Abstract
Introduction:
Adolescent Depression (AD) although is widely prevalent and is a prioritized disorder, it is under-diagnosed and under reported in primary-care. We document the post-test probability of three measures and select the best measure for identifying AD in primary-care settings in India based on the clinical utility.
Materials and Methods:
Three measures have been validated in India for AD and thus can be further evaluated for primary-care use; we calculated the positive (+PTP) and negative (-PTP) post-test probability from the prevalence of AD in India for Beck Depression Inventory-21 item version (BDI-21), Patient Health Questionnaire-9 item version (PHQ-9), and Children's Depression Rating Scale-Revised version (CDRS-R) using the Bayes theorem. The usefulness of the measure was defined a priori based on the odds ratio (OR) of +PTP (OR > 3) and −PTP (OR < 0.1).
Results:
The +PTP and −PTP for BDI-21 was 43% (95%CI = 40, 45%; OR = 0.7) and 25% (95%CI = 13, 43%; OR = 0.3) respectively. Similarly, the +PTP and − PTP for PHQ-9 was 74% (95%CI = 66, 81%; OR = 2.9) and 10% (95%CI = 6, 17%; OR = 0.1). Finally, +PTP and − PTP for CDRS-R was 78% (95%CI = 69, 84%; OR = 3.5) and 12% (95%CI = 7, 18%; OR = 0.1). Only CDRS-R achieved the useful decided a priori as can be seen in the Fagan's Nomograms.
Conclusion:
This research provides the evidence base for selecting CDRS-R as the screening measure, for Adolescent Depression, for clinical use in Primary-care settings in India.
Keywords: Adolescent, clinical-utility, depression, primary-care, screen
Introduction
The prevalence of depression among adolescents in India varies from 0.1 to 68% depending on the setting or methodology; and the consequent disease burden is enormous in India.[1] The Adolescent Depression (AD) is a Priority Mental Health Disorder of WHO, and therefore needs to be identified as well as treated in the Primary-care settings.[2] There is much under-reporting, under-diagnoses, and under-treatment of AD.[3] Low inter-rater reliability of 0.56 for Depressive Disorders[4] and 0.28 for Major Depression 0.28[5] in international diagnostic systems results in poor identification rates globally. Furthermore, about 50% of Major Depression diagnosis is missed because of lack of screening by primary-care physicians, in their day-to-day clinical work.[6] In these circumstances the use of psychometrically validated measures could help improve the diagnostic reasoning and identification of adolescent depression. Therefore, we studied the post-test probability of three measures validated for identifying adolescent depression in India from the perspective of: (1) Do they all satisfy the post-test probability criteria to adopt them for primary-care use; (2) which one of the three available measures is best suited for clinical use in primary-care setting.
Materials and Methods
Setting
This secondary research was done based on published data available about Adolescent Depression since 2007 in India. Therefore, no informed consent, ethical clearance, and permission from the local Institution Review Board were needed.
Measures
There are a variety of screening measures for AD; in India till date only three measures have been validated and thus can be further evaluated for primary-care use. We studied these measures: Beck Depression Inventory-21(BDI-21) item version,[7] Patient Health Questionnaire-9 item version (PHQ-9)[8] and Children's Depression Rating Scale-Revised version (CDRS-R) validated for Adolescents.[9] All the diagnostic accuracy, reliability, and validity of the three measures were documented for India, their post-test probabilities, the essential parameter for recommendation in clinical use, were not documented.
Beck Depression Inventory (version I) - 21 item (BDI-21) is a self-rated 21 item depression inventory, with each itemrated in a 0–3 likert scale of increasing intensity. A clinical cut-off score of ≥21 is diagnostic of depression in India, and can be completed in about 10 minutes.[7] Although the diagnostic cut-off score is higher in the Indian population, in the Western populations, this measure, classifies depression as minimal depression (score of 0–13), mild depression (score of 14–19), moderate depression (score of 20–28), and severe depression (score of 29–63). Beck Depression Inventory (version I) is free and available in open domain.
