Abstract
Context:
Intelligible speech and language is a useful marker for the child's overall development and intellect. Timely identification of delay by primary care physicians can allow early intervention and reduce disability. Data from India on this subject is limited.
Aims:
To study the prevalence and risk factors of speech-language delay among children aged 1-12 years.
Settings and Design:
A cross sectional study was conducted at the Pediatric outpatient department of a teaching hospital.
Materials and Methods:
Eighty four children (42 children with delayed speech and 42 controls) aged 1-12 years were included. The guardians of these children were requested to answer a questionnaire. History of the child's morbidity pattern and the risk factors for speech delay were recorded. The child's developmental milestones were assessed.
Statistical Analysis Used:
Data entry was analyzed using SPSS software, version 16. Standard statistical tests were used. A p value of less than 0.05 was taken as statistically significant.
Results:
Speech and Language delay was found in 42 out of 1658 children who attended the OPD. The risk factors found to be significant were seizure disorder (P=< 0.001)), birth asphyxia (P=0.019), oro-pharyngeal deformity (P=0.012), multilingual family environment (P=< 0.001), family history (P=0.013), low paternal education (P=0.008), low maternal education (P=< 0.001), consanguinity (P=< 0.001) and inadequate stimulation (P=< 0.001).
Conclusions:
The prevalence of speech and language delay was 2.53%. and the medical risk factors were birth asphyxia, seizure disorder and oro-pharyngeal deformity. The familial causes were low parental education, consanguinity, positive family history, multilingual environment and inadequate stimulation.
Keywords: Prevalence, risk factors, speech and language delay
Background
Developmental delay is diagnosed when a child does not attain normal developmental milestones at the expected age.[1] Speech is the sound produced, while language is a measure of comprehension.[2] The acquisition of intelligible speech and language is a useful marker for the child's overall development and intellect.[3] Speech delay is defined as when the child's conversational speech sample is either more incoherent than would be expected for age or is marked by speech sound error patterns not appropriate for age.[4,5]
Evidence implies that untreated speech and language delay can persist in 40%–60% of the children and these children are at a higher risk of social, emotional, behavioral, and cognitive problems in adulthood.[6,7] Prevalence of speech delay has been difficult to estimate because traditionally there is a belief that speech delay may run in families and it is not a cause of alarm. Often a “wait-and-watch” policy leads to late diagnosis and intervention for speech delay. Primary care clinicians and family physicians are the first point of contact for children with speech and language delay. It thus becomes their responsibility to identify obvious speech and language delay and address parental concerns.
Hearing loss is a well-documented etiology of speech delay.[8,9] However, the causes of speech–language delay are compound and represent an intricate relationship between the biological development and social environment in which the child learns to speak.[9]
Data on this subject from India are sparse compared with the West.[10] Thus, a cross-sectional study assessing the prevalence and factors affecting speech and language delay in children between 1 and 12 years was undertaken.
Materials and Methods
This cross-sectional study was conducted at the pediatric outpatient department (OPD) of a tertiary care teaching hospital during the month of January 2018 after obtaining approval from the Institutional ethics committee. Written informed consent was obtained from the guardians prior to enrolment of the children.
Every consecutive child (age 1–12 years) who was brought by caregivers for suspected delayed speech or who was referred specifically for speech delay or who was found to have delayed speech on DQ/IQ testing and every child undergoing speech therapy was included. Children whose caregivers did not give consent for participation in the study were excluded. A total of 42 children formed the study group and 42 children without speech-language delay were enrolled as the control group after obtaining consent from their guardians.
The caregivers of all these children were requested to answer a predesigned, pretested, and validated questionnaire. The questionnaire consisted of questions related to demographic data, birth history, history of the morbidity pattern of the child (any illness for which the child was treated either on an OPD basis or hospitalized), along with the high-risk factors for speech delay. The child's growth was assessed using anthropometry (weight, height, head circumference), and developmental milestones were examined at the time of contact and recorded in a data collection sheet.
