Summary
Background
Low-income and middle-income countries (LMICs) face major challenges in achieving the UN's Sustainable Development Goals (SDGs) for vulnerable adolescents. We aimed to test the UN Development Programme's proposed approach of development accelerators—provisions that lead to progress across multiple SDGs—and synergies between accelerators on achieving SDG-aligned targets in a highly vulnerable group of adolescents in South Africa.
Methods
We did standardised interviews and extracted longitudinal data from clinical records at baseline (2014–15) and 18-month follow-up (2016–17) for adolescents aged 10–19 years living with HIV in the Eastern Cape province of South Africa. We used standardised tools to measure 11 SDG-aligned targets—antiretroviral therapy adherence, good mental health, no substance use, HIV care retention, school enrolment, school progression, no sexual abuse, no high-risk sex, no violence perpetration, no community violence, and no emotional or physical abuse. We also assessed receipt at both baseline and follow-up of six hypothesised development accelerators—government cash transfers to households, safe schools (ie, without teacher or student violence), free schools, parenting support, free school meals, and support groups. Associations of all provisions with SDG-aligned targets were assessed jointly in a multivariate path model, controlling for baseline outcomes and sociodemographic and HIV-related covariates, and adjusted for multiple outcome testing. Cumulative effects were tested by marginal effects modelling.
Findings
1063 (90%) of 1176 eligible adolescents were interviewed. Three provisions were shown to be development accelerators. Parenting support was associated with good mental health (odds ratio 2·13, 95% CI 1·43–3·15, p<0·0001), no high-risk sex (2·44, 1·45–5·03, p=0·005), no violence perpetration (2·59, 1·63–4·59, p<0·0001), no community violence (2·43, 1·65–3·86, p<0·0001), and no emotional or physical abuse (2·38, 1·65–3·76; p<0·0001). Cash transfers were associated with HIV care retention (1·87, 1·15–3·02, p=0·010), school progression (2·05, 1·33–3·24, p=0·003), and no emotional or physical abuse (1·76, 1·12–3·02, p=0·025). Safe schools were associated with good mental health (1·74, 1·30–2·34, p<0·0001), school progression (1·57, 1·17–2·13, p=0·004), no violence perpetration (2·02, 1·45–2·91, p<0·0001), no community violence (1·81, 1·30–2·55, p<0·0001), and no emotional or physical abuse (2·20, 1·58–3·17, p<0·0001). For five of 11 SDG-aligned targets, a combination of two or more accelerators showed cumulative positive associations, suggesting accelerator synergies of combination provisions. For example, the fitted probability of adolescents reporting no emotional or physical abuse (SDG 16.2) with no safe schools, cash transfers, or parenting support was 0·25 (0·16–0·34). With cash transfer alone it was 0·37 (0·33–0·42), with safe school alone 0·42 (0·30–0·55), and with parenting support alone 0·44 (0·30–0·59). With all three development accelerators combined, the probability of adolescents reporting no emotional or physical abuse was 0·76 (0·67–0·84). After correcting for multiple tests, four of the SDG-aligned targets (antiretroviral therapy adherence, no substance use, school enrolment, and no sexual abuse) were not associated with any hypothesised accelerators.
Interpretation
The findings suggest the UN's accelerator approach for this high-risk adolescent population has policy and potential financing usefulness. Services that simultaneously promote several SDG targets, or combine to support particular targets, might be important to meet not only health-related targets, but also to ensure that adolescents in LMICs thrive within a new development framework.
Funding
Nuffield Foundation, UK Research and Innovation Global Challenges Research Fund, UKAID, Janssen Pharmaceutica, International AIDS Society, John Fell Fund, European Research Council, Economic and Social Research Council, Philip Leverhulme Trust, and UNICEF.
Introduction
Africa's adolescents are the world's fastest-growing population: rising from 229 million in 2015 to a projected 435 million by 2050.1 The region's future success will depend on attaining the Sustainable Development Goals (SDGs) for this group. Africa's youth possess immense dynamism, creativity, and promise—adolescence is a sociobiological window of opportunity, with a second spurt of physical and brain development alongside a major transition to adult life trajectories.2 With effective investments now in adolescent human capital, the demographic dividend from this population could be US$500 billion per year—a third of regional gross domestic product—for the next 30 years.3
Research in context.
Evidence before this study
Accelerators are a UN development system approach for interventions that can lead to progress across multiple Sustainable Development Goals (SDG) and dimensions of development (social, economic, and environmental). We searched PubMed, the Public Library of Science, and Google scholar, as well as UN reports and UN programmatic publications for any quantitative studies with the keywords “development accelerators” (published between Jan 1, 2014, and July 31, 2018) with no language restrictions, but identified no known studies assessing this approach. While studies have examined whether access to SDG-aligned provisions (such as employment) are associated with single outcomes (such as HIV mortality), they have not explicitly tested for combinations of provisions that affect multiple SDG targets and goals.
Added value of this study
This study corroborated a novel solution to a major global development challenge. It showed that, for a highly vulnerable group of adolescents living with HIV in South Africa, development accelerators have positive associations across the targets of several SDGs that include and reach beyond health. Moreover, combinations of accelerators are associated with synergies of increased breadth and depth, yielding more substantive effects across a wider range of SDG-aligned targets.
Implications of all the available evidence
As UN agencies work with low-income and middle-income countries to achieve the SDGs in local contexts, this study provides important supporting evidence for strategic interventions. The identification of locally effective development accelerators can contribute to multiple SDG goals and targets, even for the highest-risk children and adolescents.
However, adolescents in the region face acute barriers, such as poor services, inadequate provision, and fractured infrastructure. More than half of them live within conflict, or political or economic instability.4 For many, multiple vulnerabilities exacerbate each other. Research has led to major advances in addressing defined problems through stand-alone programmes (eg, intimate partner violence prevention or school success),5 but a new approach might be required to achieve the multidimensional and mutually reinforcing SDGs.6
The UN Development Programme (UNDP) has spearheaded UN support for countries in identifying development accelerators, within the UN Sustainable Development Group's mainstreaming, acceleration, and policy support approach.7 At the highest level, these accelerators identify the actions benefiting the three domains of sustainable development: economic, social, and environmental. Accelerators encompass key interventions, provisions, services, or programmatic areas (such as social protection or tobacco control) that simultaneously make positive impact across multiple SDGs or targets in a given context.8 This model has yet to be comprehensively and empirically tested. There might also be synergistic effects of combining provisions. For example, in South Africa, adolescents receiving both government cash transfers and parenting support had greater outcomes across more SDG goals than those receiving either alone.9
The challenge is to identify which interventions act as accelerators in different contexts, and which combinations enhance efficacy. Therefore, we aimed to test this model of development accelerators within the social and economic domains of sustainable development in a group disproportionately left behind in the SDGs: adolescents living with HIV. We identified possible accelerators in two stages: first, we had a year of consultation with the African Union, UN agencies, donors, and sub-Saharan African governments (May, 2017, to April, 2018); and second, we reviewed the scientific literature for quantitative or qualitative evidence suggesting possible effects across multiple SDG domains. We hypothesised six accelerators, expected to be similarly effective across different contexts while maintaining commonalities (information on the specific agencies that identified these accelerators is in the appendix). Free schooling shows increases in adolescent enrolment, with follow-on benefits such as sexual health.10 Cash transfers show good evidence among African adolescents for sexual and mental health, and initial evidence for reduced violence.11 Safety within school settings is associated with better mental health, school retention, and possibly with improved school performance.12 Access to an HIV support group has been suggested, in mainly qualitative evidence, to improve retention in HIV care, and sexual and mental health.13 There is evidence of improved enrolment and educational functioning with free school meals.14 Parenting support is associated with reduced adolescent sexual risk, substance use, and violence perpetration, although evidence is primarily from high-income countries.15
We also aimed to test the model of accelerator synergies by which accelerators might provide more substantial effects through their multiple associations with particular SDG-aligned targets and across a wider range of SDG-aligned targets—ie, to increase depth and breadth through an integrated strategy.
