Abstract
Context
Advance care planning (ACP) improves alignment between patient preferences for life-sustaining treatment and care received at end of life (EOL).
Objectives
To evaluate implementation of lay navigator-led ACP.
Methods
A convergent, parallel mixed-methods design was employed to evaluate implementation of navigator-led ACP across 12 cancer centers. Data collection included: (1) electronic navigation records, (2) navigator surveys (n=45), (3) claims-based patient outcomes (n=820), and (4) semi-structured navigator interviews (n=26). Outcomes of interest included (1) the number of ACP conversations completed, (2) navigator self-efficacy, (3) patient resource utilization, hospice use, and chemotherapy at EOL, and (4) navigator-perceived barriers and facilitators to ACP.
Results
From 6/1/14–12/31/15, 50 navigators completed Respecting Choices® First Steps ACP Facilitator training. Navigators approached 18% (1319/8704) of patients; 481 completed; 472 in process; 366 declined. Navigators were more likely to approach African American patients than Caucasian patients (20% vs. 14%, p < 0.001). Significant increases in ACP self-efficacy were observed after training. The mean score for feeling prepared to conduct ACP conversations increased from 5.6/10 to 7.5/10 (p<0.001). In comparison to patients declining ACP participation (n=171), decedents in their final 30 days of life who engaged in ACP (n=437) had fewer hospitalizations (46% vs 56%, p=0.02). Key facilitators of successful implementation included physician buy-in, patient readiness and prior ACP experience; barriers included space limitations, identifying the “right” time to start conversations, and personal discomfort discussing EOL.
Conclusion and Relevance
A navigator-led ACP program was feasible and may be associated with lower rates of resource utilization near EOL.
Introduction
In the days to weeks before death, nearly all individuals will experience periods of being unable to make decisions for themselves about their preferred end of life (EOL) care. Professional organizations, including the American Society of Clinical Oncology and the Institute of Medicine, recommend that persons with serious, life-limiting illness engage in advance care planning (ACP).[1, 2] The Patient Self-Determination Act (PDSA) of 1991 requires hospitals to provide patients the opportunity to complete advance directives.[3] ACP is defined by the National Hospice and Palliative Care Organization as “making decisions about the care you would want to receive if you become unable to speak for yourself.”[4] ACP interventions have been shown to increase patient and family satisfaction, reduce caregiver depression and anxiety, and reduce healthcare utilization at the end of life.[5–9] [5, 6, 10–13]
Despite ACP’s demonstrated benefit, widespread institutional implementation remains challenging.[14] For example, 30–38% of cancer patients at EOL do not engage in discussions about EOL care with their physicians.[10, 15] In the SUPPORT study, only 47% of physicians reported knowing their patient’s preferences for cardiopulmonary resuscitation.[16] A national survey found that 90% of individuals believe that it is important to talk about EOL, but only 27% have actually done so.[17] This problem is especially pronounced in the Southeastern US which has a high proportion of African-Americans and a large rural, underserved population, all of whom have been shown to have lower rates of advanced directives and high resource utilization at the EOL.[18, 19]
ACP is time-consuming, which is a significant barrier to successful delivery in the face of competing interests for clinician time and resources.[14] One potential solution to implementing ACP is to delegate the task to lay (non-clinical) patient navigators. Navigators are currently required both for Commission on Cancer certification and for participation in Medicare’s new payment reform project, the Oncology Care Model; thus navigators are increasingly prevalent in US cancer care delivery.[20–22] Patient navigators provide emotional support, information, opportunities for problem solving, and logistical assistance to mitigate or overcome obstacles to health.[22, 23]
In 2012, a lay (non-clinical) navigation program called Patient Care Connect Program (PCCP) was implemented at the University of Alabama at Birmingham (UAB) and 11 affiliate community-based cancer centers in Alabama, Georgia, Florida, Mississippi, and Tennessee as part of a Health Care Innovation Challenge Grant from the Centers for Medicare and Medicaid Innovation. Within this previously described program,[24] navigators did not have nursing or social work backgrounds, although they may have had personal experience with cancer or have been employed in healthcare. The overarching goal of PCCP was to enhance the health of geriatric (age ≥ 65) Medicare patients with cancer through a focus on patient empowerment and by providing an extra layer of support from diagnosis through survivorship and EOL.[24, 25] Navigators within PCCP were trained to facilitate ACP using the Respecting Choices® program.
Respecting Choices®, a nationally recognized ACP program, offers certification programs to prepare individuals in the skills of ACP conversations. This standardized program includes scripted interview tools and communication techniques to engage patients through the process of understanding ACP, exploring personal values, identifying an appropriate healthcare decision-maker, and communicating preferences for EOL care with healthcare agents and healthcare providers.[26] The Respecting Choices® blended curriculum consisted of 6 online educational modules focusing on concepts of effective communication, advance directives and ACP, selection of healthcare agents, and national and local policies related to ACP. This program was selected due to mounting research evidence that the Respecting Choices program is acceptable to patients and impacts hospice use.[26–30] Furthermore, the scripted, standardized nature of the program was appealing for a non-clinical workforce, which may lack the experience and confidence to initiate these conversations independently.
To our knowledge, lay navigators have not been trained to provide ACP, and information is not available on the feasibility, barriers and challenges of this model of delivering ACPs. We hypothesized that lay navigators could be trained to deliver ACP conversation as Respecting Choices® First Steps ACP Facilitators.[31] To examine implementation of navigator-led ACP in the PCC program, we conducted a mixed-methods study to evaluate: (1) number of ACP conversations using electronic navigation records, (2) navigator self-efficacy and site culture using navigator surveys, (3) association between ACP conversation participation and patient EOL utilization outcomes from Medicare claims data, and (4) barriers and facilitators to navigator-led ACP using navigator interviews.