Statistical analysis
Data entry was done using Microsoft Excel 2007 and was analyzed using Statistical Package for Social Sciences (SPSS) software, version 16. Descriptive analysis was presented as mean, standard deviation, and frequency. Statistical tests of significance used were unpaired t-test, Chi-square test, and Fisher's exact test. A P value of less than 0.05 was taken as statistically significant.
Results
A total of 1658 children belonging to the age group 1–12 years attended the pediatric OPD during the study period [Figure 1]. In all, 42 children (2.53%) were found to have speech and language delay. Of these children, one child had autistic features, one child had cerebral palsy, and another child had hearing loss as a comorbidity.
Figure 1.
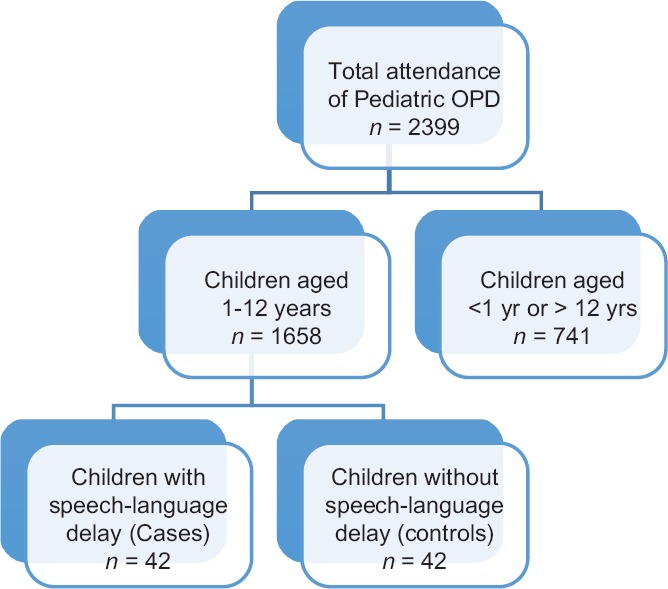
Flowchart showing children with speech delay attending the pediatric OPD
The study group and controls were compared for baseline characteristics, and there was no statistically significant difference between the two groups in terms of age, gender, religion, and socioeconomic status [Table 1].
Table 1.
Comparison of baseline characteristics between study and control groups
| Characteristic | Study group (n=42) | Control group (n=42) | P |
|---|---|---|---|
| Age (years) | 65.9+36.08 | 62.74+34.3 | 0.675*** |
| Gender | 0.510* | ||
| M | 25 (59.5%) | 22 (52.4%) | |
| F | 17 (40.5%) | 20 (47.6%) | |
| Religion | |||
| Hindu | 27 (64.3%) | 26 (61.9%) | 0.821* |
| Muslim | 15 (35.7%) | 16 (38.1%) | |
| Low socioeconomic status | 29 (69%) | 22 (52.4%) | 0.118* |
*Chi-square test; **Unpaired t-test; ***= Fisher's exact test, P value <0.05 is statistically significant
Seven medical risk factors for speech–language delay were compared in both the groups [Table 2]. There was a statistically significant difference between the two groups for three factors – seizure disorder, birth asphyxia, and physical (oro-pharyngeal) deformity, suggesting an association between these risk factors and speech–language delay.
Table 2.
Comparison of medical risk factors for speech-language delay between study and control groups
| Factor | Study group (n=42) | Control group (n=42) | P |
|---|---|---|---|
| Hearing loss | 1 (2.4%) | 0 | 1.000*** |
| Persistent otitis media | 2 (4.8%) | 0 | 0.494*** |
| Seizure disorder | 11 (26.2%) | 0 | <0.001* |
| Birth asphyxia | 11 (26.2%) | 3 (7.1%) | 0.019* |
| Low birth weight | 10 (23.8%) | 5 (11.9%) | 0.15* |
| Preterm birth | 5 (11.9%) | 2 (4.8%) | 0.433*** |
| Physical (oro-pharyngeal) | 7 (16.7%) | 0 | 0.012*** |
*Chi-square test; **Unpaired t-test; ***Fisher's exact test. Bold: P value <0.05 is statistically significant
Eleven family–based risk factors were also studied between the two groups [Table 3]. Multilingual family environment, positive family history of speech–language delay, consanguinity, low paternal education, and low maternal education were found to be associated with speech–language delay. There was a statistically significant difference between the two groups for these five factors.
