Abstract
Introduction:
Newborn vaccination is an integral part of routine immunization program in India, but program implementation gaps exist. The focus of this article is to identify and describe an implementation strategy which could improve the newborn vaccination at the facility level.
Materials and Methods:
A situation analysis was conducted through a mixed-methods approach to identify the lacunae in the health system and the same was used to develop an implementation strategy to improve newborn vaccination coverage across the six priority states.
Results:
Issues in stewardship and human resource, vaccine-related stock-outs, and poor service delivery were some of the reasons for low facility-level vaccination coverage. After implementation of a health system–based strategy, the new born vaccination improved from 55% to 88% across 10 quarters of program implementation. Factors such as sensitization of stakeholders, vaccination on holidays, rigorous documentation, and supportive supervision of health staff were primary reasons for improvement in service delivery.
Conclusion:
Importance of newborn immunization at birth is well established. The results from six states prove that “health systems approach” as an implementation strategy is a viable tool to improve newborn immunization at birth.
Keywords: Health systems approach, newborn vaccination, public health facilities
Introduction
Vaccination is a proven and one of the most cost-effective child survival interventions.[1] Over the years, significant gains have been made in global immunization coverage, but it has stagnated to around 85% in the past few years; as per the World Health Organization (WHO) estimates, an additional 1.5 million child deaths can be prevented annually if immunization coverage improves.[2] Immunization services are provided free of cost in India through the public healthcare delivery system and include both immunization and outreach session sites and birth doses at public healthcare facilities.[3]
Bacillus Calmette–Guerin (BCG), oral polio vaccine (OPV), and hepatitis B are the three vaccines which need to be administered to a newborn as per the National Immunization Schedule (NIS) in India. While hepatitis B vaccine should be given at birth or as early as possible within 24 h, the OPV birth dose can be given till 15 days of age and the BCG vaccine can be given till 1 year of age, but it is important to give the said vaccines to as close to the time of birth as possible.[4]
Immunization at birth not only prevents the child from the three deadly diseases but also facilitates early registration in health records and parent sensitization resulting in timely follow-up for routine immunization. Moreover, WHO has identified timely delivery of birth dose of hepatitis B vaccine as an important parameter for evaluating the overall performance of immunization programs.[5]
In 2015, the global coverage of one dose of hepatitis B vaccine to newborns within 24 h of birth was just 39% globally and 29% for South East Asia of which India is a part.[6] The global coverage of hepatitis B birth dose improved slightly to 43% by 2017.[2]
Available data thus suggest that the healthcare delivery system needs to prioritize newborn vaccination to optimize coverage and utilization of the three vaccines. With this background, this article attempts to present a health systems approach to identify and address systemic bottlenecks present across six different states in India with regard to vaccination at birth.
Aims of the Intervention
The current intervention aims to understand various issues and challenges in improving coverage of vaccination at birth in public health facilities and describe a systems-based approach to solve these challenges.
Materials and Methods
Ethics
The intervention was implemented as part of the VRIDDHI project that provided technomanagerial support to the Ministry of Health and Family Welfare, Government of India, and state governments. The data presented here came from routine care delivery processes at the facilities and did not require any additional data source. For competency measurement at baseline, we obtained written consent from the care providers. For endline assessment, approval was obtained from the Center for Operations Research and Training IRB (No. EC-CORT/1730). Written consent forms were obtained for observation of deliveries and competency measurement of staff.
Intervention design
The implementation exercise uses a before- and after-study design and tracks the progress on vaccination coverage in 141 intervention facilities.
Intervention setting and population
The intervention was undertaken as part of VRIDDHI, a project funded by USAID, which is providing technical support for scale up of RMNCH+A interventions across 26 poorly performing districts designated as high-priority districts of six states of Delhi, Punjab, Haryana, Himachal Pradesh, Jharkhand, and Uttarakhand in India. The project had prioritized improving quality of care (QOC) at the time of birth through an integrated “Care around Birth” approach.[7]
Guided by WHO's “Quality of Care (QoC)” framework[8] for maternal and newborn health and the national RMNCH+A strategy, the “Care around Birth” approach is premised around the effective implementation of evidence-based technical interventions during intrapartum and immediate postpartum period – the most critical time for maternal and newborn survival. The current intervention was focused at 141 high-delivery case load public health facilities spread across priority districts across the six states outlined in Table 1.