Methods
Design
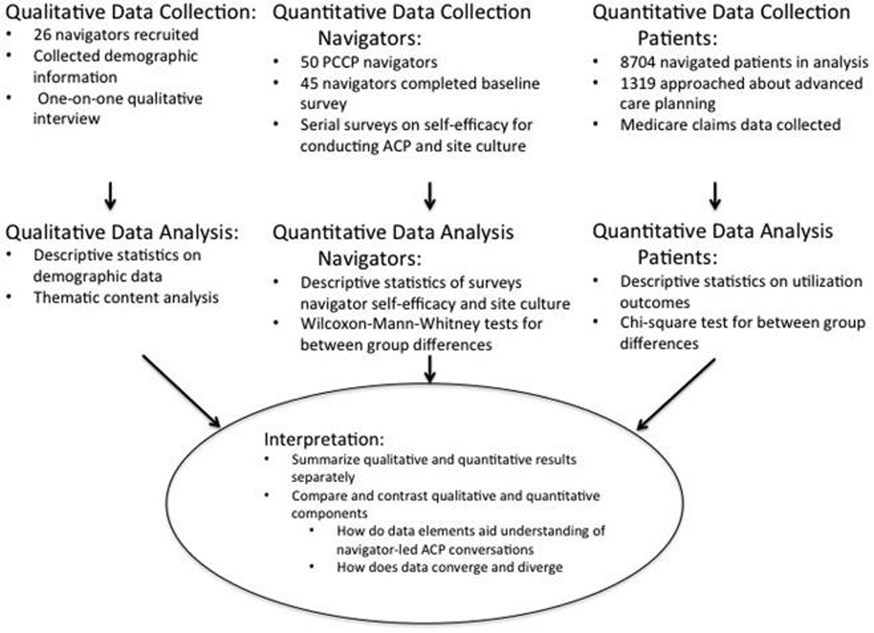
We conducted a convergent, parallel mixed-methods study to evaluate implementation of a lay navigator-led ACP that consisted of a quantitative component and a qualitative component (Figure 1).[32] The quantitative component or strand, as described in detail below, included ACP conversation timing extracted from the medical records, self-efficacy in facilitating ACP conversations and site culture as measured by self-report questionnaires, and EOL utilization outcomes abstracted from the claims data. The qualitative strand, collected within the same time frame as the quantitative strand, consisted of one-on-one interviews (n=26 PCC navigators) to elicit barriers and facilitators to navigator-led ACP. Nine authors (GR, EK, SN, JND-0, CSH, KK, KB, AW, CW) reviewed the qualitative themes derived from the navigator interviews to ascertain what additional layer of insight could complement the quantitative survey data. The rationale for this mixed-methods approach was that themes generated from qualitative interviews would provide additional insight to findings from the quantitative strand, such as specific reasons for any differences in perceived self-efficacy to facilitate ACP. This study was approved by the Institutional Review Board of the UAB.
Fig. 1.
Mixed-method study schema. PCCP = Patient Care Connect Program; ACP = advance care planning.
Respecting Choices® Training
From 6/1/14–12/31/15, 50 PCC navigators completed Respecting Choices® First Steps ACP Facilitator certification training.[33]After completing the online modules, navigators attended an in-person, 1-day certification course led by certified Respecting Choices® Instructors including the PCCP training manager (NL), director of nursing (RT), medical director (GR), and UAB’s Director for Ambulatory Palliative Care (EK). The classroom course focused on achieving competency in facilitating ACP conversations through video demonstration, instructor role modeling, role-play exercises, and feedback on competency.[31] After certification, lay navigators completed additional practice sessions using role-modeling exercises and evaluation checklists provided during training. When the navigator and site manager were comfortable with the navigator’s skill in delivering ACP conversations, navigators began engaging with patients.
Each site was allowed to choose how their navigators identified potential patients for ACP conversations. Navigators could approach patients with any stage of cancer. Several sites preferred including material on ACP in their introductory packet for new patients, whereas other sites preferred engaging with patients with whom the navigator had a previously established relationship. ACP conversations were conducted either in clinic, infusion center, or by telephone.
Quantitative Strand
Medical Record Abstraction
Timing and Frequency of ACP Conversations
Navigators recorded activities related to ACP using a navigation documentation software system. As conversations occurred over time, they were tracked as completed, in process, or declined. The frequency of ACP conversation was abstracted from navigator’s electronic records.
Navigator Questionnaires
Navigator Self-efficacy
Navigators’ self-efficacy in facilitating ACP conversations was measured in an online survey using a self-efficacy tool designed by Respecting Choices®, which is included in the program’s curriculum. The tool includes 5 items about motivation, confidence, preparedness, and skill in conducting ACP conversations. Response options ranged from 0–10 where 0 is “strongly disagree” and 10 is “strongly agree”. Pre-training self-efficacy was measured prior to Respecting Choices® First Steps ACP Facilitator certification. Post-training surveys were conducted at multiple points over 2 years to target navigators at novice stages (i.e., completed 0–9 ACP conversations) and experienced stages (i.e., completed 10+ ACP conversations). At the time of each survey, the number of completed ACP conversations was identified for each navigator. The average time between training and receipt of navigators first and last post-training surveys were 4.8 (SD 3.5) and 11.1 (SD 5.7) months, respectively. Wilcoxon-Mann-Whitney tests were used to compare baseline (pre-training) surveys to the final navigator surveys on all of the 5 items. To better understand the impact of experience on self-efficacy, we also assessed average scores reported by novice and expert navigators.
