Abstract
Introduction:
Developing country, like India intestinal parasitic infections are still remaining as the most important health problem in public of concern. The infection remains the most leading cause of morbidity and mortality especially among the childrens. It is presumed that the prevalence is high in developing countries probably due to poor sanitary conditions and improper personal hygiene practice.
Aim:
The main aim of this study was carried to find out the prevalence of intestinal parasitic infection among rural and urban population of Puducherry, India.
Materials and Methods:
This is a cross-sectional descriptive study carried out between the period September 2016 to December 2018. Random sampling was adopted to collect stool samples from urban and rural population in Puducherry. A door to door survey was done. Stool samples were collected from rural setting (n = 500) and urban setting (n = 506) and transport to the parasitology section, Dept. of Microbiology, JIPMER were subjected to routine stool investigations. The results were recorded, and data were presented in the form of frequency and distribution. Data entry was done in MS Excel and analysis was carried out in SPSS software version 22.
Results:
Among the rural and urban population, 500 stool samples from the rural population showed nearly 40.4% intestinal parasites Giardia intestinalis (21.2%), Blastocystis spp (8.8%), Entamoeba spp (6.6%), hookworm (2.8%), Ascaris lumbricoides (1%), Hymenolepis nana (0%) and 506 stool samples from urban population showed 20.3% of intestinal parasites (Giardia intestinalis (10.4%), Blastocystis spp (3.7%), Entamoeba spp (3.3%), hookworm (1.7%), Hymenolepis nana (0.9%), Ascaris lumbricoides (0%). There was a noticeable male predominance pattern (31.4%) compared to female showing 29.1% positivity. The increase in the prevalence of intestinal parasites among rural population than the urban population was statistically significant.
Conclusion:
The stool samples collected from rural population showed high prevalence of intestinal parasite infestation when compared to urban population, hence necessary interventions like health education, awareness creation and medical intervention should be undertaken particularly among the rural population. In our study population, age group between 1-10 years are predominantly infected with these parasites.
Keywords: Helminths, hygiene, intestinal parasites, protozoa, sanitation, South India
Introduction
Intestinal parasites are widely prevalent in developing countries, probably due to poor sanitation and inadequate personal hygiene. The other factors attributable to the prevalence of these infections are poverty, illiteracy, tropical hot and humid weather conditions and contaminated drinking water resources.[1] Consequently, the epidemiological pattern of these parasites varies in different geographical regions. It is estimated that as much as 60% of the world's population is infected with gut parasites, which may play important role in causing morbidity and mortality especially among the children group due to intestinal infection.[2]
The enteric protozoan parasites and the soil-transmitted helminths are responsible for gastrointestinal disturbances leading to infections. The WHO report states that amoebiasis caused by the protozoan parasite Entamoeba histolytica is most common parasitic cause of morbidity and mortality, with an estimate of about 50 million infections worldwide[3] followed by giardiasis caused by Giardia intestinalis/duodenalis and cryptosporidiosis caused by Cryptosporidium spp. Ascaris lumbricoides and Hymenolepis nana are the commonest nematode and cestode affecting approximately 1 billion people.[4] The commonest parasitic infections reported globally are Ascaris lumbricoides (20%), hookworm (18%), Trichuris trichuira (10%) and Entamoeba histolytica (10%) WHO 1987.
Intestinal parasitic infections are a major source of health concern in India like in any other developing nations. The overall prevalence of intestinal infections, caused by enteric parasites ranges from 12.5-67% in our country. Limited studies determining the prevalence of intestinal parasitic infections have been published previously from South India.[2,5,6] These studies report the prevalence of intestinal parasitic infections among slum-dwellers and children of rural and urban locations of Chennai, Tamil Nadu respectively.[5,6] The prevalence of the pathogenic intestinal parasites has been determined among a Southern Indian rural community from Vellore district of Tamil Nadu.[2]
The studies related to the overall frequency of enteric parasites in the Union Territory of Puducherry have been scanty.[7] whereas, a study related specifically to helminthic infections in school children from Puducherry have been published in the recent past.[8] Prevalence of intestinal parasites among patients attending a tertiary care center in South India was a multicentric study conducted in JIPMER hospital.[9] To our knowledge, no studies, taking into account the overall prevalence of the intestinal parasites from rural and urban communities in Puducherry has been reported. Therefore, this study was conducted to determine the present distribution pattern of the intestinal parasites among rural and urban communities in Puducherry, South India.
