Abstract
Objective:
The aim of this study was to assess the presence and course of the anterior loop (AL) in an Odisha sample population using cone-beam computed tomography (CBCT) and to accurately identify and analyze the length, height, and diameter of AL in male and females.
Materials and Methods:
CBCT images from 1000 patients obtained for various clinical indications were randomly selected and evaluated to determine the presence, length, height, and diameter of the AL. The various parameters were then compared based on gender, age, and the side of the mandible. The data were analyzed using the Chi-square test, independent t-test, multiple post hoc procedure, and one-way ANOVA test.
Results:
An AL was identified in 9.7% of the cases, and its mean length ranged from 1.8 to 4.8 mm. The loop had a greater mean length and was significantly more prevalent in males. The diameter ranged from 1 to 4 mm and height ranged from 7.8 to 15.1 mm. The AL was most commonly found in the middle-aged patients (39–48 years) which attributed to around 27.83%.
Conclusion:
In this study, a lower prevalence of the AL of the mandibular canal was found. Being an anatomical variation, an exact evaluation of the AL must be established using the imaging techniques prior to any surgical procedure.
KEYWORDS: Anterior loop, cone-beam computed tomography, mandibular canal
INTRODUCTION
For many years, the treatment options available for people with missing teeth were fixed partial denture and removable prosthesis. Rehabilitating patients with dental implants require sound presurgical information and postsurgical assessment. To prevent iatrogenic complications and to ensurethe effectiveness of surgical procedures, the clinician should be thorough with the anatomy and its variations.[1] One such anatomical variation is the anterior loop (AL) of the inferior alveolar nerve (IAN). Although it is a benign variation, its accurate identification is necessary to prevent injury to the neurovascular bundle during dental implant placement in the inter-foraminal region of the mandible. Since the anatomy of the loop is complex, it is essential to use a diagnostic modality that allows satisfactory visualization and measurement of the loop.[2,3,4,5]
Cone-beam computed tomography (CBCT), is probably the most advantageous method for assessing the anatomy of the AL of the mandibular canal because it gives three-dimensional assessment with no magnification, unsharpness, and distortion, as seen in panoramic radiography (PR) which is otherwise the only alternative to visualize the loop.[6,7,8] Thus, the aim of the present study was to assess the presence and course of the AL in the mental foramen region along with identification and analysis of the variations in terms of length, diameter, and height of the AL in males and females in the Eastern Indian population.
MATERIALS AND METHODS
This record-based study was performed with the approval of the Institutional Ethics Committee of Kalinga Institute of Medical Sciences, KIIT, Deemed to be University (protocol number KIMS/KIIT/IEC/102/2016). Data were collected randomly from archived CBCT images which were obtained from the Department of Oral Medicine and Radiology, Kalinga Institute of Dental Sciences, Bhubaneswar. The images of the participants who have undergone a CBCT examination of premolar and molar region of the mandible was retrieved from the archival records and interpreted for assessment of AL of the mandibular canal.
From a pool of 1000 consecutive CBCT scans of the jaws obtained from June 2013 to August 2016, all the images were analyzed. The CBCT images were included if they were of adequate diagnostic quality, without fractures, artifacts, and pathologies that compromised the region of the mental foramen. The CBCT scans were acquired using a clinically available CBCT machine (Myray Hyperion X9, Italy), with a field of view of 11 cm × 8 cm. Data were acquired at a medium resolution of 0.3 mm thicknes; the average scanning time was 20 s at 90 Kvp and 10 mA current. CBCT images were analyzed using NNT software Version 2.0 (Myray Italy). Multiplanar reconstructions were made from the archived image sequences and the presence or absence of an AL was noted. After identification of AL, the following measurements were carried out from the CBCT images [Figures 1–3]
Figure 1.

Schematic representation of different measurements of variables of the anterior loop
Figure 3.