Table 1.
Delivery points across 26 HPDs
| State | Selected HPDs | No. of delivery points |
|---|---|---|
| Delhi | North-west and north-east | 8 |
| Haryana | Mewat, Palwal, Jind, Panipat, Hisar | 31 |
| Punjab | Gurdaspur, Muktasar, Barnala, Sangrur, Mansa | 25 |
| Himachal Pradesh | Chamba, Mandi, Kinnaur, Lahaul Spiti | 17 |
| Uttarakhand | Haridwar, Tehri Garhwal, Pauri Garhwal | 18 |
| Jharkhand | Lohargada, Gumla, Simdega, Godda, Dumka, Sahibganj, and Saraikela-Kharsawan | 42 |
HPD: High-priority district
Methods
A mixed-methods approach was adopted, and at the outset, a situational analysis was undertaken at intervention facilities and key health managers at both district and state levels were interviewed to identify the bottlenecks in providing birth immunization at these facilities. The interview findings were supplemented with field notes and observation of documentation practices at the said facilities. A comprehensive project Management Information System (MIS) was also devised to capture important indicators of newborn immunization at birth across time from each facility. The findings from qualitative methods were subjected to thematic analysis with focus on health system functions, and summary of issues was documented accordingly. Between October 2015 and March 2018, that is, ten quarters of the intervention, a total of 517,913 deliveries and 511,622 live births were followed to assess newborn vaccination coverage rates.
Adopting health systems approach
WHO, in its report of 2000 on Health System Performance, had identified three generic goals and four generic functions of all health systems.[9] It had emphasized that the aim of any health system is to maximize the attainment of the goals conditioned by contextual factors from outside the system that influence the level of goal attainment that can be reached. A simplified depiction of the framework is shown in Figure 1.[10]
Figure 1.
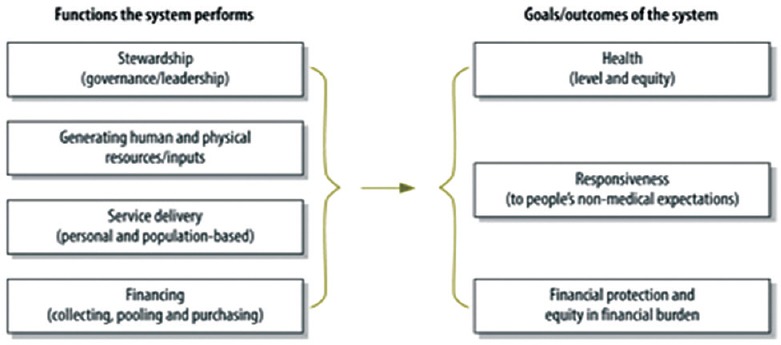
Relationship between functions and outcome of the health system
The framework describes four key health system functions, that is, stewardship, human and physical resources, service delivery, and finance. Stewardship has been defined as “the careful and responsible management of the well-being of the population,” and in the most general terms as “the very essence of good government.” Function of stewardship mainly relates to establishing and managing appropriate health information system, steering role of policy makers, program managers, leadership, and governance to make sound decisions.[11,12] The resource generation function of WHO framework points out that to perform efficiently health systems requires the combination of many properly balanced physical and technical resource inputs.[13,14] The service delivery function of the WHO framework refers to the combination of inputs into a production process that takes place in a particular organizational setting and that leads to the delivery of a series of interventions.[13]
This framework was used to analyze the qualitative data from interviews, field notes, and observation of facility-level processes. The issues and challenges were coded and grouped in the themes related to health systems components based on this framework. Using the same framework, the solutions to address these challenges were developed and put into practice during the intervention period as outlined in the results below.