Materials and Methods
Study design
This is a cross sectional descriptive study.
Study area
This study was carried out in rural setting (Ramanathampuram, Thuthippet, Pilliarkuppam and Thondamanatham) urban setting (Kuruchikuppam, Chinayakuppam, Vazakullam and Vaithiakuppam) of Pondicherry (South Indian), India [Figure 1].
Figure 1.
A geographic map showing the location of the rural and urban settings (red dots) involved in the study. This map was created using the Esri ArcMap 10.2.1 software. This image has been reproduced with the permission of ICMR, VCRC Pondicherry-06
Study population
All age groups, both the genders with symptomatic and asymptomatic were included in this study between September 2016 to December 2018.
Sample size
A random sampling was adopted to collect stool samples from urban and rural settings in Puducherry. Stool samples were collected from rural setting (n = 500) and urban setting (n = 506) door to door survey.
Data collection
Data was collected using a structured questionnaire/Details proforma to obtain the socio demographic profile and a sterile container was used to collect the stool samples.
Study period
The study was carried out between the period September 2016 to December 2018.
Ethical approval
Obtained from JIPMER Institute Ethics Committee IEC (Human Studies) Reg No: ECR/342/Inst/PY/2013.
Inclusion criteria
Infants, adults and pregnant mothers of both urban and rural settings with asymptomatic and symptomatic various complaints and who were willing to give their samples are included.
Exclusion criteria
Infants, adults and pregnant mothers who were not willing to give their samples and with anti-parasitic drugs individual were excluded.
Informed consent
Informed consent was obtained from each of the selected participants and their parents before data and sample collection.
Sample collection and transportation
Individual person was given a sterile labeled container and advised to take required amount of stool sample. The samples were transported on ice pack kept inside the box to the laboratory within 2-4 hours of collection and processed immediately.
Methods used in detection of parasites
All the samples were processed immediately without delay within 2-4 hour. Macroscopic examination was done to identify color, consistency and blood stain. Saline and iodine wet mount preparations from each sample before and after formal-ether concentration technique was done then were examined under 100 × and 400 × magnification of the light microscope to detect protozoal trophozoites and helminthic eggs or larvae.[10] The results were recorded, and the data was analysed in the form of frequency and distribution.
Statistical analysis
Data analysis was carried out using SPSS software version 22 (SPSS Inc., Chicago, USA). The prevalence of intestinal parasitic infection among urban and rural of the study participants were analyzed using descriptive statistics. The odds ratio (OR) and statistical significance (P value).
Results
A total of 1006 stool samples were collected from rural (n = 500) and urban (n = 506) during the study period. The participants are divided in to three categories based on age in years 1-10, 11-20, 21-30. Majority of the participants belonged to the age group of 1-10 (87.7%), 11-20 (9.4%) and 21-30 (2.7%) years of age. There was nearly equal distribution of male and female population, about 50.1% and 49.8% respectively. Among the total study participants 50.2% of them was from urban population and 49.7% was from rural population the data were depicted in Table 1 which gives the detail about socio demographic characteristic of the study population.
Table 1.
Sociodemographic characteristics of study population
| Particulars | Frequency | Percentage |
|---|---|---|
| (n=1006) | (%) | |
| Age (in years) | ||
| 1-10 | 883 | 87.7% |
| 11-20 | 95 | 9.4% |
| 21-30 | 28 | 2.7% |
| Gender | ||
| Male | 505 | 50.1% |
| Female | 501 | 49.8% |
| Residence | ||
| Urban | 506 | 50.2% |
| Rural | 500 | 49.7% |
Among the stool samples collected from study population, 69.6% of the total samples did not have any intestinal parasite, 15.8% of the samples showed the presence of Giardia lamblia, 6.2% showed the presence of Blastocystis spp, 4.9% of stool samples showed the presence of Entamoeba spp and 2.2% showed the presence of hookworm, 0.4% showed the presence of H. nana and Ascaris lumbricoides, which was the least when compared to other organisms were showed in Table 2 which showed about the prevalence of intestinal parasites of the study population.