Patient Health Questionnaire-9 item version (PHQ-9) is a 9- item depression measure and each item has a 3-point likert scoring with total scores ranging from 0 to 27. The diagnostic cut-off score in India for adolescent depression is ≥5; it takes about 10–15 minutes to score.[8] It further classifies Major Depression as mild (score of 5–9 where watchful waiting is suggested), moderate (score of 10–14 where counselling and/or pharmacotherapy is suggested), and severe (score of 20–27 where immediate initiation of pharmacotherapy is suggested). The PHQ-9 is free and available in public domain.
Children's Depression Rating Scale-Revised version (CDRS-R) is used as a clinician rated measure for diagnosing depression and its severity. CDRS-R has 17 symptom areas scored in a 0-5/7 point likert scale; the total score ranges from 17 to 113. A clinical cut-off score of ≥30 is diagnostic of depression in India and can be completed in about 15–20 minutes.[9] Severity classification of depression is not available for this scale and has to be bought from official sources.
Statistical analysis
In the absence a summary prevalence for adolescent depression, we considered the prevalence of 40% in the most recent well conducted school based study[10] (Singh et al., 2017) as our pre-test probability of depression for analysing the post-test probability for adolescent depression after using PHQ-9, BDI-12, and CDRS-R. We calculated the positive likelihood ration (+LR) and negative likelihood ratio (-LR), and their 95% Confidence Interval (95%CI), from the sensitivity and specificity. A priori we decided that for a depression test to be recommended for primary-care use, the odds ratio (OR) for the positive post-test probability should demonstrate a ≥3-fold increase. Likewise, we expected the OR for the negative post-test probability ≤0.1. A positive post-test probability with an OR <3 and a negative post-test probability of >0.1 would be considered as indeterminate and not useful in diagnostic reasoning and would not be suggested to the primary care clinicians as having clinically utility. We used the Bayes theorem for calculating the post-test probabilities.[11]
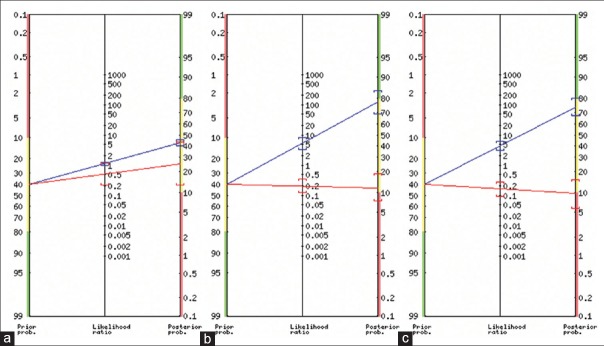
In the Fagan's Nomogram, the left column represent the pre-test probability, where the red band denotes that the pre-test probability of AD is low with clinical examination and known prevalence, and the primary-care clinician might not order for depression test. The green band indicates the pre-test probability is so high for AD that the clinician after the clinical examination would treat the AD even without ordering for the test. The yellow band represents that the pre-test probability is indeterminate where ordering the test is most useful in diagnostic reasoning. The blue line and red line representing the movement of pre-test probability to positive and negative post-test probability through the middle column, which represents the positive and the negative likelihood ratios. The right column represents the post-test probability; if the blue line reaches the green band it had achieved the required a priori positive post test probability, and if the red line reached the red band it has achieved the negative post-test probability; being in the yellow band suggests that even if the test is ordered it would not help the diagnostic reasoning.