Site Culture
Five questions were added to the final post-training questionnaire pertaining to site culture, including assessment of support for navigator-led ACP by the institution, medical oncologist, other physicians, nurses, and social workers. Wilcoxon-Mann-Whitney tests were used to assess site culture surveys.
Claims-based Analysis
Patient EOL Utilization Outcomes
Medicare claims data from January 2012 through March 2015 were extracted from the Centers for Medicare & Medicaid Services Chronic Condition Data Warehouse and linked to health system data. Hospitalizations, ER visits, ICU visits, and chemotherapy were each assessed as within the last 30 days of life. Hospice use was identified as any utilization during the quarter of death. Hospitalizations, ER, and ICU were identified from inpatient and outpatient-based claims. Chemotherapy was assessed by Healthcare Common Procedure Coding System (HCPCS) codes, National Drug Codes (NDC) codes, ICD-9 procedure codes, and Berenson-Eggers Type of Service (BETOS) codes. Frequencies and percentages of utilization outcomes are presented and chi-square tests were used to assess between-group differences in resource utilization for (1) those who engaged or declined ACP and (2) reported having or not having an advance directive. All analyses were performed using SAS v.9.4 with a two-sided 0.05 level of significance.
Qualitative Strand
Navigator-Reported Barriers and Facilitators to Implementing ACPs
Navigators from 11 Patient Care Connect sites participated in one-on-one, face-to-face semi-structured interviews regarding their experiences delivering Respecting Choices® First Steps ACP conversations. One site declined participation in interviews and surveys. The interview guide was developed by coauthors (GR, EK, JND-O, RT, NL) and included questions regarding training in ACP, knowledge and comfort with delivering ACP conversations, and barriers and facilitators associated with implementation. To ensure consistency, all interviews were conducted from April-July 2015 by one member of the study team (JND-O) with expertise and experience in qualitative interviewing. After signing informed consent, participating navigators completed a demographic data form that included age, race, sex, education, religious affiliation, healthcare experience, navigation experience, and whether they had personal experience with cancer.
All interviews were audio-recorded and transcribed verbatim by a professional transcription service. Thematic analysis was conducted using QSR International’s NVivo 10 Software.[34, 35] Investigator triangulation methodology was conducted;[36, 37] the two-member analysis team (SN, CSH) with experience in qualitative methodology in social sciences disciplines (clinical psychology and medical sociology) independently reviewed transcripts through line-by-line coding. After initial categories and themes were generated in a cyclical, iterative process, the full research team refined existing categories, themes, and subthemes. Discrepancies, though infrequent, were addressed with the research team. Inter-rater agreement was assessed using Cohen’s Kappa (=0.81), indicating high agreement.[38]
Results
Quantitative Strand
Medical Record Abstraction
Timing and Frequency of ACP Conversations
From 6/1/14–12/31/15, 50 navigators initiated ACP conversations with 15% (1319/8704) of patients; 481 (36%) completed the conversation, 472 (36%) were in process at time of analysis, and 366 (28%) declined. Patient demographics are shown in Table 1. Navigator engagement varied by site, with one site completing only 6 ACP conversations and one site completing 272 conversations. In addition, individual navigators completed up to 76 conversations. At the time of navigator surveys, 12 navigators completed 10 or more ACP conversations. Navigators were more likely to approach African American patients (20% vs. 14%, p < 0.001; Table 1). African American and Caucasian patients were equally likely to participate in ACP, with 72% participating in each subset (Table 1).
Table 1.
Patient and Navigator Demographics
| Demographics of PCCP Navigated Subjects (n = 8704) | ||||||
| Completed/Pending | Refused | Not Approached | ||||
| n = 953 | % | n = 366 | % | n = 7385 | % | |
| Age at first diagnosis, yrs | ||||||