Table 2.
Percentage of intestinal parasites in stool samples of study population
| Parasites | Number | Percentage (%) |
|---|---|---|
| No parasites | 701 | 69.6% |
| Giardia intestinalis | 159 | 15.8% |
| Blastocystis spp | 63 | 6.2% |
| Entamoeba spp | 50 | 4.9% |
| hookworm | 23 | 2.2% |
| Ascaris lumbricoides | 5 | 0.4% |
| H. nana | 5 | 0.4% |
| Total | 1006 | 100% |
The prevalence of Giardia intestinalis was found to be 21.2% in stool samples collected from rural population and 10.4% in the samples collected from urban population, Blastocystis spp was found in 8.8% of the samples collected from rural population and 3.7% in the samples from urban population, Entamoeba spp was found in 6.6% in the samples collected from rural population and 3.3% in the samples collected from urban population, hookworm was found in 2.8% in the samples collected from rural and 1.7% in the samples collected from urban, Ascaris lumbricoides was found in 1% in the samples collected from rural population and absence in the samples collected from urban, Hymenolepis nana was found absence in the samples collected from rural population and 0.9% in the samples from urban population were showed in Figure 2 about the distribution of intestinal parasites among the rural and urban population.
Figure 2.
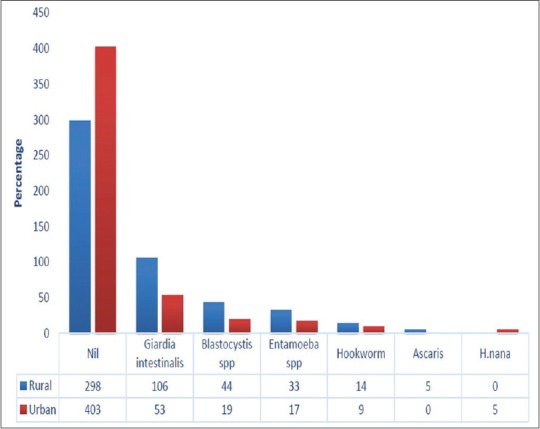
Distribution of intestinal parasites among rural and urban population
The prevalence of intestinal parasites in the stool samples among the rural population (66%) was more when compared to the urban population (34%), which were depicted in Figure 3 and the statistically significant association (P ≤ 0.05) and Odds ratio found to be 2.65 times higher risk of acquiring intestinal parasitic infection in rural population were showed in Table 3.
Figure 3.
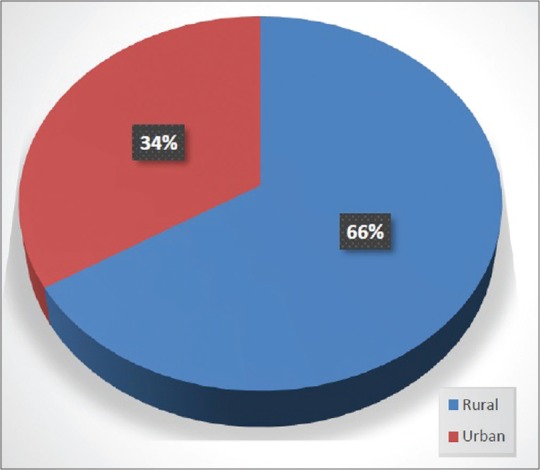
Comparison of rural and urban samples based on presence of intestinal parasites
Table 3.