Results
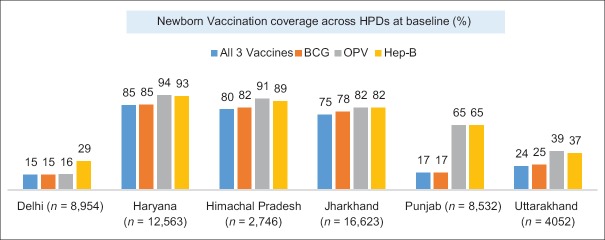
The baseline assessment of the facilities (October–December 2015) reported the coverage rates across the six states for newborn immunization for all the three antigens to be 55%. Within the states, it varied from 15% in Uttarakhand to 84% in Haryana. Among the different antigens, BCG and OPV had the lowest coverage rate of 15% and 16%, respectively, while Hepatitis B was at 29%. Another important point to note was that states of Haryana, Himachal Pradesh, and Jharkhand were comparatively better off when compared with the other three [Figure 2].
Figure 2.
Newborn vaccine coverage across high-priority districts at baseline
Prevailing challenges at public health facilities
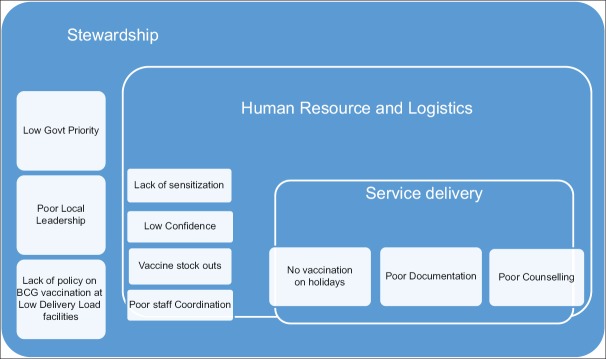
Some of the prevailing challenges and bottlenecks that were attributed to low vaccination coverage rates voiced by the facility head and staff were categorized into three themes illustrated below [Figure 3].
Figure 3.
Prevailing issues for low newborn vaccination at the facility level
Stewardship issues
The issues under this function related broadly to the lack of policy clarity at low-delivery facilities about BCG as at such facilities BCG vaccination was often avoided due to high wastage factor, poor local leadership, and low government priority accorded to vaccination of neonates before discharge.
Human resource and logistics issues
The issues under this function pertained to poor staff sensitization especially staff nurses and Auxillary Nurse Midwife (ANM) who were not aware about its importance, low confidence about intradermal injection required for BCG vaccine, and poor coordination among the staff.
Service delivery issues
Some of the issues identified in this functional area were missed vaccination on holidays, poor or no counseling at the time of service delivery, and poor documentation.
Strategic implementation framework for improving newborn immunization
Looking at the existing challenges, an interventional approach was framed adopting a four-pronged strategy which was primarily based on the “health systems approach” to overcome the systemic issues with locally relevant solutions [Figure 4].
Figure 4.
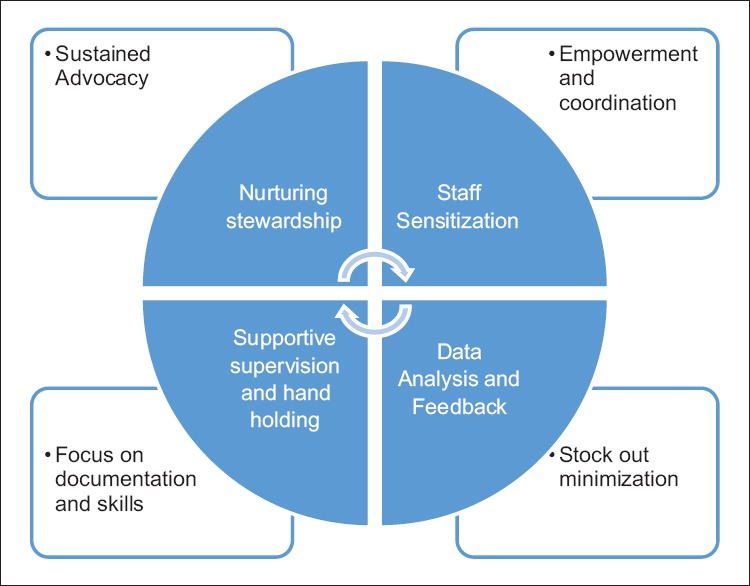
Strategic implementation framework for improving newborn immunization
Nurturing stewardship
To bring in a responsive health system, the intervention focused on nurturing programmatic stewardship at all levels through sustained advocacy and regular evidence-based feedbacks.