Results
The BDI-21 had sensitivity (91%) and specificity (18%) (Baskar et al., 2007) provided the +LR and −LR of 1.11 (95%CI = 0.99, 1.24) and 0.50 (95%CI = 0.22, 1.15). From the LR values the calculated positive post-test probability was 43% (95%CI = 40, 45%; OR = 0.7) and negative post-test probability as 25% (95%CI = 13, 43%; OR = 0.3). Similarly, with the sensitivity (87%) and specificity (80%) for the PHQ-9 (Ganguly et al., 2013), we calculated the +LR and −LR of 4.35 (95%CI = 2.96, 6.40) and 0.16 (95%CI = 0.09, 0.30). The positive post-test probability for PHQ-9 was 74% (95%CI = 66, 81%; OR = 2.9) and negative post-test probability as 10% (95%CI = 6, 17%; OR = 0.1). Finally, the sensitivity and specificity of CDRS-R was 83% and 84% respectively, which provided the + LR and − LR of 5.19 (95%CI = 3.33, 8.08) and 0.20 (95%CI = 0.12, 0.34). From the LR values the calculated positive post-test probability was 78% (95%CI = 69, 84%; OR = 3.5) and negative post-test probability as 12% (95%CI = 7, 18%; OR = 0.1). The Fagan's Nomogram representing the positive and negative post-test probability and the colour bands that depict the clinical usefulness decided a priori are presented in Figure 1.
Figure 1.
The post-test probability of Beck Depression Inventory (a), Patient Health Questionnaire-9 (b), and Children's Depression Rating Scale (c) for adolescent in India
Discussion
Considering the magnitude of this treatable condition among adolescents, which otherwise result in long-term social, emotional, and financial burdens for the individual, family, and society, screening for AD in primary-care settings is indispensable in India. The family physicians remain the first port of call for the physical illnesses and a myriad of psychiatric disorders. In fact, often the family physicians is only health care professional available to address the adolescent mental health concerns, as the human resources for mental health is low in most of the low and middle income countries including India; in addition AD being one of the Priority Mental Health Disorders recognised by the World Health Organization, the identification and effective management of AD preferably has to happen in primary-care settings by family physicians.[12] Collaborative training workshops between family physicians and child and adolescent psychiatrists have been found to be further useful in India in achieving this goal.[13] Among the three measures we studied for identifying Adolescent Depression, we found the BDI-21 did not satisfy the a priori criteria for recommendation; the positive post-test probability was below the required OR threshold (should be >3) and negative post-test probability was above the OR threshold (should be <0.1). The PHQ-9 had the required negative post-test probability but was just short of the required positive post-test probability OR threshold. The CDRS-R satisfied the positive post-test probability and negative post-test probability threshold. Therefore, CDRS-R is the best measure for identifying Depressive Disorder or Major Depression among adolescent. As screening so essential to ensure accurate diagnosis, effective treatment and follow-up, if a clinician in primary-care is unable to procure CDRS-R, then PHQ-9 could be used as the measure has it has just fallen short on the positive post-test probability and is available in open domain.
Watchful waiting include increasing the frequency of follow-up visits, encouraging the adolescent to engage in regular exercise and activities, and identifying peer and adult support.[14,15] If the adolescent needs active treatment, psychotherapy and/or medications, the guidelines recently published by the Indian Psychiatric Society could be followed in the primary-care settings.[16] Adolescents with atypical depressions, treatment resistance, concurrent mental health problems, and intolerance to antidepressants may be referred to appropriate secondary or tertiary care management.