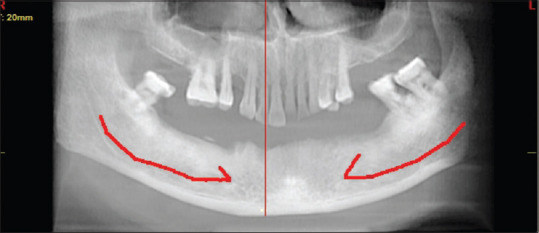
Panoramic reconstructed image showing the course of the mandibular canal and forming an anterior loop in a curved fashion along premolar region
Figure 2.

Cropped panoramic section demonstrating the different variables of the anterior loop measured in the study
L = Length of AL
H1 = Height from the superior cortex of mental foramen to the lower border of the mandible in panoramic reconstructed images and sagittal sections
H2 = Height from anterior-most point of the AL to the lower border of the mandible in panoramic images and sagittal sections
H3 = Height from the inferior border of the IAN canal to the lower border of the mandible (reference point is mental foramen in the sagittal image) in panoramic reconstructed images and sagittal sections
D = Diameter of AL.
The length of AL was measured using the amount of consecutive coronal reconstructions situated between the anterior border of mental foramen and the anterior border of the loop. This number was multiplied by the thickness of slices (0.3 mm).
According to Apostolakis and Brown,[7] the AL can be differentiated from the incisive canal based on the fact that the incisive canal has a diameter of <3 mm. When only a single round hypodense image was visualized, it was interpreted as the incisive canal if it exhibited a diameter smaller than 3 mm. If the diameter was larger than 3 mm, the anterior extension of the mandibular canal was considered to be an AL. An AL was also considered to be present when two round hypodense areas were observed, with one corresponding to the lumen of the mandibular canal that traverses the mental foramen anteriorly and inferiorly, and the other reflecting the doubling back (loop) of the mandibular canal, leading to the externalization of the IAN.
The data were summarized and analyzed by “Pearson Chi-square” test, “independent t-test,” “multiple post hoc” procedure, and “One-way ANOVA” test. Statistical Package for the Social Sciences (SPSS; IBM, California, USA) version 20.0 was used to perform the statistical analysis. P < 0.05 was considered to be statistically significant.
RESULTS
From a pool of 1000 CBCT scans used in this study, 97 scans demonstrated the presence of AL, while 903 scans did not show the presence of AL. Out of these 97 (9.7%) scans, 58 (5.8%) belonged to males and 39 (3.9%) belonged to females. The distributions of samples were divided into four different age groups, and males and females were divided accordingly.
A total of 97 individuals (out of 1000) had the presence of AL in the CBCT scans. In the age group G1 (18–28) years, 21 paients had the presence of AL (12 males and 9 females). In G2 (29–38 years), 22 patients had AL (20 males and 2 females). In G3 (39–48 years), 30 patients had the presence of AL (17 males and 13 females). In G4 (49–58 years), 24 patients demonstrated the presence of AL (9 males and 15 females) [Table 1 and Graphs 1 and 2].
Table 1.
Distribution of samples by age groups and gender, showing the presence of anterior loop
| Age groups (years) | Male (%) | Female (%) | Total (%) |
|---|---|---|---|
| 18-28 | 12 (57.14) | 9 (42.86) | 21 (21.65) |
| 29-38 | 20 (90.91) | 2 (9.09) | 22 (22.68) |
| 39-48 | 17 (56.67) | 13 (43.33) | 30 (30.93) |
| 49-48 | 9 (37.50) | 15 (62.50) | 24 (24.74) |
| Total | 58 (59.79) | 39 (40.21) | 97 (100.00) |
| χ2, P | 14.0052, 0.0030* | ||
*P<0.05 (P<0.05 is considered to be statistically significant)
Graph 1.
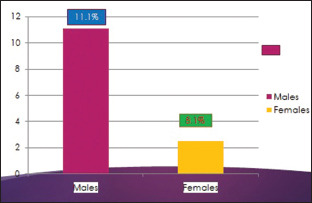
Presence of anterior loop among males and females
Graph 2.