| Mean, SD | 73.3 | 7.3 | 73.0 | 7.0 | 72.9 | 7.5 |
| Age at death, yrs | ||||||
| Mean, SD | 79.6 | 7.1 | 76.0 | 6.8 | 76.1 | 7.1 |
| Gender | ||||||
| Female | 480 | 51.7 | 205 | 56.5 | 3840 | 53.2 |
| Male | 448 | 48.3 | 158 | 43.5 | 3373 | 46.8 |
| Race | ||||||
| Black | 167 | 18.1 | 64 | 17.9 | 913 | 12.7 |
| Other | 6 | 0.7 | 6 | 1.7 | 112 | 1.6 |
| White | 751 | 81.3 | 288 | 80.5 | 6166 | 85.8 |
| Comorbidity score | ||||||
| Mean, SD | 2.5 | 2.2 | 2.31 | 2.2 | 2.27 | 2.3 |
| Score-category | ||||||
| 0 | 186 | 20.2 | 81 | 22.6 | 1843 | 25.7 |
| 1 | 192 | 20.9 | 80 | 22.4 | 1601 | 22.3 |
| 2–3 | 285 | 30.9 | 106 | 29.6 | 1961 | 27.3 |
| 4+ | 258 | 28.0 | 91 | 25.4 | 1769 | 24.7 |
| High acuitya | ||||||
| Yes | 359 | 37.7 | 136 | 37.2 | 183 | 38.1 |
| Demographics of Deceased PCCP Navigated Subjects (n = 2752) | ||||||
| Completed/Pending | Refused | Not Approached | ||||
| n = 437 | % | n = 171 | % | n = 2144 | % | |
| Age at first diagnosis, yrs | ||||||
| Mean, SD | 74.2 | 7.4 | 74.1 | 7.2 | 73.9 | 7.7 |
| Age at death, yrs | ||||||
| Mean, SD | 76.6 | 7.1 | 76.0 | 6.8 | 76.1 | 7.1 |
| Gender | ||||||
| Female | 188 | 44.0 | 82 | 48.2 | 905 | 43.0 |
| Male | 239 | 56.0 | 88 | 51.8 | 1199 | 57.0 |
| Race | ||||||
| Black | 84 | 19.6 | 26 | 15.3 | 276 | 13.1 |
| Other | 2 | 0.5 | 3 | 1.8 | 27 | 1.3 |
| White | 342 | 79.9 | 141 | 82.9 | 1811 | 85.7 |
| Comorbidity score | ||||||
| Mean, SD | 3.0 | 2.3 | 2.9 | 2.3 | 3.0 | 2.5 |
| Score-category | ||||||
| 0 | 53 | 12.4 | 24 | 14.1 | 313 | 14.9 |
| 1 | 86 | 20.2 | 28 | 16.5 | 386 | 18.3 |
| 2–3 | 139 | 32.6 | 60 | 35.3 | 633 | 30.1 |
| 4+ | 148 | 34.7 | 58 | 34.1 | 774 | 36.8 |
| High acuitya | ||||||
| Yes | 226 | 51.7 | 97 | 56.7 | 1234 | 57.6 |
| Demographics of Navigators (n = 26) | ||||||
| Age, yrs | ||||||
| Mean, SD | 44.7 | 13.5 | ||||
| Gender | ||||||
| Female | 21 | 80.8 | ||||
| Male | 5 | 19.2 | ||||
| Race | ||||||
| Black | 10 | 38.5 | ||||
| Other | 1 | 3.9 | ||||
| White | 15 | 57.7 | ||||
| Education | ||||||
| High school or GED | 1 | 3.9 | ||||
| Some college, vocational or technical school | 5 | 19.2 | ||||
| College graduate (four years) | 14 | 53.9 | ||||
| Masters | 6 | 23.1 | ||||
| Religious affiliation | ||||||
| Protestant | 18 | 69.2 | ||||
| Nondenominational | 4 | 15.4 | ||||
| Catholic | 1 | 3.9 | ||||
| No religious affiliation | 1 | 3.9 | ||||
| Other | 2 | 7.7 | ||||
| Navigator experience, yrs | ||||||
| Mean (range) | 2.07 (0.7–2.3) | |||||
| SD | 1.9 | |||||
| Prior employment in healthcare | ||||||
| Yes | 23 | 88.5 | ||||
| No | 3 | 11.5 | ||||
| Personal experience with cancer | ||||||
| Yes, I have a family member with cancer | 18 | 64.3 | ||||
| Yes, I have a friend with cancer | 5 | 17.9 | ||||
| No | 4 | 14.3 | ||||
| Other | 1 | 3.6 | ||||
PCCP = Patient Care Connect Program; GED = General Educational Development.
High-acuity cancer defined as cancers of the brain, pancreas, ovaries, lung, and head & neck or any stage IV cancer.
Navigator Questionnaires
Navigator Self-efficacy
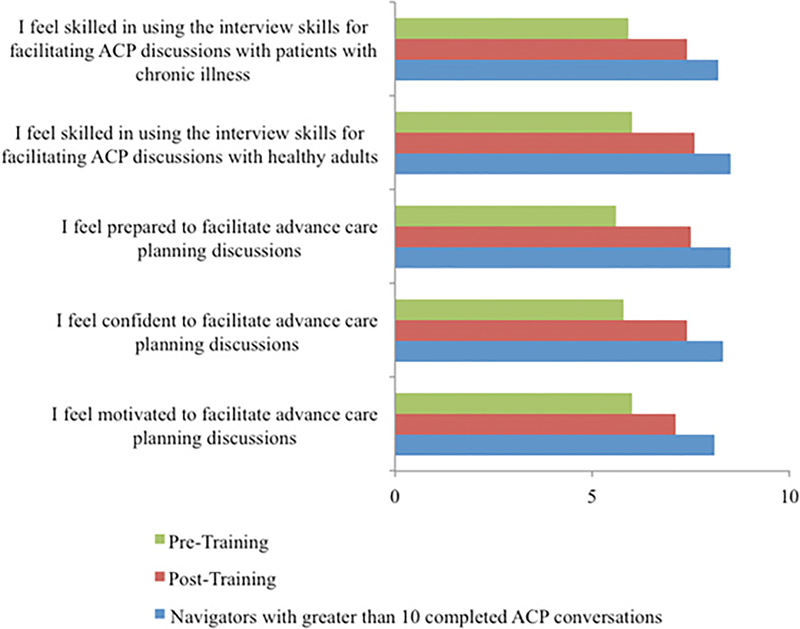
Forty-five of the 50 navigators trained participated in the baseline survey; 33 navigators (73%)completed at least one follow-up survey. The maximum number of follow-up surveys was 3. Four of five elements of self-efficacy significantly increased from baseline to the last completed survey (all p<.05, Figure 2). At baseline, the mean score for feeling prepared to conduct ACP conversations was 5.6, which increased to 7.5 at the last survey (p < 0.001). Navigators completing 10 or more conversations were considered experienced, based on feedback from both trainers and navigators. The experienced navigators had a trend toward higher self-efficacy than navigators with <10 conversations (novice) (Figure 2).
Fig. 2.
Self-efficacy results. ACP = advance care planning.
Site culture
Navigators who completed 10 or more conversations (n= 12) were more likely to report support from their institutions for conducting ACP conversations (8.6 vs 6.5, p = 0.02). They also reported more support for their role from medical oncologists (8.3 vs 6.0, p = 0.03) and nursing staff (8.0 vs 5.5, p = 0.05). Support from social workers (7.4 vs 8.5, p = 0.23) and other physicians (7.5 vs. 4.5, p=0.13) were similar for experienced navigators and novice navigators.