Methods
Study design and participants
We did standardised interviews and extracted prospective data from clinical records at baseline (2014–15) and 18-month follow-up (2016–17) from adolescents aged 10–19 years living with HIV in the Eastern Cape province of South Africa. The study was established as the region's first large-scale community-traced cohort of this group, tracking not only clinical outcomes, but also social, educational, familial, sexual health, and community experiences. The province is characterised by high morbidity, low human development, and poor infrastructure. In a district comprising rural, urban, and periurban settlements, we identified all 52 primary clinics, hospitals, and community health centres providing HIV treatment to adolescents. In each facility, all files (paper and computer) were reviewed to identify all individuals aged 10–19 years who had ever initiated HIV treatment. To include those lost to follow-up as well as those retained in care, adolescents were traced to 180 communities and interviewed at home or a location of their choice. At 18 months post baseline, all adolescents who had given consent to be re-approached were asked for consent for follow-up. Because of migration, participants lived in six provinces at follow-up: Eastern Cape, Free State, Gauteng, KwaZulu-Natal, North-West, and Western Cape.
Ethical approval was given by the University of Cape Town (Cape Town, South Africa; CSSR 2013/4), Oxford University (Oxford, UK; CUREC2/12-21), Provincial Departments of Health and Education, and all participating health-care facilities. All adolescents and their primary caregivers gave written informed consent at both timepoints in their language of choice (Xhosa or English), which was also read aloud in cases of low literacy. There were no financial incentives, but the study's adolescent advisory group recommended a certificate, snack, and small gift pack including soap and pencils. These were provided to all adolescents, regardless of interview completion.
To avoid unintended disclosure of HIV status or HIV-associated stigma, we presented the research focus as general adolescent health and social needs, and 456 neighbouring adolescents were additionally interviewed (not included in analyses). Confidentiality was maintained except in cases of risk of harm. For individuals who had been abused or raped, or showed suicidal planning or behaviour or untreated severe illness (eg, symptomatic tuberculosis), researchers made immediate health and social service referrals with follow-up support.
Procedures
Adolescent clinical records were reviewed, and research staff supported participants to complete tablet-based questionnaires in the language of their choice, lasting 60–90 min. Input to questionnaire design was provided by an adolescent advisory group; the South African National Departments of Health, Social Development, Basic Education and National AIDS Council; UNICEF, PEPFAR-USAID, and local non-governmental organisations. Pre-piloting was done locally with 25 adolescents living with HIV.
Given that the study was initiated before 2015, we retrospectively identified 11 adolescent outcomes that were aligned to (or proxies for) specific targets within four SDGs: antiretroviral therapy adherence in the past week, good mental health, no substance abuse, HIV care retention, school enrolment, school progression, no sexual abuse, no high-risk sex, no violence perpetration, no community violence, and no emotional or physical abuse (table 1). Identification of alignment was undertaken in consultation with UNDP, UNICEF, and UNAIDS, followed by literature review to check for possible effects across development domains. All were measured at baseline and 18-month follow-up.
Table 1.
SDG targets, definitions, and scales used in this analysis
| Operationalised measure in this study | Measure | Instrument | ||
|---|---|---|---|---|
| 3.3: End the epidemic of AIDS | Antiretroviral therapy adherence in the past week | Self-reported >85% adherence to antiretroviral therapy in the past week (including weekend) | Patient Medication Adherence Questionnaire; self-report validated using viral failure measured in clinical records, defined as undetectable most recent viral load (within 1 year of study follow-up) <50 copies per mL | |
| 3.4: Promote mental health | Good mental health | No symptoms of depression (past 2 weeks), anxiety (past 1 month), or post-traumatic stress (past 1 month) | Child Depression Inventory − Short Form (α=0·59), Revised Children's Manifest Anxiety Scale (α=0·79),16 Short-form Child PTSD Checklist (α=0·89)17 | |
| 3.5: Prevention of substance use | No substance abuse | No self-reported past-month use of alcohol or drugs, or visiting a tavern or shebeen* | Child Behavior Checklist,18 WHO Global School-based Health Survey19 | |
| 3.8: Access to essential health-care services | HIV care retention | Past-year retention in HIV care, with no missed clinic appointments or medication collections in the past year in self-report or clinic files | Self-reported clinic attendance and medication collection, clinic patient files | |
| 4.1: All girls and boys complete primary and secondary education | School enrolment† | Self-reported school enrolment | Based on Census South Africa measures of school enrolment | |
| 4.4: Increase relevant skills for employment | School progression | Self-reported passed last school grade and able to concentrate in school during past 6 months | Attention scale (α=0·65) of Strengths and Difficulties Questionnaire20 | |
| 5.2: Eliminate sexual exploitation | No sexual abuse | Self-reported no sexual abuse, defined as any lifetime (at baseline) and past-year (at follow-up) contact sexual abuse or forced sex | Juvenile Victimization Questionnaire,21 Intimate partner violence items from HTPN068 study in South Africa22 | |
| 5.6: Universal access to sexual and reproductive health | No high-risk sex | Self-reported no past-year unprotected sex, multiple concurrent sexual partnerships, or casual or age-disparate partnerships | South African National Survey of HIV and Risk Behavior23 | |
| 16.1: Reduce all forms of violence and related deaths | ||||
| 16.1a: No violence perpetration | No violence perpetration | Self-reported no involvement in perpetration of violent or acquisitive crime | Child Behaviour Checklist24 items for assault, theft, and added items for gang membership and carrying weapons | |
| 16.1b: No community violence | No community violence | Self-reported no past-year witnessing of shootings, stabbings, or being physically attacked in the neighbourhood | Child Exposure to Community Violence checklist25 | |
| 16.2: End violence against children | No emotional or physical abuse | Self-reported no past-year physical or emotional abuse victimisation | UNICEF Measures for National-level Monitoring of Orphans and Vulnerable Children26 | |
SDG=Sustainable Development Goal. PTSD=post-traumatic stress disorder. α=internal reliability of each scale in this sample.
Informal bar or club.
Still relevant for older youths in the Eastern Cape, where more than two-thirds of final-year students are older than 18 years.