Table 3.
Comparison of family-based risk factors for speech-language delay between study and control groups
| Factor | Study group (n=42) | Control group (n=42) | P |
|---|---|---|---|
| Multilingual family environment | 31 (73.8%) | 3 (7.11%) | <0.001* |
| Family history of speech disorder | 10 (23.8%) | 2 (4.8%) | 0.013* |
| Large family size | 19 (45.2%) | 23 (54.8%) | 0.383* |
| Family discord | 9 (21.4%) | 6 (14.3%) | 0.383* |
| Low paternal education (<10th std) | 30 (71.4%) | 18 (42.9%) | 0.008* |
| Low maternal education (<10th std) | 34 (81%) | 12 (28.6%) | <0.001* |
| Mother-child separation | 3 (7.1%) | 0 | 0.241*** |
| Absence of father | 4 (9.5%) | 0 | 0.116*** |
| Maternal occupation | 5 (11.9%) | 3 (7.11%) | 0.713*** |
| Consanguinity | 25 (59.5%) | 8 (19%) | <0.001* |
| High birth order | 13 (31%) | 7 (16.7%) | 0.124 |
*Chi-square test; **Unpaired t-test; ***Fisher's exact test. Bold: P value < 0.05 is statistically significant
Environmental factors such as trauma, chronic noise exposure, television viewing >2 h, and inadequate stimulation were studied [Table 4]. Of these, only inadequate stimulation was found to be statistically significantly different in the study group. Figure 2 summarizes the eight statistically significant risk factors associated with speech-language delay.
Table 4.
Comparison of environmental risk factors for speech-language delay
| Factor | Study group (n=42) | Control group (n=42) | P |
|---|---|---|---|
| Trauma | 1 (2.4%) | 0 | 1.000*** |
| Chronic noise exposure >65 db | 9 (21.4%) | 6 (14.3%) | 0.393* |
| Television viewing >2 h | 16 (38.1%) | 15 (35.7%) | 0.821* |
| Inadequate stimulation | 26 (61.9%) | 0 | <0.001* |
*Chi-square test; **Unpaired t-test; ***Fisher's exact test. Bold: P value < 0.05 is statistically significant
Figure 2.
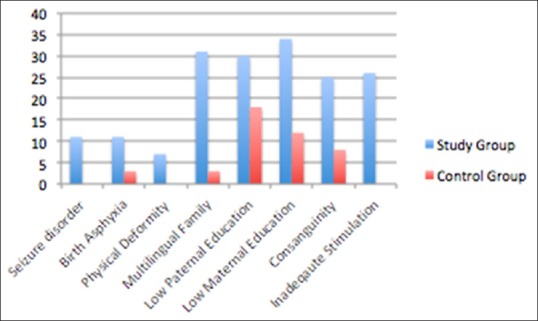
Significant risk factors associated with speech–language delay
Discussion
In our study, speech–language delay was found in 2.53% of the children attending pediatric OPD. These results are similar to the prevalence reported from developed countries which ranges from 2% to 8%.[3,11] Other studies have shown a higher incidence of speech–language delay in males[12] and attributed it to the slower maturation of the central nervous system among boys and also by the influence of testosterone which stops cell death and makes proper connections difficult.[12] However, our study found no gender difference.
A number of medical factors related to language delay were assessed – hearing loss, persistent otitis media, seizure disorder, birth asphyxia, low birth weight, preterm birth, and physical (oro-pharyngeal) deformity. Birth asphyxia, seizure disorder, and physical (oro-pharyngeal) deformity were found to be statistically significant risk factors. The association between birth asphyxia and language delay has been well documented by other studies.[13] The effect of epilepsy on speech–language has been reported by Mehta B et al.[14] The hypoxic insult to the brain during a seizure could prove detrimental in various areas of development and can manifest as speech and language delay. The association of oral and pharyngeal abnormalities with speech–language delay has been reported.[15] Hearing loss has been implicated in delayed language acquisition by other studies.[8,9] However, it was not found to be a significant risk factor as only one child had hearing impairment in our study.