Association between presence of intestinal parasites among rural and urban population
| Residence | Presence of Parasites | Absence of Parasites | Total | P | Odds ratio | ||
|---|---|---|---|---|---|---|---|
| Number | Percentage (%) | Number | Percentage (%) | ||||
| Rural | 202 | 40.4% | 298 | 59.6% | 500 | ||
| Urban | 103 | 20.3% | 403 | 79.6% | 506 | <0.001 | 2.65 |
| Total | 305 | 30.3% | 701 | 69.6% | 1006 | ||
Discussion
Intestinal parasitic infections among children are one of the most important social health problems commonly encountered in developing countries especially like India. A few of the studies earlier conducted the prevalence of parasitic infections in different settings like tertiary health care hospital and schools children in Pondicherry, but our present study focused the prevalence of parasitic infections in rural and urban communities with special attention to both intestinal protozoa and helminthes, with our knowledge this study serve as first study conducted in Pondicherry communities, which help the primary healthcare professionals and family physicians to get adequately knowledge about the significance of high burden of intestinal parasitic infection.
A total of 1006 samples was studies and the overall prevalence of intestinal parasites in the stool samples among the rural and urban study population was found to be 40.4% in rural and 20.3% in urban which is similar to the overall India prevalence rate, which is similar to a study done in prevalence of intestinal parasites in rural southern part of India was carried out by Kang G et al.[2]
Among the stool samples showing protozoal infections, Giardia intestinalis, Blastocystis spp and Entamoeba spp showed high prevalence of 54% than the helminthic infections A. lumbricoides, and hookworm which was 5.5% and nematode H. nana which was 0.9% which is similar to a study done by Fernandez MC et al. 2002.[5]
In this study, male showed higher prevalence rate of parasites in their stool samples when compared to female, which have been observed in similar studies R. Saraswathi et al.[11] Despite the fact that, the risk of intestinal parasitic infection does not depend on the gender, our study showed a notable predominance pattern in males, this could be probably males are more exposure to the environment factors.
The prevalence of intestinal parasites in the stool samples collected from rural population is 40.4% where as it is 91% in a similar study done by Fernandez et al.[5] On the contrary the prevalence of infection in urban population is 20.3% whereas, it is 33% in the study done of Fernandez et al.[5] This shows that there is great reduction in the overall parasitic infection rate among rural population and mild reduction of infection rate among urban population. But in our study finding the prevalence of intestinal parasites have been observed in similar studies N. Mareeswaran et al. 2018.[12]
The stool samples showing the parasites such as of A. lumbricoides (1%), H. nana (0%), A. duodenale (2.8%), is less when compared to the study done Fernandez et al.[5] which shows 53% of Ascaris, 37.6% of Ancylostoma among the rural population. But the stool samples showing Entamoeba is more (6.6%) and Giardia (21.2%) when compared to the study done (Fernandez) showing 4%. and 16% This suggests that there is poor sanitary condition and possibility of recent faecal contamination in the drinking water.
In this study, the samples from the urban population did not show any Ascaris lumbricoides infestation and the samples from the rural population did not show any H. nana, when compared to Fernandez et al. which shows a prevalence of 52.8% and 1.01% respectively, this signifies that the protection against Ascaris lumbricoides and H. nana were excellent in the urban and rural population. The stool samples showing Giardia intestinalis was more (21.2%) from rural and 10.4% from the urban in this study and it's showing similar prevalence when compared to a study done by Fernandez et al. and Nitin s et al. showing 22%.[5,13]
The limitation of the current study was that examination of a single stool specimen from each participant is not adequate and the methods were not very sensitive. Triple faeces test could have increased the frequency of the parasitic occurrence to some folds compared to that of a single sample. One study done in CMC Vellore by Kang G et al. where they used three stool samples for each participant, this may be appropriate when there is manifest gastrointestinal symptom, it may be inadequate when intensity of infection is low in the case of asymptomatic carrier participant, this would help and gave a clear picture of the prevalence burden of intestinal parasitic infections.[2]
Conclusion
The outcomes of this study will help the primary healthcare professionals and family physicians to get adequately knowledge about the significance of high burden of intestinal parasitic infection. The overall prevalence in rural population is comparatively higher than the urban population, hence necessary interventions like improving the sanitary conditions, periodic de-worming, mass screening, awareness creation programs and the public should be educated regarding faecal contamination of water and necessity of drinking boiled water, personal and environment hygienic practices. These measures will help in bringing down the prevalence of intestinal parasitic infection, which could directly improve the overall health and well-being of both the individual and the community.