Following evidence that provisions need to be sustained and predictable to benefit adolescents, we assessed receipt of real-world government and community services with high external validity as access at both baseline and follow-up for six hypothesised accelerators (ie, provisions that are positively associated with adolescent outcomes across three or more SDGs). (1) Free school, measured as either a no-fees school or an individual school fees exemption. (2) Government cash transfer, measured using items based on South Africa's census as household receipt of any of child support grant, foster child grant, pension, disability, or care dependency grant. (3) Safe school, measured as no past-year physical violence by teachers or students, using the Social and Health Assessment.26 (4) Access to a support group, measured as regular monthly attendance of a youth-focused or general support group (either HIV-specific or non-specific) in the community or clinic. (5) Free school meals, measured using items drafted with the National Department of Basic Education as provision of either lunch or breakfast at school every day. (6) A high level of parenting support, measured as consistently high parental monitoring using this subscale of the Alabama Parenting Questionnaire.27
Covariates included nine sociodemographic and HIV-related cofactors, all measured at baseline: age (dichotomised as 10–14 or 15–19 years); sex; urban or rural residence; housing (formal or informal shack housing); maternal orphanhood and paternal orphanhood, both measured using items based on South Africa's Census; mode of infection (vertical or horizontal) assessed using clinical files, date of antiretroviral therapy initiation, and parental HIV status;28 general health, self-reported using the WHO International Classification of Functioning, Disability and Health checklist (past 6 months);29 and poverty, measured as access to eight highest socially perceived necessities for children in the nationally representative South African Social Attitudes Survey (enough food, money for school fees, to see a doctor when needed, school uniform, basic clothing, soap, school books, and shoes).30
Statistical analysis
Analysis took place in six steps in SPSS, STATA, and MPlus. The first three steps were to assess frequencies, sample representativeness, and reliability of outcome measures. In step 1, eligible participants included in the study were compared with those excluded for sociodemographic characteristics that were available for both groups (age, sex, and urban or rural location) using χ2 tests (reported in text). Next, participants who were retained and not retained at follow-up were compared on all variables used in this study. In step 2, frequencies for all SDG-aligned targets, hypothesised accelerator provisions, and covariates were reported. In step 3, self-reported antiretroviral therapy adherence was validated in a multivariable logistic regression against undetectable viral load, controlling for all nine covariates. In step 4, we tested for associations of hypothesised development accelerators with SDG-aligned targets by doing a multivariate path analysis in MPlus that applied the remaining five provisions and nine covariates to all the outcomes simultaneously; two of the 45 paths had to be removed because a sparse and an empty cell prevented model fit. In step 5 we controlled for test multiplicity using the Benjamini-Hochberg method, checking for associations between predictors and outcomes for a false-positive rate of 0·1. We also checked for collinearity. In step 6, we tested for possible cumulative effects between the development accelerators that emerged, using marginal effects models with each combination of the accelerators, holding significant covariates at mean values, and providing probabilities and 95% CIs.
Role of the funding source
The funders of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. LDC had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Results
At baseline, 1063 (90%) of 1176 eligible adolescents aged 10–19 years identified in patient files were interviewed. Health and social service referrals with follow-up support were made for 145 (14%) individuals, and 69 (6%) individuals were not retained at follow-up. 48 (4%) refused participation (adolescent or caregiver), ten (<1%) had cognitive delay too severe to understand consent procedures, 42 (4%) were untraceable, and 13 (1%) had migrated beyond the study area. 20 (2%) were recorded in clinic files as alive, but had actually died. At follow-up, 994 (94%) adolescents re-consented and were re-interviewed. Between baseline and follow-up, 14 (1%) adolescents had died. Comparisons between included and excluded samples showed no differences on baseline age, sex, or urban or rural location. There were three differences at baseline between those retained and not retained at follow-up: those retained were on average 10 months younger and lived in rural areas, with higher rates of maternal orphanhood (table 2).
Table 2.
Sociodemographic factors, hypothesised accelerator provisions, and SDG-aligned targets at baseline and follow-up
|
Baseline |
Follow-up |
||||
|---|---|---|---|---|---|
| Retained (n=994) | Not retained (n=69) | p value* | Retained (n=994) | ||
| Sociodemographic characteristics | |||||
| Age (years) | 13·78 (2·83) | 14·67 (3·03) | 0·012 | 15·35 (2·92) | |
| Age ≥15 years | 369 (37%) | 33 (48%) | 0·076 | 561 (56%) | |
| Sex | |||||
| Female | 549 (55%) | 38 (55%) | 0·98 | 549 (55%) | |
| Male | 445 (45%) | 31 (45%) | .. | 445 (45%) | |
| Rural location† | 266 (27%) | 10 (14%) | 0·024 | 244 (24%) | |
| Informal housing‡ | 186 (19%) | 13 (19%) | 0·98 | 146 (15%) | |
| No poverty | 319 (32%) | 26 (38%) | 0·34 | 220 (22%) | |
| Maternal orphanhood | 446 (45%) | 19 (28%) | 0·0050 | 460 (46%) | |
| Paternal orphanhood | 297 (30%) | 24 (35%) | 0·39 | 333 (34%) | |
| Poor health | 59 (6%) | 3 (4%) | 0·59 | 41 (4%) | |
| HIV acquired via horizontal transmission§ | 216 (23%) | 16 (25%) | 0·64 | 216 (23%) | |
| Hypothesised accelerators | |||||
| Free school | 292 (29%) | 16 (23%) | 0·27 | 221 (22%)¶ | |
| Safe school | 402 (40%) | 23 (33%) | 0·24 | 300 (30%)¶ | |
| Free school meals | 817 (82%) | 52 (75%) | 0·16 | 585 (59%)¶ | |
| Cash transfer | 942 (95%) | 64 (93%) | 0·47 | 879 (88%)¶ | |
| Parenting support | 341 (34%) | 18 (26%) | 0·16 | 161 (16%)¶ | |
| HIV support group | 44 (4%) | 0 | 0·074 | 44 (4%)¶ | |
| SDG-aligned target indicators‖ | |||||
| 3.3: Antiretroviral therapy adherence in the past week | 635 (64%) | 38 (55%) | 0·14 | 489 (49%) | |
| 3.4: No mental health issues | 145 (15%) | 9 (13%) | 0·73 | 367 (37%) | |
| 3.5: No substance abuse | 832 (84%) | 58 (84%) | 0·94 | 812 (82%) | |
| 3.8: Retention in care | 778 (78%) | 48 (70%) | 0·093 | 743 (75%) | |
| 4.1: Enrolled at school | 937 (94%) | 62 (90%) | 0·14 | 881 (89%) | |
| 4.4: School progression | 165 (17%) | 13 (19%) | 0·63 | 430 (43%) | |
| 5.2: No sexual abuse | 903 (91%) | 64 (93%) | 0·59 | 842 (85%) | |
| 5.6: No high-risk sex | 756 (76%) | 47 (68%) | 0·14 | 680 (68%) | |
| 16.1a: No violence perpetration | 561 (56%) | 35 (51%) | 0·36 | 718 (72%) | |
| 16.1b: No community violence | 399 (40%) | 22 (32%) | 0·17 | 561 (56%) | |
| 16.2: No emotional or physical abuse | 543 (55%) | 38 (55%) | 0·94 | 458 (46%) | |
Data are mean (SD) or n (%). SDG=Sustainable Development Goal.