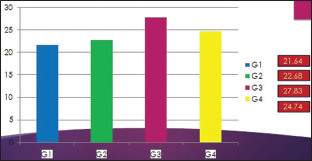
Presence of anterior loop among different age groups
In the present study, the mean value of length of AL on the left side was calculated to be 3.16 mm in males and 2.9 mm in females. The mean value of length of AL on the right side was calculated to be 3.4 mm in males and 3.57 mm in females. Similarly, the mean values for H1 (height from the superior cortex of the mental foramen to the lower border of mandible) on the left side were estimated to be 12.58 mm in males and 12.85 mm in females. The mean value of H2 on the right side was 12.65 mm in males and 12.8 mm in females. The mean values for H2 (height from anterior-most point of the AL to the lower border of mandible) on the left side was calculated to be 10.93 mm in males and 10.69 mm in females. On the right side, the mean value of H2 was found to be 10.29 mm in males and 9.92 mm in females. On the contrary, the mean values of H3 (height from the inferior border of the IAN canal to the lower border of the mandible) were calculated on the left side to be 11.01 mm in males and 10.94 mm in females. On the right side, the mean value of H3 was 10.79 mm in males and 10.71 mm in females. The mean diameter of AL on the left side in the present study was calculated to be 2.22 mm in males and 2.32 mm in females. On the right side, it was 4.83 mm in males and 2.64 mm in females [Table 2]. Analysis of different parameters for AL was carried out using one-way ANOVA and pair-wise comparisons by Tukey's multiple post hoc procedures [Tables 3–5].
Table 2.
Comparison of males and females with respect to different variables by “independent t-test”
| Variable | Gender | Mean | SD | SE | t | P |
|---|---|---|---|---|---|---|
| Length (mm) left | Male | 3.16 | 0.90 | 0.15 | 1.2553 | 0.2143 |
| Female | 2.90 | 0.59 | 0.12 | |||
| Length (mm) right | Male | 3.40 | 0.87 | 0.14 | −0.8674 | 0.3888 |
| Female | 3.57 | 0.74 | 0.14 | |||
| H1 (mm) left | Male | 12.58 | 1.52 | 0.25 | −0.6843 | 0.4965 |
| Female | 12.85 | 1.60 | 0.32 | |||
| H1 (mm) right | Male | 12.65 | 1.08 | 0.17 | −0.5640 | 0.5746 |
| Female | 12.80 | 1.04 | 0.19 | |||
| H2 (mm) left | Male | 10.93 | 1.74 | 0.29 | 0.5111 | 0.6112 |
| Female | 10.69 | 1.89 | 0.38 | |||
| H2 (mm) right | Male | 10.29 | 1.72 | 0.27 | 0.9223 | 0.3596 |
| Female | 9.92 | 1.56 | 0.29 | |||
| H3 (mm) left | Male | 11.01 | 1.31 | 0.22 | 0.1952 | 0.8459 |
| Female | 10.94 | 1.58 | 0.32 | |||
| H3 (mm) right | Male | 10.79 | 1.37 | 0.21 | 0.2354 | 0.8146 |
| Female | 10.71 | 1.54 | 0.29 | |||
| Average H (mm) right | Male | 11.50 | 1.35 | 0.22 | 0.0316 | 0.9749 |
| Female | 11.49 | 1.53 | 0.31 | |||
| Average H (mm) right | Male | 11.24 | 1.22 | 0.19 | 0.3531 | 0.7251 |
| Female | 11.14 | 1.16 | 0.22 | |||
| Diameter (mm) left | Male | 2.22 | 0.72 | 0.12 | −0.5913 | 0.5566 |
| Female | 2.32 | 0.54 | 0.11 | |||
| Diameter (mm) right | Male | 4.83 | 15.25 | 2.38 | 0.7723 | 0.4426 |
| Female | 2.64 | 0.73 | 0.13 |
*P<0.05 (P<0.05 is considered to be statistically significant). SE=Standard error, SD=Standard deviation
Table 3.