Claims-based Analysis
Resource Utilization in Patient Completing ACPs
2752 deceased patients were included in the analysis; 437 participated in ACP; 171 declined, and 2144 were not approached. Patients who started or completed an ACP discussion with a navigator had significantly lower hospitalization rates (46% vs 56%; p = 0.02). Trends were observed toward lower chemotherapy use (14% vs 19%, p =0.17), fewer ICU admission (18% vs 24%; p = 0.07), and fewer ER visits in the last 30 days of life (46% vs 53%; p = 0.08) for patients engaging in ACP than those who declined. Hospice use at the EOL was similar (68% vs. 71%; p =0.47; Table 3).
Table 3.
Barriers and Facilitators to Navigator-Led Advance Care Planning Conversations Emerged From Semistructured Interviews
| Categories | Theme | Subtheme | Selected Quotes |
|---|---|---|---|
| Patient-level | Barriers | Limited health literacy | “Sure, they're anxious about usually whether or not they want to be on what they deem to be life-supportive equipment or whether they want a CPR. It kinda gets into the medical jargon.” [NV#05] |
| Fear | “It's amazing how much fear—and I'm gonna tell ya something crazy that I see all the time. How much fear of cancer and how much fear of dying that these patients have” [NV#22] | ||
| Battle mode | “My experience has been that people come to the hospital wanting their lives to be saved. Either in survivorship, so they were kind of distanced from it and didn't wanna engage too much in cancer conversation, or they were in more or less battle mode. Still trying to receive treatment to the very end … there was still an avoidance of not being fully engaged in the conversation.” [NV#16] | ||
| Facilitators | Prior exposure to death or advance care planning | “If they have experienced someone who have not had an advance directive, and something happen, and it's like a big family feud— that helps. Oh, no, we're not going through this. We're going to get this in writing, and that's it.” [NV#02] | |
| Navigator-level | Barriers | Identify best timing | “Knowing exactly when is a good time to bring it up. I think that's a barrier cuz you never can tell what place somebody is in at that time. You may bring it up this day and they don't want anything to do with it … I guess the barrier of just knowing when to present it.” [NV#01] |
| Personal discomfort | “The difficulty is just dealing with somewhat your own—not issues, but your own reserves about this.” [NV#03] | ||
| Facilitators | Respect patient readiness | “I formulated a way where I could do it where I felt that I wasn't pressuring them because it just—it has the title of Respecting Choices, and that's exactly what it needs to be, their choice.” [NV#06] | |
| Establish rapport and trust | “Of course, all of these patients, as I've stated earlier, have a relationship with me. Have rapport with me. I have seen them several times previously before I bring it up, so they know who I am and what I look like. They trust me. I have a rapport with them. I'm established with them.” [NV#24] | ||
| Continues follow-up | “I'll explain the type of services I can offer. The first time I may just mention it and tell them that one of the things that we can offer is advance care planning and we can talk about that another time if you're more interested.” [NV#14] | ||
| System-level | Barriers | Lack of time and space | “it's just hard to deliver given our time with the patient and actually space to actually have a private conversation with them. We don't really have the space for it. Overall, the program is a great thing to have and to put in place. It's just hard to execute it.” [NV#01] |
| Lack of stakeholder support | “… when certain initiatives are pushed, it's always pushback because it's something new or it's something that, at that time, a lot of providers or nurses or people that work in clinics don't agree with, but yet they won't give an ear to it. They don't even give it a chance, to say, ‘Okay, well, we'll try it,’ or, ‘We'll be behind this,’ or, ‘It will work.’” [NV#03] | ||
| Cultural suspicion | “I think it's just—there's a cultural suspicion about it … they call people who would discuss these things like death panels … I don't know if that's just our region or whatever … the difficulty is, I think, getting people to understand this is for their benefit.” [NV#21] | ||
| Facilitators | Physician engagement | “I want to get into the clinics and I want to have where the doctor will say to the patient, ‘Your navigator is gonna come in, and they're gonna cover all of this, including advance directive, and I think that everybody should get it done.’” [NV#19] | |
| Referral or consultation support | “… if they start askin' questions that I'm not sure of, then I'll get a nurse that we work—we'll get her. I'll ask her questions, and I'll come back to ‘em. I mean, if there's medical questions I'm not sure of. A lot of them—I've had one that would ask about, well, how long would they keep feeding me before they would turn me off or whatever … I wasn't sure, so I went and got an MD to answer the question for me.” [NV#12] |
Qualitative Strand
Navigator Characteristics
Navigators (N=26) participating in interviews were predominantly female (81%), with college or advanced degrees (77%), and had an average of 2 years of navigation experience. Thirty-nine percent were African American. The majority had personal experience with cancer (86%), either with family or friends or as a survivor (Table 1).
Navigator Identified Barriers and Facilitators to Care
During interviews, navigators identified multi-level barriers and facilitators to conducting ACP conversations (Table 2). Three domains of Facilitators and Barriers emerged: patient, navigator, and system domains. At the patient level, prior exposure to ACP, such as witnessing family conflicts due to the lack of an AD, enhanced their openness to engage in ACP conversations. Barriers included limited health literacy, fears, lack of readiness, and a “battle” mentality. At the navigator level, key facilitators included established rapport, patient readiness, and the ability to engage in continuous follow-up. Navigators reported challenges identifying the best timing to initiate ACP conversations with different cancer stages and prognosis. Some navigators also noted they did not feel comfortable initiating the conversation due to personal reservations about discussing death and dying. System facilitators included physician introduction of navigators to patients as part of the ACP process and establishment of a referral or consultation support system to support navigator-led ACP conversations facilitated implementation. System barriers included lack of time and space specifically designated for ACP conversations, lack of stakeholder buy-in, and cultural suspicion linking ACP facilitators as “death panels.”