Two-sample t tests for continuous variables and Pearson's χ2 tests for categorical variables.
n=992 among retained participants, due to missing values.
n=993 among retained participants, due to missing values.
n=960 among retained participants, due to missing values, n=60 among non-retained participants, due to missing values.
Access to hypothesised accelerator at both baseline and follow-up.
Variables were operationalised as described in table 1.
Missing data was less than 1%, except for viral load measures. Rates of reaching SDG-aligned targets, access to hypothesised development accelerators, and covariates are in table 2. Only 44 (4%) of adolescents reported any support group attendance, therefore this factor was excluded from the analysis due to low sample size. 521 (49%) patients' medical records included a viral load measure taken within 1 year of the outcome measure. Within those, self-reported adherence was associated with a viral load less than 50 copies per mL (odds ratio 1·65, 95% CI 1·11–2·44, p=0·013) independent of all nine covariates (appendix).
Table 3 shows the results of the overall multivariate path model spanning the remaining five provisions and 11 SDG-aligned targets, simultaneously controlling for nine covariates and the outcomes at baseline (the saturated model was sustained for comparability across outcomes). Associations among the five provisions were small (all Spearman's correlation coefficients ≤0·018), indicating no collinearity (table 4). After correcting for multiple comparisons, three of the provisions were deemed to be development accelerators (table 3). Parenting support was associated with good mental health (SDG 3.4), no high-risk sex (SDG 5.6), no violence perpetration, no community violence, and no emotional or physical abuse (SDG 16.1a, 16.1b, and 16.2, respectively). Government cash transfers were associated with HIV care retention (SDG 3.8), school progression (SDG 4.4), and no emotional or physical abuse (SDG 16.2). Safe schools were associated with good mental health (SDG 3.4), school progression (SDG 4.4), no violence perpetration, no community violence, and no emotional or physical abuse (SDG 16.1a, 16.1b, and 16.2, respectively). Free school meals were associated with positive effects across two targets within two goals—HIV care retention (SDG 3.8) and no emotional or physical abuse (SDG 16.2). After correcting for multiple comparisons, four of the SDG-aligned targets—antiretroviral therapy adherence (SDG 3.3), no substance abuse (SDG 3.5), school enrolment (SDG 4.1), and no sexual abuse (SDG 5.2)— were not associated with any hypothesised accelerators (table 3). In all, the three accelerators provided associations across seven SDG-aligned targets spanning four goals.
Table 3.
Multivariate path analysis of associations between accelerator provisions and SDG-aligned targets
| 3.3: Antiretroviral therapy adherence in the past week | 3.4: No mental health issues | 3.5: No substance abuse | 3.8: HIV care retention | 4.1: Enrolled at school | 4.4: School progression | 5.2: No sexual abuse | 5.6: No high-risk sex | 16.1a: No violence perpetration | 16.1b: No community violence | 16.2: No emotional or physical abuse | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Hypothesised accelerators | |||||||||||
| Free school | 0·85 (0·62–1·19; 0·33) | 0·88 (0·60–1·23; 0·48) | 1·18 (0·67–2·05; 0·56) | 1·41 (0·99–2·20; 0·090) | NA* | 1·44 (1·02–2·01; 0·034) | 0·90 (0·54–1·61; 0·71) | 0·84 (0·53–1·33; 0·44) | 1·73 (1·16–2·66; 0·010) | 0·87 (0·61–1·20; 0·40) | 0·93 (0·63–1·34; 0·71) |
| Safe school | 1·28 (0·95–1·77; 0·11) | 1·74 (1·30–2·34; <0·0001) | 1·35 (0·88–2·13; 0·20) | 1·37 (0·98–2·05; 0·094) | 0·94 (0·55–1·61; 0·81) | 1·57 (1·17–2·13; 0·004) | 1·15 (0·73–1·93; 0·57) | 0·84 (0·58–1·20; 0·36) | 2·02 (1·45–2·91; <0·0001) | 1·81 (1·30–2·55; <0·0001) | 2·20 (1·58–3·17; <0·0001) |
| Free school meals | 1·22 (0·94–1·64; 0·15) | 1·26 (0·94–1·71; 0·13) | 1·32 (0·86–2·10; 0·20) | 1·60 (1·16–2·20; 0·005) | 1·51 (0·90–2·53; 0·12) | 0·67 (0·49–0·88; 0·006) | 1·30 (0·86–1·98; 0·22) | 1·36 (0·96–1·93; 0·095) | 0·85 (0·61–1·15; 0·32) | 1·38 (1·05–1·84; 0·029)† | 1·41 (1·04–1·94; 0·031) |
| Cash transfer | 1·34 (0·86–2·08; 0·21) | 1·10 (0·69–1·76; 0·70) | 1·53 (0·90–2·57; 0·12) | 1·87 (1·15–3·02; 0·010) | 1·71 (0·91–3·21; 0·097) | 2·05 (1·33–3·24; 0·003) | 2·00 (1·13–3·59; 0·016)† | 1·49 (0·94–2·42; 0·095) | 1·47 (0·92–2·28; 0·093) | 0·63 (0·39–0·94; 0·039)† | 1·76 (1·12–3·02; 0·025) |
| Parenting support | 1·23 (0·86–1·75; 0·25) | 2·13 (1·43–3·15; <0·0001) | NA* | 1·28 (0·83–2·22; 0·32) | 3·99 (0·90–17·64; 0·068) | 1·31 (0·88–1·99; 0·19) | 2·65 (1·27–12·92; 0·29) | 2·44 (1·45–5·03; 0·005) | 2·59 (1·63–4·59; <0·0001) | 2·43 (1·65–3·86; <0·0001) | 2·38 (1·65–3·76; <0·0001) |
| Covariates | |||||||||||
| Outcome at baseline | 1·41 (1·05–1·89; 0·020) | 1·03 (0·70–1·51; 0·90) | 2·51 (1·62–4·26; <0·0001) | 1·82 (1·22–2·61; 0·002) | NA* | 0·85 (0·58–1·20; 0·41) | 2·82 (1·05–7·32; 0·036) | 2·28 (1·52–3·54; <0·0001) | 1·49 (1·11–2·02; 0·011) | 1·15 (0·88–1·58; 0·36) | 5·93 (4·53–8·41; <0·0001) |