Staff sensitization
Staff sensitization was an important aspect which was required to ensure the availability of trained human resource. Vaccine hesitancy in parents is a major challenge for public health experts which can be mitigated by proper patient–provider interaction.[15,16,17] Taking cognizant of this fact, the ANMs involved in immunization services and other staff posted in labor rooms were adequately sensitized using a structured training package.
Supportive supervision and hand-holding
Supportive supervision is one of the methods which can ensure quality service delivery by providing technical consultations.[18,19] Regular supportive supervision visits to the facilities by the project staff provided an opportunity to hand-hold the health workers in not only building their skills and confidence but also ensuring proper documentation and record updating.
Data analysis and feedback
The district health staff was trained and empowered to use regular analysis of the facility data to identify facilities with frequent stock-outs and supply chain issues. They were also trained to identify facilities performing poorly despite the absence of such issues. The feedback thus generated was shared periodically at all levels and was also used in the district- and state-level review meetings.
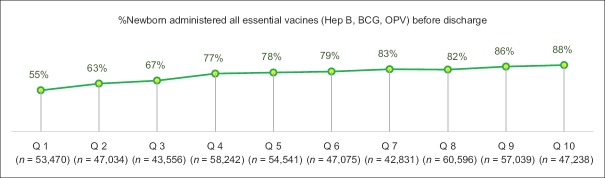
Improved outcomes
Positive outcomes in newborn immunization rates were observed in all six states because of the interventions done. As visible from Figure 5, with every quarter, new born vaccination administered at the facility level before discharge improved steadily from 55% to 88% across 10 quarters of strategic interventions.
Figure 5.
Percentage of newborn administered with all essential birth doses
Intervention resulted in increment in hepatitis B and OPV coverage across the six states to 94% and 96%, respectively, and BCG coverage to 89% [Tables 2-4]. The results confirm that the high levels of newborn vaccination were achieved and sustained over the intervention period.
Table 2.
Percentage of newborn given hepatitis B birth dose
| Hepatitis B | Qrt 1 | Qrt 2 | Qrt 3 | Qrt 4 | Qrt 5 | Qrt 6 | Qrt 7 | Qrt 8 | Qrt 9 | Qrt 10 |
|---|---|---|---|---|---|---|---|---|---|---|
| Oct 15-Dec 15 | Jan 16-Mar 16 | Apr 16-Jun 16 | Jul 16-Sep 16 | Oct 16-Dec 16 | Jan 17-Mar 17 | Apr 17-Jun 17 | Jul 17-Sep 17 | Oct 17-Dec 18 | Jan 18-Mar 18 | |
| Delhi | 29% | 19% | 36% | 92% | 94% | 90% | 90% | 81% | 92% | 94% |
| Haryana | 93% | 95% | 94% | 88% | 88% | 91% | 90% | 92% | 94% | 94% |
| Himachal | 89% | 98% | 98% | 99% | 98% | 99% | 97% | 98% | 99% | 98% |
| Jharkhand | 82% | 86% | 90% | 91% | 93% | 92% | 89% | 88% | 90% | 92% |
| Punjab | 65% | 100% | 98% | 97% | 89% | 86% | 94% | 96% | 98% | 97% |
| Uttarakhand | 37% | 64% | 69% | 77% | 72% | 78% | 89% | 91% | 86% | 93% |
| Six states’ avg. | 70% | 77% | 81% | 91% | 90% | 89% | 91% | 90% | 93% | 94% |
Table 4.
