of Washington School of Medicine (Seattle, Washington) where he serves as co-chair of the Housestaff Quality and Safety Council. He completed his residency training in emergency medicine at the Hospital of the University of Pennsylvania (Philadelphia, Pennyslvania).
Erica R Tabakin is an assistant professor of clinical emergency medicine at the Perelman School of Medicine at the University of Pennylvania, Philadelphia, Pennyslvania.
Frances S Shofer is the director of epidemiology and biostatistics and adjunct professor in the Department of Emergency Medicine at the Perelman School of Medicine at the Universtiy of Pennyslvania, Philadelphia, Pennyslvania.
Jennifer S Myers is director, Center for Healthcare Improvement and Patient Safety, and professor and director of quality and safety education, Department of Medicine, Perelman School of Medicine, University of Pennsylvania, Philadelphia, Pennyslvania.
Angela M Mills is a professor and chair for the Department of Emergency Medicine, Columbia University Vagelos College of Physicians & Surgeons, New York, NY.
Appendix A
Survey Instrument used for Data Collection. Question 7a was Omitted at the Control Site and in the Pre- and Postintervention Period at the Intervention site
Authors’ Note: C.J.O., E.R.T., and J.S.M. conceived the study and designed the trial. C.J.O., E.R.T., J.S.M., and A.M.M. supervised the conduct of the trial and data collection. C.J.O. and E.R.T. undertook recruitment of participating centers and patients and managed the data, including quality control. F.S.S. provided statistical advice on study design and analyzed the data, C.J.O. drafted the manuscript, and all authors contributed substantially to its revision. A.M.M. takes responsibility for the paper as a whole. The study was presented at the American College of Emergency Physicians Scientific Assembly, Las Vegas, NV, October 2016; Society for Hospital Medicine, Las Vegas, NV, May 2017; Emergency Department Operations Study Group, Nashville, TN, June 2017.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported by The Housestaff and Advanced Practice Provider Quality Council at the Hospital of the University of Pennsylvania.
References
- 1. Bensing JM, Dronkers J. Instrumental and affective aspects of physician behavior. Med Care. 1992;30:283–98. doi:10.1097/00005650-199204000-00001. [DOI] [PubMed] [Google Scholar]
- 2. Taylor DM, Wolfe R, Cameron PA. Complaints from emergency department patients largely result from treatment and communication problems. Emerg Med. 2002;14:43–9. doi:10.1046/j.1442-2026.2002.00284.x. [DOI] [PubMed] [Google Scholar]
- 3. Kadzombe EA, Coals J. Complaints against doctors in an accident and emergency department: a 10-year analysis. Arch Emerg Med. 1992;9:134–42. doi:10.1136/emj.9.2.134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Engel KG, Buckley BA, Mccarthy DM, Forth VE, Adams JG. Communication amidst chaos: challenges. Clin Commun. 2010;17:449–52. [Google Scholar]
- 5. Finefrock D, Patel S, Zodda D, Nyirenda T, Nierenberg R, Feldman J, et al. Patient-centered communication behaviors that correlate with higher patient satisfaction scores. J Patient Exp. 2018:237437351775041 doi:10.1177/2374373517750414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Swayden KJ, Anderson KK, Connelly LM, Moran JS, McMahon JK, Arnold PM. Effect of sitting vs. standing on perception of provider time at bedside: a pilot study. Patient Educ Couns. 2012;86:166–71. doi:10.1016/j.pec.2011.05.024. [DOI] [PubMed] [Google Scholar]
- 7. Haney S, Lee D, Sur D, Hale L. Patient perception of physician position (4P Study): does physician position influence patient perception of time? Proceedings of UCLA Healthcare. 2007;11:1–7. [Google Scholar]
- 8. Lin CT, Albertson GA, Schilling LM, Cyran EM, Anderson SN, Ware L, et al. Is patients’ perception of time spent with the physician a determinant of ambulatory patient satisfaction? Arch Intern Med. 2001;161:1437–42. doi:10.1001/archinte.161.11.1437. [DOI] [PubMed] [Google Scholar]
- 9. Merel SE, Mckinney CM, Ufkes P, Kwan AC, White AA. Sitting at patients’ bedsides may improve patients’ perceptions of physician communication skills. J Hosp Med. 2016; 11:865–68. doi:10.1002/jhm.2634. [DOI] [PubMed] [Google Scholar]
- 10. Clever SL, Jin L, Levinson W, Meltzer DO. Does doctor-patient communication affect patient satisfaction with hospital care? Results of an analysis with a novel instrumental variable. Health Serv Res. 2008;43:1505–19. doi:10.1111/j.1475-6773.2008.00849.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Haskard Zolnierek KB, DiMatteo MR. Physician communication and patient adherence to treatment. Med Care. 2009;47(8):826–34. doi:10.1097/MLR.0b013e31819a5acc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Blumenthal D, Jena AB. Hospital value-based purchasing. J Hosp Med. 2013;8:271–77. doi:10.1002/jhm.2045. [DOI] [PubMed] [Google Scholar]
- 13. Johnson RL, Sadosty AT, Weaver AL, Goyal DG. To sit or not to sit? Ann Emerg Med. 2008;51:188–193 , 193-2. doi:10.1016/j.annemergmed.2007.04.024. [DOI] [PubMed] [Google Scholar]
- 14. Curtis JR, Back AL, Ford DW, et al. Effect of communication skills training for residents and nurse practitioners on quality of communication with patients with serious illness: a randomized trial. JAMA. 2013;310:2271–81. doi:10.1001/jama.2013.282081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Voyer B. “Nudging” behaviours in healthcare: insights from behavioural economics. Br J Healthc Manag. 2015;21:130–35. doi:10.12968/bjhc.2015.21.3.130. [Google Scholar]
- 16. Lambert C. The marketplace of perceptions. Harv Mag. 2006:50–95. http://www.altruists.org/static/files/TheMarketplaceofPerceptions(CraigLambert).pdf. Accessed January 23, 2017.
- 17. Loewenstein G, Brennan T, Volpp KG. Asymmetric paternalism to improve health behaviors. JAMA. 2007;298:2415–2417. doi:10.1001/jama.298.20.2415. [DOI] [PubMed] [Google Scholar]
- 18. Halpern SD, Ubel PA, Asch DA. Harnessing the power of default options to improve health care. N Engl J Med. 2007;357:1340–44. [DOI] [PubMed] [Google Scholar]
- 19. Patel MS, Volpp KG. Nudging students toward healthier food choices – applying insights from behavioral economics. JAMA Pediatr. 2015;169:425–26. doi:10.1001/jamapediatrics.2015.0217. [DOI] [PubMed] [Google Scholar]