| Age ≥15 years | 1·32 (0·93–1·84; 0·12) | 0·64 (0·44–0·90; 0·012) | 0·20 (0·12–0·32; <0·0001) | 1·27 (0·83–1·98; 0·27) | 0·16 (0·08–0·32; <0·0001) | 0·60 (0·42–0·83; 0·004) | 0·39 (0·23–0·62; <0·0001) | 0·21 (0·13–0·30; <0·0001) | 0·75 (0·52–1·09; 0·13) | 0·80 (0·56–1·10; 0·19) | 1·06 (0·72–1·56; 0·78) |
| Female | 1·28 (0·97–1·68; 0·077) | 0·82 (0·60–1·07; 0·19) | 1·31 (0·85–2·12; 0·22) | 1·07 (0·77–1·45; 0·69) | 0·42 (0·23–0·74; 0·003) | 1·17 (0·88–1·57; 0·29) | 0·71 (0·45–1·09; 0·11) | 0·98 (0·67–1·38; 0·89) | 1·14 (0·85–1·59; 0·42) | 1·34 (1·01–1·80; 0·046) | 0·97 (0·72–1·32; 0·87) |
| Rural location | 1·18 (0·88–1·61; 0·29) | 2·18 (1·61–3·00; <0·0001) | 0·78 (0·49–1·25; 0·31) | 1·18 (0·83–1·79; 0·41) | 0·82 (0·46–1·45; 0·50) | 0·97 (0·71–1·37; 0·87) | 0·89 (0·54–1·45; 0·63) | 1·64 (1·11–2·55; 0·020) | 1·21 (0·84–1·76; 0·32) | 1·62 (1·19–2·27; 0·003) | 1·62 (1·15–2·29; 0·006) |
| Informal housing | 0·74 (0·51–1·08; 0·10) | 0·69 (0·47–1·01; 0·058) | 1·86 (1·10–3·48; 0·036) | 0·99 (0·67–1·57; 0·98) | 0·90 (0·49–1·68; 0·75) | 1·13 (0·81–1·64; 0·50) | 1·21 (0·71–2·20; 0·52) | 1·32 (0·85–2·20; 0·23) | 0·92 (0·60–1·41; 0·72) | 1·12 (0·77–1·63; 0·54) | 0·70 (0·45–1·03; 0·085) |
| No poverty | 0·99 (0·73–1·32; 0·93) | 1·14 (0·83–1·54; 0·41) | 1·14 (0·72–1·82; 0·58) | 1·31 (0·92–1·92; 0·15) | 2·23 (1·20–4·17; 0·012) | 1·15 (0·86–1·53; 0·34) | 1·14 (0·73–1·93; 0·59) | 1·10 (0·72–1·63; 0·64) | 0·85 (0·62–1·17; 0·33) | 1·13 (0·85–1·55; 0·43) | 1·27 (0·92–1·77; 0·14) |
| Maternal orphanhood | 1·14 (0·87–1·53; 0·35) | 0·91 (0·69–1·22; 0·52) | 0·88 (0·58–1·36; 0·55) | 1·29 (0·94–1·80; 0·13) | 1·11 (0·66–1·89; 0·69) | 0·69 (0·51–0·89; 0·007) | 0·86 (0·55–1·37; 0·52) | 0·95 (0·65–1·36; 0·80) | 0·82 (0·59–1·13; 0·23) | 1·20 (0·91–1·63; 0·23) | 0·76 (0·56–1·02; 0·081) |
| Paternal orphanhood | 0·90 (0·66–1·20; 0·52) | 1·06 (0·76–1·46; 0·72) | 0·88 (0·56–1·35; 0·59) | 1·08 (0·76–1·54; 0·68) | 0·65 (0·39–1·09; 0·10) | 1·39 (1·05–1·90; 0·035) | 1·01 (0·66–1·65; 0·98) | 1·11 (0·76–1·64; 0·61) | 1·08 (0·79–1·54; 0·64) | 1·00 (0·74–1·34; 1·00) | 1·02 (0·70–1·39; 0·92) |
| Poor health | 0·92 (0·48–1·65; 0·77) | 0·78 (0·38–1·43; 0·47) | 1·53 (0·73–4·12; 0·33) | 1·32 (0·69–2·99; 0·45) | 0·56 (0·24–1·32; 0·18) | 0·89 (0·46–1·61; 0·72) | 1·52 (0·75–4·73; 0·38) | 0·86 (0·37–2·14; 0·73) | 1·44 (0·75–3·16; 0·33) | 1·47 (0·79–2·80; 0·23) | 0·94 (0·47–1·80; 0·86) |
| HIV acquired via horizontal transmission | 0·73 (0·48–1·08; 0·12) | 1·38 (0·94–2·04; 0·12) | 0·40 (0·24–0·64; <0·0001) | 0·91 (0·58–1·47; 0·69) | 0·22 (0·12–0·38; <0·0001) | 0·66 (0·43–1·01; 0·050) | 0·49 (0·28–0·79; 0·007) | 0·36 (0·22–0·56; <0·0001) | 0·89 (0·58–1·33; 0·57) | 0·93 (0·63–1·36; 0·72) | 1·16 (0·73–1·81; 0·53) |
SDG=Sustainable Development Goal. NA=not applicable. Data are adjusted odds ratios (95% CI; p value). Analyses done in MPlus, which only provides p values to three decimal places. Variables were operationalised as described in table 1.
These three paths had to be removed because of empty or very sparse cells (respondents not enrolled at school do not receive free school, only five respondents with strong parenting support abused alcohol or drugs, and only two respondents re-enrolled in school at follow-up).
The Benjamini-Hochberg procedure was applied to control for false discovery rate, which resulted in the re-classification of these accelerators as incorrect rejections of the null hypothesis.
Table 4.
Bivariate correlations between predictor variables*
| Free school | Safe school | Free school meals | Cash transfer | Parenting support | |
|---|---|---|---|---|---|
| Free school | 1·00 | .. | .. | .. | .. |
| Safe school | −0·006 (−0·018 to 0·007; 0·36) | 1·00 | .. | .. | .. |
| Free school meals | 0·002 (−0·018 to 0·015; 0·74) | 0·018 (0·003 to 0·033; 0·014) | 1·00 | .. | .. |
| Cash transfer | 0·002 (0·006 to 0·010; 0·67) | 0·002 (−0·007 to 0·011; 0·65) | 0·016 (−0·007 to 0·026; 0·001) | 1·00 | .. |
| Parenting support | 0·010 (0·002 to 0·021; 0·052) | 0·014 (0·002 to 0·026; 0·017) | 0·014 (0·002 to 0·025; 0·022) | 0·007 (0·000 to 0·013; 0·050) | 1·00 |
Data are Spearman's correlation coefficients (95% CI; p value). Analyses done with MPlus, which only provides p values to three decimal places.
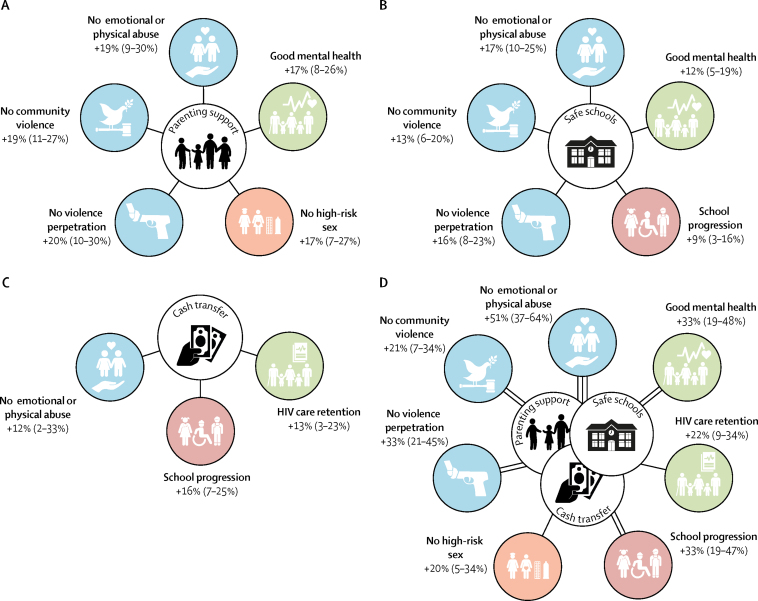
Accelerator synergies were encountered for five of the 11 SDG-aligned targets—good mental health, no high-risk sex, no violence perpetration, no community violence, and no emotional or physical abuse—in that two or more accelerators were associated with a given target and were associated with greater effects when combined. Marginal effects models (table 5) identified the contributions to these targets of the separate accelerator provisions (figure, panels A–C), and also the increased probability of achieving these targets by access to all three accelerators (figure, panel D).