The nonmedical risk factors were divided into two groups – family-based risk factors and environmental risk factors. The family-based risk factors studied were as follows: multilingual family environment, high birth order, consanguinity, family history of speech–language disorders, large family size, family discord, low paternal education, low maternal education, maternal occupation, mother–child separation, and absence of father. Our study found multilingual family environment, consanguinity, a positive family history of speech–language disorder, low paternal education, and low maternal education to be significant factors associated with speech–language delay. A multilingual home environment, commonly seen in India, could confuse the child during the early stages of learning a language.
We found consanguinity to be a statistically significant risk factor. Other studies have documented the association between consanguinity as an important risk factor for hearing loss leading to speech delay.[16] Interestingly, in our study consanguinity was found to be a significant risk factor for speech–language delay even in the absence of hearing loss.
A positive family history of speech-reading disorders (stuttering, unclear speech, late speaking, poor vocabulary, dyslexia) with the affected member being a first-degree relative has been known to be associated with speech and language delay.[10,17] Parents with better education not only engage their children more but also use more complex words that in turn stimulate and enhance the language skills of their children.[3] A large family size being a significant factor in speech delay was documented by Karbasi et al.[18] In our study, large family size was found in both the groups, and hence family size was not found to be significant.
The environmental factors analyzed were as follows: trauma, chronic noise exposure >65 db, television viewing for more than 2 h, low socioeconomic status, and inadequate stimulation. We found inadequate stimulation to be statistically significant which is in agreement with other studies.[19] Although there is a considerable amount of literature demonstrating higher birth order and low socioeconomic status as a risk factor for communication problems,[10,20] our study failed to do so.
Strengths of the study
The strengths of the study are that we have studied a large number of risk factors not routinely examined by Indian authors. The results of this study can help family physicians and primary care clinicians identify risk factors to facilitate timely detection and provide early intervention for speech and language delay.
Limitations of the study
The limitations of this study are that our study population was small and strictly hospital-based which could cause some amount of sample bias. Second, only a cross-sectional assessment was made to diagnose speech–language delay in children.
Future directions
Large multicentric follow-up studies should be done for a better understanding of the factors influencing speech–language development.
Conclusion
The prevalence of speech and language delay was 2.53% and the risk factors associated with it were both biological and environmental. The medical risk factors were birth asphyxia, seizure disorder, and oro-pharyngeal deformity. The familial and environmental causes were low paternal education, low maternal education, consanguinity, positive family history, multilingual environment, and inadequate stimulation.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
The authors would like to thank Dr. Satish Mali, Assistant Professor, Department of Community Medicine, K. J. Somaiya Medical College and Research Centre for statistical guidance.