Table 2.
Healthcare Utilization Among Decedents According to Advance Directive and Respecting Choices First Steps ACP Facilitator Status
| Completed/In Process | Declined | P-value | |||
|---|---|---|---|---|---|
| n = 437 | % | n = 171 | % | ||
| ER visit within 14 days of death | 146 | 33.4 | 72 | 42.1 | 0.04 |
| ER visit within 30 days of death | 199 | 45.5 | 91 | 53.2 | 0.09 |
| ICU visit within 14 days of death | 64 | 14.7 | 34 | 19.9 | 0.11 |
| ICU visit within 30 days of death | 77 | 17.6 | 41 | 24.0 | 0.07 |
| Hospitalization within 14 days of death | 159 | 36.4 | 75 | 43.9 | 0.09 |
| Hospitalization within 30 days of death | 200 | 45.8 | 96 | 56.1 | 0.02 |
| Hospice less than three daysa | 20 | 6.6 | 11 | 9.1 | 0.37 |
| Any hospice useb | 296 | 67.7 | 121 | 70.8 | 0.47 |
| Chemotherapy within 30 days of death | 62 | 14.2 | 32 | 18.7 | 0.17 |
ER = emergency room; ICU = intensive care unit.
P-values are from χ2 test.
Proportion of subjects in last quarter of life that who had hospice and were enrolled for less than three days before death.
In the quarter of death.
Mixed Methods Findings
The qualitative and quantitative analysis were confirmatory, without evidence of divergence. Wide variation in navigator experiences and self-efficacy were reflected in this surveys and interviews, as well as the number of completed ACP conversations (range 0–76). The qualitative themes revealed that oncologist engagement and personal comfort of both navigators and patient readiness to discuss EOL played a large role in navigator perception of their role and desire to complete ACPs. Concerns expressed during interviews regarding clinical staff buy-in were substantiated by the site culture survey, where experienced navigators more often reported support from both administration and collaborating physicians. Navigators reported lower levels of support from nurses and social workers than physicians. This corresponded to the qualitative analysis where navigators expressed concern about roles and responsibilities of navigators compared to the social workers and nurses, including whether or not ACP should fall within the scope of these clinical providers instead of the navigator.
Discussion
To our knowledge, this is the first published report of training and engaging lay navigators to perform ACP conversations. Our results demonstrated that lay healthcare navigators or similar community health workers can be successfully trained and can confidently facilitate Respecting Choices® First Steps ACP conversations. Initiation of an ACP conversation with a navigator was associated with fewer hospitalizations and trends toward lower ER visits, and ICU admissions at the EOL. This finding is consistent with previous literature indicating that ACP conversations lead to improved quality of care and decreased aggressiveness of care at EOL.[12, 39]
The time intensive nature of ACP limits integration into physician and nursing practice.[14] However, navigators are able to spend greater time focused on ACP. In our program, only about a quarter of patients approached by navigators for ACP conversations declined to have them, thus demonstrating that this model is acceptable for patients. Moreover, navigator self-efficacy to facilitate ACP conversations improved with training and experience. Self-efficacy improved after a 6-hour set of online didactic modules and a 1-day in-person training. This suggests that a systematic training curriculum, such as Respecting Choices® First Steps, is an approach that supports wide dissemination to other health systems using navigators. Furthermore, navigator self-efficacy increased even further with experience in delivering ACP conversations.
It is noteworthy that this program was implemented in a Deep South “bible belt” region, where strong religious beliefs and community involvement play an important role in health care decision making and EOL care planning, particularly among African American population.[40–42] PCCP navigators are hired from within their communities and 38.5% of navigators were African American. Lay navigators may be ideally positioned to provide culturally sensitive ACP for the communities they serve, which is supported by higher engagement with the African American population in this study. This population has been historically difficult to access for ACP interventions due to mistrust of the medical community;[43, 44] however in this study, African American patients were as likely to complete ACP as their Caucasian counterparts. These findings are highly relevant to other community-based population health management strategies employing lay community health-workers as front-line care delivery personnel.
Implementation of navigator-led ACP appeared to be significantly affected by system factors, particularly oncology provider buy-in and infrastructure support. Our findings are consistent with previous work showing that effective leadership is important for successful program implementation.[45, 46] Oncologist endorsement of the navigator as part of the care-team may increase patient uptake of these conversations. Patients may be more receptive to participating in ACP discussions with navigators when oncology providers communicate to patients the navigator’s role in this conversation. Appreciation of the multi-level components, catalysts, and synergies of a system wide implementation to improve ACP will be essential to the replication of positive results. Future work should explore the impact that provider and clinical staff engagement has on enhancing buy-in prior to implementing navigator-led ACP.
This mixed methods study had some limitations. Data were initially collected for training purposes, which resulted in an inability to identify individual’s baseline survey responses, and we do not have complete demographic information on all navigators who were trained to facilitate ACP conversations. However, the demographic data collected at the time of the interviews was felt to be representative of the navigator population. Another limitation is the potential reporting bias due to more engaged, experienced navigators being more likely to respond to the survey and report higher self-efficacy, limiting ability to make causal inferences. In addition, the sites utilized varied approaches for targeting patients. Thus, further investigation of the navigator experience is warranted with a larger number of health systems and navigators. In addition, although we utilized the self-efficacy survey used by Respecting Choices® First Steps ACP Instructors throughout the country, little data is published and available for comparison. Evaluation of patient outcomes is limited by incomplete information on the entire navigated population, as not all patients were asked to engage in ACPs. We also did not capture why patients declined to participate in ACPs. We did not track the paper advanced directive documents or how these documents were used for specific patients at the end of life, as each institution had different methods to store such documents; thus the ability to evaluate alignment of care with patient preference was not possible. We prioritized “advance care planning”, rather than completion of a specific advance directive, as this has been shown to impact patient outcomes.[10] The limited sample size in some comparisons increases the risk that important trends are statistically non-significant due to type 2 error. There may be inherent differences in patients who decline ACP discussions.