Table 5.
Associations of individual accelerator and combined accelerator synergy provisions with SDG-aligned targets
| 3.3:Antiretroviral therapy adherence in the past week | 3.4: No mental health issues | 3.5: No substance abuse | 3.8: HIV care retention | 4.1: Enrolled at school | 4.4:School progression | 5.2: No sexual abuse | 5.6: No high-risk sex | 16.1a: No violence perpetration | 16.1b: No community violence | 16.2: No emotional or physical abuse | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| No intervention | 0·41 (0·31–0·51) | 0·28 (0·19–0·37) | 0·83 (0·75–0·90) | 0·63 (0·54–0·73) | 0·93 (0·89–0·98) | 0·25 (0·17–0·34) | 0·80 (0·72–0·89) | 0·66 (0·55–0·76) | 0·58 (0·48–0·69) | 0·60 (0·50–0·70) | 0·25 (0·16–0·34) |
| Safe school | 0·47 (0·36–0·58) | 0·40 (0·29–0·52) | 0·86 (0·79–0·93) | 0·70 (0·60–0·81) | 0·93 (0·87–0·98) | 0·35 (0·24–0·46) | 0·83 (0·74–0·91) | 0·61 (0·49–0·74) | 0·74 (0·65–0·83) | 0·72 (0·63–0·82) | 0·42 (0·30–0·55) |
| Cash transfer | 0·48 (0·44–0·53) | 0·30 (0·26–0·34) | 0·88 (0·85–0·91) | 0·76 (0·73–0·80) | 0·96 (0·94–0·98) | 0·41 (0·37–0·45) | 0·89 (0·86–0·92) | 0·74 (0·70–0·78) | 0·67 (0·63–0·72) | 0·48 (0·44–0·53) | 0·37 (0·33–0·42) |
| Parenting support | 0·46 (0·34–0·59) | 0·45 (0·32–0·58) | NA* | 0·69 (0·56–0·81) | 0·98 (0·95–1·01) | 0·31 (0·19–0·42) | 0·92 (0·84–0·99) | 0·82 (0·72–0·93) | 0·78 (0·68–0·89) | 0·78 (0·69–0·88) | 0·44 (0·30–0·59) |
| All accelerators | 0·59 (0·50–0·68) | 0·61 (0·52–0·70) | 0·91 (0·87–0·94) | 0·85 (0·79–0·91) | 0·99 (0·97–1·01) | 0·59 (0·49–0·68) | 0·96 (0·93–0·99) | 0·85 (0·77–0·93) | 0·92 (0·87–0·96) | 0·80 (0·73–0·87) | 0·76 (0·67–0·84) |
Marginal effects models with covariates held at their mean values. Data are fitted probabilities (95% CI). SDG=Sustainable Development Goal. NA=not applicable. Variables were operationalised as described in table 1.
This path was removed because of a very sparse cell (only five respondents with strong parenting support reported alcohol or drug abuse).
Figure.
Modelled effects of development accelerators and synergy effects of all three accelerators
The accelerators identified are parenting support (A), safe schools (B), and cash transfers (C); the modelled effects of synergy between all three accelerators are shown in part D. Data are percentage-point improvements (95% CIs) in percentage probabilities of achieving the Sustainable Development Goal-aligned targets compared with no intervention. Double lines indicate a synergy effect of two accelerators, triple lines indicate a synergy effect of all three accelerators.
Discussion
This study—which focused on an exceptionally vulnerable subpopulation, adolescents living with HIV in Africa—identified three real-world development accelerators for achieving SDG targets in this population: parenting support, government cash transfers, and safe schools, each showing positive associations across targets in three SDGs. Furthermore, it identified accelerator synergies of specific combinations of accelerators showing both depth effects (ie, cumulative positive associations with SDG-aligned targets) and breadth effects (ie, positive associations across a broader range of targets and goals). For example, access to both parenting support and cash transfers is positively associated with seven SDG-aligned targets and four SDG goals measured in this study.
The SDGs present a daunting and exciting agenda to promote holistic adolescent achievement. They challenge countries to meet wide-ranging development needs comprehensively and in combination. They also challenge services to reach the most vulnerable individuals, for whom multiple related vulnerabilities reinforce risks, and who need additional support to reach the same targets as those at lower risk. For LMICs, these new demands occur within constrained revenues and donor-funding streams, as well as differential capacities to deliver quality public services.
Our findings suggest that the UN's new development accelerator approach provides an innovative solution. Each accelerator we studied had evidence of effective and cost-effective programmes in Sub-Saharan Africa, and their combined delivery at scale could enhance adolescent outcomes across development domains.31, 32, 33 By identifying services (or simple combinations of services) associated with synergies across and within SDG goals and targets, governments and donors can maximise positive policy effects. Innovative research on co-financing suggests feasibility of shared funding across government ministries for programmes with cross-cutting effects.34 For intervention science, this calls for a shift from single-focus outcomes to cross-disciplinary priorities within a broader view of human development. A previous cross-sectional study from this dataset examined provisions associated with reducing adolescent mortality risk,35 but does not expand to the cross-SDG set of outcomes that reflects both the new development paradigm and the concerns of populations living with HIV.
This study had several limitations. First, it used quasi-experimental analyses, and development accelerators should be tested in future randomised trials, with provisions and population groups relevant to specific settings, and should include testing of intervention quality and potential harms. However, a strength of this study was the real-world sample of adolescents receiving provisions that already occur (to variable extents) in a resource-constrained South African setting. Of course, such real-world settings also bring variable exposure to different provisions, causing challenges in attributing temporal change to exposures. The second limitation was that eligibility was restricted to adolescents living with HIV who had ever engaged with HIV care, and might therefore have underestimated the level of vulnerability by missing those who had never tested, or who had died before the study start. Third, there might have been even higher vulnerability among the 10% of individuals not included at baseline because of false addresses, severe cognitive delay, or refusal, although community tracing of all adolescents identified in clinical files, including those not engaged in care, provided high inclusion across the spectrum of health-care access. The 69 adolescents not retained at follow-up were largely similar, in terms of demographic characteristics, to those retained on baseline outcomes or access to hypothesised accelerators. Overall, the study is likely to have good generalisability to South African adolescents who have had contact with public HIV care in very-low-resource areas. However, it might not be representative of different ethnic groups, groups using private health care, and those in better-resourced areas. We also noted that the real-world setting meant that several possible accelerators could not be tested because of negligible access or lack of data. These included voluntary savings groups, differentiated HIV care, career advice, and breastfeeding. These limitations highlight the need for further testing of accelerators using birth cohorts and in other settings.