Conclusion
This research provides the evidence base for selecting the CDRS-R as the screening measure, for Adolescent Depression, for clinical use in in family medicine as well as Primary-care settings in India.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Ogbo FA, Mathsyaraja S, Koti RK, Perz J, Page A. The burden of depressive disorders in South Asia, 1990-2016: Findings from the global burden of disease study. BMC Psychiatry. 2018;18:333. doi: 10.1186/s12888-018-1918-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization: Child and Adolescent Mental Health Policies and Plans 2005. Geneva: World Health Organization; 2005. [Google Scholar]
- 3.Polanczyk GV, Salum GA, Sugaya LS, Caye A, Rohde LA. Annual research review: A meta-analysis of the worldwide prevalence of mental disorders in children and adolescents. J Child Psychol Psychiatry. 2015;56:345–65. doi: 10.1111/jcpp.12381. [DOI] [PubMed] [Google Scholar]
- 4.Richieri R, Boyer L, Lancon C. Analysis of the reliability of diagnostic criteria and classifications in psychiatry. Sante Publique. 2011;23(Suppl 6):S31–8. [PubMed] [Google Scholar]
- 5.Regier DA, Narrow WE, Clarke DE, Kraemer HC, Kuramoto SJ, Kuhl EA, et al. DSM-5 field trials in the United States and Canada, Part II: Test-retest reliability of selected categorical diagnoses. Am J Psychiatry. 2013;170:59–70. doi: 10.1176/appi.ajp.2012.12070999. [DOI] [PubMed] [Google Scholar]
- 6.U.S. Preventive Services Task Force. Screening for depression: Recommendations and rationale. Ann Intern Med. 2002;136:760–4. doi: 10.7326/0003-4819-136-10-200205210-00012. [DOI] [PubMed] [Google Scholar]
- 7.Basker M, Moses PD, Russell S, Russell PS. The psychometric properties of beck depression inventory for adolescent depression in a primary-care paediatric setting in India. Child Adolesc Psychiatry Ment Health. 2007;1:8. doi: 10.1186/1753-2000-1-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ganguly S, Samanta M, Roy P, Chatterjee S, Kaplan DW, Basu B. Patient health questionnaire-9 as an effective tool for screening of depression among Indian adolescents. J Adolesc Health. 2013;52:546–51. doi: 10.1016/j.jadohealth.2012.09.012. [DOI] [PubMed] [Google Scholar]
- 9.Basker MM, Russell PS, Russell S, Moses PD. Validation of the children's depression rating scale- revised for adolescents in primary-care pediatric use in India. Indian J Med Sci. 2010;64:72–80. [PubMed] [Google Scholar]
- 10.Singh MM, Gupta M, Grover S. Prevalence and factors associated with depression among schoolgoing adolescents in Chandigarh, north India. Indian J Med Res. 2017;146:205–15. doi: 10.4103/ijmr.IJMR_1339_15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fagan TJ. Letter: Nomogram for bayes theorem. N Engl J Med. 1975;293:257. doi: 10.1056/NEJM197507312930513. [DOI] [PubMed] [Google Scholar]
- 12.Russell PS, Mammen P, Nair MK, Russell S, Shankar SR. Priority mental health disorders of children and adolescents in primary-care pediatric setting in India 1: Developing a child and adolescent mental health policy, program, and service model. Indian J Pediatr. 2012;79(Suppl 1):S19–26. doi: 10.1007/s12098-011-0426-9. [DOI] [PubMed] [Google Scholar]
- 13.Russell PS, Nair MK. Strengthening the paediatricians project 1: The need, content and process of a workshop to address the priority mental health disorders of adolescence in countries with low human resource for health. Asia Pac Fam Med. 2010;9:4. doi: 10.1186/1447-056X-9-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zuckerbrot RA, Cheung AH, Jensen PS, Stein RE, Laraque D GLAD-PC Steering Group. Guidelines for adolescent depression in primary care (GLAD-PC): I. Identification, assessment, and initial management. Pediatrics. 2007;120:e1299–1312. doi: 10.1542/peds.2007-1144. [DOI] [PubMed] [Google Scholar]
- 15.Cheung AH, Zuckerbrot RA, Jensen PS, Ghalib K, Laraque D, Stein RE GLAD-PC Steering Group. Guidelines for adolescent depression in primary care (GLAD-PC): II. Treatment and ongoing management. Pediatrics. 2007;120:e1313–26. doi: 10.1542/peds.2006-1395. [DOI] [PubMed] [Google Scholar]
- 16.Grover S, Avasthi A. Clinical practice guidelines for the management of depression in children and adolescents. Indian J Psychiatry. 2019;61(Suppl 2):226–40. doi: 10.4103/psychiatry.IndianJPsychiatry_563_18. [DOI] [PMC free article] [PubMed] [Google Scholar]