Despite these limitations, the data suggests a benefit to navigator-initiated ACPs in terms of fewer ICU stays and hospitalizations and trends in a number of other outcomes. Expansion of the role of the lay navigator or other community health workers to initiate ACPs may be an option for engaging a greater number of patients in ACPs.
Conclusions
Training navigators to facilitate Respecting Choices® First Steps ACP conversations is feasible, with improvements in navigator self-efficacy scores after training. Navigator uptake of the program is facilitated by physician and administrator engagement. Further work is needed to understand the cost-effectiveness of training lay personal as ACP facilitators, the role of other healthcare providers in ACPs, contributing factors to enhance space, time, and staff support from health care systems, and impact on patient experiences and health outcomes.
Disclosures and Acknowledgements
We would like to acknowledge the Patient Care Connect Group for their contribution to this project and manuscript. This publication was made possible by Grant Number 1C1CMS331023 from the Department of Health and Human Services, Centers for Medicare & Medicaid Services. The research presented was conducted by the awardee. Results may or may not be consistent with or confirmed by the findings of the independent evaluation contractor. The contents of this publication are solely the responsibility of the authors and do not necessarily represent the official views of the U.S. Department of Health and Human Services or any of its agencies. Dr. Rocque is supported by a Walter B. Frommeyer, Jr. Fellowship in Investigative Medicine. This funding source had no role in the design and conduct of the study; collection, management, analysis, or interpretation of the data; and preparation, review, or approval of the manuscript for publication.
Role of Funding Source: This study was funded by the Center for Medicare and Medicaid Innovation. The sponsor had no role in the design, conduct, or interpretation of results.
References
- 1.Peppercorn JM, et al. , American society of clinical oncology statement: toward individualized care for patients with advanced cancer. J Clin Oncol, 2011. 29(6): p. 755–60. [DOI] [PubMed] [Google Scholar]
- 2.Medicine, I.o., Dying in America: Improving Quality and Honoring Individual Preferences Near the End of Life, ed. T.N.A. Press; 2014, Washington D.C. [Google Scholar]
- 3.Silveira MJ, Wiitala W, and Piette J, Advance directive completion by elderly Americans: a decade of change. J Am Geriatr Soc, 2014. 62(4): p. 706–10. [DOI] [PubMed] [Google Scholar]
- 4.Organization, N.H.a.P.C. Advance Care Planning. 2016. [cited 2016 3/9/16]; Available from: http://www.nhpco.org/advance-care-planning.
- 5.Detering KM, et al. , The impact of advance care planning on end of life care in elderly patients: randomised controlled trial. BMJ, 2010. 340: p. c1345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Khandelwal N, et al. , Estimating the effect of palliative care interventions and advance care planning on ICU utilization: a systematic review. Crit Care Med, 2015. 43(5): p. 1102–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dionne-Odom JN, et al. , Benefits of Early Versus Delayed Palliative Care to Informal Family Caregivers of Patients With Advanced Cancer: Outcomes From the ENABLE III Randomized Controlled Trial. J Clin Oncol, 2015. 33(13): p. 1446–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wright AA, et al. , Associations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment. JAMA, 2008. 300(14): p. 1665–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Houben CH, et al. , Efficacy of advance care planning: a systematic review and meta-analysis. J Am Med Dir Assoc, 2014. 15(7): p. 477–89. [DOI] [PubMed] [Google Scholar]
- 10.Narang AK, Wright AA, and Nicholas LH, Trends in Advance Care Planning in Patients With Cancer: Results From a National Longitudinal Survey. JAMA Oncol, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tang ST, et al. , Physician-patient end-of-life care discussions: correlates and associations with end-of-life care preferences of cancer patients-a cross-sectional survey study. Palliat Med, 2014. 28(10): p. 1222–30. [DOI] [PubMed] [Google Scholar]
- 12.Mack JW, et al. , Associations between end-of-life discussion characteristics and care received near death: a prospective cohort study. J Clin Oncol, 2012. 30(35): p. 4387–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bernacki RE, Block SD, and F. American College of Physicians High Value Care Task, Communication about serious illness care goals: a review and synthesis of best practices. JAMA Intern Med, 2014. 174(12): p. 1994–2003. [DOI] [PubMed] [Google Scholar]
- 14.Lund S, Richardson A, and May C, Barriers to advance care planning at the end of life: an explanatory systematic review of implementation studies. PLoS One, 2015. 10(2): p. e0116629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Liu PH, et al. , Physicians’ propensity to discuss prognosis is associated with patients’ awareness of prognosis for metastatic cancers. J Palliat Med, 2014. 17(6): p. 673–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.A controlled trial to improve care for seriously ill hospitalized patients. The study to understand prognoses and preferences for outcomes and risks of treatments (SUPPORT). The SUPPORT Principal Investigators. JAMA, 1995. 274(20): p. 1591–8. [PubMed] [Google Scholar]
- 17.Goodman E, The Conversation Project. 2013.