Financial support and sponsorship
The study was supported by Intramural Research Grant from Jawaharlal Institute of Postgraduate Medical Education and Research (JIPMER), Puducherry, India. The authors would like to acknowledge and thanks the staff nurses, Lab assistants both RHC and UHC, Anganwadi workers of both the rural and urban for their immense help in data collection and helping for the samples collection and special thanks to Dr. Hari Kishan Raju. K and Dr. P. Jambulingam, Director, Vector Control Research Centre (VCRC), ICMR, Pondicherry for their help in reproduced geographic map using the Esri ArcMap 10.2.1 software and support to carry out this study.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Sadeghi H, Borji H. A survey of intestinal parasites in a population in Qazvin, north of Iran. Asian Pac J Trop Dis. 5:231–3. [Google Scholar]
- 2.Kang G, Mathew MS, Rajan DP, Daniel JD, Mathan MM, Mathan VI, et al. Prevalence of intestinal parasites in rural Southern Indians. Trop Med Int Health. 1998;3:70–5. doi: 10.1046/j.1365-3156.1998.00175.x. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization. Prevention and Control of Intestinal Parasitic Infections. Geneva: WHO; 2002. [Google Scholar]
- 4.CDC, DPDx. Laboratory Identification of parasite of Public Health Concern. Atlanta: Centre for Disease Control and Prevention, USA; 2006. [Google Scholar]
- 5.Fernandez MC, Verghese S, Bhuvaneswari R, Elizabeth SJ, Mathew T, Anitha A, et al. A comparative study of the intestinal parasites prevalent among children living in rural and urban settings in and around Chennai. J Comm Dis. 2002;34:35–9. [PubMed] [Google Scholar]
- 6.Dhanabal J, Selvadoss PP, Muthuswamy K. Comparative study of the prevalence of intestinal parasites in low socioeconomic areas from South Chennai, India. J Parasitol Res. 2014:630968. doi: 10.1155/2014/630968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Parija SC, Rao RS. Prevalence of parasitic infections in Pondicherry. Indian J Parasitol. 11:63–5. [Google Scholar]
- 8.Ragunathan L, Kalivaradhan SK, Ramadass S, Nagaraj M, Ramesh K. Helminthic infections in school children in Puducherry, South India. J Microbiol Immunol Infect. 43:228–32. doi: 10.1016/S1684-1182(10)60036-9. [DOI] [PubMed] [Google Scholar]
- 9.Manochitra K, Padukone S, Selvaratthinam PA, Parija SC. Prevalence of intestinal parasites among patients attending a tertiary care centre in South India. Int J Curr Microbiol App Sci. 2016;5:190–7. [Google Scholar]
- 10.Allen AVH, Ridley DS. Further observations on the formol-ether concentration technique for faecal parasites. J Clin Pathol. 23:545–7. doi: 10.1136/jcp.23.6.545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Saraswathi R, Lalithambigai J, Vazhavandal G, Uma A, Prabhusaran N, Velayutharaj A. Prevalence of intestinal parasitic pathogens in stools from medical speciality units of tertiary rural teaching hospital, Tamilnadu, India. Int J Curr Microbiol App Sci. 2016;5:429–35. [Google Scholar]
- 12.Mareeswaran N, Savitha AK, Gopalakrishnan S. Prevalence of intestinal parasites among urban and rural population in Kancheepuram district of Tamil Nadu. Int J Community Med Public Health. 2018;5:2585–9. [Google Scholar]
- 13.Nitin S, Venkatesh V, Husain N, Masood J, Agarwal GG. Overview of intestinal parasitic prevalence in rural and urban population in Lucknow, north India. J Commun Dis. 2007;39:217–23. [PubMed] [Google Scholar]