Comparison of age groups with respect to mean length (mm) at the left and right side by “one-way ANOVA”
| Age groups (years) | Length (mm) left | Length (mm) right | ||
|---|---|---|---|---|
| Mean | SD | Mean | SD | |
| 18-28 | 2.87 | 0.61 | 3.56 | 0.89 |
| 29-38 | 3.11 | 0.97 | 3.56 | 0.86 |
| 39-48 | 3.07 | 0.76 | 3.31 | 0.78 |
| 49-48 | 3.15 | 0.88 | 3.52 | 0.82 |
| Total | 3.05 | 0.79 | 3.47 | 0.82 |
| F | 0.3337 | 0.4187 | ||
| P | 0.8010 | 0.7402 | ||
| Pair-wise comparisons by Tukey’s multiple post hoc procedures | ||||
| 18-28 years versus 29-38 years | P=0.8783 | P=0.9999 | ||
| 18-28 years versus 39-48 years | P=0.8997 | P=0.8173 | ||
| 18-28 years versus 49-48 years | P=0.7823 | P=0.9995 | ||
| 29-38 years versus 39-48 years | P=0.9992 | P=0.7883 | ||
| 29-38 years versus 49-48 years | P=0.9992 | P=0.9990 | ||
| 39-48 years versus 49-48 years | P=0.9908 | P=0.8498 | ||
*P<0.05 (P<0.05 is considered to be statistically significant). SD=Standard deviation
Table 5.
Comparison of age groups with respect to mean diameter (mm) at the left and right side by “one-way ANOVA”
| Age groups (years) | Diameter (mm) left | Diameter (mm) right | ||
|---|---|---|---|---|
| Mean | SD | Mean | SD | |
| 18-28 | 2.11 | 0.40 | 2.56 | 0.84 |
| 29-38 | 2.37 | 0.83 | 2.63 | 0.79 |
| 39-48 | 2.23 | 0.65 | 2.28 | 0.72 |
| 49-48 | 2.35 | 0.70 | 2.64 | 0.73 |
| Total | 2.26 | 0.65 | 2.51 | 0.76 |
| F | 0.4678 | 1.0106 | ||
| P | 0.7059 | 0.3937 | ||
| Pair-wise comparisons by Tukey’s multiple post hoc procedures | ||||
| 18-28 years versus 29-38 years | P=0.7490 | P=0.9964 | ||
| 18-28 years versus 39-48 years | P=0.9498 | P=0.6916 | ||
| 18-28 years versus 49-48 years | P=0.7456 | P=0.9911 | ||
| 29-38 years versus 39-48 years | P=0.9445 | P=0.5131 | ||
| 29-38 years versus 49-48 years | P=0.9999 | P=0.9999 | ||
| 39-48 years versus 49-48 years | P=0.9515 | P=0.4362 | ||
*P<0.05 (P<0.05 is considered to be statistically significant). SD=Standard deviation
Table 4.
Comparison of age groups with respect to mean of H1, H2, and H3 (mm) at the left and right side by “one-way ANOVA”
| Age groups (years) | Mean of H1, H2, H3 left | Mean of H1, H2, H3 right | ||
|---|---|---|---|---|
| Mean | SD | Mean | SD | |
| 18-28 | 11.33 | 1.62 | 10.55 | 1.25 |
| 29-38 | 11.45 | 1.42 | 11.30 | 1.21 |
| 39-48 | 11.53 | 1.36 | 11.03 | 1.11 |
| 49-48 | 11.64 | 1.40 | 11.83 | 0.97 |
| Total | 11.50 | 1.41 | 11.20 | 1.19 |
| F | 0.1268 | 3.6857 | ||
| P | 0.9438 | 0.0162* | ||
| Pair-wise comparisons by Tukey’s multiple post hoc procedures | ||||
| 18-28 years versus 29-38 years | P=0.9966 | P=0.2678 | ||
| 18-28 years versus 39-48 years | P=0.9778 | P=0.5998 | ||
| 18-28 years versus 49-48 years | P=0.9328 | P=0.0110* | ||
| 29-38 years versus 39-48 years | P=0.9987 | P=0.8793 | ||
| 29-38 years versus 49-48 years | P=0.9850 | P=0.5200 | ||
| 39-48 years versus 49-48 years | P=0.9960 | P=0.1197 | ||
*P<0.05 (P<0.05 is considered to be statistically significant). SD=Standard deviation
DISCUSSION
The mandibular intermental area is assumed to be a safe area for implant insertion and is involved in many other surgical procedures. It is essential to understand the anatomy of the region for avoiding injuries to the neurovascular bundle. The recently developed all-on-four procedure permits a quick placement of four dental implants in the interforaminal area of the lower jaw associated with a fixed prosthesis with immediate placement. The location of the foramen, as well as, the possibility that an AL of the mental nerve may be present mesial to the mental foramen need to be considered before osteotomy to avoid mental nerve injury.[9]
Preoperative radiographic examination is an essential diagnostic method to determine these anatomical structures. Two-dimensional (2D) imaging modalities which include conventional imaging techniques such as periapical and PR are the radiographic methods of choice for preoperative evaluation and are recommended to assist preoperative examination.[10,11,12] Superimposition of overlying anatomy, distortion and magnification, and processing artifacts and lack of information in the third dimension are some of the known drawbacks of this type of imaging.[12]