- 18.Barnato AE, et al. , Racial and ethnic differences in preferences for end-of-life treatment. J Gen Intern Med, 2009. 24(6): p. 695–701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Loggers ET, et al. , Racial differences in predictors of intensive end-of-life care in patients with advanced cancer. J Clin Oncol, 2009. 27(33): p. 5559–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fashoyin-Aje LA, Martinez KA, and Dy SM, New patient-centered care standards from the commission on cancer: opportunities and challenges. J Support Oncol, 2012. 10(3): p. 107–11. [DOI] [PubMed] [Google Scholar]
- 21.Center for Medicare and Medicaid Services. Oncology Care Model. 2015. [cited 2015 2/14/15]; Available from: http://innovation.cms.gov/initiatives/Oncology-Care/.
- 22.Paskett ED, Harrop JP, and Wells KJ, Patient navigation: an update on the state of the science. CA Cancer J Clin, 2011. 61(4): p. 237–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Carroll JK, et al. , Patients’ experiences with navigation for cancer care. Patient Educ Couns, 2010. 80(2): p. 241–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rocque GB, et al. , The Patient Care Connect Program: Transforming Health Care Through Lay Navigation. J Oncol Pract, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rocque GB, et al. , Guiding Lay Navigation in Geriatric Patients With Cancer Using a Distress Assessment Tool. J Natl Compr Canc Netw, 2016. 14(4): p. 407–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kirchhoff KT, et al. , Effect of a disease-specific advance care planning intervention on end-of-life care. J Am Geriatr Soc, 2012. 60(5): p. 946–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Boettcher I, Turner R, and Briggs L, Telephonic advance care planning facilitated by health plan case managers. Palliat Support Care, 2015. 13(3): p. 795–800. [DOI] [PubMed] [Google Scholar]
- 28.Lyon ME, et al. , A longitudinal, randomized, controlled trial of advance care planning for teens with cancer: anxiety, depression, quality of life, advance directives, spirituality. J Adolesc Health, 2014. 54(6): p. 710–7. [DOI] [PubMed] [Google Scholar]
- 29.Lyon ME, et al. , Family-centered advance care planning for teens with cancer. JAMA Pediatr, 2013. 167(5): p. 460–7. [DOI] [PubMed] [Google Scholar]
- 30.Schellinger S, Sidebottom A, and Briggs L, Disease specific advance care planning for heart failure patients: implementation in a large health system. J Palliat Med, 2011. 14(11): p. 1224–30. [DOI] [PubMed] [Google Scholar]
- 31.Respecting Choices. Respecting Choices® Advance Care Planning. [cited 2016 5/17/2016]; Available from: http://www.gundersenhealth.org/respecting-choices.
- 32.Creswell J C.P., Designing and Conducting Mixed Methods Research, 2nd Edition. 2011, Washington DC: Sage Publications, Inc. [Google Scholar]
- 33.Pecanac KE, et al. , Respecting Choices(R) and advance directives in a diverse community. J Palliat Med, 2014. 17(3): p. 282–7. [DOI] [PubMed] [Google Scholar]
- 34.Braun V, C.V., Using thematic analysis in psychology, in Qual Res Psychol.
- 35.NVivo qualitative data analysis Software. Vol. Version 10. 2012: QSR International Pty Ltd. [Google Scholar]
- 36.Thurmond VA, The point of triangulation. J Nurs Scholarsh, 2001. 33(3): p. 253–8. [DOI] [PubMed] [Google Scholar]
- 37.Giacomini MK and Cook DJ, Users’ guides to the medical literature: XXIII. Qualitative research in health care B. What are the results and how do they help me care for my patients? Evidence-Based Medicine Working Group. JAMA, 2000. 284(4): p. 478–82. [DOI] [PubMed] [Google Scholar]
- 38.Viera AJ and Garrett JM, Understanding interobserver agreement: the kappa statistic. Fam Med, 2005. 37(5): p. 360–3. [PubMed] [Google Scholar]
- 39.Lopez-Acevedo M, et al. , Timing of end-of-life care discussion with performance on end-of-life quality indicators in ovarian cancer. Gynecol Oncol, 2013. 130(1): p. 156–61. [DOI] [PubMed] [Google Scholar]
- 40.Sanders JJ, Robinson MT, and Block SD, Factors Impacting Advance Care Planning among African Americans: Results of a Systematic Integrated Review. J Palliat Med, 2016. 19(2): p. 202–27. [DOI] [PubMed] [Google Scholar]
- 41.Johnson KS, Elbert-Avila KI, and Tulsky JA, The influence of spiritual beliefs and practices on the treatment preferences of African Americans: a review of the literature. J Am Geriatr Soc, 2005. 53(4): p. 711–9. [DOI] [PubMed] [Google Scholar]
- 42.Waters CM, Understanding and supporting African Americans’ perspectives of end-of-life care planning and decision making. Qual Health Res, 2001. 11(3): p. 385–98. [DOI] [PubMed] [Google Scholar]
- 43.Johnson KS, Kuchibhatla M, and Tulsky JA, What explains racial differences in the use of advance directives and attitudes toward hospice care? J Am Geriatr Soc, 2008. 56(10): p. 1953–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Koss CS and Baker TA, Race Differences in Advance Directive Completion: The Narrowing Gap Between White and African American Older Adults. J Aging Health, 2016. [DOI] [PubMed] [Google Scholar]
- 45.McFadden KL, Stock GN, and Gowen CR 3rd, Leadership, safety climate, and continuous quality improvement: impact on process quality and patient safety. J Nurs Adm, 2014. 44(10 Suppl): p. S27–37. [DOI] [PubMed] [Google Scholar]
- 46.Kelloway EK, Mullen J, and Francis L, Divergent effects of transformational and passive leadership on employee safety. J Occup Health Psychol, 2006. 11(1): p. 76–86. [DOI] [PubMed] [Google Scholar]