Percentage newborn given BCG birth dose
| BCG | Qrt 1 | Qrt 2 | Qrt 3 | Qrt 4 | Qrt 5 | Qrt 6 | Qrt 7 | Qrt 8 | Qrt 9 | Qrt 10 |
|---|---|---|---|---|---|---|---|---|---|---|
| Oct 15-Dec 15 | Jan 16-Mar 16 | Apr 16-Jun 16 | Jul 16-Sep 16 | Oct 16-Dec 16 | Jan 17-Mar 17 | Apr 17-Jun 17 | Jul 17-Sep 17 | Oct 17-Dec 18 | Jan 18-Mar 18 | |
| Delhi | 15% | 17% | 34% | 90% | 94% | 92% | 87% | 92% | 91% | 98% |
| Haryana | 85% | 87% | 83% | 80% | 83% | 88% | 89% | 91% | 94% | 93% |
| Himachal | 82% | 90% | 91% | 94% | 94% | 95% | 95% | 97% | 99% | 98% |
| Jharkhand | 78% | 83% | 85% | 85% | 82% | 83% | 82% | 82% | 83% | 81% |
| Punjab | 17% | 56% | 56% | 60% | 64% | 64% | 78% | 84% | 88% | 88% |
| Uttarakhand | 25% | 43% | 52% | 59% | 68% | 67% | 73% | 70% | 67% | 80% |
| Six states’ avg. | 56% | 65% | 69% | 79% | 81% | 82% | 84% | 86% | 88% | 89% |
BCG: Bacillus Calmette-Guerin
Table 3.
Percentage newborn given OPV birth dose
| OPV | Qrt 1 | Qrt 2 | Qrt 3 | Qrt 4 | Qrt 5 | Qrt 6 | Qrt 7 | Qrt 8 | Qrt 9 | Qrt 10 |
|---|---|---|---|---|---|---|---|---|---|---|
| Oct 15-Dec 15 | Jan 16-Mar 16 | Apr 16-Jun 16 | Jul 16-Sep 16 | Oct 16-Dec 16 | Jan 17-Mar 17 | Apr 17-Jun 17 | Jul 17-Sep 17 | Oct 17-Dec 18 | Jan 18-Mar 18 | |
| Delhi | 16% | 19% | 36% | 88% | 94% | 94% | 93% | 106% | 91% | 100% |
| Haryana | 94% | 96% | 91% | 88% | 89% | 90% | 91% | 94% | 95% | 95% |
| Himachal | 91% | 97% | 98% | 99% | 99% | 98% | 97% | 98% | 99% | 98% |
| Jharkhand | 82% | 88% | 89% | 86% | 88% | 91% | 89% | 87% | 89% | 92% |
| Punjab | 65% | 100% | 98% | 97% | 89% | 87% | 94% | 96% | 98% | 97% |
| Uttarakhand | 39% | 61% | 68% | 78% | 85% | 84% | 94% | 93% | 87% | 95% |
| Six states’ avg. | 68% | 77% | 80% | 89% | 90% | 90% | 92% | 94% | 93% | 96% |
OPV: oral polio vaccine
Discussion
With current intervention, the states of Delhi, Uttarakhand, and Punjab have shown remarkable improvement in all the three birth doses’ coverage. Immunization on government holidays and Sundays had been a major bottleneck which was attended to in nearly all facilities across all states. The states of Delhi and Punjab were facing issues of poor documentation and record-keeping practices along with laxity on the part of staff to administer the birth doses of the vaccine within 24 h. In Uttarakhand and Himachal Pradesh, the primary issue was lack of proper vaccine storage and geographical access. Here, the vaccine carriers were used at the facility level near labor rooms to store vaccines, and vaccination to every newborn within 24 h of birth in the facility was ensured. In Jharkhand and Haryana, coordination between the labor staff and ANMs providing immunization services was strengthened which led to a healthy increase in newborn vaccination.