Fourth, outcomes such as abuse and sexual risk are often under-reported, and in very low-resource settings justice, social, and health administrative records are unreliable. We validated self-reported adherence using the gold standard of clinic-recorded viral load, but half of all clinic files reported no viral load within a 2-year period. Rates of viral suppression among untested adolescents are unknown. The absence of associations for sexual abuse and school dropout might reflect low frequencies, and should be tested in larger samples. Fifth, to our knowledge, no prospective adolescent cohorts in LMICs are yet established with exact SDG target indicators. This study used proxies, but could not test all SDG targets and indicators. Future research should further explore opportunities for operationalising SDGs in research.
Sixth, our sample of adolescents already living with HIV limits the capacity to assess the SDG 3.3 target of end the epidemic of AIDS. Strong evidence shows that maintaining antiretroviral therapy adherence and low viral load is essential to ending the epidemic, via reducing infectiveness and preventing AIDS progression.36 However, future research in general populations should also measure access to effective HIV prevention. More broadly, generalisability to other groups is unknown, and there is a clear need to identify accelerators and synergies for other children and adolescents across low and middle income settings.
Seventh, although longitudinal, this study had some overlap of measurement times. All outcomes were measured at follow-up, and controlled for baseline outcome values and covariates, measured 18 months previously. Hypothesised accelerators were measured as stable access from baseline to follow-up, following evidence that consistency of provisions is important in adolescent development. Studies with additional and longer follow-ups will be important to track impacts of accelerators into adulthood.
The strengths of the study include use of prospective cohort data, a sampling strategy that reached more than 90% of a highly vulnerable population, and 94% follow-up. Where we reported benefits associated with receipt of two or more accelerators, the data were from adolescents who accessed these accelerators simultaneously. Our findings will be incorporated into forthcoming UNDP/UNICEF country-level training for mainstreaming, acceleration and policy support (MAPS) for SDG implementation. It is the first empirical test of the UNDP's approach of development accelerators, demonstrating validity even in a high-risk group, and goes further to identify accelerator synergies, whereby access to two or more accelerators is associated with cumulative breadth and depth benefits across SDG-aligned targets. This is the focus of a new large-scale Global Challenges Research Fund (GCRF) initiative the UK GCRF Accelerating Advantage for Africa's Adolescents Hub (ACCELERATE), beginning in March, 2019. The next decade is an important window of opportunity to provide services with cross-SDG benefits: capitalising on political will for a new development agenda, and establishing how adolescent outcomes can improve as the number of young people in Africa reaches half a billion.
The SDGs present not only a development challenge, but also a unique opportunity to improve health and non-health outcomes. This study provides an empirical test of accelerators and their synergies, identifying services that simultaneously promote multifaceted human development goals and that provide a part of the response to the multiple challenges facing those most left behind. Together, they suggest a pathway to reaching the potential of Africa's adolescents as a global demographic dividend.
For full questionnaires see www.mzantsiwakho.co.za
Acknowledgments
Acknowledgments
We thank the adolescents and health-care facilities who participated in this study, the superb Mzantsi Wakho field teams, the Oxford University and University of Cape Town support teams, and Gaelen Pinnock for the graphic design. This project was funded by the Nuffield Foundation [CPF/41513], but the views expressed are those of the authors and not necessarily those of the Foundation. This project was also funded by the UK Research and Innovation Global Challenges Research Fund award [ES/S008101/1]; Evidence for HIV Prevention in Southern Africa, a UKAID programme managed by Mott MacDonald; Janssen Pharmaceutica NV; UNICEF Eastern and Southern Africa Office; and the International AIDS Society through the CIPHER grant (155-Hod; 2018/625-TOS). The views expressed in written materials or publications do not necessarily reflect the official policies of the International AIDS society. Further funding was provided by the Claude Leon Foundation (08 559/C) and Oak Foundation (R46194/AA001). Additional funding was provided by the John Fell Fund (103/757 and 161/033); the University of Oxford's Economic and Social Research Council Impact Acceleration Account (IAA-MT13-003; 1602-KEA-189; K1311-KEA-004); the Leverhulme Trust (PLP-2014-095); Research England; the European Research Council (ERC) under the European Union's (EU) Seventh Framework Programme (FP7/2007-2013)/ERC grant agreement 313421, the EU's Horizon 2020 research and innovation programme/ERC grant agreement 737476); the UK Medical Research Council (MRC) and the UK Department for International Development (DFID) under the MRC/DFID Concordat agreement, and by the Department of Health Social Care through its National Institutes of Health Research (MR/R022372/1|), and the Oxford University Clarendon-Green Templeton College Scholarship.
Contributors
LDC and ET conceptualised the overarching study and led data collection. LDC, FMO, LC, AC, ET, DW, and LS conceptualised the research question. FMO, LDC, LC, and ET did the data analysis. LC and AC compiled the tables. LDC, FMO, LC, AC, ET, DW, and LS interpreted the findings and wrote the paper.
Declaration of interests
LDC reports editorial fees from Taylor and Francis; and grants from the UK Research and Innovation Global Challenges Research Fund, Nuffield Foundation, UKAID and Sweden-Norad, Janssen Pharmaceutica NV and Janssen Pharmaceutica (PTY) LTS South Africa, International AIDS Society, UNICEF Eastern and Southern Africa, John Fell Fund, European Research Council, Philip Leverhulme Trust, and the Economic and Social Research Council. ET reports grants from Evidence for HIV Prevention in Southern Africa (UKAID), the Nuffield Foundation, Janssen Pharmaceutica NV, Janssen Pharmaceutica (South Africa), UNICEF Eastern and South Africa, Higher Education Funding Council for England, Gates Foundation, UK Medical Research Council, European Research Council, and the International AIDS Society (CIPHER grant). DW is an employee of the UN Development Programme. LS reports grants from Sweden/Norad, grants from the US National Institutes of Health, and the UK Medical Research Council; speaking fees from Gilead; and editorial fees from Taylor and Francis. FMO, LC, and AC declare no competing interests.