Identification of AL using panoramic radiographs and periapical radiographs resulted in high percentage of false-positive and false-negative findings. In addition to this, several discrepancies and limitations were observed while viewing AL using 2D radiographic methods. Image overlapping and degree of corticalization of the bony canals are factors that may affect the visualization of AL. Moreover, detecting and interpretation of AL was a difficult task on panoramic radiographs. PR images also demonstrated an underestimation of the length of AL, suggesting that this 2D imaging modality does not offer reliable information about the location of the neurovascular structures of the anterior mandible.[12,13,14]
Several authors have postulated that visibility of AL decreases with age, which was not in accordance with our study because our study demonstrated a high prevalence of AL among older age groups. Group III patients (27.83%) with age group followed by Group IV (24.74%) > Group II (22.68%) > Group I (21.64%). Our data presented with significant differences associated with gender, with a higher prevalence of AL among males (11.1%) than females (8.1%). This was similar to the prevalence rates of the studies carried out by Rosa et al. in 2013, Sahman and Sisman in 2016, and Panjnoush et al. in 2015.[15,16,17]
AL s in our study were observed in the right side (37.11%), followed by the bilateral presence (35.05%) and then the unilateral presence on the left side (27.83%). The length of AL has been reported to vary in different populations. The length of the AL in our study was in the range of 1.8 mm to 4.8 mm which was in accordance with the previous studies reported by Vujanovic-Eskenazi et al. in 2015.[6] The mean length of the AL as reported by Kilic et al. in 2012 was 1.5–6 mm.[13] These differences may be, at least, partly due to the racial influence. The longest loop in the literature is reported by Neiva et al. being 11 mm.[6,9,18]
The studies conducted by do Nascimento et al.[1] highlighted the importance of knowledge regarding this anatomical variation. They measured the prevalence of AL along with its length among males and females of various age groups (13–87 years). They also found a mean length of AL to be 1.1–4 mm which was in accordance with our study. The diameter of AL in our study was defined in the range of 1–4 mm, which was in accordance with the studies conducted by Parnia et al.[9]
Our study also measured the height of the AL from three different points and was calculated in the mean range of: H1 = 10.2–15.1 mm, H2 = 7.9–13.8 mm, H3 = 7–13.9 mm. Considering these findings, it is important to consider a minimum safe distance to the AL, which may vary widely in function of the different studies carried out: 2 mm, 4 mm, or 6 mm.[19,20,21,22,23,24] In practical terms, we emphasize the importance of a case by case evaluation and no specific measurements for a safety distance. Individual, gender, age, race, assessing technique used, and degree of alveolar bone atrophy largely influence the different anatomical variations. It suggests that the clinicians should carefully identify these anatomical landmarks, by analyzing all influencing factors, prior to their surgical procedures.
CONCLUSION
We consider that a CBCT should be recommended when planning implant placement and all the surgical procedures carried out in the interforaminal region in order to maximize the use of the available space from the prosthetic point of view and to minimize the risk of injury to the neurovascular bundles. A safe distance anterior to mental foramen of about 4 mm should be determined for each patient to avoid injury to the mental nerve. We recommend that there is a need to increase the number of patients in further studies in order to make a strong recommendation with regard to safety margins. The AL of the mental nerve becomes a critical surgical reference point during treatment planning. Analyzing CBCT scans for assessment of AL in all dimensions described in this study can be a useful tool for avoiding surgical complications.