Many earlier studies closely corroborate with learnings identified in the current intervention and have identified factors relating to supply and procurement of vaccines, knowledge and motivation of healthcare workers, and monitoring and supervision of programs with effective management and cooperation between the involved staff as areas to improve vaccine coverage at facility level.[20,21] In yet another study, unavailability of vaccines, limited vaccination hours, lack of institutional mechanisms to deliver vaccine at birth, and absence of proper documentation were found to be important factors hindering vaccination at birth.[22] A study from Patiala concluded that improving parental awareness, better coordination between immunization and maternal health staff, improved communication, and clear delineation of responsibility and answerability in the immunization service delivery can have a good impact on vaccination of newborns. The same study also concluded that the modification in the delivery of immunization service from twice a week to daily has had a good impact on the vaccination of newborns.[23]
An assessment of hepatitis B vaccination too had concluded that poor stock management (“stock-outs or nil stocks” at various levels), incomplete recording and reporting, perceived costly vaccine and related fear of wastage of vaccine in 10 dose vial, and incomplete knowledge among health functionaries about vaccination schedule were the main reasons for poor coverage of hepatitis vaccine in the study area.[24] A recent study advocates cross-sectoral systems strengthening strategy to improve vaccination outcomes.[25] Another study from Philippines found that only 22% of children were vaccinated within 24 h of delivery and noted that availability of a copy of hepatitis B vaccination policy and providing trainings to health workers was associated with increased coverage with birth dose.[26] Another study from Haryana recommends equitable resource allocation to tackle supply side gaps in providing immunization services.[27]
Learnings for implementation science
Health systems strengthening framework of WHO has been advocated for overall system improvement which can enable improvement in various types of service delivery provisions. However, adapting a health systems approach to achieve coverage and quality improvements in specific components of health service delivery has not been explicitly used. This large-scale experience of improving vaccination coverage with adaptation of a systems approach suggests that implementation of programs that have a specific intervention focus can be substantially helped with such an approach. While this experience does not use an established theory to discuss the learnings for implementation science, a consolidated framework of implementation research (CFIR)[28] comes closest to the health systems approach used here. At both the stages – understanding the barriers of and designing solutions to improve vaccination coverage – a variety of constructs were considered. The intervention used constructs related to the five major domains of CFIR – intervention characteristics (newborn vaccination at birth is an evidenced-based intervention and part of NIS), outer setting (availability of vaccination resources and supplies), inner setting (improving stewardship and culture), characteristics of the individuals involved (knowledge, skills, and motivation of service providers), and the process of implementation (improvement steps, tracking the change, and reviews). The experience further builds on the idea that often there are multiple factors and their interactions that act as barriers for service delivery coverage and quality, and hence the solution applied needs to use holistic methods for improvement.[29] Health systems approach thus provides a clear and simpler way to address similar implementation problems and can be researched further for its utility as an improvement model under the field of implementation science.
Conclusion
Strengthening facility service delivery using health systems–based approach is not a new concept and has been advocated by many experts before.[30] This approach helps in understanding the issues in a comprehensive manner and ensures that attention is not diverted just to a specific aspect. The health systems approach thereby ensures that any improvement in the immunization services is likely to contribute to the strengthening of other maternal and child health services as well. Cross learning of best practices, nurturing stewardship at the highest level, and focusing on micro-level contextually relevant solutions are important considerations requiring appropriate action. However, implementation and sustainability of desired impact over time requires timely policy reforms and an internal driven system control and strengthening mechanism which are backed by evidence-based operational guidelines and strong support from the highest level.
Financial support and sponsorship
This work was made possible by the support of the American people through the United States Agency for International Development and its VRIDDHI (scaling up RMNCH+A Interventions) Project, implemented by IPE Global Ltd. under the terms of Cooperative Agreement Number AID 386 A 14 00001. The contents of this article represent the views of the authors and do not necessarily reflect the views of USAID.
Conflicts of interest
There are no conflicts of interest.