References
- 1.Meschino S. A child with developmental delay: An approach to etiology. Paediatr Child Health. 2003;8:16–9. doi: 10.1093/pch/8.1.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Saeed HT, Abdulaziz B, AL-Daboon SJ. Prevalence and risk factors of primary speech and language delay in children less than seven years of age. J Community Med Health Educ. 2018;8:608. [Google Scholar]
- 3.Sidhu M, Malhi P, Jerath J. Early language development in Indian children: A population-based pilot study. Ann Indian Acad Neurol. 2013;16:371–5. doi: 10.4103/0972-2327.116937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shriberg LD. Four new speech and prosody-voice measures for genetics research and other studies in developmental phonological disorders. J Speech Hear Res. 1993;36:105–40. doi: 10.1044/jshr.3601.105. [DOI] [PubMed] [Google Scholar]
- 5.Shriberg LD, Austin D, Lewis BA, McSweeny JL, Wilson DL. The speech disorders classification system (SDCS): Extensions and life span reference data. J Speech Lang Hear Res. 1997;40:723–40. doi: 10.1044/jslhr.4004.723. [DOI] [PubMed] [Google Scholar]
- 6.Law J, Rush R, Schoon I, Parsons S. Modeling developmental language difficulties from school entry into adulthood: Literacy mental health and employment outcomes. J Speech Lang Hear Res. 2009;52:1401–16. doi: 10.1044/1092-4388(2009/08-0142). [DOI] [PubMed] [Google Scholar]
- 7.Morgans A, Ttofari Eecen K, Pezic A, Brommeyer K, Mei C, Eadie P, et al. Who to refer for speech therapy at 4 years of age versus who to watch and wait. J Pediatr. 2017;185:200–4.e1. doi: 10.1016/j.jpeds.2017.02.059. [DOI] [PubMed] [Google Scholar]
- 8.Wooles N, Swann J, Hoskison E. Speech and language delay in children: A case to learn from. Br J Gen Pract. 2018;68:47–8. doi: 10.3399/bjgp17X694373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shriberg LD, Kent RD, Kraals’ HB, McSweeny JL, Nadler CJ, Brown RL. A diagnostic marker for speech delay associated with otitis media with effusion: Backing of obstruents. Clin Linguist Phon. 2003;17:529–47. doi: 10.1080/0269920031000138132. [DOI] [PubMed] [Google Scholar]
- 10.Mondal N, Bhat B, Plakkal N, Thulasingam M, Ajayan P, Rudhan R. Prevalence and risk factors of speech and language delay in children less than three years of age. J Compr Ped. 2016;7:e33173. [Google Scholar]
- 11.Wren Y, Miller L, Peter JT, Emond A, Ralston S. Prevalence and predictors of persistent speech sound disorder at eight years old: Findings from a population cohort study. J Speech Lang Hear Res. 2016;59:647–73. doi: 10.1044/2015_JSLHR-S-14-0282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Silva GM, Couto MI, Molini-Avejonas DR. Risk factors identification in children with speech disorders: Pilot study. Codas. 2013;25:456–62. doi: 10.1590/S2317-17822013000500010. [DOI] [PubMed] [Google Scholar]
- 13.Stanton-Chapman TL, Chapman DA, Bainbridge NL, Scott KG. Identification of early risk factors for language impairment. Res Dev Disabil. 2002;23:390–405. doi: 10.1016/s0891-4222(02)00141-5. [DOI] [PubMed] [Google Scholar]
- 14.Mehta B, Chawla VK, Parakh M, Parakh P, Bhandari B, Gurjar AS. EEG abnormalities in children with speech and language impairment. J Clin Diagn Res. 2015;9:CC04–7. doi: 10.7860/JCDR/2015/13920.6168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lyons DC. Relationship of oral and pharyngeal abnormalities to speech. Arch Otolaryngol. 1932;15:734–8. [Google Scholar]
- 16.Reddy VVM, Bindu HL, Reddy PP, Rani UP. Role of consanguinity in congenital neurosensory deafness. Int J Human Genet. 2006;6:357–8. [Google Scholar]
- 17.Hayiou-Thomas ME, Carroll JM, Leavett R, Hulme C, Snowling MJ. When does speech sound disorder matter for literacy? The role of disordered speech errors, co-occurring language impairment and family risk of dyslexia? J Child Psychol Psychiatry. 2016;58:197–205. doi: 10.1111/jcpp.12648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Karbasi SA, Fallah R, Golenstan M. The prevalence of speech disorder in primary school students in Yazd-Iran. 2011;49:33–7. [PubMed] [Google Scholar]
- 19.Leung AK, Kao CP. Evaluation and management of the child with speech delay. J Am Board Fam Med. 1999;59:3121–8. [PubMed] [Google Scholar]
- 20.Chaimay B, Thinkhamrop P, Thinkhamrop J. Risk factors associated with language development problems in childhood – A literature review. J Med Assoc Thai. 2006;89:1080–6. [PubMed] [Google Scholar]