Supplementary Material
References
- 1.UN DESA . United Nations Secretariat Department of Economic and Social Affairs; New York: 2017. 2017 Revision of World Population Prospects. [Google Scholar]
- 2.Sherr L. Mental health challenges and interventions for adolescents—the first 1,000 weeks. In: Lansford J, Banati P, editors. Handbook of adolescent development research and its impact on global policy. Oxford University Press; Oxford: 2018. [Google Scholar]
- 3.UNFPA . UNFPA; New York: 2014. The power of 1·8 billion: adolescents, youth and the transformation of the future. [Google Scholar]
- 4.World Bank. UNICEF . UNICEF and the World Bank Group; Washington DC: 2016. Ending extreme poverty: a focus on children. [Google Scholar]
- 5.Aber JL, Tubbs C, Torrente C. Promoting children's learning and development in conflict-affected countries: testing change process in the Democratic Republic of the Congo. Dev Psychopathol. 2017;29:53–67. doi: 10.1017/S0954579416001139. [DOI] [PubMed] [Google Scholar]
- 6.Nilsson M, Griggs D, Visbeck M. Policy: map the interactions between Sustainable Development Goals. Nature. 2016;534:320–322. doi: 10.1038/534320a. [DOI] [PubMed] [Google Scholar]
- 7.UN Development Group . United Nations Development Group; New York: 2015. Maps–mainstreaming, acceleration and policy support for the 2030 Agenda. [Google Scholar]
- 8.UN Development Programme. Secretariat of the WHO Framework Convention on Tobacco Control . United Nations Development Programme; New York: 2017. The WHO Framework Convention on Tobacco Control: an accelerator for Sustainable Development. Discussion paper. [Google Scholar]
- 9.Cluver L, Orkin FM, Meinck F, Boyes ME, Yakubovich AR, Sherr L. Can social protection improve sustainable development goals for adolescent health? PLoS One. 2016;11:e0164808. doi: 10.1371/journal.pone.0164808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Psacharopoulos G, Patrinos H. Returns to investment in education: a decennial review of the global literature. Education Economics. 2018;26:445–458. [Google Scholar]
- 11.UNICEF . UNICEF; Florence: 2015. Social cash transfers and children's outcomes: a review of evidence from Africa. [Google Scholar]
- 12.Devries K, Child J, Allen E, Walakira E, Parkes J, Naker D. School violence, mental health, and educational performance in Uganda. Pediatrics. 2013;133:1542. doi: 10.1542/peds.2013-2007. [DOI] [PubMed] [Google Scholar]
- 13.Mark D, Armstrong A, Andrade C. HIV treatment and care services for adolescents: a situational analysis of 218 facilities in 23 sub-Saharan African countries. J Int AIDS Soc. 2017;20(suppl 3):21591. doi: 10.7448/IAS.20.4.21591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jomaa LH, McDonnell E, Probart C. School feeding programs in developing countries: impacts on children's health and educational outcomes. Nutr Rev. 2011;69:83–98. doi: 10.1111/j.1753-4887.2010.00369.x. [DOI] [PubMed] [Google Scholar]
- 15.WHO Global Partnership to End Violence against Children . World Health Organization; Geneva: 2016. INSPIRE: seven strategies for ending violence against children. [Google Scholar]
- 16.Reynolds C, Richmond B. What I think and feel: a revised measure of children's anxiety. J Abnorm Child Psychol. 1978;6:271–280. doi: 10.1007/BF00919131. [DOI] [PubMed] [Google Scholar]
- 17.Amaya-Jackson L, McCarthy G, Cherney MS, Newman E. Duke University Medical Center; Durham: 1995. Child PTSD checklist. [Google Scholar]
- 18.Achenbach T. University of Vermont; Burlington: 1992. Manual for the child behaviour checklist/2-3 and 1992 profile. [Google Scholar]
- 19.Centers for Disease Control and Prevention . Centers for Disease Control and Prevention; Atlanta: 2012. Global school-based student health survey. [Google Scholar]
- 20.Goodman R. The strengths and difficulties questionnaire: a research note. J Child Psychol Psychiatry. 1997;38:581–586. doi: 10.1111/j.1469-7610.1997.tb01545.x. [DOI] [PubMed] [Google Scholar]
- 21.Finkelhor D, Hamby S, Turner H, Ormrod R. Crimes Against Children Research Center; Durham: 2011. The juvenile victimization questionnaire: 2nd revision (JVQ-R2) [Google Scholar]
- 22.Pettifor A, MacPhail C, Hughes JP. The effect of a conditional cash transfer on HIV incidence in young women in rural South Africa (HPTN 068): a phase 3, randomised controlled trial. Lancet Glob Health. 2016;4:e978–e988. doi: 10.1016/S2214-109X(16)30253-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pettifor AE, Rees HV, Steffenson A. Health Systems Trust; Johannesburg: 2005. Reproductive health research unit (University of the Witswatersrand), Lovelife. The national survey of HIV and sexual behaviour among young South Africans. [Google Scholar]
- 24.Martinez P, Richters J. The NIMH community violence project: II. children's distress symptoms associated with violence exposure. Psychiatry. 1993;56:22–35. doi: 10.1080/00332747.1993.11024618. [DOI] [PubMed] [Google Scholar]
- 25.Snider L, Dawes A. UNICEF; Cape Town: 2006. Psychosocial vulnerability and resilience measures for national-level monitoring of orphans and other vulnerable children: recommendations for revision of the UNICEF psychological indicator. [Google Scholar]
- 26.Ruchkin V, Schwab-Stone M, Vermeiren R. Yale University; New Haven: 2004. Social and health assessment (SAHA) psychometric development summary. [Google Scholar]
- 27.Frick P. University of Alabama; Tuscaloosa: 1991. The Alabama parenting questionnaire. [Google Scholar]
- 28.Slogrove AL, Mahy M, Armstrong A, Davies MA. Living and dying to be counted: what we know about the epidemiology of the global adolescent HIV epidemic. J Int AIDS Soc. 2017;20(suppl 3):21520. doi: 10.7448/IAS.20.4.21520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.WHO . World Health Organization; Geneva: 2003. ICF checklist version 2.1a. Clinician Form for international classification of functioning, disability and health. [Google Scholar]
- 30.Pillay U, Roberts B, Rule S. HSRC press; Cape Town: 2006. South African social attitudes: changing times, diverse voices. [Google Scholar]
- 31.Devries KM, Knight L, Child JC. The good school toolkit for reducing physical violence from school staff to primary school students: a cluster-randomised controlled trial in Uganda. Lancet Glob Health. 2015;3:e378–e386. doi: 10.1016/S2214-109X(15)00060-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Greco G, Knight L, Ssekadde W, Namy S, Naker D, Devries K. Economic evaluation of the good school toolkit: an intervention for reducing violence in primary schools in Uganda. BMJ Glob Health. 2018;3:e000526. doi: 10.1136/bmjgh-2017-000526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cluver L, Meinck F, Steinert J. Parenting for lifelong health: a pragmatic cluster randomised controlled trial of a non-commercialised parenting programme for adolescents and their families in South Africa. BMJ Global Health. 2018;3:e000539. doi: 10.1136/bmjgh-2017-000539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Remme M, Vassall A, Lutz B, Luna J, Watts C. Financing structural interventions: going beyond HIV-only value for money assessments. AIDS. 2014;28:425–434. doi: 10.1097/QAD.0000000000000076. [DOI] [PubMed] [Google Scholar]
- 35.Cluver L, Pantelic M, Orkin M, Toska E, Medley S, Sherr L. Sustainable survival for adolescents living with HIV: do SDG-aligned provisions reduce potential mortality risk? J Int AIDS Soc. 2018;21(suppl 1):e25056. doi: 10.1002/jia2.25056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.UNAIDS . Joint United Nations Programme on HIV and AIDS; Geneva: 2018. Miles to go—closing gaps, breaking barriers, righting injustices. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.