References
- 1.State of the World's Vaccines and Immunization. 3rd ed. Geneva, Switzerland: WHO; 2009. [Google Scholar]
- 2.Immunization coverage: Fact sheet. World Health Organization. [Last accessed on 2019 Feb 17]. Available from: http://www.who.int/en/news-room/fact-sheets/detail/immunization-coverage .
- 3.Mathew JL. Evidence-based options to improve routine immunization. Vaccine. 2009;95:4. [PubMed] [Google Scholar]
- 4.Immunization Handbook for Medical Officers. [Last accessed on 2019 Feb 17]. pp. 15–19. Available from: http://nihfw.org/pdf/nchrc-publications/immunihandbook.pdf .
- 5.WHO. Hepatitis B. [Last accessed on 2019 Feb 17]. Available from: http://apps.who.int/iris/bitstream/10665/255841/1/WER9227.pdf?ua=1 .
- 6.World Health Organization. Global routine vaccination coverage 2014. [Last accessed on 2019 Feb 17];Wkly Epidemiol Rec. 2015 46:617–32. Available from: http://www.who.int/wer/2015/wer9046.pdf . [Google Scholar]
- 7.Vriddhi: Scaling up RMNCH+A Interventions. [Last accessed on 2019 Feb 17]. Available from: http://rmncha.in/project-interventions/care-around-birth/
- 8.Tunçalp Ö, Were WM, MacLennan C, Oladapo OT, Gülmezoglu AM, Bahl R, et al. Quality of care for pregnant women and newborns – The WHO vision. BJOG. 2015;122:1045–9. doi: 10.1111/1471-0528.13451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.The World Health Report 2000: Health Systems: Improving Performance. Geneva, Switzerland: 2000. [Last accessed on 2019 Feb 17]. p. 215. Available from: http://www.who.int/whr/2000/en/whr00_en.pdf?ua=1 . [Google Scholar]
- 10.Duran A, Kutzin J, Martin-Moreno JM, Travis P. Understanding health systems: Scope, functions and objectives. In: Figueras J, McKee M, editors. Health Systems, Health, Wealth and Societal Well-being: Assessing the Case for Investing in Health Systems. Berkshire, UK: Open University Press; 2011. pp. 19–36. [Google Scholar]
- 11.Saltman RB, Davis OF. The concept of stewardship in health policy. Bull World Health Organ. 2000;78:732–9. [PMC free article] [PubMed] [Google Scholar]
- 12.Kapoor N, Kumar D, Thakur N. Core attributes of stewardship; foundation of sound health system? Int J Health Policy Manag. 2014;3:5–6. doi: 10.15171/ijhpm.2014.52. doi: 10.15171/IJHPM.2014.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Adams O, Shengelia B, Goubarev A, Issakov A, Kwankam SY, Stilwell B, et al. Human, Physical and Intellectual Resource Generation – Proposals for Monitoring. WHO. Evidence and Information for Policy Cluster (EIP) Discussion Paper Series. 2002; WHO/EIP/OSD/DP 02.49 [Google Scholar]
- 14.Murray Christopher JL, Frenk JA. WHO Framework for Health System Performance Assessment. Geneva, Switzerland: WHO, Global Programme on Evidence for Health Policy; 1999. [Last accessed on 2019 Feb 17]. p. 29. Available from: http://www.who.int/iris/handle/10665/66267 . [Google Scholar]
- 15.Kumar D, Chandra R, Mathur M, Samdariya S, Kapoor N. Vaccine hesitancy: Understanding better to address better? Israel J Health Policy Res. 2016;5:2. doi: 10.1186/s13584-016-0062-y. doi: 10.1186/s13584-016-0062-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.World Health Organization. Meeting of the SAGE on immunization – Conclusions and recommendations, 2014. [Last accessed on 2019 Feb 17];Wkly Epidemiol Rec. 2014 50:561–76. Available from: http://www.who.int/wer/2014/wer8950.pdf?ua=1 . [Google Scholar]
- 17.Dasgupta P, Bhattacherjee S, Mukherjee A, Dasgupta S. Vaccine hesitancy for childhood vaccinations in slum areas of Siliguri, India. Indian J Public Health. 2018;62:253–8. doi: 10.4103/ijph.IJPH_397_17. [DOI] [PubMed] [Google Scholar]