FINANCIAL SUPPORT AND SPONSORSHIP
Nil.
CONFLICTS OF INTEREST
There are no conflicts of interest.
ACKNOWLEDGMENT
The author's acknowledge Dr. Shivalingappa Javali for his contribution in analyzing the data and in proofreading of the paper.
REFERENCES
- 1.do Nascimento EH, Dos Anjos Pontual ML, Dos Anjos Pontual A, da Cruz Perez DE, Figueiroa JN, Frazão MA, et al. Assessment of the anterior loop of the mandibular canal: A study using cone-beam computed tomography. Imaging Sci Dent. 2016;46:69–75. doi: 10.5624/isd.2016.46.2.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Iyengar AR, Patil S, Nagesh KS, Mehkri S, Manchanda S. Detection of anterior loop and other patterns of entry of mental nerve into the mental foramen: A radiographic study in panoramic images. J Dent Implant. 2013;3:21–5. [Google Scholar]
- 3.de Oliveira-Santos C, Souza PH, de Azambuja Berti-Couto S, Stinkens L, Moyaert K, Rubira-Bullen IR, et al. Assessment of variations of the mandibular canal through cone beam computed tomography. Clin Oral Investig. 2012;16:387–93. doi: 10.1007/s00784-011-0544-9. [DOI] [PubMed] [Google Scholar]
- 4.Phraisukwisarn P, Asvanund P, Kretapirom K. Measurement of anterior loop of inferior alveolar nerve using cone beam computed tomography. M Dent J. 2017;37:83–9. [Google Scholar]
- 5.Kuzmanovic DV, Payne AG, Kieser JA, Dias GJ. Anterior loop of the mental nerve: A morphological and radiographic study. Clin Oral Implants Res. 2003;14:464–71. doi: 10.1034/j.1600-0501.2003.00869.x. [DOI] [PubMed] [Google Scholar]
- 6.Vujanovic-Eskenazi A, Valero-James JM, Sánchez-Garcés MA, Gay-Escoda C. A retrospective radiographic evaluation of the anterior loop of the mental nerve: Comparison between panoramic radiography and cone beam computerized tomography. Med Oral Patol Oral Cir Bucal. 2015;20:e239–45. doi: 10.4317/medoral.20026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Apostolakis D, Brown JE. The anterior loop of the inferior alveolar nerve: Prevalence, measurement of its length and a recommendation for interforaminal implant installation based on cone beam CT imaging. Clin Oral Implants Res. 2012;23:1022–30. doi: 10.1111/j.1600-0501.2011.02261.x. [DOI] [PubMed] [Google Scholar]
- 8.de Brito AC, Nejaim Y, de Freitas DQ, de Oliveira Santos C. Panoramic radiographs underestimate extensions of the anterior loop and mandibular incisive canal. Imaging Sci Dent. 2016;46:159–65. doi: 10.5624/isd.2016.46.3.159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Parnia F, Moslehifard E, Hafezeqoran A, Mahboub F, Mojaver-Kahnamoui H. Characteristics of anatomical landmarks in the mandibular interforaminal region: A cone-beam computed tomography study. Med Oral Patol Oral Cir Bucal. 2012;17:e420–5. doi: 10.4317/medoral.17520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Harris D, Buser D, Dula K, Grondahl K, Haris D, Jacobs R, et al. E.A.O. Guidelines for the use of diagnostic imaging in implant dentistry. A consensus workshop organized by the European association for osseointegration in trinity college Dublin. Clin Oral Implants Res. 2002;13:566–70. doi: 10.1034/j.1600-0501.2002.130518.x. [DOI] [PubMed] [Google Scholar]
- 11.Frederiksen NL. Diagnostic imaging in dental implantology. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995;80:540–54. doi: 10.1016/s1079-2104(05)80153-2. [DOI] [PubMed] [Google Scholar]