- 18.Som M, Panda B, Pati S, Nallala S, Anasuya A, Chauhan AS, et al. Effect of supportive supervision on routine immunization service delivery – A randomized post-test study in Odisha. Glob J Health Sci. 2014;6:61–7. doi: 10.5539/gjhs.v6n6p61. doi: 10.5539/gjhs.v6n6p61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Babu G, Singh V, Nandy S, Jana S. Supportive supervision and immunization coverage: Evidence from India. Int J Epidemiol. 2010:9. [Google Scholar]
- 20.Wang S, Smith H, Peng Z, Xu B, Wang W. Increasing coverage of hepatitis B vaccination in China: A systematic review of interventions and implementation experiences. Medicine (Baltimore) 2016;95:e3693. doi: 10.1097/MD.0000000000003693. doi: 10.1097/MD.0000000000003693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Guan X, Qi Q, Yang C, et al. Analysis of the project effect on MOH/GAVI increasing the coverage rate of timely – Birth dose hepatitis B vaccine in the remote minority areas in Sichuan Province (Chinese) Chin J Vaccines Immun. 2011. pp. 540–4. Available from: http://en.cnki.com.cn/Article_en/CJFDTotal-ZGJM201106019.htm .
- 22.Taneja G, Mentey VK, Jain M, Sagar KS, Tripathi B, Favin M, et al. Institutionalizing early vaccination of newborns delivered at government health facilities: Experiences from India? Int J Med Res Rev. 2015;3:521–7. doi: 10.17511/ijmrr.2015.i5.089. [Google Scholar]
- 23.Oberoi S, Amarjit S, Avneet R, Neha C, Patnaik S. Positive impact of rescheduling Bacillus Calmette-Guerin vaccinations at birth. J Fam Community Med. 2017;24:13–7. doi: 10.4103/2230-8229.197176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lahariya C, Subramanya BP, Sosler S. An assessment of hepatitis B vaccine introduction in India: Lessons for roll out and scale up of new vaccines in immunization programs. Indian J Public Health. 2013;57:8–14. doi: 10.4103/0019-557X.111357. [DOI] [PubMed] [Google Scholar]
- 25.Gurnani V, Haldar P, Aggarwal MK, Das MK, Chauhan A, Murray J, et al. Improving vaccination coverage in India: Lessons from Intensified Mission Indradhanush, a cross-sectoral systems strengthening strategy. BMJ. 2018;363:k4782. doi: 10.1136/bmj.k4782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sobel HL, Mantaring JB 3rd, Cuevas F, Ducusin JV, Thorley M, Hennessey KA, et al. Implementing a national policy for hepatitis B birth dose vaccination in Philippines: Lessons for improved delivery. Vaccine. 2011;29:941–5. doi: 10.1016/j.vaccine.2010.11.047. [DOI] [PubMed] [Google Scholar]
- 27.Prinja S, Monga D, Rana SK, Sharma A, Dalpath S, Bahuguna P, et al. District Level Analysis of Routine Immunization in Haryana State: Implications for Mission Indradhanush under Universal Immunization Programme. Indian journal of community medicine: Official publication of Indian Association of Preventive & Social Medicine. 2018;43:209–14. doi: 10.4103/ijcm.IJCM_306_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: A consolidated framework for advancing implementation science. Implement Sci. 2009;4:50. doi: 10.1186/1748-5908-4-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bauer MS, Damschroder L, Hagedorn H, Smith J, Kilbourne AM. An introduction to implementation science for the non-specialist. BMC Psychol. 2015;3:32. doi: 10.1186/s40359-015-0089-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lahariya C. “Health system approach” for improving immunization program performance? J Family Med Prim Care. 2015;4:487–94. doi: 10.4103/2249-4863.174263. doi:10.4103/2249-4863.174263. [DOI] [PMC free article] [PubMed] [Google Scholar]