- 12.Nair UP, Yazdi MH, Nayar GM, Parry H, Katkar RA, Nair MK, et al. Configuration of the inferior alveolar canal as detected by cone beam computed tomography. J Conserv Dent. 2013;16:518–21. doi: 10.4103/0972-0707.120964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kilic C, Kamburoǧlu K, Ozen T, Balcioglu HA, Kurt B, Kutoglu T, et al. The position of the mandibular canal and histologic feature of the inferior alveolar nerve. Clin Anat. 2010;23:34–42. doi: 10.1002/ca.20889. [DOI] [PubMed] [Google Scholar]
- 14.do Couto-Filho CE, de Moraes PH, Alonso MB, Haiter-Neto F, Olate S, de Albergaria-Barbosa JR, et al. Accuracy in the diagnosis of the mental nerve loop. A comparative study between panoramic radiography and cone beam computed tomography. Int J Morphol. 2015;33:327–32. doi: 10.4067/S0717-95022015000100051. [DOI] [PubMed] [Google Scholar]
- 15.Rosa MB, Sotto-Maior BS, Machado Vde C, Francischone CE. Retrospective study of the anterior loop of the inferior alveolar nerve and the incisive canal using cone beam computed tomography. Int J Oral Maxillofac Implants. 2013;28:388–92. doi: 10.11607/jomi.2648. [DOI] [PubMed] [Google Scholar]
- 16.Sahman H, Sisman Y. Anterior loop of the inferior alveolar canal: A Cone-beam computerized tomography study of 494 cases. J Oral Implantol. 2016;42:333–6. doi: 10.1563/aaid-joi-D-15-00038. [DOI] [PubMed] [Google Scholar]
- 17.Panjnoush M, Rabiee ZS, Kheirandish Y. Assessment of location and anatomical characteristics of mental foramen, anterior loop and mandibular incisive canal using cone beam computed tomography. J Dent (Tehran) 2016;13:126–32. [PMC free article] [PubMed] [Google Scholar]
- 18.Neiva RF, Gapski R, Wang HL. Morphometric analysis of implant-related anatomy in Caucasian skulls. J Periodontol. 2004;75:1061–7. doi: 10.1902/jop.2004.75.8.1061. [DOI] [PubMed] [Google Scholar]
- 19.Moghddam MR, Davoudmanesh Z, Azizi N, Rakhshan V, Shariati M. Prevalence and length of the anterior loop of the inferior alveolar nerve in iranians. J Oral Implantol. 2017;43:333–6. doi: 10.1563/aaid-joi-D-16-00212. [DOI] [PubMed] [Google Scholar]
- 20.Shaban B, Khajavi A, Khaki N, Mohiti Y, Mehri T, Kermani H, et al. Assessment of the anterior loop of the inferior alveolar nerve via cone-beam computed tomography. J Korean Assoc Oral Maxillofac Surg. 2017;43:395–400. doi: 10.5125/jkaoms.2017.43.6.395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zmyslowska-Polakowska E, Radwanski M, Ledzion S, Leski M, Zmyslowska A, Lukomska-Szymanska M, et al. Evaluation of size and location of a mental foramen in the polish population using cone-beam computed tomography. Biomed Res Int. 2019;2019:1659476. doi: 10.1155/2019/1659476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Voon YS, Patil PG. Safe zone in anterior mandible related to the genial tubercle for implant osteotomy in a Chinese-Malaysian population: A CBCT study. J Prosthet Dent. 2018;119:568–73. doi: 10.1016/j.prosdent.2017.05.011. [DOI] [PubMed] [Google Scholar]
- 23.Aldosimani MA, Aljarbou FA, Althumairy RI, Alhezam AA, Aldawsari AI. Analysis of mandibular premolar root position in relation to adjacent cortical plates and mental foramen using cone beam computed tomography in the Saudi population. Saudi Med J. 2019;40:298–301. doi: 10.15537/smj.2019.3.23597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Husain MA, Tetradis S. Radiographic assessment for implants in the aesthetic zone. In: Schoenbaum T, editor. Implants in the Aesthetic Zone. Cham: Springer. 2019. pp. 23–45. [Google Scholar]


